Table of Contents - Issue
Recent articles
-
Substance Use Prevention: Knowledge, Attitude and Practices among Secondary School Workers in Enugu StateAuthor: Chinwe F.S EzeruigboDOI: 10.21522/TIJPH.2013.11.04.Art001
Substance Use Prevention: Knowledge, Attitude and Practices among Secondary School Workers in Enugu State
Abstract:
The phase of adolescence holds significant importance as it marks a critical period for initiating habits that can have enduring effects. This is crucial in preventing avoidable illnesses and fatalities resulting from unfavorable health-related actions, like the use of substances. This current research was conducted to assess the understanding, perspectives, and actions of secondary school educators regarding the prevention of substance use among adolescents. This initiative seeks to identify factors that might impede the efficacy of substance use prevention programs within secondary educational institutions. Descriptive research design was carried out in three select secondary schools: Uwani Secondary School, Maryland Secondary School, and Federal Government College Enugu, in Enugu state. Ninety-two (92) participants were sampled using a multi-stage sampling technique. The self-administering questionnaire was used as a tool for data gathering. The filled questionnaires that met the criteria for analysis were coded into the computer using SPSS software and data were analyzed using descriptive statistics and presented in frequency and percentage. Knowledge of the attributes that increase the risk of adolescent substance use is poor at 88% of the respondents, while attitude and practice were fair. The knowledge of attitudes and practices of secondary school teachers in Enugu state on the preventive measures for substance use among adolescents is inadequate. Therefore, for effective intervention on substance use preventive strategies in adolescents, teachers and other workers in secondary schools should be equipped with adequate knowledge concerning substance use preventive practice.
Keywords: Attitude; Enugu State; Knowledge; Practices; Substance use prevention; Secondary school workers.Substance Use Prevention: Knowledge, Attitude and Practices among Secondary School Workers in Enugu State
References:
[1] Azuike, R., Oni, A. & Dirisu, O. (2012). Stakeholders’ view on substance abuse and the development of effective and sustainable interventions in Nigeria: findings from a consultative forum. Retrieved on the 5/April 2020, accessed from: http://www.freedomfoundationng.org/userfiles/Stakeholders%27%20views.pdf.
[2] Romer, D., Reyna, V. F., & Satterthwaite, T. D. (2017). Beyond stereotypes of adolescent risk taking: Placing the adolescent brain in developmental context. Developmental Cognitive Neuroscience, 27, 19–34. https://doi.org/10.1016/j.dcn.2017.07.007.
[3] Santelli, J. S., Baldwin, W., & Heitel, J. (2015). Rising wealth, improving health? Adolescents and inequality. Lancet (London, England), 385(9982), 2026–2028. https://doi.org/10.1016/S0140-6736(14)61892-4.
[4] Selemon, L. (2013). A role for synaptic plasticity in the adolescent development of executive function. Transl Psychiatry 3, e238. https://doi.org/10.1038/tp.2013.7.
[5] Smith, A. R., Chein, J., & Steinberg, L. (2014). Peers increase adolescent risk taking even when the probabilities of negative outcomes are known. Developmental Psychology, 50(5), 1564–1568. https://doi.org/10.1037/a0035696.
[6] van den Bos, W., & Hertwig, R. (2017). Adolescents display distinctive tolerance to ambiguity and to uncertainty during risky decision making. Sci Rep 7, 40962. https://doi.org/10.1038/srep40962.
[7] WHO (2013). Substance abuse. Accessed from: https://www.afro.who.int/health-topics/substance-abuse.
[8] UNODC (2018), Drug Use in Nigeria, United Nations Office on Drugs and Crime, Vienna.
[9] Mehanović, E., Virk, H. K., Akanidomo, I., Pwajok, J., Prichard, G., van der Kreeft, P., & Vigna-Taglianti, F. (2020). Correlates of cannabis and other illicit drugs use among secondary school adolescents in Nigeria. Drug and Alcohol Dependence, 206, 107457.
[10] Unplugged Nigeria Coordination group (2019). An effective school-based program for the prevention of substance use among adolescents. EU-Dap – European drug addiction prevention trial - final technical report n.1, Turin, Italy. www.eudap.net.
[11] Ogba, F. N., & Igu, N. C. (2019). Violence in Nigerian secondary schools: Implications for educational management and sustainable development. In School Violence in International Contexts (pp. 57-70). Springer, Cham.
[12] Abasiubong, F.U, John, U.A, Idung, A., & Udoh, S., Jombo, H.E. (2014). Pattern of psychoactive substance use in the northern region of Nigeria. 13. 107-115.
[13] Hecker, L. L. (2015). Ethical, legal, and professional issues in marriage and family therapy. In J. L. Wetchler & L. L. Hecker (Eds.), An introduction to marriage and family therapy (pp. 505–545). Routledge/Taylor & Francis Group.
[14] Sprinthall, Norman.A., & Collins, W.Andrew., (1995). Adolescent Psychology: A Developmental View. (3rd ed). McGraw-Hill Inc.
[15] Gaik, L.P., Abdullah, M.C., Elias, H., & Uli, J. (2010). Development of antisocial behaviour. Procedia Social and Behavioral Sciences. 7(C): 383–388. doi: 10.1016/j.sbspro.2010.10.052.
[16] Oketch, S. (2008). Understanding and Treating Drug Abuse. Nairobi: Queenex Holdings Ltd.
[17] Patterson, E. (2021). History of drug abuse. American addiction centers. Accessed from: https://drugabuse.com/addiction/history-drug-abuse/.
[18] Patterson, G.R. (1992). Developmental changes in antisocial behaviour. In R.D. Peters, R.J. MacMahon & V.L. pdfs/qualitativerep.pdf.
[19] Olaniyi, D.T. (2020). Substance Abuse and criminal behavior among commercial vehicle drivers in Lagos state. Forensis Research and Criminology International journal. 8(1), PP42-50.
[20] Black, D. (2006). What Causes Antisocial Personality Disorder? Psych Central. Accessed from: http://psychcentral.com/lib/.
[21] U.S. Department of Health and Human Services, Office of the Surgeon General. (November 2016). Facing Addiction in America: The Surgeon General’s Report on Alcohol, Drugs, and Health. Washington, DC.
[22] Handrianto, C., Jusoh, A. J., Choo, P. G. S., Abdul Rashid, N., Rahman, M. A. (2020). The Role of Teachers in Drug Abuse Prevention in Schools. International Journal of Academic Research in Business and Social Sciences. 10(11), 708-716.
[23] Moreira, A., Vóvio, C. L., & Micheli, D. D. (2015). Drug abuse prevention in school: challenges and possibilities for the role of the educator. Educação e Pesquisa, 41(1), 119-135. https://doi.org/10.1590/S1517-97022015011670.
[24] Chan, Y. F., Sidhu, G. K., Lim, P. C., & Wee, E. H. (2016). Students’ Perceptions of Substance Abuse Among Secondary School Students in Malaysia. Pertanika Journal of Social Sciences & Humanities, 24(2).
[25] Razali, A., & Madon, Z. (2016). Issues and challenges of drug addiction among students in Malaysia. Advances in Social Sciences Research Journal, 3(8). doi: 10.14738/assrj.38.2126.
[26] Reckless, W.C. (1967). The Crime Problem, Fourth Edition. New York, NY: Appleton-Century Crofts.
[27] Kennedy, J.P. (2015). Losing Control: A Test of Containment Theory and Ethical Decision Making. International Journal of Criminal Justice Sciences. 10 (1): 48–64.
[28] Obidile, Ifeoma & Stella, Chinyere & Helen e, Uzoekwe & Akuezuilo, Juliana. (2017). Perceived factors influencing academic performance of students in accounting in secondary schools in Anambra State. IOSR Journal of Humanities and Social Science. 22. 96-99. 10.9790/0837-2202039699.
[29] Odo, A. N., Samuel, E. S., Nwagu, E. N., Nnamani, P. O., Atama, C. S. (2018). Sexual and reproductive health services (SRHS) for adolescents in Enugu state, Nigeria: a mixed-methods approach, BMC Health Serv. Res. 18 (1) 92, https://doi.org/10.1186/s12913-017-2779-x.
[30] Al Gharsan, M & Alarfaj, I. (2019). Knowledge and practice of secondary school teachers about first aid. J Fam Med Prim Care. 8(5):1587–93. https://doi.org/10.4103/jfmpc.jfmpc_76_19.
[31] Yunos R. (2019). Knowledge, attitude, and practice of first aid among primary school teachers in petaling Jaya.
[32] Al-Tameemi, H. & Khudair, F. (2016). Knowledge and attitudes of primary school teachers toward first aid in Al-Najaf Al-Ashraf City. Int J Curr Res Acad Rev.4(12):64–79. https://doi.org/10.20546/ijcrar.2016.412.006.
[33] Taklual, W., Mekie, M. & Yenew, C. (2020). Determinants of First Aid Knowledge and Basic Practice Among Elementary School Teachers in Debre Tabor Town, Northcentral Ethiopia. Open Public Health J.13(1):380–7.
[34] Ganfure, G., Ameya, G., Tamirat, A., Lencha, B. & Bikila, D. (2018). First aid knowledge, attitude, practice, and associated factors among kindergarten teachers of Lideta sub-city Addis Ababa, Ethiopia. Plos one.13(3): e0194263. https://doi.org/10.1371/journal.pone.0194263.
[35] Mirwanti, R, (2017). Editor Attitude and knowledge of elementary school teachers towards first aid on emergency condition in children. Int Conf Disaster Manage Infect Control; 17:1–10.
[36] Midani, O., Tillawi, T., Saqer, A., Hammami, M. B., Taifour, H. & Mohammad, H. (2019). Knowledge and attitude toward first aid: a cross-sectional study in the United Arab Emirates. Avicenna J Med. 9(1):1–7. https://doi.org/10.4103/ajm.AJM_140_18.
[37] Al-Yahya, I. A., Almohsen, H. A., AlSaleem, I. A., Al-Hamid, M. M., Arafah, A. M. & Al-Turki, Y. A. (2019). Assessment of knowledge, attitude, and practice about first aid among male school-teachers and administrators in Riyadh, Saudi Arabia. J Fam Med Prim Care. 8(2):684–8. https://doi.org/10.4103/jfmpc.jfmpc_316_18.
[38] Taqi, A. H, Salwa, H. A. & Akbar, S. (2015). The influence of gender on teaching students. Sci Educ 8: 182-190.
[39] Alufohai, P. J. & Ibhafidon, H. (2015). Influence of teachers’ age, marital status, and gender on students’ academic achievement. Asian J Educ Res 3: 60-66.
Viewed PDF 867 77 -
 Unlocking the Future: Predicting Malaria Vaccine Uptake and Likely Barriers in NigeriaAuthor: Odis Adaora IsabellaDOI: 10.21522/TIJPH.2013.11.04.Art002
Unlocking the Future: Predicting Malaria Vaccine Uptake and Likely Barriers in NigeriaAuthor: Odis Adaora IsabellaDOI: 10.21522/TIJPH.2013.11.04.Art002Unlocking the Future: Predicting Malaria Vaccine Uptake and Likely Barriers in Nigeria
Abstract:
Malaria vaccination was identified as a major effort to curb the Africa’s challenge of death amongst children under 5. As malaria vaccines are yet to be distributed in Nigeria, there is a debate on their acceptability, accessibility, and barriers to receiving them. This study was conducted to assess the uptake of the malaria vaccination, and its determinants among internet users in Nigeria. An online survey was conducted between July and August 2023 using a semi-structured questionnaire. It was set up using kobotoolbox forms and data were collected online. Data collected were analyzed using GNU PSPP. A total of 399 respondents participated in the study, with a mean age of 43.52 years (± 10.90). The majority of the respondents were young adults. The majority of our respondents (72.9%) have heard of the malaria vaccine while the majority said they would take the malaria vaccine if available (85.2%). The major source of information on the malaria vaccine was the internet (55.4%), health workers (51.9%), and media (Radio/Television/Posters/Billboards/Pamphlets) (44.9%). Malaria vaccination uptake had a significant positive association with the level of education and level of monthly income (p < 0.05 respectively). Lack of availability, information, knowledge, awareness, cost of a malaria vaccine, the long distance to get to vaccination centers were the leading barriers to vaccine uptake. This calls for key stakeholders to ensure that malaria vaccination sensitization is championed immediately in Nigeria and discouragement of the spread of conspiracy theories to eliminate the infodemic associated factors will reduce vaccine hesitancy and thereby increase malaria vaccination uptake in Nigeria.Keywords: Barriers, Determinant, Malaria, Malaria vaccine, Uptake, Vaccine.Unlocking the Future: Predicting Malaria Vaccine Uptake and Likely Barriers in Nigeria
References:
[1] WHO, 2021, Malaria, https://www.who.int/news-room/fact-sheets/detail/malaria.
[2] Omolola Oyinkan Adeshina, Solomon Nyame, James Milner, Ai Milojevic, Kwaku Poku Asante, (2022), Barriers and facilitators to nationwide implementation of the malaria vaccine in Ghana, https://academic.oup.com/heapol/article/38/1/28/6694852?login=false.
[3] WHO, 2020, Vaccines-and-immunization, https://www.who.int/health-topics/vaccines-and-immunization.
[4] University of Oxford, 2021, Malaria vaccine becomes first to achieve WHO-specified 75% efficacy goal https://www.ox.ac.uk/news/2021-04-23-malaria-vaccine-becomes-first-achieve-who-specified-75-efficacy-goal.
[5] Makoge V, Maat H, Vaandrager L, Koelen M. Poverty-related diseases (PRDs): unravelling complexities in disease responses in Cameroon. Trop Med Health. 2017; 45: 2.
[6] Adaora Anyichie – Odis, Progress report review on Malaria vaccination clinical trials, https://www.linkedin.com/pulse/progress-report-review-malaria-vaccination-clinical-anyichie-odis.
[7] WHO, 2021, https://www.who.int/news/item/06-10-2021-who-recommends-groundbreaking-malaria-vaccine-for-children-at-risk.
[8] Yeboah D, Owusu-Marfo J, Agyeman YN. Predictors of malaria vaccine uptake among children 6-24 months in the Kassena Nankana Municipality in the Upper East Region of Ghana. Malar J. 2022 Nov 16;21(1):339. doi: 10.1186/s12936-022-04378-1. PMID: 36384655; PMCID: PMC9666942. https://pubmed.ncbi.nlm.nih.gov/36384655/.
[9] WHO, (2022), https://www.who.int/news-room/feature-stories/detail/learning-lessons-from-the-pilots--overcoming-knowledge-gaps-around-the-malaria-vaccine-schedule-in-support-of-vaccine-uptake.
[10] Hassan Mumtaz, Abdullah Nadeem, Wajeeha Bilal, Farrukh Ansar, Saira Saleem, Qaisar Ali Khan, Tamara Tango, Christopher Farkouh, Naod F. Belay, Ravina Verma (2023), Acceptance, availability, and feasibility of RTS, S/AS01 malaria vaccine: A review https://onlinelibrary.wiley.com/doi/full/10.1002/iid3.899.
[11] Aremu TO, Singhal C, Ajibola OA, Agyin-Frimpong E, Appiah-Num Safo AA, Ihekoronye MR, Nabirye SE, Okoro ON. Assessing Public Awareness of the Malaria Vaccine in Sub-Saharan Africa. Tropical Medicine and Infectious Disease. 2022; 7(9):215. https://doi.org/10.3390/tropicalmed7090215.
[12] Nationonline, 2014, Nigeria, https://www.nationsonline.org/oneworld/nigeria.htm
[13] Worldometers, 2023, Nigeria, https://www.worldometers.info/world-population/nigeria-population/.
[14] Araoye, M.O. (2003) Research methodology with statistics for health and social sciences, First edition Nathadex Publisher Ilorin Nigeria. Page 119.
[15] Odis, A. I., et al (2022), Epidemics and Vaccination Dilemma in Complex Networks: A Case Study of Kosefe and Shomolu Local Government Area Lagos Nigeria.
[16] Odis, A. I. (2021) Attitude, Knowledge, and Use of Self–Medication with Antibiotics by Outpatients of Gbagada General Hospital Gbagada Lagos.
[17] Bosun Tijjani et al, (2023) COVID-19 Vaccine Uptake and its Determinants: Findings From A Web-Based Survey in Nigeria https://www.researchgate.net/publication/372587622_COVID19_Vaccine_Uptake_and_its_Determinants_Findings_From_A_Web-Based_Survey_in_Nigeria.
[18] Maduka D, Adaobi IO, Henrietta U. Acceptance of malaria vaccine by a rural community in Nigeria. Niger J Med. 2018; 27: 199. doi:10.4103/1115-2613.278781.
[19] Ozawa S, Clark S, Portnoy A, Grewal S, Brenzel L, Walker DG. Return on investment from childhood immunization in low- and middle-income countries, 2011-20. Health Aff. 2016; 35(2): 199-207.
[20] Pecenka C, Parashar U, Tate JE, et al. Impact and cost-effectiveness of rotavirus vaccination in Bangladesh. Vaccine. 2017; 35(32): 3982-3987.
[21] Letsa TS, Owusu-Agyei S. Community perceptions of a malaria vaccine in the Kintampo districts of Ghana. Malar J. 2013; 12:156. doi:10.1186/1475-2875-12-156.
[22] Mtenga S, Kimweri A, Romore I, et al. Stakeholders’ opinions and questions regarding the anticipated malaria vaccine in Tanzania. Malar J. 2016; 15: 189. doi:10.1186/s12936-016-1209-6.
[23] Dimala CA, Kika BT, Kadia BM, Blencowe H. Current challenges, and proposed solutions to the effective implementation of the RTS, S/AS01 malaria vaccine program in sub-Saharan Africa: a systematic review. PLoS One. 2018; 13(12): e0209744.
[24] Arora N, Anbalagan C, Pannu L. Towards eradication of malaria: is the WHO’s RTS, S/AS01 vaccination effective enough? Risk Manag Healthc Policy. 2021; 14: 1033-1039.
[25] Fran Bodine, (2022), GeoPoll Reports: Parent Perceptions of the Malaria Vaccine in sub-Saharan Africa, https://www.geopoll.com/blog/malaria-vaccine-parent-perceptions/?utm_feeditemid=,utm_device=c,utm_term=,utm_source=google,utm_medium=ppc,utm_campaign={utmcampaign},hsa_cam=13471823478,hsa_grp=123134039453,hsa_mt=,hsa_src=g,hsa_ad=5
27037284790,hsa_acc={97673848},hsa_net=adwords,hsa_kw=,hsa_tgt=dsa-39587879683&utm_feeditemid=&utm_device=c&adgroupid=123134039453&utm_term=&utm_source=googleb2badsutm_medium=cpc&utm_medium=ppc&utm_campaign={b2b_Dynamic_Ads}&utm_content=527037284790&hsa_cam=13471823478&hsa_grp=123134039453&hsa_mt=&hsa_src=g&hsa_ad=527037284790&hsa_acc=9672540637&hsa_net=adwords&hsa_kw=&hsa_tgt=dsa-39587879683&hsa_ver=3&gclid=Cj0KCQjwrfymBhCTARIsADXTabl3ODXXGzlmRQw1cfGLkS8XKaUZ3A5IsNhi7r5qEyZ3YTCBzWxR-44aApILEALw_wcB.[26] Adjei, M.R., Amponsa-Achiano, K., Okine, R. et al. Post introduction evaluation of the malaria vaccine implementation programme in Ghana, 2021. BMC Public Health 23, 586 (2023). https://doi.org/10.1186/s12889-023-15481-6.
Viewed PDF 1157 94 -
Assessment of Awareness, Willingness, and Practice of Human Immunodeficiency Virus Pre-Exposure Prophylaxis Among Female Sex Workers in Uyo, Akwa Ibom, NigeriaAuthor: Ughweroghene Kingston Omo-EmmanuelDOI: 10.21522/TIJPH.2013.11.04.Art003
Assessment of Awareness, Willingness, and Practice of Human Immunodeficiency Virus Pre-Exposure Prophylaxis Among Female Sex Workers in Uyo, Akwa Ibom, Nigeria
Assessment of Awareness, Willingness, and Practice of Human Immunodeficiency Virus Pre-Exposure Prophylaxis Among Female Sex Workers in Uyo, Akwa Ibom, Nigeria
References:
[1] UNAIDS. In Danger: UNAIDS Global AIDS Update. Geneva: Joint United Nations Programme on HIV/AIDS; 2022. https://www.unaids.org/en/resources/fact-sheet. Assessed August 2022.
[2] World Health Organization (WHO). Prevention and treatment of HIV and other sexually transmitted infections for sex workers in low- and middle-income countries: Recommendations for a public health approach. Geneva, Switzerland: World Health Organization; 2012.
[3] Shannon K, Strathdee SA, Goldenberg SM, Duff P. Global epidemiology of HIV among female sex workers: Influence of structural determinants. Lancet. 2015: 385(1): 55–71. https://doi.org/10.1016/s0140-6736(14)60931-4.
[4] Sabin K, Zhao J, Garcia Calleja JM, Sheng Y, Arias Garcia S, Reinisch A, Komatsu R. Availability, and quality of size estimations of female sex workers, men who have sex with men, people who inject drugs and transgender women in low- and middle-income countries. PLoS One; 2016: 11(5): e0155150.
[5] UNAIDS. Global AIDS Update — Confronting inequalities — Lessons for pandemic responses from 40 years of AIDS. Geneva: Joint United Nations Programme on HIV/AIDS; 2021. https://www.unaids.org/en/resources/documents/2021/2021-global-aids-update. Assessed December 2021.
[6] Eluwa, GI., Strathdee, SA., Adebajo, SB., Ahonsi, B, Azeez, A, & Anyanti, J. Sexual risk behaviors and HIV among female sex workers in Nigeria. JAIDS Journal of Acquired Immune Deficiency Syndromes, 2012: 61(4), 507–514.
[7] NACA. Revised National HIV and AIDS Strategic Framework 2019–2021. Nigeria National Agency for the Control of AIDS Abuja; 2019.
[8] Camlin, CS., Kwena, ZA., & Dworkin, S.L. Jaboya vs. jakambi: Status, negotiation, and HIV risks among female migrants in the “sex for fish” economy in Nyanza Province, Kenya. AIDS Education and Prevention, 2013: 25(3), 216–231.
[9] Scorgie, F, Chersich, MF, Ntaganira, I, Gerbase, A, Lule, F, & Lo, YR. Socio-demographic characteristics, and behavioral risk factors of female sex workers in sub-Saharan Africa: a systematic review. AIDS and Behavior, 2012: 16(4), 920–933.
[10] Rosenthal, L, & Levy, SR. Understanding Women’s Risk for HIV Infection Using Social Dominance Theory, and the Four Bases of Gendered Power. Psychology of Women Quarterly, 2010: 34(1), 21–35. https://doi.org/10.1111/j.1471-6402.2009.01538.x.
[11] Shannon K, Kerr T, Strathdee SA, Shoveller J, Montaner JS, Tyndall MW et al. Prevalence and structural correlates of gender based violence among a prospective cohort of female sex workers BMJ; 2000: 339: b2939 doi:10.1136/bmj. b2939.
[12] UNAIDS (2019). Global AIDS update 2019 — Communities at the Centre. Geneva: Joint United Nations Programme on HIV/AIDS; https://www.unaids.org/en/resources/documents/2019/2019-global-AIDS-update. Assessed December 2019.
[13] Nwokolo, N, Hill, A, McOwan, A, & Pozniak, A. Rapidly declining HIV infection in MSM in central London. The Lancet HIV, 2017: 4(11), e482–e483.
[14] Grulich, AE., Guy, R, Amin, J, Jin, F, Selvey, C, Holden, J, Schmidt, HMA., Zablotska, I, Price, K, & Whittaker, B. Population-level effectiveness of rapid, targeted, high-coverage roll-out of HIV pre-exposure prophylaxis in men who have sex with men: the EPIC-NSW prospective cohort study. The Lancet HIV, 2018: 5(11), e629–e637.
[15] Del, RC. HIV prevention: Integrating biomedical and behavioral interventions. Topics in Antiviral Medicine, 2014: 22, 702–706.
[16] Mayer, K.H., Skeer, M, & Mimiaga, MJ. Biomedical approaches to HIV prevention alcohol research & health. Journal of the National Institute on Alcohol Abuse and Alcoholism, 2010: 33, 195–202.
[17] Bradley J, Rajaram SP, Moses S, Boily MC, Ramesh BM, Isac S, Lobo A, Gowda GC, Rushpalatha R, Gurav K, Kumar S, Washington R, Pickles M, Alary M. Why do condoms break? A study of female sex workers in Bangalore, South India. Sexually Transmitted Infections. 2012: 88(3):163–170. doi: 10.1136/sextrans-2011-050283.
[18] Mukumbang FC. Actions of female sex workers who experience male condom failure during penetrative sexual encounters with clients in Cape Town: Implications for HIV prevention strategies. South Afr J HIV Med. 2017 Apr 4;18(1):698. doi: 10.4102/sajhivmed. v18i1.698. PMID: 29568633; PMCID: PMC5843032.
[19] Twizelimana D, and Muula AS. Actions taken by female sex workers (FSWs) after condom failure in semi urban Blantyre, Malawi. BMC Womens Health. 2020: 20(1):273. doi: 10.1186/s12905-020-01142-y. PMID: 33298055; PMCID: PMC7727183.
[20] Onovo, A., Kalaiwo, A., & Okechukwu, E. One-stop shop: a community-based antiretroviral therapy (ART) clinic model to improve human immunodeficiency virus (HIV) prevention and treatment Cascade for key populations in Nigeria. Open Forum Infectious Diseases, 2016: 3(suppl_1), 483.
[21] Lwanga, S. and Lemeshow, S. Sample Size Determination in Health Studies. A Practical Manual. 1991. http://www.tbrieder.org/publications/books_english/lemeshow_samplesize.pdf Assessed December 2019.
[22] Tomko, C, Park, JN, Allen, ST, Glick, J, Galai, N, Decker, MR, Footer, KHA., & Sherman, SG. Awareness and interest in HIV pre-exposure prophylaxis among street-based female sex workers: results from a US context. AIDS Patient Care and STDs, 2019: 33(2), 49–57.
[23] Restar, AJ., Tocco, JU., Mantell, JE., Lafort, Y, Gichangi, P, Masvawure, TB., Chabeda, SV, & Sandfort, TG. M. Perspectives on HIV pre-and post-exposure prophylaxes (PrEP and PEP) among female and male sex workers in Mombasa, Kenya: implications for integrating biomedical prevention into sexual health services. AIDS Education and Prevention, 2017: 29(2), 141–153.
[24] Logie, CH, Wang, Y, Lalor, P, Williams, D, & Levermore, K. Pre- and Post-exposure Prophylaxis Awareness and Acceptability Among Sex Workers in Jamaica: A Cross-Sectional Study. AIDS and Behavior, 2021: 25(2), 330–343.
[25] Emmanuel, G, Folayan, M, Undelikwe, G, Ochonye, B, Jayeoba, T, Yusuf, A, Aiwonodagbon, B, Bilali, C, Umoh, P, & Ojemeiri, K. Community perspectives on barriers and challenges to HIV pre-exposure prophylaxis access by men who have sex with men and female sex workers access in Nigeria. BMC Public Health, 2020: 20(1), 1–10.
[26] Simões, D, Meireles, P, Rocha, M, Freitas, R, Aguiar, A, & Barros, H. Knowledge, and Use of PEP and PrEP Among Key Populations Tested in Community Centers in Portugal. Frontiers in Public Health, 2021: 9.
[27] Haberer, JE, Baeten, JM, Campbell, J, Wangisi, J, Katabira, E, Ronald, A, Tumwesigye, E, Psaros, C, Safren, S A, & Ware, NC. Adherence to antiretroviral prophylaxis for HIV prevention: a substudy cohort within a clinical trial of serodiscordant couples in East Africa. PLoS Medicine, 2013: 10(9), e1001511.
[28] Mutya, E and MM. HIV Pre-Exposure Prophylaxis Adherence Among Female Sex Workers
in Mutare Urban, Zimbabwe. IJRDO - Journal of Health Sciences and Nursing, 2021: 6(2), 31–43.[29] Fearon, E, Phillips, A, Mtetwa, S, Chabata, ST, Mushati, P, Cambiano, V, Busza, J, Napierala, S, Hensen, B, & Baral, S. How can programs better support female sex workers to avoid HIV infection in Zimbabwe? A prevention cascade analysis. Journal of Acquired Immune Deficiency Syndromes, 2019: 81(1), 24.
Viewed PDF 975 45 -
 Malaria Transmission and Home-based Preventive Practices Amongst Women of Reproductive Age in South-South NigeriaAuthor: Emmanuel Friday OsagiedeDOI: 10.21522/TIJPH.2013.11.04.Art004
Malaria Transmission and Home-based Preventive Practices Amongst Women of Reproductive Age in South-South NigeriaAuthor: Emmanuel Friday OsagiedeDOI: 10.21522/TIJPH.2013.11.04.Art004Malaria Transmission and Home-based Preventive Practices Amongst Women of Reproductive Age in South-South Nigeria
Abstract:
Malaria infection accounts for over 60% of outpatient visits to healthcare facilities, 30% of child fatalities, 25% of infant deaths, and 11% of maternal mortality in Nigeria. Notably, in Nigeria, children under five years of age and pregnant women are especially vulnerable to malaria-related illnesses and death. The study, therefore, seeks to assess the knowledge of malaria disease, transmission, and use of home-based prevention strategies amongst women of reproductive age group. A cross-sectional study design was employed to assess the knowledge of malaria transmission and home-based preventive practices amongst a multistage sample of 379 women of reproductive age seeking healthcare services at the public PHC facilities in South-South, Nigeria. Data was collected using an interviewer-administered semi-structured questionnaire. Descriptive and inferential analyses of data collected were carried out using the IBM SPSS version 20 software. The mean age of the respondents surveyed in this study was 32.2 (SD ± 6.9) years. Most respondents [88.4% (n = 335)] had good knowledge of malaria transmission and prevention; however, the majority were not knowledgeable about the period mosquitoes commonly enter the house (71.5%) and the peak mosquito biting period (63.1%). There were varied degrees of practice of the various malaria home-based prevention strategies. In conclusion, a significant proportion of the surveyed reproductive-age women had some grasp on the fundamental issues of malaria transmission and prevention with some identified gaps, and they used different home-based malaria prevention measures at varied degrees.
Keywords: Home-based malaria preventive practices, Knowledge, Malaria transmission and prevention, Primary healthcare, Reproductive age women, South-South Nigeria.Malaria Transmission and Home-based Preventive Practices Amongst Women of Reproductive Age in South-South Nigeria
References:
[1] WHO, “World Malaria Report 2020 Regional Briefing kit,” Geneva, 2020. Accessed: Jun. 19, 2022. [Online]. Available: https://www.who.int/docs/default-source/malaria/world-malaria-reports/world-malaria-report-2020-regional-briefing-kit-eng.pdf?sfvrsn=3ff894_7.
[2] World Health Organization., “World Malaria Report 2018,” World Health Organization, Geneva, Nov. 2018. Accessed: May 31, 2023. [Online]. Available: https://www.who.int/publications/i/item/9789241565653.
[3] M. Accrombessi and S. Issifou, “Malaria control and elimination in sub-Saharan Africa: data from antenatal care centres,” The Lancet Global Health, vol. 7, no. 12. Elsevier Ltd, pp. e1595–e1596, Dec. 01, 2019. Doi: 10.1016/S2214-109X (19)30420-6.
[4] WHO Regional Office for Africa, “Report on malaria in Nigeria 2022,” 2022. [Online]. Available: http://apps.who.int/bookorders.
[5] National Malaria Elimination Programme, National Guidelines for Diagnosis and Treatment of Malaria, 3rd ed. Abuja: Federal Ministry of Health, Nigeria, 2015.
[6] USAID, “Eliminating malaria in Nigeria: five ways the USAID’s ‘president’s malaria initiative for states’ is making a difference,” Apr. 2021. Accessed: Aug. 16, 2022. [Online]. Available: https://www.usaid.gov/news-information/news/eliminating-malaria-nigeria-five-ways-usaid%E2%80%99s-%E2%80%98president%E2%80%99s-malaria-initiative.
[7] World Health Organization, “World Malaria Report 2021,” Geneva, 2021. Accessed: Jul. 06, 2022. [Online]. Available: https://www.who.int/teams/global-malaria-programme/reports/world-malaria-report-2021#.
[8] National Malaria Elimination Programme, “National Malaria Strategic Plan,” Abuja, 2014. Accessed: Jul. 05, 2022. [Online]. Available: https://www.health.gov.ng/doc/NMEP-Strategic-Plan.pdf.
[9] Support to the National Malaria Programme in Nigeria (SuNMaP), “Malaria control in Nigeria - Lessons learnt,” Abuja, 2016. Accessed: Jul. 05, 2022. [Online]. Available: https://www.malariaconsortium.org/sunmap/pages/about-sunmap/lessons-learnt.
[10] Support to the National Malaria Programme in Nigeria (SuNMaP), “Achievements in insecticide treated net ownership and use in Nigeria, and challenges in sustaining the gains,” Abuja, 2020. Accessed: Jul. 05, 2022. [Online]. Available: https://www.malariaconsortium.org/.
[11] Edo State Ministry of Health, “Edo State Government: State strategic health development plan (2010-2015),” Benin City, Nigeria., 2010.
[12] Edo State Government, “Edo State Primary Healthcare Development Agency (EDPHCDA-PHCUOR) Implementation Committee Final Report,” Benin City, Nov. 2021.
[13] G. Cochran, Sampling Techniques, 2nd ed. New York: John Wiley and Sons, Inc., 1963.
[14] A. M. Adebayo, O. O. Akinyemi, and E. O. Cadmus, “Knowledge of malaria prevention among pregnant women and female caregivers of under-five children in rural southwest Nigeria,” Peer, vol. 3, p. e792, Feb. 2015, Doi: 10.7717/peerj.792.
[15] R. Saadeh et al., “Osteoporosis among Postmenopausal Women in Jordan: A National Cross-Sectional Study,” Int J Environ Res Public Health, vol. 19, no. 14, p. 8803, Jul. 2022, Doi: 10.3390/ijerph19148803.
[16] IBM SPSS., “Statistical Package for the Social Sciences (SPSS) version 20.0. IBM SPSS;” 2014.
[17] World Atlas, “List of Countries by Literacy Rate,” 2020. Accessed: Aug. 22, 2023. [Online]. Available: https://www.worldatlas.com/articles/the-highest-literacy-rates-in-the-world.html.
[18] F. Okonofua, L. Ntoimo, J. Ogungbangbe, S. Anjorin, W. Imongan, and S. Yaya, “Predictors of women’s utilization of primary health care for skilled pregnancy care in rural Nigeria,” BMC Pregnancy Childbirth, vol. 18, no. 1, p. 106, Dec. 2018, Doi: 10.1186/s12884-018-1730-4.
[19] L. C. Steinhardt et al., “Effectiveness of insecticide-treated bed nets in malaria prevention in Haiti: a case-control study,” Lancet Glob Health, vol. 5, no. 1, pp. e96–e103, Jan. 2017, Doi: 10.1016/S2214-109X (16)30238-8.
[20] O. Amoran, “Impact of health education intervention on malaria prevention practices among nursing mothers in rural communities in Nigeria,” Nigerian Medical Journal, vol. 54, no. 2, p. 115, 2013, Doi: 10.4103/0300-1652.110046.
[21] K. E. Oladimeji, J. M. Tsoka-Gwegweni, E. Ojewole, and S. T. Yunga, “Knowledge of malaria prevention among pregnant women and non-pregnant mothers of children aged under 5 years in Ibadan, Southwest Nigeria,” Malar J, vol. 18, no. 1, p. 92, Dec. 2019, Doi: 10.1186/s12936-019-2706-1.
[22] A. R. Alhassan, “Pregnant Women and Malaria Preventive Measures: A Case of Tamale Teaching Hospital, Ghana,” J Trop Med, vol. 2021, pp. 1–9, Dec. 2021, Doi: 10.1155/2021/6150172.
[23] W. G. Stromquist, “Malaria control from the engineering point of view,” Am J Public Health, vol. 10, pp. 497–501, 1920, Accessed: Jul. 14, 2023. [Online]. Available: https://ajph.aphapublications.org/doi/pdf/10.2105/AJPH.10.6.497.
[24] C. E. Bisong and C. M. Dongmo, “Utilization of malaria prevention methods by pregnant women in Yaounde,” Pan African Medical Journal, vol. 15, 2013, Doi: 10.11604/pamj.2013.15.89.2324.
Viewed PDF 660 28 -
Heterogeneity in the Adoption of COVID-19 Preventive Measures Among Adults in Ethiopia: A Cluster Analysis ApproachAuthor: Luwaga LilianeDOI: 10.21522/TIJPH.2013.11.04.Art005
Heterogeneity in the Adoption of COVID-19 Preventive Measures Among Adults in Ethiopia: A Cluster Analysis Approach
Abstract:
This study investigates the extent of heterogeneity in the adoption of preventive measures among adult individuals in Ethiopia. Utilizing a nationally representative cross-sectional survey conducted by the World Health Organization in 2021, encompassing 895 participants, we explore the varying patterns of preventive measure adoption. Hierarchical cluster analysis is employed to discern potential subgroups within the respondents based on their adoption of preventive measures. Subsequently, logistic regression analysis is applied to ascertain the factors associated with the identified group divisions. We identify two distinct groups characterized by their responses to nine preventive measures. Group 1 comprises the majority of respondents (87%) who exhibit lower frequencies of adopting preventive measures. In contrast, Group 2 consists of 13% of respondents who demonstrate a higher frequency of adopting preventive measures. The amalgamation of cluster analysis and logistic regression outcomes yields insightful implications for the profile of preventive measure adoption. Our logistic regression analysis delves into the determinants influencing membership in the identified subgroups. Notably, it uncovers that individuals with a higher educational attainment exhibit a 2.33-fold greater likelihood of belonging to Group 1, signifying their relatively lesser adoption of preventive measures. In conclusion, this study not only sheds light on the heterogeneity within the adoption of preventive measures among Ethiopian adults but also underscores the influence of education on the propensity to adopt such measures. The findings contribute to better understanding of the dynamics surrounding public health behavior in the context of a pandemic.Keywords: COVID-19, Cluster analysis, Ethiopia, Heterogeneity, Logistic regression, Preventive measures.Heterogeneity in the Adoption of COVID-19 Preventive Measures Among Adults in Ethiopia: A Cluster Analysis Approach
References:
[1] Escandón, K., et al., COVID-19 false dichotomies and a comprehensive review of the evidence regarding public health, COVID-19 symptomatology, SARS-CoV-2 transmission, mask wearing, and reinfection. BMC infectious diseases, 2021. 21(1): p. 710.
[2] Gostin, L.O., R. Habibi, and B.M. Meier, has global health law risen to meet the COVID-19 challenge? Revisiting the International Health Regulations to prepare for future threats. The Journal of Law, Medicine & Ethics, 2020. 48(2): p. 376-381.
[3] Tadesse, S. and W. Muluye, The impact of COVID-19 pandemic on education system in developing countries: a review. Open Journal of Social Sciences, 2020. 8(10): p. 159-170.
