Table of Contents - Issue
Recent articles
-
 Prevalence of Work-Related Musculoskeletal Disorders among Primary Health Care Workers in Minna, Niger StateAuthor: Otojareri KADOI: 10.21522/TIJPH.2013.11.03.Art001
Prevalence of Work-Related Musculoskeletal Disorders among Primary Health Care Workers in Minna, Niger StateAuthor: Otojareri KADOI: 10.21522/TIJPH.2013.11.03.Art001Prevalence of Work-Related Musculoskeletal Disorders among Primary Health Care Workers in Minna, Niger State
Abstract:
Keywords: Work-related musculoskeletal disorders, Low back pain, prevalence, Healthcare worker, clinicians, primary health care centers, Minna metropolis, Niger State.Prevalence of Work-Related Musculoskeletal Disorders among Primary Health Care Workers in Minna, Niger State
References:
[1] Yassi A. (2000). Work-related musculoskeletal disorders. Curr Opin Rheumatol. 12(2):124-30. doi: 10.1097/00002281-200003000-00006.
[2] Punnett L, Wegman DH. (2004). Work-related musculoskeletal disorders: epidemiologic evidence and the debate. J Electromyography and Kinesio. 14:13-23.
[3] Korhan O, Memon AA. (2019). Work-Related Musculoskeletal Disorders. London: IntechOpen.
[4] Bernard BP. (1997). Musculoskeletal Disorders and Workplace Factors. A Critical Review of Epidemiologic Evidence for Work-Related Musculoskeletal Disorders of the Neck, Upper Extremity, and Low Back. US Department of Health and Human Services. Public Health Service. Centers for Disease Control and Prevention. National Institute for Occupational Safety and Health. Cincinnati. https://doi.org/10.26616/nioshpub97141.
[5] Smith DR, Leggat PA. (2003). Musculoskeletal disorders in nursing. Australian Nursing Journal. 11:1-4.
[6] Mark, G and Smith, A. (2011). Occupational Stress, Job characteristics, Coping & Mental Health of Nurse Practitioners. Journal of Health Psychology.
[7] Yasobant S, Rajkumar P. (2014). Work-related musculoskeletal disorders among health care professionals: A cross-sectional assessment of risk factors in a tertiary hospital, India. Indian J Occup Environ Med. 18(2):75-81. doi.org/10.1177/096032718900800518.
[8] Silverstein B, Clark R. (2004). Interventions to reduce work-related musculoskeletal disorders. J Electromyogr Kinesiol. 4:135-52.
[9] Ries JD. (2018). Rehabilitation for individuals with dementia: facilitating success. Curr Geriatr Rep. 7(11):59–70. doi:10.1007/s13670-018-0237-1.
[10] Ergan M, Başkurt F, Başkurt Z. (2017). The examination of work-related musculoskeletal discomforts and risk factors in veterinarians. Arh Hig Rada Toksikol. 68:198-205. https://doi.org/10.1515/aiht-2017-68-3011.
[11] Rozenfeld V, Ribak J, Danziger J, Tsamir J, Carmeli E. (2009). Prevalence, risk factors and preventive strategies in work-related musculoskeletal disorders among Israeli physical therapists. Physiother Res Int. 15(3):176-84.
[12] Spector JT, Adams D, Silverstein B, (2011). Burden of work-related knee disorders in Washington State, 1999 to 2007. J Occup Environ Med. 53(5):537-547. doi:10.1097/JOM.0b013e31821576ff.
[13] Thomsom, M., Dipsych, B., Mappsych, S. (2006). Psychological determinants of Occupational burnout. Stress medicine, 8(3):151-159.
[14] Ayanniyi O, Lasisi OT, Adegoke BOA, Oni-Orisan MO. (2007) Management of Low Back Pain: - attitudes and treatment preferences of physiotherapists in Nigeria. Afri J. Biomed Res.10:41-49. doi:10.4314/ajbr.v10i1.48970.
[15] Sharma R, Singh R. (2014). Work-related musculoskeletal disorders, job stressors and gender responses in foundry industry. Int J Occup Saf Ergon. 20(2):363-373. doi:10.1080/ 10803548.2014.11077053.
[16] Adegoke BO, Akodu AK, Oyeyemi AL. (2008). Work-related musculoskeletal disorders among Nigerian Physiotherapists. BMC Musculoskelet Disord. 9:112. https://doi.org/10.1186/ 1471-2474-9-112.
[17] WHO Scientific Group on the Burden of Musculoskeletal Conditions at the Start of the New Millennium. (2003). The burden of musculoskeletal conditions at the start of the new millennium. World Health Organ Tech Rep Ser. 919: http://www.ncbi.nlm.nih.gov/pubmed/ 14679827. Accessed July 16, 2022.
[18] Downie R.S., Fyfe C., Tannahill A. (1990). Health Promotion Models and Values. Oxford: Oxford Medical Publications.
[19] World Health Organization (1978). Primary Health Care: Report of the International Conference on Primary Health Care. Geneva: WHO.
[20] Otaru E.O. And Abubakar A.S. (2019). Geospatial Analysis of Primary Healthcare Facilities in Periurban Area of Minna, Niger State, Nigeria. African Scholar Journal of Env. Design & Construction Mgt. 15(4).
[21] Adeyemo, D.O. (2005): Local government and health care delivery in Nigeria in J. Hum Ecol. 149- 160.
[22] Eguagie, I and Okosun, V. (2010). The role of primary health care in Nigeria. Health care delivery systems: problems and prospects. 21:1.
[23] Sprinter, M. K. (2018). Geography of Minna, Published, Abomed Printers, ISBN: 123136723.
[24] Andersson K, Karlehagen S, Jonsson B, (1987). The importance of variations in questionnaire administration, Appl Ergon, 1987, vol. 18 (pg. 229-232).
[25] Kuorinka I, Jonsson B, Kilbom A, et al, (1987). Standardized Nordic questionnaires for the analysis of musculoskeletal symptoms, Appl Ergon,18:(pg. 233-237).
[26] Awosan KJ, Yikawe SS, Oche OM, Oboirien M. (2017). Prevalence, perception, and correlates of low back pain among healthcare workers in tertiary health institutions in Sokoto, Nigeria. Ghana Med J. 51(4):164-174 doi:10.4314/GMJ.V51I4.4.
[27] American Psychiatric Association, (2013). Diagnostic and statistical manual of mental disorders
(5th ed.). Washington, DC, USA: American Psychological Association.[28] Chou R, Qaseem A, Snow V, et al, (2007). Diagnosis and treatment of low back pain: A joint clinical practice guideline from the American college of physicians and the American pain society. Ann Intern Med. 2007; 147:478-491. doi:10.7326/0003-4819-147-7-200710020-00006.
[29] Cho HY, Kim EH, Kim J, (2014). Effects of the core exercise program on pain and active range of motion in patients with chronic low back pain. J Phys Ther Sci. 26(8):1237-40. doi:10.1589/jpts.26.1237.
[30] Fransen K, Cruwys T, Haslam C, et al, (2022). Leading the way together: a cluster randomised controlled trial of the 5r shared leadership program in older adult walking groups. Int J Behav Nutr Phys Act. 19(1):63. doi:10.1186/s12966-022-01297.
Viewed PDF 911 51 -
 Assessment of the Impact of Caregivers Complementary Feeding Knowledge on Undernutrition among Children 6 to 36 Months in Borno State, NigeriaAuthor: Nyeapa YakubuDOI: 10.21522/TIJPH.2013.11.03.Art002
Assessment of the Impact of Caregivers Complementary Feeding Knowledge on Undernutrition among Children 6 to 36 Months in Borno State, NigeriaAuthor: Nyeapa YakubuDOI: 10.21522/TIJPH.2013.11.03.Art002Assessment of the Impact of Caregivers Complementary Feeding Knowledge on Undernutrition among Children 6 to 36 Months in Borno State, Nigeria
Abstract:
This paper is an assessment of the impact of Caregivers complementary feeding Knowledge on undernutrition among children 6-36 Months in Borno state. Large-scale renewables raise new challenges and provide new opportunities across Health systems. The paper considers the barriers faced by health workers and caregivers in Maiduguri Metropolitan Council in providing nutritional services to infants. We review the current state of knowledge in relation to nutrition. This paper then explores key issues in health and nutrition system structure, the main challenges to the uptake of renewables, and the various existing fiscal and policy approaches to encouraging health services. We also highlight possible ways of moving forward to ensure more widespread health management systems.
Keywords: Caregivers, Feed Knowledge. Maiduguri Metropolitan Council, Undernutrition.Assessment of the Impact of Caregivers Complementary Feeding Knowledge on Undernutrition among Children 6 to 36 Months in Borno State, Nigeria
References:
[1] WHO/UNICEF, 2003. Global Strategy for Infant and Young Child Feeding. Geneva: WHO/UNICEF.
[2] Fewtrell M., Bronsky J., Campoy C., Domellöf M., Embleton N., Fidler Mis N., Hojsak I., Hulst J.M., Indrio F., Lapillonne A., et al. Complementary feeding: A position paper by the European Society for Paediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN) Committee on nutrition. J. Pediatr. Gastroenterol. Nutr. 2017; 64:119–132. doi: 10.1097/MPG.0000000000001454. https://pubmed.ncbi.nlm.nih.gov/28027215/, and https://journals.lww.com/jpgn/fulltext/2017/01000/complementary_feeding__a_position_paper_by_the.21.aspx.
[3] Scientific Advisory Committee on Nutrition Feeding in the First Year of Life. [(accessed on 23 April 2020)];2018 Available online: https://www.gov.uk/government/publications/feeding-in-the-first-year-of-life-sacn-report.
[4] United States Department of Agriculture Timing of Introduction of Complementary Foods and Beverage and Developmental Milestones: A Systematic Review. [(accessed on 23 April 2020)]; Available online: https://nesr.usda.gov/sites/default/files/2019-04/Timing%20of%20CFB-Developmental%20Milestones-NE..._0.pdf.
[5] DiMaggio D.M., Cox A., Porto A.F. Updates in infant nutrition. Pediatr. Rev. 2017; 38:449–462. doi: 10.1542/pir.2016-0239. https://pubmed.ncbi.nlm.nih.gov/28972048/, and https://publications.aap.org/pediatricsinreview/article-abstract/38/10/449/32000/Updates-in-Infant-Nutrition?redirectedFrom=fulltext.
[6] Black RE, Victoria CG, Walker SP, Bhutta ZA, Christian P, De Onis M, Ezzati M, Grantham S, Katz J, Martorell R and Uauy R; 2013. Maternal and Child Nutrition and Underweight in Low.
[7] Bakalemwa, R., 2014. Association between malnutrition and feeding practice among children aged six to twenty-four months at Mbagathi District Hospital Kenya. A dissertation submitted to the University of Nairobi.
[8] Hainkens G.T., 2008. Case management HIV infected severe malnourished children: challenges in the area with highest prevalence. The Lancet, 2008, Vol. 371, pp. 13051307.
[9] De Onis, M, Frongillo, E.A. and Blossner, M.I., 2000. Malnutrition Declining? An analysis is in Levels of Child Malnutrition Since 1980. Geneva: Word Health Organization.
[10] National Department of Health 2005: Directorate Nutrition. the integrated nutritional progaramme; nutritional satus. Johannesburg, South Africa.
[11] UNICEF, 2013. The Conceptual Framework on Maternal and Child Nutrition.
[12] Bégin F, Aguayo VM (2017) First foods: Why improving young children's diets matter. Maternal and child nutrition, 13(S2).
[13] Frankenberg E, Buttenheim A, Sikoki B, Suriastini W, (2009) Do women increase their use of reproductive health care when it becomes more available? Evidence from Indonesia. Studies in Family Planning, 40: 27-38.
[14] Bhalotra S, Karlsson M, Nilsson T, (2017) Infant health and longevity: Evidence from a historical intervention in Sweden. JEEA 15: 1101-1157.
[15] Lazuka V (2017) The lasting health and income effects of public health formation in Sweden (No. 153). Department of Economic History, Lund University.
[16] Hjort J, Sølvsten M, Wüst M (2017) Universal investment in infants and long-run health: Evidence from Denmark's 1937 home visiting program. American Economic Journal: Applied Economics 9: 78-104.
[17] Jama NA, Wilford A, Masango Z, Haskins L, Coutsoudis A, et al. (2017) Enablers and barriers to success among mothers planning to exclusively breastfeed for six months: a qualitative prospective cohort study in KwaZulu-Natal, South Africa. Int Breastfeed J 1:12-43.
[18] Samuel FO, Olaolorun FM, Adeniyi JD (2016) A training intervention on child feeding among primary healthcare workers in Ibadan Municipality. Afr J Prim Health Care Fam Med 8:81-86.
[19] Saleem AF, Mahmud S, Baig-Ansari N, Zaidi AK (2014). Impact of maternal education about complementary feeding on their infants' nutritional outcomes in low-and middle-income households: a community-based randomized interventional study in Karachi, Pakistan. J Health Popul Nutr 32: 623.
[20] Inayati DA, Scherbaum V, Purwestri RC, Wirawan NN, Suryantan J, et al. (2012) Improved nutrition knowledge and practice through intensive nutrition education: a study among caregivers of mildly wasted children on Nias Island, Indonesia. Food and nutrition bulletin, 33: 117-127.
[21] Imdad A, Yakoob MY, Bhutta ZA (2011) Impact of maternal education about complementary feeding and provision of complementary foods on child growth in developing countries. BMC public health 11(S25).
[22] Christiana, N-A., 2018.Gaps in knowledge levels of Health Workers on recommended Child feeding practices and Growth Monitoring and Promotion Actions. 2018.
Ivankova, N.V., Cresswell, J. W. & Stick, S. L 2006. Using Mixed Methods Sequential Explanatory Design: From Theory to Practice. Sage Publications, 18(3) 3 - 11. Doi:10.1177/1525822X05282260.Viewed PDF 996 37 -
 Assessing Self-Care Practises of People Living With HIV/AIDS Attending the Antiretroviral Clinic of the University of Abuja Teaching Hospital, NigeriaAuthor: Opeyemi AdebayoDOI: 10.21522/TIJPH.2013.11.03.Art003
Assessing Self-Care Practises of People Living With HIV/AIDS Attending the Antiretroviral Clinic of the University of Abuja Teaching Hospital, NigeriaAuthor: Opeyemi AdebayoDOI: 10.21522/TIJPH.2013.11.03.Art003Assessing Self-Care Practises of People Living With HIV/AIDS Attending the Antiretroviral Clinic of the University of Abuja Teaching Hospital, Nigeria
Abstract:
In pursuance of the Global and National Goals of achieving HIV-AIDS epidemic control, it’s imperative to explore the Promotion of self-care management among people living with HIV/AIDS. Self-care management involves adhering to treatment regimens, good dietary patterns, increased physical exercise, social support, and health-seeking behaviours. The study reviewed five core pillars of self-care management: physical, psychological, emotional, spiritual, and workplace/professional. A cross-sectional descriptive, analytical study with a quantitative approach was conducted at the Antiretroviral Clinic of the University of Abuja Teaching Hospital from October to December 2020. Using random sampling, 372 people living with AIDS participated in the study. Trained research assistants collected data through a structured questionnaire administered at the antiretroviral clinic. The data was analysed using SPSS version 25.0, employing frequencies, computations, percentages, averages, means, standard deviation, and correlations, with a confidence interval of 95%. The study’s findings indicate that the weighted matrix scores (WMS) for various aspects of self-care were significantly above average, suggesting that PLHIV attending the antiretroviral clinic at the University of Abuja Teaching Hospital exhibit good self-care practices. However, psychological and workplace self-care requires some strengthening. The study revealed differences between self-reported appointment adherence and the calculated average appointment gap (3 visits). Associations were found between the average appointment gap and viral load among participants. The study did not establish any significant association between Total Matrixed self-care scores, adherence (appointment gap), or viral load suppression. The COVID epidemic and the nationwide ENDSARS protest in Nigeria during the study period were significant confounders and limitations.
Keywords: Antiretroviral drugs, appointment adherence, HIV/AIDS, psychological health, self-care management.Assessing Self-Care Practises of People Living With HIV/AIDS Attending the Antiretroviral Clinic of the University of Abuja Teaching Hospital, Nigeria
References:
[1] HIV/AIDS. (n.d.). Retrieved April 19, 2021, from https://www.who.int/news-room/fact-sheets/detail/hiv-aids.
[2] WHO | What do we mean by self-care? (2019). WHO.
[3] National AIDS and STI’s Control Programme Federal Ministry of Health. (2016). National Guidelines for HIV Prevention, Treatment and Care 2016 (C. and S. N.-L. E. Dr. Emeka Asadu (Head Treatment, Dr. Chukwuma Anyaike (Head Prevention NASCP), Dr. Isaac Elon (WHO Consultant for the Guidelines Review), Dr. Justus Jiboye (Senior Programme Manager CHAI), Dr. Solomon Odafe (Senior Programme Specialist CDC), Dr. Ikechukwu Amamilo, (Programme Officer CHAI), & Dr. Daniel Adeyinka (Focal Person Paediatric ART NASCP) (Eds.)). Federal Ministry of Health, Abuja, Nigeria. https://aidsfree.usaid.gov/sites/default/files/2016_nigeria_natl_guidelines_hiv_treat_prev.pdf.
[4] Deshpande, A. K., Jadhav, S. K., & Bandivdekar, A. H. (2011). Possible transmission of HIV Infection due to human bite. AIDS Research and Therapy, 8. https://doi.org/10.1186/1742-6405-8-16.
[5] Aids, N. (2018). Rapid_Advice_Art. 1–28. papers://a4f304c0-1221-416b-a5f4-91fa037bb717/Paper/p3699.
[6] WHO | Antiretroviral therapy (ART) coverage among all age groups. (2018). WHO. https://www.who.int/gho/hiv/epidemic_response/ART_text/en/.
[7] Prevention, C. for D. C. and. (2015). HIV/AIDS. https://www.who.int/news-room/fact-sheets/detail/hiv-aids.
[8] Bernell, S., & Howard, S. W. (2016). Use Your Words Carefully: What Is a Chronic Disease? Frontiers in Public Health, 4. https://doi.org/10.3389/fpubh.2016.00159.
[9] Choi, B. C. K., Morrison, H., Wong, T., Wu, J., & Yan, Y. P. (2007). Bringing chronic disease epidemiology and infectious disease epidemiology back together. In Journal of Epidemiology and Community Health (Vol. 61, Issue 9, p. 832). BMJ Publishing Group. https://doi.org/10.1136/jech.2006.057752.
[10] Unwin, N., Jordan, J. A. E., Bonita, R., Ackland, M., Choi, B. C. K., & Puska, P. (2004). Rethinking the terms non-communicable disease and chronic disease [1] (multiple letters). In Journal of Epidemiology and Community Health (Vol. 58, Issue 9, p. 801). BMJ Publishing Group. https://doi.org/10.1136/jech.2003.015040.
[11] Swendeman, D., Ingram, B. L., & Rotheram-Borus, M. J. (2009). Common elements in self-management of HIV and other chronic illnesses: An integrative framework. AIDS Care - Psychological and Socio-Medical Aspects of AIDS/HIV, 21(10), 1321–1334. https://doi.org/10.1080/09540120902803158.
[12] What is Self-Care? - ISF. (n.d.). Retrieved May 22, 2020, from https://isfglobal.org/what-is-self-care/.
[13] Riegel, B., Moser, D. K., Buck, H. G., VaughanDickson, V., B.Dunbar, S., Lee, C. S., Lennie, T. A., Lindenfeld, J. A., Mitchell, J. E., Treat-Jacobson, D. J., & Webber, D. E. (2017). Self-care for the prevention and management of cardiovascular disease and stroke: A scientific statement for healthcare professionals from the American heart association. Journal of the American Heart Association, 6(9). https://doi.org/10.1161/JAHA.117.006997.
[14] Narasimhan, M. (n.d.). WHO Consolidated Guideline on Self-care Interventions for Health Sexual and Reproductive Health and Rights.
[15] Narasimhan, M., Allotey, P., & Hardon, A. (2019). Self-care interventions to advance health and wellbeing: A conceptual framework to inform normative guidance. BMJ (Online), 365. https://doi.org/10.1136/bmj.l688.
[16] Remme, M., Narasimhan, M., Wilson, D., Ali, M., Vijayasingham, L., Ghani, F., & Allotey, P. (2019). Self-care interventions for sexual and reproductive health and rights: Costs, benefits, and financing. BMJ (Online), 365. https://doi.org/10.1136/bmj.l1228.
[17] SELF-CARE INTERVENTIONS FOR HEALTH: SEXUAL & REPRODUCTIVE HEALTH AND RIGHTS Communications Toolkit. (2014). https://apps.who.int/iris/bitstream/hand.
[18] Yamane, T. (1967). 2nd Edition.
[19] Fang-Yu Chou, R. N., & Holzemer, W. L. (2004). Linking HIV/AIDS clients’ self-care with outcomes. Journal of the Association of Nurses in AIDS Care, 15(4), 58–67. https://doi.org/10.1177/1055329003255592.
[20] Chou, F. Y., Holzemer, W. L., Portillo, C. J., & Slaughter, R. (2004). Self-care strategies and sources of information for HIV/AIDS symptom management. Nursing Research, 53(5), 332–339. https://doi.org/10.1097/00006199-200409000-00008.
[21] Nokes, K. M., & Nwakeze, P. C. (2005). Assessing self-management information needs of persons living with HIV/AIDS. AIDS Patient Care and STDs, 19(9), 607–613. https://doi.org/10.1089/apc.2005.19.607.
[22] Chou, F. Y. (2004). Testing a Predictive Model of the Use of HIV/AIDS Symptom Self-Care Strategies. AIDS Patient Care and STDs, 18(2), 109–117. https://doi.org/10.1089/108729104322802533.
[23] Okoronkwo, I. (2015). Assessing Self Care Practices of People Living with AIDS attending antiretroviral clinic Kafanchan, Kaduna State, Nigeria. Journal of AIDS & Clinical Research, 06(12). https://doi.org/10.4172/2155-6113.1000528.
[24] Determining Sample Size Degree of Variability. (n.d.).Onyango, A. C., Walingo, M. K., Mbagaya, G., & Kakai, R. (2012). Assessing nutrient intake and nutrient status of HIV seropositive patients attending clinic at Chulaimbo sub-district Hospital, Kenya. Journal of Nutrition and Metabolism, 2012. https://doi.org/10.1155/2012/306530.
Viewed PDF 861 27 -
 Role of Helper, Cytotoxic T-cells and Interleukin-6 amongst Chronic Obstructive Pulmonary Disease Patients Post Exposure to Tobacco or Tuberculosis in Yaoundé CameroonAuthor: Yayah Emerencia NgahDOI: 10.21522/TIJPH.2013.11.03.Art004
Role of Helper, Cytotoxic T-cells and Interleukin-6 amongst Chronic Obstructive Pulmonary Disease Patients Post Exposure to Tobacco or Tuberculosis in Yaoundé CameroonAuthor: Yayah Emerencia NgahDOI: 10.21522/TIJPH.2013.11.03.Art004Role of Helper, Cytotoxic T-cells and Interleukin-6 amongst Chronic Obstructive Pulmonary Disease Patients Post Exposure to Tobacco or Tuberculosis in Yaoundé Cameroon
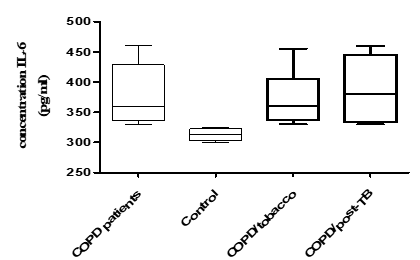
Abstract:
The pro-inflammatory cytokine Interleukin-6 (IL-6) –and T- T-cells play a major role in the pathogenesis and prognosis of many respiratory tract infections. Our study aimed to evaluate the role of T-Lymphocyte and IL-6 in Chronic Obstructive Pulmonary Disease (COPD) patients post-exposure to Tobacco or Tuberculosis. A cross-sectional prospective study was carried out from February 2021 to July 2022. Participants were enrolled at the Yaoundé Jamot Hospital. The intervention group comprised patients with post-TB/AFO (Tuberculosis/Airflow obstruction) and those with COPD related to tobacco, healthy subjects served as control. Spirometry results were obtained from the medical records. T-lymphocyte and IL-6 concentrations were measured by flow cytometry and ELISA (Enzyme-linked immunosorbent Assay) respectively. 150 participants were enrolled, 90 COPD patients and 60 healthy people. The COPD patients consisted of 50 with a history of smoking (COPD/tobacco) and 40 with a history of tuberculosis (post-TB/AFO). The level of IL-6 and CD4 cells (cluster differentiation) was higher in COPD patients compared to the control group (p-value 0.0001 and 0.0006 respectively). CD8 counts were higher in COPD/tobacco than in post-TB/AFO (p = 0.0043). IL-6 and CD4 were not statistically different between COPD/tobacco and post-TB/AFO. There was an inverse and non-significant correlation between IL-6 and CD8; and a non-significant positive correlation between IL-6 and CD4 with r = -0335, p = 0.087; R = 0.355; P = 0.069 respectively. IL-6 and CD8 T cells are involved in the pathogenesis of both COPD related to tobacco and post-TB airflow obstruction, with higher counts of blood CD8 cells in COPD/tobacco.
Keywords: COPD, Inflammation, IL-6, T-lymphocyte, Tobacco, Tuberculosis.Role of Helper, Cytotoxic T-cells and Interleukin-6 amongst Chronic Obstructive Pulmonary Disease Patients Post Exposure to Tobacco or Tuberculosis in Yaoundé Cameroon
References:
[1] Daniel Lange, Casey E Ciavaglia, J Alberto Neder, Katherine A., Webb, and Denis E O’Donnell. Lung hyperinflation in chronic obstructive pulmonary disease: mechanisms, clinical implications, and treatment. 10.1586/17476348.2014.949676 2014 Informa UK Ltd ISSN 1747-6348.
[2] GOLD: Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. 2019. http://goldcopd.org/wp-content/uploads Accessed 10 April 2020.
[3] Roche N., Huchon G. Epidemiology of chronic obstructive pulmonary disease. Rev Prat., 2004, 54, 1408-1413.
[4] Pefura-Yone EW, Kengne AP, Tagne-Kamdem PE, Afane-Ze E. Clinical significance of low forced expiratory flow between 25% and 75% of vital capacity following treated pulmonary tuberculosis: a cross-sectional study. BMJ Open 2014; 4: e005361.
[5] Dina S., Shyamala G., Adam T.C., Meldrum C.A., Raja M., Adam M. G., Jeffrey L. C., Fernando J. M., Hershenson M.B., Umadevi S. Increased Cytokine Response of Rhinovirus-infected Airway Epithelial Cells in Chronic Obstructive Pulmonary Disease. Am J Respir Crit Care Med Vol 182. pp 332–340, 2010 DOI: 10.1164/rccm.200911-1673OC on April 15, 2010.
[6] Buist S. MD: Global Burden of COPD: risk factors, prevalence and future trends. the lancet 2007, 370:765-773.
[7] Gadgil A., Duncan S.R. Role of T-lymphocytes and pro-inflammatory mediators in the pathogenesis of chronic obstructive pulmonary disease. International Journal of COPD 2008:3(4) 531–541.
[8] Guiedem Elise, Mondinde Ikomey George, Nkenfou Céline, Pefura‑Yone Eric Walter, Mesembe Martha, Chegou Njweipi Novel, Graeme Brendon Jacobs, Okomo Assoumou Marie Claire. Chronic obstructive pulmonary disease (COPD): neutrophils, macrophages, and lymphocytes in patients with anterior tuberculosis compared to tobacco-related COPD. BMC Res Notes. 2018 ; 11 :192.
[9] Grubek-Jaworska H., Paplinska M., Hermanowiecz-Salamon J., Bialek-Gosk K., Dabrowska M., Grabczak E. IL-6 and IL-13 in induced sputum, of COPD and Asthma patients: correlation with respiratory tests. Respiration, 2012, 84(2), 7-101.
[10] Celli B., Locantore N., Yates J., Tal-Singer R., Miller B., Bakke P. Inflammatory biomarkers improve clinical prediction of mortality in chronic obstructive pulmonary diseases. Am J respir crit care Med., 185, 72-106572.
[11] Suleyman S.H., Hakan G., Levent C.M., Aysun B.K., Ismail T. Association between cytokines in induced sputum and severity of chronic obstructive pulmonary disease. 0954-6111. doi: 10.1016/j.rmed.2005.08.022.
[12] Hurst J.R., Perera W.R., Wilkinson T.M., Donaldson G.C., Wedzicha J.A. Systemic and upper and lower airway inflammation at exacerbation of chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2006; 173: 71-78
[13] Mallia P, Message SD, Contoli M, et al. Lymphocyte subsets in experimental rhinovirus infection in chronic obstructive pulmonary disease. Respir Med. 2014 ;108(1)78-85. doi: http://dx.doi.org/10.1016/j.rmed.2013.09.010.
[14] Gadgil A., Zhu X., Sciurba F., Ducan S. altered T-cell phenotypes in chronic obstructive pulmonary disease. Proc Am Thorac Soc. 2006; 3:487–8.
[15] Mikhak Z, Farsidjani A, Luster AD. Endotoxin augmented antigen induced Th1 cell trafficking amplifies airway neutrophilic inflammation. J Immunol. 2009; 182(12): 7946-7956. doi: http://dx.doi.org/10.4049/jimmunol.0803522.
[16] Mustimbo E.P, Higgs BW, Brohawn P, Brohawn, Pilataxi F., Xiang G., Kuziora M., Bowler R.P., White W.I. CD4+ T-cell profiles and peripheral blood ex-vivo responses to T-cell directed stimulation delineate COPD phenotypes. J COPD F. 2(4): 268-280. doi: http://dx.doi.org/10.15326/jcopdf.2.4.2015.0131.
[17] Roberts MEP, Higgs BW, Brohawn P, et al. CD4+ T-cell profiles and peripheral blood ex-vivo responses to T-cell directed stimulation delineate COPD phenotypes. J COPD F. 2(4): 268-280.
[18] Dienz O., Eaton S., Bond J., Neveu W., Moquin D., Noubade R. The induction of antibody production by IL-6 is indirectly mediated by IL-12 produced by CD4+ T cells. J Exp Med., 2009, 206, 69-78.
[19] Dina S., Shyamala G., Adam T.C., Meldrum C.A., Raja M., Adam M. G., Jeffrey L. C., Fernando J. M., Hershenson M.B., Umadevi S. Increased
Cytokine Response of Rhinovirus-infected Airway Epithelial Cells in Chronic Obstructive Pulmonary Disease. Am J Respir Crit Care Med Vol 182. pp 332–340, 2010 DOI: 10.1164/rccm.200911-1673OC.[20] Aubier M., Marthan R., Berger P., Chambellan A., Chanez P., Aguilaniu B. BPCO et Inflammation : mise au point par un groupe d’experts. Les mécanismes de l’inflammation et du remodelage. 0761-8425/S. doi : 10.1016/j.rmr.2010.10.004.
[21] Perez T., Mal H., Aguilaniu B., Brillet P.Y., Chaouat A., Louis R., Muir, J.-F. et al. BPCO et inflammation : mise au point d’un groupe d’experts. Les phénotypes en lien avec l’inflammation. 2010, 10.1016/j.rmr.
Viewed PDF 841 48 -
 Properties of Natural Materials as Alternative to Nylon Bristles – An Exploratory Study for Reduction of Polymer UsageAuthor: Murukesan SDOI: 10.21522/TIJPH.2013.11.03.Art005
Properties of Natural Materials as Alternative to Nylon Bristles – An Exploratory Study for Reduction of Polymer UsageAuthor: Murukesan SDOI: 10.21522/TIJPH.2013.11.03.Art005Properties of Natural Materials as Alternative to Nylon Bristles – An Exploratory Study for Reduction of Polymer Usage
Abstract:
Background: Nylon bristles are the most commonly used type of bristle in toothbrushes, but they have both advantages and disadvantages. Nylon bristles can be too hard or abrasive for some people's teeth and gums. Nylon is not biodegradable and can harbor bacteria if not cleaned properly. Aims: In order to explore the possibility of using natural fibers this study was conducted. Materials and Methods: Twigs of neem, banyan, babool and miswak were purchased as fresh twigs, wiped clean, hammered on a hard wood base to obtain fibers of desired lengths. Physical appearance, Bend Recovery, Folding Endurance and Antibacterial adhesion against B. Subtilis were evaluated. All experiments were performed as triplicate and mean and standard deviation were reported. Results: Digital microscopy showed well defined fibers of fairly constant diameter, apparent from the superimposed scale. Results of bend recovery analysis showed that miswak fibers were flexible and recovery was good. Folding Endurance test showed miswak and banyan were having great folding endurance. Bacterial adhesion with B. Subtilis was heavy in all fibres. The antibacterial activity of four extracts showed that all groups had identifiable antimicrobial activity at 2000 µg concentrations. Conclusion: From results of the study, it can be inferred that miswak is the most suitable material to be used for fabricating bristles in its native form.
Keywords: Babool, Banyan, Bristles, Natural Fibres; Neem Miswak.Properties of Natural Materials as Alternative to Nylon Bristles – An Exploratory Study for Reduction of Polymer Usage
References:
[1] ADA.org. (2012, November 12). Toothbrushes – American Dental Association. https://www.ada.org/en/resources/research/science-and-research-institute/oral-health-topics/toothbrushes.
[2] Plastic toothbrush – Design life. (2023, June 15). http://www.designlife-cycle.com/plastic-toothbrush#:~:text=The%20materials%20that%20are%20used,the%20main%20material%20of%20bristles.
[3] Phillips, R. W., & Swartz, M. L., 1953, Effects of diameter of nylon bristles on enamel surface. Journal of the American Dental Association, 47(1), 20–26.
[4] Rajeswaran, S. A., & Sankari Malaiappan, D. J. AS SG.,2021, A Comparative Study on the efficacy of plaque removal of three natural toothbrushes-an in-vitro study. NVEO-natural volatiles and essential oils Journal, 6054–6069.
[5] Offsets, C. Calculator CF. Biodegradable bamboo toothbrush: Greenwashing or eco-friendly?
[6] Assari, A. S., Mohammed Mahrous, M., Ahmad, Y. A., Alotaibi, F., Alshammari, M., AlTurki, F., & AlShammari, T., 2022, Efficacy of different sterilization techniques for toothbrush decontamination: An ex vivo study. Cureus, 14(1), e21117.
[7] E. I. du Pont de Nemours, 1979, Stiffness: Folding endurance test. Bend recovery of TYNEX® and HEROX® nylon filaments, technical data Bulletin No. 5. Plastics Department.
[8] Nair, A. B., Kumria, R., Harsha, S., Attimarad, M., Al-Dhubiab, B. E., & Alhaider, I. A., 2013, In vitro techniques to evaluate buccal films. Journal of Controlled Release, 166(1), 10–21.
[9] Khan, G., Yadav, S. K., Patel, R. R., Nath, G., Bansal, M., & Mishra, B., 2016, Development and evaluation of biodegradable chitosan films of metronidazole and levofloxacin for the management of periodontitis. AAPS PharmSciTech, 17(6), 1312–1325.
[10] Carranza, F. A., 2003, Clinical periodontology (9th ed). Saunders.
[11] Wilkins, E. M., McCullough, P. A., 1999, Clinical practice of the dental hygienist (3rd ed). Lea & Febiger.
[12] Bass, C. C. (1948). The optimum characteristics of toothbrushes for personal oral hygiene. Dental Items of Interest, 70(7), 697–718.
[13] Hine, M. (1956). The toothbrush. International Dental Journal. Google Scholar, 6, 15–25.
[14] Kumar, S., Kumari, M., Acharya, S., & Prasad, R., 2014, Comparison of surface abrasion produced on the enamel surface by a standard dentifrice using three different toothbrush bristle designs: A profilometric in vitro study. Journal of Conservative Dentistry, 17(4), 369–373.
[15] Nur Diyana, A. F., Khalina, A., Sapuan, M. S., Lee, C. H., Aisyah, H. A., Nurazzi, M. N., & Ayu, R. S., 2022, Physical, mechanical, and thermal properties and characterization of natural fiber composites reinforced poly (lactic acid): Miswak (Salvadora persica L.) fibers. International Journal of Polymer Science, 2022, 1–20.
[16] Thandavamoorthy, R., & Palanivel, A., 2020, Testing and evaluation of tensile and impact strength of neem/banyan fiber-reinforced hybrid composite. Journal of Testing and Evaluation, 48(1), 647–655.
[17] Mrudhula, R., Dinesh Sankar Reddy, P., & Veeresh Kumar, G. B., 2023, Preparation of cellulose nanofibers (CNFs) from Cajanus cajan (pigeon pea) and Acacia arabica (babul plant). In Recent trends in product design and intelligent manufacturing systems (pp. 429–438). Springer Nature Singapore.
[18] Al-Bayati, F. A., & Sulaiman, K. D., 2008, In vitro antimicrobial activity of Salvadora persica L. extracts against some isolated oral pathogens in Iraq. Turkish Journal of Biology, 32, 57–62.
[19] Sofrata, A. H., Claesson, R. L., Lingström, P. K., & Gustafsson, A. K., 2008, Strong antibacterial effect of miswak against oral microorganisms associated with periodontitis and caries. Journal of Periodontology, 79(8), 1474–1479.
[20] Almas, K., & Al-Zeid, Z., 2004, The immediate antimicrobial effect of a toothbrush and miswak on cariogenic bacteria: a clinical study. The Journal of Contemporary Dental Practice, 5(1), 105–114.
[21] Elangovan, A., Muranga, J., & Joseph, E., 2012, Comparative evaluation of the antimicrobial efficacy of four chewing sticks commonly used in South India: An in vitro study. Indian Journal of Dental Research, 23(6), 840.
[22] Norton, M. R., & Addy, M., 1989, Chewing sticks versus toothbrushes in West Africa. A pilot study. Clinical Preventive Dentistry, 11(3), 11–13.
[23] Gazi, M., Saini, T., Ashri, N., & Lambourne, A., 1990, Meswak chewing stick versus conventional toothbrush as an oral hygiene aid. Clinical Preventive Dentistry, 12(4), 19–23.
[24] Al-Otaibi, M., Al-Harthy, M., Söder, B., Gustafsson, A., & Angmar-Månsson, B., 2003, Comparative effect of chewing sticks and tooth brushing on plaque removal and gingival health. Oral Health and Preventive Dentistry, 1(4), 301–307.
Viewed PDF 1052 49 -
 Analysis of Quality and Quantity of Complementary Feeding and Nutrition among Children of 6 to 36 Months in Maiduguri Metropolitan Council, Borno State, NigeriaAuthor: Nyeapa YakubuDOI: 10.21522/TIJPH.2013.11.03.Art006
Analysis of Quality and Quantity of Complementary Feeding and Nutrition among Children of 6 to 36 Months in Maiduguri Metropolitan Council, Borno State, NigeriaAuthor: Nyeapa YakubuDOI: 10.21522/TIJPH.2013.11.03.Art006Analysis of Quality and Quantity of Complementary Feeding and Nutrition among Children of 6 to 36 Months in Maiduguri Metropolitan Council, Borno State, Nigeria
Abstract:
This paper provides a cross sectional analysis of the quality and quantity of complimentary feeding and nutrition among children of 6-36 months in Maiduguri Metropolitan Council. The role of health workers and parents in contextualities in driving, constraining or otherwise influencing complimentary feeding practices is explored through a review of the essential literature. Though this literature is found to have considerably expanded the scope of understanding around health and nutrition, research in the area is found to be lacking in methodological coherence and theoretical substance. Future efforts are needed to systematically bring together the array of insights, methodological approaches, and recommendations in this literature, as well as better bound, differentiate and systemize health and nutrition research in the area going forward. Two initial objectives are advanced through this paper in relation to this dual research imperative. They employed the survey research method. It revealed that knowledge of complementary feeding amongst women in emergencies are poor and government need to scale up support through local enlightenment programs that will boost good health and nutritional practices.
Keywords: Complementary Feeding, Nutrition, Quality of complimentary feeding, Maiduguri Metropolitan Council, Nigeria.Analysis of Quality and Quantity of Complementary Feeding and Nutrition among Children of 6 to 36 Months in Maiduguri Metropolitan Council, Borno State, Nigeria
References:
[1] Black RE, Victoria CG, Walker SP, Bhutta ZA, Christian P, De Onis M, Ezzati M, Grantham S, Katz J, Martorell R and Uauy R; .2013. Maternal and Child Nutrition and Underweight in Low-Income Countries.
[2] Global Nutrition Report 2008. Shining a light to spur action on nutrition. Retrieved from https://globalnutritionreport.org/reports/global-nutrition-report-2018/.
[3] Saha KK, Persson L, Rasmussen KM, Arifeen SE, Frongillo EA, et al. 2008. Appropriate infant feeding practices result in better growth of infants and young children in rural Bangladesh. Am J ClinNutr. 2008; 87: 1852-1859. Ref.: https://goo.gl/BhETH9.
[4] Pelto G.H., 2000. Improving Complementary Feeding Practices Responsive Parenting as a Primary Component Of Intervention To Prevent Malnutrition In Infancy and Early Childhood. Pediatrics. 2000; 106: 1300-1301. Ref.: https://goo.gl/rH6JHw.
[5] Müller O, Krawinkel M., 2005. Malnutrition and health in developing countries. CMAJ. 2005 173: 279-86. Ref.: https://goo.gl/SrR5Eb.
[6] Chesire EJ, Orago AS, Oteba LP, Echoka E, 2008. Determinants of under nutrition among school age children in a Nairobi peri-urban slum. East Afr Med J. 2008;85(10):471–9.
[7] UNICEF, WHO, World Bank Group. Levels and trends in child malnutrition. New York. The World Bank Joint Child Malnutrition Estimates; 2015.
[8] Munthali T, Jacobs C, Sitali L, Dambe R, Michelo C (2015). Mortality and morbidity patterns in under-five children with severe acute malnutrition (SAM) in Zambia: a five-year retrospective review of hospital-based records (2009-2013). Arch Public Health. 2015;73(1):146. doi:10.1186/s13690-015-0072-1.
[9] NDHS: 2013; National Population Commission (NPC) (Nigeria) and ICF International. (2014). Nigeria Demographic and Health Survey 2013. Abuja, Nigeria, and Rockville, Maryland, USA: NPC and ICF International. Retrieved from https://dhsprogram.com/pubs/pdf/fr293/fr293.pdf.
[10] NDHS: 2018: National Population Commission (NPC) (Nigeria) and ICF (2019). Nigeria Demographic and Health Survey 2018. Abuja, Nigeria and Rockville, Maryland, USA: NPC and ICF. Retrieved from https://dhsprogram.com/pubs/pdf/fr359/fr359.pdf.
[11] Multiple Indicator Cluster Survey 2016 – 2017.
[12] Aggarwal A., Verman, S., Faridi, M & Dayachand 92008). Complementary feeding – reasons for inappropriateness in timing, quantity, and consistency. Indian Journal of Pediatrics 75 (1): 49 – 53.
[13] World Health Organisation, Children: reducing mortality. Fact sheet. [Accessed November 30, 2016] http://www.who.int.mediacentre/factshetts/fs178/en/.
[14] World Health Organization Infant and young child feeding. 2016. [Accessed March 31st, 2016] http://who.int/mediacentre/factsheets/fs342/en/.
[15] WHO (2013). Essential Nutrition Actions: Mainstreaming Nutrition through the Life-Course. World Health Organization. Retrieved from https://apps.who.int/iris/bitstream/handle/10665/84409/9789241505550_eng.pdf?sequence=1.
[16] WHO 2003. Global Strategy for Infant and Young Child Feeding. World Health Organization. Retrieved from https://www.who.int/nutrition/topics/global_strategy/en/.
[17] Zere, E., and Mcintyre D. 2003. Inequities in under-five child malnutrition South Africa. International Journal for Equity in Health, 2(1), 7. https://doi.org/10.1186/1475-9276-2-7.
[18] World Health Organization: Standards for Maternal and Neonatal Care 2006.
[19] Victora CG, de Onis M, Hallal PC, Blossner M and Shrimpton R. 2010. Worldwide timing of growth faltering: revisiting implications for interventions. Pediatrics. 2010;125(3):473-480.
[20] Moore AC, Akhter S, Aboud FE. 2006. Responsive complementary feeding in rural Bangladesh. Soc Sci Med. 2006;62(8):1917-1930.
[21] Ivankova, N.V., Cresswell, J. W. & Stick, S. L 2006. Using Mixed Methods Sequential Explanatory Design: From Theory to Practice. Sage Publications, 18(3) 3 - 11. Doi:10.1177/1525822X05282260.
Viewed PDF 6480 60 -
 Telehealth Utilisation in HIV Care Services in Harare, Zimbabwe: Awareness and Acceptability among Healthcare WorkersAuthor: Stanford ChigaroDOI: 10.21522/TIJPH.2013.11.03.Art007
Telehealth Utilisation in HIV Care Services in Harare, Zimbabwe: Awareness and Acceptability among Healthcare WorkersAuthor: Stanford ChigaroDOI: 10.21522/TIJPH.2013.11.03.Art007Telehealth Utilisation in HIV Care Services in Harare, Zimbabwe: Awareness and Acceptability among Healthcare Workers
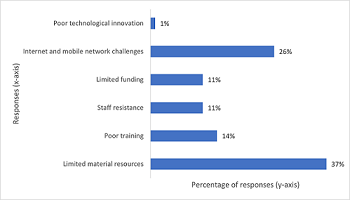
Abstract:
Access to healthcare in developing countries is generally poor due to limited health facilities and shortage of healthcare workers. Recent developments in technology and telehealth promise to address challenges of access to health facilities through remote service provision. However, the level of awareness and acceptability of telehealth in HIV care among healthcare workers in Zimbabwe is not well known. The main objective of this study is to assess the level of awareness and acceptability of telehealth among healthcare workers involved in HIV care in Harare, Zimbabwe. A cross-sectional survey was employed to conveniently sample and interview 395 healthcare workers from 15 public healthcare facilities and 34 private healthcare facilities in Harare. A pretested questionnaire was employed to collect data. Logistic regression analysis was carried out to establish possible association of the independent variable and dependent variables (awareness and acceptance). All statistical analyses were performed using SPSS software version 28.0.1.1. Of the 395 healthcare workers interviewed, 87% were aware of telehealth, while 85% found it acceptable. Logistic regression analysis identified educational level, and type of profession to be significantly (p < 0.05) associated with telehealth awareness. There was an association between telehealth acceptance and level of education (p < 0.05). Lack of resources was a major barrier to telehealth utilisation. The findings of this study reveal high awareness and acceptability of telehealth in HIV care among healthcare workers in Harare. The findings provide optimism for telehealth uptake and the promotion of telehealth as an important intervention in HIV care.
Keywords: Acceptability, Awareness, HIV care, Telehealth.Telehealth Utilisation in HIV Care Services in Harare, Zimbabwe: Awareness and Acceptability among Healthcare Workers
References:
[1] World Health Organization. (n.d.). Social determinants of health. Retrieved 3 August 2022, from https://www.who.int/health-topics/social-determinants-of-health#tab=tab_1.
[2] Loewenson, R., & Masotya, M. (2018). Equity Watch: Assessing progress towards equity in health in Zimbabwe, 2018 Training and Research Support Centre, Regional Network for Equity in Health in East and Southern Africa (EQUINET). https://www.tarsc.org/publications/documents/Zim%20equitywatch%2009.pdf.
[3] Mangundu, M., Roets, L., & Van Rensberg, E. J. (2020). Accessibility of healthcare in rural Zimbabwe: The perspective of nurses and healthcare users. African Journal of Primary Health Care & Family Medicine, 12(1). https://doi.org/10.4102/phcfm.v12i1.2245.
[4] Tessema, Z. T., Worku, M. G., Tesema, G. A., Alamneh, T. S., Teshale, A. B., Yeshaw, Y., Alem, A. Z., Ayalew, H. G., & Liyew, A. M. (2022). Determinants of accessing healthcare in Sub-Saharan Africa: A mixed-effect analysis of recent Demographic and Health Surveys from 36 countries. BMJ Open, 12(1), e054397. https://doi.org/10.1136/bmjopen-2021-054397.
[5] Oleribe, O. E., Momoh, J., Uzochukwu, B. S., Mbofana, F., Adebiyi, A., Barbera, T., Williams, R., & Taylor Robinson, S. D. (2019). Identifying Key Challenges Facing Healthcare Systems In Africa And Potential Solutions. International Journal of General Medicine, Volume 12, 395–403. https://doi.org/10.2147/IJGM.S223882.
[6] Druetz, T. (2018). Integrated primary health care in low- and middle-income countries: A double challenge. BMC Medical Ethics, 19(S1), 48. https://doi.org/10.1186/s12910-018-0288-z.
[7] Tafuma, T. A., Mahachi, N., Dziwa, C., Moga, T., Baloyi, P., Muyambo, G., Muchedzi, A., Chimbidzikai, T., Ncube, G., Murungu, J., Nyagura, T., & Lew, K. (2018). Barriers to HIV service utilisation by people living with HIV in two provinces of Zimbabwe: Results from 2016 baseline assessment. Southern African Journal of HIV Medicine, 19(1), 721. https://doi.org/10.4102/hivmed.v19i1.721.
[8] Keesara, S., Jonas, A., & Schulman, K. (2020). Covid-19 and Health Care’s Digital Revolution. New England Journal of Medicine, 382(23), e82. https://doi.org/10.1056/NEJMp2005835.
[9] Health Resources and Services Administration. (2020). Glossary. https://bhw.hrsa.gov/glossary#t.
[10] Lurie, N., & Carr, B. G. (2018). The Role of Telehealth in the Medical Response to Disasters. JAMA Internal Medicine, 178(6), 745. https://doi.org/10.1001/jamainternmed.2018.1314.
[11] Miyawaki, A., Tabuchi, T., Ong, M. K., & Tsugawa, Y. (2021). Age and Social Disparities in the Use of Telemedicine During the COVID-19 Pandemic in Japan: Cross-sectional Study. Journal of Medical Internet Research, 23(7), e27982. https://doi.org/10.2196/27982.
[12] Williams, C., & Shang, D. (2023). Telehealth Usage Among Low-Income Racial and Ethnic Minority Populations During the COVID-19 Pandemic: Retrospective Observational Study. Journal of Medical Internet Research, 25, e43604. https://doi.org/10.2196/43604.
[13] Fouad, A. A., Osman, M. A., Abdelmonaem, Y. M. M., & Karim, N. A. H. A. (2023). Awareness, knowledge, attitude, and skills of telemedicine among mental healthcare providers. Middle East Current Psychiatry, 30(1), 5. https://doi.org/10.1186/s43045-022-00272-3.
[14] Ammenwerth, E. (2019). Technology Acceptance Models in Health Informatics: TAM and UTAUT. Studies in Health Technology and Informatics, 263, 64–71. https://doi.org/10.3233/SHTI190111.
[15] Venkatesh, Morris, Davis, & Davis. (2003). User Acceptance of Information Technology: Toward a Unified View. MIS Quarterly, 27(3), 425. https://doi.org/10.2307/30036540.
[16] López-Cabarcos, M. Á., Piñeiro-Chousa, J., & Quiñoá-Piñeiro, L. (2021). An approach to a country’s innovation considering cultural, economic, and social conditions. Economic Research-Ekonomska Istraživanja, 34(1), 2747–2766. https://doi.org/10.1080/1331677X.2020.1838314.
[17] Chitungo, I., Mhango, M., Mbunge, E., Dzobo, M., Musuka, G., & Dzinamarira, T. (2021). Utility of telemedicine in sub‐Saharan Africa during the COVID ‐19 pandemic. A rapid review. Human Behavior and Emerging Technologies, 3(5), 843–853. https://doi.org/10.1002/hbe2.297.
[18] Furusa, S. S., & Coleman, A. (2018). Factors influencing e-health implementation by medical doctors in public hospitals in Zimbabwe. SA Journal of Information Management, 20(1). https://doi.org/10.4102/sajim.v20i1.928.
[19] International Center for AIDS Care and Treatment Program (2020). Zimbabwe population-based HIV impact assessment. https://phia.icap.columbia.edu/zimbabwe2020-final-report/
[20] Banya, N. (2018). Zimbabwe’s health delivery system. ZimFact. https://zimfact.org/factsheet-zimbabwes-health-delivery-system/.
[21] Raosoft. (2004). Sample Size Calculator. http://www.raosoft.com/samplesize.html.
[22] Mugarisi, V. (2022). Zimbabwe conducts health labour market analysis. World Health Organization. https://www.afro.who.int/countries/zimbabwe/news/zimbabwe-conducts-health-labour-market-analysis.
[23] Gurupur, V. P., & Wan, T. T. H. (2017). Challenges in implementing mHealth interventions: A technical perspective. MHealth, 3, 32–32. https://doi.org/10.21037/mhealth.2017.07.05.
[24] Ministry of Child and Child Care. (n.d.). National Health Strategy 2020-2025 on the cards. Retrieved 3 September 2023, from http://www.mohcc.gov.zw/index.php?option=com_content&view=article&id=343:national-health-strategy-2020-2025-on-the-.
[25] Naqvi, S. Z., Ahmad, S., Rocha, I. C., Ramos, K. G., Javed, H., Yasin, F., Khan, H. D., Farid, S., Mohsin, A., & Idrees, A. (2022). Healthcare Workers’ Knowledge and Attitude Toward Telemedicine During the COVID-19 Pandemic: A Global Survey. Cureus. https://doi.org/10.7759/cureus.30079.
[26] Elhadi, M., Elhadi, A., Bouhuwaish, A., Bin Alshiteewi, F., Elmabrouk, A., Alsuyihili, A., Alhashimi, A., Khel, S., Elgherwi, A., Alsoufi, A., Albakoush, A., & Abdulmalik, A. (2021). Telemedicine Awareness, Knowledge, Attitude, and Skills of Health Care Workers in a Low-Resource Country During the COVID-19 Pandemic: Cross-sectional Study. Journal of Medical Internet Research, 23(2), e20812. https://doi.org/10.2196/20812.
[27] Ayatollahi, H., Sarabi, F. Z. P., & Langarizadeh, M. (2015). Clinicians’ Knowledge and Perception of Telemedicine Technology. Perspectives in Health Information Management, 12(Fall), 1c.
[28] Renu, N. (2021). Technological advancement in the era of COVID-19. SAGE Open Medicine, 9, 205031212110009. https://doi.org/10.1177/20503121211000912.
[29] Mahtta, D., Daher, M., Lee, M. T., Sayani, S., Shishehbor, M., & Virani, S. S. (2021). Promise and Perils of Telehealth in the Current Era. Current Cardiology Reports, 23(9), 115. https://doi.org/10.1007/s11886-021-01544-w.
[30] Yaghobian, S., Ohannessian, R., Iampetro, T., Riom, I., Salles, N., De Bustos, E. M., Moulin, T., & Mathieu-Fritz, A. (2022). Knowledge, attitudes and practices of telemedicine education and training of French medical students and residents. Journal of Telemedicine and Telecare, 28(4), 248–257. https://doi.org/10.1177/1357633X20926829.
[31] Ncube, B., Mars, M., & Scott, R. E. (2023). Perceptions and attitudes of patients and healthcare workers towards the use of telemedicine in Botswana: An exploratory study. PLOS ONE, 18(2), e0281754. https://doi.org/10.1371/journal.pone.0281754.
Viewed PDF 1016 47 -
 Assessing the Availability and Utilisation of Adolescent Reproductive Health Services in Northern Region of GhanaAuthor: Abdul-Malik AbdulaiDOI: 10.21522/TIJPH.2013.11.03.Art008
Assessing the Availability and Utilisation of Adolescent Reproductive Health Services in Northern Region of GhanaAuthor: Abdul-Malik AbdulaiDOI: 10.21522/TIJPH.2013.11.03.Art008Assessing the Availability and Utilisation of Adolescent Reproductive Health Services in Northern Region of Ghana
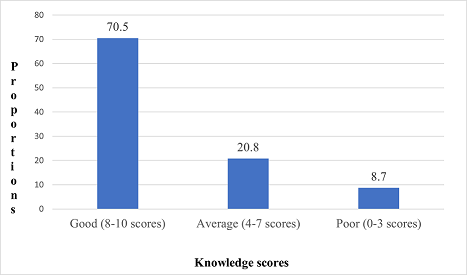
Abstract:
Youth-friendly sexual and reproductive health services involved range of Sexual and Reproductive Health services that are delivered to the specific needs, vulnerabilities, and desires of young people. This study aims to determine the availability and utilization of adolescent sexual and reproductive health services among youths in selected districts and municipalities in the Northern Region of Ghana. A descriptive cross-sectional study design was conducted in four selected districts using a mixed method of quantitative and qualitative approaches to data collections. Both male and female adolescent and young person aged 10-24 years were selected by simple random sampling through balloting. Convenient sampling was used to select four health workers for interviews. Quantitative data was analysed using descriptive and inferential statistics, and qualitative analysis was done using manual thematic analysis. The qualitative data was collected using an unstructured interview guide and analysed with thematic analysis. Findings showed average age was 16.64 years, and 70.5% had good knowledge score of SRH services availability. Types of SRH services provided include counselling and education on SRH issues, STIs screening, diagnosis, and management. About 69.8% have ever visited the health facilities for SRH service, and 36.1% covered more than an hour before accessing SRH services. About 21% had access contraceptives and family planning services. Barriers to accessing SRH services were attributed to; cost of healthcare (21.9%), long queues at facilities (15.3%), and distance to healthcare facility (12.4%). Associated factors were sex (OR = 1.72; 95%CI 1.16-2.57; p = 0.007), father educational attainment (OR = 2.03; 95%CI 1.35-3.03; p = 0.0001), and district of residence (OR = 5.72; 95%CI 2.01-16.25; p = 0.0005). Most adolescents and young people from the study findings had increased knowledge score on the types and availability of SRH services in the district health facilities. But utilization of the SRH services was low because, the point of delivery of these SRH services were far, and most have to cover long distance.
Keywords: Adolescent, Availability, Utilization, Reproductive Health Service, Ghana.
Assessing the Availability and Utilisation of Adolescent Reproductive Health Services in Northern Region of Ghana
References:
[1] World Health Organization. (2018). Family Planning Evidence Brief: Reducing early and unintended pregnancies among adolescents. WHO/RHR/17.10. www.who.int.
[2] Bam, V., Bilal, S.M., Spigt, M., Dinant, G. J., & Blanco, R., (2019). Utilization of sexual and reproductive health services in Ethiopia. Does it affect sexual activity among high school students? Journal of Sexual Reproductive Health, 6(1), 14-18.
[3] Abajobir, A. A., & Seme, A. (2014). Reproductive health knowledge and services utilization among rural adolescents in east Gojjam zone, Ethiopia: A community-based cross-sectional study. BMC Health Services Research, 14(1), 1–11.
[4] Ghana Statistical Service (2014). Ghana demographic and health survey,2015. Rockville, Maryland, USA: GSS, GHS, and ICF International.
[5] Ghana Health Service (2016). Monthly family planning performance feedback (Fact sheet). Accra: GHS, MOH. April 2.
[6] Kumi-Kyereme, A., (2021). ‘Sexual and reproductive health services utilisation amongst in-school young people with disabilities in Ghana’, African Journal of Disability 10(0), a671.
[7] Maguire, M., & Delahunt, B. (2017). Doing a thematic analysis: A practical, step-by step guide for learning and teaching scholars. Dundalk in state of technology. J of Teaching and Learning in Higher Education, 8(3).
[8] Awusabo-Asare, K., Yankey, B.A., Baiden, F., & Eliason, S. (2014). Determinants of unintended pregnancies in rural Ghana. BMC J of pregnancy and childbirth, 14 (2015), 1-9.
[9] Ajike, S. O., & Mbegbu, V. C. (2016). Adolescent / Youth utilization of reproductive health services : Knowledge still a barrier. The Need for Adolescents and Youths. PloS One Journal, 2(3), 17–22.
[10] Dapaah, J. M., Christopher, S., Appiah, Y., Amankwaa, A., & Ohene, L. R. (2016). Knowledge about Sexual and Reproductive Health Services and Practice of What Is Known among Ghanaian Youth , a Mixed Method Approach. January, 1–13.
[11] Bedho, C., Bankole, A., & Malarcher, S. (2014). Removing barriers to adolescents’ access to contraceptive information and services. J Studies in Fam Planning, 4(1), 117–124.