[4] Yan, E., et al., Predicting public adherence to COVID-19 preventive measures: A cross-sectional study in Hong Kong. International Journal of Environmental Research and Public Health, 2021. 18(23): p. 12403.
[5] Gebreheat, G., et al., Adherence to COVID-19 preventive measures and associated factors in Ethiopia: A systematic review and meta-analysis. PLoS One, 2022. 17(10): p. e0275320.
[6] de Bruin, Y.B., et al., Initial impacts of global risk mitigation measures taken during the combatting of the COVID-19 pandemic. Safety Science, 2020: p. 104773.
[7] Tamirat, T. and L. Abute, Adherence towards COVID‐19 prevention measures and associated factors in Hossana town, South Ethiopia, 2021. International journal of clinical practice, 2021. 75(12): p. e14530.
[8] Desalegn, Z., et al., COVID-19 and the public response: Knowledge, attitude and practice of the public in mitigating the pandemic in Addis Ababa, Ethiopia. PloS one, 2021. 16(1): p. e0244780.
[9] Abeya, S.G., et al., Adherence to COVID-19 preventive measures and associated factors in Oromia regional state of Ethiopia. PloS one, 2021. 16(10): p. e0257373.
[10] Dueñas, M., et al., Knowledge of COVID-19 and prevention measures among university workers. Identification of subgroups through cluster analysis. Educación Médica, 2022. 23(5): p. 100764.
[11] Swart, L.-A., et al., The converging influence of social, economic, and psychological factors on public responsiveness to the COVID-19 pandemic in South Africa. BMC Public Health, 2022. 22(1): p. 1-11.
[12] López, L. and X. Rodó, The end of social confinement and COVID-19 re-emergence risk. Nature Human Behaviour, 2020. 4(7): p. 746-755.
[13] Mooi, E., M. Sarstedt, and I. Mooi-Reci, Market research: The process, data, and methods using Stata. 2018: Springer.
[14] Chessen, E.G., et al., Population Segmentation for COVID-19 Vaccine Outreach: A Clustering Analysis and Implementation in Missouri. Journal of Public Health Management and Practice, 2023. 29(4): p. 563-571.
[15] Thaker, J., L.M. Richardson, and D.C. Holmes, Audience segmentation analysis of public intentions to get a COVID-19 vaccine in Australia. Public Understanding of Science, 2023. 32(4): p. 470-488.
[16] Kaufman, L. and P.J. Rousseeuw, Finding groups in data: an introduction to cluster analysis. 2009: John Wiley & Sons.
[17] Jain, A.K. and R.C. Dubes, Algorithms for clustering data. 1988: Prentice-Hall, Inc.
[18] Caliński, T. and J. Harabasz, A dendrite method for cluster analysis. Communications in Statistics-theory and Methods, 1974. 3(1): p. 1-27.
[19] Duda, R., et al., Pattern classification, chapter nonparametric techniques. 2000, Wiley-Interscience Publication.
[20] Balakrishnan, K. and S. Anand, Sub-cities of Bengaluru: Urban heterogeneity through empirical typologies. Economic and Political Weekly, 2015: p. 63-72.
[21] Shewasinad Yehualashet, S., et al., Predictors of adherence to COVID-19 prevention measure among communities in North Shoa Zone, Ethiopia based on health belief model: A cross-sectional study. PloS one, 2021. 16(1): p. e0246006.
[22] Gelgelu, T.B., et al., Compliance with COVID-19 preventive measures among chronic disease patients in Wolaita and Dawuro zones, Southern Ethiopia: A proportional odds model. Plos one, 2022. 17(10): p. e0276553.
[23] Matovu, J.K., et al., COVID-19 awareness, adoption of COVID-19 preventive measures, and effects of COVID-19 lockdown among adolescent boys and young men in Kampala, Uganda. Journal of community health, 2021: p. 1-12.
[24] Carmichael, F., et al., School closures and educational attainment in Ethiopia: Can extra classes
help children to catch up? British Educational Research Journal, 2022. 48(4): p. 640-664.[25] Alagili, D.E. and M. Bamashmous, The Health Belief Model as an explanatory framework for COVID-19 prevention practices. Journal of infection and public health, 2021. 14(10): p. 1398-1403.
[26] Kim, S. and S. Kim, Analysis of the impact of health beliefs and resource factors on preventive behaviors against the COVID-19 pandemic. International journal of environmental research and public health, 2020. 17(22): p. 8666.
[27] Nutbeam, D. and I. Kickbusch, Health promotion glossary. Health promotion international, 1998. 13(4): p. 349-364.
[28] Rodríguez, H., et al., Communicating risk and uncertainty: Science, technology, and disasters at the crossroads. Handbook of disaster research, 2007: p. 476-488.
[29] Powell-Wiley, T.M., et al., social determinants of cardiovascular disease. Circulation research, 2022. 130(5): p. 782-799.
Viewed PDF 668 20 -
 Drug and Therapeutics Committee Structure and Roles in Hospitals: A Scoping ReviewAuthor: Samuel KiruyiDOI: 10.21522/TIJPH.2013.11.04.Art006
Drug and Therapeutics Committee Structure and Roles in Hospitals: A Scoping ReviewAuthor: Samuel KiruyiDOI: 10.21522/TIJPH.2013.11.04.Art006Drug and Therapeutics Committee Structure and Roles in Hospitals: A Scoping Review
Abstract:
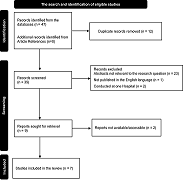
Drug and Therapeutics Committees (DTCs) have been identified and promoted as a fundamental model in advancing the rational management and use of essential medicines and health supplies in hospitals since the 1970s. However, there is still a scarcity of comprehensive literature on their current structure and actual roles performed in various countries. We conducted a scoping review using the Pubmed and ResearchGate databases and included eligible articles published between 2010 and 2023, to assess the structure and roles performed by hospital DTCs. The database search yielded 47 potential records, but only seven of these were eligible for inclusion. Studies included were from both high-income and low- and middle-income countries. The structure of DTCs is generally similar across these countries, with minor contextual variations. All DTCs are heterogeneous in composition and contain both medical and non-medical staff. The DTC leadership comprises a chairperson who is usually a senior clinician, and a secretary who is usually a pharmacist. The majority of the DTCs have at least one sub-committee, and antimicrobial stewardship is the most common. The DTCs still perform their customary roles, although their role scope is expanding. In some countries, the DTCs have taken on additional roles due to the evolving medicines management and use problems, and technologies. There is however still a dearth of recent primary data on the structure and roles of DTCs in many countries. We recommend more primary research to understand the status of DTCs in various countries and to provide more insights into the existence and functionality of the DTC sub-committees.
Keywords: Drug and Therapeutics Committee; DTC; Irrational Use; P&T Committee; Review; Hospital.Drug and Therapeutics Committee Structure and Roles in Hospitals: A Scoping Review
References:
[1] Religioni U, Pakulska T. Rational drug use in hospital settings – areas that can be changed. J Med Econ [Internet]. 2020;23(10):1205–8. Available from: https://doi.org/10.1080/13696998.2020.1801455.
[2] Tan EL, Pharm B, Hons BP, Ph D, Day RO, P FRAC, et al. Perspectives on Drug and Therapeutics Committee policy implementation. 2010;1(2005):526–45.
[3] World Health Organization. Drug and Therapeutics Committees. A practical Guide. Holloway K, Terry G, editors. Geneva: World Health Organization; 2003.
[4] Tan EL, Day RO, Brien J anne E. Drug and therapeutics committees — are they fulfilling their potential to improve the quality use of medicines? Int J Pharm Pract. 2010;11(3):175–81.
[5] Fadare JO, Ogunleye O, Obiako R, Orubu S, Enwere O, Ajemigbitse AA, et al. Expert Review of Clinical Pharmacology Drug and therapeutics committees in Nigeria: evaluation of scope and functionality. Expert Rev Clin Pharmacol [Internet]. 2018;11(12):1255–62. Available from: https://doi.org/10.1080/17512433.2018.1549488.
[6] Res M. Rational use of medicines: Cost consideration & way forward. 2016;(October):502–5.
[7] Shankar PR, Humagain ÆB, Nisha RMPÆ, Bidur JÆ. Establishing and strengthening a medicine and therapeutics committee in a medical college in Nepal: initial experiences. 2009;241–5.
[8] Seyoum H, Feleke Z, Bikila D, Yaregal A, Demisie A, Ali S, et al. Drug and Therapeutics Committee (DTC) evolvement and expanded scope in Ethiopia. Gates Open Res. 2023; 5:70.
[9] Vogenberg FR, Gomes J. The Changing Roles of P & T Committees A Look Back at the Last Decade and a Look Forward to 2020. 2020;39(11).
[10] Mashaba TP, Matlala M, Godman B, Meyer JC, Mashaba TP, Matlala M, et al. Expert Review of Clinical Pharmacology Implementation and monitoring of decisions by pharmacy and therapeutics committees in South African public sector hospitals Implementation and monitoring of decisions by pharmacy and therapeutics. Expert Rev Clin Pharmacol [Internet]. 2018;00(00):1–10. Available from: https://doi.org/10.1080/17512433.2018.1545572.
[11] Yang J, Yu- LZMS. Evaluating the effectiveness of drug and therapeutics committees (DTCs) in controlling irrational drug use: A retrospective analysis. 2022;(December 2021):995–1001.
[12] Perrone J, Nelson LS. Pharmacy and Therapeutics Committees: Leadership Opportunities in Medication Safety for Medical Toxicologists. 2011;99–102.
[13] Matlala M, Gous AGS, Godman B, Meyer JC, Matlala M, Gous AGS, et al. Expert Review of Clinical Pharmacology Structure and activities of pharmacy and therapeutics committees among public hospitals in South Africa; findings and implications. Expert Rev Clin Pharmacol [Internet]. 2017;00(00):1–8. Available from: https://doi.org/10.1080/17512433.2017.1364625.
[14] Marcos-rodríguez JA, Cordero-ramos J, Alvarado-fernández MD. Policy Multi-criteria Decision Analysis as a Decision-Support Tool for Drug Evaluation: A Pilot Study in Pharmacy. 2018.
[15] Santos-ramos B, Dura E. Literature review on the structure and operation of Pharmacy and Therapeutics Committees. 2011;475–83.
[16] Hoffmann M. The right drug, but from whose perspective? A framework for analysing the structure and activities of drug and therapeutics committees. 2013; 69:79–87.
[17] Page MJ, Mckenzie JE, Bossuyt PM, Boutron I, Hoffmann C, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews Systematic reviews and Meta-Analyses. 2021.
[18] Tricco AC, Lillie E, Zarin W, Brien KKO, Colquhoun H, Levac D, et al. R ESEARCH AND R EPORTING M ETHODS PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. 2018;(August 2016).
[19] Mak S, Thomas A. Steps for Conducting a Scoping Review. J Grad Med Educ. 2022;14(5):565–7.
[20] Peters MDJ, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc. 2015;13(3):141–6.
[21] Maros H, Juniar S. Beginer’s guide for systematic reviews. 2016;1–23.
[22] Almeida CPB de, Goulart BNG de. How to avoid bias in systematic reviews of observational studies. Rev CEFAC. 2017;19(4):551–5.
[23] THe World Bank Group. Country classification by income [Internet]. [cited 2023 Aug 21]. Available from: https://datahelpdesk.worldbank.org/knowledgebase/topics/19280-country-classification.
[24] Alefan Q, Alshareef S, Al-Shatnawi S. Drug, and therapeutics committees in jordanian hospitals: A nation-wide survey of organization, activities, and drug selection procedures. Pharm Pract (Granada). 2019;17(4):1–6.
[25] Plet HT, Hallas J, Nielsen GS, Kjeldsen LJ. Drug and Therapeutics Committees in Danish Hospitals: A Survey of Organization, Activities and Drug Selection Procedures. Basic Clin Pharmacol Toxicol. 2013;112(4):264–9.
[26] Puigventós F, Santos-Ramos B, Ortega A, Durán-García E. Structure and procedures of the pharmacy and therapeutic committees in Spanish hospitals. Pharm World Sci. 2010;32(6):767–75.
[27] Kabba JA, Koroma MM, James PB, Kitchen C, Xu S, Chang J, et al. Pilot drug, and therapeutic committee programme in Sierra Leone: A descriptive mixed method study. Br J Clin Pharmacol. 2023;89(1):20–33.
[28] Ministry of Health. Medicine and Therapeutics Committees Manual. 2018;(December):173. Available from: https://health.go.ug/sites/default/files/MTC Manual FINAL_print copy_21st Jan_19 %281%29.pdf.
[29] Ministry of Health Kenya. Guidelines for the Establishment and Operationalization of Medicines and Therapeutics Committees. 2020;(October).
[30] Management Sciences for Health. Treatment Guidelines and Formulary Manuals. MDS-3Managing Access to Med Heal Technol. 2012;17.1-17.5.
[31] Ciccarello C, Leber MB, Leonard MC, Nesbit T, Petrovskis MG, Pherson E, et al. ASHP Guidelines on the Pharmacy and Therapeutics Committee and the Formulary System. Am J Heal Pharm. 2021;78(10):907–18.
[32] Mannebach MA, Ascione FJ, Gaither CA, Bagozzi RP, Cohen IA, Ryan ML. Activities, functions, and structure of pharmacy and therapeutics committees in large teaching hospitals. Am J Heal Pharm. 1999;56(7):622–8.
[33] Björkman IK, Bernsten CB, Schmidt IK, Holmström I. The role of drug and therapeutics committees: Perceptions of chairs and information officers. Int J Health Care Qual Assur. 2005;18(4):235–48.
[34] Ramli A, Aljunid SM, Sulong S, Yusof FA. Structures and activities of Drug and Therapeutic Committees in formulary management: findings from a national survey and key informant interviews. 2014;14(Suppl 1):2458.
Viewed PDF 1768 139 -
Adolescence Substance Use Prevention Strategies: A Review of Key InterventionsAuthor: Chinwe F.S EzeruigboDOI: 10.21522/TIJPH.2013.11.04.Art007
Adolescence Substance Use Prevention Strategies: A Review of Key Interventions
Abstract:
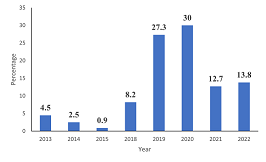
The rise in the prevalence of substance use among adolescents has triggered researchers for more studies on substance use and intervention strategies. The aim of the review is to provide a synthesis of effective preventive strategies in the face of multiple and variant literature on adolescent substance use data. A Google Scholar, and PUBMED academic literature published in English from 2012 to 2022 were included. A Google search of Keywords for the search were adolescent, substance use and preventive strategies. The described principles of prevention science provide examples of efficacious preventive interventions. It describes challenges and potential solutions necessary to take efficacious prevention policies and programs. It tends to scale and conclude with recommendations on how to reduce the burden of adolescent substance use mortality and morbidity worldwide through preventive interventions. Effective strategies share common goals with strengthening ‘protective factors,’ such as well-developed social skills, strong family bonds, attachment, active involvement, community, and religious organizations, while reducing ‘risk factors’ that increase vulnerability to substance use. In conclusion, several strategies are positive and effective, while some lack acceptable evidence for interventions. These attributes can help resource-constrained nations mount effective control measures against substance use.
Keywords: Adolescence; Intervention; Substance Use; Strategies.Adolescence Substance Use Prevention Strategies: A Review of Key Interventions
References:
[1] Louie E, Barrett EL, Baillie A, Haber P, Morley KC. Implementation of evidence based practice for alcohol and substance use disorders: protocol for systematic review. Systematic Reviews. 2020 Feb 7;9(1).
[2] Das JK, Salam RA, Arshad A, Finkelstein Y, Bhutta ZA. Interventions for Adolescent Substance Abuse: An Overview of Systematic Reviews. Journal of Adolescent Health [Internet]. 2019 Oct;59(4): S61–75. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5026681/.
[3] Secker-Walker R, Gnich W, Platt S, Lancaster T. Community interventions for reducing smoking among adults. Cochrane Database of Systematic Reviews. 2002 Apr 22.
[4] Fowler Ef, Baum Lm, Jesch E, Haddad D, Reyes C, Gollust Se, et al. Issues Relevant to Population Health in Political Advertising in the United States, 2011‐2012 and 2015‐2016. The Milbank Quarterly. 2019 Oct 24;97(4):1062–107.
[5] U.S. Department of Education, (2000). Key School-Linked Strategies and Principles for Preventing Substance Abuse and Violence. http://notes.edc.org/HHD/MSC/mscres.nsf/0/5044870fadcb56d6852568e800532418/FILE/Topic3- Strategy.doc.
[6] Shahzad M, Upshur R, Donnelly P, Bharmal A, Wei X, Feng P, et al. A population-based approach to integrated healthcare delivery: a scoping review of clinical care and public health collaboration. BMC Public Health [Internet]. 2019 Jun 7;19(1):1–15. Available from: https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-019-7002-z.
[7] Iwasaki Y. The role of youth engagement in positive youth development and social justice youth development for high-risk, marginalised youth. International Journal of Adolescence and Youth. 2015 Jul 25;21(3):267–78.
[8] States. U. ESEA, Drug-free Schools. 1999.
[9] WHO (2016). Shanghai declaration on health promotion in the 2030 agenda for sustainable development: ensuring sustainable health and well-being for all. Geneva: WHO. (https://www.who.int/healthpromotion/conferences/9gchp/shanghaideclaration/en/ https://www.who. int/healthpromotion/conferences/9gchp/shanghai-declaration.pdf, accessed 20 December 2019).
[10] Mahmood N, Othman S, Al-Tawil N, Al-Hadithi T. Impact of an education intervention on knowledge of high school students concerning substance use in Kurdistan Region-Iraq: A quasi-experimental study. Nicoletti A, editor. Plos one. 2018 Oct 31;13(10): e0206063.
[11] Jones SC, Andrews K, Francis K. Combining social norms and social marketing to address underage drinking: development and process evaluation of a whole-of-community intervention. Plos One. 2017;12(1): e0169872. https://doi.org/10.1371/journal.pone.0169872.
[12] Svensson R, Johnson B, Kronkvist K. A community intervention to reduce alcohol consumption and drunkenness among adolescents in Sweden: a quasi-experiment. BMC Public Health. 2021 Apr 21;21(1).
[13] Fathian-Dastgerdi Z, Eslami AA, Ghofranipour F, Mostafavi F. Effectiveness of Community-based Substance Use Prevention Program Among Adolescents - Using Social Cognitive Theory. 2021 Sep 8.
[14] Heijdra Suasnabar JM, Hipple Walters B. Community-based psychosocial substance use disorder interventions in low-and-middle-income countries: a narrative literature review. International Journal of Mental Health Systems. 2020 Oct 8;14(1).
[15] The United Nations Office on Drugs and Crime (UNODC) (2021). Strategic Vision for Nigeria 2030. UNODC. https://www.unodc.org/documents/nigeria/UNODC.
[16] Stockings E, Bartlem K, Hall A, Hodder R, Gilligan C, Wiggers J, et al. Whole-of-community interventions to reduce population-level harms arising from alcohol and other drug use: a systematic review and meta-analysis. Addiction. 2018 Jul 5;113(11):1984–2018.
[17] Komro KA, Perry CL, Veblen-Mortenson S, Farbakhsh K, Toomey TL, Stigler MH, et al. Outcomes from a randomized controlled trial of a multi-component alcohol use preventive intervention for urban youth: Project Northland Chicago. Addiction. 2008 Apr;103(4):606–18.
[18] Dube SR, Anda RF, Felitti VJ, Chapman DP, Williamson DF, Giles WH. Childhood Abuse, Household Dysfunction, and the Risk of Attempted Suicide Throughout the Life Span. JAMA [Internet]. 2001 Dec 26;286(24):3089. Available from: https://jamanetwork.com/journals/jama/article-abstract/194504.
[19] Adeson & Crewll (2000). The Prevalence of Drug of Abuse Among Youth (Adolescents) Stile/m of education and Research 2 www.cdcnpin.org/hiv/faq/prevention]itiTi.
[20] Jhanjee S. Evidence based psychosocial interventions in substance use. Indian Journal of Psychological Medicine. 2014;36(2):112.
[21] Griffin KW, Botvin GJ. Evidence-Based Interventions for Preventing Substance Use Disorders in Adolescents. Child and Adolescent Psychiatric Clinics of North America [Internet]. 2010 Jul;19(3):505–26. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2916744/pdf/nihms-189310.pdf.
[22] Obiechina, G. O. & Isiguzo, B. C. (2016). Curbing the menace of drug use among secondary school students in Nigeria. European Journal of Research and Reflection in Educational Sciences 4;1 2056-5852.
[23] Tait RJ, Christensen H. Internet-based interventions for young people with problematic substance use: a systematic review. Med J Aust. 2010;192(S11): S15-21.
[24] National Institute on Drug Abuse. Preventing Drug Misuse and Addiction: The Best Strategy [Internet]. National Institute on Drug Abuse. 2020. Available from: https://nida.nih.gov/publications/drugs-brains-behavior-science-addiction/preventing-drug-misuse-addiction-best-strategy.
[25] Okey-Orji, S. & Ekenedo, G. O. (2019). life Skills Acquisition: A Panacea for Domestic Violence Among Adolescents in Nigeria. Academic Research International. 10(3).
[26] Dupuy, K., Bezu, S., Knudsen, A., Halvorsen, S., Kwauk, C., Braga, A., … Brookings Institution, C. for U. E. (2018). Life Skills in Non-Formal Contexts for Adolescent Girls in Developing Countries. CMI Report Number 5. Center for Universal Education at The Brookings Institution. 1775 Massachusetts Avenue NW, Washington, DC 20036. http://www.brookings.edu/about/centers/universal-education.
[27] World Health Organization. (1997). Promoting health through schools. Report of the WHO Expert Committee on Comprehensive School, Health Education and Promotion. WHO Technical Report No. 870 Geneva. Switzerland.
[28] Dhingra, R., & Chauha, K. S. (2017). Assessment of life-skills of adolescents in relation to selected variables. International Journal of Scientific Research; 7(8), 201 -211.
[29] Botvin GJ, Griffin KW. Life Skills Training: A competence enhancement approach to tobacco, alcohol, and drug abuse prevention. Handbook of adolescent drug use prevention: Research, intervention strategies, and practice. 2015;177–96.
[30] Stockings E, Hall WD, Lynskey M, Morley KI, Reavley N, Strang J, et al. Prevention, early intervention, harm reduction, and treatment of substance use in young people. Lancet Psychiatry. 2016;3(3):280-96.
[31] Lorenc T, Lester S, Sutcliffe K, et al. Interventions to support people exposed to adverse childhood experiences: systematic review of systematic reviews. BMC Public Health 20, 657 (2020). https://doi.org/10.1186/s12889-020-08789-0.
[32] Schleider JL, Mullarkey MC, Fox KR, Dobias ML, Shroff A, Hart EA, et al. A randomized trial of online single-session interventions for adolescent depression during COVID-19. Nature Human Behaviour [Internet]. 2021 Dec 9;1–11. Available from: https://www.nature.com/articles/s41562-021-01235-0#Sec2.
[33] Ott MA, Santelli JS. Abstinence and abstinence-only education. Current Opinion in Obstetrics and Gynecology [Internet]. 2007 Oct;19(5):446–52. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5913747/.
[34] Cloitre M. The “one size fits all” approach to trauma treatment: should we be satisfied? European Journal of Psychotraumatology. 2015 May 19;6(1):27344.
[35] Volkow ND, Poznyak V, Saxena S, Gerra G. Drug use disorders: impact of public health rather than a criminal justice approach. World Psychiatry [Internet]. 2017 Jun 1;16(2):213–4. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5428163/.
[36] Dunham, D. (2015). Addictions, Biblical Counseling, Body Of Christ.https://www.biblicalcounselingcoalition.org/2015/03/04/biblical-counseling-addictions-and-the-body-of-christ.
Viewed PDF 1070 44 -
 Trends in Diarrhea Hospitalization among Children <5 Years Old Before and During the Covid-19 Season in Fako Division, Cameroon: A Situation Clouded by Sociopolitical ConflictAuthor: Beatrice Ameh Tangunyi LohDOI: 10.21522/TIJPH.2013.11.04.Art008
Trends in Diarrhea Hospitalization among Children <5 Years Old Before and During the Covid-19 Season in Fako Division, Cameroon: A Situation Clouded by Sociopolitical ConflictAuthor: Beatrice Ameh Tangunyi LohDOI: 10.21522/TIJPH.2013.11.04.Art008Trends in Diarrhea Hospitalization among Children <5 Years Old Before and During the Covid-19 Season in Fako Division, Cameroon: A Situation Clouded by Sociopolitical Conflict
Abstract:
Diarrhea is a major cause of illness and death for children under 5 in sub-Saharan Africa, with around 500k deaths annually. COVID-19 affected hospitalization rates for diarrhea. This study was done in four hospitals in Fako Division on diarrhea hospitalization records of children under 5 from 2013 to 2022. Stratified sampling was used, and data was summarized using means, standard deviations, frequencies, and percentages. Differences were evaluated using chi square with a significance level of P<0.05. Diarrhea hospitalization rate was high at 30.9%, with more cases reported during Covid-19 than before. Peak hospitalization occurred in 2019 and 2020. However, there was a significant decrease in hospitalization rates in 2021 and 2022. Children aged 0-5 months had the highest rates of diarrhea hospitalization at 29.4%. High diarrhea rates in the study area were due to conflict-related population influx. COVID-19 season saw higher hospitalization rates due to virus-induced diarrhea and population influx. Infants under 5 are most vulnerable to diarrhea. More diarrhea hospitalizations in COVID-19 season due to influx of displaced families and COVID-19 - induced diarrhea caused unusual data.
Keywords: Age, COVID-19, Children, Coverage, Diarrhea, Rotavirus, Vaccine, Vaccination, Sub-Saharan Africa.Trends in Diarrhea Hospitalization among Children <5 Years Old Before and During the Covid-19 Season in Fako Division, Cameroon: A Situation Clouded by Sociopolitical Conflict
References:
[1] Troeger C, Blacker BF, Khalil IA, Rao PC, Cao S, Zimsen SRM, et al. Estimates of the global, regional, and national morbidity, mortality, and aetiologies of diarrhoea in 195 countries: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Infect Dis [Internet]. 2018;18 (11):1211–28. Available from: http://dx.doi.org/10.1016/s1473-3099(18)30362-1.
[2] Dairo MD, Ibrahim TF, Salawu AT. Prevalence and determinants of diarrhoea among infants in selected primary health centres in Kaduna north local government area, Nigeria. Pan Afr Med J [Internet]. 2017;28. Available from: http://dx.doi.org/10.11604/pamj.2017.28.109.8152.
[3] Gidudu J, Sack DA, Pina M, Hudson MJ, Kohl KS, Bishop P, et al. Diarrhea: Case definition and guidelines for collection, analysis, and presentation of immunization safety data. Vaccine [Internet]. 2011;29 (5):1053–71. Available from: http://dx.doi.org/10.1016/j.vaccine.2010.11.065.
[4] Pires SM, Fischer-Walker CL, Lanata CF, Devleesschauwer B, Hall AJ, Kirk MD, et al. Aetiology-specific estimates of the global and regional incidence and mortality of diarrhoeal diseases commonly transmitted through food. PLoS One [Internet]. 2015;10(12):e0142927. Available from: http://dx.doi.org/10.1371/journal.pone.0142927.
[5] Who.int. [cited 2023 Sep 13]. Available from: https://www.who.int/news-room/fact-sheets/detail/diarrhoeal-disease.
[6] Saeed A, Abd H, Sandstrom G. Microbial aetiology of acute diarrhoea in children under five years of age in Khartoum, Sudan. J Med Microbiol [Internet]. 2015;64(4):432–7. Available from: http://dx.doi.org/10.1099/jmm.0.000043.
[7] Who.int. [cited 2023 Sep 13]. Available from: https://www.who.int/teams/health-product-policy-and-standards/standards-and-specifications/vaccines-quality/rotavirus.
[8] Riera R, Bagattini ÂM, Pacheco RL, Pachito DV, Roitberg F, Ilbawi A. Delays and disruptions in cancer health care due to COVID-19 pandemic: Systematic review. JCO Glob Oncol [Internet]. 2021;(7):311–23. Available from: http://dx.doi.org/10.1200/go.20.00639.
[9] Toczylowski K, Jackowska K, Lewandowski D, Kurylonek S, Waszkiewicz-Stojda M, Sulik A. Rotavirus gastroenteritis in children hospitalized in northeastern Poland in 2006–2020: Severity, seasonal trends, and impact of immunization. Int J Infect Dis [Internet]. 2021;108:550–6. Available from: http://dx.doi.org/10.1016/j.ijid.2021.05.070.
[10] Cohen AL, Platts-Mills JA, Nakamura T, Operario DJ, Antoni S, Mwenda JM, et al. Aetiology and incidence of diarrhoea requiring hospitalisation in children under 5 years of age in 28 low-income and middle-income countries: findings from the Global Pediatric Diarrhea Surveillance network. BMJ Glob Health [Internet]. 2022;7(9):e009548. Available from: http://dx.doi.org/10.1136/bmjgh-2022-009548.
[11] Terzian, M. As Khartoum’s health systems collapse, MSF teams at the Turkish Hospital have been able to keep up operations, despite the challenges and risks [Internet]. ReliefWeb. 2023; [cited 2023 Sep 13]. Available from: https://reliefweb.int/report/sudan/khartoums-health-systems-collapse-msf-teams-turkish-hospital-have-been-able-keep-operations-despite-challenges-and-risks.
[12] Dunn, G. Panafrican-med-journal.com. 2016. [cited 2023 Sep 13]. Available from: https://www.panafrican-med-journal.com/content/article/11/73/fullhttps://doi.org/10.11604/pamj.2012.11.73.1548.
[13] Ndze, V. N., Akum, A. E., Kamga, G. H., Enjema, L. E., Esona, M. D., Banyai, K., & Marie Therese, O. A. Epidemiology of rotavirus diarrhea in children under 5 years in Northern Cameroon. PAMJ [Internet]. 2012; 11(73). Available from: https://www.panafrican-med-journal.com/content/article/11/73/fullhttps://doi.org/10.11604/pamj.2012.11.73.1548.
[14] Hugho EA, Kumburu HH, Amani NB, Mseche B, Maro A, Ngowi LE, et al. Enteric pathogens detected in children under five years old admitted with diarrhea in Moshi, Kilimanjaro, Tanzania. Pathogens [Internet]. 2023;12(4):618. Available from: http://dx.doi.org/10.3390/pathogens12040618.
[15] Vlasova AN, Takanashi S, Miyazaki A, Rajashekara G, Saif LJ. How the gut microbiome regulates host immune responses to viral vaccines. Curr Opin Virol [Internet]. 2019;37:16–25. Available from: http://dx.doi.org/10.1016/j.coviro.2019.05.001.
[16] Manjate F, Quintó L, Chirinda P, Acácio S, Garrine M, Vubil D, et al. Impact of rotavirus vaccination on diarrheal hospitalizations in children younger than 5 years of age in a rural southern Mozambique. Vaccine [Internet]. 2022;40(44):6422–30. Available from: http://dx.doi.org/10.1016/j.vaccine.2022.09.050.
[17] Fukuda Y, Tsugawa T, Nagaoka Y, Ishii A, Nawa T, Togashi A, et al. Surveillance in hospitalized children with infectious diseases in Japan: Pre- and post-coronavirus disease 2019. J Infect Chemother [Internet]. 2021;27(11):1639–47. Available from: http://dx.doi.org/10.1016/j.jiac.2021.07.024.
[18] Negsso A, Arega B, Abdissa F, Zewdu B, Teshome A, Minda A, et al. Effect of COVID-19 pandemic on the incidence of acute diarrheal disease and pneumonia among under 5 children in Ethiopia- A database study. PLOS Glob Public Health [Internet]. 2023;3(6):e0000304. Available from: http://dx.doi.org/10.1371/journal.pgph.0000304.
[19] Azene ZN, Merid MW, Muluneh AG, Geberu DM, Kassa GM, Yenit MK, et al. Adherence towards COVID-19 mitigation measures and its associated factors among Gondar City residents: A community-based cross-sectional study in Northwest Ethiopia. PLoS One [Internet]. 2020;15(12):e0244265. Available from: http://dx.doi.org/10.1371/journal.pone.0244265.
[20] Holshue ML, DeBolt C, Lindquist S, Lofy KH, Wiesman J, Bruce H, et al. First case of 2019 novel Coronavirus in the United States. N Engl J Med [Internet]. 2020;382(10):929–36. Available from: http://dx.doi.org/10.1056/nejmoa2001191.
[21] Wang F, Zheng S, Zheng C, Sun X. Attaching clinical significance to COVID-19-associated diarrhea. Life Sci [Internet]. 2020;260(118312):118312. Available from: http://dx.doi.org/10.1016/j.lfs.2020.118312.
Viewed PDF 724 21 -
Key Stakeholders’ Perspectives on Implementation and Scale-up of Telehealth in HIV Care in Harare, ZimbabweAuthor: Stanford ChigaroDOI: 10.21522/TIJPH.2013.11.04.Art009
Key Stakeholders’ Perspectives on Implementation and Scale-up of Telehealth in HIV Care in Harare, Zimbabwe
Abstract:
The World Health Organisation recommends telehealth as an alternative to help reach remote or underserved areas. Telehealth adoption is therefore key to ending the HIV pandemic. Successful implementation and scale-up of telehealth heavily rely on stakeholders’ involvement. This study explored key stakeholders’ perspectives on the implementation and scale-up of telehealth in HIV care in Harare. In-depth interviews were conducted with professionals within the Ministry of Health and Childcare and its partners, between May and August 2023. Fourteen purposively selected stakeholders were interviewed. Thematic approach to analysis with a coding framework guided by Consolidated Framework for Implementation Research was adopted. Key stakeholders perceived telehealth as a potentially effective intervention, which can improve health delivery. Key stakeholders cited the following challenges for implementation and scale-up of telehealth in HIV care: poor internet and mobile network; financial challenges; and unavailability of policies. Key stakeholders suggested the following strategies to the successful implementation and scale-up: multi-sectoral collaboration for reliable and affordable mobile and internet connectivity; policy formulation, donors’ engagement; and recruitment of competent staff. The study findings showed the confidence of key stakeholders in Harare to effectively sustain telehealth in HIV intervention. Despite its promising potential, significant hurdles to telehealth implementation exist and should be addressed to realise the full potential. Further research incorporating telehealth end-users is recommended, to fully understand challenges and hence inform policy.
Keywords: HIV; Key Stakeholders; Telehealth; Utilisation.Key Stakeholders’ Perspectives on Implementation and Scale-up of Telehealth in HIV Care in Harare, Zimbabwe
References:
[1] Thomas, L. T., Lee, C. M. Y., McClelland, K., Nunis, G., Robinson, S., & Norman, R. (2023). Health workforce perceptions on telehealth augmentation opportunities. BMC Health Services Research, 23(1), 182. https://doi.org/10.1186/s12913-023-09174-4.
[2] Oleribe, O. E., Momoh, J., Uzochukwu, B. S., Mbofana, F., Adebiyi, A., Barbera, T., Williams, R., & Taylor Robinson, S. D. (2019). Identifying Key Challenges Facing Healthcare Systems in Africa and Potential Solutions. International Journal of General Medicine, Volume 12, 395–403. https://doi.org/10.2147/IJGM.S223882.
[3] Nchasi, G., Okonji, O. C., Jena, R., Ahmad, S., Soomro, U., Kolawole, B. O., Nawaz, F. A., Essar, M. Y., & Aborode, A. T. (2022). Challenges faced by African healthcare workers during the third wave of the pandemic. Health Science Reports, 5(6), e893. https://doi.org/10.1002/hsr2.893.
[4] World Health Organisation. (n.d.). Global strategy on digital health 2020-2025. World Health Organization. Retrieved 3 April 2023, from https://apps.who.int/iris/bitstream/handle/10665/344249/9789240020924-eng.pdf.
[5] Breton, M., Sullivan, E. E., Deville-Stoetzel, N., McKinstry, D., DePuccio, M., Sriharan, A., Deslauriers, V., Dong, A., & McAlearney, A. S. (2021). Telehealth challenges during COVID-19 as reported by primary healthcare physicians in Quebec and Massachusetts. BMC Family Practice, 22(1), 192. https://doi.org/10.1186/s12875-021-01543-4.
[6] Snoswell, C. L., Taylor, M. L., Comans, T. A., Smith, A. C., Gray, L. C., & Caffery, L. J. (2020). Determining if Telehealth Can Reduce Health System Costs: Scoping Review. Journal of Medical Internet Research, 22(10), e17298. https://doi.org/10.2196/17298.
[7] Eze, N. D., Mateus, C., & Cravo Oliveira Hashiguchi, T. (2020). Telemedicine in the OECD: An umbrella review of clinical and cost-effectiveness, patient experience and implementation. PLOS ONE, 15(8), e0237585. https://doi.org/10.1371/journal.pone.0237585.
[8] Salgado, S., Felzien, G., & Brumbeloe, J. (2021). Georgia Leverages Telehealth to Expand HIV Care Management in Underserved Areas. American Journal of Preventive Medicine, 61(5 Suppl 1), S55–S59. https://doi.org/10.1016/j.amepre.2021.07.001.
[9] Phan, J. M., Kim, S., Linh, Đ. T. T., Cosimi, L. A., & Pollack, T. M. (2022). Telehealth Interventions for HIV in Low- and Middle-Income Countries. Current HIV/AIDS Reports, 19(6), 600–609. https://doi.org/10.1007/s11904-022-00630-0.
[10] Pollack, T. M., Nhung, V. T. T., Vinh, D. T. N., Hao, D. T., Trang, L. T. T., Duc, P. A., Kinh, N. V., Dung, N. T. H., Dung, D. L., Ninh, N. T., Huyen, H. T. T., Huy, V. X., Hai, D. M., Khanh, T. H., Hien, N. T. T., Khuong, P. T. A., Trong, N. T., Lam, N. V., Phinh, V. N., … Cosimi, L. (2020). Building HIV healthcare worker capacity through telehealth in Vietnam. BMJ Global Health, 5(4), e002166. https://doi.org/10.1136/bmjgh-2019-002166.
[11] Speyer, R., Denman, D., Wilkes-Gillan, S., Chen, Y., Bogaardt, H., Kim, J., Heckathorn, D., & Cordier, R. (2018). Effects of telehealth by allied health professionals and nurses in rural and remote areas: A systematic review and meta-analysis. Journal of Rehabilitation Medicine, 50(3), 225–235. https://doi.org/10.2340/16501977-2297.
[12] Huang, Z., Tao, H., Meng, Q., & Jing, L. (2015). MANAGEMENT OF ENDOCRINE DISEASE: Effects of telecare intervention on glycemic control in type 2 diabetes: a systematic review and meta-analysis of randomized controlled trials. European Journal of Endocrinology, 172(3), R93–R101. https://doi.org/10.1530/EJE-14-0441.
[13] Nair, U., Armfield, N. R., Chatfield, M. D., & Edirippulige, S. (2018). The effectiveness of telemedicine interventions to address maternal depression: A systematic review and meta-analysis. Journal of Telemedicine and Telecare, 24(10), 639–650. https://doi.org/10.1177/1357633X18794332.