[12] Akatukwasa, C., Bajunirwe, F., Nuwamanya, S., Kansime, N., Aheebwe, E., & Tamwesigire, I. K. (2019). Integration of HIV-sexual reproductive health services for young people and the barriers at public health facilities in Mbarara Municipality , Southwestern Uganda : A qualitative assessment. BMJ Journal, 12(3).
[13] Binu, W., Marama, T., Gerbaba, M., & Sinaga, M. (2018). Sexual and reproductive health services utilization and associated factors among secondary school students in Nekemte town, Ethiopia. Bio Med Central, Reproductive Health, 15 (64), 1-10.
[14] Luvai, U.N., Kipmerewo, M., & Onyango, O.K. (2017). Utilization of youth friendly reproductive health services among the youth Bureti Sub County in Kenya (Abstract). European Journal of Pharmaceutical and Medical Research, 4(4), 203-212.
[15] Murigi, M., Butto, D., Barasa, S., Maina, E., & Munyalo, B. (2016). Over coming barriers to contraceptive uptake among adolescents: Kiambu County , Kenya. 05(3), 1–10.
[16] McIntyre, P., Glen, W., & Peattie, S. (2012). Peer influence on sexual activities among adolescents in Ghana. Population Council, 4(6),1, 1.19.
[17] Schalet, A.T., Santelli, J.S., Russell, S.T., & Halpern, C.T. (2014). Adolescence building solid foundations for long life flourishing: World Health Organization. The European Magazine for Sexual and reproductive Health, 80.
[18] Darrroch, J.E., Woog, V., Bankole, A., & Ashford, L.S. (2016). Adding it up: Costsand benefits of meeting the contraceptives needs of adolescents. New York; Guttmacher Institute.
[19] Tlaye, K. G., Belete, M. A., Demelew, T. M., & Getu, M. A. (2018). Reproductive health services utilization and its associated factors among adolescents in Debre Berhan town , Central Ethiopia : a community-based cross-sectional study. 1–11.
[20] Igras, S. M., Macieira, M., Murphy, E., & Lundgren, R. (2014). Investing in very young adolescents ‘ sexual and reproductive health. Global Public Health, 9(5), 555–569.
[21] Pinyopornpanish, K., Thanamee, S., & Angkurawaranon, C. (2017). Sexual health, risky sexual behavior and condom use among adolescents’ young adults and older adults in Chiang Mai, Thailand: Findings of a population-based survey. BMC Research Journal, 10 (1), 682.
[22] Shayan, Z. (2015). Gender Inequality in Education in Afghanistan : Access and Barriers. May, 277–284.
[23] Breaken, P., & Rondinelli, K.A. (2012). Work-family interference among Ghanaian women in higher status occupations. (Ph.DThesis), University of Nottingham, Nottingham.
[24] Asibi, A.A.& Anaba, E.A., (2019). Barriers on access to and use of adolescent health services in Ghana. Journal of Health Research, 33(3), 197-207.
[25] Kuhn, I. (2019). Advancing the sexual and reproductive health rights of adolescent girls and young woman: A focus on safe abortion in 2030, Agenda for sustainable development. Chapel Hill, USA. Advocates for Youth. www.advocatesforyouth.org
[26] Abrafi, B., Weller, W. E., Minkovitz, C. S., & Anderson, G. F. (2018). Utilization of medical and health-related services among school-age children and adolescents with special health care needs (1994 national health interview survey on disability [NHIS-D] baseline data). Pediatrics,11(2), 593–603.
[27] Geremew, G., Tlaye, K., Belete, M. A., Demelew, T. M., & Getu, M. A. (2018). Reproductive health services utilization and its associated factors among adolescents in Debre Berhan town, Central Ethiopia: A community-based cross-sectional study, 1–1.
[28] Ivanova, O., Rai, M., & Kemigisha, E. (2018). A systematic review of sexual and reproductive health knowledge, experiences, and access to services among refugee, migrant and displaced girls and young women in Africa. International Journal of Environmental Research and Public Health, 15(8), 1583.
[29] Morris, J. L., & Rushwan, H. (2015). International Journal of Gynecology and Obstetrics Adolescent sexual and reproductive health : The global challenges. International Journal of Gynecology and Obstetrics, 131, S40–S42.
[30] Ganchimeg, T., Ota, E., Morisaki, N., Laopaiboon, M., Lumbiganon, P., & Zhang, J. (2014). Pregnancy and childbirth outcomes among adolescent mothers: a World Health Organization multicountry study. BJOG : An International Journal of Obstetrics and Gynaecology, 121 Suppl(June 2018), 40–48.
Viewed PDF 871 33 -
 An Investigation into NAFDAC Intervention on the Incidence of Fake and Counterfeit Drugs in NigeriaAuthor: Olakunle Daniel OlaniranDOI: 10.21522/TIJPH.2013.11.03.Art009
An Investigation into NAFDAC Intervention on the Incidence of Fake and Counterfeit Drugs in NigeriaAuthor: Olakunle Daniel OlaniranDOI: 10.21522/TIJPH.2013.11.03.Art009An Investigation into NAFDAC Intervention on the Incidence of Fake and Counterfeit Drugs in Nigeria
Abstract:
Various interventions, including innovative technologies, have been used to solve problems. Over the years, the Nigerian government has introduced a good healthcare delivery system, including providing quality, efficacious and affordable drugs. The study used a qualitative design method adopting a focus group discussion approach. The selected states for the study are Lagos, Kano, Anambra and FCT Abuja. The study population comprised NAFDAC stakeholders who are dealers in pharmaceutical products or Marketing Authorization Holders (MAHs) of medicines, Consumers and Policymakers. The focus group participants were selected based on convenience sampling. The interventions highlighted were Mobile Authentication Services (MAS), on-the-spot checks on drugs through a TruScan, Black-Eye and Radio Frequency Identification Devices (RFID). The respondents also highlighted using NAFDAC registration numbers and holograms as important ways of checking the features of medicine before using it. The participants also highlighted the lack of public awareness about these interventions and the need for proper regulation and enforcement of laws against the sale and distribution of fake drugs as challenges that hinder the successful development and implementation of interventions against fake and counterfeit drugs. The participants suggested KYC measures to address issues within the supply chain to evaluate the effectiveness of their current strategies. Regular meetings, advocacy efforts, and educational workshops are recommended to raise awareness and educate stakeholders about their roles and responsibilities in pursuit of addressing the challenges related to counterfeit drug interventions.
Keywords: Focus group discussion (FGD), Investigation, Intervention, Counterfeit, Technology.An Investigation into NAFDAC Intervention on the Incidence of Fake and Counterfeit Drugs in Nigeria
References:
[1] Buowari, O. V. (2012). Fake and Counterfeit Drug: A review. AFRIMEDIC Journal, 3(2), 1–4. http://www.ajol.info/index.php/afrij/article/view/86573.
[2] Akunyili D., (2007). Counterfeit medicines: A serious crime against humanity. Proceedings of the Director General of the National Agency for Food and Drug Administration and Control (NAFDAC), Nigeria, to the European Parliament in Brussels. 1–7.
[3] Amadi, L., & Amadi2, M. (2014a). Sustainable Drug Consumption, Regulatory Dynamics and Fake Drug Repositioning in Nigeria: A Case of NAFDAC. Journal of Scientific Issues, 2(9), 412–419. http://www.sci-afric.org.
[4] Adelusi A J (2000) Drug Distribution: Challenges and Effects on The Nigerian Society. Keynote address at the &3rd Annual National Conference of the Pharmaceutical Society of Nigeria held at Nicon Hilton Hotel, Abuja ,6th -10th, November 2000.
[5] Akinyandenu O (2013) Counterfeit drugs in Nigeria: A threat to public health. African Journal of Pharmacy and Pharmacology. Vol. 7(36), pp. 2571-2576.
[6] Reggi, V. (2007). Counterfeit medicines: An intent to deceive. International Journal of Risk & Safety in Medicine, 19(1/2), 105–108. http://search.ebscohost.com/login.aspx?direct=true&db=a9h&AN=25215283&site=ehost-live.
[7] Ubajaka, C. F., Obi-okaro, A. C., Emelumadu, O. F., Azumarah, M. N., Ukegbu, A. U., & Ilikannu, S. O. (2016). Factors Associated with Drug Counterfeit in Nigeria : A Twelve Year Review. 12(4), 1–8. https://doi.org/10.9734/BJMMR/2016/21342.
[8] Akunyili, D. (2010). The challenges faced by NAFDAC in the National regulatory process relate to essential drugs for preventing maternal and newborn deaths in Nigeria. Tropical Journal of Obstetrics and Gynaecology, 27(April 2010).
[9] NAFDAC. (2017). NAFDAC Anti-counterfeiting Strategies. https://www.nafdac.gov.ng/about-nafdac/nafdac-anti-counterfeiting-strategies/.
[10] Horalek, J. & Sobeslav, V (2017). Track & Trace System with Serialization Prototyping Methodology for Pharmaceutical Industry in EU. 14th International Conference, https://link.springer.com/chapter/10.1007/978-3-319-65515-4_15.
[11] Egwu, P. E. (2018). Audience exposure and attitude towards NAFDAC’S ‘Mobile Authentication Service’ (MAS) campaigns in three selected southeast states. In Energies (Vol. 6, Issue 1). https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&cad=rja&uact=8&ved=2ahUKEwjFkJvyhujAhWTM8AKHc7iB5oQFnoECBcQAQ&url=http%3A%2F%2Frepository.unn.edu.ng%2Fbitstream%2Fhandle%2F123456789%2F9142%2FEgwu%2C%2520Patrick%2520Ejike%2520Jnr.pdf%3Fsequ.
[12] Akinyandenu, O. (2013). Counterfeit drugs in Nigeria: A threat to public health. African Journal of Pharmacy and Pharmacology, 7(36), 2571–2576. https://doi.org/10.5897/ajpp12.343.
[13] Chinedu-Okeke, C. F., Okoro, N., & Obi, I. (2021). Mobile Authentication Service (MAS) Scheme and Public Participation in Eradicating Fake Drugs in Southeast Nigeria. International Journal of Research and Innovation in Social Science, 05(06), 90–98. https://doi.org/10.47772/ijriss.2021.5605.
[14] Elizabeth Uzochukwu, C. (2017). Audience awareness and use of mobile authentication service (MAS) in identifying fake and substandard drugs in Nigeria. Journal of African Studies. Journal of African Studies, 77(11), 46–66.
[15] NAFDAC. (2010). The National Agency for Food and Drug Administration and Control (NAFDAC) Mobile Authentication Service Scheme Guidelines for the Procurement and Management of the NAFDAC Mobile Authentication Service (MAS) Scheme. NAFDAC’s MAS Implementation Guide.
[16] Adekoya, H. O., & Ekeh, C. M. (2021). Awareness and Adoption of Drug Mobile Authentication Service : A Conscious Approach in Eradication of Fake and Counterfeit Drugs in Nigeria. 7(1), 43–51.
[18] Mhando, L., Jande, M. B., Liwa, A., Mwita, S., & Marwa, K. J. (2016). Public Awareness and Identification of Counterfeit Drugs in Tanzania: A View on Antimalarial Drugs. Advances in Public Health, 2016, 1–8. https://doi.org/10.1155/2016/6254157.
[19] Adisa, R., Adeniyi, O. R., & Fakeye, T. O. (2019). Knowledge, awareness, perception and reporting of experienced adverse drug reactions among outpatients in Nigeria. International Journal of Clinical Pharmacy, 41(4), 1062–1073. https://doi.org/10.1007/s11096-019-00849-9.
[20] Adigwe, O. P., Onavbavba, G., & Wilson, D. O. (2022). Challenges Associated with Addressing Counterfeit Medicines in Nigeria: An Exploration of Pharmacists’ Knowledge, Practices, and Perceptions. Integrated Pharmacy Research and Practice, Volume 11(November), 177–186. https://doi.org/10.2147/iprp.s387354.
[21] Bansal, D., Malla, S., Gudala, K., & Tiwari, P. (2013). Anti-counterfeit technologies: A pharmaceutical industry perspective. Scientia Pharmaceutica, 81(1), 1–13. https://doi.org/10.3797/scipharm.1202-03.
Viewed PDF 1535 33 -
 Prevalence of Substance Use Disorders During the Covid-19 Pandemic: A Cross-Sectional Study in Kanyama Township of Lusaka District, ZambiaAuthor: Steward MudendaDOI: 10.21522/TIJPH.2013.11.03.Art010
Prevalence of Substance Use Disorders During the Covid-19 Pandemic: A Cross-Sectional Study in Kanyama Township of Lusaka District, ZambiaAuthor: Steward MudendaDOI: 10.21522/TIJPH.2013.11.03.Art010Prevalence of Substance Use Disorders During the Covid-19 Pandemic: A Cross-Sectional Study in Kanyama Township of Lusaka District, Zambia
Abstract:
The coronavirus disease (Covid-19) pandemic has caused suffering and pain to mankind leading to many individuals practising self-medication and substance abuse that could elevate substance use disorders (SUDs). This study assessed the impact of Covid-19 on SUDs among Kanyama residents of Lusaka district, Zambia. We conducted a retrospective cross-sectional study using patient files at Kanyama First-Level Hospital from September 2021 to October 2021. Data analysis was done using IBM SPSS version 26.0. Of the 101 participants, 86.1% were male. The study showed that Covid-19 had an impact on SUDs with alcohol (83.2%) being the most abused substance. There was no significant difference in the type of substances abused (p=0.870) and intoxication symptoms (p=0.331) between the pre-Covid and post-Covid groups. There was a significant difference between substance use (p=0.001) and withdrawal symptoms (p=0.002) in both cohorts, with the post-Covid group consuming more substances and experiencing more withdrawal symptoms. Factors that influenced substance abuse included recent unemployment (p<0.001), boredom (p<0.001), overcrowding at home (p<0.001), and gender-based violence (p<0.001) influenced the change in the pattern of substance use. Recreational use was not associated with a change in the pattern of substance abuse (p=0. 667). This study found that the Covid-19 pandemic increased the practices of substance abuse among Kanyama residents, especially those who were unemployed, bored, overcrowded at home and experienced gender-based violence. There is a need to heighten the monitoring and restriction of substance use, especially among adolescents and youths to curb some mental health problems.
Keywords: Covid-19; Pandemic; Self-medication; Substance abuse; substance use disorders; Zambia.Prevalence of Substance Use Disorders During the Covid-19 Pandemic: A Cross-Sectional Study in Kanyama Township of Lusaka District, Zambia
References:
[1] Fournier, A.; Laurent, A.; Lheureux, F.; Ribeiro-Marthoud, M.A.; Ecarnot, F.; Binquet, C.; Quenot, J.P. Impact of the Covid-19 Pandemic on the Mental Health of Professionals in 77 Hospitals in France. PLoS One 2022, 17, e0263666, doi: 10.1371/journal.pone.0263666.
[2] Joaquim, R.M.; Pinto, A.L.C.B.; Guatimosim, R.F.; de Paula, J.J.; Souza Costa, D.; Diaz, A.P.; da Silva, A.G.; Pinheiro, M.I.C.; Serpa, A.L.O.; Miranda, D.M.; et al. Bereavement and Psychological Distress during Covid-19 Pandemics: The Impact of Death Experience on Mental Health. Curr. Res. Behav. Sci. 2021, 2, 100019, doi: 10.1016/j.crbeha.2021.100019.
[3] Dawood, B.; Tomita, A.; Ramlall, S. ‘Unheard,’ ‘Uncared for’ and ‘Unsupported’: The Mental Health Impact of Covid -19 on Healthcare Workers in KwaZulu-Natal Province, South Africa. PLoS One 2022, 17, e0266008, doi: 10.1371/JOURNAL.PONE.0266008.
[4] Mudenda, S.; Chabalenge, B.; Matafwali, S.; Daka, V.; Chileshe, M.; Mufwambi, W.; Mfune, R.L.; Chali, J.; Chomba, M.; Banda, M.; et al. Psychological Impact of Covid-19 on Healthcare Workers in Africa, Associated Factors and Coping Mechanisms: A Systematic Review. Adv. Infect. Dis. 2022, 12, 518–532, doi:10.4236/AID.2022.123038.
[5] Pitlik, S.D. Covid-19 Compared to Other Pandemic Diseases. Rambam Maimonides Med. J. 2020, 11, e0027.
[6] Mudenda, S.; Mukosha, M.; Godman, B.; Fadare, J.O.; Ogunleye, O.O.; Meyer, J.C.; Skosana, P.; Chama, J.; Daka, V.; Matafwali, S.K.; et al. Knowledge, Attitudes, and Acceptance of Covid-19 Vaccines among Secondary School Pupils in Zambia: Implications for Future Educational and Sensitisation Programmes. Vaccines 2022, 10, 2141, doi:10.3390/VACCINES10122141.
[7] Etando, A.; Amu, A.A.; Haque, M.; Schellack, N.; Kurdi, A.; Alrasheedy, A.A.; Timoney, A.; Mwita, J.C.; Rwegerera, G.M.; Patrick, O.; et al. Challenges and Innovations Brought about by the Covid-19 Pandemic Regarding Medical and Pharmacy Education Especially in Africa and Implications for the Future. Healthcare 2021, 9, 1722, doi:10.3390/healthcare9121722.
[8] Kasanga, M.; Mudenda, S.; Gondwe, T.; Chileshe, M.; Solochi, B.; Wu, J. Impact of Covid-19 on Blood Donation and Transfusion Services at Lusaka Provincial Blood Transfusion Centre, Zambia. Pan Afr. Med. J. 2020, 35, 74, doi: 10.11604/pamj.supp.2020.35.2.23975.
[9] Chileshe, M.; Mulenga, D.; Mfune, R.L.; Nyirenda, T.H.; Mwanza, J.; Mukanga, B.; Mudenda, S.; Daka, V. Increased Number of Brought-in-Dead Cases with Covid-19: Is It Due to Poor Health-Seeking Behaviour among the Zambian Population? Pan Afr. Med. J. 2020, 37, 136, doi:10.11604/pamj.2020.37.136.25967.
[10] Opanga, S.A.; Rizvi, N.; Wamaitha, A.; Abebrese Sefah, I.; Godman, B. Availability of Medicines in Community Pharmacy to Manage Patients with Covid-19 in Kenya; Pilot Study and Implications. Sch. Acad. J. Pharm. 2021, 10, 36–42, doi:10.36347/sajp. 2021.v10i03.001.
[11] Lee, A.M.; Wong, J.G.W.S.; McAlonan, G.M.; Cheung, V.; Cheung, C.; Sham, P.C.; Chu, N.M.; Wong, P.C.; Tsang, K.W.T.; Chua, S.E. Stress and Psychological Distress among SARS Survivors 1 Year after the Outbreak. Can. J. Psychiatry 2007, 52, 233–240, doi:10.1177/070674370705200405.
[12] Khalid, I.; Khalid, T.J.; Qabajah, M.R.; Barnard, A.G.; Qushmaq, I.A. Healthcare Workers Emotions, Perceived Stressors and Coping Strategies during a MERS-CoV Outbreak. Clin. Med. Res. 2016, 14, 7–14, doi:10.3121/cmr.2016.1303.
[13] Liu, X.; Kakade, M.; Fuller, C.J.; Fan, B.; Fang, Y.; Kong, J.; Guan, Z.; Wu, P. Depression after Exposure to Stressful Events: Lessons Learned from the Severe Acute Respiratory Syndrome Epidemic. Compr. Psychiatry 2012, 53, 15–23, doi: 10.1016/j.comppsych.2011.02.003.
[14] Wu, P.; Liu, X.; Fang, Y.; Fan, B.; Fuller, C.J.; Guan, Z.; Yao, Z.; Kong, J.; Lu, J.; Litvak, I.J. Alcohol Abuse/Dependence Symptoms among Hospital Employees Exposed to a SARS Outbreak. Alcohol Alcohol. 2008, 43, 706–712, doi:10.1093/alcalc/agn073.
[15] Maunder, R.; Hunter, J.; Vincent, L.; Bennett, J.; Peladeau, N.; Leszcz, M.; Sadavoy, J.; Verhaeghe, L.M.; Steinberg, R.; Mazzulli, T. The Immediate Psychological and Occupational Impact of the 2003 SARS Outbreak in a Teaching Hospital. C. Can. Med. Assoc. J. 2003, 168, 1245–1251.
[16] Maunder, R.G. Was SARS a Mental Health Catastrophe? Gen. Hosp. Psychiatry 2009, 31, 316–317.
[17] Chua, S.E.; Cheung, V.; McAlonan, G.M.; Cheung, C.; Wong, J.W.S.; Cheung, E.P.; Chan, M.T.; Wong, T.K.; Choy, K.M.; Chu, C.M.; et al. Stress and Psychological Impact on SARS Patients during the Outbreak. Can. J. Psychiatry 2004, 49, 385–390, doi:10.1177/070674370404900607.
[18] Jeong, H.; Yim, H.W.; Song, Y.J.; Ki, M.; Min, J.A.; Cho, J.; Chae, J.H. Mental Health Status of People Isolated Due to Middle East Respiratory Syndrome. Epidemiol. Health 2016, 38, e2016048, doi:10.4178/epih. e2016048.
[19] Delanerolle, G.; Zeng, Y.; Shi, J.-Q.; Yeng, X.; Goodison, W.; Shetty, A.; Shetty, S.; Haque, N.; Elliot, K.; Ranaweera, S.; et al. Mental Health Impact of the Middle East Respiratory Syndrome, SARS, and Covid-19: A Comparative Systematic Review and Meta-Analysis. World J. Psychiatry 2022, 12, 739–765, doi:10.5498/wjp. v12.i5.739.
[20] Abramson, A. Substance Use During the Pandemic. Am. Psychol. Assoc. 2021, 52, 22.
[21] Melamed, O.C.; Hauck, T.S.; Buckley, L.; Selby, P.; Mulsant, B.H. Covid-19 and Persons with Substance Use Disorders: Inequities and Mitigation Strategies. Subst. Abus. 2020, 41, 286–291, doi:10.1080/08897077.2020.1784363.
[22] Thiyagarajan, A.; James, T.G.; Marzo, R.R. Psychometric Properties of the 21-Item Depression, Anxiety, and Stress Scale (DASS-21) among Malaysians during Covid-19: A Methodological Study. Humanit. Soc. Sci. Commun. 2022, 9, 220, doi:10.1057/s41599-022-01229-x.
[23] Marzo, R.R.; Aye, S.S.; Naing, T.W.; Kyaw, T.M.; Win, M.T.; Soe, H.H.K.; Soe, M.; Kyaw, Y.W.; Soe, M.M.; Lin, N. Factors Associated with Psychological Distress among Myanmar Residents during Covid-19 Pandemic Crises. J. Public Health Res. 2021, 10, jphr.2021.2279, doi:10.4081/jphr.2021.2279.
[24] Marzo, R.R.; Ismail, Z.; Nu Htay, M.N.; Bahari, R.; Ismail, R.; Villanueva, E.Q.; Singh, A.; Lotfizadeh, M.; Respati, T.; Irasanti, S.N.; et al. Psychological Distress during Pandemic Covid-19 among Adult General Population: Result across 13 Countries. Clin. Epidemiol. Glob. Heal. 2021, 10, 100708, doi: 10.1016/j.cegh.2021.100708.
[25] Marzo, R.R.; Villanueva, E.Q.; Faller, E.M.; Baldonado, A.M. Factors Associated with Psychological Distress among Filipinos during Coronavirus Disease-19 Pandemic Crisis. Open Access Maced. J. Med. Sci. 2020, 8, 309–313, doi:10.3889/oamjms.2020.5146.
[26] RilleraMarzo, R.; Villanueva, E.Q.; Chandra, U.; Htay, M.N.N.; Shrestha, R.; Shrestha, S. Risk Perception, Mental Health Impacts and Coping Strategies during Covid-19 Pandemic among Filipino Healthcare Workers. J. Public Health Res. 2021, 10, jphr.2021.2604, doi:10.4081/jphr.2021.2604.
[27] El-Abasiri, R.A.; Marzo, R.R.; Abdelaziz, H.; Boraii, S.; Abdelaziz, D.H. Evaluating the Psychological Distress of the Coronavirus Disease 2019 Pandemic in Egypt. Eur. J. Mol. Clin. Med. 2020, 7, 1–12.
[28] Htay, M.N.N.; Marzo, R.R.; AlRifai, A.; Kamberi, F.; Radwa Abdullah, E.A.; Nyamache, J.M.; Hlaing, H.A.; Hassanein, M.; Moe, S.; Su, T.T.; et al. Immediate Impact of Covid-19 on Mental Health and Its Associated Factors among Healthcare Workers: A Global Perspective across 31 Countries. J. Glob. Health 2020, 10, 020381, doi:10.7189/jogh.10.020381.
[29] Htay, M.N.N.; Marzo, R.R.; Bahari, R.; AlRifai, A.; Kamberi, F.; El-Abasiri, R.A.; Nyamache, J.M.; Hlaing, H.A.; Hassanein, M.; Moe, S.; et al. How Healthcare Workers Are Coping with Mental Health Challenges during Covid-19 Pandemic? - A Cross-Sectional Multi-Countries Study. Clin. Epidemiol. Glob. Heal. 2021, 11, 100759, doi: 10.1016/j.cegh.2021.100759.
[30] Marzo, R.R.; Singh, A.; Mukti, R.F. A Survey of Psychological Distress among Bangladeshi People during the Covid-19 Pandemic. Clin. Epidemiol. Glob. Heal. 2021, 10, 100693, doi: 10.1016/j.cegh.2020.100693.
[31] Ali, F.; Russell, C.; Nafeh, F.; Rehm, J.; LeBlanc, S.; Elton-Marshall, T. Changes in Substance Supply and Use Characteristics among People Who Use Drugs (PWUD) during the Covid-19 Global Pandemic: A National Qualitative Assessment in Canada. Int. J. Drug Policy 2021, 93, 103237, doi: 10.1016/j.drugpo.2021.103237.
[32] Layman, H.M.; Thorisdottir, I.E.; Halldorsdottir, T.; Sigfusdottir, I.D.; Allegrante, J.P.; Kristjansson, A.L. Substance Use Among Youth During the Covid-19 Pandemic: A Systematic Review. Curr. Psychiatry Rep. 2022, 24, 307–324.
[33] Ornell, F.; Moura, H.F.; Scherer, J.N.; Pechansky, F.; Kessler, F.H.P.; von Diemen, L. The Covid-19 Pandemic and Its Impact on Substance Use: Implications for Prevention and Treatment. Psychiatry Res. 2020, 289, 113096.
[34] Ignaszewski, M.J. The Epidemiology of Drug Abuse. J. Clin. Pharmacol. 2021, 61, S10–S17, doi:10.1002/jcph.1937.
[35] Arble, E.; Manning, D.; Arnetz, B.B.; Arnetz, J.E. Increased Substance Use among Nurses during the Covid-19 Pandemic. Int. J. Environ. Res. Public Health 2023, 20, 2674, doi:10.3390/ijerph20032674.
[36] Ritchie, H.; Arriagada, P.; Roser, M. Opioids, Cocaine, Cannabis and Illicit Drugs Available online: https://ourworldindata.org/illicit-drug-use (accessed on 28 June 2023).
[37] Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The Psychological Impact of Quarantine and How to Reduce It: Rapid Review of the Evidence. Lancet 2020, 395, 912–920.
[38] Venkatesh, A.; Edirappuli, S. Social Distancing in Covid-19: What Are the Mental Health Implications? BMJ 2020, 369, m1379.
[39] Conway, F.N.; Samora, J.; Brinkley, K.; Jeong, H.; Clinton, N.; Claborn, K.R. Impact of Covid-19 among People Who Use Drugs: A Qualitative Study with Harm Reduction Workers and People Who Use Drugs. Harm Reduct. J. 2022, 19, 72, doi:10.1186/s12954-022-00653-1.
[40] Dubey, S.; Biswas, P.; Ghosh, R.; Chatterjee, S.; Dubey, M.J.; Chatterjee, S.; Lahiri, D.; Lavie, C.J. Psychosocial Impact of Covid-19. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 779–788, doi: 10.1016/j.dsx.2020.05.035.
[41] Alonso, S.; Català, M.; López, D.; Álvarez-Lacalle, E.; Jordan, I.; García-García, J.J.; Fumadó, V.; Muñoz-Almagro, C.; Gratacós, E.; Balanza, N.; et al. Individual Prevention and Containment Measures in Schools in Catalonia, Spain, and Community Transmission of SARS-CoV-2 after School Re-Opening. PLoS One 2022, 17, e0263741, doi: 10.1371/journal.pone.0263741.
[42] Giallonardo, V.; Sampogna, G.; Del Vecchio, V.; Luciano, M.; Albert, U.; Carmassi, C.; Carrà, G.; Cirulli, F.; Dell’Osso, B.; Nanni, M.G.; et al. The Impact of Quarantine and Physical Distancing Following Covid-19 on Mental Health: Study Protocol of a Multicentric Italian Population Trial. Front. Psychiatry 2020, 11, 533, doi:10.3389/fpsyt.2020.00533.
[43] Piret, J.; Boivin, G. Pandemics Throughout History. Front. Microbiol. 2021, 11, 631736.
[44] Harker, N.; Johnson, K.; Erasmus, J.; Myers, B. Covid-19—Impact on Substance Use Treatment Utilization and Provision in South Africa. Subst. Abus. Treat. Prev. Policy 2022, 17, 15, doi:10.1186/s13011-022-00446-6.
[45] Panchal, N.; Kamal, R.; Cox, C.; Garfield, R. The Implications of Covid-19 for Mental Health and Substance Use | KFF Https://Www.Kff.Org/Coronavirus-Covid-19/Issue-Brief/the-Implications-of-Covid-19-for-Mental-Health-and-Substance-Use/ The Implications of Covid-19 for Mental Health and Substance Use. Kaiser Fam. Found. 2021, 1–16, doi:10.1377/hpb20201228.198475/full.
[46] Simulundu, E.; Mupeta, F.; Chanda-Kapata, P.; Saasa, N.; Changula, K.; Muleya, W.; Chitanga, S.; Mwanza, M.; Simusika, P.; Chambaro, H.; et al. First Covid-19 Case in Zambia — Comparative Phylogenomic Analyses of SARS-CoV-2 Detected in African Countries. Int. J. Infect. Dis. 2021, 102, 455–459, doi: 10.1016/j.ijid.2020.09.1480.