[14] Udsen, F. W., Hejlesen, O., & Ehlers, L. H. (2014). A systematic review of the cost and cost-effectiveness of telehealth for patients suffering from chronic obstructive pulmonary disease. Journal of Telemedicine and Telecare, 20(4), 212–220. https://doi.org/10.1177/1357633X14533896.
[15] Hui CY., Walton R., McKinstry B., Jackson T., Parker R., & Pinnock H. (2017). The use of mobile applications to support self-management for people with asthma: a systematic review of controlled studies to identify features associated with clinical effectiveness and adherence. Journal of the American Medical Informatics Association, 24(3), 619–632. 10.1093/jamia/ocw143.
[16] 16. Liptrott, S., Bee, P., & Lovell, K. (2018). Acceptability of telephone support as perceived by patients with cancer: A systematic review. European Journal of Cancer Care, 27(1), e12643. https://doi.org/10.1111/ecc.12643
[17] 17. Liddy, C., Drosinis, P., & Keely, E. (2016). Electronic consultation systems: Worldwide prevalence and their impact on patient care—a systematic review. Family Practice, 33(3), 274–285. https://doi.org/10.1093/fampra/cmw024.
[18] Labisi, T., Regan, N., Davis, P., & Fadul, N. (2022). HIV Care Meets Telehealth: A Review of Successes, Disparities, and Unresolved Challenges. Current HIV/AIDS Reports. https://doi.org/10.1007/s11904-022-00623-z.
[19] Centre for Disease Control and Prevention. (2018). Telehealth for HIV Prevention and Care Services. Centre for Disease Control and Disease. https://www.cdc.gov/hiv/effective-interventions/treat/telehealth/index.html.
[20] Esmaeili, E. D., Azizi, H., Dastgiri, S., & Kalankesh, L. R. (2023). Does telehealth affect the adherence to ART among patients with HIV? A systematic review and meta-analysis. BMC Infectious Diseases, 23(1), 169. https://doi.org/10.1186/s12879-023-08119-w.
[21] Dandachi, D., Freytag, J., Giordano, T. P., & Dang, B. N. (2020). It is Time to Include Telehealth in Our Measure of Patient Retention in HIV Care. AIDS and Behavior, 24(9), 2463–2465. https://doi.org/10.1007/s10461-020-02880-8.
[22] Mgbako, O., Miller, E. H., Santoro, A. F., Remien, R. H., Shalev, N., Olender, S., Gordon, P., & Sobieszczyk, M. E. (2020). COVID-19, Telemedicine, and Patient Empowerment in HIV Care and Research. AIDS and Behavior, 24(7), 1990–1993. https://doi.org/10.1007/s10461-020-02926-x.
[23] International Center for AIDS Care and Treatment Program. (2020). Zimbabwe population-based HIV impact assessment. https://phia.icap.columbia.edu/zimbabwe2020-final-report/.
[24] Aniteye, P., & Mayhew, S.H. (2013). Shaping legal abortion provision in Ghana: Using policy theory to understand provider-related obstacles to policy implementation. Health Research and Policy Systems, 11(23). https://doi.org/10.1186/1478-4505-11-23.
[25] Bennett, S., Mahmood, S.S., Edward, A., Tetui, M. & Ekirapa-Kiracho, E. (2017). Strengthening scaling up through learning from implementation: Comparing experiences from Afghanistan, Bangladesh and Uganda. Health Research and Policy Systems, 15(108). https://doi.org/10.1186/s12961-017-0270-0.
[26] Tong, A., Sainsbury, P., & Craig, J. (2007). Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. International Journal for Quality in Health Care, 19(6), 349–357. https://doi.org/10.1093/intqhc/mzm042.
[27] Saunders, B., Sim, J., Kingstone, T., Baker, S., Waterfield, J., Bartlam, B., Burroughs, H., & Jinks, C. (2018). Saturation in qualitative research: Exploring its conceptualization and operationalization. Quality & Quantity, 52(4), 1893–1907. https://doi.org/10.1007/s11135-017-0574-8.
[28] Iliffe, S., Wilcock, J., Drennan, V., Goodman, C., Griffin, M., Knapp, M., Lowery, D., Manthorpe, J., Rait, G., & Warner, J. (2015). Changing practice in dementia care in the community: Developing and testing evidence-based interventions, from timely diagnosis to end of life (EVIDEM). Programme Grants for Applied Research, 3(3), 1–596. https://doi.org/10.3310/pgfar03030.
[29] Chang, C.-P., Lee, T.-T., & Mills, M. E. (2013). Telecare for the elderly—Community nurses’ experiences in Taiwan. Computers, Informatics, Nursing: CIN, 31(1), 29–35. https://doi.org/10.1097/NXN.0b013e318266ca94.
[30] Adeloye, D., Adigun, T., Misra, S., & Omoregbe, N. (2017). Assessing the Coverage of E-Health Services in Sub-Saharan Africa: A Systematic Review and Analysis. Methods of Information in Medicine, 56(03), 189–199. https://doi.org/10.3414/ME16-05-0012.
[31] Aranda-Jan, C. B., Mohutsiwa-Dibe, N., & Loukanova, S. (2014). Systematic review on what works, what does not work and why of implementation of mobile health (mHealth) projects in Africa. BMC Public Health, 14, 188. https://doi.org/10.1186/1471-2458-14-188.
[32] Kruse, C., Betancourt, J., Ortiz, S., Valdes Luna, S. M., Bamrah, I. K., & Segovia, N. (2019). Barriers to the Use of Mobile Health in Improving Health Outcomes in Developing Countries: Systematic Review. Journal of Medical Internet Research, 21(10), e13263. https://doi.org/10.2196/13263.
[33] Yelverton, V., Qiao, S., Weissman, S., Olatosi, B., & Li, X. (2021). Telehealth for HIV Care Services in South Carolina: Utilization, Barriers, and Promotion Strategies During the COVID-19 Pandemic. AIDS and Behavior, 25(12), 3909–3921. https://doi.org/10.1007/s10461-021-03349-y.
[34] Mulawa, M. I., Rosengren, A. L., Amico, K. R., Hightow-Weidman, L. B., & Muessig, K. E. (2021). mHealth to reduce HIV-related stigma among youth in the United States: A scoping review. MHealth, 7, 35. https://doi.org/10.21037/mhealth-20-68.
[35] Asah, F. N., Kaasbøll, J. J., & Anthun, K. S. (2022). Obstacles of eHealth Capacity Building and Innovation Promotion Initiative in African Countries. In B. Blobel, B. Yang, & M. Giacomini (Eds.), Studies in Health Technology and Informatics. IOS Press. https://doi.org/10.3233/SHTI220961.
[36] Queirós, A., Faria, D., & Almeida, F. (2017). Strengths and limitations of qualitative and quantitative research methods. European Journal of Education Studies. 3(9).a.
Viewed PDF 724 24 -
 Seasonal Malaria Chemo-Prevention Strategy: A Cross-Sectional Study of Healthcare Workers in Public Primary Healthcare Facilities in Edo State, NigeriaAuthor: Emmanuel Friday OsagiedeDOI: 10.21522/TIJPH.2013.11.04.Art010
Seasonal Malaria Chemo-Prevention Strategy: A Cross-Sectional Study of Healthcare Workers in Public Primary Healthcare Facilities in Edo State, NigeriaAuthor: Emmanuel Friday OsagiedeDOI: 10.21522/TIJPH.2013.11.04.Art010Seasonal Malaria Chemo-Prevention Strategy: A Cross-Sectional Study of Healthcare Workers in Public Primary Healthcare Facilities in Edo State, Nigeria
Abstract:
Malaria infection is one of the most significant public health problems and the leading cause of global morbidity and mortality. Pregnant women and under-five (U5) children are particularly at risk in areas where malaria is endemic. The U5 children account for about 80% of all malaria-related deaths. This study aims to assess the adherence to the national guidelines for administering seasonal malaria chemoprevention (SMC) in U5 children by healthcare workers (HCWs) working in public Primary Health Care (PHC) facilities in Edo State, Nigeria. A cross-sectional study design was employed to assess the sociodemographic characteristics, awareness, and prescription of chemo-preventive therapy for the U5 by 200 HCWs in public PHC facilities in Edo State, with the aid of the researcher-designed pretested, self-administered, semi-structured questionnaire. Descriptive and inferential data analyses were carried out using the IBM SPSS version 20 software. All p-values had two tails and were deemed statistically significant if < 0.05. The majority of HCWs (71.5%) did not adhere to the national guideline for using chemo-preventive treatment for malaria in children, and there was a statistically significant relationship between many sociodemographic factors and compliance. The length of the HCW’s work (in years) was a critical indicator of compliance with the recommendation. In conclusion, the use of malaria chemo-preventive treatment in accordance with the Nigerian malaria diagnosis and treatment guidelines is being practiced ineffectively by HCWs in public PHCs in Edo State. A longer period of employment (in years) predicts a better practice.
Keywords: Implementation, Nigeria, Primary healthcare (PHC), Seasonal malaria chemoprevention (SMC), Under-five children.Seasonal Malaria Chemo-Prevention Strategy: A Cross-Sectional Study of Healthcare Workers in Public Primary Healthcare Facilities in Edo State, Nigeria
References:
[1] CDC, “Malaria’s Impact Worldwide,” Washington D. C., Feb. 2021.
[2] World Health Organization, “Malaria,” Malaria. WHO, Geneva, pp. 1–4, 2022. Accessed: Mar. 14, 2022. [Online]. Available: https://www.who.int/data/gho/data/themes/malaria.
[3] Centers for Disease Control and Prevention, “About Malaria,” U.S. Department of Health & Human Services, Dec. 12, 2021.
[4] P. Jagannathan and A. Kakuru, “Malaria in 2022: Increasing challenges, cautious optimism,” Nature Communications, vol. 13, no. 1. Nature Research, Dec. 01, 2022. Doi: 10.1038/s41467-022-30133-w.
[5] G. Gachelin, P. Garner, E. Ferroni, J. P. Verhave, and A. Opinel, “Evidence and strategies for malaria prevention and control: a historical analysis,” Malar J, vol. 17, no. 1, p. 96, Dec. 2018, Doi: 10.1186/s12936-018-2244-2.
[6] WHO, “Promoting malaria chemoprevention,” Geneva, Jun. 2022. Accessed: Sep. 03, 2023. [Online]. Available: https://www.who.int/activities/promoting-malaria-chemoprevention#.
[7] A. B. Tiono, A. Ouédraogo, C. Remy, and K. Hamed, “Treatment of Asymptomatic Carriers of Plasmodium falciparum with Artemether–Lumefantrine: Impact on the Prevalence of Anemia,” Infect Dis Ther, vol. 2, no. 1, pp. 47–58, Jun. 2013, Doi: 10.1007/s40121-013-0005-7.
[8] Federal Ministry of Health Nigeria, “National Guidelines for Diagnosis and Treatment of Malaria.,” Abuja, May 2020. Accessed: Feb. 15, 2022. [Online]. Available: https://mcp.gov.ng.
[9] C. Paul, R. Kramer, A. Lesser, C. Mutero, M. L. Miranda, and K. Dickinson, “Identifying barriers in the malaria control policymaking process in East Africa: insights from stakeholders and a structured literature review,” BMC Public Health, vol. 15, no. 1, p. 862, Dec. 2015, Doi: 10.1186/s12889-015-2183-6.
[10] D. M. Maslove, A. Mnyusiwalla, E. J. Mills, J. McGowan, A. Attaran, and K. Wilson, “Barriers to the effective treatment and prevention of malaria in Africa: A systematic review of qualitative studies,” BMC Int Health Hum Rights, vol. 9, no. 1, p. 26, Dec. 2009, Doi: 10.1186/1472-698X-9-26.
[11] Edo State Ministry of Health, “Edo State Government: State strategic health development plan (2010-2015),” Benin City, Nigeria., 2010.
[12] Edo State Ministry of Health, “2011 survey of health facilities in Edo State (Unpublished).,” Benin, 2011.
[13] Edo State Government, “Edo State Primary Healthcare Development Agency (EDPHCDA-PHCUOR) Implementation Committee Final Report,” Benin City, Nov. 2021.
[14] Edo State Government of Nigeria, “Primary Healthcare Under One Roof (PHCUOR) Implementation Committee’s Final Report,” Benin City, Nov. 2021.
[15] G. Cochran, Sampling Techniques, 2nd ed. New York: John Wiley and Sons, Inc., 1963.
[16] A. Mpimbaza et al., “Adherence to malaria management guidelines by health care workers in the Busoga sub-region, eastern Uganda,” Malar J, vol. 21, no. 1, p. 25, Jan. 2022, Doi: 10.1186/s12936-022-04048-2.
[17] R. Saadeh et al., “Osteoporosis among Postmenopausal Women in Jordan: A National Cross-Sectional Study,” Int J Environ Res Public Health, vol. 19, no. 14, p. 8803, Jul. 2022, Doi: 10.3390/ijerph19148803.
[18] IBM SPSS., “Statistical Package for the Social Sciences (SPSS) version 20.0. IBM SPSS;” 2014.
[19] C. V. Plowe, “Malaria chemoprevention and drug resistance: a review of the literature and policy implications,” Malar J, vol. 21, no. 1, p. 104, Mar. 2022, Doi: 10.1186/s12936-022-04115-8.
[20] S. Chatio, N. A. Ansah, D. A. Awuni, A. Oduro, and P. O. Ansah, “Community acceptability of
Seasonal Malaria Chemoprevention of morbidity and mortality in young children: A qualitative study in the Upper West Region of Ghana,” Plos One, vol. 14, no. 5, p. e0216486, May 2019, Doi: 10.1371/journal.pone.0216486.[21] WHO, “Updated WHO recommendations for malaria chemoprevention among children and pregnant women,” Geneva, Jun. 2022. Accessed: Aug. 20, 2023. [Online]. Available: https://www.who.int/news/item/03-06-2022-Updated-WHO-recommendations-for-malaria-chemoprevention-among-children-and-pregnant-women.
[22] H. J. Oladipo et al., “Increasing challenges of malaria control in sub-Saharan Africa: Priorities for public health research and policymakers,” Annals of Medicine & Surgery, vol. 81, Sep. 2022, Doi: 10.1016/j.amsu.2022.104366.
Viewed PDF 708 20 -
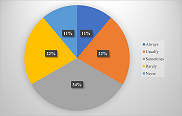 Social Media and Dental Practitioner's Knowledge of Misinformation, Infodemic and Fact-Checking on Dental InformationAuthor: Sachin NaikDOI: 10.21522/TIJPH.2013.11.04.Art011
Social Media and Dental Practitioner's Knowledge of Misinformation, Infodemic and Fact-Checking on Dental InformationAuthor: Sachin NaikDOI: 10.21522/TIJPH.2013.11.04.Art011Social Media and Dental Practitioner's Knowledge of Misinformation, Infodemic and Fact-Checking on Dental Information
Abstract:
Social media is currently among the most popular web activities among dental professionals. The study aimed to assess social media usage, knowledge about misinformation, infodemic and fact-checking among dental professionals on dental information. The current study design was a descriptive cross-sectional study conducted among dental professionals from Riyadh City, Saudi Arabia. The questionnaire comprised demographic data of study participants and knowledge about misinformation, infodemic and fact-checking about social media use for their dental profession. Descriptive statistics were used for analysis. A total of 1192 dental practitioners responded to the questionnaire. In our study, most participating dentists were young and had 1-5 years of experience (51%). Most participants responded that sometimes (49%), they fact-check social media content about dental information. The google is the most used to check the fact content. About 90% of dentists never received notification about factual errors. The knowledge about misinformation and fact-checking is moderate among dental practitioners.
Keywords: Dental practitioner, Dentists, Descriptive study, Fact-checking, Misinformation, social media.Social Media and Dental Practitioner's Knowledge of Misinformation, Infodemic and Fact-Checking on Dental Information
References:
[1] M. Muhlen and L. Ohno-Machado, “Reviewing social media use by clinicians,” J. Am. Med. Inform. Assoc., vol. 19, no. 5, p. 777, Sep. 2012, doi: 10.1136/AMIAJNL-2012-000990.
[2] “Saudi Arabia: social network penetration 2017 | Statista.” https://www.statista.com/statistics/284451/saudi-arabia-social-network-penetration/ (accessed Dec. 27, 2022).
[3] “Saudi Arabia: social media user growth 2022 | Statista.” https://www.statista.com/statistics/1318265/saudi-arabia-social-media-user-growth/ (accessed Sep. 16, 2022).
[4] S. A. Moorhead, D. E. Hazlett, L. Harrison, J. K. Carroll, A. Irwin, and C. Hoving, “A new dimension of health care: Systematic review of the uses, benefits, and limitations of social media for health communication,” J. Med. Internet Res., vol. 15, no. 4, 2013, doi: 10.2196/JMIR.1933.
[5] C. Lee Ventola, “Social Media and Health Care Professionals: Benefits, Risks, and Best Practices,” Pharm. Ther., vol. 39, no. 7, p. 491, 2014.
[6] M. A. Dias da Silva and A. D. Walmsley, “Fake news and dental education,” Br. Dent. J. 2019 2266, vol. 226, no. 6, pp. 397–399, Mar. 2019, doi: 10.1038/s41415-019-0079-z.
[7] “Charcoal Toothpaste: What Is It? | Colgate® Oral Care.” https://www.colgate.com/en-sg/oral-health/selecting-dental-products/charcoal-toothpaste--what-is-it (accessed Feb. 11, 2023).
[8] C. Snijders, R. Conijn, E. de Fouw, and K. van Berlo, “Humans and Algorithms Detecting Fake News: Effects of Individual and Contextual Confidence on Trust in Algorithmic Advice,” Int. J. Human–Computer Interact., vol. 39, no. 7, pp. 1483–1494, 2023, doi: 10.1080/10447318.2022.2097601.
[9] R. W. Law, S. Kanagasingam, and K. A. Choong, “Sensationalist social media usage by doctors and dentists during Covid-19:” Digit. Heal., vol. 7, pp. 1–2, 2021, doi: 10.1177/20552076211028034.
[10] A. A. AlBaker, Y. S. H. Al-Ruthia, M. AlShehri, and S. Alshuwairikh, “The characteristics and distribution of dentist workforce in Saudi Arabia: A descriptive cross-sectional study,” Saudi Pharm. J., vol. 25, no. 8, pp. 1208–1216, Dec. 2017, doi: 10.1016/j.jsps.2017.09.005.
[11] Makkar, D. Lawrence, D. Veeresh, A. Banik, A. Kumar, and A. S. Mehar, “Assessment of social media usage and its influence among dental faculty members in Davangere city – A cross sectional survey,” J. Indian Assoc. Public Heal. Dent., vol. 16, no. 3, p. 246, 2021, doi: 10.4103/JIAPHD.JIAPHD_143_17.
[12] F. D. Davis, “Perceived usefulness, perceived ease of use, and user acceptance of information technology,” MIS Q. Manag. Inf. Syst., vol. 13, no. 3, pp. 319–339, 1989, doi: 10.2307/249008.
[13] R. M. Merchant and D. A. Asch, “Protecting the Value of Medical Science in the Age of social media and ‘Fake News,’” JAMA, vol. 320, no. 23, pp. 2415–2416, Dec. 2018, doi: 10.1001/JAMA.2018.18416.
[14] P. M. Waszak, W. Kasprzycka-Waszak, and A. Kubanek, “The spread of medical fake news in social media – The pilot quantitative study,” Heal. Policy Technol., vol. 7, no. 2, pp. 115–118, Jun. 2018, doi: 10.1016/j.hlpt.2018.03.002.
[15] A. Ho, C. McGrath, and N. Mattheos, “Social media patient testimonials in implant dentistry:
information or misinformation?” Clin. Oral Implants Res., vol. 28, no. 7, pp. 791–800, 2017, doi: 10.1111/clr.12883.[16] S. H. Al-Amad and A. Hussein, “Anxiety among dental professionals and its association with their dependency on social media for health information: insights from the COVID-19 pandemic,” BMC Psychol. 2021 91, vol. 9, no. 1, pp. 1–9, 2021, doi: 10.1186/S40359-020-00509-Y.
[17] C. M. David Laze, Matthew Baum, Nir Grinberg, Lisa Friedland, Kenneth Joseph, Will Hobbs, “Combating Fake News: An Agenda for Research and Action | Shorenstein Center,” 2017. https://shorensteincenter.org/combating-fake-news-agenda-for-research/ (accessed Feb. 16, 2023).
[18] M. A. Dias da Silva and A. D. Walmsley, “Fake news and dental education,” Br. Dent. J. 2019 2266, vol. 226, no. 6, pp. 397–399, 2019, doi: 10.1038/s41415-019-0079-z.
[19] C. J. Gary, “Fake News in Dentistry: Misinformed Consent. False and misleading information, easily accessible online, is complicating dentists’ ethical and legal responsibility to provide their patients with the best possible treatment.,” N. Y. State Dent. J., vol. 83, no. 2, pp. 2–3, Mar. 2017.
[20] J. Melkers, D. Hicks, S. Rosenblum, K. R. Isett, and J. Elliott, “Dental Blogs, Podcasts, and Associated Social Media: Descriptive Mapping and Analysis,” J. Med. Internet Res., vol. 19, no. 7, 2017, doi: 10.2196/JMIR.7868.
Viewed PDF 599 21 -
Analysis of Caesarean Delivery in General Hospitals in Sokoto State Using Robson’s Ten Classification: A Cross-Sectional StudyAuthor: Jennifer Adaeze ChukwuDOI: 10.21522/TIJPH.2013.11.04.Art012
Analysis of Caesarean Delivery in General Hospitals in Sokoto State Using Robson’s Ten Classification: A Cross-Sectional Study
Analysis of Caesarean Delivery in General Hospitals in Sokoto State Using Robson’s Ten Classification: A Cross-Sectional Study
References:
[1] Meh, C.; Thind, A.; Ryan, B.; Terry, A. Levels and Determinants of Maternal Mortality in Northern and Southern Nigeria. BMC Pregnancy Childbirth 2019, 19, 1–13, doi:10.1186/S12884-019-2471-8/TABLES/3.
[2] Thompson, J.F.; Roberts, C.L.; Currie, M.; Ellwood, D.A. Prevalence and Persistence of Health Problems after Childbirth: Associations with Parity and Method of Birth. Birth 2002, 29, 83–94, doi:10.1046/J.1523-536X.2002.00167. X.
[3] Office of Communications NIH What Are Some Common Complications during Labor and Delivery? | NICHD - Eunice Kennedy Shriver National Institute of Child Health and Human Development Available online: https://www.nichd.nih.gov/health/topics/labor-delivery/topicinfo/complications# (accessed on 22 January 2023).
[4] WHO Maternal Health - GLOBAL Available online: https://www.who.int/health-topics/maternal-health#tab=tab_2 (accessed on 20 January 2023).
[5] Hamad, R.; Rehkopf, D.H. Poverty, Pregnancy, and Birth Outcomes: A Study of the Earned Income Tax Credit. Paediatr. Perinat. Epidemiol. 2015, 29, 444, doi:10.1111/PPE.12211.
[6] National Bureau of Statistics Nigeria Launches Its Most Extensive National Measure of Multidimentaional Poverty Available online: https://nigerianstat.gov.ng/news/78 (accessed on 22 January 2023).
[7] DailyTimes 40,000 Women Die from Pregnancy-Related Complications Yearly in Nigeria - Official Available online: https://www.premiumtimesng.com/news/headlines/516133-40000-women-die-from-pregnancy-related-complications-yearly-in-nigeria-official.html (accessed on 22 January 2023).
[8] Adewuyi, E.O.; Auta, A.; Khanal, V.; Tapshak, S.J.; Zhao, Y. Cesarean Delivery in Nigeria: Prevalence and Associated Factors―a Population-Based Cross-Sectional Study. BMJ Open 2019, 9, doi:10.1136/BMJOPEN-2018-027273.
[9] Ngongo, C.J.; Raassen, T.J.I.P.; Mahendeka, M.; Lombard, L.; van Roosmalen, J. Iatrogenic Genito-Urinary Fistula Following Cesarean Birth in Nine Sub-Saharan African Countries: A Retrospective Review. BMC Pregnancy Childbirth 2022, 22, doi:10.1186/S12884-022-04774-0.
[10] Maddah, G.; Fattahi, A.S.; Rahnama, A.; Jamshidi, S.T. Uterocutaneous Fistula Following Cesarean Section: Successful Management of a Case - PMC. 2016, 41, 157–160.
[11] Amutah-Onukagha, N.; Rodriguez, M.; Opara, MPH, I.; Gardner, M.; Assan, M.A.; Hammond, R.; Plata, J.; Pierre, K.; Farag, E. Progresses and Challenges of Utilizing Traditional Birth Attendants in Maternal and Child Health in Nigeria. Int. J. MCH AIDS 2017, 6, 130, doi:10.21106/IJMA.216.
[12] United Nations Development Programme Nigeria MDGs End-Point Report 2015 | United Nations Development Programme Available online: https://www.undp.org/nigeria/publications/nigeria-mdgs-end-point-report-2015 (accessed on 22 January 2023).
[13] Iwu, C.A.; Uwakwe, K.; Oluoha, U.; Duru, C.; Nwaigbo, E. Empowering Traditional Birth Attendants as Agents of Maternal and Neonatal Immunization Uptake in Nigeria: A Repeated Measures Design. BMC Public Health 2021, 21, 1–8, doi:10.1186/S12889-021-10311-Z/FIGURES/3.
[14] Abubeker, F.A.; Gashawbeza, B.; Gebre, T.M.; Wondafrash, M.; Teklu, A.M.; Degu, D.; Bekele, D. Analysis of Cesarean Section Rates Using Robson Ten Group Classification System in a Tertiary Teaching Hospital, Addis Ababa, Ethiopia: A Cross-Sectional Study. BMC Pregnancy Childbirth 2020, 20, 1–7, doi:10.1186/S12884-020-03474-X/TABLES/3.
[15] WHO; UNFPA; UNICEF; AMDD Monitoring Emergency Obstetric Care: A Handbook Available online: https://apps.who.int/iris/handle/10665/44121 (accessed on 20 January 2023).
[16] Robson, M.; Hartigan, L.; Murphy, M. Methods of Achieving and Maintaining an Appropriate Caesarean Section Rate. Best Pract. Res. Clin. Obstet. Gynaecol. 2013, 27, 297–308, doi: 10.1016/J.BPOBGYN.2012.09.004.
[17] WHO WHO Statement on Caesarean Section Rates. Reprod. Health Matters 2015, 23, 149–150, doi: 10.1016/J.RHM.2015.07.007.
[18] Betran, A.P.; Ye, J.; Moller, A.B.; Souza, J.P.; Zhang, J. Trends and Projections of Caesarean Section Rates: Global and Regional Estimates. BMJ Glob. Heal. 2021, 6, doi:10.1136/BMJGH-2021-005671.
[19] Okoli, U.; Morris, L.; Oshin, A.; Pate, M.A.; Aigbe, C.; Muhammad, A. Conditional Cash Transfer Schemes in Nigeria: Potential Gains for Maternal and Child Health Service Uptake in a National Pilot Programme. BMC Pregnancy Childbirth 2014, 14, 1–13, doi:10.1186/S12884-014-0408-9/TABLES/4.
[20] Alsulami, S.M.; Ashmawi, M.T.; Jarwan, R.O.; Malli, I.A.; Albar, S.K.; Al-Jifree, H.M. The Rates of Cesarean Section Deliveries According to Robson Classification System During the Year of 2018 Among Patients in King Abdul-Aziz Medical City, Jeddah, Saudi Arabia. Cureus 2020, 12, doi:10.7759/CUREUS.11529.
[21] Bayrampour, H.; Heaman, M. Comparison of Demographic and Obstetric Characteristics of Canadian Primiparous Women of Advanced Maternal Age and Younger Age. J. Obstet. Gynaecol. Can. 2011, 33, 820–829, doi:10.1016/S1701-2163(16)34985-4.
[22] Olowolafe, T.A.; Adebowale, A.S.; Fagbamigbe, A.F.; Bolarinwa, O.A.; Akinyemi, J.O. Shifts in Age Pattern, Timing of Childbearing and Trend in Fertility Level across Six Regions of Nigeria: Nigeria Demographic and Health Surveys from 2003–2018. Plos One 2023, 18, doi: 10.1371/JOURNAL.PONE.0279365.
[23] Bolarinwa, O.A.; Tessema, Z.T.; Frimpong, J.B.; Babalola, T.O.; Ahinkorah, B.O.; Seidu, A.A. Spatial Distribution and Factors Associated with Adolescent Pregnancy in Nigeria: A Multi-Level Analysis. Arch. Public Heal. 2022, 80, 1–13, doi:10.1186/S13690-022-00789-3/TABLES/2.
[24] Sah, S.; Goel, R.; Goel, J.K. Analysis of Caesarean Section Rate According to Robson’s Criteria in Tertiary Care Centre. Int. J. Reprod. Contraception, Obstet. Gynecol. 2018, 7, 3060–3064, doi:10.18203/2320-1770.IJRCOG20182947.
[25] Triunfo, S.; Ferrazzani, S.; Lanzone, A.; Scambia, G. Identification of Obstetric Targets for Reducing Cesarean Section Rate Using the Robson Ten Group Classification in a Tertiary Level Hospital. Eur. J. Obstet. Gynecol. Reprod. Biol. 2015, 189, 91–95, doi: 10.1016/J.EJOGRB.2015.03.030.
[26] Costa, M.L.; Cecatti, J.G.; Souza, J.P.; Milanez, H.M.; Gülmezoglu, M.A. Using a Caesarean Section Classification System Based on Characteristics of the Population as a Way of Monitoring Obstetric Practice. Reprod. Health 2010, 7, 13, doi:10.1186/1742-4755-7-13.
[27] Litorp, H.; Kidanto, H.L.; Nystrom, L.; Darj, E.; Essén, B. Increasing Caesarean Section Rates among Low-Risk Groups: A Panel Study Classifying Deliveries According to Robson at a University Hospital in Tanzania. BMC Pregnancy Childbirth 2013, 13, 1–10, doi:10.1186/1471-2393-13-107/TABLES/4.
[28] Parveen, R.; Khakwani, M.; Naz, A.; Bhatti, R. Analysis of Cesarean Sections Using Robson’s Ten Group Classification System. Pakistan J. Med. Sci. 2021, 37, 567, doi:10.12669/PJMS.37.2.3823.
[29] Akadri, A.A.; Imaralu, J.O.; Salami, O.F.; Nwankpa, C.C.; Adepoju, A.A. Robson Classification of Caesarean Births: Implications for Reducing Caesarean Section Rate in a Private Tertiary Hospital in Nigeria. BMC Pregnancy Childbirth 2023, 23, 1–8, doi:10.1186/S12884-023-05557-X/TABLES/5.
[30] Ochejele, S.; Emoekpere, H.; Nkawu, M.; Alagh, M. Robson Classification of Caesarean Sections at the Federal Medical Centre, Makurdi. Trop. J. Obstet. Gynaecol. 2021, 38, 261–265.
Viewed PDF 710 25 -
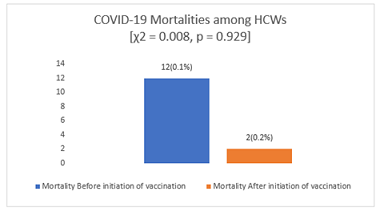 Prevalence and Factors Associated with Covid-19 Infection and Mortality Among Frontline Healthcare Workers in Kaduna StateAuthor: Hananiya Dauda SamuelDOI: 10.21522/TIJPH.2013.11.04.Art013
Prevalence and Factors Associated with Covid-19 Infection and Mortality Among Frontline Healthcare Workers in Kaduna StateAuthor: Hananiya Dauda SamuelDOI: 10.21522/TIJPH.2013.11.04.Art013Prevalence and Factors Associated with Covid-19 Infection and Mortality Among Frontline Healthcare Workers in Kaduna State
Abstract:
This study in Kaduna State, Nigeria, examined the prevalence, and factors as associated with COVID-19 infection and mortality among frontline healthcare workers (HCWs) in a descriptive, cross- sectional study, where data of HCWs from secondary source, Surveillance Outbreak Response Management and Analysis System (SORMAS), was exported to Microsoft excel and evaluated using SPSS version 26 to provide a snapshot of the vaccine uptake among HCWs in Kaduna state. The study population were all healthcare workers in Kaduna State, Nigeria that were tested for COVID-19 from the onset of the pandemic in Kaduna to 29th August 2022. The consents of all persons were obtained prior to testing data upload to the electronic platform of SORMAS. Prevalence of COVID-19 infection was notably higher pre-vaccination (12%) but dropped to 5.9% post-vaccination, showcasing the vaccine’s effectiveness in reducing HCW infections. However, COVID-19-related mortality rates remained relatively consistent, irrespective of vaccination status. Demographics played a role in infection risk. Female HCWs, urban dwellers, and those with higher education levels faced elevated infection risks. Additionally, close contacts with probable COVID-19 cases increased infection likelihood. Concerning mortality, males experienced more COVID-19-related deaths, but no significant links were found with age, residential area, or contact history. Symptoms significantly associated with COVID-19 infection included fever, abdominal pain, cough, sore throat, loss of taste, and loss of smell. The prevalence of COVID-19 infection among the HCWs was higher before the COVID-19 vaccination was introduced (12%) compared to after the vaccine was introduced in Kaduna State. These findings offer valuable insights into the pandemic’s impact on frontline workers in Nigeria’s Kaduna State.
Keywords: COVID-19, Healthcare workers (HCWs), Infection, Vaccination, Mortality, Prevalence, Risk factors, Symptoms, mental, Psychological.Prevalence and Factors Associated with Covid-19 Infection and Mortality Among Frontline Healthcare Workers in Kaduna State
References:
[1] Poudel K, Subedi P. Impact of COVID-19 pandemic on socioeconomic and mental health aspects in Nepal. Int J Soc Psychiatry. 2020;66(8):748–55.
[2] Tong X, Ning M, Huang R, Jia B, Yan X, Xiong Y, et al. Surveillance of SARS-CoV-2 infection among frontline health care workers in Wuhan during COVID-19 outbreak. Immunity, Inflamm Dis. 2020;8(4):840–3.
[3] Abdel Wahed WY, Hefzy EM, Ahmed MI, Hamed NS. Assessment of Knowledge, Attitudes, and Perception of Health Care Workers Regarding COVID-19, A Cross-Sectional Study from Egypt. J Community Health [Internet]. 2020;45(6):1242–51. Available from: https://doi.org/10.1007/s10900-020-00882-0.
[4] Htay MNN, Marzo RR, Bahari R, AlRifai A, Kamberi F, El-Abasiri RA, et al. How healthcare workers are coping with mental health challenges during COVID-19 pandemic? -A cross-sectional multi-countries study. Clin Epidemiol Glob Heal. 2021;11:100759.
[5] World Health Organization. The impact of COVID-19 on health and care workers: a closer look at deaths. Health Workforce Department - Working Paper 1. Geneva; 2021.
[6] Organization WH. Joint WHO/ILO policy guidelines on improving health worker access to prevention, treatment and care services for HIV and TB. 2010.
[7] Wu Z, McGoogan JM. Characteristics of and Important Lessons from the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72314 Cases from the Chinese Center for Disease Control and Prevention. JAMA - J Am Med Assoc. 2020;323(13):1239–42.
[8] Peckham H, de Gruijter NM, Raine C, Radziszewska A, Ciurtin C, Wedderburn LR, et al. Male sex identified by global COVID-19 meta-analysis as a risk factor for death and ITU admission. Nat Commun. 2020;11(1):1–10.
[9] Mariam Saleh. • Africa: COVID-19 vaccination rate by country [Internet]. 2022 [cited 2022 Jul 2]. p. 1–2. Available from: https://www.statista.com/statistics/1221298/covid-19-vaccination-rate-in-african-countries/.
[10] Organization WH. WHO Regional Committee for South-East Asia: Report of the Seventy-third session, Thailand (Virtual), 9-10 September 2020. World Health Organization. Regional Office for South-East Asia; 2021.
[11] Commission NP. Priority table, volume four: Population distribution by age and sex. Natl Popul Comm Abuja. 2010.
[12] Stephen RI, Olumoh J, Tyndall J, Adegboye O. Risk Factors for COVID-19 Infection among Healthcare Workers in North-East Nigeria. Healthc. 2022;10(10).
[13] Alasia DD, Maduka O. Prevalence and Pattern of COVID-19 among Healthcare Workers in Rivers State Nigeria. Occup Dis Environ Med. 2021;09(01):20–32.
[14] Alajmi J, Jeremijenko AM, Abraham JC, Alishaq M, Concepcion EG, Butt AA, et al. COVID-19 infection among healthcare workers in a national healthcare system: The Qatar experience. Int J Infect Dis. 2020;100:386–9.
[15] The Centers for Disease Control and Prevention. Characteristics of Health Care Personnel with COVID-19 —. MMWR Morb Mortal Wkly Rep. 2020;69(15):477–81.
[16] Dzinamarira T, Nkambule SJ, Hlongwa M, Mhango M, Iradukunda PG, Chitungo I, et al. Risk Factors for COVID-19 Infection Among Healthcare Workers. A First Report from a Living Systematic Review and meta-Analysis. Saf Health Work. 2022;13(3):263–8.
[17] Soegiarto G, Purnomosari D, Wulandari L, Mahdi BA, Fahmita KD, Hadmoko ST, et al. Incidence of SARS-CoV-2 infection in hospital workers before and after vaccination programme in East Java, Indonesia–A retrospective cohort study. Lancet Reg Heal - Southeast Asia. 2023;10(December 2022):100130.
[18] Elsayed MEG, El-Abasiri RA, Marzo RR, Dardeer KT, Kamal MA, Abdelaziz H, et al. Mental health, risk perception, and coping strategies among healthcare workers in Egypt during the COVID-19 pandemic. PLoS One. 2023;18(2):e0282264.
[19] Marzo RR, ElSherif M, Abdullah MSAM Bin, Thew HZ, Chong C, Soh SY, et al. Demographic and work-related factors associated with burnout, resilience, and quality of life among healthcare workers during the COVID-19 pandemic: A cross sectional study from Malaysia. Front Public Heal. 2022;10:1021495.
[20] Marzo RR, Khaled Y, ElSherif M, Abdullah MSAM Bin, Zhu Thew H, Chong C, et al. Burnout, resilience and the quality of life among Malaysian healthcare workers during the COVID-19 pandemic. Front Public Heal. 2022;10:1021497.
[21] Hwaij RA, Ghrayeb F, Marzo RR, AlRifai A. Palestinian healthcare workers mental health challenges during COVID-19 pandemic: a cross-sectional study. Med Res Arch. 2022;10(10).
[22] RilleraMarzo R, Villanueva Iii EQ, Chandra U, Htay MNN, Shrestha R, Shrestha S. Risk perception, mental health impacts and coping strategies during COVID-19 pandemic among Filipino healthcare workers. J Public health Res. 2021;10(2_suppl):jphr-2021.
[23] Kamberi F, Sinaj E, Jaho J, Subashi B, Sinanaj G, Jaupaj K, et al. Impact of COVID-19 pandemic on mental health, risk perception and coping strategies among health care workers in Albania-evidence that needs attention. Clin Epidemiol Glob Heal. 2021;12:100824.
[24] Htay MNN, Marzo RR, AlRifai A, Kamberi F, El-Abasiri RA, Nyamache JM, et al. Immediate impact of COVID-19 on mental health and its associated factors among healthcare workers: A global perspective across 31 countries. J Glob Health. 2020;10(2).
[25] Chandan S, Khan SR, Deliwala S, Mohan BP, Ramai D, Chandan OC, et al. Postvaccination SARS‐CoV‐2 infection among healthcare workers – A Systematic Review and meta‐analysis. J Med Virol. 2021;1–14.
[26] Bruxvoort KJ, Sy LS, Qian L, Ackerson BK, Luo Y, Lee GS, et al. Effectiveness of mRNA-1273 against delta, mu, and other emerging variants of SARS-CoV-2: Test negative case-control study. BMJ. 2021;375:1–10.
[27] Chemaitelly H, Yassine HM, Benslimane FM, Al Khatib HA, Tang P, Hasan MR, et al. mRNA-1273 COVID-19 vaccine effectiveness against the B.1.1.7 and B.1.351 variants and severe COVID-19 disease in Qatar. Nat Med. 2021;27(9):1614–21.
[28] Elimian K, Musah A, King C, Igumbor E, Myles P, Aderinola O, et al. COVID-19 mortality rate and its associated factors during the first and second waves in Nigeria. PLOS Glob Public Heal. 2022;2(6):e0000169.
[29] Elimian KO, Ochu CL, Ebhodaghe B, Myles P, Crawford EE, Igumbor E, et al. Patient characteristics associated with COVID-19 positivity and fatality in Nigeria: Retrospective cohort study. BMJ Open. 2020;10(12):1–16.
[30] Matheson J, Nathan M, Pickard H, Vanino E. Why has coronavirus affected cities more than rural areas? Economics Observatory. 2020.
[31] Raghupathi V, Raghupathi W. The influence of education on health: an empirical assessment of OECD countries for the period 1995 – 2015. Arch Public Heal. 2020;78:20.
[32] Abdullah M, Chai P, Chong M, Tohit E, Ramasamy R, Pei C, et al. Gender effect on in vitro lymphocyte subset levels of healthy individuals. Cell Immunol. 2012;272(2):214–9.
[33] Ekawati LL, Arif A, Hidayana I, Nurhasim A, Munziri MZ, Lestari KD, et al. Mortality among healthcare workers in Indonesia during 18 months of COVID-19. PLOS Glob Public Heal. 2022;2(12):e0000893.
Viewed PDF 696 21 -
Impacts of Early Marriage on Fertility Outcomes in NigeriaAuthor: Muhamma Murtala IbrahimDOI: 10.21522/TIJPH.2013.11.04.Art014
Impacts of Early Marriage on Fertility Outcomes in Nigeria
Abstract:
Nigeria is the most populous country in Africa and projected to be the 3rd in the World by 2050. Despite measures to control the country’s population over the years, the total fertility rate has remained high. Fertility rate is associated with various factors but there is limited evidence on the role of early marriage as a predictor or barrier to fertility outcome. This study determined the association between early marriage and fertility outcome in Nigeria. This study is based on secondary data analysis of the 2018 Nigeria Demographic and Health Survey (NDHS). It is a descriptive cross-sectional study with sample that comprised of married women aged 20-24 years old. Data was analyzed using SPSS version 20. The multivariate regression analysis revealed higher likely of women in early marriage to have childbirth in the first year of marriage (OR=2.26, 95%CI=1.96-2.61); and number of children ever born (OR=4.24, 95% CI=3.40-5.27) but lower odd of repeated childbirth in less than twenty-four months (OR=0.66, 95%CI=0.52-0.83) and ever use of contraceptive (OR=0.52, 95%CI=0.45-0.61). However, the adjusted odd ratio only showed significant association between early marriage and number of children ever born (AOR=10.28, 95%CI=2.57-41.13). The nuanced analysis indicates that marriage at any age below 18 had higher effect on fertility than marriage at 18 and above. Early marriage predisposes married women to higher fertility and women with lower age of marriage have likelihood of higher fertility. Improving access of girls to education and contraceptives will delay the timing of pregnancy and childbirth.
Keywords: Child marriage, Childbirth, Contraceptive, Early marriage, Fertility, Nigeria.
Impacts of Early Marriage on Fertility Outcomes in Nigeria
References:
[1] World Bank (2022). Health Nutrition and Population Statistics: Population estimates and projections. Data Bank. https://databank.worldbank.org/Population/id/fdaa1724.
[2] World Population Review (2023). Total Fertility Rate 2023. https://worldpopulationreview.com/country-rankings/total-fertility-rate.
[3] Olaosebikan, J.S., Ogundana, C.F, Sunmola, K.A (2021). Contextual Determinants of Children ever born among women of Reproductive Age in selected Southwest State in Nigeria. European Journal of Sociology ISSN 2709-5886 (online) Vol.4, Issue 1, pp 15 – 24.
[4] World Health Organization (2019). Trends in maternal mortality 2000 to 2017: estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division. Geneva: Licence: CC BY-NC-SA 3.0 IGO.
[5] Anthony Mark Ochen, Primus Che Chi and Stephen Lawoko (2019). Predictors of teenage pregnancy among girls aged 13–19 years in Uganda: a community-based case-control study. BMC Pregnancy and Childbirth 19:211 https://doi.org/10.1186/s12884-019-2347-y.
[6] Finlay JE, Mejı´a-Guevara I, Akachi Y (2018) Inequality in total fertility rates and the proximate determinants of fertility in 21 subSaharan African countries. PLoS ONE 13(9): e0203344. https://doi.org/10.1371/journal. pone.0203344.
[7] UNICEF (2020). UNICEF Global Data Bases. Data.unicef.org. Accessed 25th August 2020
[8] Nasrullah, M., Muazzam, S., Bhutta, Z. A., & Raj, A. (2014). Girl child marriage and its effect on fertility in Pakistan: findings from Pakistan Demographic and Health Survey, 2006-2007. Maternal and child health journal, 18(3), 534–543. https://doi.org/10.1007/s10995-013-1269-y.
[9] Yaya, S., Odusina, E.K. & Bishwajit, G. (2019). Prevalence of child marriage and its impact on fertility outcomes in 34 sub-Saharan African countries. BMC Int Health Hum Rights 19, 33. https://doi.org/10.1186/s12914-019-0219-1.
[10] Uche C. Isiugo-Abanihe , Kola A. Oyediran, Olufunke A. Fayehun (2022). Differentials in girl-child marriage and high fertility in Nigeria. African Journal of Reproductive Health; 26 (9):103 DOI:10.29063/ajrh2022/v26i9.11.
[11] World Health Organization. (2007). Report of a WHO technical consultation on birth spacing: Geneva, Switzerland 13-15 June 2005. World Health Organisation. https://apps.who.int/iris/handle/10665/69855.
[12] Onukwugha, F.I., Magadi, M.A., Sarki, A.M. et al. (2020). Trends in and predictors of pregnancy termination among 15–24 -year-old women in Nigeria: a multi-level analysis of demographic and health surveys 2003–2018. BMC Pregnancy Childbirth 20, 550. https://doi.org/10.1186/s12884-020-03164-8.
[13] Sagalova V, Nanama S, Zagre NM, Vollmer S. (2021). Long-term consequences of early marriage and maternity in West and Central Africa: Wealth, education, and fertility. J Glob Health. 10;11:13004. doi: 10.7189/jogh.11.13004. PMID: 34484711; PMCID: PMC8397277.
[14] Bolarinwa OA, Ahinkorah BO, Seidu A-A, Mohammed A, Effiong FB, Hagan JE Jr, et al. (2023) Predictors of young maternal age at first birth among women of reproductive age in Nigeria. PLoS ONE 18(1): e0279404. https://doi.org/10.1371/journal.pone.0279404.
[15] Negash WD, Asmamaw DB (2022). Time to first birth and its predictors among reproductive age women in high fertility countries in Sub-Saharan Africa: Inverse Weibull gamma shared frailty model. BMC Pregnancy Childbirth. 16;22(1):844. doi: 10.1186/s12884-022-05206-9. PMID: 36384519; PMCID: PMC9670487.
[16] Melesse et al. (2021). Inequalities in early marriage, childbearing and sexual debut among adolescents in sub-Saharan Africa. Reprod Health, 18(Suppl 1):117 https://doi.org/10.1186/s12978-021-01125-8.
[17] Fagbamigbe, A.F., Idemudia, E.S. (2016). Survival analysis and prognostic factors of timing of first childbirth among women in Nigeria. BMC Pregnancy Childbirth 16, 102. https://doi.org/10.1186/s12884-016-0895-y.
[18] Winfred A. Avogo and Oluwaseyi D. Somefun (2019). Early Marriage, Cohabitation, and Childbearing in West Africa. Hindawi Journal of Environmental and Public Health Volume, Article ID 9731756, 10 pages https://doi.org/10.1155/2019/9731756.
[19] Olowolafe TA, Adebowale AS, Fagbamigbe AF, Bolarinwa OA, Akinyemi JO (2023) Shifts in age pattern, timing of childbearing and trend in fertility level across six regions of Nigeria: Nigeria Demographic and Health Surveys from 2003–2018. PLoS ONE 18(1): e0279365. https://doi.org/10.1371/journal.pone.0279365.
[20] Bola Lukman SOLANKE (2015). Marriage Age, Fertility Behavior, and Women’s Empowerment in Nigeria. SAGE Open: 1–9. DOI: 10.1177/2158244015617989 sgo.sagepub.com.
[21] Afeez O. Akintayo, Mutiu A. Sulaimon, Lateefat O. Akinwale (2021). Structural Equation Modeling of Factors Influencing Fertility among Married Women of Reproductive Age in Kaduna State, Nigeria. International Journal of Innovative Science and Research Technology. Volume 6, Issue 5. ISSN No: -2456-2165.
[22] Amusa, L., & Yahya, W. (2019). Stepwise Geoadditive Modelling of the Ideal Family Size in Nigeria. Türkiye Klinikleri Biyoistatistik, 11(2), 123-132.
[23] Nyarko, S. H. (2021). Socioeconomic determinants of cumulative fertility in Ghana. Plos one, 16(6), e0252519.
[24] Fouelifack, F.Y., Tameh, T.Y., Mbong, E.N. et al. (2014). Outcome of deliveries among adolescent girls at the Yaoundé central hospital. BMC Pregnancy Childbirth 14, 102. https://doi.org/10.1186/1471-2393-14-102.
[25] Fawole, A. O., Shah, A., Fabanwo, A. O., Adegbola, O., Adewunmi, A. A., Eniayewun, A. B., Dara, K., El-Ladan, A. M., Umezulike, A. C., Alu, F. E., Adebayo, A. A., Obaitan, F. O., Onala, O. E., Usman, Y., Sullayman, A. O., Kailani, S., & Sa'id, M. (2012). Predictors of maternal mortality in institutional deliveries in Nigeria. African health sciences, 12(1), 32–40.
[26] Onagoruwa, A., & Wodon, Q. (2018). Measuring the Impact of Child Marriage on Total Fertility: A Study for fifteen Countries. Journal of Biosocial Science, 50(5), 626-639. doi:10.1017/S0021932017000542.
[27] Wegbom, A. I., Bademosi, A., Edet, C. K., Green, K. I., Sapira-Ordu, L., & Fagbamigbe, A. F. (2022). Rural-urban disparities in birth interval among women of reproductive age in Nigeria. Scientific reports, 12(1), 17488. https://doi.org/10.1038/s41598-022-22142-y.
[28] Pimentel, J., Ansari, U., Omer, K. et al. (2020). Factors associated with short birth interval in low- and middle-income countries: a systematic review. BMC Pregnancy Childbirth 20, 156. https://doi.org/10.1186/s12884-020-2852-z.
[29] Desta Hailu, Teklemariam Gulte (2016). "Determinants of Short Interbirth Interval among Reproductive Age Mothers in Arba Minch District, Ethiopia", International Journal of Reproductive Medicine, vol. 2016, Article ID 6072437, 17 pages, https://doi.org/10.1155/2016/6072437
[30] Mihretie GN, Getie SA, Shiferaw S, Ayele AD, Liyeh TM, Kassa BG, et al. (2022). Interbirth interval practices among reproductive age women in rural and Urban kebeles in Farta Woreda: Casecontrol study. PLoS ONE 17(1): e0256193. https://doi.org/10.1371/journal.pone.0256193.
[31] Dim, C. C., Ugwu, E. O., & Iloghalu, E. I. (2013). Duration and determinants of inter-birth interval among women in Enugu, south-eastern Nigeria. Journal of obstetrics and gynaecology: the journal of the Institute of Obstetrics and Gynaecology, 33(2), 175–179. https://doi.org/10.3109/01443615.2012.747494.
[32] Ahinkorah, B.O., Aboagye, R.G., Okyere, J. et al. (2023). Correlates of repeat pregnancies among adolescent girls and young women in sub-Saharan Africa. BMC Pregnancy Childbirth 23, 93. https://doi.org/10.1186/s12884-023-05361-7.
[33] Nnaji, H. C., Asimadu, E. E., & Aniebue, U. U. (2022). The effect of short interpregnancy interval on birthweight and other pregnancy outcomes in Enugu, Southeast Nigeria. Journal of obstetrics and gynaecology: the journal of the Institute of Obstetrics and Gynaecology, 42(2), 244–247. https://doi.org/10.1080/01443615.2021.1904230.
[34] Onwuka, C. C., Ugwu, E. O., Obi, S. N., Onwuka, C. I., Dim, C. C., Eleje, G. U., Ezugwu, E. C., Agu, P. U., Nwagha, U. I., & Ozumba, B. C. (2020). Effects of short inter-pregnancy interval on maternal and perinatal outcomes: A cohort study of pregnant women in a low-income country. Nigerian journal of clinical practice, 23(7), 928–933. https://doi.org/10.4103/njcp.njcp_423_19.
[35] Islam, M. Z., Billah, A., Islam, M. M., Rahman, M., & Khan, N. (2022). Negative effects of short birth interval on child mortality in low- and middle-income countries: A systematic review and meta-analysis. Journal of global health, 12, 04070. https://doi.org/10.7189/jogh.12.04070.
[36] Ba DM, Zhang Y, Pasha-Razzak O, Khunsriraksakul C, Maiga M, Chinchilli VM, et al. (2023) Factors associated with pregnancy termination in women of childbearing age in 36 low-and middle-income countries. PLOS Glob Public Health 3(2): e0001509. https://doi.org/10.1371/journal.pgph.0001509.
[37] Ojo, I. E., Ojo, T. O., & Orji, E. O. (2021). Why do married women procure abortion? Experiences from Ile-Ife, southwestern Nigeria. African health sciences, 21(1), 327–337. https://doi.org/10.4314/ahs.v21i1.42.
[38] Bankole, A., Adewole, I. F., Hussain, R., Awolude, O., Singh, S., & Akinyemi, J. O. (2015). The Incidence of Abortion in Nigeria. International perspectives on sexual and reproductive health, 41(4), 170–181. https://doi.org/10.1363/4117015.
[39] Shallon Atuhaire (2019). Abortion among adolescents in Africa: A review of practices, consequences, and control strategies. The International Journal of Health Planning and Management. Volume34, Issue4. https://doi.org/10.1002/hpm.2842.
[40] National Population Commission (NPC) [Nigeria] and ICF (2019). Nigeria Demographic and Health Survey 2018. Abuja, Nigeria, and Rockville, Maryland, USA: NPC and ICF.
[41] Hutchinson, P.L., Anaba, U., Abegunde, D. et al. (2021). Understanding family planning outcomes in northwestern Nigeria: analysis and modeling of social and behavior change factors. BMC Public Health 21, 1168. https://doi.org/10.1186/s12889-021-11211-y
[42] Speizer, I.S., Lance, P. (2015). Fertility desires, family planning use and pregnancy experience: longitudinal examination of urban areas in three African countries. BMC Pregnancy Childbirth 15, 294. https://doi.org/10.1186/s12884-015-0729-3.
[43] Muhammad Murtala Ibrahim (2020). Sources of Contraceptive Information as Predictors of Contraceptive Use among Women in Tarauni Local Government Area of Kano State, Nigeria. Texila International Journal of Public Health ISSN: 2520-3134 DOI: 10.21522/TIJPH.2013.08.01.Art020.
[44] Irit Sinai, Jennifer Anyanti, Mohsin Khan, Ramatu Daroda and Olugbenga Oguntunde (2017). Demand for Women’s Health Services in Northern Nigeria: A Review of the Literature. Afr J Reprod Health 2017; 21[2]: 96-108).
[45] Idris, S. H., Sambo, M. N., & Ibrahim, M. S. (2013). Barriers to utilisation of maternal health services in a semi-urban community in northern Nigeria: The clients' perspective. Nigerian Medical Journal: Journal of the Nigeria Medical Association, 54(1), 27–32. https://doi.org/10.4103/0300-1652.108890.
[46] Muhammad Murtala Ibrahim (2019). An Assessment of Socioeconomic Determinants of Contraceptive use among Women of Reproductive Age in Tarauni Local Government Area of Kano State, Nigeria. Texila International Journal of Public Health, Volume 7, Issue 4, DOI: 10.21522/TIJPH.2013.07.04.Art029 ISSN: 2520-3134.
[47] D. J. P. K Hedo, and N. Simarmata (2022) "What Predict Modern Contraception Use? A Study of Reproductive Age Married Couples in Indonesia," Journal Promosi Kesehatan Indonesia, vol. 18, no. 1, pp. 1-7. https://doi.org/10.14710/jpki.18.1.1-7.
[48] Audu Alayande, Bahijjatu Bello-Garko, Zubaida Abubakar, Hafsat Kagara1 and Islamiyat A. Nuhu (2019) Medical Perspective of Childhood Marriage in Nigeria: Body of Evidence from 2013 Nigeria Demographic and Health Survey. Current Women’s Health Reviews, 15, 188-195. DOI: 10.2174/1573404814666181026095357.
[49]Sebany, M., Barre, I., and John, N. (2018). The Power of Choice: How early & delayed marriage impact decisionmaking in Ibadan, Nigeria. Washington, DC: International Center for Research on Women.
[50] Ganchimeg T, Ota E, Morisaki N, Laopaiboon M, Lumbiganon P, Zhang J, Yamdamsuren B, Temmerman M, Say L, Tuncalp O, € Vogel JP, Souza JP, Mori R, on behalf of the WHO (2014). Multicountry Survey on Maternal Newborn Health Research Network. Pregnancy and childbirth outcomes among adolescent mothers: a World Health Organization multicountry study. BJOG 121 (Suppl. 1): 40–48.
[51] Fan, S., Koski, A. (2022). The health consequences of child marriage: a systematic review of the evidence. BMC Public Health 22, 309. https://doi.org/10.1186/s12889-022-12707-x.
[52] Nour N. M. (2006). Health consequences of child marriage in Africa. Emerging infectious diseases, 12(11), 1644–1649. https://doi.org/10.3201/eid1211.060510.
[53] Belachew, T.B., Asmamaw, D.B. & Negash, W.D. (2023). Short birth interval and its predictors among reproductive age women in high fertility countries in sub-Saharan Africa: a multilevel
analysis of recent Demographic and Health Surveys. BMC Pregnancy Childbirth 23, 81. https://doi.org/10.1186/s12884-023-05403-0.[54] Muhammad Murtala Ibrahim and Tinuola Femi Rufus (2023). The Effects of Early Marriage on the Utilization of Maternal Health Services in Nigeria. Texila International Journal of Nursing ISSN: 2520-3126 DOI: 10.21522/TIJNR.2015.09.01.Art002.
[55] M. A. Mowafy, N. M. Kamal Elden (2020). Assessment of Contraception Use among Early Married Females in Rural Districts in Giza Governorate, Egypt. Egyptian Family Medicine Journal (EFMJ) Vol .4(1), www.efmj-eg.org.
[56] Bolarinwa, O.; Olagunju, O.; Olaniyan, A. (2020). Influence of Husband Consent to Family Planning and Spousal Communication on the Use of Family Planning among Young Mothers in Peri-Urban, Nigeria. Preprints 2020, 2020090148. https://doi.org/10.20944/preprints202009.0148.v1.
[57] Srivastava, S., Mohanty, P., Muhammad, T. et al. (2023). Socio-economic inequalities in non-use of modern contraceptives among young and non-young married women in India. BMC Public Health 23, 797. https://doi.org/10.1186/s12889-023-15669-w.
Viewed PDF 830 31 -
Adverse Childhood Experiences and Self-Reported Sexually Transmitted Infections among Adolescents and Young Adults in ZimbabweAuthor: Edson ChipaloDOI: 10.21522/TIJPH.2013.11.04.Art015
Adverse Childhood Experiences and Self-Reported Sexually Transmitted Infections among Adolescents and Young Adults in Zimbabwe
Abstract:
Sexually transmitted infections (STIs) are a public health crisis that can be devastating to individuals with adverse childhood experiences (ACEs). This study examined the prevalence and association between ACEs and self-reported STIs among adolescents and young adults in Zimbabwe. Data for this study was derived from the 2017 Zimbabwe Violence Against Children Survey (ZVACS) from the participants aged 13 to 24 (n=504). The self-reported prevalence estimates of STIs were calculated using weighted frequencies and percentages. Two logistic regression models were employed to assess an association between eight ACE types and self-reported STIs. The findings revealed that STIs were higher among orphans (52.2%), followed by participants with a history of lifetime suicide ideation or attempts (49.8%), were exposed to any ACE (42.5%), and had moderate/severe mental distress in the past 30 days (44.8%). Additionally, self-reported STI rates were higher for participants who experienced any form of physical violence (30.8%), witnessed physical violence (22.4%), experienced sexual violence (16.1%) and emotional violence (11.7%). In unadjusted regression models, all ACEs, except participants who experienced emotional violence, were significantly associated with self-reported STIs. However, after adjusting for covariates in the model, none of the ACEs maintained a significant association with self-reported STIs. Despite this, it is evident that interventions remain crucial for effectively preventing STIs for individuals with ACEs. There is a pressing need to implement and expand STI prevention programs nationally, including identifying and addressing ACEs and early screening, diagnosis, and treatment of STIs among adolescents and young adults in Zimbabwe.
Keywords: Adverse childhood experiences (ACEs), Adolescents, sexually transmitted infections (STIs), Violence, Young adults, Zimbabwe.
Adverse Childhood Experiences and Self-Reported Sexually Transmitted Infections among Adolescents and Young Adults in Zimbabwe
References:
[1] World Health Organization [WHO], Sexually transmitted infections: fact sheet: more than 1 million people acquire a sexually transmitted infection every day. 2014, World Health Organization.
[2] WHO, Global health sector strategy on sexually transmitted infections 2016-2021: toward ending STIs. 2016, World Health Organization.
[3] Nubed, C.K. and J.-F.T.K. Akoachere, Knowledge, attitudes, and practices regarding HIV/AIDS among senior secondary school students in Fako Division, Southwest Region, Cameroon. BMC public health, 2016. 16(1): p. 1-10.
[4] Somba, M.J., et al., Sexual behaviour, contraceptive knowledge and use among female undergraduates’ students of Muhimbili and Dar es Salaam Universities, Tanzania: a cross-sectional study. BMC women’s health, 2014. 14(1): p. 1-8.
[5] World Health Organization [WHO]. Sexually Transmitted Infections (STIs) 2015 [cited 2023 July 2023]; Available from: http://www.who.int/mediacentre/factsheets/fs110/en/.
[6] World Health Organization [WHO], More than 1 million new curable sexually transmitted infections every day. World Health Organization: Geneva, Switzerland, 2019.
[7] Gerbase, A. and T. Mertens, sexually transmitted diseases in Africa: time for action. Africa health, 1998. 20(3): p. 10-12.
[8] Ngidi, N.D., et al., Qualitative evaluation of selected social factors that impact sexual risk-taking behaviour among African students in Kwazulu-Natal, South Africa. Sahara-J: Journal of Social Aspects of HIV/AIDS, 2016. 13(1): p. 96-105.
[9] Talwar, P. and M.F.B. Abd Rahman, Assessment of HIV knowledge among university students using the HIV-KQ-18 scale: A cross-sectional study. Southeast Asia Journal of Public Health, 2015. 5(1): p. 33-38.
[10] Hillis, S.D., et al., Adverse childhood experiences and sexually transmitted diseases in men and women: a retrospective study. Pediatrics, 2000. 106(1): p. e11-e11.
[11] Chang, X., et al., Associations between adverse childhood experiences and health outcomes in adults aged 18–59 years. PloS one, 2019. 14(2): p. e0211850.
[12] Campbell, J.A., R.J. Walker, and L.E. Egede, Associations between adverse childhood experiences, high-risk behaviors, and morbidity in adulthood. American Journal of Preventive Medicine, 2016. 50(3): p. 344-352.
[13] Bryant, D.J., M. Oo, and A.J. Damian, The rise of adverse childhood experiences during the COVID-19 pandemic. Psychological Trauma: Theory, Research, Practice, and Policy, 2020. 12(S1): p. S193.
[14] Lee, N., et al., Adverse childhood experiences and associated mental distress and suicide risk: results from the Zambia Violence Against Children Survey. Journal of interpersonal violence, 2022. 37(21-22): p. NP21244-NP21265.
[15] Karatekin, C., Adverse childhood experiences (ACEs), stress and mental health in college students. Stress and Health, 2018. 34(1): p. 36-45.
[16] Chigiji, H., et al., Risk factors and health consequences of physical and emotional violence against children in Zimbabwe: a nationally representative survey. BMJ global health, 2018. 3(3): p. e000533.
[17] Thomas, J.L., et al., Associations between adverse childhood experiences and sexual risk among postpartum women. International Journal of environmental research and public health, 2021. 18(7): p. 3848.
[18] London, S., et al., Adverse experiences in childhood and sexually transmitted infection risk from adolescence into adulthood. Sexually transmitted diseases, 2017. 44(9): p. 524.
[19] Wilson, H.W., G.R. Donenberg, and E. Emerson, Childhood violence exposure and the development of sexual risk in low-income African American girls. Journal of Behavioral Medicine, 2014. 37: p. 1091-1101.
[20] Voisin, D.R., A. Hotton, and T. Neilands, Exposure to community violence and sexual behaviors among African American youth: Testing multiple pathways. Behavioral medicine, 2018. 44(1): p. 19-27.
[21] Berenson, A.B., C.M. Wiemann, and S. McCombs, Exposure to violence and associated health-risk behaviors among adolescent girls. Archives of Pediatrics & Adolescent Medicine, 2001. 155(11): p. 1238-1242.
[22] Wilson, H.W., et al., Patterns of violence exposure and sexual risk in low-income, urban African American girls. Psychology of violence, 2012. 2(2): p. 194.
[23] Brown, M.J., et al., Sex disparities in adverse childhood experiences and HIV/STIs: Mediation of psychopathology and sexual behaviors. AIDS and Behavior, 2017. 21: p. 1550-1566.
[24] Small, E., Y.K. Kim, and M. Yu, sexually transmitted diseases among college students in Sierra Leone: A life course ecological analysis. Sexuality & culture, 2021. 25: p. 884-903.
[25] Odgers, C.L., S.J. Robins, and M.A. Russell, Morbidity, and mortality risk among the “forgotten few”: why are girls in the justice system in such poor health? Law and Human Behavior, 2010. 34: p. 429-444.
[26] Wilson, H.W. and C.S. Widom, sexually transmitted diseases among adults who had been abused and neglected as children: A 30-year prospective study. American Journal of Public Health, 2009. 99(S1): p. S197-S203.
[27] Fergusson, D.M., L.J. Horwood, and M.T. Lynskey, Childhood sexual abuse, adolescent sexual behaviors and sexual revictimization. Child abuse & neglect, 1997. 21(8): p. 789-803.
[28] Wingood, G.M. and R.J. DiClemente, Child sexual abuse, HIV sexual risk, and gender relations of African American women. American journal of preventive medicine, 1997. 13(5): p. 380-384.
[29] Kelly, P. and J. Koh, sexually transmitted infections in alleged sexual abuse of children and adolescents. Journal of paediatrics and child health, 2006. 42(7‐8): p. 434-440.
[30] Schwarcz, S.K. and W.L. Whittington, Sexual assault, and sexually transmitted diseases: detection and management in adults and children. Reviews of infectious diseases, 1990. 12(Supplement_6): p. S682-S690.
[31] Bretz, L.A., N. Keshwani, and M. Raphael, Relationship between mental health diagnoses and sexually transmitted infections. Bulletin of the Menninger Clinic, 2023. 87(2): p. 115-134.
[32] Coverdale, J.H. and S.H. Turbott, Risk behaviors for sexually transmitted infections among men with mental disorders. Psychiatric Services, 2000. 51(2): p. 234-238.
[33] Bender, S. and K. Hill, sexually transmitted infections–diagnoses, stigma, and mental health, in Research anthology on mental health stigma, education, and treatment. 2021, IGI Global. p. 103-120.
[34] Kenedi, C., et al., Evaluating the risk of sexually transmitted infections in mentally ill patients. Current Psychiatry, 2017. 16(1): p. 22-36.
[35] Thompson, M.P., J. Kingree, and D. Lamis, Associations of adverse childhood experiences and suicidal behaviors in adulthood in a US nationally representative sample. Child: care, health, and development, 2019. 45(1): p. 121-128.
[36] Control, C.f.D. and Prevention [CDC], Definitions: Self-directed violence. Injury prevention and control: Division of violence, 2015.
[37] Han, B., et al., Estimating the rates of deaths by suicide among adults who attempt suicide in the United States. Journal of Psychiatric Research, 2016. 77: p. 125-133.
[38] Ginieri-Coccossis, M., et al., Quality of life and depression in chronic sexually transmitted infections in UK and Greece: The use of WHOQOL-HIV/STI BREF. Psychiatrike= Psychiatriki, 2018. 29(3): p. 209-219.
[39] Mustanski, B., et al., A syndemic of psychosocial health disparities and associations with risk for attempting suicide among young sexual minority men. American Journal of Public Health, 2014. 104(2): p. 287-294.
[40] Wang, S., et al., Psychosocial Syndemic of suicidal ideation: a cross-sectional study among sexually transmitted infection patients in Shanghai, China. BMC Public Health, 2020. 20: p. 1-11.
[41] Getachew, H., et al., psychological distress and its predictors in AIDS orphan adolescents in Addis Ababa city: A comparative survey. Ethiopian Journal of Health Development, 2011. 25(2): p. 135-142.
[42] Birdthistle, I.J., et al., From affected to infected? Orphanhood and HIV risk among female adolescents in urban Zimbabwe. Aids, 2008. 22(6): p. 759-766.
[43] Operario, D., et al., Orphanhood and completion of compulsory school education among young people in South Africa: Findings from a national representative survey. Journal of Research on Adolescence, 2008. 18(1): p. 173-186.
[44] Kidman, R. and P. Anglewicz, why are orphaned adolescents more likely to be HIV positive? Distinguishing between maternal and sexual HIV transmission using 17 nationally representative data sets in Africa. Journal of Adolescent Health, 2017. 61(1): p. 99-106.
[45] VanderEnde, K., et al., Adverse childhood experiences and HIV sexual risk-taking behaviors among young adults in Malawi. Journal of interpersonal violence, 2018. 33(11): p. 1710-1730.
[46] Kappel, R.H., et al., Prevalence of adverse childhood experiences (ACEs) and associated health risks and risk behaviors among young women and men in Honduras. Child abuse & neglect, 2021. 115: p. 104993.
[47] Dunne, M.P., et al., ISPCAN Child Abuse Screening Tools Retrospective version (ICAST-R): Delphi study and field testing in seven countries. Child abuse & neglect, 2009. 33(11): p. 815-825.
[48] Finkelhor, D., et al., The Juvenile Victimization Questionnaire: reliability, validity, and national norms. Child abuse & neglect, 2005. 29(4): p. 383-412.
[49] Finkelhor, D., Child sexual abuse: Challenges facing child protection and mental health professionals, in Childhood and Trauma. 2019, Routledge. p. 101-116.
[50] Juan, C., et al., Associations between mental distress, poly-victimisation, and gender attitudes among adolescent girls in Cambodia and Haiti: an analysis of Violence Against Children surveys. Journal of Child & Adolescent Mental Health, 2019. 31(3): p. 201-213.
[51] Prochaska, J.J., et al., Validity study of the K6 scale as a measure of moderate mental distress based on mental health treatment need and utilization. International journal of methods in psychiatric research, 2012. 21(2): p. 88-97.
[52] Nguyen, K.H., et al., Coerced and forced sexual initiation and its association with negative health outcomes among youth: results from the Nigeria, Uganda, and Zambia violence against children surveys. Child abuse & neglect, 2019. 96: p. 104074.
[53] Aarons, G.A., M. Hurlburt, and S.M. Horwitz, Advancing a conceptual model of evidence-based practice implementation in public service sectors. Administration and Policy in Mental Health and Mental Health Services Research, 2011. 38(1): p. 4-23.
[54] Zimbabwe Ministry of Health and Childcare, oung Adult Survey of Zimbabwe: A Violence Against Children Survey, 2017. 2019.
[55] Kaida, A., et al., A high burden of asymptomatic genital tract infections undermines the syndromic management approach among adolescents and young adults in South Africa: implications for HIV prevention efforts. BMC infectious diseases, 2018. 18(1): p. 1-11.
[56] Ayerdi Aguirrebengoa, O., et al., Risk factors associated with sexually transmitted infections and HIV among adolescents in a reference clinic in Madrid. PloS one, 2020. 15(3): p. e0228998.
[57] Mokgatle, M.M., S. Madiba, and L. Cele, A comparative analysis of risky sexual behaviors, self-reported sexually transmitted infections, knowledge of symptoms and partner notification practices among male and female university students in Pretoria, South Africa. International journal of environmental research and public health, 2021. 18(11): p. 5660.
[58] Shisana, O., et al., South African national HIV prevalence, incidence, and behaviour survey, 2012. 2014.
[59] Territo, H., Chlamydia screening post COVID-19. Contemporary OB/GYN, 2021. 66(7): p. 1-4.
[60] Oharume, I.M., Knowledge, sexual behaviours and risk perception of sexually transmitted infections among students of the polytechnic, Ibadan, Oyo state. African Health Sciences, 2020. 20(1): p. 39-44.
[61] Sychareun, V., et al., Risk perceptions of STIs/HIV and sexual risk behaviours among sexually experienced adolescents in the Northern part of Lao PDR. BMC public health, 2013. 13(1): p. 1-13.
[62] Osingada, C.P., et al., Perceived risk of HIV infection and associated factors among secondary school students in Wakiso district, Uganda. Advances in Public Health, 2016. 2016.
[63] Quinn, T.C. and J. Overbaugh, HIV/AIDS in women: an expanding epidemic. Science, 2005. 308(5728): p. 1582-1583.
[64] Wood, S.K., et al., Adverse childhood experiences and their relationship with poor sexual health outcomes: results from four cross-sectional surveys. International Journal of Environmental Research and Public Health, 2022. 19(14): p. 8869.
Viewed PDF 676 25 -
 Prevalence of Social Media Use for Dental Information Among Dental ProfessionalsAuthor: Sachin NaikDOI: 10.21522/TIJPH.2013.11.04.Art016
Prevalence of Social Media Use for Dental Information Among Dental ProfessionalsAuthor: Sachin NaikDOI: 10.21522/TIJPH.2013.11.04.Art016Prevalence of Social Media Use for Dental Information Among Dental Professionals
Abstract:
Social media is a powerful tool most used among dental professionals. The present study assessed the prevalence of SM usage for dental information among dental professionals. A descriptive cross-sectional study was conducted among dental professionals Riyadh, Saudi Arabia. The questionnaire consisted of demographic data of study participants and questions to assess the prevalence and type of SM use. Study results showed Twitter (24%), Instagram (19%), and YouTube (18%) are the three most popular SM platforms utilized by dental professionals, respectively. Prevalence of SM use among dental professionals for dental information.
Keywords: Dentists, Dental professionals, Descriptive study, Social media, Twitter, YouTube.Prevalence of Social Media Use for Dental Information Among Dental Professionals
References:
[1] Patil P, Pawar AM, Wahjuningrum DA, Luke AM, Reda R, Testarelli L. Connectivity, and Integration of Instagram® Use in the Lives of Dental Students and Professionals: A Country-Wide Cross-Sectional Study Using the InstaAA© Questionnaire. J Multidiscip Healthc 2023; Volume 16:2963–76. https://doi.org/10.2147/JMDH.S430973.
[2] Alanzi T, Al-Yami S. Physicians’ attitude towards the use of social media for professional purposes in Saudi Arabia. Int J Telemed Appl 2019;2019. https://doi.org/10.1155/2019/6323962.
[3] Lee Ventola C. social media and Health Care Professionals: Benefits, Risks, and Best Practices. Pharm Ther 2014; 39:491.
[4] Makkar N, Lawrence D, Veeresh D, Banik A, Kumar A, Mehar AS. Assessment of social media usage and its influence among dental faculty members in Davangere city – A cross sectional survey. J Indian Assoc Public Heal Dent 2021; 16:246. https://doi.org/10.4103/JIAPHD.JIAPHD_143_17.
[5] Moorhead SA, Hazlett DE, Harrison L, Carroll JK, Irwin A, Hoving C. a New Dimension of Health Care: Systematic Review of the Uses, Benefits, and Limitations of social media for Health Communication. J Med Internet Res 2013;15(4)E85 https://WwwJmirOrg/2013/4/E852013;15:e1933. https://doi.org/10.2196/JMIR.1933.
[6] Henry RK, Molnar A, Henry JC. A survey of US dental practices’ use of social media. J Contemp Dent Pract 2012; 13:137–41. https://doi.org/10.5005/JP-Journals-10024-1109.
[7] Bahabri RH, Zaidan AB. The impact of social media on dental practice promotion and professionalism amongst general dental practitioners and specialists in KSA. J Taibah Univ Med Sci 2021; 16:456–60. https://doi.org/10.1016/J.JTUMED.2020.12.017.
[8] Snyman L, Visser JH. The adoption of social media and social media marketing by dentists in South Africa. SADJ 2014; 69:262–4.
[9] Al-Khalifa KS, Al-Swuailem AS, AlSheikh R, Muazen YY, Al-Khunein YA, Halawany H, et al. The use of social media for professional purposes among dentists in Saudi Arabia. BMC Oral Health 2021; 21:1–8. https://doi.org/10.1186/s12903-021-01390-w.
[10] Ustdal G, Guney AU. YouTube as a source of information about orthodontic clear aligners. Angle Orthod 2020; 90:419–24. https://doi.org/10.2319/072419-491.1.
[11] Affendi NHK, Hamid NFA, Razak MSA, Nudin III. The Pattern of Social Media Marketing by Dentist in Malaysia. Malays Dent J 2020; 1:24–42.
[12] Simplício AH de M. social media and Dentistry: ethical and legal aspects. Dental Press J Orthod 2019; 24:80. https://doi.org/10.1590/2177-6709.24.6.080-089.SAR.
[13] Ajwa N, Mohsen S Al, Kuwail A, Osaif E Al. The Impact of Using Social Media Networks on Dental Treatment Marketing in Saudi Arabia: The Practitioners and Patient ‘s Perspectives Th e Impact of Using Social Media Networks on Dental Treatment Marketing in Saudi Arabia: Th e Practitioners and Pati. J Oral Heal Dent Sci 2018; 2:1–10.