[47] Mudenda, S.; Botha, M.; Mukosha, M.; Daka, V.; Chileshe, M.; Mwila, K.; Banda, M.; Mfune, R.L.; Mufwambi, W.; Kampamba, M.; et al. Knowledge and Attitudes towards Covid-19 Prevention Measures among Residents of Lusaka District in Zambia. Aquademia 2022, 6, ep22005, doi:10.21601/AQUADEMIA/12210.
[48] Mudenda, S.; Witika, B.A.; Sadiq, M.J.; Banda, M.; Mfune, R.L.; Daka, V.; Kalui, D.; Phiri, M.N.; Kasanga, M.; Mudenda, F.; et al. Self-Medication and Its Consequences during & after the Coronavirus Disease 2019 (Covid-19) Pandemic: A Global Health Problem. Eur. J. Environ. Public Heal. 2020, 5, em0066, doi:10.29333/ejeph/9308.
[49] Amukoto, S. Experiences on Alcohol Abuse among Adolescents of Kanyama Compound, Lusaka District. Dissertation 2022.
[50] Mudenda, S.; Mukosha, M.; Mwila, C.; Saleem, Z.; Kalungia, A.C.; Munkombwe, D.; Daka, V.; Witika, B.A.; Kampamba, M.; Hikaambo, C.N.; et al. Impact of the Coronavirus Disease on the Mental Health and Physical Activity of Pharmacy Students at the University of Zambia: A Cross-Sectional Study. Int. J. Basic Clin. Pharmacol. 2021, 10, 324, doi:10.18203/2319-2003.ijbcp20211010.
[51] Mudenda, S.; Mainza, P.; Mfune, R.L.; Mufwambi, W.; Hangoma, J.; Kampamba, R.M.; Muungo, T.L.; Hikaambo, C.N.; Kampamba, M.; Mohamed, S.; et al. Psychological Impact of Covid-19 on Community Pharmacists: A Cross-Sectional Study in Lusaka District, Zambia. Fortune J. Heal. Sci. 2022, 5, 579–587.
[52] Mudenda, S.; Chomba, M.; Mukosha, M.; Daka, V.; Chileshe, M.; Okoro, R.N.; Fadare, J.; Al-Fayyadh, S.; Munsaka, S.; Kampamba, M.; et al. Psychological Impact of Coronavirus Disease (Covid-19) on Health Professions Students at the University of Zambia: A Cross-Sectional Study. Pan Afr. Med. J. 2022, 42, 237, doi:10.11604/PAMJ.2022.42.237.34041.
[53] Mudenda, S. Coronavirus Disease 2019 (Covid-19) and Its Psychological Impact on Students in Zambia. Acad. Lett. 2021, 837, doi:10.20935/AL837.
[54] Lorenz, H.S.; Stuebing, M.D.; Nambeye, C.; Lungu, G.; Littlefield, L.M. Substance Use Treatment Using Cultural Arts and 12 Steps: Curriculum Training and Community-Led Implementation in Zambia. Addict. Behav. Reports 2022, 15, 100424, doi: 10.1016/j.abrep.2022.100424.
[55] Tyler, K.A.; Handema, R.; Schmitz, R.M.; Phiri, F.; Kuyper, K.S.; Wood, C. Multi-Level Risk and Protective Factors for Substance Use Among Zambian Street Youth. Subst. Use Misuse 2016, 51, 922–931, doi:10.3109/10826084.2016.1156702.
[56] Hammerstein, N.; Paul, R.; Ncheka, J. Increasing Problem of Alcohol Abuse among the Zambian Population in the Psychiatric Setting. Heal. Press Zambia Bull 2017, 1, 29–34.
[57] Masiye, I.; Ndhlovu, D. Drug and Alcohol Abuse Prevention Education in Selected Secondary Schools in Zambia: Policy Guidelines Used. Int. J. Humanit. Soc. Sci. Educ. 2016, 3, 42–48, doi:10.20431/2349-0381.0311006.
[58] Charan, J.; Biswas, T. How to Calculate Sample Size for Different Study Designs in Medical Research? Indian J. Psychol. Med. 2013, 35, 121–126, doi:10.4103/0253-7176.116232.
[59] Chacon, N.C.; Walia, N.; Allen, A.; Sciancalepore, A.; Tiong, J.; Quick, R.; Mada, S.; Diaz, M.A.; Rodriguez, I. Substance Use during Covid-19 Pandemic: Impact on the Underserved Communities. Discoveries 2021, 9, e141, doi:10.15190/d.2021.20.
[60] Zaami, S.; Marinelli, E.; Varì, M.R. New Trends of Substance Abuse During Covid-19 Pandemic: An International Perspective. Front. Psychiatry 2020, 11, 700, doi:10.3389/fpsyt.2020.00700.
[61] Wang, Q.Q.; Kaelber, D.C.; Xu, R.; Volkow, N.D. Covid-19 Risk and Outcomes in Patients with Substance Use Disorders: Analyses from Electronic Health Records in the United States. Mol. Psychiatry 2021, 26, 30–39, doi:10.1038/s41380-020-00880-7.
[62] Spagnolo, P.A.; Montemitro, C.; Leggio, L. New Challenges in Addiction Medicine: Covid-19 Infection in Patients with Alcohol and Substance Use Disorders—the Perfect Storm. Am. J. Psychiatry 2020, 177, 805–807.
[63] Dodge, K.A.; Skinner, A.T.; Godwin, J.; Bai, Y.; Lansford, J.E.; Copeland, W.E.; Benjamin Goodman, W.; McMahon, R.J.; Goulter, N.; Bornstein, M.H.; et al. Impact of the Covid-19 Pandemic on Substance Use among Adults without Children, Parents, and Adolescents. Addict. Behav. Reports 2021, 14, 100388, doi: 10.1016/j.abrep.2021.100388.
[64] Avena, N.M.; Simkus, J.; Lewandowski, A.; Gold, M.S.; Potenza, M.N. Substance Use Disorders and Behavioral Addictions During the Covid-19 Pandemic and Covid-19-Related Restrictions. Front. Psychiatry 2021, 12, 653674.
[65] European Monitoring Centre for Drugs and Drug Addiction; Europol EU Drug Markets: Impact of Covid-19; 2020.
[66] Ismail, R.; Manaf, M.R.A.; Hassan, M.R.; Nawi, A.M.; Ibrahim, N.; Lyndon, N.; Amit, N.; Zakaria, E.; Razak, M.A.A.; Nor, N.I.Z.; et al. Prevalence of Drug and Substance Use among Malaysian Youth: A Nationwide Survey. Int. J. Environ. Res. Public Health 2022, 19, 4684, doi:10.3390/ijerph19084684.
[67] Jadnanansing, R.; Blankers, M.; Dwarkasing, R.; Etwaroo, K.; Lumsden, V.; Dekker, J.; Bipat, R. Prevalence of Substance Use Disorders in an Urban and a Rural Area in Suriname. Trop. Med. Health 2021, 49, 12, doi:10.1186/s41182-021-00301-7.
[68] Zewdu, S.; Hanlon, C.; Fekadu, A.; Medhin, G.; Teferra, S. Treatment Gap, Help-Seeking, Stigma and Magnitude of Alcohol Use Disorder in Rural Ethiopia. Subst. Abus. Treat. Prev. Policy 2019, 14, 4, doi:10.1186/s13011-019-0192-7.
[69] Kaggwa, M.M.; Abaatyo, J.; Alol, E.; Muwanguzi, M.; Najjuka, S.M.; Favina, A.; Rukundo, G.Z.; Ashaba, S.; Mamun, M.A. Substance Use Disorder among Adolescents before and during the Covid-19 Pandemic in Uganda: Retrospective Findings from a Psychiatric Ward Registry. PLoS One 2022, 17, e0269044, doi: 10.1371/journal.pone.0269044.
[70] Compton, W.M.; Flannagan, K.S.J.; Silveira, M.L.; Creamer, M.L.R.; Kimmel, H.L.; Kanel, M.; Blanco, C.; Volkow, N.D. Tobacco, Alcohol, Cannabis, and Other Drug Use in the US Before and During the Early Phase of the Covid-19 Pandemic. JAMA Netw. open 2023, 6, e2254566, doi:10.1001/jamanetworkopen.2022.54566.
[71] Sylvestre, M.P.; Dinkou, G.D.T.; Naja, M.; Riglea, T.; Pelekanakis, A.; Bélanger, M.; Maximova, K.; Mowat, D.; Paradis, G.; O’Loughlin, J. A Longitudinal Study of Change in Substance Use from before to during the Covid-19 Pandemic in Young Adults. Lancet Reg. Heal. 2022, 8, 100168, doi: 10.1016/j.lana.2021.100168.
[72] Karn, M.; Kandel, D.; Subedi, N. Prevalence of Substance Abuse and Its Associated Factors among Medical Students: A Cross-Sectional Study. F1000Research 2022, 10, 797, doi:10.12688/f1000research.54585.2.
[73] Blows, S.; Isaacs, S. Prevalence and Factors Associated with Substance Use among University Students in South Africa: Implications for Prevention. BMC Psychol. 2022, 10, 309, doi:10.1186/s40359-022-00987-2.
[74] Mavura, R.A.; Nyaki, A.Y.; Leyaro, B.J.; Mamseri, R.; George, J.; Ngocho, J.S.; Mboya, I.B. Prevalence of Substance Use and Associated Factors among Secondary School Adolescents in Kilimanjaro Region, Northern Tanzania. PLoS One 2022, 17, e0274102, doi: 10.1371/journal.pone.0274102.
[75] Olanrewaju, J.A.; Hamzat, E.O.; Enya, J.I.; Udekwu, M.O.; Osuoya, Q.; Bamidele, R.; Feyisike Johnson, O.; Johnson, B.S.; Olanrewaju, I.; Owolabi, J.O. An Assessment of Drug and Substance Abuse Prevalence: A Cross-Sectional Study among Undergraduates in Selected Southwestern Universities in Nigeria. J. Int. Med. Res. 2022, 50, 03000605221130039, doi:10.1177/03000605221130039.
[76] Siziya, S.; Muula, A.S.; Besa, C.; Babaniyi, O.; Songolo, P.; Kankiza, N.; Rudatsikira, E. Cannabis Use and Its Socio-Demographic Correlates among in-School Adolescents in Zambia. Ital. J. Pediatr. 2013, 39, 13, doi:10.1186/1824-7288-39-13.
[77] Jones, C.M.; Clayton, H.B.; Deputy, N.P.; Roehler, D.R.; Ko, J.Y.; Esser, M.B.; Brookmeyer, K.A.; Hertz, M.F. Prescription Opioid Misuse and Use of Alcohol and Other Substances Among High School Students - Youth Risk Behavior Survey, United States, 2019. MMWR Suppl. 2020, 69, 38–46, doi:10.15585/mmwr.su6901a5.
[78] Byregowda, H.; Alinsky, R.; Wang, X.; Johnson, R.M. Non-Medical Prescription Opioid Use among High School Students in 38 U.S. States. Addict. Behav. Reports 2023, 17, 100498, doi: 10.1016/j.abrep.2023.100498.
[79] Creamer, M.L.R.; Everett Jones, S.; Gentzke, A.S.; Jamal, A.; King, B.A. Tobacco Product Use Among High School Students - Youth Risk Behavior Survey, United States, 2019. MMWR Suppl. 2020, 69, 56–63, doi:10.15585/mmwr.su6901a7.
[80] Sung, C.W.; Chen, C.H.; Fan, C.Y.; Chang, J.H.; Hung, C.C.; Fu, C.M.; Wong, L.P.; Huang, E.P.C.; Lee, T.S.H. Mental Health Crisis in Healthcare Providers in the Covid-19 Pandemic: A Cross-Sectional Facility-Based Survey. BMJ Open 2021, 11, e052184, doi:10.1136/bmjopen-2021-052184.
[81] Nguemeni Tiako, M.J. Addressing Racial & Socioeconomic Disparities in Access to Medications for Opioid Use Disorder amid Covid-19. J. Subst. Abuse Treat. 2021, 122, 108214, doi: 10.1016/j.jsat.2020.108214.
[82] Yazdi-Feyzabadi, V.; Mehrolhassani, M.H.; Zolala, F.; Haghdoost, A.A.; Oroomiei, N. Determinants of Risky Sexual Practice, Drug Abuse and Alcohol Consumption in Adolescents in Iran: A Systematic Literature Review. Reprod. Health 2019, 16, 115, doi:10.1186/s12978-019-0779-5.
[83] Singh, S.; Balhara, Y.P.S.; Gupta, P.; Christodoulou, N.G. Primary and Secondary Prevention Strategies against Illicit Drug Use among Adults Aged 18–25: A Narrative Review. Australas. Psychiatry 2020, 28, 84–90.
[84] Medina-Mora, M.E. Prevention of Substance Abuse: A Brief Overview. World Psychiatry 2005, 4, 25–30.
[85] Griffin, K.W.; Botvin, G.J. Evidence-Based Interventions for Preventing Substance Use Disorders in Adolescents. Child Adolesc. Psychiatr. Clin. N. Am. 2010, 19, 505–526.
[86] Kvillemo, P.; Hiltunen, L.; Demetry, Y.; Carlander, A.K.; Hansson, T.; Gripenberg, J.; Elgán, T.H.; Einhorn, K.; Skoglund, C. How to Prevent Alcohol and Illicit Drug Use among Students in Affluent Areas: A Qualitative Study on Motivation and Attitudes towards Prevention. Subst. Abus. Treat. Prev. Policy 2021, 16, 83, doi:10.1186/s13011-021-00420-8.
[87] Hsiung, H.; Patel, K.; Hundal, H.; Baccouche, B.M.; Tsao, K.-W. Preventing Substance Abuse in Adolescents: A Review of High-Impact Strategies. Cureus 2022, 14, e27361, doi:10.7759/cureus.27361.
[88] Griswold, M.G.; Fullman, N.; Hawley, C.; Arian, N.; Zimsen, S.R.M.; Tymeson, H.D.; Venkateswaran, V.; Tapp, A.D.; Forouzanfar, M.H.; Salama, J.S.; et al. Alcohol Use and Burden for 195 Countries and Territories, 1990-2016: A Systematic Analysis for the Global Burden of Disease Study 2016. Lancet (London, England) 2018, 392, 1015–1035, doi:10.1016/S0140-6736(18)31310-2.
[89] Enrico, C.; Caldiroli, A.; Di Brita, C.; Colmegna, F.; Nava, R.; Colzani, L.C.; Sibilla, M.; Prodi, T.; Buoli, M.; Clerici, M. Profile of Patients Attending Psychiatric Emergency Care during the Coronavirus 2019 (Covid 19) Pandemic: A Comparative Cross-Sectional Study between Lockdown and Post-Lockdown Periods in Lombardy, Italy. Int. J. Psychiatry Clin. Pract. 2022, 26, 132–138, doi:10.1080/13651501.2021.1939385.
[90] Syed, N.K.; Griffiths, M.D. Nationwide Suicides Due to Alcohol Withdrawal Symptoms during Covid-19 Pandemic: A Review of Cases from Media Reports. J. Psychiatr. Res. 2020, 130, 289–291.
[91] Kristensen, P.; Weisaeth, L.; Heir, T. Bereavement and Mental Health after Sudden and Violent Losses: A Review. Psychiatry 2012, 75, 76–97.
[92] de Miquel, C.; Domènech-Abella, J.; Felez-Nobrega, M.; Cristóbal-Narváez, P.; Mortier, P.; Vilagut, G.; Alonso, J.; Olaya, B.; Haro, J.M. The Mental Health of Employees with Job Loss and Income Loss during the Covid-19 Pandemic: The Mediating Role of Perceived Financial Stress. Int. J. Environ. Res. Public Health 2022, 19, 3158, doi:10.3390/ijerph19063158.
[93] Blomqvist, S.; Högnäs, R.S.; Virtanen, M.; LaMontagne, A.D.; Magnusson Hanson, L.L. Job Loss and Job Instability during the Covid-19 Pandemic and the Risk of Depression and Anxiety among Swedish Employees. SSM - Popul. Heal. 2023, 22, 101424, doi: 10.1016/j.ssmph.2023.101424.
[94] Griffiths, D.; Sheehan, L.; van Vreden, C.; Petrie, D.; Grant, G.; Whiteford, P.; Sim, M.R.; Collie, A. The Impact of Work Loss on Mental and Physical Health During the Covid-19 Pandemic: Baseline Findings from a Prospective Cohort Study. J. Occup. Rehabil. 2021, 31, 455–462, doi:10.1007/s10926-021-09958-7.
[95] Veeroja, P.; Goodall, Z.; Guity-Zapata, N.A.; Stone, W. Private Renters in Shared Housing: Investigating Housing Conditions and Mental Well-Being in Australia during Covid-19. J. Hous. Built Environ. 2023, 1–22, doi:10.1007/s10901-023-10038-w.
[96] Dubey, S.; Sahoo, K.C.; Dash, G.C.; Sahay, M.R.; Mahapatra, P.; Bhattacharya, D.; Barrio, M.O. del; Pati, S. Housing-Related Challenges during Covid-19 Pandemic among Urban Poor in Low- and Middle-Income Countries: A Systematic Review and Gap Analysis. Front. Public Heal. 2022, 10, 1029394.
[97] Newton, D.; Lucock, M.; Armitage, R.; Monchuk, L.; Brown, P. Understanding the Mental Health Impacts of Poor Quality Private-Rented Housing during the UK’s First Covid-19 Lockdown. Heal. Place 2022, 78, 102898, doi: 10.1016/j.healthplace.2022.102898.
[98] Sediri, S.; Zgueb, Y.; Ouanes, S.; Ouali, U.; Bourgou, S.; Jomli, R.; Nacef, F. Women’s Mental Health: Acute Impact of Covid-19 Pandemic on Domestic Violence. Arch. Womens. Ment. Health 2020, 23, 749–756, doi:10.1007/s00737-020-01082-4.
[99] Raj, A.; Johns, N.E.; Barker, K.M.; Silverman, J.G. Time from Covid-19 Shutdown, Gender-Based Violence Exposure, and Mental Health Outcomes among a State Representative Sample of California Residents. EClinicalMedicine 2020, 26, 100520, doi: 10.1016/j.eclinm.2020.100520.
[100] Mittal, S.; Singh, T. Gender-Based Violence During Covid-19 Pandemic: A Mini-Review. Front. Glob. Women’s Heal. 2020, 1, 570087, doi:10.3389/FGWH.2020.00004/BIBTEX.
[101] Alibudbud, R. Gender in Mental Health: Gender-Based Violence, Suffering, Recovery, and the Greater Responsibility of Society during the Covid-19 Pandemic. Asian J. Psychiatr. 2022, 67, 102953.
[102] Madanes, S.B.; Levenson-Palmer, R.; Szuhany, K.L.; Malgaroli, M.; Jennings, E.L.; Anbarasan, D.; Simon, N.M. Acute Stress Disorder, and the Covid-19 Pandemic. Psychiatr. Ann. 2020, 50, 295–300, doi:10.3928/00485713-20200611-01.
[103] Zhang, J.; Shuai, L.; Yu, H.; Wang, Z.; Qiu, M.; Lu, L.; Cao, X.; Xia, W.; Wang, Y.; Chen, R. Acute Stress, Behavioural Symptoms and Mood States among School-Age Children with Attention-Deficit/Hyperactive Disorder during the Covid-19 Outbreak. Asian J. Psychiatr. 2020, 51, 102077, doi: 10.1016/j.ajp.2020.102077.
[104] Taylor, S.; Paluszek, M.M.; Rachor, G.S.; McKay, D.; Asmundson, G.J.G. Substance Use and Abuse, Covid-19-Related Distress, and Disregard
for Social Distancing: A Network Analysis. Addict. Behav. 2021, 114, 106754, doi: 10.1016/j.addbeh.2020.106754.[105] Marzo, R.R.; Vinay, V.; Bahari, R.; Chauhan, S.; Ming, D.A.F.; Nelson Fernandez, S.F.A.; Johnson, C.C.P.; Thivakaran, A.Q.A.; Rahman, M.M.; Goel, S. Depression and Anxiety in Malaysian Population during Third Wave of the Covid-19 Pandemic. Clin. Epidemiol. Glob. Heal. 2021, 12, 100868, doi: 10.1016/j.cegh.2021.100868.
[106] Kamberi, F.; Sinaj, E.; Jaho, J.; Subashi, B.; Sinanaj, G.; Jaupaj, K.; Stramarko, Y.; Arapi, P.; Dine, L.; Gurguri, A.; et al. Impact of Covid-19 Pandemic on Mental Health, Risk Perception and Coping Strategies among Health Care Workers in Albania - Evidence That Needs Attention. Clin. Epidemiol. Glob. Heal. 2021, 12, 100824, doi: 10.1016/j.cegh.2021.100824.
[107] Marzo, R.R.; Khanal, P.; Ahmad, A.; Rathore, F.A.; Chauhan, S.; Singh, A.; Shrestha, S.; Alrifai, A.; Lotfizadeh, M.; Younus, D.A.; et al. Quality of Life of the Elderly during the Covid-19 Pandemic in Asian Countries: A Cross-Sectional Study across Six Countries. Life 2022, 12, 365, doi:10.3390/life12030365.
Viewed PDF 1194 33 -
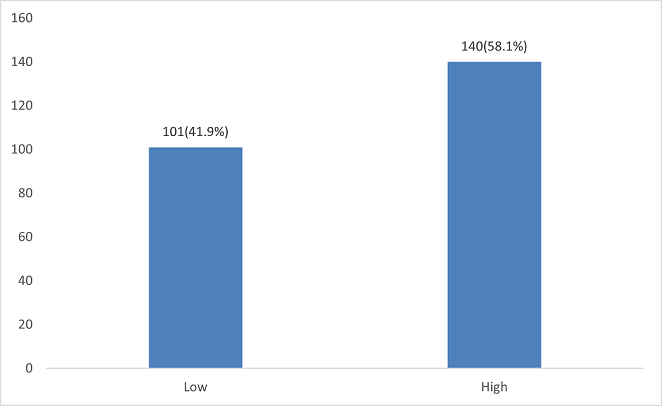 Perceived Quality of Health Care Provided to Mothers during Immediate Postpartum Period at Health Facilities in Kakamega County, KenyaAuthor: Obulemire Edriey RonnieyDOI: 10.21522/TIJPH.2013.11.03.Art011
Perceived Quality of Health Care Provided to Mothers during Immediate Postpartum Period at Health Facilities in Kakamega County, KenyaAuthor: Obulemire Edriey RonnieyDOI: 10.21522/TIJPH.2013.11.03.Art011Perceived Quality of Health Care Provided to Mothers during Immediate Postpartum Period at Health Facilities in Kakamega County, Kenya
Abstract:
Health care workers are essential in averting the high infant and mortality rates in Kenya. The immediate postpartum period is a delicate period when the mother and infant's health is in danger with evidence indicating the majority of deaths occurring during this period. The aim of the study was to assess mothers' perception of quality of care during the immediate postpartum period in selected facilities in Kakamega County in Kenya. Socio-demographic factors, knowledge and health services provided during the immediate postpartum period were evaluated. A cross-sectional descriptive study design to collect quantitative data was adopted. Self-administered questionnaires were utilized to collect data. The study participants were 257 postnatal mothers who were systematically sampled from facilities within Kakamega County. Quantitative data was analyzed using SPSS version 21.0. Descriptive statistics were used to present quantitative data in frequency tables, charts, and graphs. Inferential statics were done using Chi-Square tests at a 95% confidence interval (p<0.05). The results revealed majority of the women perceived the quality of postpartum care as slightly above average at 3.18(63.6%). 58.1% of participants had high knowledge on immediate postpartum care. Knowledge level (p = 0.018) had a significant association with the perceived postpartum care quality. Socio-demographic factors such as age (p=0.014), education (p=0.001), and parity (p=0.029) were associated with the perceived quality of postpartum care. Availability of family planning (p=0.050), immunization (p=0.001), and nutritional counseling services (p=0.012) was associated with the perceived quality of postpartum care. In conclusion the perceived quality of postpartum care was slightly above average with availability of health services positively influencing perception.
Keywords: Perception, Quality, and Immediate postpartum care.Perceived Quality of Health Care Provided to Mothers during Immediate Postpartum Period at Health Facilities in Kakamega County, Kenya
References:
[1] WHO 2022 Recommendations on Maternal and Newborn Care for a Positive Postnatal Experience. Accessed on 2nd October 2022 from: https://www.who.int/publications/i/item/9789240045989.
[2] Immigration and Checkpoints Authority (ICA) (Singapore). Singapore Report on Registration of Births and Deaths 2020. Singapore: Immigration and Checkpoints Authority (ICA) (Singapore). https://www.ica.gov.sg/docs/default-source/ica/stats/annual-bd-statistics/stats_2021_annual_rbd_report.pdf.
[3] KNBS and ICF. 2023. Kenya Demographic and Health Survey 2022. Key Indicators Report. Nairobi, Kenya and Rockville, Maryland, USA: KNBS and ICF. https://dhsprogram.com/pubs/pdf/PR143/PR143.pdf.
[4] WHO Technical Consultation Postpartum and postnatal care. Managing newborn Problems: a guide for doctors’ nurses and midwives. Accessed on 28th Jan 2021 on https://www.who.int/publications/i/item/WHO-MPS-10.03.
[5] Richard Scholnik 2022, Maternal and Infant Mortality Data Factsheet; Ranking of Countries. https://data.worldbank.org/indicator/SP.DYN.IMRT.IN.
[6] UNFPA & Kenyan Ministry of Health 2018, The UNFPA Advocacy Campaign Report to End Preventable Maternal and Newborn Mortality in Kenya. Accessed on https://kenya.unfpa.org/sites/default/files/pub-pdf/UNFPA%20RMNCAH%20Advocacy%20Campaign%20Assessment%20Summary%5BTo%20Print%5D.pdf.
[7] Ihudiebube-Splendor, C. N., & Chikeme, P. C, 2020, A descriptive cross-sectional study: Practical and Feasible Design in investigating Health Care–Seeking Behaviors of Undergraduates. In SAGE Research Methods Cases: Medicine and Health. SAGE Publications, Ltd., https://dx.doi.org/10.4135/9781529742862.
[8] WHO Programming Strategies for Postpartum Family Planning 2013: Family planning services, Counseling, Postpartum Period & Contraception. https://apps.who.int/iris/bitstream/handle/10665/93680/9789241506496_eng.pdf.
[9] Ministry of Health Kenya: National Orientation Package for Targetted Post Natal Care 2011. http://guidelines.health.go.ke:8000/media/Orientation_Package_for_Targeted_Post_Natal_Care_1.pdf.
[10] Ministry of Health Kenya- National Guidelines for Quality Obstetric and Perinatal Care http://guidelines.health.go.ke:8000/media/National_Guidelines_for_Quality_Obstetrics_and_Perinatal_Care.pdf.
[11] Ministry of Health Kenya- Emergency Obstetric and Neonatal Care- A Harmonized Competency Based Training Curriculum for Kenya https://pdf.usaid.gov/pdf_docs/pa00jvxx.pdf.
[12] National Bureau of Statistics-Kenya and ICF International. 2015. 2014 KDHS Key Findings. Rockville, Maryland, USA: KNBS and ICF International. https://dhsprogram.com/pubs/pdf/fr308/fr308.pdf, https://www.dhsprogram.com/pubs/pdf/sr227/sr227.pdf.
[13] Wickramasinghe, S.A., Gunathunga, M.W. & Hemachandra, D.K.N.N 2019. Client perceived quality of the postnatal care provided by public sector specialized care institutions following a normal vaginal delivery in Sri Lanka: a cross sectional study. BMC Pregnancy Childbirth 19, 485. https://doi.org/10.1186/s12884-019-2645-4.
[14] Larson E, Hermosilla S, Kimweri A, Mbaruku GM, Kruk ME., 2014, Determinants of perceived quality of obstetric care in rural Tanzania: a cross-sectional study. BMC Health Serv Res. 2014 Oct 18; 14:483. doi: 10.1186/1472-6963-14-483. PMID: 25326007; PMCID: PMC4283093.
[15] Sagawa, J., Kabagenyi, A., Turyasingura, G. et al., 2021, Determinants of postnatal care service utilization among mothers of Mangochi district, Malawi: a community-based cross-sectional study. BMC Pregnancy Childbirth 21, 591. https://doi.org/10.1186/s12884-021-04061-4.
[16] Gabee, Niebyl, Simpson, Landon, Galn, Jauniaux, Driscoll, Berghella & Grobman, 2017: Obstetrics Normal and Problem Pregnancies, Seventh Edition, Postpartum care. Elsevier publishers- New York. Pg 467-517.
[17] WHO 2019: Maternal Mortality Fact Sheets. https://www.who.int/news-room/fact-sheets/detail/maternal-mortality.
[18] World Health Organization. Maternal and Newborn Health/Safe Motherhood Unit. (1998). Postpartum care of the mother and newborn: a practical guide: report of a technical working group. World Health Organization. https://apps.who.int/iris/handle/10665/66439.
[19] Mugyenyi GR, Ngonzi J, Wylie BJ, Haberer JE, Boatin AA.,2021, Quality of vital sign monitoring during obstetric hospitalizations at a regional referral and teaching hospital in Uganda: an opportunity for improvement. Pan Afr Med J. 2021 Mar 11; 38:252. doi: 10.11604/pamj.2021.38.252.21749. PMID: 34104300; PMCID: PMC8164430.
[20] Kairithia Fredrick, Karanja, G. Joseph, Eunice Cheserem, Kinuthia John, Chege Mwangi, Wamalwa Dalton 2015, Adequacy of vital signs monitoring post-delivery mothers at the Naivasha District Hospital of Nakuru County, Kenya. International Journal of Medical and Clinical Sciences, Vol. 2(1): pp 030-035, January 2015.Copyright © 2014 Spring Journals. FullLength Research Paper Accessed on 15th July 2021on https://www.springjournals.net/full-articles/springjournals.netijmcsarticleskairithiaetal.,.pdf?view=inline.
[21] Ngare DK, Mutunga JN, 1999, Prevalence of malnutrition in Kenya. East Africa Medical Journal. 1999 July; 76(7):376-80. PMID: 10520364.
[22] De Vita, M., Scolfaro, C., Santini, B. et al, 2019, Malnutrition, morbidity, and infection in the informal settlements of Nairobi, Kenya: an epidemiological study. Ital J Pediatr 45, 12 (2019). https://doi.org/10.1186/s13052-019-0607-0.