[14] AlBaker AA, Al-Ruthia YSH, AlShehri M, Alshuwairikh S. The characteristics and distribution of dentist workforce in Saudi Arabia: A descriptive cross-sectional study. Saudi Pharm J 2017; 25:1208–16. https://doi.org/10.1016/j.jsps.2017.09.005.
[15] Henry R, Molnar A, Henry J. A survey of US dental practices’ use of social media. J Contemp Dent Pract 2012; 13:137–41. https://doi.org/10.5005/JP-JOURNALS-10024-1109.
[16] Hamasha AA-H, Alghofaili N, Obaid A, Alhamdan M, Alotaibi A, Aleissa M, et al. Social Media Utilization among Dental Practitioner in Riyadh, Saudi Arabia. Open Dent J 2019; 13:101–6. https://doi.org/10.2174/1874210601913010101.
[17] Din H, McDaniels-Davidson C, Nodora J, Madanat H. Profiles of a Health Information-Seeking Population, and the Current Digital Divide: Cross-Sectional Analysis of the 2015-2016 California Health Interview Survey. J Med Internet Res 2019;21: e11931. https://doi.org/10.2196/11931.
[18] Number of social media users 2025 | Statista n.d. https://www.statista.com/statistics/278414/number-of-worldwide-social-network-users/ (accessed November 10, 2021).
[19] Al-Khalifa KS, Al-Swuailem AS, AlSheikh R, Muazen YY, Al-Khunein YA, Halawany H, et al. The use of social media for professional purposes among dentists in Saudi Arabia. BMC Oral Health 2021; 21:1–8. https://doi.org/10.1186/S12903-021-01390-W/TABLES/3.
[20] Cain J, Policastri A. Using Facebook as an Informal Learning Environment. Am J Pharm Educ 2011; 75:1–8. https://doi.org/10.5688/AJPE7510207.
[21] Sevil JSA, Navarro JL, Bernal-Agustín JL. Youtube & Facebook as educational tools in the teaching-learning process. experience in higher education. ICERI2014 Proc 2014:940–9.
[22] Aboalshamat K, Alkiyadi S, Alsaleh S, Reda R, Alkhaldi S, Badeeb A, et al. Attitudes toward social media among Practicing Dentists and Dental Students in Clinical Years in Saudi Arabia. Open Dent J 2019; 13:143–9. https://doi.org/10.2174/1874210601913010143.
[23] Makkar, Lawrence D, Veeresh D, Banik A, Kumar A, Mehar AS. Assessment of social media usage and its influence among dental faculty members in Davangere city – A cross sectional survey. J Indian Assoc Public Heal Dent 2021; 16:246. https://doi.org/10.4103/JIAPHD.JIAPHD_143_17.
[24] Javed MW, Bhatti R. Usage of social media by Medical and Dental Students at Nishtar Medical College, Multan, Pakistan. J Hosp Librariansh 2015; 15:53–64. https://doi.org/10.1080/15323269.2015.982031.
[25] Burns LE, Abbassi E, Qian X, Mecham A, Simeteys P, Mays KA. YouTube used among dental students for learning clinical procedures: A multi-institutional study. J Dent Educ 2020; 84:1151–8. https://doi.org/10.1002/JDD.12240.
[26] Fox S, Duggan M. Health Online 2013. vol. 15. 2013.
[27] Almozainy M. Assessing the Use of social media as a Source of Information Related to Dentistry in Saudi Arabia. J Dent Heal Oral Disord Ther 2017;8. https://doi.org/10.15406/jdhodt.2017.08.00312.
Viewed PDF 592 14 -
HIV/AIDS Education among Young Adolescent for Better Quality of Life: Health Belief ModelAuthor: Farhana Kamarul BahrinDOI: 10.21522/TIJPH.2013.11.04.Art017
HIV/AIDS Education among Young Adolescent for Better Quality of Life: Health Belief Model
Abstract:
HIV remains a significant global public health challenge, having caused the loss of 40.1 million lives to date, with ongoing transmission in all countries worldwide (World Health Organization, 2023). By the end of 2021, there were approximately 38.4 million people living with HIV/AIDS (World Health Organization, 2023). HIV/AIDS education targeted at young individuals plays a crucial role in ending the AIDS epidemic on a global scale. In Malaysia, by the end of 2021, an estimated 81,942 people were living with HIV (PLHIV) (Ministry of Health, 2022). 600 Penang students between the ages of 15 and 17 participated in the study, which had three sessions total—a pre-test, an intervention, and a post-test. The findings were analyzed using SPSS 22.0 software. The results revealed a positive change in the respondents' knowledge following the implementation of the intervention process. This study demonstrates that early health education can effectively reduce the risk behaviors associated with HIV/AIDS among young adolescents. The aim is to ensure that they lead a better quality of life and maintain their overall well-being.
Keywords: Health Belief Model, HIV/AIDS Education, Public Health Education, Quality of life, Social Work in School.
HIV/AIDS Education among Young Adolescent for Better Quality of Life: Health Belief Model
References:
[1] Boler T., Ibrahim A., Adoss R., & Shaw M. (2013) The sound of silence. Difficulties in communicating on HIV / AIDS in schools. Experiences from India and Kenya. London, England, ActionAid, 2013. 53 p.
[2] Ministry of Health Malaysia (2022). 2022 Global AIDS Monitoring Report 2022.
[3] UNAIDS (2019), 2019 Progress report on the Global Plan.
[4] Ma, Z.Q., Fisher, M.A., & Kuller, L.H. (2014). School-based HIV/AIDS education is associated with reduced risky sexual behaviors and better grades with gender and race/ethnicity differences. Health Educ Res. 2014 Apr;29(2):330- 9.doi: 10.1093/her/cyt110.
[5] Rahim V., Mohammad R., Mansoure A., Masumeh S. & Maryam A. (2015). The Effects of Speech Training, Guidebook and Simultaneous Method, on the Knowledge and Attitude of Students about HIV/AIDS. International Jounal Pediatrics, Vol.3, N.3-1, Serial No.17, May 2015.
[6] Vijayageetha M., Narayanamurthy M.R., Vidya G.S., & Renuka M. (2016). Knowledge and attitude on HIV/AIDS among adolescent school children in urban Mysuru, Karnataka, India: a cross sectional study, International Jounal Community Med Public Health. 2016 May;3(5):1224-1228.
[7] Siegel, D., DiClemente, R., Durbin, M., Krasnovsky, F., & Saliba, P. (1995). Change in junior high school students' AIDS-related knowledge, misconceptions, attitudes, and HIV-preventive behaviors: effects of a school-based intervention. AIDS Educ Prev. 1995 Dec;7(6):534-43.
[8] Eaton, L. & Flisher, A.J. (2000). HIV/AIDS knowledge among South African youth. Southern African. Journal Child and Adolescent Mental Health, 12: 97-124.
[9] Muhammad, A., & Nasruddin, S. (2016). Different levels of HIV/AIDS knowledge and stigma of GMI and UKM students based on levels of education. Jurnal Psikologi Malaysia 30 (1) (2016): 61-68 ISSN-2289-8174.
[10] Harding, A.K., Anadu, E.C., Gray, L.A., & Champeau, D.A. (1999). Nigerian university students' knowledge, perceptions, and behaviours about HIV/AIDS: are these students at risk? The Journal of the Royal Societies to Promote Health. 1999 Mar;119(1):23-31.
[11] Kennedy, O. & Mary, O. (2015). HIV/AIDS Education programs in Kenya: Contexts of implementation in secondary schools in Kisii County in the impact of HIV/AIDS on education worldwide. Retrieved from: https://www.emeraldinsight.com/doi/abs/10.1108/S14793679%282012%290000018005.
[12] Valerio, A., & Bundy, D. (2002). Education and HIV/AIDS: A sourcebook of HIV/AIDS Prevention Programs. Washington, DC: World Bank.
[13] Rosli, N. F., Rabe, N. S., & Mohamed Osman, M. (2018). Perception Of Quality of Life Among Community in Selangor, Planning Malaysia: Journal of the Malaysian Institute of Planners. Vol 16 Issues 2 (2018), Page 12 – 20.
[14] Hassan, N., Mohd Jaafar, N. I., Raja Ariffin, R. N., Abu Samah, A., & Jaafar, M. N. (2013). Perceptions On Quality of Life in Malaysia: The Urban rural Divide. Planning Malaysia: Journal of the Malaysian Institute of Planners. Vol XI (2013) Page 21– 40.
[15] Glanz, K., Rimer, B.K. & Lewis, F.M. (2002). Health Behavior and Health Education. Theory, Research and Practice. (3rd ed). San Francisco: Jossey-Bass.
[16] Griffin, M.J. (2012). Health belief model, social support, and intention to screen for colorectal cancer in older African American men. Health Promotion & Education. 2012;51(1):12– 22.
[17] Ministry of Health Malaysia (2010). Garis panduan pemasaran sosial promosi kesihatan. Kementerian Kesihatan Malaysia 2010 dalam Program Promosi Kesihatan.
[18] Khadijeh S. & Sadigheh S.T., (2016). Using the health belief model regarding HIV/ AIDS prevention among female high school students, J Research & Health 2016;6(1):161-166.
[19] Oladepo, O., & Fayemi, M.M. (2011). Perceptions about sexual abstinence and knowledge of HIV/AIDS prevention among in school adolescents in a Western Nigerian city. BMC Public Health 2011. https://doi.org/10.1186/1471-2458-11-304.
[20] Kelly, M. & Stone, S. (2009). An analysis of factors shaping interventions used by school social workers. Children & Schools 31(3): 163-176.
[21] Skidmore, R.A. (1997). Introduction to Social Work (7th eds.). Allyn and Bacon.
[22] World Health Organization. (2012). Sexual and reproductive health of adolescents and youths in Malaysia: a review of literature and projects 2012.
[23] Amna, M.N, Rozumah, B., Abdullah, A.M., & Tan, J. P. (2003). Sistem sekolah dan sosialisasi pelajar. Serdang: Penerbit Universiti Putra
[24] Azizan, B. (2010). Permasalahan Sosial Pelajar: Keperluan Kepada Kerja Sosial Sekolah.
Viewed PDF 662 26 -
Evaluation of a Community-based Intervention to Improve Maternal New-born and Child Health Coverage in the Rural and Hard-to-reach Communities of Adamawa State NigeriaAuthor: Mohammed Bello HammanDOI: 10.21522/TIJPH.2013.11.04.Art018
Evaluation of a Community-based Intervention to Improve Maternal New-born and Child Health Coverage in the Rural and Hard-to-reach Communities of Adamawa State Nigeria
Abstract:
The healthcare inequities in hard-to-reach (HTR) areas of developing countries, such as Nigeria, have significant implications for disease prevention and control, particularly in maternal and child health. The aim of this study is to look at how well mobile outreach and health facility outreach programs work to improve health outcomes in rural, underserved, and hard-to-reach (HTR) areas in Adamawa State, Nigeria. The focus is on key indicators of maternal, newborn, and child health. The key interventions include antenatal care (ANC), family planning, routine immunization, vitamin A supplementation, deworming of children under 5 years, and Diarrhea treatment. The study applied a cross-sectional design using before-and-after assessments to assess the outcome of the mobile outreach interventions using quantitative health facility-level data from the District Health Information System (DHIS 2.0) on the intervention. Following a successful intervention, the coverage of these indicators prior to and following the intervention was compared using the data. The study shows a cumulative improvement in ANC (21%), institutional delivery (18%), and Penta 3 coverage (28%). Mobile and hard-to-reach strategies utilizing community health workers and volunteers from the LGA, and health facilities can be effective in improving coverage of MNCH services and hold promise for better maternal and child survival in rural, HTR, and under-resourced parts of Adamawa State, Nigeria, and Sub-Saharan Africa at large. In addition, the mobile outreach interventions have contributed to improving MNCH services in hard-to-reach communities, so scaling up the strategy is highly recommended.
Keywords: Hard-to-reach, Interventions, Outreach, Communities, Adamawa State, Nigeria.Evaluation of a Community-based Intervention to Improve Maternal New-born and Child Health Coverage in the Rural and Hard-to-reach Communities of Adamawa State Nigeria
References:
[1] Haruna, U., Dandeebo, G., & Galaa, S. Z. (2019). Improving access and utilization of maternal healthcare services through focused antenatal care in rural Ghana: a qualitative study. Advances in Public Health, 2019.
[2] Esamai, F., Nangami, M., Tabu, J., Mwangi, A., Ayuku, D., & Were, E. (2017). A system approach to improving maternal and child health care delivery in Kenya: innovations at the community and primary care facilities (a protocol). Reproductive health, 14, 1-18.
[3] Hanif, M., Khalid, S., Rasul, A. & Mahmood, K. (2021). Maternal mortality in rural areas of Pakistan: challenges and prospects. Rural Heal, 27, 1040-1047.
[4] Blackwell, S., Louis, J. M., Norton, M. E., Lappen, J. R., Pettker, C. M., Kaimal, A., ... & Landis, R. (2020). Reproductive services for women at high risk for maternal mortality: a report of the workshop of the Society for Maternal-Fetal Medicine, the American College of Obstetricians and Gynecologists, the Fellowship in Family Planning, and the Society of Family Planning. American Journal of Obstetrics & Gynecology, 222(4), B2-B18.
[5] McIntyre, D., Thiede, M., & Birch, S. (2009). Access as a policy-relevant concept in low- and middle-income countries. Health economics, policy, and law, 4(Pt 2), 179–193. https://doi.org/10.1017/S1744133109004836
[6] Oluwadare, C. (2009). The social determinants of routine immunisation in Ekiti State of Nigeria. Studies on Ethno-Medicine, 3(1), 49-56.
[7] DHS Program retrieved from: https://www.dhsprogram.com/pubs/pdfAssessed August 2023.
[8] Tsegaye, Z. T., Sinamo, T., Desta, B. F., Beshir, I. A.& Abawollo, H. S. (2022). Integrated Periodic Outreach Strategy to Improve Maternal and Child health Service Access Among Hard-to-Reach Areas in Ethiopia.
[9] Garchitorena, A., Miller, A. C., Cordier, L. F., Rabeza, V. R., Randriamanambintsoa, M., Razanadrakato, H. T. R., ... & Bonds, M. H. (2018). Early changes in intervention coverage and mortality rates following the implementation of an integrated health system intervention in Madagascar. BMJ global health, 3(3), e000762.
[10] Roodenbeke, E. D., & World Health Organization. (2011). Outreach services as a strategy to increase access to health workers in remote and rural areas. World Health Organization.
[11] Mweemba, C., Mapulanga, M., Jacobs, C., Katowa-Mukwato, P., & Maimbolwa, M. (2021). Access barriers to maternal healthcare services in selected hard-to-reach areas of Zambia: a mixed methods design. Pan African Medical Journal, 40(1).
[12] DHIS 2 retrieved from: https://www.dhis2.0.org. Assessed January 2022
[13] Mweemba, C., Mapulanga, M., Jacobs, C., Katowa-Mukwato, P., & Maimbolwa, M. (2021). Access barriers to maternal healthcare services in selected hard-to-reach areas of Zambia: a mixed methods design. Pan African Medical Journal, 40(1).
[14] Partapuri, T., Steinglass, R., & Sequeira, J. (2012). Integrated delivery of health services during outreach visits: a literature review of program experience through a routine immunization lens. Journal of Infectious Diseases, 205(suppl_1), S20-S27.
[15] Yaya, S., Komlan K., Amos B., and Ghose B. (2019). “Antenatal Visits Are Positively Associated with Uptake of Tetanus Toxoid and Intermittent Preventive Treatment in Pregnancy in Ivory Coast.”: 1–12.
[16] Nuamah, G. B., Agyei-Baffour, P., Mensah, K. A., Boateng, D., Quansah, D. Y., Dobin, D., & Addai-Donkor, K. (2019). Access and utilization of maternal healthcare in a rural district in the forest belt of Ghana. BMC pregnancy and childbirth, 19, 1-11.
[17] Tsegaw, Menen. 2022. “Modern Contraceptive Utilization and Associated Factors Among Married Women in Liberia: Evidence from the 2019 Liberia Demographic and Health Survey.” (February): 17–28.
[18] Lun, C. N., Aung, T., & Mya, K. S. (2021). Utilization of modern contraceptive methods and its determinants among youth in Myanmar: Analysis of Myanmar Demographic and Health Survey (2015-2016). Plos one, 16(10), e0258142.
[19] Hailu, S., Astatkie, A., Johansson, K. A., & Lindtjørn, B. (2019). Low immunization coverage in Wonago district, southern Ethiopia: a community-based cross-sectional study. PloS one, 14(7), e0220144.
[20] Animaw, W., Taye, W., Merdekios, B., Tilahun, M., & Ayele, G. (2014). Expanded program of immunization coverage and associated factors among children aged 12–23 months in Arba Minch town and Zuria District, Southern Ethiopia, 2013. BMC public health, 14(1), 1-10.
[21] Berihun, B., Chemir, F., Gebru, M., & GebreEyesus, F. A. (2023). Vitamin A supplementation coverage and its associated factors among children aged 6–59 months in West Azernet Berbere Woreda, Southwest Ethiopia. BMC pediatrics, 23(1), 1-13.
[22] Belay, D. G., Kibret, A. A., Diress, M., Gela, Y. Y., Sinamaw, D., Simegn, W., ... & Chilot, D. (2022). Deworming among preschool age children in sub-Saharan Africa: pooled prevalence and multi-level analysis. Tropical Medicine and Health, 50(1), 74.
[23] Forson, A. O., Abdul-Basit, S., Awusi, G. K., Taiwo, M. O., & Baidoo, I. A. (2023). A comparative study on the prevalence of intestinal hel-minths in dewormed and non-dewormed healthy persons in Ghana. J Clin Images Med Case Rep, 4(3), 2322.
[24] Zegeye, B., Ahinkorah, B. O., Idriss-Wheeler, D., Olorunsaiye, C. Z., Adjei, N. K., & Yaya, S. (2021). Modern contraceptive utilization and its associated factors among married women in Senegal: a multilevel analysis. BMC Public Health, 21(1), 1-13.
[25] Manyeh, A. K., Amu, A., Williams, J., & Gyapong, M. (2020). Factors associated with the timing of antenatal clinic attendance among first-time mothers in rural southern Ghana. BMC pregnancy and childbirth, 20(1), 1-7.
[26] Ahuru, R. R. & Omon, I. J. (2019). Predictors of Antenatal Care Utilization in Primary Healthcare Centers in Eight Rural Communities in Delta State, Nigeria. African Journal of Health Economics, 8, 1-2.
[27] Nuamah, G. B., Agyei-Baffour, P., Mensah, K. A., Boateng, D., Quansah, D. Y., Dobin, D., & Addai-Donkor, K. (2019). Access and utilization of maternal healthcare in a rural district in the forest belt of Ghana. BMC pregnancy and childbirth, 19, 1-11.
[28] Debebe, S., Miteku A. L. and Belete, B. (2017). “Modern Contraceptive Methods Utilization and Associated Factors among Reproductive Aged Women in Rural Dembia District, Northwest Ethiopia: Community Based Cross-Sectional Study.” International Journal of Reproductive BioMedicine 15(6): 367–74.
[29] Maxwell T. Kumbenia and Paschal A. Apangab. (2021). “Institutional Delivery and Associated Factors among Women in Ghana: Findings from a 2017 – 2018 Multiple Indicator Cluster Survey.”: 1–7.
[30] Asekun O E, Adebimpe W, Bamidele J, Odu O, Asekun O I, Ojofeitimi E. Barriers to use of modern contraceptives among women in an inner-city area of Osogbo metropolis, Osun state, Nigeria. Int J Women H. 2013;11(5):647–655
[31] Durowade KA, Omokanye LO, Elegbede OE, Adetokunbo S, Olomofe CO, Ajiboye AD, Adeniyi MA, Sanni TA. Barriers to Contraceptive Uptake
among Women of Reproductive Age in a Semi-Urban Community of Ekiti State, Southwest Nigeria. Ethiop J Health Sci. 2017 Mar;27(2):121-128.[32] Haddrill, R., Jones, G. L., Mitchell, C. A., & Anumba, D. O. (2014). Understanding delayed access to antenatal care: a qualitative interview study. BMC pregnancy and childbirth, 14(1), 1-14.
[33] Modibbo, U. M., Ali, I., & Ahmed, A. (2021). Multi-objective optimization modelling for analysing sustainable development goals of Nigeria: Agenda 2030. Environment, Development and Sustainability, 23(6), 9529-9563.
[34] Galadima, A. N., Zulkefli, N. A. M., Said, S. M., & Ahmad, N. (2021). Factors influencing childhood immunisation uptake in Africa: a systematic review. BMC Public Health, 21(1), 1-20.
[35] Nour, T. Y., Farah, A. M., Ali, O. M., & Abate, K. H. (2020). Immunization coverage in Ethiopia among 12–23-month-old children: systematic review and meta-analysis. BMC Public Health, 20(1), 1-12.
Viewed PDF 737 24 -
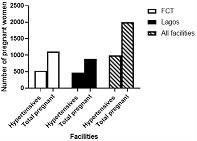 Control of Hypertension in Pregnant Women in Secondary Health Facilities in Nigeria: A Cross-Sectional StudyAuthor: Jennifer Adaeze ChukwuDOI: 10.21522/TIJPH.2013.11.04.Art019
Control of Hypertension in Pregnant Women in Secondary Health Facilities in Nigeria: A Cross-Sectional StudyAuthor: Jennifer Adaeze ChukwuDOI: 10.21522/TIJPH.2013.11.04.Art019Control of Hypertension in Pregnant Women in Secondary Health Facilities in Nigeria: A Cross-Sectional Study
Abstract:
Hypertension is among the non-communicable diseases that complicate pregnancies in women. Diagnosis and control of this condition are important in reducing the risk of maternal and foetal mortality. This study was aimed at determining the prevalence and control of hypertension among pregnant women visiting secondary health care facilities in four Local Government Areas in Lagos (2) and Abuja (Federal Capital Territory) (2), Nigeria. Our findings showed that there was a high prevalence of hypertension in these facilities (50%). Our finding also revealed that the overall level of control was 30.45%, which decreased with time in the course of the management. The control was highest in the first quarter and lowest in the third (last) quarter. The consistent and appropriate use of antihypertensives is important to prevent the complications associated with non-communicable diseases like hypertension during pregnancy. Healthcare providers should therefore advocate early diagnosis and management of hypertension during pregnancy.
Keywords: Control, Hypertension, Non-communicable diseases, Pregnancy, Secondary healthcare.Control of Hypertension in Pregnant Women in Secondary Health Facilities in Nigeria: A Cross-Sectional Study
References:
[1] WHO Hypertension Available online: https://www.who.int/news-room/fact-sheets/detail/hypertension (accessed on 19 October 2023).
[2] Braunthal, S.; Brateanu, A. Hypertension in Pregnancy: Pathophysiology and Treatment. SAGE Open Med. 2019, 7, doi:10.1177/2050312119843700.
[3] Msughter, A.E. “Pregnancy Induced Hypertension in Kabo Local Government Area of Kano State, Nigeria.” Biomed. J. Sci. Tech. Res. 2021, 39, doi:10.26717/BJSTR.2021.39.006321.
[4] Mammaro, A.; Carrara, S.; Cavaliere, A.; Ermito, S.; Dinatale, A.; Pappalardo, E.M.; Militello, M.; Pedata, R.; Cacciatore, A. Hypertensive Disorders of Pregnancy. J. Prenat. Med. 2009, 3, 1.
[5] Beech, A.; Mangos, G. Management of Hypertension in Pregnancy. Aust. Prescr. 2021, 44, 148, doi:10.18773/AUSTPRESCR.2021.039.
[6] Kintiraki, E.; Papakatsika, S.; Kotronis, G.; Goulis, D.G.; Kotsis, V. Pregnancy-Induced Hypertension. Hormones (Athens). 2015, 14, 211–223, doi:10.14310/HORM.2002.1582.
[7] Hossain, N.; Shaikh, Z.F. Maternal Deaths Due to Indirect Causes: Report from a Tertiary Care of a Developing Country. Obstet. Med. 2022, 15, 176, doi:10.1177/1753495X211037916.
[8] Carey, R.M.; Muntner, P.; Bosworth, H.B.; Whelton, P.K. Prevention and Control of Hypertension: JACC Health Promotion Series. J. Am. Coll. Cardiol. 2018, 72, 1278, doi:10.1016/J.JACC.2018.07.008.
[9] Muti, M.; Tshimanga, M.; Notion, G.T.; Bangure, D.; Chonzi, P. Prevalence of Pregnancy Induced Hypertension and Pregnancy Outcomes among Women Seeking Maternity Services in Harare, Zimbabwe. BMC Cardiovasc. Disord. 2015, 15, 1–8, doi:10.1186/S12872-015-0110-5/TABLES/3.
[10] Ebeigbe, P..; Igberase, G..; Aziken, M.. Hypertensive Disorders in Pregnancy: Experience with 442 Recent Consecutive Cases in Benin City, Nigeria. Niger. Med. J. 2007, 48, doi:10.4314/NMJ.V48I4.50895.
[11] Singh, S.; Ahmed, E.B.; Egondu, S.C.; Ikechukwu, N.E. Hypertensive Disorders in Pregnancy among Pregnant Women in a Nigerian Teaching Hospital. Niger. Med. J. 2014, 55, 384, doi:10.4103/0300-1652.140377.
[12] Bello, N.A.; Zhou, H.; Cheetham, T.C.; Miller, E.; Getahun, D.T.; Fassett, M.J.; Reynolds, K. Prevalence of Hypertension Among Pregnant Women When Using the 2017 American College of Cardiology/American Heart Association Blood Pressure Guidelines and Association with Maternal and Fetal Outcomes. JAMA Netw. Open 2021, 4, e213808–e213808, doi:10.1001/JAMANETWORKOPEN.2021.3808.
[13] Tebeu, P.M.; Foumane, P.; Mbu, R.; Fosso, G.; Biyaga, P.T.; Fomulu, J.N. Risk Factors for Hypertensive Disorders in Pregnancy: A Report from the Maroua Regional Hospital, Cameroon. J. Reprod. Infertil. 2011, 12, 227.
[14] Brown, C.M.; Garovic, V.D. Drug Treatment of Hypertension in Pregnancy. Drugs 2014, 74, 283, doi:10.1007/S40265-014-0187-7.
[15] Hoeltzenbein, M.; Beck, E.; Fietz, A.K.; Wernicke, J.; Zinke, S.; Kayser, A.; Padberg, S.; Weber-Schoendorfer, C.; Meister, R.; Schaefer, C. Pregnancy Outcome after First Trimester Use of Methyldopa: A Prospective Cohort Study. Hypertension 2017, 70, 201–208, doi:10.1161/HYPERTENSIONAHA.117.09110.
[16] Folic, M.M.; Jankovic, S.M.; Varjacic, M.R.; Folic, M.D. Effects of Methyldopa and Nifedipine on Uteroplacental and Fetal Hemodynamics in Gestational Hypertension. Hypertens. pregnancy 2012, 31, 31–39, doi:10.3109/10641955.2010.525274.
[17] Alavifard, S.; Chase, R.; Janoudi, G.; Chaumont, A.; Lanes, A.; Walker, M.; Gaudet, L. First-Line Antihypertensive Treatment for Severe Hypertension in Pregnancy: A Systematic Review and Network Meta-Analysis. Pregnancy Hypertens. 2019, 18, 179–187, doi:10.1016/J.PREGHY.2019.09.019.
[18] Podymow, T.; August, P. Antihypertensive Drugs in Pregnancy. Semin. Nephrol. 2011, 31, 70–85, doi:10.1016/J.SEMNEPHROL.2010.10.007.
[19] Gupta, M.; Khalili, Y. Al Methyldopa. xPharm Compr. Pharmacol. Ref. 2023, 1–5, doi:10.1016/B978-008055232-3.62162-2.
[20] Cohen, J.S. Adverse Drug Effects, Compliance, and Initial Doses of Antihypertensive Drugs Recommended by the Joint National Committee vs the Physicians’ Desk Reference. Arch. Intern. Med. 2001, 161, 880–885, doi:10.1001/ARCHINTE.161.6.880.
[21] Taibanguay, N.; Chaiamnuay, S.; Asavatanabodee, P.; Narongroeknawin, P. Effect of Patient Education on Medication Adherence of Patients with Rheumatoid Arthritis: A Randomized Controlled Trial. Patient Prefer. Adherence 2019, 13, 119, doi:10.2147/PPA.S192008.
Viewed PDF 645 17 -
Development and Evaluation of Tuberculosis Case Detection and Management Training for Community Pharmacists in Lagos, NigeriaAuthor: Okafor, Ukamaka GladysDOI: 10.21522/TIJPH.2013.11.04.Art020
Development and Evaluation of Tuberculosis Case Detection and Management Training for Community Pharmacists in Lagos, Nigeria
Abstract:
Training enhances efficiency and develops a systematic way of performing duties. Community pharmacists are well-positioned as safety nets and can be trained to play a significant role in halting the progression of Tuberculosis (TB) disease. The study aimed at developing and evaluating the appropriateness of TB case detection and management training for community pharmacists in Lagos State, Nigeria. A one-day training to identify and refer individuals with TB symptoms to diagnostic facilities, was developed, conducted, and evaluated on a 5-point Likert scale, a semi-structured questionnaire, that was administered to 285 randomly sampled respondents. Participants’ opinion was rated on the training content, resource persons, and sufficiency of the training. The results of pre and post-tests were manually analyzed. Quantitative data were coded and analyzed using Statistical Package for Social Sciences Version 17. Descriptive statistics: percentage, frequency, mean and standard deviation were also used to analyze the data. Open-ended responses were analyzed thematically. The response rate was 67.02%. Respondents strongly agreed (47.37%) and agreed (46.05%) that the training was sufficient to enable community pharmacies to provide TB services in their pharmacy. Respondents expressed themselves on what they valued most about the training and made recommendations to improve and ensure the progress of the intervention. Exposure of community pharmacists to appropriate training significantly increased their knowledge in TB case detection and management. The training was fit for the purpose it was designed for. Community pharmacists could be a valuable asset in the prevention and control of TB in Nigeria.
Keywords: Evaluation, Pharmacists, Training, Tuberculosis.Development and Evaluation of Tuberculosis Case Detection and Management Training for Community Pharmacists in Lagos, Nigeria
References:
[1] United States Embassy in Nigeria, 2012, Tuberculosis Fact Sheet 2012, https://photos.state.gov/libraries/nigeria/487468/pdfs/JanuaryTuberculosisFactSheet.pdf//.
[2] FMOH: The National Strategic Plan for TB control, 2015.
[3] WHO, 2015, Tuberculosis: DOTS case detection rate 2015, https://www.who.int/whosis/whostat2006TuberculosisDOTSDetectionRate.pdf.
[4] World Health Organization, 2020, Global TB report, 2020, Geneva, Switzerland: WHO, https://www.who.int/publications-detail-redirect/9789240013131.
[5] Federal Ministry of Health National TB and leprosy control program annual report 2019, https://www.health.gov.ng/doc/Draft-2019-NTBLCP-Annual-report-22032020.pdf.
[6] World Health Organization, 2021, Gearing towards a TB free Nigeria- WHO and partners scale up action, https://www.afro.who.int/news/gearing-towards-tb-free-nigeria-who-and-partners-scale-action.
[7] The World Health Organization, 2023, Tuberculosis report, https://www.who.int/news-room/fact-sheets/detail/tuberculosis.
[8] TB Online: Information for Activists, patients, health workers and researchers working to end TB, www. tbonline.info/posts/category/Article.
[9] Government of India and India Pharmaceutical Association, 2013, RNTCP Training Modules for Community Pharmacists 2013. http://www.pci.nic.in/Circulars/Training%20Module.pdf.
[10] Konduri, N., Delmotte, E. and Rutta E., 2017, Engagement of the private pharmaceutical sector for TB control: rhetoric or reality? Journal of Pharmaceutical Policy and Practice, 10:6 DOI 10.1186/s40545-016-0093-3.
[11] Amrita, D., Nita, J., Madhukar, P., 2017, Enhancing the role of pharmacists in the cascade of tuberculosis care, Journal of Epidemiology and Global Health, 7(1), 1-4, ISSN 2210-6006, https://doi.org/10.1016/j.jegh.2016.05.001.
[12] Jakeman, B., Gross, B., Fortune, D., Babb, S., Tinker, D., Bachyrycz, A., 2015, Evaluation of a pharmacist-performed tuberculosis testing initiative in New Mexico, Journal of the American Pharmacists Association, 55(3), 307-312, ISSN 1544-3191, https://doi.org/10.1331/JAPhA.2015.14141.
[13] Gelband, H., Miller, Petrie, M., Pant, S., Gandra, S., Levinson, J., Barter, D., ... & Laxminarayan, R., 2015, The state of the world’s antibiotics 2015, Wound healing southern africa, 8(2), 30-34.
[14] Kotwani, A., & Holloway, K., 2011. Trends in antibiotic use among outpatients in New Delhi, India, BMC infectious diseases, 11, 1-9.
[15] Bell, C. A., Duncan, G. J., Eang, R., & Saini, B., 2015, Stakeholder perceptions of a pharmacy-initiated tuberculosis referral program in cambodia, 2005-2012, Asia Pacific Journal of Public Health, 27(2), NP2570-NP2577.
[16] Lonnroth, K., Lambregts, K., Nhien, D. T. T., Quy, H. T., & Diwan, V. K., 2000, Private pharmacies and TB control–a survey of case detection skills and reported anti-TB dispensing in private pharmacies in Ho Chi Minh City, Vietnam, International Journal of Tuberculosis and Lung Disease, 4, 1052-1059.
[17] Vu, D. H., Van Rein, N., Cobelens, F. G. J., Nguyen, T. T. H., Le, V. H., & Brouwers, J. R. B. J., 2012, Suspected tuberculosis case detection and referral in private pharmacies in Viet Nam, The International journal of tuberculosis and lung disease, 16(12), 1625-1629.
[18] Chalker, J., Chuc, N. T. K., Falkenberg, T., & Tomson, G., 2002, Private pharmacies in Hanoi, Vietnam: a randomized trial of a 2‐year multi‐component intervention on knowledge and stated practice regarding ARI, STD and antibiotic/steroid requests, Tropical Medicine & International Health, 7(9), 803-810.
[19] Hurtig, A. K., Pande, S. B., Baral, S. C., Porter, J. D. H., & Bam, D. S., 2000, Anti-tuberculosis treatment in private pharmacies, Kathmandu Valley, Nepal, The International Journal of Tuberculosis and Lung Disease, 4(8), 730-736.
[20] Bell, C. A., Eang, M. T., Dareth, M., Rothmony, E., Duncan, G. J., & Saini, B., 2012, Provider perceptions of pharmacy-initiated tuberculosis referral services in Cambodia, 2005–2010, The International journal of tuberculosis and lung disease, 16(8), 1086-1091.
[21] Rutta, E., Tarimo, A., Delmotte, E., James, I., Mwakisu, S., Kasembe, D., ... & Valimba, R., 2014, Understanding private retail drug outlet dispenser knowledge and practices in tuberculosis care in Tanzania, The international journal of tuberculosis and lung disease, 18(9), 1108-1113.
[22] Kalkidan, Y., 2016, Suspected Tuberculosis Patient Identification and Referral by Private Drug Retail Outlet Workers in South Wollo, Ethiopia Thesis submitted to University of Oslo for fulfillment of Master of Philosophy Degree in International Community Health, https://www.duo.uio.no/bitstream/handle/10852/52330/sosna.pdf?sequence=1&isAllowed=y.
[23] Okafor, U.G, Oreagba, I., 2019, Assessment of Level of Community Pharmacists’ Knowledge and Involvement in Tuberculosis Case Detection and Management in Lagos State, Nigeria, Texila International Journal of Public Health, 7(2).
[24] Darko, S., Plange, E. D., & Tetteh-Bator, E., 2020, Factors Contributing to Low Tuberculosis Case Detection in West Akim Municipality of the Eastern Region of Ghana; A Community and Health Facility Based Study, https://pdfs.semanticscholar.org/de9e/ee0ee026df52c232cb2c909ccb80528a0082.pdf.
[25] Harshit, T., 2012, Evaluation of Training and Development: An Analysis of Various Models, IOSR Journal of Business and Management (IOSR-JBM), ISSN: 2278-487X, 5 (2), 16-22, http://iosrjournals.org/iosr-jbm/papers/Vol5-issue2/B0521622.pdf.
[26] Suja, N.S., 2013, Health Ministry develops training module for community pharmacists under RNTCP 2013, http://pharmabiz.com/PrintArticle.aspx?aid=74734&sid=1.
[27] Gopal, Effectiveness of executive Training Programs, The Indian Journal of Commerce, 2008; 62(3):143-150.
[28] Nagar, V., 2009, Measuring Training Effectiveness, The Indian Journal of Commerce, 62(4): 86-90.
[29] UN World Urbanization Prospects, 2023, https://worldpopulationreview.com/world-cities/lagos-population.
[30] Adejumo, O. A., Daniel, O. J., Otesanya, A. F., & Adejumo, E. N., 2016, Determinants of health system delay at public and private directly observed treatment, short course facilities in Lagos State, Nigeria: A cross-sectional study, International Journal of Mycobacteriology, 5(3), 257-264, https://www.sciencedirect.com/science/article/pii/S2212553116300164.
[31] Adejumo, O. A., Daniel, O. J., Abdur-Razzaq, H. A., Shogbamimu, Y. O., Femi-Adebayo, T., Adepoju, V. A., ... & Sodipo, O. O., 2017, Trend of tuberculosis case notification and treatment outcome in Lagos State, Nigeria: a 5-year retrospective study, Transactions of the Royal Society of Tropical Medicine and Hygiene, 111(7), 300-307, https://academic.oup.com/trstmh/article-abstract/111/7/300/4643092.
[32] Adejumo, O. A., Daniel, O. J., Adejumo, E. N., Oluwole, E. O., & Olumuyiwa, O. O., 2015, Treatment outcomes of tuberculosis patients managed at the public and private DOTS Facilities in Lagos Nigeria, International Journal of Tropical Disease & Health, 10(2), 1-9, https://api-ir.unilag.edu.ng/server/api/core/bitstreams/c0e54ae4-9773-4ec2-8fe5-58534af124f8/content.
[33] Cochran, W. G., 1977, Sampling techniques (3rd ed.). New York: John Wiley & Sons.
[34] PCN: A list of Registered Pharmacists and Pharmaceutical Premises in Nigeria; A publication of the Pharmacists Council of Nigeria 2015.
[35] Shaira Alliah de Castro, Citation Preview: Curriculum planning sources and influences, https://www.scribd.com/presentation/475077775/Curriculum-planning-sources-and-influences and https://pdfcoffee.com/pec-103docx-pdf-free.html.
[36] Eliot & Associates, Guidelines for conducting a Focus Group 2005, https://assessment.trinity.duke.edu/documents/ How_to_Conduct_a_Focus_Group.pdf.
[37] Carolyn, B., Palena, N., 2006, Conducting In-depth Interviews: a guide for designing and conducting in-depth interviews for evaluation input, Pathfinder International Tool Series 2006, www.pathfinder.org/site/m_e_tool_series_indepth_interviews.pdf.
[38] Bajorek, B. V., Lemay, K. S., Magin, P. J. et al., 2015, Preparing pharmacists to deliver a targeted service in hypertension management: evaluation of an interprofessional training program, BMC Med Educ., 15:157 https://link.springer.com/article/10.1186/s12909-015-0434-y.
[39] Zahra, N. W., 2011, Survey on the knowledge Attitude and Practices on Tuberculosis among Healthcare workers in Kingston and St. Andrew, Jamaica, http://www.support.liverpoolonline.com/~/media/Files/UOLCSS/mph/MPH_Quantitative_Dissertation_2.pdf.
[40] Yejide O. O., Margaret O. A., 2020, Development and Evaluation of Health Promotion Training Program for Community Pharmacists in Oyo State, Nigeria, https://journals.sagepub.com/doi/abs/10.1177/2373379920918614.
[41] Parisa, A., Shalom, I. B., Ines, K., 2006, Development and evaluation of a training program to
foster the use of written drug information in community pharmacies 2006: Part 1–Development, https://pharmacyeducation.fip.org/pharmacyeducation/article/view/102/82.[42] Saini, B., Smith, L., Armour, C., et al., 2006, An educational intervention to train community pharmacists in providing specialized asthma care, American journal of pharmaceutical education, 70(5): 118. https://doi.org/10.5688/aj7005118.
[43] Fitzgerald, N., Watson, H., McCaig, D. et al., 2009, Developing and evaluating training for community pharmacists to deliver interventions on alcohol issues, Pharm World Sci, 31:149–153.https://link.springer.com/article/10.1007%2Fs11096-009-9284-1#citeas.
[44] Lilly MDR-TB Partnership, 2014, Creating champions of change. Enrolling community pharmacists in a national tuberculosis control initiative, The Lilly MDR-TB Partnership, https://lillypad.lilly.com/WP/wp-content/uploads/CreatingChampions-of-Change.pdf.
[45] PATH, 2011, Public-private mix. Involving pharmacies and other providers in TB control – a Cambodia case study, https://www.path.org/publications/ files/CP_cambodia_ppm_tb_cs.pdf.
[46] Chemonics International, 2006, Philippine Tuberculosis Initiatives for the Private Sector Final Report, USAID Contract No. 492-C-00-02-00031.
[47] Morris, O., Freddy, E.K., Bush, H.A., et al., 2012, Strengthening Community Pharmacies Role in Early Tuberculosis Case Detection and Referrals – Case Study of Jinja Municipality, https://www.scribd.com/document/240247366.
[48] Bloch, R., Fox, S., Monroy, J., et al., 2015, Urbanisation and Urban Expansion in Nigeria. Urbanisation Research Nigeria (URN) Research Report. London: ICF, International Creative Commons Attribution-Non-Commercial-Share Alike CC, https://core.ac.uk/download/pdf/96701289.pdf.
Viewed PDF 651 22 -
Medical Male Circumcision and HIV Testing Practices among Men Aged 15 to 59 Years Old: Evidence from Zambia Demographics and Health SurveyAuthor: Edson ChipaloDOI: 10.21522/TIJPH.2013.11.04.Art021
Medical Male Circumcision and HIV Testing Practices among Men Aged 15 to 59 Years Old: Evidence from Zambia Demographics and Health Survey
Abstract:
Medical male circumcision (MMC) and HIV testing have been recommended by the World Health Organization (WHO) as part of a comprehensive approach to HIV prevention. Zambia has integrated MMC with HIV testing interventions. This study examined the syndemic relationship between MMC and HIV testing, as well as sociodemographic characteristics influencing both MMC and HIV testing in Zambia. Data were derived from the 2018 Zambia Demographic and Health Survey (ZDHS), a nationally representative cross-sectional survey conducted among 12,123 men aged 15 to 59 years. Descriptive characteristics were summarized using frequencies and proportions. Two multivariate logistic regression models examined the relationship between independent and dependent variables (HIV testing and MMC alternatively). The results showed that 76.8% of men reported having ever tested for HIV, and 26% performed MMC. The logistic regression results showed that MMC was significantly associated with ever being tested for HIV and vice versa. Sociodemographic characteristics, including province, resident type, age, marital status, education, wealth status, and religion, were also significantly associated with MMC and having tested for HIV among men in Zambia. By and large, this study has identified that both MMC and HIV have an intricate relationship with health benefits to reduce the risk of HIV infections for men in Zambia. There is a need for continuous scaling up the perceived benefits of MMC and HIV testing uptake. In addition, more robust awareness is needed in specific provinces, rural areas, and other sociodemographic variables with lower incidences of MMC and HIV testing practices among men in Zambia.
Keywords: HIV testing, Men, Medical male circumcision, Sociodemographic characteristics, Zambia.Medical Male Circumcision and HIV Testing Practices among Men Aged 15 to 59 Years Old: Evidence from Zambia Demographics and Health Survey
References:
[1] Task Force on Circumcision, Male circumcision. Pediatrics, 2012. 130(3): p. e756-e785.
[2] Dévieux, J.G., et al., Knowledge, attitudes, practices and beliefs about medical male circumcision (MMC) among a sample of health care providers in Haiti. Plos one, 2015. 10(8): p. e0134667.
[3] Drain, P.K., et al., Male circumcision, religion, and infectious diseases: an ecologic analysis of 118 developing countries. BMC infectious diseases, 2006. 6(1): p. 1-10.
[4] Totaro, A., et al., Circumcision: history, religion and law. Urologia Journal, 2011. 78(1): p. 1-9.
[5] Odoyo-June, E., et al., Unexpected complications following adult medical male circumcision using the PrePex Device. Urologia Internationalis, 2016. 96(2): p. 188-193.
[6] Samuelson, J., R. Baggaley, and G. Hirnschall, Innovative device methods for adult medical male circumcision for HIV prevention: lessons from research. 2013, LWW. p. 127-129.
[7] Zulu, R., et al., Sexual satisfaction, performance, and partner response following voluntary medical male circumcision in Zambia: the spear and shield project. Global Health: Science and Practice, 2015. 3(4): p. 606-618.
[8] Kamanga, J., et al., Improved HIV case finding among key populations after differentiated data driven community testing approaches in Zambia. Plos one, 2021. 16(12): p. e0258573.
[9] Hargreaves, J.R., et al., The association between HIV stigma and HIV incidence in the context of universal testing and treatment: analysis of data from the HPTN 071 (PopART) trial in Zambia and South Africa. Journal of the International AIDS Society, 2022. 25: p. e25931.
[10] Gray, R.H., et al., Male circumcision for HIV prevention in men in Rakai, Uganda: a randomised trial. The lancet, 2007. 369(9562): p. 657-666.
[11] Mwiinga, K., Male circumcision in Lusaka, Zambia. Southern African Journal of Demography, 2020. 20(1): p. 1-31.
[12] Garenne, M. and A. Matthews, Voluntary medical male circumcision and HIV in Zambia: expectations and observations. Journal of Biosocial Science, 2020. 52(4): p. 560-572.
[13] Weiss, S.M., et al., Increasing early infant male circumcision uptake in Zambia: Like father like son. PloS one, 2023. 18(8): p. e0289819.
[14] Bendera, A., et al., Factors Associated with Low Uptake of Medical Male Circumcision Among Adolescent Boys in Tanzania: A Multinomial Logistic Regression Modeling. HIV/AIDS-Research and Palliative Care, 2022: p. 565-575.
[15] Lindsay, B.R., et al., Peer community health workers improve HIV testing and ART linkage among key populations in Zambia: retrospective observational results from the Z‐CHECK project, 2019–2020. Journal of the International AIDS Society, 2022. 25(11): p. e26030.
[16] Bicer, S., et al., At what age range should children be circumcised? Iranian Red Crescent Medical Journal, 2015. 17(3).
[17] Haacker, M., N. Fraser-Hurt, and M. Gorgens, Effectiveness of and financial returns to voluntary medical male circumcision for HIV prevention in South Africa: an incremental cost-effectiveness analysis. PLoS Medicine, 2016. 13(5): p. e1002012.
[18] Kelly, M.E., et al., The impact of social activities, social networks, social support and social relationships on the cognitive functioning of healthy older adults: a systematic review. Systematic reviews, 2017. 6(1): p. 1-18.
[19] Ntsabane, M., G. Letamo, and M. Keetile, Factors associated with low uptake of safe male circumcision (SMC) and the intention not to undergo circumcision among men in Botswana. Journal of Public Health, 2023: p. 1-11.
[20] Jiang, J., et al., Acceptance of male circumcision among male rural-to-urban migrants in western China. AIDS research and human retroviruses, 2013. 29(12): p. 1582-1588.
[21] Keetile, M. and S.D. Rakgoasi, Male Circumcision; willingness to undergo safe male circumcision and HIV risk behaviors among men in Botswana. African Population Studies, 2014. 28(3): p. 1345-1361.
[22] Mangombe, K. and I. Kalule-Sabiti, Predictors of male circumcision among men aged 15–35 years in Harare, Zimbabwe. Journal of biosocial science, 2018. 50(2): p. 193-211.
[23] Nanteza, B.M., et al., Knowledge on voluntary medical male circumcision in a low uptake setting in northern Uganda. BMC public health, 2018. 18(1): p. 1-7.
[24] Kibira, S.P., et al., Differences in risky sexual behaviors and HIV prevalence of circumcised and uncircumcised men in Uganda: evidence from a 2011 cross-sectional national survey. Reproductive health, 2014. 11: p. 1-8.
[25] Gasasira, R.A., et al., Determinants of circumcision and willingness to be circumcised by Rwandan men, 2010. BMC public health, 2012. 12: p. 1-8.
[26] Bailey, R.C., S. Neema, and R. Othieno, Sexual behaviors and other HIV risk factors in circumcised and uncircumcised men in Uganda. Journal of Acquired Immune Deficiency Syndromes (1999), 1999. 22(3): p. 294-301.
[27] Chikutsa, A., A.C. Ncube, and S. Mutsau, Association between wanting circumcision and risky sexual behaviour in Zimbabwe: evidence from the 2010–11 Zimbabwe demographic and health survey. Reproductive Health, 2015. 12: p. 1-8.
[28] Kateule, E., et al., A cross-sectional study of the factors associated with male circumcision status among college youth in Ndola, Zambia, 2016. Southern African Journal of HIV Medicine, 2019. 20(1): p. 1-7.
[29] Wambura, M., et al., Acceptability of medical male circumcision in the traditionally circumcising communities in Northern Tanzania. BMC public health, 2011. 11(1): p. 1-8.
[30] Qian, H.-Z., et al., Lower HIV risk among circumcised men who have sex with men in China: Interaction with anal sex role in a cross-sectional study. Journal of acquired immune deficiency syndromes (1999), 2016. 71(4): p. 444.
[31] Peltzer, K., et al., Prevalence and acceptability of male circumcision in South Africa. African Journal of Traditional, Complementary and Alternative Medicines, 2014. 11(4): p. 126-130.
[32] Musheke, M., et al., A systematic review of qualitative findings on factors enabling and deterring uptake of HIV testing in Sub-Saharan Africa. BMC public health, 2013. 13(1): p. 1-16.
[33] Zambia Statistics Agency, M.o.H.Z. and ICF, Zambia demographic and health survey 2018. Lusaka, Zambia, and Rockville, Maryland, USA: Zambia Statistics Agency, Ministry of Health, and ICF, 2019.
[34] Hargreave, T., Male circumcision: towards a World Health Organisation normative practice in resource limited settings. Asian journal of andrology, 2010. 12(5): p. 628.
[35] Hatzold, K., et al., HIV self‐testing: breaking the barriers to uptake of testing among men and adolescents in sub‐Saharan Africa, experiences from STAR demonstration projects in Malawi, Zambia and Zimbabwe. Journal of the International AIDS Society, 2019. 22: p. e25244.
[36] Ministry of Health. Male Circumcision Situation Analysis. 2009; Available from: https://www.malecircumcision.org/sites/default/files/document_library/Zambia_MC_Situation_Analysis_Report.pdf.
[37] Ministry of Health. Attain the goal of circumcising 2 000 000 males by the year 2020. 2019 [cited 2019 November 23rd]; Available from: https://www.moh.gov.zm/?p=5842.
[38] Schafer, K.R., et al., The continuum of HIV care in rural communities in the United States and Canada: what is known and future research directions. Journal of acquired immune deficiency syndromes (1999), 2017. 75(1): p. 35.
[39] Mutombo, N., B. Maina, and M. Jamali, Male circumcision and HIV infection among sexually active men in Malawi. BMC Public Health, 2015. 15(1): p. 1-9.
[40] World Health Organization [WHO]. Male circumcision Global trends and determinants of prevalence, safety, and acceptability. 2007 [cited 2021 November 23rd].
[41] Vermund, S.H., et al., Can combination prevention strategies reduce HIV transmission in generalized epidemic settings in Africa? The HPTN 071 (PopART) study plan in South Africa and Zambia. JAIDS Journal of Acquired Immune Deficiency Syndromes, 2013. 63: p. S221-S227.
[42] Mukuka, D.M., A theological critique of the declaration of Zambia as a Christian nation and the response of the Roman Catholic Church from 1991-2001. 2014.
[43] Vigliotti, V., et al., Religion, faith, and spirituality influences on HIV prevention activities: A scoping review. PloS one, 2020. 15(6): p. e0234720.
[44] Kalule-Sabiti, I. and K. Mangombe, Knowledge about male circumcision and perception of risk for HIV among youth in Harare, Zimbabwe. Southern African Journal of HIV Medicine, 2019. 20(1): p. 1-9.
[45] Sharkey, T., et al., Use of “Strengthening Our Vows” Video Intervention to Encourage Negotiated Explicit Sexual Agreements in Zambian Heterosexual HIV Seroconcordant-Negative Couples. Archives of Sexual Behavior, 2023: p. 1-19.
[46] Kiyai, R.N., D.L. Ejalu, and D. Kimuli, Missed opportunity: low uptake of VMMC among men attending the OPD of a public health facility offering free VMMC services in Uganda. BMC Public Health, 2023. 23(1): p. 1-10.
[47] Wilcken, A., et al., Male circumcision for HIV prevention-a cross-sectional study on awareness among young people and adults in rural Uganda. BMC public health, 2010. 10: p. 1-11.
[48] Lau, F.K., S. Jayakumar, and S.K. Sgaier, Understanding the socio-economic and sexual behavioural correlates of male circumcision across eleven voluntary medical male circumcision priority countries in southeastern Africa. BMC Public Health, 2015. 15: p. 1-11.
[49] Mishra, V., et al., HIV infection does not disproportionately affect the poorer in sub-Saharan Africa. 2007, LWW. p. S17-S28.
[50] Chiringa, I.O., D.U. Ramathuba, and N.S. Mashau, Factors contributing to the low uptake of medical male circumcision in Mutare Rural District, Zimbabwe. African Journal of Primary Health Care and Family Medicine, 2016. 8(2): p. 1-6.
[51] Skolnik, L., et al., A cross-sectional study describing motivations and barriers to voluntary medical male circumcision in Lesotho. BMC public health, 2014. 14(1): p. 1-10.
[52]McGill, N., Education attainment linked to health throughout lifespan: Exploring social determinants of health. 2016, American Public Health Association.
[53] Tusabe, J., et al., Factors Influencing the Uptake of Voluntary Medical Male Circumcision Among Boda-Boda Riders Aged 18–49 Years in Hoima, Western Uganda. HIV/AIDS-Research and Palliative Care, 2022: p. 437-449.
Viewed PDF 1022 65 -
The Awareness of Depression Among School Teachers at Smka Al-Mashoor Perempuan, Penang IslandAuthor: Farhana Kamarul BahrinDOI: 10.21522/TIJPH.2013.11.04.Art022
The Awareness of Depression Among School Teachers at Smka Al-Mashoor Perempuan, Penang Island
Abstract:
This study aims to explore the awareness of teachers at SMKA Al-Mashoor Perempuan, Penang Island, regarding the issue of depression. Additionally, it investigates the coping strategies practiced by teachers to address depression. According to the World Health Organization (WHO), around 3.8% of the population is estimated to grapple with depression, encompassing 5% of adults (with a breakdown of 4% among men and 6% among women). Moreover, 5.7% of adults aged over 60 years are affected by depression. Depression is also said to have an impact on other health problems, whether chronic diseases or the increasing suicide rate in a country. Out of 22,000 depression patients treated at the psychiatric clinic in Universiti Malaya Medical Centre, 10% of them are reported to be teachers.Previous studies have indicated a lack of public knowledge about depression. Therefore, this study focuses on the knowledge of teachers regarding depression. To address the research objectives, an in-depth interview method was employed. The findings of this study were analyzed thematically. The results show that teachers are aware of the issue of depression. The coping strategies applied by teachers to address depression include social support and religious aspects. The study also suggests intervention methods to address depression, such as seeking treatment from experts and the importance of counseling sessions. The findings highlight the need for social workers in schools to address the increasing prevalence of depression among teachers, in addition to raising awareness about depression among educators.
Keywords: Coping Strategies, Depression, Mental Health, School Teacher, Social Work in School.
The Awareness of Depression Among School Teachers at Smka Al-Mashoor Perempuan, Penang Island
References:
[1] Mo Lee, G., Udin, A., & Aziz, M. H. A. (2012). Persepsi Guru Terhadap Kesihatan Mental Di Sekolah Menengah di Perak. Journal of Educational Psychology & Counseling Mental Health, 7, 1–10, http://www.ijepc.com/home.asm.
[2] Zakaria Ummi Kalsom. (2014). Faktor-Faktor Yang Mempengaruhi Tekanan Kerja Dalam Kalangan Guru Sekolah Menengah Daerah Hulu Terengganu, Terengganu Darul Iman. Disertasi Sarjana. Universiti Utara Malaysia: Kedah. 141, https://etd.uum.edu.my/5102/.
[3] Institute for Public Health. (2015). National Health And Morbidity Survey 2015 (NHMS 2015). Ministry of Health Malaysia. (Vol. II). Kuala Lumpur: Ministry of Health Malaysia, https://iku.nih.gov.my/nhms-2015.
[4] Sipon, S. (n.d.). Stres Kerja Guru : Punca, Kesan Dan Strategi Daya Tindak. Dalam Prosiding Seminar Profesion Perguruan. https://www.researchgate.net/profile/Sapora-Sipon/publication/280114629_Stress_Kerja_Guru_Punca_Kesan_dan_Strategi_Daya_Tindak/links/55aadaef08aea994672417e9/Stress-Kerja-Guru-Punca-Kesan-dan-Strategi-Daya-Tindak.pdf.
[5] Desouky, D., & Allam, H. (2017). Occupational Stress , Anxiety And Depression Among Egyptian Teachers. Journal of Epidemiology and Global Health, 7(3), 191–198, https://www.atlantis-press.com/journals/jegh/125905823.
[6] Ahola, K., Honkonen, T., & Isometsa, E. (2005). The Relationship Between Job-Related Burnout And Depressive Disorders — Results from the Finnish Health 2000 Study. Journal of Affective Disorders, 88(2005), 55–62, https://www.sciencedirect.com/science/article/abs/pii/S0165032705001606.
[7] Iacovides, A., Fountoulakis, K. N., Kaprinis, S., & Kaprinis, G. (2003). The Relationship Between Job Stress , Burnout And Clinical Depression. Journal of Affective Disorders, 75(2003), 209–221, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6424886/.
[8] Mohamad, M. S., & Ibrahim, R. (2018). Perbezaan gender tekanan psikologikal dan kesihatan mental dalam kalangan pelajar prasiswazah. Jurnal Personalia Pelajar, 21(1), 55–66. http://journalarticle.ukm.my/15985/.
[9] World Health Organization. (2022). World Health Statistics 2021 : MonitoringHhealth for the SDGs. Geneva: World Health Organization. https://www.who.int/data/gho/publications/world-health-statistics.
[10] Beaudry, M. B., Swartz, K., Miller, L., Schweizer, B., Glazer, K., & Wilcox, H. (2019). Effectiveness of The Adolescent Depression Awareness Program (ADAP) on Depression Literacy And Mental Health Treatment. Journal of School Health, (3), 165–172. https://www.sciencedirect.com/science/article/abs/pii/S0165032713003923.
[11] World Health Organization. (2018). World Health Statistics 2017 : Monitoring Health for the SDGs. Geneva: World Health Organization. https://www.who.int/publications/i/item/9789241565486.
[12] Abdullah, N. A. S., & Rosli, N. A. (2018). Kemurungan dalam Kalangan Mualaf di Pusat Pengajian PERKIM Wilayah Persekutuan. Malaysian Online Journal of Counseling, 5(1), 52–63. https://ejournal.um.edu.my/index.php/MOJC/article/view/10778.
[13] Sidana, S., Kishore, J., Ghosh, V., Gulati, D., Jiloha, R., & Anand, T. (2012). Prevalence Of Depression In Students Of A Medical College in New Delhi: A cross-sectional study. Australasian Medical Journal, 5(5), 247–250. https://www.semanticscholar.org/paper/Prevalence-of-depression-in-students-of-a-medical-A-Sidana-Kishore/9a2eeeddd5e3093f17c3e06843c75e5c3bc2611f.
[14] Ramli, J., Yahaya, A., Yahaya, N., & Lazin, S. Z. M. (2010). Kemurungan dalam Kalangan Penghuni Rumah Anak Yatim di daerah Kota Bharu, Kelantan. Journal of Science & Mathematics Education. https://www.semanticscholar.org/paper/Kemurungan-Dalam-Kalangan-Penghuni-Rumah-Anak-Yatim-Ramli-Yahaya/c3af4cb7478a00251fe8b520c0469556cb53ed89
[15] Othman, Z., & Sivasubramaniam, V. (2019). Depression, Anxiety, And Stress Among Secondary School Teachers in Klang, Malaysia. International Medical Journal, 26(2), 71–74. https://www.researchgate.net/publication/331430927_Depression_Anxiety_and_Stress_among_Secondary_School_Teachers_in_Klang_Malaysia.
[16] Akinsulore, A., Esimai, O. A., Mapayi, B. M., & Aloba, O. O. (2018). Public Awareness and Attitude towards Depression: A Community Based Study Among An Adult Population In Ile-Ife South-Western Nigeria. Community Mental Health Journal, 54(6), 866–874. https://link.springer.com/article/10.1007/s10597-017-0222-8.
[17] Safari, I. N. M., Kassim, N., Iskandar, N. F., Mohamed, M. H., & Abdullah, M. Y. (2011). Tahap Pengetahuan Mengenai Kesihatan Mental Dalam Kalangan Pelajar Institut Pengajian Tinggi Awam (IPTA) : kajian kes di UKM, Bangi. Jurnal Personalia Pelajar, 14, 37-44. http://journalarticle.ukm.my/4511/.
[18] Khan, T. M. (2009). Evaluation Of Public Knowledge And Clinical Management Of Depression In The State of Penang, Malaysia. Disertasi Sarjana Sains. Universiti Sains Malaysia: Penang. 135 pp. http://eprints.usm.my/29140/1/Evaluation_of_public_knowledge_and_clinical_management_of_depression_in_the_state_of_Penang%2C_Malaysia.pdf.
[19] Morris Anak Lat, & Han, C. G. K. (2018). Hubungan Antara Beban Tugas Dengan Stres Guru Kolej Vokasional di Negeri Sabah. Jurnal Pemikir Pendidikan, 9, 71–78. https://sainshumanika.utm.my/index.php/sainshumanika/article/view/1174.
[20] Buric, I., & Macuka, I. (2017). Self-Efficacy, Emotions And Work Engagement Among Teachers : A Two Wave Cross-Lagged Analysis. Journal of Happiness, 19(7), 1917-1933. https://link.springer.com/article/10.1007/s10902-017-9903-9.
[21] Azizi Yahaya, & Jamaludin Ramli. (2010). Stres Dalam Kalangan Guru Sekolah Menengah Di Empat Buah Negeri di Malaysia. Asia Pacific Journal of Educators and Education, 25, 103–136. http://apjee.usm.my/APJEE_25_2010/APJEE_25_07_Azizi%20(103-136).pdf.
[22] Kamaruddin, K. (2007). Tekanan Kerja di Kalangan Guru Sekolah Menengah. Jurnal Kemanusiaan, 10, 104-118. https://www.researchgate.net/publication/41804661_Tekanan_kerja_di_kalangan_guru_sekolah_menengah.
[23] Han, S., Yoon, A., Kim, M. J., & Yoon, J.-H. (2022). What influences tourist behaviors during and after the COVID-19 pandemic? Focusing on theories of risk, coping, and resilience. Journal of Hospitality and Tourism Management, 50, 355–365. https://www.sciencedirect.com/science/article/pii/S1447677022000365.
[24] Lazarus R. S., Folkman S. (1984). Stress, Appraisal and Coping. New York: Springer. https://link.springer.com/referenceworkentry/10.1007/978-1-4419-1005-9_215.
[25] Lazarus, R. S. (1993). Coping theory and research: past, present, and future. Psychosomatic Medicine, 55(3). https://link.springer.com/referenceworkentry/10.1007/978-1-4419-1005-9_215.
[26] Abdullah, S., Sipon, S., Baharudin, D. F., & Sawai, R. P. (2011). Strategi Daya Tindak Versi Bahasa Melayu. PERKAMA International Counseling Convention, 1–8. https://oarep.usim.edu.my/jspui/handle/123456789/5856.
[27] Bullare@Bahari, F., Ismail, R., Madlan@Endalan, L., & Lajuma, S. (2015). Strategi Daya Tindak Remaja Sekolah Dan Hubungannya Dengan Kemurungan. Jurnal Psikologi Malaysia, 1(29), 21–38. https://spaj.ukm.my/ppppm/jpm/issue/view/22.
[28] Votta, E., & Manion, I. G. (2003). Factors In The Psychological Adjustment Of Homeless Adolescent Males: The Role Of Coping Style. Journal of the American Academy of Child and Adolescent Psychiatry, 42(7), 778–785. https://www.sciencedirect.com/science/article/abs/pii/S0890856709609771.
[29] Ministry of Education Malaysia, 2017. https://www.moe.gov.my/en/.
[30] World Federation for Mental Health. (2010). Depression : What you know can help you - International perspectives on depression for people living with depression and their families. USA: World Federation for Mental Health. https://www.who.int/news-room/fact-sheets/detail/depression.
[31] Huberty, T. (2010). Depression: Supporting Students At School. Helping Children at Home and School III: Handouts for Families and Educators, 1–3. https://www.aap.org/en/patient-care/school-health/mental-health-in-schools/supporting-students-with-depression-in-school/.
[32] Bahrin, F. K. (2018). Pembentukan Dan Keberkesanan Modul Dalam Perubahan Pengetahuan, Persepsi Dan Tingkah Laku Pelajar Sekolah Menengah Terhadap HIV/AIDS di Pulau Pinang. Tesis Doktor Falsafah. Universiti Sains Malaysia: Penang. 232 pp. http://eprints.usm.my/43987/.
[33] Gani, F. A. (2019). Gejala Kemurungan : Kesedihan Biasa Atau Penyakit ? Kolumnis Awani Malaysia. https://www.astroawani.com/berita-malaysia/kolumnis-kelesuan-pandemik-impak-psikologi-akibat-pandemik-yang-berpanjangan-305577.
[34] Jalil, S. J. A. (2017). Pengaruh Program Keagamaan Dan Sokongan Sosial Terhadap Konsep Kendiri, Kebimbangan Dan Kemurungan : Kajian
Dalam Kalangan Banduan Wanita Di Malaysia. PhD Tesis. Universiti Malaya: Kuala Lumpur. 307 pp. http://studentsrepo.um.edu.my/7232/.[35] Gurung, R. A. R. (2006). Health Psychology : A Cultural Approach. (3rd Edition). San Francisco: Wadsworth. https://link.springer.com/article/10.1007/s10926-009-9222-z.
[36] Singh, P. S. J. (2015). Strategi Daya Tindak Ahli Keluarga Pengguna Dadah di Pulau Pinang. PhD Tesis. Universiti Sains Malaysia: Pulau Pinang. 454 pp. http://eprints.usm.my/31492/.
[37] Asalal, N., Zakaria, E., & Wahab, H. A. (2012). Intervensi Kerja Sosial Sekolah Dalam Menangani Masalah Sosial Pelajar. Jurnal Pendidikan Malaysia, 38(1), 42-51. http://journalarticle.ukm.my/7994/.
Viewed PDF 3199 44 -
Factors Affecting Dietary Intake and Physical Activities of Primary Health Care Workers in Nasarawa State NigeriaAuthor: Iliyasu Tunga SalihuDOI: 10.21522/TIJPH.2013.11.04.Art023
Factors Affecting Dietary Intake and Physical Activities of Primary Health Care Workers in Nasarawa State Nigeria
Abstract:
This study adopted a cross-sectional study design and deployed a quantitative methodology to assess the factors affecting dietary intake and physical activities in Nasarawa state. The questionnaire was adapted as an instrument for data collection. 400 respondents were sampled through a multistage sampling technique and 300 were interviewed with the aid of the epi-info mobile data collection tool. Data from the field survey were presented in frequency and simple percentages informed by tables and charts. The study reveals that Location and Level of income are some of the basic factors affecting dietary intake and physical exercise among Primary Health Care workers in Nasarawa state however, it was also observed that income and location do not necessarily affect dietary intake and physical exercise all the time, but motivation could also play a role most especially in maintaining good physical activity. The study also reveals that PHC staff in Nasarawa state may be aware of their daily exercise and diet needs theoretically but in practice, they don’t “practice what they preach”. It was concluded that Primary health care workers in Nasarawa state maintain a poor level of diet and physical activities, dietary intake and physical activities affect the performance of PHC staff, and PHC workers don’t practice and maintain good diet and physical activity habits, there is a need for promotion of health education activities related to diet and physical activities at PHC level across the state to inspire and motivate PHC staff to take up healthy diet and exercise habit.
Keywords: Affect, Dietary, Exercise, Habit, Healthy, Intake, Physical, study, Planned, Performance.Factors Affecting Dietary Intake and Physical Activities of Primary Health Care Workers in Nasarawa State Nigeria
References:
[1] World Health Organization (WHO), 2019, “Healthy diet,” pp. 20, https://.who.int/iris/bitstream/handle/10665/325828/EMROPUB-2019-en-23536.pdf/
[2] C. D. M. Cunha, P. R. F. Costa, L. P. M. De Oliveira, V. A. D. O. Queiroz, J. C. D. Pitangueira, and A. M. Oliveira, “Dietary patterns and cardiometabolic risk factors among adolescents: Systematic review and meta-analysis,” British Journal of Nutrition, vol. 119, no. 8. Cambridge University Press, pp. 859–879, Apr. 28, 2018. doi: 10.1017/S0007114518000533.
[3] B. M. Margetts, P. Little, and D. Warm, “Interaction between physical activity and diet: Implications for blood pressure management in primary care,” Public Health Nutr, vol. 2, no. 3 A, pp. 377–382, 1999, doi: 10.1017/S1368980099000518.
[4] Institute for Health Metric and Evaluation (IHME), 2017 “The Global Burden of diseases that are diet and lifestyle-related”, University of Washington. Healthdata.org.
[5] C. R. Nigg and K. S. Geller, “Theoretical Approaches to Physical Activity Intervention,” The Oxford Handbook of Exercise Psychology, no. May 2012, doi 10.1093/oxfordhb/9780195394313.013.0014.
[6] World Health Organization (WHO), “Global status report on physical activity” 2022, https://apps.who.int/iris/rest/bitstreams/1489640/retrieve.
[7] M. Blake, “Differences in food intake, nutrition knowledge, and fitness assessment measurements in high school students who have completed the Nutricise 4 life program and students who have not,” 2009.
[8] “Healthy diet.” [Online]. Available: http://www.who.int/mediacentre/factsheets/fs394/en/.
[9] M. A. Elmagd, “Benefits, need for and importance of daily exercise,” ~ 22 ~ International Journal of Physical Education, Sports, and Health, vol. 3, no. 5, pp. 22–27, 2016.
[10] Sustainable Development Goals I IISD Perspectives on the 2030 Agenda for Sustainable Development Sustainable Development Goals,” 2016. [Online]. Available: www.iisd.org.
[11] I. O. Ayenigbara, “The contributions of physical activity and fitness for the optimal health and wellness of the elderly people,” Journal of Gerontology and Geriatrics, vol. 68, no. 1, pp. 40–46, 2020, doi: 10.36150/2499-6564-351.
[12] C. E. Abadía-Barrero and M. Bugbee, “Primary Health Care for Universal Health Coverage? Contributions for a Critical Anthropological Agenda,” Medical Anthropology: Cross-Cultural Studies in Health and Illness, vol. 38, no. 5. Taylor and Francis Inc., pp. 427–435, Jul. 04, 2019. doi: 10.1080/01459740.2019.1620744.
[13] G. N. Hailu, H. B. Gebru, and D. Siyoum Belay, “Assessment of Healthy Diet and Physical Activity Among Students of Mekelle University, Northern Ethiopia: A Cross-Sectional Study,” Nutr Diet Suppl, vol. Volume 13, pp. 103–112, 2021, doi: 10.2147/nds.s287278.
[14] D. Pandit-Agrawal, A. Khadilkar, and S. Chiplonkar, “Knowledge of nutrition and physical activity in apparently healthy Indian adults,” vol. 21, no. 9, pp. 1743–1752, 2018, doi: 10.1017/S1368980017004268.
[15] N. Walliman, “RESEARCH METHODS”: The Basics, 2nd Edition, 2017, Routledge, London, pp. 246, https://doi,org/10.4324/9781315529011.
[16] “Primary health care Draft operational framework Primary health care: transforming vision into action.” [Online]. Available: https://apps.who.int/iris/handle/10665/328065.
[17] E. L. Deci and R. M. Ryan, “Self-Determination Theory: A Macrotheory of Human Motivation, Development, and Health,” vol. 49, no. 3, pp. 182–185, 2008, doi: 10.1037/a0012801.
[18] Ajzen, 1991, “Theory-of-Planned-Behaviour”, Centre for people building, pp 50, 179-211, http://ascnhighered.org/ACSN/change-theries/collection/planned-behaviour.html.
[19] T. H. Id, “Dietary intake and its associated factors among in-school adolescents in Ghana,” pp. 1–13, 2022, doi: 10.1371/journal.pone.0268319.
[20] T. Hormenu, “Dietary intake and its associated factors among in-school adolescents in Ghana,” PLoS One, vol. 17, no. 5 May, May 2022, doi: 10.1371/journal.pone.0268319.
[21] N. Ntoumanis, C. Thørgersen-Ntoumani, E. Quested, and N. Chatzisarantis, “Theoretical
Approaches to Physical Activity Promotion,” in Oxford Research Encyclopedia of Psychology, Oxford University Press, 2018. doi: 10.1093/acrefore/9780190236557.013.212.Viewed PDF 626 18 -
An Assessment of Knowledge of Health Workers in Hospitals of Southern Province of Zambia, towards Marketing of Breastmilk Substitutes RegulationsAuthor: Chipo Muleya Siafwa SikazweDOI: 10.21522/TIJPH.2013.11.04.Art024
An Assessment of Knowledge of Health Workers in Hospitals of Southern Province of Zambia, towards Marketing of Breastmilk Substitutes Regulations
Abstract:
Background: Optimal breastfeeding practices have been undermined by unregulated marketing of breastmilk substitutes worldwide, resulting in about 820, 000 preventable deaths per year among children under five years globally. The International Code (thereafter called the Code) of Marketing breastmilk substitutes was developed by the World Health Organization, the United Nations Children's Emergency Fund, and stakeholders to protect, promote and support breastfeeding. Member states are expected to domesticate the Code. Zambia enacted Statutory Instrument No. 48 of 2006, Regulations on marketing of breastmilk substitutes. Successful implementation calls for a good level of knowledge among health workers. However, we found no study, in Zambia on marketing of breastmilk substitutes Regulations. Objective: To assess the level of knowledge of health workers on Zambia’s Regulations on marketing breastmilk substitutes. Study design and methods: A mixed-method cross-sectional study. Data was collected online and in person. Probability proportional to size calculation yielded an estimated sample size of 384. A sample size of 410 after adjusting upwards assumed non-response rate, 401 participants responded. Quantitative data were analyzed using the Social Statistical Package for Social Sciences. Knowledge results were described by frequencies and percentages. Tests were conducted using univariable linear and multivariable regression analysis. A p-value of <0.05 was considered statistically significant. Thematic analysis was used for qualitative data analysis. Results: The mean overall level of good knowledge of health workers was 0.339 or 34% [SE: 0.0221; 95%CI: (0.2959, 0.3828)]. Conclusion: The level of knowledge among health workers in hospitals of Southern Province, Zambia was poor.
Keywords: Breastmilk substitute Regulations, Health worker, Knowledge.An Assessment of Knowledge of Health Workers in Hospitals of Southern Province of Zambia, towards Marketing of Breastmilk Substitutes Regulations
References:
[1] Piwoz and Huffman (2015). The Impact of Marketing of Breast-Milk Substitutes on WHO-Recommended Breastfeeding Practices. Food Nutr. Bull. 36, 373–386. https://journals.sagepub.com/doi/pdf/10.1177/0379572115602174.
[2] Hernandez-Cordero,S., Lozada‐Tequeanes, A. L., Shamah-Levy, T., Lutter,C., González de Cosio, T., Saturno-Hernández, P., dommarco, J. R., Grummewr-Strawn,L. (2018).Violations of the International Code of Marketing of Breast-milk Substitutes in Mexico. Matern. Child Nutr., 15(1), Article e12682 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7199041/pdf/MCN-15-e12682.pdf.
[3] WHO and UNICEF. (2022). How the Marketing of Formula Milk influences our decisions on Infant Feeding. https://www.unicef.org/media/115916/file/Multicountry%20study%20examining%20the%20impact%20of%20BMS%20marketing%20on%20infant%20feeding%20decisions%20and%20practices,%20UNICEF,%20WHO%202022.pdf.
[4] Victoria, C.G., Bahl, R., Barros, A.J.D., França, G.V.A., Horton, S. (2016). Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet. 387(10017):475–90. https://doi.org/10.1016/S0140-6736(15)01024-7.
[5] WHO. (1981). International Code of Marketing Breastmilk Substitutes. https://breastfeedingcanada.ca/wp-content/uploads/2020/03/TheCode-En.pdf.
[6] WHO (2020). The International Code of Marketing of breast-milk substitutes-Frequently asked questions https://www.who.int/publications/i/item/9789240005990.
[7] Brady, J.P. (2012). Marketing breast milk substitutes: problems and perils throughout the world. Arch Dis Child (97) :529–532. https://adc.bmj.com/content/archdischild/97/6/529.full.pdf.
[8] Becker, G., Paul, Z., Constance, C., Jennifer, C. Allison, B., Eva, P., Janice. D and Roger, M. (2021). Global evidence of persistent violations of the International Code of Marketing of Breastmilk Substitutes: A systematic scoping review. Matern Child Nutr. 18(S3):e13335. https://onlinelibrary.wiley.com/doi/epdf/10.1111/mcn.13335.