[23] Gudu, E., Obonyo, M., Omballa, V. et al, 2020, Factors associated with malnutrition in children < 5 years in western Kenya: a hospital-based unmatched case control study. BMC Nutr 6, 33. https://doi.org/10.1186/s40795-020-00357-4.
[24] Mkoka, D.A., Goicolea, I., Kiwara, A. et al, 2014, Availability of drugs and medical supplies for emergency obstetric care: experience of health facility managers in a rural District of Tanzania. BMC Pregnancy Childbirth 14, 108. https://doi.org/10.1186/1471-2393-14-108.
[25] Pattinson RC, Makin JD, Pillay Y, Van den Broek N, Moodley J, 2015, Basic and comprehensive emergency obstetric and neonatal care in 12 South African health districts. S Afr Med J. 2015 Apr; 105(4):256-60. doi: 10.7196/samj.9181. PMID: 26294861.
[26] Berhane, B., Gebrehiwot H., and Weldemariam, S. et al. 2019: Quality of basic Emergency obstetric and newborn care (BEmONC) services from patients’ perspective in Adigrat town, Eastern zone of Tigray, Ethiopia. 2017: A cross sectional study. BMC Pregnancy Childbirth 19, 190 (2019). https://doi.org/10.1186/s12884-019-2307-6.
[27] Tamirat G, Merga D, Addis E, Bikila B and Tesfaye A.Y, Ahmadinezhad M, Vizeshfar F, Pakniat A 2022. Mothers' Perceptions of the Quality of Postnatal Care Provided in Health Centers and the Associated Factors: A Cross-Sectional Study. International Journal of Community Based Nursing and Midwifery. 2022 Apr; 10(2):110-119. doi:10.30476/IJCBNM.2021.90057.1663. PMID: 35372630; PMCID: PMC8957657.
[28] Kamau, Immaculate & Mwanza, (2022). Factors Influencing Delivery of Postnatal Care Education to Mothers Pre-discharge in health facilities in Nairobi County, Kenya. 10.24105/gjbahs.7.1.1803.
[29] Immaculate Wambui Kamau, K. Njoroge, Albert Bundi 2016: Adequacy of Postnatal Care Education Given to Mothers Pre-Discharge in Health Facilities in Nairobi County. European International Journal of Science and Technology Vol. 15. No: 4. https://www.academia.edu/40590069/.
[30] Charlotte et al. 2018: Opportunities for African Newborn; Postnatal Care, Chapter 4. New York Publisher – New York. Page 80 – 120.
[31] Jemberia, M.M., Berhe, E.T., Mirkena, H.B. et al., 2018, Low level of knowledge about neonatal danger signs and its associated factors among postnatal mothers attending at Woldia general hospital, Ethiopia. matern health, neonatol and perinatol 4, 5 (2018). https://doi.org/10.1186/s40748-018-0073-5.
[32] Leta M, 2022, Level of knowledge toward essential newborn care practices among postnatal mothers in governmental hospitals of Harar Town, Eastern Ethiopia. SAGE Open Med. 2022 Feb 8; 10:20503121221076364. doi: 10.1177/20503121221076364. PMID: 35154740; PMCID: PMC8832633.
[33] Dhingra U, Gittelsohn J, Suleiman AM, Suleiman SM, Dutta A, Ali SM, Gupta S, Black RE, Sazawal S, 2014, Delivery, immediate newborn, and cord care practices in Pemba Tanzania: a qualitative study of community, hospital staff and community level care providers for knowledge, attitudes, belief systems and practices. BMC Pregnancy Childbirth. 2014 May 22; 14:173. doi: 10.1186/1471-2393-14-173. PMID: 24885689; PMCID: PMC4049503.
[34] Parashar M, Singh S, Kishore J, Patavegar BN, 2015, Breastfeeding Attachment and Positioning Technique, Practices, and Knowledge of Related Issues Among Mothers in a Resettlement Colony of Delhi. ICAN: Infant, Child, & Adolescent Nutrition. 2015;7(6):317-322. doi:10.1177/1941406415602528.
[35] Megersa, Nega & Gutema, Befikadu & Bancha, Takalign & Amana, Gizachew & Hajo, Abdo & Kusse, Yisehak & Zerihun, Eshetu & Aschalew, Zeleke, 2019, Breast Feeding Practice: Positioning and Attachment during Breast Feeding among Lactating Mothers Visiting Health Facility in Areka Town, Southern Ethiopia. International Journal of Pediatrics. 2019. 1-6. 10.1155/2019/8969432.
Viewed PDF 1582 94 -
 Vaccine Management Practices Among Healthcare Workers in Northwestern State, Nigeria: A Comparative StudyAuthor: Adefisoye Oluwaseun AdewoleDOI: 10.21522/TIJPH.2013.11.03.Art012
Vaccine Management Practices Among Healthcare Workers in Northwestern State, Nigeria: A Comparative StudyAuthor: Adefisoye Oluwaseun AdewoleDOI: 10.21522/TIJPH.2013.11.03.Art012Vaccine Management Practices Among Healthcare Workers in Northwestern State, Nigeria: A Comparative Study
Abstract:
Effective vaccine stock management is one of the criteria for a functional vaccine supply chain. The study evaluated vaccine management practices among healthcare workers in equipped and non-equipped public health facilities in Jigawa State, Northwest Nigeria. A cross sectional comparative study was conducted to assess vaccine management knowledge and practices amongst healthcare workers rendering routine immunization. A multistage sampling technique was used for the selection of respondents. A semi-structured questionnaire was used to obtain information from respondents. Level of significance set at p<0.05. There was a significant difference for response on vaccine vail monitors are the only temperature monitoring devices that routinely accompany vaccines throughout the entire supply chain among healthcare workers from equipped health facilities 213 (77.2%) as compared to those from non-equipped health facilities 63 (22.8%). There was a statistical difference in attitude of vaccines and cold chain management between both groups. Respondents from equipped health facilities had good practices of vaccines and cold chain management as compared to those from non-equipped health facilities. The study revealed that healthcare workers from equipped health facilities had good knowledge and positive attitude on vaccines and cold chain management as compared to their counterparts from non-equipped health facilities. Drivers of effective vaccine stock management are length of years working in health facilities, good knowledge, and practices on vaccine stock management as evident among healthcare workers from equipped health facilities. Findings from this study could be used to improve effective vaccine stock management at the state, LGA, and health facility levels.
Keywords: Comparative study, Healthcare workers, Nigeria, Practices, Vaccine management.Vaccine Management Practices Among Healthcare Workers in Northwestern State, Nigeria: A Comparative Study
References:
[1] World Health Organization, 2009, Immunization against diseases of public health importance. The cost effectiveness of vaccination. Declaration of Alma-Ata. International Conference on Primary Health Care, Alma-Ata, USSR; 6-12, 1978, http://www.who.int/publications/almaata_declaration_en.pdf.
[2] Bloom, D., Canning, D., Weston, M., 2005, “The value of vaccination.” World Econ., 6(3), 15–39, https://doi.org/10.1007/978-1-4419-7185-2_1.
[3] World Health Organization and UNICEF, 2005, GIVS Global immunization vision and strategy 2006-2015. World Health Organization. http://www.who.int/vaccines-documents/DocsPDF05/GIVS_Final_ EN.pdf.
[4] Brison, M, LeTallec, Y., 2017, Transforming cold chain performance and management in lower income countries. Vaccine, 35(17), 2107–9, https://doi.org/10.1016/j.vaccine.2016.11.067.
[5] Moeti, M., Nandy, R., Berkley, S., Davis, S., Levine, O., 2017, No product, no program: The critical role of supply chains in closing the immunization gap. Vaccine, 35(17), 2101–2, https://doi.org/10.1016/j.vaccine.2017.02.061.
[6] Yadav, P., 2015, Health Product Supply Chains in Developing Countries: Diagnosis of the Root Causes of Underperformance and an Agenda for Reform. Heal. Syst. Reform, 1(2), 142–154, https://doi:10.4161/23288604.2014.968005.
[7] Anderson, R., Perrier, T., Pervaiz, F., Sisouveth, N., Kumar, B., Phongphila, S., 2014, Supporting immunization programs with improved vaccine cold chain information systems. In: IEEE global humanitarian technology conference (GHTC 2014), https://doi:10.1109/GHTC.2014.6970284.
[8] National Primary Health Care Development Agency, 2022, Routine Immunization SMS Platform.
[9] Kelsey, J., Whitte, A., Evans, A., 1996, Methods in observational epidemiology. 2nd ed,” Oxford Univ. Press.
[10] Ameen, H., Salaudeen, A., Musa, O., Aderibigbe, S., Akande, T., Ameen, K., 2016, Predictors of vaccine management practices among primary healthcare workers (PHCWs) in Ilorin, North Central Nigeria. Res. J. Heal. Sci., 4(2), 148–161, https://www.researchgate.net/publication/305495236.
[11] Joao Carlos de, T., Gunnar, B., 2007, Cold Chain Management: Knowledge and practice. Ethiopian. J. Heal. Dev., 21(2), 130–135, https://www.ajol.info/index.php/ejhd/article/view/10040/14082.
[12] Ogboghodo, E., Omuemu, V., Odijie, O., 2018, Cold chain management: An assessment of knowledge and attitude of health workers in primary healthcare facilities in Edo State Nigeria. Sahel Med. J., 21(2), 75–82, https://www.smjonline.org/article.asp?issn=1118-8561;year=2018;volume=21;issue=2;spage=75;epage=82;aulast=Ogboghodo.
[13] Saari, L., Judge, T., 2004, Employee Attitudes and Job Satisfaction. Hum. Resour. Manage., 43, 395–407, https://www.scirp.org/(S(351jmbntvnsjt1aadkposzje))/reference/ReferencesPapers.aspx?ReferenceID=2119513.
[14] Adebimpe, W., Adeoye, O., 2021, Knowledge and practice of vaccination logistics management among primary health care workers in Nigeria., Hum. Vaccin Immunother., 17(5), 1490-1495, https://doi:10.1080/21645515.2020.1827609.
[15] Nwankwo, B., Joga, S., Olorukooba, A., Amadu, L., Onoja-Alexander, K., Hamza, M.O., 2018, Knowledge, attitude, and practice of cold chain management among primary health care workers in Giwa, Northwestern Nigeria. Arch. Med. Surg., 3(2), 71–76, https://www.archms.org/article.asp?issn=2543-1951;year=2018;volume=3;issue=2;spage=71;epage=76;aulast=Nwankwo.
[16] Azira, B., Norhayati, M., Norwati, D., 2013, Knowledge, attitude, and adherence to cold chain among general practitioners in Kelatan, Malaysia. Int J Collab Res Med Public Heal., 5, 3–11, https://www.researchgate.net/publication/263165247_Knowledge_Attitude_and_Adherence_to_Cold_Chain_among_General_Practitioners_in_Kelantan_Malaysia.
[17] Immunization action coalition, 2011, Checklist for safe vaccine handling and storage. 3035, https://www.immunize.org/catg.d/p3035.pdf.
[18] Centers for Disease Control and Prevention, 2012, Vaccine Storage and Handling Toolkit. National Centre for Immunization and Respiratory Diseases, 1-104, https://reliefweb.int/report/world/vaccine-storage-and-handling-toolkit-november-2012.
[19] Carr, C., Byles, J., Durrheim, D., 2004, Practice nurses best protect the vaccine cold chain in general practice. Aust J Adv Nurs, 27(2), 30–40, https://www.researchgate.net/publication/237650218_Practice_nurses_best_protect_the_vaccine_cold_chain_in_general_practice.
[20] Mohammed, S., Workneh, B., Kahissay, M, 2021, Knowledge, attitude and practice of vaccinators and vaccine handlers on vaccine cold chain management in public health facilities, Ethiopia: Cross-sectional study. PLoS One, 16(2), e0247459, https://www.doi:10.1371/journal.pone.0247459.
Viewed PDF 972 22 -
 Sexual Practices and HIV Risk Profile of Female Sex Workers During COVID-19 Pandemic in Uyo, NigeriaAuthor: Ughweroghene Kingston Omo-EmmanuelDOI: 10.21522/TIJPH.2013.11.03.Art013
Sexual Practices and HIV Risk Profile of Female Sex Workers During COVID-19 Pandemic in Uyo, NigeriaAuthor: Ughweroghene Kingston Omo-EmmanuelDOI: 10.21522/TIJPH.2013.11.03.Art013Sexual Practices and HIV Risk Profile of Female Sex Workers During COVID-19 Pandemic in Uyo, Nigeria
Abstract:
Female sex workers (FSW) are among the Human Immunodeficiency Virus (HIV) most-at-risk sub-populations worldwide. During COVID-19 pandemic, movement of people including FSWs was restricted in many parts of Nigeria. This paper reports on a study conducted to determine sexual practices and risk profile among FSWs during the COVID-19 pandemic in Uyo, Nigeria. This study was a cross-sectional study among FSWs at Uyo One-stop-shop for Key Populations from June 2020–August 2020 using a structured questionnaire. Participants were selected using systematic random sampling. Responses to consistent condom use and sexual practices with different categories of clients, prophylaxis use, and adherence were collected. Bivariate analyses were done using the Chi-square test as well as Fisher’s exact test while multivariate analysis was with logistic regression analysis and P-value of <0.05 considered statistically significant. 357 FSWs interviewed, but only 344(96.4%) had complete response. 37.2% of the respondents were within the 25-29 years age range and mean (standard deviation-SD) age of 29.06(5.20). 72.4% of the respondents reported they consistently use condoms with first-time clients and 65.7% with repeat clients. 88.7% of the respondents were unmarried and 74.4% have been FSW for ≤5 years with a mean (SD) duration of 4.95(4.02) years. 47.4% of respondents had unprotected sex when incentivized by clients. Cases of HIV exposure among respondents without prophylaxis were reported by 34.9% and 38.1% of the respondents, respectively. Overall adherence to PEP was 30.9%. A high proportion of FSWs engage in high-risk behaviors. FSWs should be advised on their role in HIV prevention through consistent condom use.
Keywords: COVID-19, Female Sex Workers, Pre- and Post-Exposure Prophylaxis, Sexual Behaviours, Sexual Practices.Sexual Practices and HIV Risk Profile of Female Sex Workers During COVID-19 Pandemic in Uyo, Nigeria
References:
[1] Eluwa, G. I., Strathdee, S. A., Adebajo, S. B., Ahonsi, B., Azeez, A., & Anyanti, J. (2012). Sexual risk behaviors and HIV among female sex workers in Nigeria. JAIDS Journal of Acquired Immune Deficiency Syndromes, 61(4), 507–514.
[2] Sabin, K., Zhao, J., Garcia Calleja, J. M., Sheng, Y., Arias Garcia, S., Reinisch, A., & Komatsu, R. (2016). Availability and quality of size estimations of female sex workers, men who have sex with men, people who inject drugs and transgender women in low-and middle-income countries. PLoS One, 11(5), e0155150.
[3] NACA (2014). The 2014 National Prevention Plan, National Agency for the Control of AIDS.
[4] Vickerman, P., Ndowa, F., O’Farrell, N., Steen, R., Alary, M., & Delany-Moretlwe, S. (2010). Using mathematical modelling to estimate the impact of periodic presumptive treatment on the transmission of sexually transmitted infections and HIV among female sex workers. Sexually Transmitted Infections, (3), 163–168.
[5] Shahmanesh, M., Patel, V., Mabey, D., & Cowan, F. (2008). Effectiveness of interventions for the prevention of HIV and other sexually transmitted infections in female sex workers in resource poor setting: a systematic review. Tropical Medicine & International Health,13 (5), 659–679.
[6] Attia, S., Egger, M., Müller, M., Zwahlen, M., & Low, N. (2009). Sexual transmission of HIV according to viral load and antiretroviral therapy: systematic review and meta-analysis. Aids, 23(11), 1397–1404.
[7] Rodger, A. J., Cambiano, V., Bruun, T., Vernazza, P., Collins, S., van Lunzen, J., Corbelli, G. M., Estrada, V., Geretti, A. M., & Beloukas, A. (2016). Sexual activity without condoms and risk of HIV transmission in serodifferent couples when the HIV-positive partner is using suppressive antiretroviral therapy. Jama, 316(2), 171–181.
[8] Rodger, A. J., Cambiano, V., Bruun, T., Vernazza, P., Collins, S., Degen, O., Corbelli, G. M., Estrada, V., Geretti, A. M., & Beloukas, A. (2019). Risk of HIV transmission through condomless sex in serodifferent gay couples with the HIV-positive partner taking suppressive antiretroviral therapy (PARTNER): final results of a multicentre, prospective, observational study. The Lancet, 393(10189), 2428–2438.
[9] Giannou, F. K., Tsiara, C. G., Nikolopoulos, G. K., Talias, M., Benetou, V., Kantzanou, M., Bonovas, S., & Hatzakis, A. (2016). Condom effectiveness in reducing heterosexual HIV transmission: a systematic review and meta-analysis of studies on HIV serodiscordant couples. Expert Review of Pharmacoeconomics; Outcomes Research, 16 (4), 489–499.
[10] Onovo, A., Kalaiwo, A., & Okechukwu, E. (2016). One-stop shop: a community-based antiretroviral therapy (ART) clinic model to improve human immunodeficiency virus (HIV) prevention and treatment Cascade for key populations in Nigeria. Open Forum Infectious Diseases, 3(suppl_1), 483.
[11] Kaplan, J. E., Dominguez, K., Jobarteh, K., Spira, T. J. (2015). Postexposure prophylaxis against human immunodeficiency virus (HIV): new guidelines from the WHO: a perspective. Clinical Infectious Diseases, 60(suppl_3), S196–S199.
[12] Creswell, J. W. (2014). Qualitative, quantitative, and mixed methods approaches. Sage.
[13] (UNAIDS), J. U. N. P. on H. (2016). Prevention gap report. Geneva: UNAIDS.
[14] Lwanga, S. and Lemeshow, S. (1991) Sample Size Determination in Health Studies. A Practical Manual.
http://www.tbrieder.org/publications/books_english/lemeshow_samplesize.pdf.[15] Kioko, R., Muthami, L., & Gikunju, J. (2013). Knowledge, attitude, and practice of post exposure prophylaxis among female sex workers at Majengo, Nairobi. African Journal of Health Sciences, 24(1), 84–91.
[16] Mutya, E., and Mhlanga. M. (2021). HIV Pre-Exposure Prophylaxis Adherence Among Female Sex Workers in Mutare Urban, Zimbabwe. IJRDO - Journal of Health Sciences and Nursing, 6(2), 31–43.
[17] Khan, M. R., Turner, A. N., Pettifor, A., van Damme, K., Rabenja, N. L., Ravelomanana, N., Swezey, T., Jamieson, D., & Behets, F. (2009). Unmet need for contraception among sex workers in Madagascar. Contraception, 79(3), 221–227.
[18] Deering, K. N., Boily, M.-C., Lowndes, C. M., Shoveller, J., Tyndall, M. W., Vickerman, P., Bradley, J., Gurav, K., Pickles, M., & Moses, S. (2011). A dose-response relationship between exposure to a large-scale HIV preventive intervention and consistent condom use with different sexual partners of female sex workers in southern India. BMC Public Health, 11(6), 1–14.
[19] Lopman, B., Lewis, J., Nyamukapa, C., Mushati, P., Chandiwana, S., & Gregson, S. (2007). HIV incidence and poverty in Manicaland, Zimbabwe: is HIV becoming a disease of the poor? AIDS (London, England), 21(Suppl 7), S57.
[20] Elmes, J., Nhongo, K., Ward, H., Hallett, T., Nyamukapa, C., White, P. J., & Gregson, S. (2014). The price of sex: condom use and the determinants of the price of sex among female sex workers in eastern Zimbabwe. The Journal of Infectious Diseases, 210(suppl_2), S569–S578.
[21] Cowan, F. M., Mtetwa, S., Davey, C., Fearon, E., Dirawo, J., Wong-Gruenwald, R., Ndikudze, T., Chidiya, S., Benedikt, C., & Busza, J. (2013). Engagement with HIV prevention treatment and care among female sex workers in Zimbabwe: a respondent driven sampling survey. PloS One, 8(10), e77080.
[22] Johnston, C. L., Callon, C., Li, K., Wood, E., & Kerr, T. (2010). Offer of financial incentives for unprotected sex in the context of sex work. Drug and Alcohol Review, 29(2), 144–149.
[23] Todd, C. S., Nasir, A., Stanekzai, M. R., Scott, P. T., Close, N. C., Botros, B. A., Strathdee, S. A., & Tjaden, J. (2011). HIV awareness and condom use among female sex workers in Afghanistan: implications for intervention. AIDS Care, 23 (3), 348–356.
[24] Remple, V. P., Johnston, C., Patrick, D. M., Tyndall, M. W., & Jolly, A. M. (2007). Conducting HIV/AIDS research with indoor commercial sex workers: Reaching a hidden population. Progress in Community Health Partnerships: Research, Education, and Action, 1(2), 161–168.
[25] Izulla, P., McKinnon, L. R., Munyao, J., Karanja, S., Koima, W., Parmeres, J., Kamuti, S., Kioko, R., Nagelkerke, N., & Gakii, G. (2013). HIV postexposure prophylaxis in an urban population of female sex workers in Nairobi, Kenya. JAIDS Journal of Acquired Immune Deficiency Syndromes, 62(2), 220–225.
[26] Chacko, L., Ford, N., Sbaiti, M., & Siddiqui, R. (2012). Adherence to HIV post-exposure prophylaxis in victims of sexual assault: a systematic review and meta-analysis. Sexually Transmitted Infections, 88 (5), 335–341.
[27] Loutfy, M. R., Macdonald, S., Myhr, T., Husson, H., du Mont, J., Balla, S., Antoniou, T., & Rachlis, A. (2008). Prospective cohort study of HIV post-exposure prophylaxis for sexual assault survivors. Antiviral Therapy,13 (1), 87.
[28] Bentz, L., Enel, P., Dunais, B., Durant, J., Poizot-Martin, I., Tourette-Turgis, C., Rebillon, M., le Duff, F., Dellamonica, P., Pradier, C. (2010). Evaluating counseling outcome on adherence to prophylaxis and follow-up after sexual HIV-risk exposure: a randomized controlled trial. AIDS Care, (12), 1509–1516.
[29] Tissot, F., Erard, V., Dang, T., Cavassini, M. (2010). Nonoccupational HIV post‐exposure prophylaxis: a 10‐year retrospective analysis. HIV Medicine, (9), 584–592.
[30] Armishaw, J., Hoy, J. F., Watson, K. M., Wright, E. J., Price, B. G., Pierce, A. B. (2011). Non-occupational post-exposure prophylaxis in Victoria, Australia: responding to high rates of re-presentation and low rates of follow-up. International Journal of STD & AIDS, 22 (12), 714–718.
[31] Day, S., Mears, A., Bond, K., & Kulasegaram, R. (2006). Post-exposure HIV prophylaxis following sexual exposure: a retrospective audit against recent draft BASHH guidance. Sexually Transmitted Infections, 82(3), 236–237.
[32] Abrahams, N., & Jewkes, R. (2010). Barriers to post-exposure prophylaxis (PEP) completion after rape: a South African qualitative study. Culture, Health & Sexuality, 12(5), 471–484.
[33] Roland, M. E., Neilands, T. B., Krone, M. R., Katz, M. H., Franses, K., Grant, R. M., Busch, M. P., Hecht, F. M., Shacklett, B. L., & Kahn, J. O. (2005). Seroconversion following nonoccupational postexposure prophylaxis against HIV. Clinical Infectious Diseases, 41(10), 1507–1513.
[34] Olsthoorn, A. v, Sivachandran, N., Bogoch, I., Kwantampora, J., Kimani, M., Kimani, J., & Kaul, R. (2016). Barriers to the uptake of postexposure prophylaxis among Nairobi-based female sex workers. Aids, 30(1), 99–103.
Viewed PDF 1122 38 -
 Qualitative Analysis of Factors Influencing the Use of DHIS2 for Tuberculosis Surveillance: A Case Study in GuineaAuthor: Magassouba Aboubacar SidikiDOI: 10.21522/TIJPH.2013.11.03.Art014
Qualitative Analysis of Factors Influencing the Use of DHIS2 for Tuberculosis Surveillance: A Case Study in GuineaAuthor: Magassouba Aboubacar SidikiDOI: 10.21522/TIJPH.2013.11.03.Art014Qualitative Analysis of Factors Influencing the Use of DHIS2 for Tuberculosis Surveillance: A Case Study in Guinea
Abstract:
Tuberculosis (TB) is a major public health problem in Guinea, where many cases are undetected and untreated. A robust health information system is needed to improve TB case detection and treatment outcomes. DHIS2 (District Health Information Software 2) is a web-based system that collects, analyses and reports data on TB indicators. However, its use and use in Guinea is affected by various factors. We explored these factors using a qualitative survey with health workers and managers who use DHIS2 for TB surveillance. We collected data through a survey with open-ended questions and analysed them using classical content analysis. We conducted a qualitative survey with 35 health workers and managers who use DHIS2 for TB surveillance at different levels of the health system in Guinea. We collected data through an online survey with open-ended questions and analysed them using classical content analysis with NVivo software. We identified four main themes: technical issues (such as internet connection, data synchronisation, and validation rules), data quality issues (such as data validation, data aberrations, and data completeness), training and support issues (such as data analysis techniques, online training, orientation on DHIS2), and organisational issues (such as integration of community data, standardisation of data elements, meetings for data validation). We discussed how these findings could inform the improvement of DHIS2 for TB surveillance in Guinea and other similar settings.
Keywords: DHIS2, Health information system, Surveillance, Tuberculosis, Qualitative study.
Qualitative Analysis of Factors Influencing the Use of DHIS2 for Tuberculosis Surveillance: A Case Study in Guinea
References:
[1] WHO W. WHO | Definitions and reporting framework for tuberculosis [Internet]. WHO. 2013 [cited 2019 Jun 29]. Available from: https://www.who.int/tb/publications/definitions/en/.
[2] WHO COVID-19 Case definition [Internet]. [cited 2021 Jun 28]. Available from: https://www.who.int/publications-detail-redirect/WHO-2019-nCoV_Surveillance_Case_Definition-2020.2.
[3] WHO. Global tuberculosis report [Internet]. 2021 [cited 2022 Jul 28]. Available from: https://www.who.int/publications-detail-redirect/9789240037021.
[4] Programme National de lutte anti-tuberculeuse. Rapport Annuel de Lutte Antittuberculeuse. 2022.
[5] WHO: WHO Global tuberculosis report [Internet]. WHO. 2018 [cited 2019 Sep 10]. Retrieved from: http://www.who.int/tb/publications/global_report/en/.
[6] WHO. WHO treatment guidelines for drug-resistant tuberculosis. 2016.
[7] Dehnavieh R, Haghdoost A, Khosravi A, Hoseinabadi F, Rahimi H, Prsh A, et al. The District Health Information System (DHIS2): A literature review and meta-synthesis of its strengths and operational challenges based on the experiences of 11 countries. Health Inf Manag J. 2018 Jun 13; 48:183335831877771.
[8] Dehnavieh R, Haghdoost A, Khosravi A, Hoseinabadi F, Rahimi H, Poursheikhali A, et al. The District Health Information System (DHIS2): A literature review and meta-synthesis of its strengths and operational challenges based on the experiences of 11 countries. Health Inf Manag J. 2019 May 1;48(2):62–75.
[9] Kiberu VM, Matovu JK, Makumbi F, Kyozira C, Mukooyo E, Wanyenze RK. Strengthening district-based health reporting through the district health management information software system: the Ugandan experience. BMC Med Inform Decis Mak. 2014 May 13; 14:40.
[10] Reynolds E, Martel LD, Bah MO, Bah M, Bah MB, Boubacar B, et al. Implementation of DHIS2 for Disease Surveillance in Guinea: 2015–2020. Front Public Health [Internet]. 2022 [cited 2022 Feb 11]; 9. Available from: https://www.frontiersin.org/article/10.3389/fpubh.2021.761196.
[11] Karuri J, Waiganjo P, Orwa D. Determinants of Acceptance and Use of DHIS2 in Kenya: UTAUT-Based Model. J Health Inform Dev Ctries [Internet]. 2017 Dec 10 [cited 2021 Aug 16];11(2). Available from: https://www.jhidc.org/index.php/jhidc/article/view/167.
[12] Moungui HC, Nana-Djeunga HC, Nko’Ayissi GB, Sanou A, Kamgno J. Mixed-methods evaluation of acceptability of the District Health Information Software (DHIS2) for neglected tropical diseases program data in Cameroon. J Glob Health Rep. 2021 Aug 9;5: e2021071.
[13] Maina JK, Macharia PM, Ouma PO, Snow RW, Okiro EA. Coverage of routine reporting on malaria parasitological testing in Kenya, 2015-2016. Glob Health Action. 2017;10(1):1413266.
[14] Hsieh HF, Shannon S. Three Approaches to Qualitative Content Analysis. Qual Health Res. 2005 Dec 1; 15:1277–88.
[15] Data Quality - DHIS2 Documentation [Internet]. [cited 2022 Feb 23]. Available from: https://docs.dhis2.org/en/use/user-guides/dhis-core-version-235/collecting-data/data-quality.html.
[16] McHugh ML. Interrater reliability: the kappa statistic. Biochem Medica. 2012 Oct 15;22(3):276–82.
[17] NVivo - Lumivero [Internet]. [cited 2023 Jul 20]. Available from: https://lumivero.com/products/nvivo/.
[18] Njeru I, Kareko D, Kisangau N, Langat D, Liku N, Owiso G, et al. Use of technology for public health surveillance reporting: opportunities, challenges and lessons learnt from Kenya. BMC Public Health. 2020 Jul 13; 20:1101.
[19] Sahay S, Rashidian A, Doctor HV. Challenges and opportunities of using DHIS2 to strengthen health information systems in the Eastern Mediterranean Region: A regional approach. Electron J Inf Syst Dev Ctries. 2020;86(1): e12108.
[20] Muhoza P, Tine R, Faye A, Gaye I, Zeger SL, Diaw A, et al. A data quality assessment of the first four years of malaria reporting in the Senegal DHIS2, 2014–2017. BMC Health Serv Res. 2022 Jan 2; 22:18.
[21] Githinji S, Oyando R, Malinga J, Ejersa W, Soti D, Rono J, et al. Completeness of malaria indicator data reporting via the District Health Information Software 2 in Kenya, 2011–2015. Malar J. 2017 Aug 17; 16:344.