[9] Salasibew, M., Ayyaz, K., Brian, F., Paul, G. (2008). Awareness and reported violations of the WHO International Code and Pakistan's national breastfeeding legislation; A descriptive crosssectional survey. https://pubmed.ncbi.nlm.nih.gov/8800076/.
[10] Hidayana, I., Februhartantly, J., & Parady, V. (2017). Violations of the International Code of Marketing of Breastmilk Substitutes: Indonesia context. Public Health Nutrition 20(1), 165-173. https://pubmed.ncbi.nlm.nih.gov/27323845/.
[11] Velasco. A. C. C. F., Maria. I. C. O and Cristiano. S. B. (2022). Harassment of health professionals by the infant food industry at scientific events. https://www.scielosp.org/article/rsp/2022.v56/70/https://www.scielosp.org/article/rsp/2022.v56/70/.
[12] Čatipović, M., Zrink, P., Drita, P., Paula, C., and Josip, G. (2022). Behaviour, attitudes, and knowledge of healthcare workers on Breastfeeding. Children (9): 1173. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9406792/pdf/children-09-01173.pdf.
[13] Doherty, T., Catherine, J.P., Silondile, L., Lyn, H., Gillian. K., Sithembile, D., Gilbert. T., and Chistiane, H. (2022). They push their products through me: Health Professionals’ perspectives on and exposure to marketing of commercial milk formula in Cape Town and Johannesburg, South Africa – a qualitative study. https://bmjopen.bmj.com/content/bmjopen/12/4/e055872.full.pdf.
[14] Champeny, M.,Pereira, C., Sweet, L., Khin, M.,Coly, N.,Gueye,E., … Huffman,S. (2016). Point-of-sale Promotion of Breastmilk Substitutes and Commercially Produced Complementary Foods in Cambodia, Nepal. Senegal and Tanzania: Maternal & Child Nutrition. Matern Child Nutri. 12(2): 126–139. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5071702/.
[15] Aguayo, V.M., Jay, S. R., Souleyman., and Ander, N.O. (2003). Monitoring compliance with the International Code of Marketing of Breastmilk Substitutes in West Africa: Multisite cross-sectional survey in Togo and Burkina Faso. BMJ 236 (7381):127. doi: 10.1136/bmj.326.7381.127 i: 10.1136/bmj.326.7381.127.
[16] Emerson, J., Kouassi, F., Kouamé,r. O., Damey, F. N., Cissel, A.S., Tharaney, M. ( (2021). Mothers' and Health workers' exposure to breastmilk substitutes promotions in Abidjan, Côte d'Ivoire. Matern. Child Nutr., 7, Article e13230. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8476441/pdf/MCN-17-e13230.pdf.
[17] Government of Zambia. (2006). Statutory Instrument No. 48 of 2006. The Food and Drug Act (Laws, Volume 17, Cap 303) Food and Drugs (Marketing of Breast Milk Substitutes) Regulations, 2006. http://extwprlegs1.fao.org/docs/pdf/zam66935.pdf.
[18] Government of Zambia. (2010). Monitoring Compliance and Enforcement of Breastmilk Substitutes Regulations: A Manual for Environmental Health Officers; A Guide for Administration of Food and Drugs (Marketing of Breastmilk Substitutes') Regulations, 2006 (Statutory 48 of 2006). https://www.researchgate.net/publication/315669425_Marketing_of_breast-milk_substitutes_in_Zambia_Evaluation_of_compliance_to_the_international_regulatory_code/link/5bbd0c14299bf1049b78623e/download.
[19] Funduluka,P., Bosomprah, S., Chilengi, R., Mugode, R.H., Bwembya,P. A., Mudenda, B. (2017). Marketing of breast-milk substitutes in Zambia: evaluation of compliance to the international regulatory code, Journal of Public Health, 40, (1), e1–e7, https://doi.org/10.1093/pubmed/fdx023.
[20] Nyaboke, C. (2021). Assessment of knowledge, attitude and practices on Kenya’s breast milk substitutes Act (2012) among nurses in Mbagathi and Pumwani Hospitals, Kenya http://repository.kemu.ac.ke/bitstream/handle/123456789/1265/Clement%20thesis%20Clearance%20%281%29.pdf?sequence=1&isAllowed=y.Viewed PDF 667 17 -
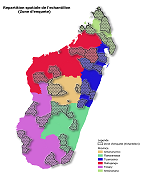 Bridging the Knowledge Gap: Discerning the Association between Adequately Iodized Salt Coverage and Household Knowledge, Attitudes and Practices in MadagascarAuthor: Smaila GnegneDOI: 10.21522/TIJPH.2013.11.04.Art025
Bridging the Knowledge Gap: Discerning the Association between Adequately Iodized Salt Coverage and Household Knowledge, Attitudes and Practices in MadagascarAuthor: Smaila GnegneDOI: 10.21522/TIJPH.2013.11.04.Art025Bridging the Knowledge Gap: Discerning the Association between Adequately Iodized Salt Coverage and Household Knowledge, Attitudes and Practices in Madagascar
Bridging the Knowledge Gap: Discerning the Association between Adequately Iodized Salt Coverage and Household Knowledge, Attitudes and Practices in Madagascar
References:
[1] World Health Organization, Assessment of iodine deficiency disorders and monitoring their elimination: a guide for programme managers, 3rd ed éd., WHO Press, 2007.
[2] United Nations Children's Fund, Monitoring the situation of children and women, [En ligne]. Available: https://data.unicef.org/topic/nutrition/iodine/ [Accès le 12 09 2021].
[3] R. V. Randremanana, A. Bast, R. LP, P. Piola, D. Rakotonirina, J. O. Razafinimanana, M. H. Ramangakoto, L. Andriantsarafara, H. Randriamasiarijaona, A. Tucker‐Brown, A. Harimanana and S. Namana, “First national iodine survey in Madagascar demonstrates iodine deficiency associated with low household coverage of iodized salt,” Maternal & Child Nutrition, vol. 15, no. 2, p. 15, 2018.
[4] L. Locatelli-Rossi, Problemes et solutions pour ameliorer le programme d'iodation su sel à madagascar,2017.
[5] Department of Economic and Social Affairs of the United Nations Secretariat is, Designing Household Survey Samples: Practical Guidelines, 2005.
[6] W. G. Cochran, Sampling techniques,Third Edition, John Willey & Sons, 1977.
[7] Y. F. Macías and P. Glasauer, “Guidelines for assessing nutrition-related knowledge, attitudes and practices,” Food and Agriculture Organization of the United Nations (FAO), 2014.
[8] H. Gerensea, A. Yohannse, B. Baymot, H. Atsbha, K. Nguse, L. Gebru and S. G/kel, “Knowledge, attitude and practice (KAP) towards iodized salt utilization in HaweltiKebelle, Axum, Tigray, Ethiopia,2015,” Edorium J Pathol 2016, vol. 2, pp. 1-8, 2015.
[9] N. Karmakar, A. Datta, K. Nag, S. S. Datta and S. Datta, “Knowledge, attitude, and practice regarding household consumption of iodized salt among rural women of Tripura, India: A mixed-methods study,” J Edu Health Promot, vol. 8, no. 1, p. 21, 2019.
[10] Demographics and Health Surveys (DHS) program, The DHS wealth index categorizes households into 5 wealth quintiles, allowing you to see how health differs between the poor and wealthy, 2016. [En ligne]. Available: https://dhsprogram.com/topics/wealth-index/index.cfm [Accès le 12 07 2021].
[11] V. Mannar, M. G, J. T. Dunn et W. H. Organization, Salt iodization for elimination of iodine deficiency, p. 126, 1995.
[12] A. A. Alamneh, C. T. Leshargie, M. Desta, M. Y. Birhanu, M. A. Assemie, H. T. Denekew, Y. M. Alamneh et D. B. Ketema, Availability of adequately iodized salt at the household level in Ethiopia: A systematic review and meta-analysis, PloS one, vol. 16, n° %12, 2021.
[13] P. L. Jooste, M. J. Weight et C. J. Lombard, Iodine concentration in household salt in South Africa, vol. 79, Bulletin of the World Health Organization, 2001, p. 534–540.
[14] P. Sai Deepika, B. Thirumala Rao, A. Vamsi, K. Valleswary et M. Chandra Sekhar, A cross sectional study on proper use of iodized salt in communities of rural areas and its relevant factors in Prakasam district, Andhra Pradesh, India, International Journal Of Community Medicine And Public Health, vol. 6, n° %13, pp. 1083-1090, 2019.
[15] G. Ftwi, B. Mengistie, M. Abdo et K. T. Roba, Household Salt Iodine Level and Associated Factors in Dire Dawa City Administration, East African Journal of Health and Biomedical Sciences, vol. 2, n° 12, pp. 35-44, 2018.
[16] M. Andrien, «Social communication in nutrition: a methodology for intervention, 1994.
[17] G. de Landsheere, “Assessment of nutrition-related knowledge, skills and attitudes,” Evaluation of nutrition education in third world communities, pp. 58-66, 1983.
[18] A. M. Senbeta, F. T. Mamo, B. B. Desalegn, A. K. Daba et M. T. Moral, Knowledge and practices of iodized salt utilization, health consequences, and iodine concentration on dietary salts at retailer and households in Jigjiga town, Somali, Ethiopia, Cogent Food & Agriculture, vol. 7, n° %11, 2021.
[19] Asfaw, T. Belachew et T. Gari, Effect of nutrition education on iodine deficiency disorders and iodized salt intake in southwest Ethiopian women: a cluster randomized controlled trial, BMC Women's Health, vol. 20, n° %11, pp. 1-11, 2020.
[20] Y. Yeshaw, A. M. Liyew, A. B. Teshale, T. S. Alamneh, M. G. Worku, Z. T. Tessema, A. Z. Alem et G. A. Tesema, Individual and community level factors associated with use of iodized salt in sub-
Saharan Africa: A multilevel analysis of demographic health surveys, PLoS ONE, vol. 16, n° %15, 2021.[21] World Health Organization, Assessment of iodine deficiency disorders and monitoring their elimination: a guide for programme managers, 2nd ed éd., WHO press, 2001.
[22] Médecins du Monde, Data collection>> quantitative methodes [sic]. The KAP, Médecins du Monde, Paris, 2011.
[23] A. H. Mohammad, M. R. Alam, S. Ghosh, T. Rahman, S. Reza, and S. Mamun, “Impact of knowledge, attitude, and practice on iodized salt consumption at the household level in selected coastal regions of Bangladesh,” Heliyon, vol. 7, no. 4, 2021.
Viewed PDF 679 30 -
Predictors of Chronic Debilitating Conditions Among Refugees Resettled in the United StatesAuthor: Edson ChipaloDOI: 10.21522/TIJPH.2013.11.04.Art026
Predictors of Chronic Debilitating Conditions Among Refugees Resettled in the United States
Abstract:
Refugees who have resettled in the United States encounter numerous challenges, including poor health conditions. However, knowledge of risk factors contributing to chronic debilitating conditions among refugees is scarce. Therefore, this study examined the prevalence and potential factors associated with chronic debilitating conditions within the U.S. refugee population. This study utilized secondary data from the 2019 Annual Survey of Refugees (ASR) involving 1007 refugees aged 16 years or older resettled in the U.S. between 2014 and 2018. The prevalence estimates were obtained using chi-square tests, and multiple logistic regression was used to determine the significant association between predictor variables and chronic debilitating conditions for refugees in the United States. About 25.5% of the refugees reported having chronic debilitating conditions. Regression results showed that being an older refugee and having adjusted immigration status to become a permanent resident was associated with higher odds of reporting chronic debilitating conditions. However, refugees who were currently working, married, and with good English language proficiency were associated with a lower likelihood of reporting chronic debilitating conditions. Gender and education levels of refugees were not significantly associated with chronic debilitating conditions after covariates adjustments. Interventions should focus on increasing access to education, employment opportunities to enhance health literacy, and financial resources to access healthcare crucial for mitigating chronic debilitating conditions. In addition, addressing the language barriers through language and interpretation services in clinical settings can also improve healthcare access, thus reducing the risk of chronic debilitating conditions among refugees resettled in the United States.
Keywords: Chronic debilitating conditions, English proficiency, Immigration, Refugees, United States.Predictors of Chronic Debilitating Conditions Among Refugees Resettled in the United States
References:
[1] Kennedy, J.D., et al., Refugee-like migrants have similar health needs to refugees: a New Zealand post-settlement cohort study. BJGP open, 2020. 4(1).
[2] Sagaltici, E., G. Alpak, and A. Altindag, Traumatic life events and severity of posttraumatic stress disorder among Syrian refugees residing in a camp in Turkey. Journal of loss and trauma, 2020. 25(1): p. 47-60.
[3] Chipalo, E., Exposure to Violence and Other Characteristics Associated with Posttraumatic Stress Disorder Among Students in Nyarugusu Refugee Camp, Tanzania. 2023, The University of Alabama: United States -- Alabama. p. 230.
[4] Lamb, C.F. and M. Smith, Problems refugees face when accessing health services. New South Wales public health bulletin, 2002. 13(7): p. 161-163.
[5] Fazel, M., J. Wheeler, and J. Danesh, Prevalence of serious mental disorder in 7000 refugees resettled in western countries: a systematic review. The lancet, 2005. 365(9467): p. 1309-1314.
[6] Kiss, V., et al., Building knowledge about health services utilization by refugees. Journal of Immigrant and Minority Health, 2013. 15: p. 57-67.
[7] Pavli, A. and H. Maltezou, Health problems of newly arrived migrants and refugees in Europe. Journal of travel medicine, 2017. 24(4): p. tax016.
[8] Mirza, M., et al., Barriers to healthcare access among refugees with disabilities and chronic health conditions resettled in the US Midwest. Journal of immigrant and minority health, 2014. 16: p. 733-742.
[9] Broemeling, A.-M., D.E. Watson, and F. Prebtani, Population patterns of chronic health conditions, co-morbidity, and healthcare use in Canada: implications for policy and practice. Healthcare quarterly (Toronto, Ont.), 2008. 11(3): p. 70-76.
[10] Chipalo, E., Z. Suntai, and S. Mwima, Factors Associated with Receiving Supplemental Nutrition Assistance Program (SNAP) Among Newly Resettled Refugees in the United States. J. Soc. & Soc. Welfare, 2022. 49: p. 135.
[11] Yakushko, O., et al., Career development concerns of recent immigrants and refugees. Journal of Career Development, 2008. 34(4): p. 362-396.
[12] Pyke, J., et al., Refugees in the Labour Market: Looking for cost-effective models of assistance. 2004.
[13] Kemp, C., Health services for refugees in countries of second asylum. International Nursing Review, 1993. 40(1): p. 21-24.
[14] Portes, A., D. Kyle, and W.W. Eaton, Mental illness and help-seeking behavior among Mariel Cuban and Haitian refugees in South Florida. Journal of health and social behavior, 1992: p. 283-298.
[15] Straiton, M.L. and S. Myhre, learning to navigate the healthcare system in a new country: a qualitative study. Scandinavian journal of primary health care, 2017. 35(4): p. 352-359.
[16] Divkolaye, N.S.H. and F.M. Burkle Jr, The enduring health challenges of Afghan immigrants and refugees in Iran: a systematic review. PLoS currents, 2011. 9.
[17] Baumann, K.J. and T. Adera, Sociodemographic Characteristics, and Inadequate Usual Sources of Healthcare in a National Sample of US Refugees. International Journal of Environmental Research and Public Health, 2022. 19(12): p. 7234.
[18] Urban Institute. Annual survey of refugees. Ann Arbor, MI: inter-university consortium for political and social researc. 2018 [cited 2020 September 2020]; Available from: https://doi.org/10.3886/E104642V4.
[19] Refugee Processing Center. Worldwide refugee admissions processing system. 2020 [cited 2021 December 29th]; Available from: www.wrapsnet.org
[20] Zaimi, N.H.A. and D.I. Supaat, Flood disasters in Malaysia: Examining the Impact on Older people’s Vulnerability and Right, 2023.
[21] Rosenthal, T., R.M. Touyz, and S. Oparil, Migrating populations and health: risk factors for cardiovascular disease and metabolic syndrome. Current Hypertension Reports, 2022. 24(9): p. 325-340.
[22] Krafft, C., et al. Syrian refugees in Jordan: Demographics, livelihoods, education, and health. in Economic Research Forum Working Paper Series. 2018. RAND Corporation Santa Monica, CA, USA.
[23] Sharma, S.V., et al., Peer reviewed: Social determinants of health–related needs during COVID-19 among low-income households with children. Preventing chronic disease, 2020. 17.
[24] Seiler, A., C.P. Fagundes, and L.M. Christian, The impact of everyday stressors on the immune system and health. Stress challenges and immunity in space: From mechanisms to monitoring and preventive strategies, 2020: p. 71-92.
[25] Lee, J.O., et al., young adult unemployment and later depression and anxiety: does childhood neighborhood matter? Journal of youth and adolescence, 2019. 48: p. 30-42.
[26] Peacock, S., et al., Older adult spouses with multiple chronic conditions: challenges, rewards, and coping strategies. Canadian Journal on Aging/La Revue canadienne du vieillissement, 2017. 36(2): p. 209-222.
[27] Chang, C.D., Social determinants of health and health disparities among immigrants and their children. Current problems in pediatric and adolescent health care, 2019. 49(1): p. 23-30.
[28] Hawkins, M.M., et al., Promoting the health of refugee women: a scoping literature review incorporating the social ecological model. International journal for equity in health, 2021. 20: p. 1-10.
[29] Gagnon, M., et al., Immigration Status as the Foundational Determinant of Health for People Without Status in Canada: A Scoping Review. Journal of Immigrant and Minority Health, 2021: p. 1-16.
[30] Banken, J.A., Drug abuse trends among youth in the United States. Annals of the New York Academy of Sciences, 2004. 1025(1): p. 465-471.
[31] Chou, K.-L., Psychological distress in migrants in Australia over 50 years old: A longitudinal investigation. Journal of affective disorders, 2007. 98(1-2): p. 99-108.
Viewed PDF 612 19 -
Exploring the Mental Health of Minors in Poor Areas: A Case Study of Anhui Province, ChinaAuthor: Farhana Kamarul BahrinDOI: 10.21522/TIJPH.2013.11.04.Art027
Exploring the Mental Health of Minors in Poor Areas: A Case Study of Anhui Province, China
Abstract:
As the global economy progresses and people's living standards improve, there is a growing need to redefine the notion of "health," expanding its scope beyond physical well-being to include psychological health. Given that minors bear the responsibility of fostering social progress as the hope for the future society, their mental health becomes exceptionally crucial. This research aims to investigate the mental health status of minors in poor areas of Anhui Province, assessing the existence of issues and probing into their underlying causes. The study is structured into two main segments. Initially, it delves into the essence of mental health education for minors, the current state of mental health education globally and domestically and underscores the significance of the research. Subsequently, by scrutinizing the mental health scenario of minors through case studies, the analysis reveals that psychological challenges among minors predominantly manifest in areas such as personality, learning, and interpersonal communication. Applying the social system theory, the researcher identifies several factors contributing to these psychological issues, including governmental neglect, economic underdevelopment, outdated educational ideologies, insufficient family guidance, and inadequate infrastructure. Approached from the standpoint of social workers, addressing these concerns is seen as instrumental in fostering the wholesome development of minors.
Keywords: Mental Health, Minors, Community Health, Social Work, Well-being.Exploring the Mental Health of Minors in Poor Areas: A Case Study of Anhui Province, China
References:
[1] Li,Z.Y. (2022) Revitalizing rural mental health education should be based on national strategies, policies and laws. Human Education (An Edition), (05), 29-30.
[2] Wan, G.W.&Xu, Y.C. (2022). Violence experience of rural children in China and its impact on mental health from a gender perspective Social Construction (05), 66-82.
[3] Lina,Y. (2020). On how to carry out children's mental health education in the new period. Paper presented at 2020 2nd International Education Technology and Research Conference Madrid, Spain.
[4] Zhang, Y. (2022). Strategies to strengthen mental health education for left-behind children in rural areas. Parents, (30), 7-9.
[5] Han, Y.&Liu,B. (2020). The relationship between personality, mental health and learning ability of school-age children in poor areas, Mental Health Education in Primary and Secondary Schools, (31), 16-20.
[6] Deng, Z.Z.&Liu,Z. (2023). Research progress on the relationship between childhood obesity and mental health. China Maternal and Child Health Research, (01), 21-25.
[7] Li,Y. (2020). Research on psychological barriers and counseling strategies of students in poor areas of Gansu in the new era. Academic Weekly, (15), 189-190. doi: 10.16657/j.cnki.issn1673-9132.2020.15.094.
[8] Pan,F.L. & Fang,H.Q. (2022). Psychological safety of minors: current situation, characteristics, and maintenance. Journal of Changzhou Institute of Technology (Social Science Edition), (02), 114-119.
[9] Yumin, L. (2021). On the Professional Construction of Children's Mental Health Education. Advances in Vocational and Technical Education (2021) 3: 199-203. DOI: http://dx.doi.org/10.23977/avte.2021.030240.
[10] Sun,L. (2022). The generation and countermeasures of the phenomenon of "psychological loneliness" in rural children. Yunnan Education (Vision comprehensive edition), (05), 12-14.
[11] Zhang,Y. (2022). Analysis on the Mental Health Education Countermeasures of Rural Left-behind Children under the Background of Rural Revitalization. Basic Education Reference, (04), 51-52.
[12] Bian,J Lin,R.R.& Shi,Y.H. (2022) Measurement and analysis of rural residents' family education affordability -- a case study based on a deep poverty area in the West. Modern Educational Science, (01), 1-7+22 doi: 10.13980/j.cnki. xdjykx. 2022.01.001.
[13] Du,H.G. & Chen,H.F. (2017). Study on psychological anxiety of low age boarding children in poor areas. Education modernization, (39), 224-225. Doi: 10.16541/j.cnki.2095-8420.2017.39.091.
[14] Gong,L.X. (2020). Psychological Poverty Alleviation: A New Way to Stimulate the Endogenous Motivation of the Poor Tianzhong. Academic Journal, (02), 28-36. doi: 10.14058/j.cnki.tzxk.2020.02.004.
[15] Zheng, R.Y.& Zhang, S.P. (2021). A comparative analysis of the application of advantage perspective theory and social learning theory in the mental health of rural left behind children. Economic Research Guide, (35), 64-66.
[16] Hu,J. (2022). Investigation on the mental health of rural primary school students and analysis on the existing problems and countermeasures. Exam Weekly, (38), 1-6.
[17] Shao,Y.H. (2022). The implementation dilemma and solution of mental health education class in rural primary schools. Basic Education Research, (13), 80-83.
[18] Tan, X.L.&Li,C.N. (2021) Three working paths to strengthen mental health education in rural schools. Educators, (35), 38-39.
[19] Fang,M.K. (2018). Reasons and Countermeasures for Difficulties in Implementing Mental Health Education for Rural School Pupils. Examination Weekly, (80), 16.
[20] Yang,L.Z. (2021) A Study on the Loss of Rural Teachers in Guangxi and Its Countermeasures from the Perspective of Social Exchange Theory (Master's Thesis, Nanning Normal University).
[21] He, H., Lin, Z., Peng, C.C., Guo, S.R.& Liang,G.Y. (2021).Exploring the construction of a system of caring for the mental health of left behind children in the context of rural revitalization -- taking the "companion angel" project as an example. Heilongjiang Science, (20), 138-143.
[22] Yan, Y.D.&Hao,H.J. (2021). Strategic research on mental health education in rural small-scale schools under the background of core literacy. New Curriculum, (44), 32-33.
[23] Cao,X. (2018). Mental health education curriculum from the perspective of three psychological theories. Qinghai Education, (02), 49-50.
[24] Jiang,Y.L.(2019).Analysis of the current situation and existing problems of mental health education in rural schools [J]. Academic weekly, (01): 101-102).
[25] Zhao,X.Z&Wang,J.B. (2021). The influence of school mental health education combined with family intervention on the mental health of middle school students. Chinese School Health, (03), 408-411. doi: 10.16835/j.cnki.1000-9817.2021.03.022.
[26] Liang, C.&Chang,R.X. (2020). Problems and improvement strategies of mental health education in primary and secondary schools in China. Educational Science, (03), 46-51.
[27] Su,Y.T. (2020). On the Mental Health Education of Rural Left-behind Children. Literature Education (under), (01), 162-163. doi:10.16692/j.cnki.wxjyx. 2020.01.078.
[28] Fu, J.H. (2023). Discussion on the relationship between children's mental health and behavior problems and family education. Test Questions and Research, (02), 133-135.
[29] Benito León-del-Barco. (2018). Impact of the Familiar Environment in 11–14-Year-Old Minors’ Mental Health. International Journal of Environmental Research and Public Health, 15(7), pp. 1314-1314.
[30] Gao,Y. (2020). Analysis on the Mistakes and Solutions of Family Education for High School Students in Poverty stricken Areas. Examination Weekly, (60), 5-6.
[31] Yang, C.&Liu,J.P. (2017). The impact of family atmosphere on the mental health of left behind children in rural areas: the separation of "raising" and "educating". Psychological Exploration, (04), 364-368.
[32] Zhao,D.L. (2020). Problems and solving strategies of mental health education for left-behind children in Rural Areas. Teaching educating people, (11), 18-19.
[33] Zhang,H.M. (2022). Research on school-based cultivation education system for junior high school students. Jiangxi Education, (24), 22-23
[34] Sun,Z. (2019). On the strategies of mental health and family education for left behind children. Middle school curriculum guidance (teacher education), (11), 111.
[35] Marican, S. (2006). Penyelidikan sains sosial pendekatan pragmatik. Selangor: Edusystem Sdn. Bhd.
[36] Guo, H.&Hu,Y.W. (2022). The impact of family environment and peer groups on the social behavior of rural left behind children - based on CEPS data analysis. Rural Essay, (05), 91-98.
[37] Liu,Y.J. (2012). Psychological health education of college students in the perspective of Freud's personality theory. Century Bridge (07), 119-120. doi: 10.16654/j.cnki.cn23-1464/d.2012.07.017.
[38] Zheng, R.Y.&Zhang, S.P. (2021). A comparative analysis of the application of advantage perspective theory and social learning theory in the mental health of rural left behind children. Economic Research Guide, (35), 64-66.
[39] Ai, T.T.& Song, M.Z. (2021). A study of children's personality structure from the perspective of psychoanalytic theory: a qualitative text analysis based on NVivo. Education Observation, (40), 26-28+32. doi: 10.16070/j.cnki.cn45-1388/g4s.2021.40.007.
[40] Cao,X. (2018). Mental health education curriculum from the perspective of three psychological theories. Qinghai Education, (02), 49-50.
Viewed PDF 648 19 -
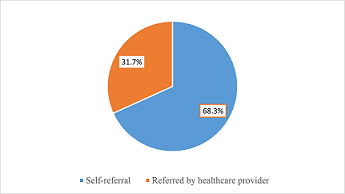 Self-Referral and Its Predictors Among Patients Accessing Healthcare Services in A Tertiary Hospital, In Calabar, Cross River State, NigeriaAuthor: Iwasam Elemi AgborDOI: 10.21522/TIJPH.2013.11.04.Art028
Self-Referral and Its Predictors Among Patients Accessing Healthcare Services in A Tertiary Hospital, In Calabar, Cross River State, NigeriaAuthor: Iwasam Elemi AgborDOI: 10.21522/TIJPH.2013.11.04.Art028Self-Referral and Its Predictors Among Patients Accessing Healthcare Services in A Tertiary Hospital, In Calabar, Cross River State, Nigeria
Abstract:
Classified as self and non-self-referrals, the ideal situation is that patients begin from lower levels of healthcare to higher levels. This improves the utilization of the primary care units, reduces unnecessary congestion of higher levels and makes for efficient healthcare delivery in general. This study aimed to assess the prevalence and predictors of self-referral among patients accessing healthcare in a tertiary hospital in Calabar, Nigeria. Ethical approval and informed consent were obtained. The study adopted quantitative data collection methods. This facility-based, cross-sectional study was carried out among 400 patients aged 18 years and above accessing care in the General Outpatient Clinic of the University of Calabar Teaching Hospital, Calabar in Cross River State. Overall, 191(47.8%) were males while 209(52.3%) were females. The mean age of study participants was 40.5±13.4 years, the most common age group was 31 to 40 years (28.2%). Prevalence of self-referral was 68.3%. Factors significantly associated with self-referral practices were sex (p<0.001), age group (p<0.001), marital status (p<0.001) and occupation (p=0.006). At multivariate regression analysis, females compared with males (OR: 5.299; 95% CI: 3.271 to 8.587), as well as those who were presently unmarried compared with those presently married (OR: 1.920; 95% CI: 1.052 to 3.505) were significantly more likely to practice self-referral. Self-referral practice is common and sex and marital status were identified as predictors. This is more so with unmarried females. Interventions to promote utilization and referral by healthcare providers through the prescribed channel is strongly recommended.
Keywords: Self- referral, Prevalence, Predictors, Healthcare, tertiary, Practice.Self-Referral and Its Predictors Among Patients Accessing Healthcare Services in A Tertiary Hospital, In Calabar, Cross River State, Nigeria
References:
[1] Carter MW, Robbins CL, Gavin L, Moskosky S (2018), Referral Practices Among U.S. Publicly Funded Health Centers That Offer Family Planning Services. J Womens Health (Larchmt), 27(8):994-1000. doi: 10.1089/jwh.2017.6487. Epub 2018 Jan 29. PMID: 29377754; PMCID: PMC6742435.
[2] WHO. Strategies to strengthen referral from primary care to secondary care in low- and middle-income countries. World Health Organization Regional Office for South-East; 2019. https://apps.who.int/iris/bitstream/handle/10665/325734/9789290227090.
[3] Federal Democratic Republic of Ethiopia Ministory of Health (2010) Guidline for implementation of a patient referral system. https://www.ncbi.nlm.nih.gov.
[4] Abdi WO, Salgedo WB (2015) Magnitude and determinants of selfreferral of patients at a general hospital Western Ethiopia. Sci J Clin Med 4(5):86–92. doi: 10.11648/j.sjcm.20150405.12.
[5] Sørbye IK, Vangen S, Oneko O, Sundby J, Bergsjø P (2011) Caesarean section among referred and self-referred birthing women: a cohort study from a tertiary hospital, northeastern Tanzania. BMC Pregnancy Childbirth. 2011 Jul 28; 11:55. doi: 10.1186/1471-2393-11-55. PMID: 21798016; PMCID: PMC3160415.
[6] Koce F, Randhawa G, Ochieng B (2019) Understanding healthcare self-referral in Nigeria from the service users’ perspective: a qualitative study of Niger state. BMC Health Serv Res, 19(1):209. doi: 10.1186/s12913-019-4046-9. PMID: 30940134; PMCID: PMC6444603.
[7] Pillay I, Mahomed OH (2019) Prevalence and determinants of self-referrals to a District-Regional Hospital in KwaZulu Natal, South Africa: a cross sectional study. Pan Afr Med J, 33(4) doi: 10.11604/pamj.2019.33.4.16963. PMID: 31303949; PMCID: PMC6607454.
[8] Okoli H, Obembe T, Osungbade K, Adeniji F (2017) Self-referral patterns among federal civil servants in oyo state, South-Western Nigeria. Pan Afr Med J. 8(26):1-11. doi:10.11604/pamj.2017.26.105.11483.
[9] Wolkite Olani Abdi, Waju Beyene Salgedo, Gebeyehu Tsega Nebeb. (2015) Magnitude and Determinants of Self-Referral of Patients at a GeneralHospital, Western Ethiopia., Science Journal of Clinical Medicine, 4, (5), pp. 86-92. doi: 10.11648/j.sjcm.20150405.1
[10] Fisseha G, Berhane Y, Worku A, Terefe W (2017) Distance from health facility and mothers’ perception of quality related to skilled delivery service utilization in northern Ethiopia. Int J Womens Health, 9:749-756. doi: 10.2147/IJWH.S140366. PMID: 29042819; PMCID: PMC5633329.
[11] Eritero AC, Gebreslasie KZ, Asgedom AT, Areba AS (2022) Self ‑ referrals and associated factors among laboring mothers at Dilla University Referral Hospital, Dilla, Gedeo Zone, Ethiopia: a cross ‑ sectional study. BMC Womens Health 1-10. doi:10.1186/s12905-022-02002-7.
[12] Cervantes K, Salgado R, Choi M (2003) Rapid Assessment of Referral Care Systems. A guide for Program Managers. Edited by: Basic J, 66. https://m.facebook.com/221666151591142/posts/referral-systems-a-summary-of-key-processes-to-guide-health-services-managersan-/286883811736042/.
[13] Murray SF (2006) Maternity referral systems in developing countries: current knowledge and future research needs. Soc Sci Med 62(9):2205–15. https://doi.org/10.1016/j.socscimed.2005.10.025
[14] Abere, TM, Atnafu, DD & Mulu, Y (2021) Self-referral and associated factors among patients attending adult outpatient departments in Debre tabor general hospital, Northwest Ethiopia. BMC Health Serv Res 21, 607. https://doi.org/10.1186/s12913-021-06642-7
[15] Wambui M (2021) Determinants of Self Directed Referral Amongst Patients Seeking Health Services At Kenyatta National Hospital, Nairobi, Kenya.’ Afribary. Afribary, https://afribary.com/works/determinants-of-self-directed-referral-amongst-patients-seeking.
[16] National Population Commission (2006) NATIONAL CENSUS Nigeria.
[17] Elisso M (2016) Assessment of the Magnitude of Bypassing Public Health Center Delivery Service and Associated Factors among Postnatal Women in Negist Eleni Memorial Hospital, South Ethiopia Int J Community Med Public Health. Available at: http://thesisbank.jhia.ac.ke/id/eprint/7109 (Accessed on: 5th December 2023).
[18] Eshetie A, Belachew TB, Negash WD, Asmamaw DB, Muktar SA, Kebede A (2023) Self-referral practice and associated factors among women
who gave birth in South Gondar zone primary hospitals, Northwest Ethiopia: a cross-sectional study design. Front Public Health 1128845. doi: 10.3389/fpubh.2023.1128845. PMID: 37342276; PMCID: PMC10277469).[19] Adoyo JO, Makunyi EG, Otieno GO, Yoos A (2021) Magnitude and determinants of self-referrals among women seeking skilled birth attendance services: a cross-sectional hospital-based study in Marsabit County, Kenya. Int J Community Med Public Health. 8:1. 10.18203/2394-6040.ijcmph20211728).
[20] Kruk ME, Hermosilla S, Larson E, Mbaruku GM (2014) Bypassing primary care clinics for childbirth: a cross-sectional study in the Pwani region, United Republic of Tanzania. Bull World Health Organ. (2014) 92:246–53. doi: http://dx.doi.org/10.2471/BLT.13.126417.
Viewed PDF 570 21 -
Safety Including Health Factors Contribute the Female Victims to Escape from Domestic Violence: A Qualitative AnalysisAuthor: Mahathir YahayaDOI: 10.21522/TIJPH.2013.11.04.Art029
Safety Including Health Factors Contribute the Female Victims to Escape from Domestic Violence: A Qualitative Analysis
Abstract:
Domestic violence is one of the public health problems, and most of the victims are female. This vulnerable group can no longer bear the suffering caused by the atrocities committed by their husbands. The various abuses that the victim experiences not only impact their health but can also threaten the level of safety of everyone in the family system. This research aims to identify the safety factors including health aspect that contribute to the female victim’s violent actions being separate from their husbands. In line with the qualitative approach, in-depth interviews with 15 female informants of domestic violence were conducted around the state of Penang and this analysis using NVIVO 8 software. The results found that the theme of victim safety factors, including injury and social systems, especially children, motivates victims to free themselves from domestic violence and seek help for personal protection. The findings of this study have yielded several recommendations in the context of social work interventions to increase the positive health and social well-being of family system life, especially among female victims of domestic violence.
Keywords: Female victim of domestic violence, Public Health Issues, Safety, Social work intervention.Safety Including Health Factors Contribute the Female Victims to Escape from Domestic Violence: A Qualitative Analysis
References:
[1] Isaacs, V., Mohamad, N., Adnan, L. H. M., Rosdi, W. H. A. W., Mustafa, N. S., Fauzi, N. F. A. M., & Zakaria, N. H. (2020). Hubungan antara Penagihan Dadah dengan Keganasan Rumah Tangga. Jurnal Undang-undang dan Masyarakat, 25, 7-14.
[2] Yusof, M. M., Azman, A., Singh, P. S. J., & Yahaya, M. (2021). A qualitative analysis of the coping strategies of female victimization after separation. Journal of human rights and social work, 1-7.
[3] Arief, H., & Rahim, R. A. (2020). Wanita dan keganasan rumah tangga di Malaysia dan Indonesia.
[4] Kementerian Pembagunan Wanita, Keluarga dan Masyarakat (KPWKM) (2021). Data terbuka Jabatan Kebajikan Masyarakat berkaitan bilangan kes keganasan rumahtangga mengikut negeri, bilangan lelaki dan perempuan dan jumlah keseluruhan tahun 2019. https://www.data.gov.my/data/ms_MY/dataset/bilangan-kes-keganasan-rumahtangga-mengikut-negeri.
[5] Aregger Lundh, A., Tannlund, C., & Ekwall, A. (2023). More support, knowledge and awareness are needed to prepare emergency department nurses to approach potential intimate partner violence victims. Scandinavian journal of caring sciences, 37(2), 397-405.
[6] Hanafi, A., & Rohani, A. R. 2015. Kekerasan Rumah Tangga Terhadap Wanita: Kajian Perbandingan Sosio-Perundangan Di Malaysia Dan Indonesia. Al ‘Adl, VII (14), 117-142.
[7] Oyunbileg, S., Sumberzul, N., Udval, N., Wang, J-D., & Janes, C. R. (2009). Prevalence and risk factors of domestic violence among Mongolian women. Journal of Women’s Health, 18(11), 1873-1880.
[8] National Women’s Policy. (1989). Objektif Dasar Wanita Negara. Retrieved from http://www.pmo.gov.my/dokumenattached/Dasar/17DASAR_WANITA_NEGARA.pdf.
[9] Domestic Violence Act 1994 (2008). Pesuruhjaya Penyemak Undang-Undang Malaysia Di bawah Kuasa Akta Penyemakan Undang-Undang 1968.
[10] Razali, A., Tohar, S. N. A. M., & Ani, F. (2017). Jenayah menggugat kelestarian wanita. Human Sustainability Procedia.
[11] Marican, S. (2006). Penyelidikan sains sosial pendekatan pragmatik. Selangor: Edusystem Sdn. Bhd.
[12] Heron, R. L., Eisma, M., & Browne, K. (2022). Why do female domestic violence victims remain in or leave abusive relationships? A qualitative study. Journal of Aggression, Maltreatment & Trauma, 31(5), 677-694.
[13] Shakila, A. M. (2011). Doing Gender in Literature. Dalam Cecilia, N., Noraida, E., & Rashidah, S. Our lived Realities: Reading gender in Malaysia. Pulau Pinang: Universiti Sains Malaysia.
[14] Archer, J. (2006). Cross-cultural differences in physical aggression between partners: A social-role analysis. Personality and Social Psychology Review, 10, 133-153.
[15] Khaw, L., & Hardesty, J. L. (2007). Theorizing the process of leaving: Turning points and trajectories in the stages of change. Family Relations, 56, 413–425.