Viewed PDF 965 34 -
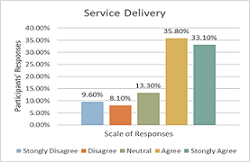 Health Systems Strengthening: A Panacea to Improving Consumption of Public Healthcare Services in Northern Namibia: A Cross Sectional StudyAuthor: Caeser MagumbaDOI: 10.21522/TIJPH.2013.11.03.Art015
Health Systems Strengthening: A Panacea to Improving Consumption of Public Healthcare Services in Northern Namibia: A Cross Sectional StudyAuthor: Caeser MagumbaDOI: 10.21522/TIJPH.2013.11.03.Art015Health Systems Strengthening: A Panacea to Improving Consumption of Public Healthcare Services in Northern Namibia: A Cross Sectional Study
Abstract:
The aim of the study was to assess the impact of health systems strengthening on the consumption of public healthcare services in Northern Namibia. The study assessed how the following components of health systems strengthening influence the consumption of public health care services; (1) timeliness and readiness of services rendered, (2) health workforce competence, (3) health information systems, (4) availability of essential medicines, (5) healthcare financing and lastly (6) leadership and governance. We used a quantitative descriptive cross-sectional study design. 672 respondents were identified using the purposive sampling technique and a well-structured Likert-scaled questionnaire was used for the interviews. Collected information was entered into data sets and analysis was done using Excel and Statistical Package for Social Sciences (SPSS) version 23.0 software. The results were that over 95% of the respondents strongly agreed with each of the factors assessed. Health systems strengthening remains an important factor in the delivery of health services. This was taken note of when 48% of the participants agreed that a good competent health workforce determines their choice of healthcare facility when they are not feeling well. This was further augmented when 49% of the participants agreed that healthcare financing influences people’s choice to go and seek healthcare services from government facilities. It was concluded that health systems strengthening is the cornerstone for improved consumption of public health care services in Northern Namibia. We recommend that governments should develop strong health systems at all levels of health service delivery.
Keywords: Consumption, Health Systems Strengthening, Public Healthcare Services.Health Systems Strengthening: A Panacea to Improving Consumption of Public Healthcare Services in Northern Namibia: A Cross Sectional Study
References:
[1] Adeoti, A.I and Awoniyi B, (2012). “Determinants of child and maternal health status and demand for health care services in Nigeria”. Editorial express.com/cgibin/conference/download.cgi?db_name=CSAE2012&paper_id=679.
[2] Everybody’s business — Strengthening health systems to improve health outcomes. WHO’s framework for action. Geneva, World Health Organization, 2007 (http://www.who.int/healthsystems/strategy/everybodys_business.pdf, accessed 26 April 2010).
[3] Monitoring and evaluation of health systems strengthening. An operational framework. Paper prepared by WHO, World Bank, Global Alliance on Vaccines Initiative (GAVI) and Global Fund to Fight AIDS, Tuberculosis and Malaria (GFATM) (http://www.who.int/healthinfo/HSS_MandE_framework_Nov_2009.pdf, accessed 15 June 2010).
[4] World health report 2000. Health systems performance assessment. Geneva, World Health Organization, 2000(http://www.who.int/whr/2000/en/ndex.html, accessed 26 April 2010).
[5] Roberts MJ, Hsiao W, Berman P, Reich MR. Getting health reform right: a guide to improving performance and equity. New York, Oxford University Press, 2008.
[6] Ghuman, B.S., Mehta Akshat 2005 Health Care for the Poor in India with Special Reference to Punjab State, Network of Asia-Pacific Schools and Institutes of Public Administration and Governance (NAPSIPAG) Annual Conference 2005, Beijing, PRC, 5-7.
[7] International Monetary Fund (2005): International Monetary Fund Annual Report 2005: Making the Global Economy Work for All, retrieved from: https://www.imf.org/en/Publications/AREB/Issues/2016/12/31/International-Monetary-Fund-Annual-Report-2005-Making-the-Global-Economy-Work-for-All-18002.
[8] Republic of Kenya (2005). Kibera Social and Economic Mapping. Household survey Report.
[9] Mwabu G.M., Ainsworth, M., Nyamete, A., (1993). “Quality of Medical Care and Choice of Medical Treatment in Kenya. An Empirical Analysis”. Journal of Human Resources 28(4), 283-291.
[10] Kothari, C.R. (2009) Research Methodology: Methods and Techniques. New Age International, 401 p.
[11] Newing, H. (2011). Conducting Research in Conservation: Social science methods and practice. Routledge, New York, United States of America.
[12] Castillo, J. J. (2009). Snowball sampling. Retrieved from Experiment Resources: http://www.experimentresources.com/snowball-sampling.html.
[13] Naing, Lin & Winn, Than & Nordin, Rusli. (2006). Practical Issues in Calculating the Sample Size for Prevalence Studies. Archives of Orofacial Sciences. 1.
[14] Lavrakas, Paul. (2008). Encyclopedia of Survey Research Methods. 10.4135/9781412963947.
[15] Miller, G. J. and Yang, K. (2008). Handbook of Research Methods in Public Administration. New York: Auerbach Publications, Taylor & Francis Group Modell, S. (2004) Performance.
[16] Scott, A.J. and Wild, C.J. (1986) Fitting Logistic Models under Case-Control or Choice Based Sampling. Journal of the Royal Statistical Society. Series B (Methodological), 48, 170-182. https://doi.org/10.1111/j.2517-6161.1986.tb01400.x.
[17] Advising on Research Methods: A Consultant’s Companion, by Herman J. Ad`er, Gideon J. Mellenberg hand David J. Hand, Huizen, Johannesvan Kessel Publishing, 2008, 574pp, ISBN978-9079418-01-5.
[18] Trochim, William M. K. (October 20, 2006). “Likert Scaling”. Research Methods Knowledge Base, 2nd Edition; Galili, Tal (2010-04-07).
[19] Montgomery, D.C., Peck, E.A. and Vining, G.G. (2001) Introduction to Linear Regression Analysis. 3rd Edition, Wiley, New York.
[20] Burns, N., and Grove, K. (2003). Understanding nursing research (3rd ed.). Philadelphia: W.B. Saunders Company.
[21] Yang, K. (2008). Handbook of Research Methods in Public Administration. Taylor & Francis Group, New York.
[22] Creswell, J. W. (2003). Research design: Qualitative, quantitative, and mixed methods approach (2nd ed.). Thousand Oaks, CA: Sage.
[23] Book Review Research Methods in Education (6th Edition) by Louis Cohen, Lawrence Manion and Keith Morrison 656 pp, Routledge, London, UK, 2007; ISBN 0-415-36878-2.
[24] Health Metrics Network framework and standards for country health information systems. Second edition. Geneva, World Health Organization, 2008 (http://www.who.int/healthmetrics/documents/hmn_framework200803.pdf, accessed 26 April 2010).
[25] Alderman, H. & Gertler, P. (1989). Substitutability of public and private health care for the treatment of children in Pakistan. Living Standards Measurement Study Working Paper 57, Washington: The World Bank.
[26] John, G., and Johnson, P. (2002). Research Methods for Managers, 3rd ed., Sage Publications, London, United Kingdom.
[27] Sapsford, R. and Jupp, V. (2006). Data collection and analysis. SAGE. pp. 28–. ISBN 978-0-7619-4363-1. Retrieved 2 November 2011.
[28] Schwartz J.B., Akin, J.S., Popkin, P.M. (1980). “Price and Income Elasticities of Demand for Modern Health Care: the case of Infant Delivery in the Philippines”. Word Economic Review.2(1):49-76.
[29] Rous, J. J. & Hotchkiss, D. R. (2003). Estimation of the determinants of household health care expenditures in Nepal with controls for endogenous illness and provider choice. Health Economics, 12: 431–451.
[30] Marczyk, G., DeMatteo, D., & Festinger, D. (2005). Essentials of research design and methodology. Hoboken, NJ: John Wiley & Sons.
[31] Namibia (2020): The Institute for Health Metrics and Evaluation. Retrieved from: https://www.healthdata.org/namibia: institute for health metrics and evaluation-Namibia, 2020.
Viewed PDF 1028 25 -
 Knowledge and Attitude of Caregivers in Paediatrics’ HIV Management and Viral Suppression in Lagos State, NigeriaAuthor: Olakunle OsinowoDOI: 10.21522/TIJPH.2013.11.03.Art016
Knowledge and Attitude of Caregivers in Paediatrics’ HIV Management and Viral Suppression in Lagos State, NigeriaAuthor: Olakunle OsinowoDOI: 10.21522/TIJPH.2013.11.03.Art016Knowledge and Attitude of Caregivers in Paediatrics’ HIV Management and Viral Suppression in Lagos State, Nigeria
Abstract:
This study assessed the knowledge, attitude and practices of caregivers of children living with HIV (Human Immuno-Deficiency Virus) in Lagos State, Nigeria. A cross-sectional study was conducted among 500 caregivers of children living with HIV who reside and are receiving treatment in a government health facility in Lagos State. The Sampling technique was purposive sampling based on some inclusion and exclusion criteria, data collection was administered by telephone interview, and the questionnaire was deployed using CAPI (Computer Assisted Personal Interviews) (Kobo Collect) for ease and time management. The study discovered that caring for children living with HIV is demanding. As most of the caregivers are married, and self-employed. The majority of the children living with HIV in this study have been on antiretroviral therapy (ART) for at least 5 years. Most caregivers are parents of the infected child/children living with HIV. Additionally, most caregivers had a good knowledge of HIV transmission and prevention, but they had limited knowledge of paediatric HIV management and had negative attitudes towards HIV. They also reported experiencing stigma and discrimination. These findings suggest that there is a need to improve the knowledge and attitudes of caregivers in order to improve the management of paediatric HIV, Interventions should be designed to address the stigma and discrimination experienced by caregivers. Accurate information should be provided to caregivers about paediatric HIV and paediatric HIV management. The results from this study may not be generalizable to other settings as this study was conducted in Lagos State. In addition, the study relied on self-reported data, which may be subject to bias.
Keywords: Attitude, Caregiver, HIV, Knowledge, Practice and Viral Load.Knowledge and Attitude of Caregivers in Paediatrics’ HIV Management and Viral Suppression in Lagos State, Nigeria
References:
[1] Afolabi, B. A., Ogunleye, O. A., Afolabi, O. A., & Adetoro, O. A. (2013). The impact of HIV/AIDS on vulnerable children: A review of the literature. African Health Sciences, 13(4), 920-926. doi:10.4314/ahs.v13i4.9.
[2] Lazarus, J. M. (2021). HIV/AIDS: A comprehensive guide to diagnosis, treatment, and care. CRC Press. ISBN: 9781138570503.
[3] Waterfield, R. (2021). HIV/AIDS: A practical guide to care and management. John Wiley & Sons. ISBN: 9781119638212.
[4] Avert. (2021). HIV & AIDS in Sub-Saharan Africa. Retrieved from https://www.avert.org/professionals/hiv-around-world/sub-saharan-africa.
[5] United Nations. (2011). Goal 6: Combat HIV/AIDS, malaria and other diseases. Available at: www.un.org/millenniumgoals/aids.shtml.
[6] Olusola, F., Fatusi, A. O., Adebayo, A. A., & Ogunyemi, O. S. (2019). Stigma and discrimination as barriers to HIV testing and care in Nigeria: A systematic review. BMC Public Health, 19(1), 1398. doi:10.1186/s12889-019-7357-0.
[7] Oke, A., Isah, A., Onyebuchi, O. C., & Nwagwu, C. (2019). Factors influencing access to antiretroviral therapy for children living with HIV in Nigeria: A qualitative study. AIDS Care, 31(1), 13-19. doi:10.1080/09540121.2018.1547140.
[8] UNICEF. (2021). Addressing discrimination and gender inequalities in the context of HIV: A guide for policy-makers and programme managers. New York: UNICEF.
[9] World Health Organization. (2011a). Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection: Recommendations for a public health approach. Geneva: World Health Organization.
[10] Badru, A. K. (2020). The role of caregivers in the success of paediatric antiretroviral therapy (ART) in Nigeria. Sokoto Educational Review, 19(1), 72-84. doi:10.35386/ser.v19i1.146.
[11] Busza, J., Lawn, S. D., Newell, M. L., & Coovadia, H. (2018). Improving health outcomes for children living with HIV in low- and middle-income countries: A critical review of the evidence. Lancet, 391(10129), 2128-2145. doi:10.1016/S0140-6736(18)30271-X.
[12] Piloya, M., Chisale, J. M., Mwale, F., Mwilambwe, S., & Maseko, P. (2021). Challenges and opportunities in the provision of HIV care to children in sub-Saharan Africa: A systematic review. BMC Public Health, 21(1), 2084. doi:10.1186/s12889-021-10977-x.
[13] Ukaegbu, E., Alibekova, R., Ali, S., Crape, B., & Issanov, A. (2022). Trends of HIV/AIDS knowledge and attitudes among Nigerian women between 2007 and 2017 using Multiple Indicator Cluster Survey data. BMC Public Health, 22(1), 440. doi:10.1186/s12889-022-12865-y.
[14] Awoleye, O. M., Ojuloge, M. A., & Siyanbola, W. O. (2012). Factors influencing adherence to antiretroviral therapy among children living with HIV/AIDS in Nigeria. AIDS Care, 24(9), 1150-1157. doi:10.1080/09540121.2011.630860.
[15] World Health Organization (2010). Antiretroviral Therapy for HIV Infection in Infants
and Children: Towards Universal Access: Recommendations for a Public Health Approach - 2010 revision. Geneva, Switzerland: http://www.who.int/hiv/pub/paediatric/infants2010/en/index.html.[16] Orenuga, S. O., Olubodun, A. A., Adejumo, A. O., Lawal, A. O., & Ogunsola, F. (2018). Nutritional status and risk of opportunistic infections among HIV-positive children in southwestern Nigeria. BMC Public Health, 18(1), 891. doi:10.1186/s12889-018-5651-8.
[17] Olowookere, S. A., Bamigboye, M. O., Oyeleke, O. M., & Oladele, J. O. (2020). Association between frequent viral load monitoring and clinical outcomes in HIV-positive children in a tertiary hospital in Nigeria. Journal of the Pediatric Infectious Diseases Society, 9(1), e20-e23. doi:10.1093/jpids/piaa104.
[18] Humphrey, A. M., Govaerts, R., Ficinski, S. Z., Masoka, E., Chandiwana, A., & Ndlovu, M. (2019). Caregivers’ attitudes towards caring for HIV-positive children and adherence to antiretroviral therapy: A cross-sectional study in Zimbabwe. AIDS Care, 31(7), 919-926. doi:10.1080/09540121.2019.1568547.
[19] Abdullahi, S.B., Ibrahim, O.R., Okeji, A.B., Yandoma, R.I., Bashir, I., Haladu, S., Idris, S.A., Oseni T.I., Suleiman, B.M., Yahaya, M. & Sufiyan, S.B. (2021). Viral suppression among HIV-positive patients on antiretroviral therapy in northwestern Nigeria: An eleven-year review of tertiary care records, January- 2009- December, 2019. BMC Infectious Diseases, 21:1031. https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-021-06722-3.
[20] Asuquo, E.F., Atowa, J.B., & Adejumo, P. (2014). Assessing the relationship between caregivers’ burden and the availability of support for family caregivers of HIV/AIDS patients in Calabar, South-East Nigeria. World Journal of AIDS, 3(4), 335-344. https://www.scirp.org/journal/paperinformation.aspx?paperid=40632.
Viewed PDF 950 27 -
Comparative Study on Drivers and Barriers of Vaccine Stock Management Practices Among Healthcare Workers in Northwestern State, NigeriaAuthor: Adefisoye Oluwaseun AdewoleDOI: 10.21522/TIJPH.2013.11.03.Art017
Comparative Study on Drivers and Barriers of Vaccine Stock Management Practices Among Healthcare Workers in Northwestern State, Nigeria
Abstract:
The growing concerns regarding stock out of vaccines at the health facility level during immunization sessions have resulted in missed opportunity and caregivers losing confidence in the health system. This study assessed the drivers and barriers to effective vaccine stock management amongst healthcare workers in equipped and non-equipped health facilities in Jigawa state, Nigeria. A cross sectional comparative study was conducted to assess barriers of vaccine stock management amongst healthcare workers rendering routine immunization. A multistage sampling technique was used for the selection of respondents. A semi-structured questionnaire was used to obtain information from respondents. Level of significance set at p<0.05. Majority of the respondents from equipped health facilities 142 (71.7%) and non-equipped health facilities 56 (28.3%) had between 1-9 years of practice. Use of target population data for vaccine forecasting had the highest responses with 60% of healthcare workers in equipped health facilities as compared to 22% from non-equipped health facilities. Reserved stock as a parameter for vaccine restocking had the least responses with 15% of healthcare workers in equipped health facilities as compared to 6% from non-equipped health facilities. Respondents from equipped health facilities had good practices of vaccines and cold chain management as compared to those from non-equipped health facilities. Poor electricity supply was statistically significant (p=0.029) with more responses from healthcare workers from equipped health facilities as compared to those from non-equipped health facilities. The findings from this study could be used to improve effective vaccine stock management at the state, LGA, and health facility levels.
Keywords: Barriers, Comparative study, Healthcare workers, Nigeria, Vaccine management, practices.Comparative Study on Drivers and Barriers of Vaccine Stock Management Practices Among Healthcare Workers in Northwestern State, Nigeria
References:
[1] World Health Organization, 2009, Immunization against diseases of public health importance. The cost effectiveness of vaccination. Declaration of Alma-Ata. International Conference on Primary Health Care, Alma-Ata, USSR; 6-12, 1978, https://www.who.int/docs/default-source/primary-health-care-conference/public-health.pdf.
[2] Bloom, D., Canning, D., Weston, M., 2005, The value of vaccination. World Econ., 6(3), 15–39, https://doi.org/10.1007/978-1-4419-7185-2_1.
[3] World Health Organization and UNICEF, 2005, GIVS Global immunization vision and strategy 2006-2015. World Health Organization. http://www.who.int/vaccines-documents/DocsPDF05/GIVS_Final_ EN.pdf.
[4] Maurice, J., Davey, S., 2009, State of the world’s vaccines and immunization. 3rd edition, World Health Organization and United Nations Children Fund, 169, https://apps.who.int/iris/handle/10665/44169.
[5] Yadav, P., 2015, Health Product Supply Chains in Developing Countries: Diagnosis of the Root Causes of Underperformance and an Agenda for Reform. Heal. Syst. Reform, 1(2), 142–154, https://doi:10.4161/23288604.2014.968005.
[6] Anderson, R., Perrier, T., Pervaiz, F., Sisouveth, N., Kumar, B., Phongphila, S., 2014, Supporting immunization programs with improved vaccine cold chain information systems. In: IEEE global humanitarian technology conference (GHTC 2014), https://doi:10.1109/GHTC.2014.6970284.
[7] Payne, S., Townend, J., Jasseh, M., Jallow, Y., Kampmann, B., 2014, Achieving comprehensive childhood immunization: An analysis of obstacles and opportunities in The Gambia. Health Policy Plan., 29(2), 193–203, https://doi:10.1093/heapol/czt004.
[8] World Health Organization, 2016, 10 facts on polio eradication. http://www.who.int/features/factfiles/polio/facts/en/index.html.
[9] National Primary Health Care Development Agency, 2022, Routine Immunization SMS Platform.
[10] Kelsey, J., Whitte, A., Evans, A., 1996, Methods in observational epidemiology. 2nd ed,” Oxford Univ. Press.
[11] Obionu, C.N., 2017, Primary Health Care for Developing Countries. 2nd Edition, Publishers Institute for Development Studies, University of Nigerian Enugu Campus, Enugu, 183-284, https://scrip.org>reference>referencespapers.
[12] Olikoye, R., Soroungbe, A., Oyegbite, K., Bamisaye, A., 1991, Strenghtening PHC at the Local Government level: the Nigerian Experience., 1st ed. Lagos: Academy Press, https://www.worldcat.org/title/strengthening-primary-health-care-at-a-local-government-level-the-nigerian-experience/oclc/40161545.
[13] Barber, S., Lorenzoni, L., Ong, P., 2019, Price setting and price regulation in health care: lessons for advancing Universal Health Coverage. Geneva: World Health Organization, Organisation for Economic Co-operation and Development., https://www.oecd.org/health/health-systems/oecd-who-price-setting-summary-report.pdf.
[14] Onwujekwe, O., Mbachu, C., Ezenwaka, U., Arize, I., Ezumah, N., 2019, Characteristics and Effects of Multiple and Mixed Funding Flows to Public Healthcare Facilities on Financing Outcomes: A Case Study From Nigeria. Front Public Heal., 7, 403, https://doi.org/10.3389/fpubh.2019.00403.
[15] Ameen, H., Salaudeen, A., Musa, O., Aderibigbe, S., Akande, T., Ameen, K., 2016, Predictors of vaccine management practices among primary healthcare workers (PHCWs) in Ilorin, North Central Nigeria. Res. J. Heal. Sci., 4(2), 148–161, https://www.researchgate.net/publication/305495236.
[16] Immunization action coalition, 2011, Checklist for safe vaccine handling and storage. 3035, https://www.immunize.org/catg.d/p3035.pdf.
[17] Centers for Disease Control and Prevention, 2012, Vaccine Storage and Handling Toolkit. National Centre for Immunization and Respiratory Diseases, 1-104, https://reliefweb.int/report/world/vaccine-storage-and-handling-toolkit-november-2012.
[18] Carr, C., Byles, J., Durrheim, D., 2004, Practice nurses best protect the vaccine cold chain in general practice. Aust J Adv Nurs, 27(2), 30–40, https://www.researchgate.net/publication/237650218_Practice_nurses_best_protect_the_vaccine_cold_chain_in_general_practice.
[19] Nwankwo, B., Joga, S., Olorukooba, A., Amadu, L., Onoja-Alexander, K., Hamza, M.O., 2018, Knowledge, attitude, and practice of cold
chain management among primary health care workers in Giwa, Northwestern Nigeria. Arch. Med. Surg., 3(2), 71–76, https://www.archms.org/article.asp?issn=2543-1951;year=2018;volume=3;issue=2;spage=71;epage=76;aulast=Nwankwo.[20] Mohammed, S., Workneh, B., Kahissay, M, 2021, Knowledge, attitude and practice of vaccinators and vaccine handlers on vaccine cold chain management in public health facilities, Ethiopia: Cross-sectional study. PLoS One, 16(2), e0247459, https://www.doi:10.1371/journal.pone.0247459.
[21] Oyefolu, A.O., Nwaeke, A.C., Audu, R.A., Akinyemi, K.O., Salu, O.B., Muller, C.P., Omilabu, S.A., 2007, Evaluation of MeaslesVaccine Cold Chain in Lagos State, Nigeria.,” African J. Clin. Exp. Microbiol., 8(1), 1–7, http://www.ajol.info/journals/ajcem.
[22] Berhane, Y., Demissie, M., 2000, Cold Chain Status at Immuni-sation Centres in Ethiopia. East Afr. Med. J., 77(9), 476–479, http://doi:10.4314/eamj.v77i9.46692.
[23] Dairo, D., Osizimete, O., 2016, Factors affecting vaccine handling and storage practices among immunizationservice providers in Ibadan, Oyo State, Nigeria.. Afr. Health Sci., 16(2), 576, http://doi: 10.4314/ahs.v16i2.27.
Viewed PDF 882 21 -
 Co-relation between ART (Anti-Retroviral Therapy) Adherence with Nutritional Status and Quality of Life among HIV-Infected AdolescentsAuthor: Rajathi SakthivelDOI: 10.21522/TIJPH.2013.11.03.Art018
Co-relation between ART (Anti-Retroviral Therapy) Adherence with Nutritional Status and Quality of Life among HIV-Infected AdolescentsAuthor: Rajathi SakthivelDOI: 10.21522/TIJPH.2013.11.03.Art018Co-relation between ART (Anti-Retroviral Therapy) Adherence with Nutritional Status and Quality of Life among HIV-Infected Adolescents
Abstract:
Successful treatment for Perinatally Infected Adolescents (PIA) faces physical challenges like the risk of co-morbidity, deferred growth, and development, often resulting in late puberty in girls, and stunting/wasting makes it difficult to reach the transition phase of adulthood. The study aims to identify the correlation between ART adherence with nutritional status and QOL and find the association between adherence scores with selected demographic variables among adolescents. A randomized Controlled Trial design was adopted. Through simple random technique, a total of 388 HIV-infected adolescents were divided into experimental (195) and control (193) groups. The data were collected from four ART clinics in Chennai, India, through standardized ART adherence, QOL, and structured nutritional assessment questionnaires. Motivational counselling was given to the experimental group, and the researcher demonstrated selected asanas. The data were collected from both groups at ‘0’, ‘3’ & 6-month intervals. Descriptive & inferential statistics were used for the analysis of data. Regarding correlation, in the experimental group, baseline assessment showed poor correlation, but in the 3rd & 6th months there was a fair and moderate correlation found and was significant at p=0.05** and P=0.001*** respectively. Whereas in a control group, throughout the assessment period showed that, there was a poor correlation. Regarding association, showed adolescents' age, sex, sex of caregivers, relationship with adolescents, and residence were found significant. Motivational counseling along with asana has a positive correlation to ART adherence to promote the health and well-being of adolescents in the experimental group than in the control group.
Keywords: Adherence, Correlation, HIV-infected adolescents, Nutrition, Quality of life.Co-relation between ART (Anti-Retroviral Therapy) Adherence with Nutritional Status and Quality of Life among HIV-Infected Adolescents
References:
[1] Cruz ML, Cardoso CA. Perinatally infected adolescents living with human immunodeficiency virus (perinatally human immunodeficiency virus). World J Virol. 2015 Aug 12;4(3):277-84. doi: 10.5501/wjv. v4.i3.277. PMID: 26279988; PMCID: PMC4534818.
[2] Vidya Vijayan KK, Karthigeyan KP, Tripathi SP, Hanna LE. Pathophysiology of CD4+ T-Cell Depletion in HIV-1 and HIV-2 Infections. Front Immunol. 2017 May 23; 8:580. doi: 10.3389/fimmu.2017.00580. PMID: 28588579; PMCID: PMC5440548.
[3] Julie S. Eggleton; Shivaraj Nagalli. Highly Active Antiretroviral Therapy (HAART) July 4, 2022.https://www.ncbi.nlm.nih.gov/books/NBK554533/.
[4] Bezabhe WM, Chalmers L, Bereznicki LR, Peterson GM. Adherence to Antiretroviral Therapy and Virologic Failure: A Meta-Analysis. Medicine (Baltimore). 2016 Apr;95(15):e3361. doi: 10.1097/MD.0000000000003361. PMID: 27082595; PMCID: PMC4839839.
[5] Simona A. Iacob, Diana G. Iacob and Gheorghita Jugulete. Improving the Adherence to Antiretroviral Therapy, a Difficult but Essential Task for a Successful HIV Treatment—Clinical Points of View and Practical Considerations. Front. Pharmacol., 23 November 2017 Sec. Drugs Outcomes Research and Policies 8 – 2017.
[6] HIV and AIDS in adolescents, UNICEF. July 2021. https://data.unicef.org/topic/hiv-aids.
[7] Bellavia A, Williams PL, DiMeglio LA, Hazra R, Abzug MJ, Patel K, Jacobson DL, Van Dyke RB, Geffner ME; International Maternal Pediatric Adolescent AIDS Clinical Trials (IMPAACT) P219/219C Study, and the Pediatric HIV/AIDS Cohort Study (PHACS). Delay in sexual maturation in perinatally HIV-infected youths is mediated by poor growth. AIDS. 2017 Jun 1;31(9):1333-1341. doi: 10.1097/QAD.0000000000001486. PMID: 28358737; PMCID: PMC5472204.
[8] Bliss JR, Njenga M, Stoltzfus RJ, Pelletier DL. Stigma as a barrier to treatment for child acute malnutrition in Marsabit County, Kenya. Matern Child Nutr. 2016 Jan;12(1):125-38. doi: 10.1111/mcn.12198. Epub 2015 May 18. PMID: 25989353; PMCID: PMC6860141.
[9] Zewen Liu, Zhangpin Ren, Jun Zhang, Chia-Chen Chuang.Role of ROS and Nutritional Antioxidants in Human Diseases Front. Physiol., Volume 9.2018 https://doi.org/10.3389/fphys. 2018.00477.
[10] Andrinopoulos K, Clum G, Murphy DA Harper G. Health Related Quality Of Life and Psychosocial Correlates Among HIV-Infected Adolescent And Young Adult Women In The Us. AIDS Educ Prev. 2011 Aug; 23(4): 367–381.
[11] Forlanini F, Albani ME, Geluardi Y, Ciceri A, Longoni E, et al. (2023) Evaluation of Quality of Life, Mental Health, Psychological and Neuro-Cognitive Aspects in Young Women Living with HIV Infection: Parallel between Vertically and Behaviorally Acquired HIV Infection. J Family Med Prim Care Open Acc 7: 211. DOI: https://doi.org/10.29011/2688-7460.100211.
[12] Bekker LG, Johnson L, Wallace M and Hosek S. Building our youth for the future.J Int AIDS Soc. 2015; 18; 2: (1). doi: 10.7448/IAS.18.2.20027.
[13] Oberdorfer P, Louthrenoo O, Puthanakit T, Sirisanthana V et al., Quality of Life Among HIV-Infected Children in Thailand. Journal of the International Association of Physicians in AIDS Care.2008; 7: (3).141-47 doi: 10.1177/1545109708318877.
[14] Verma, C. V., Kamble, A., & Krishnan, V. (2019). Exercises versus Yoga: Impact on Quality of Life amongst HIV Positive Individuals. New Insights into Disease and Pathogen Research Vol. 3, 90-98. Retrieved from https://stm1.bookpi.org/index.php/nidpr-v3/article/view/789.
[15] Naoroibam R, Metri KG, Bhargav H, Nagaratna R et al., Effect of Integrated Yoga (IY) on psychological states and CD4 counts of HIV-1 infected Patients: A Randomized controlled pilot study. Int J Yoga. 2016; 9 (1): 57-61.
[16] Mary-Ann Davies, Jorge Pinto, Marlène BrasGetting to 90-90-90 in paediatric HIV: What is needed?: 02 December 2015. https://doi.org/10.7448/IAS.18.7.20770.
[17] Looking Out for Adolescents and Youth From Key Populations. UNICEF- East Asia and Pacific Regional Office and United Nations Asia Pacific Interagency Task Team on Young Key Populations, November 2019. https://www.unicef.org/eap/media/4446/file/Looking%20out%20for%20adolescents%20and%20youth%20from%20key%20populations.pdf.
[18] Cardoso CA, Pinto JA, Candiani, TM, Carvalho IR et al., The impact of highly active antiretroviral therapy on the survival of vertically HIV-infected children and adolescents in Belo horizonte, Brazil. Memórias do Instituto Oswaldo Cruz.2012; 102: 532-538. Available in http://dx.doi.org/10.1590/S0074-02762012000400014.
[19] Koech E, Teasdale CA, Wang C, Fayorsey R et al., Characteristics and outcomes of HIV-infected youth and young adolescents enrolled in HIV care in Kenya. AIDS. 2014; 28:2729–2738.DOI:10.1097/QAD.0000000000000473.
[20] Cordova E, Yañez J, Claudia G Ismael R. Safety, and efficacy of antiretroviral therapy in perinatally HIV-1 infected patients following transition to an adult HIV-care hospital with virological failure in Buenos Aires, Argentina. Enferm Infecc Microbiol Clin. 2015;33(2):133–140 doi: 10.1016/j.eimc.2014.05.005.
[21] Botros D, Somarriba G, NeriD,Miller LT. Interventions to Address Chronic Disease and HIV: Strategies to Promote Exercise and Nutrition Among HIV-Infected Individuals Curr HIV/AIDS Rep.2012; 9: 351. doi:10.1007/s11904-012-0135-7.
[22] Kabue MM, Kekitiinwa A, Maganda A, Risser JM, Chan W, Kline MW. Growth in HIV-infected receiving antiretroviral therapy at a paediatric infectious disease’s clinic in Uganda. AIDS Patient Care STDS. 2008; 22:245–25.
[23] Eby J, Chapman J, Marukutira T et al., The adherence-outcome relationship is not altered by diary-driven adjustments of microelectronic monitor data Pharmaco epidemiol Drug Saf. 2015; 24 (12):1313-20. doi: 10.1002/pds.3887. Epub 2015 Oct 12.
[24] Swaminathan S, Padmapriyadarshini C, Yoojin L, Sukumar B et al., Nutritional Supplementation in HIV-Infected Individuals in South India: A Prospective Interventional Study. Clin Infect Dis. (2010) 51 (1): 51-57.doi: 10.1086/653111
[25] Mannheimer SB, Matts J, Telzak E, et al. Quality of life in HIV-infected individuals receiving antiretroviral therapy is related to adherence. AIDS. 2005; 1710–22.
[26] Kuntawee C, Fungladda WT ,Kaewkungwal J, Chotpittayasunon T. Social factors related to quality of life among HIV infected children in UbonRatchathani province, Thailand. The Southeast Asian journal of tropical medicine and public health.2010; 41(5):1136-44.
[27] Nyogea D, Mteng S, Henning L, Franzeck FC et al., Determinants of antiretroviral adherence among HIV positive children and teenagers in rural Tanzania: a mixed methods study. BMC Infectious Diseases (2015) 15: 28.doi 10.1186/s12879-015-0753-y.
[28] Lowenthal ED , Marukutira T,Tshume O, BA, ChapmanJ, Parental Absence From Clinic Predicts Human Immunodeficiency Virus Treatment Failure in Adolescents JAMA Pediatr. 2015 May 1; 169(5): 498–500.doi: 10.1001/jamapediatrics.2014.3785.
[29] Ogalha C, Luz E, Sampaio E, Souza R et al., A randomized, clinical trial to evaluate the impact of regular physical activity on the quality of life, body morphology and metabolic parameters of patients with AIDS in Salvador, Brazil J Acquir Immune DeficSyndr. 2011; 57(3). S179-85. doi: 10.1097/QAI.0b013e31821e9bca.
Viewed PDF 834 14 -
 Sella Turcica Bridging and its Association with Dental Anomalies - An UpdateAuthor: Safeena Abdul Khader SahebDOI: 10.21522/TIJPH.2013.11.03.Art019
Sella Turcica Bridging and its Association with Dental Anomalies - An UpdateAuthor: Safeena Abdul Khader SahebDOI: 10.21522/TIJPH.2013.11.03.Art019Sella Turcica Bridging and its Association with Dental Anomalies - An Update
Abstract:
The Sella turcica is an anatomical structure shaped explicitly like a saddle, located within the middle cranial fossa on the intracranial surface of the sphenoid bone. This structure is commonly observed on lateral cephalograms, frequently employed for orthodontic diagnosis. The Cephalometric radiographs utilize various landmarks as reference points to examine craniofacial structures and Sella Turcica (ST) is the most significant and reliable cranial landmark. The Sella point, located at the midpoint of the ST structure, is a cranial base point that accommodates the pituitary gland. The cephalometric analysis relies on this factor to identify pituitary gland-related pathologies, making it a valuable source of information for craniofacial syndromes. Facial structure development exhibits comparable characteristics to the Sella turcica. Glandular abnormalities possess the potential to be linked to functional disorders, which can result in altered hormonal levels affecting dental growth. Comprehensive understanding of the radiological anatomy and variations help assess growth and identify changes in various anomalies or pathological conditions. Additionally, it can assist in predicting the potential outcome of orthodontic treatment. The objective of this review is to determine and update whether a correlation exists between the bridging of Sella turcica and various dental anomalies related to the shape, size, structure, number, and eruption of teeth. In conclusion, it was noted that Sella turcica bridging is frequently observed in orthodontic patients measuring a clear correlation between dental anomalies and Sella bridging.
Keywords: Sella Turcica Bridging; Dental Anomalies; Genetics; Lateral Cephalogram; Orthodontist.Sella Turcica Bridging and its Association with Dental Anomalies - An Update
References:
[1] Gracco AL, Zanatta S, Forin Valvecchi F, Bignotti D, Perri A, Baciliero F. Prevalence of dental agenesis in a sample of Italian orthodontic patients: an epidemiological study. Progress in orthodontics. 2017; 18:1-7.
[2] MacDonald D, Patel A, Zou B, Yen E, Vora SR. A retrospective study of incidental findings occurring in a consecutive case series of lateral cephalograms of 12- to 20-year-old patients referred for routine orthodontic treatment. Imaging Sci Dent. 2022; 52:295-302;10.5624/isd.20220402.
[3] Seifeldin N, Eltimamy A, Abbady NA. Sella turcica variations in patients with transverse skeletal discrepancies versus patients with normal transverse relationships. a cross- sectional study. BMC Oral Health. 2023;23:301;10.1186/s12903-023-02988-y.
[4] Al-Ani AH, Antoun JS, Thomson WM, Merriman TR, Farella M. Hypodontia: An Update on Its Etiology, Classification, and Clinical Management. Biomed Res Int. 2017;2017:9378325;10.1155/2017/9378325.
[5] Alkofide EA. The shape and size of the sella turcica in skeletal Class I, Class II, and Class III Saudi subjects. The European Journal of Orthodontics. 2007;29:457-63.
[6] Bisk S, Lee FA. Abnormalities found on cephalometric radiographs. The Angle Orthodontist. 1976;46:381-6.
[7] Jones RM, Faqir A, Millett DT, Moos KF, McHugh S. Bridging and dimensions of sella turcica in subjects treated by surgical-orthodontic means or orthodontics only. Angle Orthod. 2005;75:714-8;10.1043/0003-3219(2005)75[714:Badost]2.0.Co;2.
[8] Dasgupta P, Sen S, Srikanth H, Kamath G. Sella turcica bridging as a predictor of Class II malocclusion–an investigative study. Journal of Stomatology, Oral and Maxillofacial Surgery. 2018;119:482-5.
[9] Sathyanarayana HP, Kailasam V, Chitharanjan AB. The size and morphology of sella turcica in different skeletal patterns among South Indian population: A lateral cephalometric study. Journal of Indian Orthodontic Society. 2013;47:266-71.
[10] Kjær I. Sella turcica morphology and the pituitary gland—a new contribution to craniofacial diagnostics based on histology and neuroradiology. European Journal of Orthodontics. 2015; 37:28-36.
[11] Lakshmanan L, Gurunathan D. Prevalence of congenitally missing second premolar teeth in the Dravidian population. Journal of forensic dental sciences. 2019; 11:103.
[12] Alkofide EA. Sella turcica morphology and dimensions in cleft subjects. The Cleft palate-craniofacial journal. 2008; 45:647-53.
[13] Arcos-Palomino I, Ustrell-Torrent JM. Association between sella turcica bridging and altered direction of dental eruption: A case-control study. Journal of clinical and experimental dentistry. 2019;11:e913.
[14] Jankowski T, Jedliński M, Grocholewicz K, Janiszewska-Olszowska J. Sella Turcica Morphology on Cephalometric Radiographs and Dental Abnormalities-Is There Any Association?-Systematic Review. Int J Environ Res Public Health. 2021;18;10.3390/ijerph18094456.
[15] Miletich I, Sharpe PT. Neural crest contribution to mammalian tooth formation. Birth Defects Research Part C: Embryo Today: Reviews. 2004;72:200-12.
[16] Ali B, Shaikh A, Fida M. Association between sella turcica bridging and palatal canine impaction. American Journal of Orthodontics and Dentofacial Orthopedics. 2014;146:437-41.
[17] Alqahtani H. Association between sella turcica bridging and congenitally missing maxillary lateral incisors. Journal of Dental Sciences. 2020;15:59-64.
[18] Baidas LF, Al-Kawari HM, Al-Obaidan Z, Al-Marhoon A, Al-Shahrani S. Association of sella turcica bridging with palatal canine impaction in skeletal Class I and Class II. Clinical, Cosmetic and Investigational Dentistry. 2018:179-87.
[19] Dasgupta P, Sen S, Srikanth HS, Kamath G. Sella Turcica Bridging As A Predictor Of Class II Malocclusion-An Investigative Study. J Stomatol Oral Maxillofac Surg. 2018;119:482-5;10.1016/j.jormas.2018.05.005.
[20] Jankowski T, Jedliński M, Schmeidl K, Grocholewicz K, Janiszewska-Olszowska J. Sella Turcica Abnormalities, Dental Age and Dental Abnormalities in Polish Children. Int J Environ Res Public Health. 2021;18;10.3390/ijerph181910101.
[21] Tekiner H, Acer N, Kelestimur F. Sella turcica: an anatomical, endocrinological, and historical perspective. Pituitary. 2015;18:575-8.
[22] Leonardi R, Barbato E, Vichi M, Caltabiano M. A sella turcica bridge in subjects with dental anomalies. The European Journal of Orthodontics. 2006;28:580-5.
[23] Ortiz PM, Tabbaa S, Flores-Mir C, Al-Jewair T. A CBCT investigation of the association between sella-turcica bridging and maxillary palatal canine impaction. BioMed Research International. 2018;2018.
[24] Yılmaz H, Turkkahraman H, Sayın M. Prevalence of tooth transpositions and associated dental anomalies in a Turkish population. Dento maxilla facial Radiology. 2005;34:32-5.
[25] Saokar PC, Dinesh MR, Shetty A. A correlative study of sella turcica bridging and dental anomalies related to size, shape, structure, number and eruption of teeth. J Orthod Sci. 2022;11:2;10.4103/jos.JOS_81_20.
[26] Leonardi R, Farella M, Cobourne MT. An association between sella turcica bridging and dental transposition. The European Journal of Orthodontics. 2011;33:461-5.
[27] Scribante A, Sfondrini MF, Cassani M, Fraticelli D, Beccari S, Gandini P. Sella turcica bridging and
dental anomalies: is there an association? International Journal of Paediatric Dentistry. 2017;27:568-73.[28] Russell BG, Kjær I. Postnatal structure of the sella turcica in Down syndrome. American Journal of Medical Genetics. 1999;87:183-8.
[29] Sathyanarayana HP, Kailasam V, Chitharanjan AB. Sella turcica-Its importance in orthodontics and craniofacial morphology. Dental Research Journal. 2013;10:571.
[30] Meaney S, Anweigi L, Ziada H, Allen F. The impact of hypodontia: a qualitative study on the experiences of patients. Eur J Orthod. 2012;34:547-52;10.1093/ejo/cjr061.
[31] Peck S, Peck L, Kataja M. Concomitant occurrence of canine malposition and tooth agenesis: evidence of orofacial genetic fields. American Journal of Orthodontics and Dentofacial Orthopedics. 2002;122:657-60.
[32]. Shapira Y, Kuftinec MM. Maxillary tooth transpositions: characteristic features and accompanying dental anomalies. American Journal of Orthodontics and Dentofacial Orthopedics. 2001;119:127-34.Viewed PDF 938 67 -
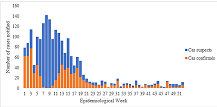 Retrospective Analysis of the Epidemiological Profile of Measles in 2022 in MaliAuthor: Kouame Stanislas KaffloumanDOI: 10.21522/TIJPH.2013.11.03.Art020
Retrospective Analysis of the Epidemiological Profile of Measles in 2022 in MaliAuthor: Kouame Stanislas KaffloumanDOI: 10.21522/TIJPH.2013.11.03.Art020Retrospective Analysis of the Epidemiological Profile of Measles in 2022 in Mali
Abstract:
Measles is a highly contagious viral disease caused by the morbillivirus of which humans are the only reservoir. Our descriptive study aims at analyzing retrospective measles surveillance data from 2022. Of the 2037 suspected measles case samples received at the laboratory, 784 (38%) were confirmed. The age group of 1-4 years is the most affected with an attack rate of 25.43 per 100,000 inhabitants. Children under 5 represent 47.71% of cases. The median age is 4 years and the average age 6.14 years (0 months-54 years). The male sex represents 51% of cases with a sex ratio of 1.06 and an attack rate of 9.72 per 100,000 inhabitants. Most confirmed measles cases (71.77%) were recorded during the dry season. The districts of Koutiala (140 cases: 17.85%), Sikasso (127 cases: 16.19%), Ségou (109 cases: 13.09%) and Bougouni (98 cases: 12.5%) record the most case. The average time for feedback from the laboratory was 3.95 days. Moreover, among the 1253 sample cases negative for measles, 8.22% were positive for rubella. The median age of patients was 6 years. Children under five are the most affected. Most of these cases are in unvaccinated people. The establishment of an enhanced vaccination program at country level considering the most affected groups could reduce the resurgence of measles epidemics.
Keywords: Epidemic, Measles, Mali, Notifiable disease (MADO), Spatiotemporal.Retrospective Analysis of the Epidemiological Profile of Measles in 2022 in Mali
References:
[1] Coulibaly H, Sangho O, Sogodogo S, Keyembé K, Dakouo H. Evaluation of measles epidemiological surveillance: Analysis of the Koulikoro health district database from 2012-2018. Mali Public Health. June 30, 2019;66 ‑9.
[2] Brenda LT. MSD Manual Professional Edition. 2021 [cited 2023 Jul 2]. Measles - Pediatrics. Available at: https://www.msdmanuals.com/fr/professional/p%C3%A9diatrie/diverses-viral-infections-in-the-infant-and-child/measles.
[3] Dia N, Fall A, Ka R, Fall A, Kiori DE, Goudiaby DG, et al. Epidemiology and Genetic Characterization of Measles Strains in Senegal, 2004-2013. PLOS ONE. 2015 May 22 ;10(5):e 0121704.
[4] Habibatou AI, Yanogo PK, Barry D, Togola OB, Adehossi E, Meda N. (PDF) Epidemiological profile of measles in Niger: analysis of measles case-based surveillance data from 2010 to 2019 [Internet]. 2019 [cité 25 avr 2023]. Disponible sur: https://www.researchgate.net/publication/363490495_Epidemiological_profile_of_measles_in_Niger_analysis_of_measles_case-based_surveillance_data_from_2010_to_2019.
[5] Koita M. Performance of the Laboratory System in the Management of the Measles Epidemic in 2020 in Mali. [Internet][ Thesis]. USTTB; 2022 [cited 2023 Jul 2]. Available at: https://www.bibliosante.ml/handle/123456789/5993.
[6] Sy EHIA, Barry D, Traoré B, Boly A, Koné B, Dembélé A, et al. Epidemiological profile of measles in Mali from 2009 to 2018. Journal of Interventional Epidemiology and Public Health [Internet]. 2021 Sep 24 [cited 2023 Apr 11];4(8). Available at: https://www.afenet-journal.net/content/series/4/3/8/full/.
[7] Regional Committee for the Western Pacific 063. Measles elimination [Internet]. WHO Regional Office for the Western Pacific; 2012 [cited 2023 Aug 8]. Available at: https://apps.who.int/iris/handle/10665/249122.
[8] Diarra MBO. Presented and defended publicly on 2017 In front of the Faculty of Medicine and Odonto-Stomatology. 2017.
[9] Mali MOH CMS. Annual national bulletin of epidemiological surveillance [Internet]. 2022 [cited 2023 May 6]. Available at: https://mali.iddsproject.org/.
[10] Mali MOH CMS. Search for annual newsletter | Mali MOH CMS [Internet]. 2021 [cited 2023 May 6]. Available at: https://mali.iddsproject.org/fr/search/node?keys=bulletin+annuel.
[11] National Population Directorate. Reports – National Population Directorate [Internet]. 2020 [cited 2023 Apr 17]. Available at: https://dnp-mali.ml/rapports/.
[12] SLIS. 2018 Statistical Yearbook of Mali's local health information system [Internet]. 2019 [cited 2023 Apr 12]. Available at: http://www.sante.gov.ml/index.php/nep-mali/item/3304-annonce-statistique-2018-du-systeme-local-d-information-sanitaire-du-mali.
[13] DHIS2. Mali Health Information System - SISM [Internet]. 2022 [cited 2023 May 6]. Available at: https://dhis2.snissmali.org/dhis/dhis-web-commons/security/login.action.
[14] Boushab BM, Mamoudou S, Sow M, Sounkalo D. Epidemiological, clinical and prognostic aspects of measles in the regional hospital center of Aïoun , Mauritania. Tropical medicine and health. 1 Jan 2015; 25:180 ‑3.
[15] Keita H. Trends in Measles Cases in Mali 2005-2014 FELTP Program, Ouagadougou, Burkina Faso. 2014. - Google Search [Internet]. 2014 [cited 2023 Apr 23]. Available at: https://www.google.com/search?client=ms-google-coop&q=Keita+H.+Tendances+%C3%A9volutives+des+cas+de+rougeole+au+Mali+2005-2014+ Program+FELTP,+Ouagadougou,+Burkina+Faso.+2014.&cx=006207468133305365192:xikjgz0wzec.
[16] Seck I, Faye A, Mbacké Leye MM, Bathily A, Diagne-Camara M, Ndiaye P, et al. Measles epidemic and its response in 2009, in the Dakar region, Senegal. Public health. 2012;24(2):121 ‑32.
[17] Alkassoum SI, Brah S, Djibo H, Djibo I, Kouwawo M, Batoure O. Bing. 2015 [cited 2023 May 13]. Epidemiological surveillance of measles in Niger: Analysis of the database of notifiable diseases (MDO) from 2003 to 2015. Int J Innov Sci Res. 2016; 27(2):264-74. Available at: https://www.bing.com/search?q=Alkassoum+SI%2C+Brah+S%2C+Djibo+H%2C+Djibo+I%2C+Kouwawo+M%2C+Batoure+O .+Epidemiological+surveillance+of+measles+in+Niger%3A+Analysis+of+the+database+of+notifiable+diseases+(+MDO)+from+2003+to+ 2015.+Int+J+Innov+SCI+RES.+2016%3B+27 (2)%3A264-74. & Cvid = C1EBC6AAEA994CB49F1BD4BBD8E860 & AQS = edge.0.69i59j69i11004.541J0J7 & FORM = ANNAB1.
[18] Cutts FT, Dabis F. Measles control in developing countries. Notebooks for French-speaking studies and research/Health. 1994 May 1;4(3):163 ‑71.
[19] Farhat BE, Salaaoui E, Tlili F, Tagorti R, El Berkri S, Turki R. yumpu.com. 2011 [cited 2023 May 13]. Surveillance of the target diseases of the national program of.
[20] Sounkalo D. EM-Consulte. 2008 [cited 2023 Aug 8]. B-08 Contribution of the laboratory in the epidemiological surveillance of measles in Mali. Available at: https://www.em-consulte.com/article/176864/b-08-apport-du-laboratoire-dans-la-surveillance-ep.
[21] DHIS2. Mali Health Information System - SISM [Internet]. 2022 [cited 2023 May 6]. Available at: https://dhis2.snissmali.org/dhis/dhis-web-commons/security/login.action.Viewed PDF 1588 86 -
 Assessing the Impact of Universal Test and Treat Implementation Strategy on Retention to Antiretroviral Therapy in HIV Care: A Retrospective Cohort ReviewAuthor: Caeser MagumbaDOI: 10.21522/TIJPH.2013.11.03.Art021
Assessing the Impact of Universal Test and Treat Implementation Strategy on Retention to Antiretroviral Therapy in HIV Care: A Retrospective Cohort ReviewAuthor: Caeser MagumbaDOI: 10.21522/TIJPH.2013.11.03.Art021Assessing the Impact of Universal Test and Treat Implementation Strategy on Retention to Antiretroviral Therapy in HIV Care: A Retrospective Cohort Review
Abstract:
Namibia has an adult HIV prevalence of 12.6% according to the Namibia population-based HIV impact assessment survey of 2017 making it one of the highest in the world. Early initiation of antiretroviral therapy (ART) has excellent outcomes for both morbidity and mortality. The National Strategic Framework for HIV and the Namibia Ministry of Health and Social Services (MoHSS) rolled out the WHO 2015 UTTS guidelines making Namibia one of the first African countries to implement UTTS. With UTTS guidelines, rolled out in October 2016, clients who test HIV positive are initiated on ART immediately preferably the same day or within seven days regardless of their HIV clinical stage or CD4 count. Retention in care is required for optimal clinical outcomes in patients with HIV infection. However, after two years of adopting the strategy, it is not well understood whether UTTS affects the retention to care. We therefore sought to establish any emerging differences in retention of ART care after the implementation of UTTS. We used a retrospective cohort review study design that employed both quantitative and qualitative methods. 879 client records were reviewed, 678 clients were initiated on treatment two years prior to the UTTS and 201 were initiated after January 2017 when the UTTS was fully rolled out and had been on treatment for at least 12 months. Data analysis was done using Excel and Statistical Package for Social Sciences (SPSS) version 23.0 software. The overall retention after 12 months of follow-up was (822/879) 93.5% (95% CI: 91.3% to 95.7%). The retention rate at 12 months among clients in the UTTS cohort was 95.5% (95% CI: 93.5% to 97.5%) and somewhat higher than that in the pre-UTTS cohort 92.9% (95% CI: 90.6% to 95.2%). At the end of the review period, attrition was higher in the pre-UTTS cohort 251/678 (37.0%; 95% CI 34.8 to 39.2) versus 42/201 (21.0%; 95% CI 19.0 to 23) during UTTS. Retention on ART was nearly 5% higher after UTTS implementation but young adults and men between 31 and 40 years of age had higher chances of attrition at the time of ART initiation. We recommend that all facilities in Namibia and other parts of sub-Saharan Africa should embrace the UTTS strategy to benefit their clients.
Keywords: Antiretroviral therapy, Retention, Retrospective cohort review, Universal test & treat.Assessing the Impact of Universal Test and Treat Implementation Strategy on Retention to Antiretroviral Therapy in HIV Care: A Retrospective Cohort Review
References:
[1] Namibia Population-Based HIV Impact Assessment, 2016-2017 https://phia.icap.columbia.edu/wp/content/uploads/2018/10/NAMPHIA-pdf.
[2] Namibia National Guideline for Antiretroviral Therapy 2016: https://aidsfree.usaid.gov/sites/default/files/na_national_guidelines_art.Pdf.
[3] World Health Organization. Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection. 2018: http://apps.who.int/iris/bitstream/10665/208825/1/.
[4] Temprano ANRS 12136 Study Group. A trial of early antiretrovirals and isoniazid preventive therapy in Africa. N England J Med. 2015.
[5] Antiretroviral Therapy Cohort Collaboration. Causes of death in HIV-1 –infected patients treated with antiretroviral therapy, 1996–2006: collaborative analysis of 13 HIV cohort studies. Clin Infect Dis. 2010; 50(10):1387–96.
[6] Insight Start Study Group. Initiation of antiretroviral therapy in early asymptomatic HIV infection. N Engl J Med. 2015; 373(9):795–807.
[7] Messeri PA, Abramson DM, Aidala AA, et al. The impact of ancillary HIV services on engagement in medical care in New York City. AIDS Care. 2002; 14(Suppl 1): S15–S29.
[8] Ulett KB, Willig JH, Lin HY, Routman JS, Abroms S, Allison J, et al. The therapeutic implications of timely linkage and early retention in HIV care. AIDS Patient Care STDS. 2009; 23(1):41–9.
[9] Mugavero MJ, Lin HY, Willig JH, Westfall AO, Ulett KB, Routman JS, et al. Missed visits and mortality among patients establishing initial outpatient HIV treatment. Clin Infect Dis. 2009; 48(2):248–56.
[10] Alhaj Mohammad, Amberbir Alemayehu, Singogo Emmanuel Banda Victor, Lettow Monique, Matengeni, Alfred (2019) et al. Retention on antiretroviral therapy during Universal Test and Treat implementation in Zomba district, Malawi: a retrospective cohort study. Journal of the International AIDS Society. 22. e25239. 10.1002/jia2.25239.
[11] McCreesh N, Andrianakis I, Nsubuga RN, Strong M, Vernon I, McKinley TJ, et al. Universal test, treat, and keep improving ART retention is key in cost effective HIV control in Uganda. BMC Infect Dis. 2017; 17(1):322.
[12] Brown LB, Havlir DV, Ayieko J, Mwangwa F, Owaraganise A, Kwarisiima D, High levels of retention in care with streamlined care and Universal Test and Treat in East Africa. AIDS. 2016; 30(18):2855–64.
[13] Dodd PJ, Garnett GP, Hallett TB. Examining the promise of HIV elimination by ‘test and treat’ in hyper-endemic settings. AIDS. 2010;24(5):729.
[14] Bigna JJ, Plottel CS, Koulla-Shiro S. Challenges in initiating antiretroviral therapy for all HIV-infected people regardless of CD4 cell count. Infect Dis Poverty. 2016;5(1):85.
[15] Hayes R, Sabapathy K, Fidler S. Universal testing, and treatment as an HIV prevention strategy: research questions and methods. Curr HIV Res. 2011;9 (6):429–45.
[16] Brown LB, Ayieko J, Mwangwa F, Owaraganise A, Kwarisiima D, Jain V, et al. Predictors of retention in HIV care among youth (15–24) in a Universal Test-and-Treat setting in Rural Kenya. J Acquir Immune Defic Syndr. 2017;76 (1): e15–8.
[17] Wolf HT, Halpern-Felsher BL, Bukusi EA, Agot KE, Cohen CR, Auerswald CL. “It is all about the fear of being discriminated [against]. . . the person suffering from HIV will not be accepted”: a qualitative study exploring the reasons for loss to follow-up among HIV-positive youth in Kisumu, Kenya. BMC Public Health. 2014; 14:1154.
[18] MacKenzie RK, Lettow M, Gondwe C, Nyirongo J, Singano V, Banda V, et al. Greater retention in care among adolescents on antiretroviral treatment accessing “Teen Club” an adolescent-centred differentiated care model compared with standard of care: a nested case–control study at a tertiary referral hospital in Malawi. J Int AIDS Soc. 2017;20(3): e25028.
[19] Tweya H, Gugsa S, Hosseinipour M, Speight C, Ng’ambi W, Bokosi M, et al. Understanding factors, outcomes, and reasons for loss to follow-up among women in Option B+ PMTCT programme in Lilongwe, Malawi. Trop Med Int Health. 2014;19(11):1360–6.
[20] Chan AK, Kanike E, Bedell R, Mayuni I, Manyera R, Mlotha W, et al. Same day HIV diagnosis and antiretroviral therapy initiation affects retention in Option B+ prevention of mother-to-child transmission services at antenatal care in Zomba District, Malawi. J Int AIDS Soc. 2016;19(1):20672.
[21] Lettow M, Bedell R, Mayuni I, Mateyu G, Landes M, Chan AK, et al. Towards elimination of mother-to-child transmission of HIV: performance of different models of care for initiating lifelong antiretroviral therapy for pregnant women in Malawi (Option B+). J Int AIDS Soc. 2014;17(1):18994.
[22] Jasseron C, Mandelbrot L, Dollfus C, Trocm e N, Tubiana R, Teglas JP, et al. non-disclosure of a pregnant woman’s HIV status to her partner is associated with non-optimal prevention of mother-to-child transmission. AIDS Behav. 2013; 17(2):488–97.
Viewed PDF 755 19 -
 An Assessment of Knowledge, Attitude, and Practice of Medical Professionals on Factors Related to Antimicrobial Resistance in Three (3) Selected University Teaching Hospital Complexes in Sierra Leone: A Cross-Sectional Analytic StudyAuthor: Aminata Tigiedankay KoromaDOI: 10.21522/TIJPH.2013.11.03.Art022
An Assessment of Knowledge, Attitude, and Practice of Medical Professionals on Factors Related to Antimicrobial Resistance in Three (3) Selected University Teaching Hospital Complexes in Sierra Leone: A Cross-Sectional Analytic StudyAuthor: Aminata Tigiedankay KoromaDOI: 10.21522/TIJPH.2013.11.03.Art022An Assessment of Knowledge, Attitude, and Practice of Medical Professionals on Factors Related to Antimicrobial Resistance in Three (3) Selected University Teaching Hospital Complexes in Sierra Leone: A Cross-Sectional Analytic Study
Abstract:
Although the growing increase of AMR is a major problem everywhere, developing nations like Sierra Leone are particularly at higher risk because of their limited resources to combat the problem. Medical Professionals are recognized as important determinants of antimicrobial abuse. To evaluate factors related to antimicrobial resistance patterns, a cross-sectional study was undertaken among 376 Medical Professionals. Doctors, nurses, pharmacists, laboratory Personnel and community health officer from three Sierra Leone University Teaching Hospital Complexes in Sierra Leone, formed the study population. KAP dimensions were assessed, and differences between groups were investigated, using descriptive statistics tests. The study highlighted the socio-demographic factors of health professionals (age, gender, profession, qualification, and years of experience) that were associated with antibiotic resistance training (p < 0.05). In the area of attitude towards antibiotics, 54% (203) and 72.9% (274) of study participants recommended that pharmacy staff be at their workstations to deliver services and dispense antibiotics prescribed by authorized prescribers as recommended by the Ministry of Health. Out of the total survey participants, 54.5% suggested antibiotics for laboratory-confirmed diseases. To prevent antibiotic resistance, 72.9% of survey participants advised patients to finish antibiotics. This study revealed the need for pharmacy staff to always be available to provide services and dispense antibiotics. Healthcare professionals must be monitored to combat AMR. More research is needed to understand and improve antibiotic stewardship practices in Sierra Leone.