[16] Macy, R. J., Nurius, P. S., Kernic, M. A., Holt, V. L. (2005). Battered women’s profiles associated with service help-seeking efforts: Illuminating opportunities for intervention. Social Work, 29(3), 137-150.
[17] Hacettepe University Institute of Population Studies. (2009). Turkey demographic and health survey 2008. Publication No. NEE-HÜ.09.01. Retrieved from http://www.hips.hacettepe.edu.tr/eng/tdhs08/TDHS-2008_Main_Report.pdf [Verified 17 August 2015].
[18] Mustaffa, J., & Ngah, K. (2015). Jenayah rogol: Isu dan penyelesaian. Sintok: Universiti Utara Malaysia.
[19] Williams, S. L., & Frieze, I. H. (2005). Patterns of violent relationships, psychological distress, and marital satisfaction in a national sample of men and women. Sex Roles, 52(11-12), 771–784.
[20] Buzawa, E.S., Buzawa, C. G., & Stark, E. (2012). Responding to domestic violence: Integration of criminal justice dan human services. United State: SAGE.
[21] Mohd Salleh, K. (1994). Wanita dan alam perjuangannya. Kuala Lumpur: Institut Kajian Dasar.
[22] Bertalanffy, L. V. (1968). General system theory (rev. ed.). New York: George Braziller.
[23] Mardiyati, I. (2015). Dampak trauma kekerasan dalam rumah tangga terhadap perkembangan psikis anak. Jurnal Studi Gender dan Anak, 26-35. Retrieved from file:///C:/Users/User/Downloads/166-523-1-PB%20(1).pdf.
[24] Evans, S. E., Davies, C., & DiLillo, D. (2008). Exposure to domestic violence: A meta-analysis of child and adolescent outcomes. Aggressive and Violent Behavior, 13, 131–140.
[25] Davis, R. E. (2002). ‘The strongest women’: Exploration of the inner resources of abused women. Qualitative Health Research, 12, 1248–1263.
[26] Bahari, R., Usman, N., & Ninggal, M. (2008). Rumahku syurgaku: Bagaimana menyelesaikan masalah rumah tangga. Seminar Kaunseling Keluarga: Falkulti Pendidikan Universiti Teknologi Malaysia.
[27] Ayotunde, T., Akintoye, O.O., & Adefunke, E.S. (2014). Influence of Women’s Attitude on the
Perpetration of Gender-Based Domestic Violence in Nigeria. Gender & Behaviour, 12(2), 6420-6429.[28] Barnett, O.W., Miller-Perrin, C.L., & Perrin, R.D. (2011). Family violence across the lifespan: an introduction. US: SAGE.
[29] Noraida, E., & Intan Hashimah, M. H. (2011). The Nature and Impact of Domestic Violence: A Study of Survivors of Wife Abuse in Malaysia. Dalam Cecilia, N., Noraida, E., & Rashidah, S. Our lived Realities: Reading gender in Malaysia. Pulau Pinang: Universiti Sains Malaysia.
[30] Harne, L., & Radford, J. (2008). Tacking domestic violence: Theories, policies, and practice. McGrawHill: Open University Press.
[31] Mariny, A. G., Sabasiah, H., & Azizul, M. (2016). Isu keganasan rumah tangga: Keberkesanan perkhidmatan kaunseling berdasarkan perspektif klien wanita mangsa keganasan. Jurnal Kemanusiaan, 25(2), 1-9.
[32] Sayuti, R., Abdul Hamid, A.S., & Fauzaman, J. (2014). Penghantar kerja sosial. Kuala Lumpur: Institut Terjemahan & Buku Malaysia Berhad.
Viewed PDF 614 29 -
Endorsement of Spousal Sexual Violence Across Gender: Evidence from Zambia Demographic and Health SurveyAuthor: Edson ChipaloDOI: 10.21522/TIJPH.2013.11.04.Art030
Endorsement of Spousal Sexual Violence Across Gender: Evidence from Zambia Demographic and Health Survey
Abstract:
Spousal sexual violence (SSV) constitutes a pressing public health and human rights crisis, exerting detrimental impacts on women's well-being and imposing significant social and economic costs on their lives. This study aimed to ascertain the comprehensive prevalence of SSV endorsement and investigate the factors associated with such endorsement among both men and women in Zambia. The 2013-2014 Zambia Demographic and Health Survey (ZDHS) served as the dataset for this study. Employing chi-square tests and two multiple logistic regression analyses stratified by gender, the research revealed that 36.6% of women and 11.5% of men endorsed SSV. Regression results highlighted significant associations between SSV endorsement and variables such as resident type, marital status, education level, and frequency of reading newspapers/magazines, cutting across genders. Among women, employment, religion, and frequency of listening to/watching television also emerged as significant factors. Conversely, wealth status and alcohol consumption significantly correlated with SSV endorsement exclusively among men in Zambia. Recognizing the potential of media platforms to shape attitudes, the study recommends leveraging them to disseminate messages discouraging SSV endorsement. Furthermore, this study emphasizes the necessity of involving multiple stakeholders, including religious leaders, traditional leaders, and non-governmental organizations (NGOs), to address cultural norms promoting SSV endorsement. The implementation of policies regulating gender-based violence and alcohol becomes imperative in diminishing both the prevalence and tolerance of SSV in Zambia. Finally, this study recommends that future research endeavors delve into men's perspectives on understanding SSV beyond the conventional focus on women victims in Zambia.
Keywords: Endorsement, spousal sexual violence, intimate partner violence, gender, media, alcohol, factors, Zambia.Endorsement of Spousal Sexual Violence Across Gender: Evidence from Zambia Demographic and Health Survey
References:
[1] Pallitto, C.C., et al., Intimate partner violence, abortion, and unintended pregnancy: results from the WHO Multi-country Study on Women's Health and Domestic Violence. International Journal of Gynecology & Obstetrics, 2013. 120(1): p. 3-9.
[2] WHO. Global and regional estimates of violence against women. 2013 [cited 2023 June 14th]; Available from: https://www.who.int/publications/i/item/9789241564625.
[3] Wake, A.D. and U.R. Kandula, The global prevalence, and its associated factors toward domestic violence against women and children during COVID-19 pandemic—” The shadow pandemic”: A review of cross-sectional studies. Women's Health, 2022. 18: p. 17455057221095536.
[4] Lee, Y.S., M. Behn, and K.M. Rexrode, Women's health in times of emergency: We must take action. Journal of Women's Health, 2021. 30(3): p. 289-292.
[5] Giudice, L.C., et al., Climate change, women’s health, and the role of obstetricians and gynecologists in leadership. International Journal of Gynecology & Obstetrics, 2021. 155(3): p. 345-356.
[6] Shukla, S., J.A. Ezebuihe, and J.I. Steinert, Association between public health emergencies and Sexual and reproductive health, gender-based violence, and early marriage among adolescent girls: a rapid review. BMC Public Health, 2023. 23(1): p. 1-14.
[7] Weiss, H.A., et al., Spousal sexual violence and poverty are risk factors for sexually transmitted infections in women: a longitudinal study of women in Goa, India. Sexually transmitted infections, 2008. 84(2): p. 133-139.
[8] Waltermaurer, E., Public justification of intimate partner violence: A review of the literature. Trauma, Violence, & Abuse, 2012. 13(3): p. 167-175.
[9] WHO. Violence Against Women. 2017 [cited 2017 June 14th]; Available from: https://www.who.int/news-room/fact-sheets/detail/violence-against-women.
[10] Gohari, M.A., et al., Prevalence of domestic violence against women and its visibility in southeast Iran. Iranian Journal of Public Health, 2023. 52(3): p. 646.
[11] Cantor, D., et al., Report on the AAU campus climate survey on sexual assault and sexual misconduct. 2015, Association of American Universities Washington, DC.
[12] Kalichman, S.C., et al., Gender attitudes, sexual violence, and HIV/AIDS risks among men and women in Cape Town, South Africa. Journal of Sex Research, 2005. 42(4): p. 299-305.
[13] Krebs, C.P., et al., The sexual assault of undergraduate women at Historically Black Colleges and Universities (HBCUs). Journal of Interpersonal Violence, 2011. 26(18): p. 3640-3666.
[14] Simona, S., M. Muchindu, and H. Ntalasha, Intimate Partner Violence (IPV) in Zambia: Socio-demographic Determinants and Association with Use of Maternal Health Care. Int'l J. Soc. Sci. Stud., 2018. 6: p. 42.
[15] Watts, C.H., et al., Sexual violence and conflict in Africa: prevalence and potential impact on HIV incidence. Sexually transmitted infections, 2010. 86(Suppl 3): p. iii93-iii99.
[16] Abramsky, T., et al., What factors are associated with recent intimate partner violence? Findings from the WHO multi-country study on women's health and domestic violence. BMC Public Health, 2011. 11(1): p. 1-17.
[17] Adebowale, A.S., Spousal age difference and associated predictors of intimate partner violence in Nigeria. BMC Public Health, 2018. 18(1): p. 1-15.
[18] Svalin, K. and S. Levander, The predictive validity of intimate partner violence risk assessments conducted by practitioners in different settings—a review of the literature. Journal of Police and Criminal Psychology, 2020. 35: p. 115-130.
[19] Lee, S. and E. Lee, Predictors of intimate partner violence among pregnant women. International Journal of Gynecology & Obstetrics, 2018. 140(2): p. 159-163.
[20] Carpenter, R.K. and J.D. Stinson, Neighborhood-level predictors of sexual violence across intimate partner and non-intimate partner relationships: a case–control study. Sexual Abuse, 2022. 34(6): p. 716-743.
[21] Koris, A., et al., Opportunities and challenges in preventing violence against adolescent girls through gender transformative, whole-family support programming in Northeast Nigeria. Conflict and Health, 2022. 16(1): p. 1-15.
[22] Okenwa, L. and S. Lawoko, Social indicators and physical abuse of women by intimate partners: A study of women in Zambia. Violence and Victims, 2010. 25(2): p. 278-288.
[23] Okenwa, L.E., S. Lawoko, and B. Jansson, Exposure to intimate partner violence amongst women of reproductive age in Lagos, Nigeria: Prevalence and predictors. Journal of Family Violence, 2009. 24: p. 517-530.
[24] Lawoko, S., Predictors of attitudes toward intimate partner violence: A comparative study of men in Zambia and Kenya. Journal of Interpersonal Violence, 2008. 23(8): p. 1056-1074.
[25] Krupa, E., et al., Catalyzing Action on Intimate Partner Violence Against Pregnant Adolescent Girls Adolescent girls and Young Women in Zambia, in Young People, Violence and Strategic Interventions in Sub-Saharan Africa. 2023, Springer. p. 163-185.
[26] Zegeye, B., et al., Understanding the factors associated with married women’s attitudes towards wife-beating in sub-Saharan Africa. BMC Women's Health, 2022. 22(1): p. 1-11.
[27] Arthur-Holmes, F., et al., Intimate partner violence and pregnancy termination among women in Sub-Saharan Africa. Journal of Interpersonal Violence, 2023. 38(1-2): p. 2092-2111.
[28] El-Bassel, N., et al., Intertwined epidemics: progress, gaps, and opportunities to address intimate partner violence and HIV among key populations of women. The Lancet HIV, 2022.
[29] Coll, C.V., et al., Intimate partner violence in 46 low-income and middle-income countries: an appraisal of the most vulnerable groups of women using national health surveys. BMJ Global Health, 2020. 5(1): p. e002208.
[30] Muluneh, M.D., et al., Gender based violence against women in sub-Saharan Africa: a systematic review and meta-analysis of cross-sectional studies. International Journal of Environmental Research and Public Health, 2020. 17(3): p. 903.
[31] Beres, L.K., et al., Intimate partner violence poly victimisation and HIV among coupled women in Zambia: Analysis of a population-based survey. Global Public Health, 2020. 15(4): p. 558-570.
[32] Muchomba, F.M., Sex composition of children and spousal sexual violence in sub-Saharan Africa. Maternal and Child Health Journal, 2019. 23: p. 1130-1139.
[33] Farrell, A.-M., et al., Regulating tech-sex and managing image-based sexual abuse: an Australian perspective. Information & Communications Technology Law, 2022: p. 1-18.
[34] Obagboye, T. and S. James, Preventing Gender-Based Violence in Africa (Nigeria And Ethiopia); Socio-Legal Considerations. Irish International Journal of Law, Political Sciences and Administration, 2022. 6(5).
[35] Aho, N., M. Gren-Landell, and C.G. Svedin, The prevalence of potentially victimizing events, poly-victimization, and its association to sociodemographic factors: A Swedish youth survey. Journal of Interpersonal Violence, 2016. 31(4): p. 620-651.
[36] United Nations Human Right. Women’s Rights are Human Rights. 2014 June 9th, 2023]; Available from: https://www.ohchr.org/documents/events/whrd/womenrightsarehr.pdf.
[37] Aborisade, R.A., On the ‘darkness of dark figure’of sexual crimes: Survivors' rape reporting experiences with the Nigerian police. International Journal of Law, Crime and Justice, 2023. 73: p. 100576.
[38] Jere, V., Causes of Gender-Based Violence in Mtenguleni and Madzimawe Villages of Chipata District. 2022.
[39] Shikupilwa, A., Everyday Violence and Women's Lives in Zambia: An Autoethnography. 2018.
[40] Payton, E., et al., Women's perceptions of intimate partner violence in Zambia. Violence and Gender, 2019. 6(4): p. 219-226.
[41] Ajayi, C.E., K. Chantler, and L. Radford, The role of cultural beliefs, norms, and practices in Nigerian women’s experiences of sexual abuse and violence. Violence against women, 2022. 28(2): p. 465-486.
[42] Shezongo-Macmillan, J., Women, and L.i.S.A.T. Zambia, Women's sexual and reproductive rights and HIV/AIDS transmission in Zambia. 2007: Women and Law in Southern Africa Research and Educational Trust-Zambia.
[43] Fine, S.L., et al., The role of violence acceptance and inequitable gender norms in intimate partner violence severity among couples in Zambia. Journal of Interpersonal Violence, 2021. 36(19-20): p. NP10744-NP10765.
[44] Murray, S.M., et al., A qualitative exploration of mechanisms of intimate partner violence reduction for Zambian couples receiving the Common Elements Treatment Approach (CETA) intervention. Social Science & Medicine, 2021. 268: p. 113458.
[45] Tadesse, G. and B. Yakob, Risky sexual behaviors among female youth in Tiss Abay, a semi-urban area of the Amhara Region, Ethiopia. PLoS One, 2015. 10(3): p. e0119050.
[46] Backe, E.L., E. Bosire, and E. Mendenhall, “Drinking Too Much, Fighting Too Much”: The Dual “Disasters” of Intimate Partner Violence and Alcohol Use in South Africa. Violence against women, 2022. 28(10): p. 2312-2333.
[47] Steele, M.E., et al., A test of General Strain Theory: Explaining intimate partner violence and alcohol use among black women. Feminist criminology, 2022. 17(2): p. 163-184.
[48] Bello, B., et al., Alcohol use and sexual risk behaviour among men and women in inner-city Johannesburg, South Africa. BMC Public Health, 2017. 17: p. 65-75.
[49] Foran, H.M. and K.D. O'Leary, Alcohol, and intimate partner violence: A meta-analytic review. Clinical psychology review, 2008. 28(7): p. 1222-1234.
[50] Wilson, I.M., K. Graham, and A. Taft, Alcohol interventions, alcohol policy and intimate partner violence: a systematic review. BMC Public Health, 2014. 14: p. 1-11.
[51] Graham, K., et al., Alcohol may not cause partner violence, but it seems to make it worse: A cross national comparison of the relationship between alcohol and severity of partner violence. Journal of interpersonal violence, 2011. 26(8): p. 1503-1523.
[52] Kane, J.C., et al., Concordance of self‐and partner‐reported alcohol consumption among couples experiencing intimate partner violence in Zambia. Alcoholism: Clinical and Experimental Research, 2019. 43(12): p. 2568-2577.
[53] Gaskins, J.L., The Impact of Gender, Sexual Orientation, and Victim Injury Severity on Perceptions of Intimate Partner Violence. 2013.
[54] Carels, C., et al., Youths’ perceptions of the relation between alcohol consumption and risky sexual behaviour in the Western Cape, South Africa: a qualitative study. Child Indicators Research, 2022. 15(4): p. 1269-1293.
[55] Babor, T.F., et al., Alcohol: no ordinary commodity: research and public policy. 2022.
[56] Rehm, J., et al., Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. The lancet, 2009. 373(9682): p. 2223-2233.
[57] Lloyd, S. and S. Ramon. Media representations of intimate partner domestic violence (IPDV) and mental health issues: a UK Case Study. in Conference: Domestic Violence and Mental Health: Empowering Women and Professionals. 2013.
[58] Sidiq, A., Function of Mass Communication in the Social Development of Afghanistan. Integrated Journal for Research in Arts and Humanities, 2022. 2(4): p. 134-139.
[59] Guðjónsdóttir, R.Á. and J. Ingvar Kjaran, Discourses on fathers who use intimate partner violence: an example from Icelandic mass media. Norma, 2023: p. 1-17.
[60] Copeland, D.A., Newspapers in the Americas. The function of newspapers in society: a global perspective, 2003: p. 103-126.
[61] Consalvo, M., “3 shot dead in courthouse”: Examining news coverage of domestic violence and mail-order brides. Women's Studies in Communication, 1998. 21(2): p. 188-211.
[62] Berns, N., “My problem and how I solved it”: Domestic violence in women's magazines. The Sociological Quarterly, 1999. 40(1): p. 85-108.
[63] Bullock, C.F. and J. Cubert, Coverage of domestic violence fatalities by newspapers in Washington State. Journal of Interpersonal Violence, 2002. 17(5): p. 475-499.
[64] Vives-Cases, C., J. Torrubiano-Domínguez, and C. Álvarez-Dardet, The effect of television news items on intimate partner violence murders. The European Journal of Public Health, 2009. 19(6): p. 592-596.
[65] Sutherland, G., et al., Mediated representations of violence against women in the mainstream news in Australia. BMC Public Health, 2019. 19: p. 1-8.
[66] Jabbi, A., et al., Prevalence and factors associated with intimate partner violence against women in The Gambia: a population-based analysis. Women & Health, 2020. 60(8): p. 912-928.
[67] Edwards, K.M. and C.M. Dardis, Disclosure recipients’ social reactions to victims’ disclosures of intimate partner violence. Journal of Interpersonal Violence, 2020. 35(1-2): p. 53-76.
[68] Hardesty, J.L. and B.G. Ogolsky, A socioecological perspective on intimate partner violence research: A decade in review. Journal of marriage and family, 2020. 82(1): p. 454-477.
[69] Alsawalqa, R.O., A qualitative study to investigate male victims’ experiences of female-perpetrated domestic abuse in Jordan. Current psychology, 2023. 42(7): p. 5505-5520.
[70] Walker, A., et al., Male victims of female-perpetrated intimate partner violence, help-seeking, and reporting behaviors: A qualitative study. Psychology of Men & Masculinities, 2020. 21(2): p. 213.
[71] Zambia Statistics Agency, M.o.H.Z. and ICF, Zambia demographic and health survey 2018. Lusaka, Zambia, and Rockville, Maryland, USA: Zambia Statistics Agency, Ministry of Health, and ICF, 2019.
[72] Phiri, B., The Role of Mass Media as a Tool for Public Enlightenment in Achieving the Sustainable Development Goals in Lusaka. 2021, Cavendish University.
[73] Mukuka, N., Gender Based Violence Against Men in Bauleni Compound of Lusaka, Lusaka Province. 2021, Cavendish University.
[74] Sterne, J.A., et al., Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ, 2009. 338.
[75] George, D., and P. Mallery, IBM SPSS statistics 27 step by step: A simple guide and reference. 2021: Routledge.
[76] Zambia Demographic and Health Survey. Central Statistics Office, Ministry of Health, Lusaka, Zambia. 2007 [cited 2021 November 23rd]; Available from: http://www.measuredhs.com/pubs/pdf/FR211/FR211 [revised-05-12-2009].pdf.
[77] Dickson, K.S., E.K. Ameyaw, and E.K.M. Darteh, Understanding the endorsement of wife beating in Ghana: evidence of the 2014 Ghana demographic and health survey. BMC Women's Health, 2020. 20(1): p. 1-7.
[78] Murray, T., Overview, and summary: Addressing social determinants of health: Progress and opportunities. OJIN: The Online Journal of Issues in Nursing, 2018. 23(3).
[79] Chirwa, E.D., et al., Prevalence and risk factors of physical or sexual intimate violence perpetration amongst men in four districts in the central region of Ghana: Baseline findings from a cluster randomised controlled trial. PloS one, 2018. 13(3): p. e0191663.
[80] Dover, P., Gender, and embodiment: Expectations of manliness in a Zambian village. African masculinities: Men in Africa from the late nineteenth century to the present, 2005: p. 173-187.
[81] Simpson, A., Sons, and fathers/boys to men in the time of AIDS: Learning masculinity in Zambia. Journal of Southern African Studies, 2005. 31(3): p. 569-586.
[82] Kimuna, S.R. and Y.K. Djamba, Gender based violence: Correlates of physical and sexual wife abuse in Kenya. Journal of Family Violence, 2008. 23: p. 333-342.
[83] Gass, J.D., et al., Gender differences in risk for intimate partner violence among South African adults. Journal of Interpersonal Violence, 2011. 26(14): p. 2764-2789.
[84] Ghose, B. and S. Yaya, Experience of intimate partner violence and help-seeking behaviour among women in Uganda. Psych, 2019. 1(1): p. 182-192.
[85] White, H.R. and P.-H. Chen, Problem drinking and intimate partner violence. Journal of Studies on Alcohol, 2002. 63(2): p. 205-214.
[86] Fulu, E., et al., Why do some men use violence against women and how can we prevent it? Quantitative findings from the United Nations multi-country study on men and violence in Asia and the Pacific. 2013.
[87] Fulu, E., et al., Why Do Some Men Use Violence Against Women and How Can We Prevent it? 2013.
[88] World Health Organization [WHO], Global Status Report on Alcohol and Health. 2011, Geneva, Switzerland: World Health Organization.
[89] Murty, S.A., et al., Physical and emotional partner abuse reported by men and women in a rural community. American Journal of Public Health, 2003. 93(7): p. 1073-1075.
[90] Peek-Asa, C., et al., Rural disparity in domestic violence prevalence and access to resources. Journal of Women's Health, 2011. 20(11): p. 1743-1749.
[91] Kusanthan, T., S. Mwaba, and J. Menon, Factors affecting domestic violence among married women in Zambia. British Journal of Education, Society & Behavioural Science, 2016. 12(2): p. 1-13.
[92] Drumm, R., et al., “God just brought me through it”: Spiritual coping strategies for resilience among intimate partner violence survivors. Clinical Social Work Journal, 2014. 42: p. 385-394.
[93] Ware, K.N., H.M. Levitt, and G. Bayer, May God help you: Faith leaders' perspectives of intimate partner violence within their communities. Journal of Religion & Abuse, 2004. 5(2): p. 55-81.
[94] Davis, M. and M. Johnson, exploring black clergy perspectives on religious/spiritual related domestic violence: First steps in facing those who wield the sword abusively. Journal of Aggression, Maltreatment & Trauma, 2021. 30(7): p. 950-971.
[95] Koch, J.R. and I.L. Ramirez, Religiosity, Christian fundamentalism, and intimate partner violence among US college students. Review of Religious Research, 2010: p. 402-410.
[96] Wang, M.-C., et al., Christian women in IPV relationships: An exploratory study of religious factors. Journal of Psychology and Christianity, 2009. 28(3): p. 224.
[97] Kafunda, C., An investigation on the declaration of Zambia as a Christian nation and its contribution to peace and conflict resolution. 2022, The University of Zambia.
[98] Dube, S.I., Praying for Change in the Nations: Prayer, Politics, and Power in Sub-Saharan Africa. Journal of Church and State, 2021. 63(3): p. 396-418.
[99] Chaudhry, T. and L. Cattaneo, Religious Help-Seeking in Survivors of Intimate Partner Violence. Journal of Family Violence, 2023: p. 1-13.
[100] Istratii, R. and P. Ali, A multi-sectoral evidence synthesis on religious beliefs, intimate partner violence and faith-based interventions. 2022.
[101] Istratii, R. and P. Ali, A Scoping Review on the Role of Religion in the Experience of IPV and Faith-Based Responses in Community and Counseling Settings. Journal of Psychology and Theology, 2023: p. 00916471221143440.
[102] Doku, D.T. and K.O. Asante, Women’s approval of domestic physical violence against wives: analysis of the Ghana demographic and health survey. BMC Women's Health, 2015. 15: p. 1-8.
[103] Owusu Adjah, E.S. and I. Agbemafle, Determinants of domestic violence against women in Ghana. BMC Public Health, 2016. 16(1): p. 1-9.
[104] Darteh, E.K.M., et al., Justification of physical intimate partner violence among men in sub-Saharan Africa: a multinational analysis of demographic and health survey data. Journal of Public Health, 2021. 29: p. 1433-1441.
[105] Darteh, E.K.M., D.T. Doku, and K. Esia-Donkoh, Reproductive health decision making among Ghanaian women. Reproductive Health, 2014. 11(1): p. 1-8.
[106] Milimo, J., et al., Economic support, education and sexual decision making among female adolescents in Zambia: a qualitative study. BMC Public Health, 2021. 21(1): p. 1-8.
[107] Hindin, M.J. and L.S. Adair, Who's at risk? Factors associated with intimate partner violence in the Philippines. Social Science & Medicine, 2002. 55(8): p. 1385-1399.
[108] Hindin, M.J., Adolescent childbearing and women’s attitudes towards wife beating in 25 sub-Saharan African countries. Maternal and Child Health Journal, 2014. 18: p. 1488-1495.
[109] Rolle, L., et al., Domestic violence and newspaper: an explorative study. Procedia-social and Behavioral Sciences, 2014. 127: p. 504-508.
[110] Haider‐Markel, D.P. and M.R. Joslyn, Gun policy, opinion, tragedy, and blame attribution: The conditional influence of issue frames. Journal of Politics, 2001. 63(2): p. 520-543.
[111] Alpert, E., A. Miles, and V. Coffey, Responding to domestic violence: An interfaith guide to prevention and intervention. Chicago: The Chicago metropolitan battered women’s network, 2005.
[112] Sikweyiya, Y., et al., Patriarchy and gender-inequitable attitudes as drivers of intimate partner violence against women in the central region of Ghana. BMC Public Health, 2020. 20: p. 1-11.
[113] Slakoff, D.C., W. Aujla, and E. PenzeyMoog, the role of service providers, technology, and mass media when home isn't safe for intimate partner violence victims: best practices and recommendations in the era of Covid-19 and beyond. Archives of Sexual Behavior, 2020: p. 1-10.
[114] Chinambu, K.K., Gender based Violence in Zambia: The Ineffective Enforcement of the Anti-Gender based Violence Act of 2011. Journal of Legal Studies & Research, 2023. 9(2): p. 127-133.
[115] Kabeya, E., A Critical Examination of The Anti-Gender Based Violence Act and Marital Rape In Zambia. 2021, Cavendish University.
[116] Lwatula, M., Gender-based violence in Zambia: a post-colonial feminist critique. 2019, University of Sussex.
[117] Brundige, E. and T. Banda, when criminal law is not enoughToward a holistic approach to gender-based violence prevention and response in Zambia and beyond, in The Routledge Handbook of African Law. 2021, Routledge. p. 392-406.
[118] Ngonga, Z., Factors contributing to physical gender based violence reported at Ndola Central Hospital, Ndola, Zambia: A case control study. Medical Journal of Zambia, 2016. 43(3): p. 145-151.
[119] Paul, R., J. Ncheka, and N. Hammerstein, Increasing problem of alcohol abuse among the Zambian population in the Psychiatric Setting. 2017.
[120] Ministry of Health. Attain the goal of circumcising 2 000 000 males by the year 2020. 2019 [cited 2019 November 23rd]; Available from: https://www.moh.gov.zm/?p=5842.
[121] Babor, T., Alcohol: no ordinary commodity: research and public policy. 2010.
[122] Markowitz, S., The price of alcohol, wife abuse, and husband abuse. Southern Economic Journal, 2000. 67(2): p. 279-303.
Viewed PDF 602 14 -
 Examining Contraceptive Ideational Disparities Among Adolescents and Young Women in NigeriaAuthor: Oluwayemisi IsholaDOI: 10.21522/TIJPH.2013.11.04.Art031
Examining Contraceptive Ideational Disparities Among Adolescents and Young Women in NigeriaAuthor: Oluwayemisi IsholaDOI: 10.21522/TIJPH.2013.11.04.Art031Examining Contraceptive Ideational Disparities Among Adolescents and Young Women in Nigeria
Abstract:
Nigeria faces a demographic challenge with a growing youth population and increasing fertility rate. However, the use of modern contraceptives among adolescent girls and young women has been declining. The young population emerges as a pivotal group in the country’s efforts to achieving the pledge of 27% modern contraceptive rate by the year 2030. This study aims to explore the disparities in contraceptive ideation among adolescents and young women in Nigeria, focusing on the role of ideational factors. The data for this study were collected through a cross-sectional household survey in four Nigerian states, involving 2,857 sexually active women aged 15-24 years. Using an ideational framework of behavior that highlights psychosocial influences, nine distinct ideational variables were examined. Multivariate logistic regression analyses were used to assess associations between ideational factors and contraceptive use among the total sample, adolescents, and youth. Statistical significance was defined as P<0.05. The study’s results revealed significant associations between the ideational variables and contraceptive use in all groups, ranging from p < .05 to p < .001. Cognitive and emotional domains were found to be the strongest predictors of contraceptive use compared to social domains in the general sample and among both groups. This study’s findings highlight the complex interplay of social, cognitive, and emotional factors in contraceptive use. Understanding these dynamics is crucial in developing effective strategies to overcome barriers and improve access to contraceptive services among young women in Nigeria.
Keywords: Adolescents, Contraception, Ideation, Youth.Examining Contraceptive Ideational Disparities Among Adolescents and Young Women in Nigeria
References:
[1] United Nations. (2022). World Population Prospects 2022. Retrieved from UN: https://population.un.org/wpp/Graphs/DemographicProfiles/Pyramid/566.
[2] Olowolafe, T. A., Adebowale, A. S., Fagbamigbe, A. F., Bolarinwa, O. A., & Akinyemi, J. O. (2023). Shifts in age pattern, timing of childbearing and trend in fertility level across six regions of Nigeria: Nigeria Demographic and Health Surveys from 2003-2018. PloS one, 18(1), e0279365. https://doi.org/10.1371/journal.pone.0279365.
[3] National Population Commission (NPC) [Nigeria] and ICF. 2019. Nigeria Demographic and Health Survey 2018. Abuja, Nigeria, and Rockville, Maryland, USA: NPC and ICF.
[4] Mandal, M., Calhoun, L., McGuire, C., & Speizer, I. (2022). Using structural equation modeling to examine the influence of family planning social norms on modern contraceptive use in Nigeria. Front. Social, 7. https://doi.org/10.3389/fsoc.2022.866254.
[5] OlaOlorun, F. M., Hindin, M. J., & Akinlo, A. D. (2014). Intention to use contraceptives and subsequent contraceptive behavior in Nigeria: does facility-level access matter?. Open Access Journal of Contraception, 5, 1-8.
[6] Babalola, S., John, N., Ajao, B., & Speizer, I. (2015). Ideation and intention to use contraceptives in Kenya and Nigeria. Demographic research, 33, 211-242. doi: 10.4054/DemRes.2015.33.8.
[7] Babalola S. (2017). Changes in Ideational Profiles of Women of Reproductive Age in Urban Nigeria: The Role of Health Communication. Health education & behavior : the official publication of the Society for Public Health Education, 44(6), 907–917. https://doi.org/10.1177/1090198117699510.
[8] Ezenwaka, U., Ibekwe, P. C., & Anozie, C. (2020). A qualitative study of ecological factors constraining adolescent’s access to contraception in southeast Nigeria. BMC public health, 20(1), 1-14. doi: 10.1186/s12889-020-09533-5.
[9] Health Communication Capacity Collaborative (HC3). (2014). Ideation: An HCS Research Primer. Baltimore, MD: HC3, Johns Hopkins Center for Communication Programs. https://healthcommcapacity.org/hc3resources/ideation-hc3-research-primer/.
[10] Sobotka, T., Zeman, K., & Kantorová, V. (2003). Demographic shifts in the Czech Republic after 1989: A second demographic transition view. European Journal of Population/Revue européenne de démographie, 19(3), 249–277. https://doi.org/10.1023/A:1024913321935.
[11] Leroy-Beaulieu. (1896). Traité Théorique et Pratique d’ Économie Politique. Paris: Librairie Guillaumin et Cie.
[12] Okigbo CC, Speizer IS, Domino ME, Curtis SL, Halpern CT, Fotso JC. (2018) Gender norms and modern contraceptive use in urban Nigeria: A multilevel longitudinal study. BMC Womens Health. Oct 29;18(1).
[13] Adedini SA, Babalola S, Ibeawuchi C, Omotoso O, Akiode A, Odeku M.(2018). Role of religious leaders in promoting contraceptive use in Nigeria: Evidence from the Nigerian Urban reproductive health initiative. Glob Heal Sci Pract. Oct 1;6(3):500–14.
[14] Moreira L.R, Ewerling F, Barros A.J.D, Silveira M.F. (2019). Reasons for nonuse of contraceptive methods by women with demand for contraception not satisfied: An assessment of low and middle-income countries using demographic and health surveys. Reprod Health [Internet]. Available from: https://reproductive-healthjournal.biomedcentral.com/articles/10.1186/s12978-019-0805-7.
[15] Fayehun F. (2017). Contraceptive use in Nigeria is incredibly low. A lack of knowledge may be why [Internet]. The conversation. Available from: https://theconversation.com/contraceptive-use-in-nigeria-is-incredibly-low-a-lack-of knowledge-may-be-why-81453.
[16] Gueye A, Speizer IS, Corroon M, Okigbo CC. (2015). Belief in family planning myths at the individual and community levels and modern contraceptive use in Urban Africa. Int Perspect Sex Reprod Health [Internet].
[17] Zavala, A. R., Palma, S. M., & Kollath-Cattano, C. L. (2020). The role of communication in contraceptive use among Hispanic young adults: A mixed-methods study. BMC Public Health, 20(1), 1-12. https://doi.org/10.1186/s12889-020-09312-5.
[18] Khadduri, R., Reece, M., Barakat, S., & Berenson, A. (2019). Examining the relationship between sexual communication and contraceptive use in young women. Journal of Women’s Health, 28(7), 940-947. https://doi.org/10.1089/jwh.2018.7139.
[19] Boyle, C., & Conrad, M. (2020). Communication about contraception and sexual risk behaviors among college students. Journal of American College Health, 68(7), 700-708. https://doi.org/10.1080/07448481.2019.1664399.
[20] Tschann, J. M., & Adler, N. E. (1997). Sexual self-acceptance, communication with partner, and contraceptive use among adolescent females: a longitudinal study. Journal of research on adolescence: the official journal of the Society for Research on Adolescence, 7(4), 413-430.
[21] Kincaid, D. L. (2000). Mass Media, Ideation, and Behavior: A Longitudinal Analysis of Contraceptive Change in the Philippines. Communication Research, 27(6), 723–763. https://doi.org/10.1177/009365000027006003.
[22] Arisukwu, O., Igbolekwu, C.O., Efugha, I., Nwogu, J., Osueke, N., & Eyitayo, O. (2021). Knowledge and Perception of Emergency Contraceptives Among Adolescent Girls in Imo State, Nigeria. Sexuality & Culture 24, 273–290. https://doi.org/10.1007/s12119-019-09639-x.
[23] Calhoun, L. M., Mirzoyants, A., Thuku, S., Benova, L., Delvaux, T., van den Akker, T., McGuire, C., Onyango, B., & Speizer, I. S. (2022). Perceptions of peer contraceptive use and its influence on contraceptive method use and choice among young women and men in Kenya: a quantitative cross-sectional study. Reproductive health, 19(1), 16. https://doi.org/10.1186/s12978-022-01331-y.
[24] Ochako, R., Mbondo, M., Aloo, S., Kaimenyi, S., Thompson, R., Temmerman, M., & Kays, M. (2015). Barriers to modern contraceptive methods uptake among young women in Kenya: a qualitative study. BMC public health, 15, 118. https://doi.org/10.1186/s12889-015-1483-1.
[25] Agyemang, J., Newton, S., & Danso, K. A. (2019). Determinants of modern contraceptive use among teenagers in Ghana: Analysis of the 2014 Ghana Demographic and Health Survey. Journal of Public Health in Africa, 10(2), 949. doi: 10.4081/jphia.2019.949.
[26] Shahabuddin, A. S., Nöstlinger, C., Delvaux, T., Sarker, M., Bardají, A., Brouwere, V. D., & Broerse, J. E. (2016). What Influences Adolescent Girls’ Decision-Making Regarding Contraceptive Methods Use and Childbearing? A Qualitative Exploratory Study in Rangpur District, Bangladesh. PloS one, 11(6), e0157664. https://doi.org/10.1371/journal.pone.0157664.
[27] Crawford, E. E., Atchison, C. J., Ajayi, Y. P., & Doyle, A. M. (2021). Modern contraceptive use among unmarried girls aged 15-19 years in South Western Nigeria: results from a cross-sectional baseline survey for the Adolescent 360 (A360) impact evaluation. Reproductive health, 18(1), 6. https://doi.org/10.1186/s12978-020-01056-w.
[28] Fehintola, F., Okoro, N., Adedibu, D., Adeniyi, K.D., Adeniyi, C., & Folorunso, O. (2022). Predictors of Willingness to Use Modern Contraceptives among female undergraduate students in a tertiary institution in Nigeria: The Health Belief Approach. Journal of Community Medicine and Primary Health Care, 34(3). DOI: 10.4314/jcmphc.v34i3.12.
[29] Boamah-Kaali, E. A., Ruiter, R. A. C., Owusu-Agyei, S., Asante, K. P., & Mevissen, F. E. F. (2023). Social-psychological determinants of hormonal contraceptive use intentions among adolescent girls in the Bono East Region of Ghana. Frontiers in public health, 11, 1110112. https://doi.org/10.3389/fpubh.2023.1110112.
[30] Agha, S., Morgan, B., Archer, H., Paul, S., Babigumira, J. B., & Guthrie, B. L. (2021). Understanding how social norms affect modern contraceptive use. BMC public health, 21(1), 1061. https://doi.org/10.1186/s12889-021-11110-2.
[31] Sanchez, E. K., Speizer, I. S., Tolley, E., Calhoun, L. M., Barrington, C., & Olumide, A. O. (2020). Influences on seeking a contraceptive method among adolescent women in three cities in Nigeria. Reproductive health, 17(1), 167. https://doi.org/10.1186/s12978-020-01019-1.
[32] Challa, S., Shakya, H. B., Carter, N., Boyce, S. C., Brooks, M. I., Aliou, S., & Silverman, J. G. (2020). Associations of spousal communication with contraceptive method use among adolescent wives and their husbands in Niger. Plos one, 15(8), e0237512. https://doi.org/10.1371/journal.pone.0237512.
Viewed PDF 698 30