Keywords: Antibiotic, Attitude, Knowledge, Practice, Resistance.An Assessment of Knowledge, Attitude, and Practice of Medical Professionals on Factors Related to Antimicrobial Resistance in Three (3) Selected University Teaching Hospital Complexes in Sierra Leone: A Cross-Sectional Analytic Study
References:
[1] World Health Organization. Antimicrobial resistance: global report on surveillance [Internet]. World Health Organization; 2014 [cited 2023 Jul 22]. xxii, 232 p. Available from: https://apps.who.int/iris/handle/10665/112642.
[2] Murray CJL, Ikuta KS, Sharara F, Swetschinski L, Robles Aguilar G, Gray A, et al. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. The Lancet. 2022 Feb;399(10325):629–55.
[3] National Academies of Sciences E, Division H and M, Practice B on PH and PH, States C on the LTH and EE of AR in the U, Palmer GH, Buckley GJ. The Health and Economic Burden of Resistance. In: Combating Antimicrobial Resistance and Protecting the Miracle of Modern Medicine [Internet]. National Academies Press (US); 2021 [cited 2023 Aug 2]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK577288/.
[4] Jasovský D, Littmann J, Zorzet A, Cars O. Antimicrobial resistance—a threat to the world’s sustainable development. Ups J Med Sci. 2016 Aug;121(3):159–64.
[5] Tadesse BT, Ashley EA, Ongarello S, Havumaki J, Wijegoonewardena M, González IJ, et al. antimicrobial resistance in Africa: a systematic review. BMC Infectious Diseases. 2017 Sep 11;17(1):616.
[6] AMR Review Paper - Tackling a crisis for the health and wealth of nations_1.pdf [Internet]. [cited 2022 Aug 12]. Available from: https://amr-review.org/sites/default/files/AMR%20Review%20Paper%20-%20Tackling%20a%20crisis%20for%20the%20health%20and%20wealth%20of%20nations_1.pdf.
[7] Kariuki S, Kering K, Wairimu C, Onsare R, Mbae C. Antimicrobial Resistance Rates and Surveillance in Sub-Saharan Africa: Where Are We Now? Infect Drug Resist. 2022 Jul 7; 15:3589–609.
[8] World Health Organization. Worldwide country situation analysis: response to antimicrobial resistance [Internet]. Geneva: World Health Organization; 2015 [cited 2021 Dec 9]. 42 p. Available from: https://apps.who.int/iris/handle/10665/163468.
[9] World Health Organization. Global action plan on antimicrobial resistance [Internet]. Geneva: World Health Organization; 2015 [cited 2023 Jul 25]. 28 p. Available from: https://apps.who.int/iris/handle/10665/193736.
[10] Hu Y, Wang X, Tucker JD, Little P, Moore M, Fukuda K, et al. Knowledge, Attitude, and Practice with Respect to Antibiotic Use among Chinese Medical Students: A Multicentre Cross-Sectional Study. Int J Environ Res Public Health. 2018 Jun;15(6):1165.
[11] Davey P, Marwick CA, Scott CL, Charani E, McNeil K, Brown E, et al. Interventions to improve antibiotic prescribing practices for hospital inpatients. Cochrane Database Syst Rev. 2017 Feb 9;2017(2):CD003543.
[12] Prestinaci F, Pezzotti P, Pantosti A. Antimicrobial resistance: a global multifaceted phenomenon. Pathog Glob Health. 2015 Oct;109(7):309–18.
[13] Lakoh S, John-Cole V, Luke RDC, Bell N, Russell JBW, Mustapha A, et al. Antibiotic use and consumption in Freetown, Sierra Leone: A baseline report of prescription stewardship in outpatient clinics of three tertiary hospitals. IJID Reg. 2023 Feb 20; 7:43–51.
[14] Barchitta M, Sabbatucci M, Furiozzi F, Iannazzo S, Maugeri A, Maraglino F, et al. Knowledge, attitudes and behaviors on antibiotic use and resistance among healthcare workers in Italy, 2019: investigation by a clustering method. Antimicrobial Resistance & Infection Control. 2021 Sep 10;10(1):134.
[15] Liu C, Liu C, Wang D, Zhang X. Knowledge, Attitudes and Intentions to Prescribe Antibiotics: A Structural Equation Modeling Study of Primary Care Institutions in Hubei, China. Int J Environ Res Public Health. 2019 Jul;16(13):2385.
[16] Kamara IF, Tengbe SM, Fofanah BD, Bunn JE, Njuguna CK, Kallon C, et al. Infection Prevention and Control in Three Tertiary Healthcare Facilities in Freetown, Sierra Leone during the COVID-19 Pandemic: More Needs to Be Done! Int J Environ Res Public Health. 2022 Apr 26;19(9):5275.
[17] Tasneem U, Siddiqui M, Faryal R, Shah A. Prevalence, and antifungal susceptibility of Candida species in a tertiary care hospital in Islamabad, Pakistan. Journal of the Pakistan Medical Association. 2017 Jul 1; 67:986–91.
[18] Nguyen NT, Wereley ST, Shaegh SAM. Fundamentals and Applications of Microfluidics, Third Edition. Artech House; 2019. 567 p.
[19] Liu X, He P, Chen W, Gao J. Improving Multi-Task Deep Neural Networks via Knowledge Distillation for Natural Language Understanding [Internet]. arXiv; 2019 [cited 2023 Jul 22]. Available from: http://arxiv.org/abs/1904.09482.
[20] Kanyike AM, Olum R, Kajjimu J, Owembabazi S, Ojilong D, Nassozi DR, et al. antimicrobial resistance and rational use of medicine: knowledge, perceptions, and training of clinical health professions students in Uganda. Antimicrobial Resistance & Infection Control. 2022 Nov 25;11(1):145.
[21] Erku DA. Antimicrobial Stewardship: A Cross-Sectional Survey Assessing the Perceptions and Practices of Community Pharmacists in Ethiopia. Interdisciplinary Perspectives on Infectious Diseases [Internet]. 2016 Nov 22 [cited 2023 Jan 26];2016. Available from: https://www.hindawi.com/journals/ipid/2016/5686752/.
[22] McNulty CAM, Cookson BD, Lewis MAO. Education of healthcare professionals and the public. J Antimicrob Chemother. 2012 Jul;67 Suppl 1: i11-18.
[23] Kalungia AC, Mwambula H, Munkombwe D, Marshall S, Schellack N, May C, et al. antimicrobial stewardship knowledge and perception among physicians and pharmacists at leading tertiary teaching hospitals in Zambia: implications for future policy and practice. J Chemother. 2019;31(7–8):378–87.
[24] Nathwani D, Varghese D, Stephens J, Ansari W, Martin S, Charbonneau C. Value of hospital antimicrobial stewardship programs [ASPs]: a systematic review. Antimicrobe Resist Infect Control. 2019 Feb 12;8(1):35.Viewed PDF 1015 18 -
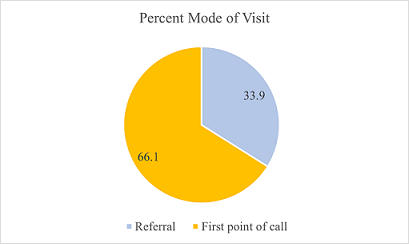 The Prevalence and Causes of Musculoskeletal Pain among Farmers in the Volta Region of Ghana: A Cross Sectional StudyAuthor: Armstrong CudjoeDOI: 10.21522/TIJPH.2013.11.03.Art023
The Prevalence and Causes of Musculoskeletal Pain among Farmers in the Volta Region of Ghana: A Cross Sectional StudyAuthor: Armstrong CudjoeDOI: 10.21522/TIJPH.2013.11.03.Art023The Prevalence and Causes of Musculoskeletal Pain among Farmers in the Volta Region of Ghana: A Cross Sectional Study
Abstract:
Musculoskeletal pain (MSK) disorder is considered one of the prime causes of severe long-term pain and physical disabilities acquired globally. Ghanaians especially, farmers have to go through vigorous physical farm activities to achieve desired output of farm activities. In the Volta Region, MSK pain has ranked among the top three reported cases at the Ho Teaching Hospital. Whilst, the quantum of reported cases is known, and treated at the hospital, the actual causes are not. Coupled with the fact that prevalence and probably the causes would differ from profession to profession the proposed research is aimed at addressing this among farmers. The overall goal of the study was to determine the prevalence and causes of MSK pain among farmers in the Volta Region of Ghana. 212 farmers were randomly selected for the study. Cross-sectional surveys were carried out to obtain the demographic and socio-economic status of the patients consenting to participate in the studies. Both, qualitative and quantitative statistical methods were employed to determine any association between the farming methods, tools used and the type of MSK pains. The most prevalent locations of MSK pain among farmers were the lower back, upper back, right and left knees. The possible causes of MSK pain reported by farmers in the Volta Region were by walking or by other transportation (riding bicycles and motorbikes) or using implements such as cutlass, hoe and spraying machine.
Keywords: Ghana, Farmers, Farming practices, Lower Back Pain, Disability-Adjusted Life Years, Work-related Musculoskeletal Disorder, Musculoskeletal pains.The Prevalence and Causes of Musculoskeletal Pain among Farmers in the Volta Region of Ghana: A Cross Sectional Study
References:
[1] Woolf, A. D., Erwin, J., & March, L. (2012). The need to address the burden of musculoskeletal conditions. In Best Practice and Research: Clinical Rheumatology, 26(2), 183–224). https://doi.org/10.1016/j.berh.2012.03.005.
[2] Kansanga, M., Andersen, P., Kpienbaareh, D., Mason-Renton, S., Atuoye, K., Sano, Y., Antabe, R., & Luginaah, I. (2019). Traditional agriculture in transition: examining the impacts of agricultural modernization on smallholder farming in Ghana under the new Green Revolution. International Journal of Sustainable Development and World Ecology, 26(1), 11–24. https://doi.org/10.1080/13504509.2018.1491429.
[3] Torgbenu, E.L., Nakua, E.K., Kyei, H. et al. Causes, trends and severity of musculoskeletal injuries in Ghana. (2017). BMC Musculoskeletal Disorder 18(349). https://doi.org/10.1186/s12891-017-1709-8.
[4] Nakua, E.K., Otupiri, E., Dzomeku, V.M., Owusu-Dabo, E., Agyei-Baffour, P., Yawson, A.E., Folson, G., & Hewlett, S.A. (2015). Gender disparities of chronic musculoskeletal disorder burden in the elderly Ghanaian population: study on global ageing and adult health (SAGE WAVE 1). BMC Musculoskeletal Disorders, 16. https://doi.org/10.1186/s12891-015-0666-3.
[5] Acquah, A.A.; A.A., D’Souza, C., Martin, B.J., Arko-Mensah, J., Dwomoh, D., Nti, A.A., Kwarteng, L., Takyi, S.A., Basu, N., Quakyi, I.A., Robins, T.G., & Fobil, J.N. (2021). Musculoskeletal Disorder Symptoms among Workers at an Informal Electronic-Waste Recycling Site in Agbogbloshie, Ghana. International Journal of Environmental Research and Public Health, 18. https://doi.org/10.3390/ijerph18042055.
[6] Osumanu, M. S. (2015). Prevalence of Musculoskeletal Disorders Among Commercial Long Distance Bus Drivers In The Greater Accra Region, Ghana. University of Ghana Digital Collections http://197.255.68.203/handle/123456789/21664.
[7] Abledu J.K., & Abledu, G.K., (2012). Multiple Logistic Regression Analysis of Predictors of Musculoskeletal Disorders and Disability among Bank Workers in Kumasi, Ghana. J Ergonomics 2(4). https://doi.org/10.4172/2165-7556.1000111.
[8] Anna, Gertrude (2020), Risk Factors Associated with Work-Related Musculoskeletal Symptoms Among Miners At Goldfields Ghana Limited, Tarkwa Mines. University of Ghana Digital Collections. https://ugspace.ug.edu.gh/bitstream/handle/123456789/36463/.
[9] The United States Department of labor. (2014). Occupational Safety and Health Administration. Ergonomics - Overview | Occupational Safety and Health Administration (osha.gov).
[10] Bernard BP, editor, U.S. Department of Health and Human Services. “Musculoskeletal disorders and workplace factors: a critical review of epidemiologic evidence for work related of the neck, upper extremity and lower back.” 1997.
[11] Canadian Center for Occupational Health and Safety, 2023, Diseases, Disorders and Injuries, Work-related Musculoskeletal Disorders (WMSDs), https://www.ccohs.ca/oshanswers/diseases/rmirsi.html.
[12] Hossain, M. D., Aftab, A., Al Imam, M. H., Mahmud, I., Chowdhury, I. A., Kabir, R. I., & Sarker, M. (2018). Prevalence of work related musculoskeletal disorders (WMSDs) and ergonomic risk assessment among ready made garment workers of Bangladesh: A cross sectional study. Plos one, 13(7), 1–18. https://doi.org/10.1371/journal.pone.0200122.
[13] Joshipura, M., Mock, C., & Gosselin, R. A. (2018). Global burden of musculoskeletal conditions. Global Orthopedics: Caring for Musculoskeletal Conditions and Injuries in Austere Settings, April, 9–11. https://doi.org/10.1007/978-1-4614-1578-7_2.
[14] Brault, M W, et al. “Prevalence and Most Common Causes of Disability Among Adults — .” United States, 2005. MMWR (2009): 58(16): 421-426.
[15] Kelley GA, Kelley KS. Community-deliverable exercise and depression in adults with arthritis: Confirmatory evidence of a meta-analysis using the IV het model. J Evid Based Med. 2018 Feb;11(1):51-55. doi: 10.1111/jebm.12229. Epub 2017 Dec 18. PMID: 28276624; PMCID: PMC5348289.
[16] Walker N, Michaud K, Wolfe F. Work limitations among working persons with rheumatoid arthritis: results, reliability, and validity of the work limitations questionnaire in 836 patients. J Rheumatol. 2005 Jun;32(6):1006-12. PMID: 15940759.
[17] Brennan-Olsen, S. L., Cook, S., Leech, M. T., Bowe, S. J., Kowal, P., Naidoo, N., Ackerman, I. N., Page, R. S., Hosking, S. M., Pasco, J. A., & Mohebbi, M. (2017). Prevalence of arthritis according to age, sex and socioeconomic status in six low and middle income countries: Analysis of data from the World Health Organization study on global Ageing and adult health (SAGE) Wave 1. BMC Musculoskeletal Disorders, 18(1), 1–12. https://doi.org/10.1186/s12891-017-1624-z.
[18] Miranda, H., Kaila-Kangas, L., Heliövaara, M., Leino-Arjas, P., Haukka, E., Liira, J., & Viikari-Juntura, E. (2010). Musculoskeletal pain at multiple sites and its effects on work ability in a general working population. Occupational and Environmental Medicine, 67(7), 449–455. https://doi.org/10.1136/oem.2009.048249
[19] Madiba, S., Hoque, M. E., & Rakgase, R. (2013). Musculoskeletal disorders among nurses in high acuity areas in a tertiary hospital in South Africa. Occupational Health Southern Africa, 19(1), 20-23.
[20] Smith, Derek R., Ning Wei, Tatsuya Ishitake, and Rui-Sheng Wang. “Musculoskeletal disorders among Chinese medical students.” The Kurume medical journal 52, no. 4 (2005): 139-146.
[21] Abla Kofi- Bediako, W., Sama, G., Yarfi, C., Ed-Bansah, D., & Appah Acquah, A. (2021). Work-Related Musculoskeletal Disorders among Nurses at the Ho Teaching Hospital, Ghana. Proceedings of the Human Factors and Ergonomics Society Annual Meeting, 65(1), 1291–1294. https://doi.org/10.1177/1071181321651342.
[22] Abledu J.K., Offei, E.B., & Abledu, G.K., (2014), Occupational and Personal Determinants of Musculoskeletal Disorders among Urban Taxi Drivers in Ghana. International Scholarly Research Notices. 2014. https://doi.org//10.1155/2014/517259.
[23] Osumanu, M. S. (2015). Prevalence of Musculoskeletal Disorders Among Commercial Long Distance Bus Drivers In The Greater Accra Region, Ghana. University of Ghana Digital Collections http://197.255.68.203/handle/123456789/21664.
[24] Torgbenu, E. L., Ashigbi, E. Y. K., Opoku, M. P., Banini, S., & Prempeh, E. B. A. (2019). Rehabilitation and management outcomes of musculoskeletal injuries in a major referral hospital in Ghana. BMC Musculoskeletal Disorders, 20(1), 1–9. https://doi.org/10.1186/s12891-019-2423-5.
[25] Plange, E. Bart (2019), work-related musculoskeletal disorders among physiotherapists in ghana: prevalence, perceived causes and coping strategies. https://ugspace.ug.edu.gh/bitstream/handle/123456789/30151/Work-Related/Musculoskeletal/Disorders/among/Physiotherapists-in-Ghana-Prevalence%2C-Perceived-Causes-and-Coping-Strategies.pdf?sequence=1.
[26] National Commission for Civic Education, NCCE, 2021, Population and Housing Census provisional results, - Volta Region | NCCE Ghana.
[27] Siedlecki, Sandra L. PhD, RN, APRN-CNS, FAAN. Understanding Descriptive Research Designs and Methods. Clinical Nurse Specialist 34(1):p 8-12, 1/2 2020. | DOI: 10.1097/NUR.0000000000000493.
[28] World Vision, Sustaining farming and livelihoods in Volta region, (2021). https://www.wvi.org/stories/ghana/sustaining-farming-and-livelihoods-volta-region.
[29] Sample size calculator, http://www.raosoft.com/samplesize.html.
[30] Crawford, J. (2007). The Nordic Musculoskeletal Questionnaire. Occupational Medicine (Lond), 57(4), 300-01.
[31] Hill, J. C., Kang, S., Benedetto, E., Myers, H., Blackburn, S., Smith, S., Dunn, K. M., Hay, E., Rees, J., Beard, D., Glyn-Jones, S., Barker, K., Ellis, B., Fitzpatrick, R., & Price, A. (2016). Development and initial cohort validation of the Arthritis Research UK Musculoskeletal Health Questionnaire (MSK-HQ) for use across musculoskeletal care pathways. BMJ Open, 6(8), 1–10. https://doi.org/10.1136/bmjopen-2016-012331.
[32] Darko, E (2021). Work-Related Musculoskeletal Disorders Among Workers of Abossey Okai Automobile Spare Parts Markets SPARE PARTS MARKET. Afribary. Retrieved from https://afribary.com/works/work-related-musculoskeletal-disorders-among-workers-of-abossey-okai-automobile-spare-parts-markets-spare-parts-market.
[33] Kabir, Elahe & Aghilinejad, Mashallah & Bahrami-Ahmadi, Amir & Abbaszadeh, Soheila & Moslemi, Sharbanou & Shahnaghi, Narges & Nassiri-Kashani, Mohammad. (2022). Role of Rice Farming in Development Risk of Musculoskeletal Disorders Among Rice Farmers: a Prospective Study in 2013. 489-494.
[34] Xiang, H., Stallones, L., & Keefe, T. J. (1999). Back pain and agricultural work among farmers: an analysis of the Colorado Farm Family Health and Hazard Surveillance Survey. American journal of industrial medicine, 35(3), 310-316.
[35] Lee H. J, Oh J-H, Yoo J.R., Ko S. Y., Kang J. H., Lee S. K., Jeong W., Seong G. M., Kang C. H, Song S. W., 2021, Prevalence of Low Back Pain and Associated Risk Factors among Farmers in Jeju, Safety and Health at Work, Volume 12, Issue 4, Pages 432-438, ISSN 2093-7911, https://doi.org/10.1016/j.shaw.2021.06.003. (https://www.sciencedirect.com/science/article/pii/S2093791121000536).
[36] Poochada, W., Chaiklieng, S., & Andajani, S. (2022). Musculoskeletal disorders among agricultural workers of various cultivation activities in upper northeastern Thailand. Safety, 8(3), 61.
[37] Malam Moussa Ahmet, H., Bika Lele, E.C., Guessogo, W.R. et al., 2023, Musculoskeletal pains among amateur and professional athletes of five disciplines in Senegal: a preliminary study. BMC Musculoskelet Disord 24, 210 (2023). https://doi.org/10.1186/s12891-023-06275-3.
Viewed PDF 1489 68 -
 Evaluation of Post-Training Monitoring of CHWs in Community-Based Epidemiological Surveillance Activities (SEBAC): Case of the Districts of Kadiolo, Kati and Kangaba in Mali from 2020 to 2021Author: Kouame Stanislas KaffloumanDOI: 10.21522/TIJPH.2013.11.03.Art024
Evaluation of Post-Training Monitoring of CHWs in Community-Based Epidemiological Surveillance Activities (SEBAC): Case of the Districts of Kadiolo, Kati and Kangaba in Mali from 2020 to 2021Author: Kouame Stanislas KaffloumanDOI: 10.21522/TIJPH.2013.11.03.Art024Evaluation of Post-Training Monitoring of CHWs in Community-Based Epidemiological Surveillance Activities (SEBAC): Case of the Districts of Kadiolo, Kati and Kangaba in Mali from 2020 to 2021
Abstract:
The post-training follow-up of actors is undeniable for an effective and efficient implementation of community surveillance activities (SEBAC). We evaluated the supervision data from the three SEBAC health districts (Kadiolo, Kati and Kangaba). The variables analyzed are as follows: The percentage of CHWs mastering the case definitions: in Kati (100%), Kangaba (82.87%) and Kadiolo (71.97%). Next, knowledge of coding: at Kati 99.18%, Kadiolo 95.62% and Kangaba 84.08%. Regarding the number of notified cases: in Kadiolo 124 cases (36%), Kati 123 (35.8%) cases and Kangaba 97 cases (28.2%). Also, for the filling of the notification and score registers: at Kati 99.18% and 100%, Kadiolo 86.18% and 86.18% and Kangaba 82.12% and 80%. As for investigations, the three districts have a parity rate of 100%; for home visits, Kati has a rate of 100%, followed by Kadiolo 95.23% and Kangaba 92.80%. Also, for the number of CHWs having sent at least one SMS: Kati 100%, Kadiolo 98.52% and Kangaba 91.50%. Finally, for data completeness, Kangaba district has 85.68%, Kadiolo 71.56% and Kati 48.91%. Post-training supervision is an effective means for building capacity in the implementation of activities, correcting shortcomings, and a source of motivation for actors.
Keywords: Supervision, community-based surveillance, post-training follow-up, SEBAC, CHW.Evaluation of Post-Training Monitoring of CHWs in Community-Based Epidemiological Surveillance Activities (SEBAC): Case of the Districts of Kadiolo, Kati and Kangaba in Mali from 2020 to 2021
References:
[1] International Federation of Red Cross and Red Crescent Societies. (IFRC). (2017). Community-based surveillance: guiding principles. CH-1211 Geneva 19 Switzerland Retrieved on 12/12/2022 from https://www.ifrc.org sites › default › files › Com.
[2] International Federation of Red Cross and Red Crescent Societies (IFRC). (2021). Community-based surveillance. Case study in Indonesia. Epidemic and Pandemic Community Preparedness Program April 2021. IFRC. Retrieved 12/12/2022 from https://www.ifrc.org sites › default › files › IFR.
[3] Living Goods. (2021). Guide to performance management. How Living Goods optimizes community health systems. Living Goods.
[4] USAID, MAHEFA and JSI. (2017). Motivations of Community Agents: MAHEFA’s multi-faceted approach to supporting the motivation of CHWs. JSI Research & Training Institute, Inc. | 44 Farnsworth Street, Boston, MA 02210 617.482.9485, Accessed 12/12/2022 from https://publications.jsi.com Inc › _download pub.
[5] N’Guessan, S., Attiey, HB, Ndiaye, S., Diarrassouba, M., McLain, G., Shamamba, L., Traoré, Y., Hamidou, RT & Karemere, H. (2019a). Community-based surveillance: A pilot experiment in the Kabadougou-Bafing-Folon health region in Côte d´Ivoire. Journal of Interventional Epidemiology and Public Health, 2(3). Retrieved 12/22/2022 from https://doi.org/10.37432/jieph.2019.2.3.20.
[6] Ridde V. (2007). The Bamako initiative 15 after: An unfinished agenda. IBRD/ The World Bank 1818 H Street, NW Washington, DC 20433. Accessed 12/23/22 at https://documents1.worldbank.org pdf › 3037.
[7] Ministry of Health & Social Affairs; Ministry of Livestock, Fisheries, Ministry of the Environment, Sanitation and Sustainable Development; The Minister of Agriculture. (2020). Guide to implementing community-based epidemiological surveillance in Mali, November 2020, 61 pages.
[8] Ministry of Health and Social Development, General Directorate of Health, and Public Hygiene. Mali MOH. 2021 [cited 2023 Aug 4]. Report of the SEBAC pilot in Mali | Mali MOH CMS. Available at: https://mali.iddsproject.org/fr/node/84.
[9] Ministry of Health & Social Affairs. Plan for the extension of community-based epidemiological surveillance in Mali. In: 1st ed. 2021. Available at: https://mali.iddsproject.org/fr/node/83.
[10] Linnea. (2022, July 19). Community health workers’ experiences of supervision in maternal and child health programs in low- and middle-income countries: A qualitative evidence synthesis. DOI: 10.1111/hsc.13893.
[11] Health 4 Africa. (2013, February 9). Supportive supervision. https://www.health4africa.net/2013/02/training-supervision/.
[12] Mark L. & Kean L. (2002). Making supervision supportive and sustainable: new approaches to old problems. Consulted on the site on 08/12/2022 on Semantic scholar.
[13] Ministry of Health and Social Development of Mali. (2022). Technical guide for integrated disease surveillance and response in Mali. MALI REP. Consulted on 23/12/22 on the site https://files.aho.afro.who.int production › files.
[14] Avortri, GS, Nabukalu, JB & Nabyonga-Orem, J. (2019). Supportive supervision to improve service delivery in low-income countries: is there a conceptual problem or a strategy problem? BMJ Global Health, 4(Suppl. 9), e001151. Retrieved 12/10/2022 from https://doi.org/10.1136/bmjgh-2018-001151.
[15] O’Donovan, J., Saul Namanda, A. & Hamala, R. (2021). Exploring supervision for volunteer community health workers in Mukono District, Uganda: An exploratory mixed-methods study. Global Public Health, 17(9), 1958-1972. Retrieved 12/16/2022 from https://doi.org/10.1080/17441692.2021.1969671.
[16] Diaby, A., Diouf, A., Azhar, SM, Sylla, A., Sall, MG, Raven, J. & Martineau, T. (2019). Perception of motivation and performance incentive among community health workers in the district of Rufisque in Senegal: a case study. African and Malagasy Review for Scientific Research / Health Science. Vol.1(No. 2). Retrieved 12/17/2022 from https://www.researchgate.net/publication/337285172.
[17] Madeleine B. Community Health Workers in Pandemics: Evidence and Investment Implications | Global Health: Science and Practice [Internet]. 2022 [cité 4 Aout 2023]. Disponible sur: https://www.ghspjournal.org/content/10/2/e2100648.
[18] 1. Kok MC, Vallières F, Tulloch O, Kumar MB, Kea AZ, Karuga R, et al. Does supportive supervision enhance community health worker motivation? A mixed-methods study in four African countries. Health Policy Plan. nov 2018;33(9):988‑98.
[19] 2. Kok MC, Dieleman M, Taegtmeyer M, Broerse JEW, Kane SS, Ormel H, et al. Which intervention design factors influence performance of community health workers in low- and middle-income countries? A systematic review. Health Policy Plan. nov 2015;30(9):1207‑27.
[20] Hill Z, Dumbaugh M, Benton L, Källander K, Strachan D, Ten Asbroek A, et al. Supervising community health workers in low-income countries – a review of impact and implementation issues. Global Health Action. déc 2014;7(1):24085.
Viewed PDF 841 23 -
 A Cross-Sectional Study Evaluating the Contribution of Systems and Structures to Tackling Antimicrobial Resistance (AMR) in Three Selected University Teaching Hospital Complexes in Sierra Leone: An Analysis of Key FactorsAuthor: Aminata Tigiedankay KoromaDOI: 10.21522/TIJPH.2013.11.03.Art025
A Cross-Sectional Study Evaluating the Contribution of Systems and Structures to Tackling Antimicrobial Resistance (AMR) in Three Selected University Teaching Hospital Complexes in Sierra Leone: An Analysis of Key FactorsAuthor: Aminata Tigiedankay KoromaDOI: 10.21522/TIJPH.2013.11.03.Art025A Cross-Sectional Study Evaluating the Contribution of Systems and Structures to Tackling Antimicrobial Resistance (AMR) in Three Selected University Teaching Hospital Complexes in Sierra Leone: An Analysis of Key Factors
Abstract:
Antimicrobial Resistance (AMR) is a global security threat that poses a significant risk to humanity. Addressing AMR requires effective organizations and processes. This study investigates the systems and structures that may contribute to tackling AMR in three Sierra Leonean University Teaching Hospital Complexes.The hospitals were selected based on their high patient load and availability of laboratory facilities for AMR testing, pharmaceuticals, and infection prevention and control (IPC) programs. Healthcare administrators and unit leaders were interviewed using a standardized questionnaire. The reliability of the questionnaires was assessed using Cronbach’s alpha coefficient. The questionnaire was pretested to ensure its validity and reliability. The findings indicate that nurses constitute a significant portion of the health workforce in the three institutions. PCMH Hospital showed the best monitoring system, covering 78% of the essential components, including, IPC guidelines, antibiotic stock verification and waste and antibiotic disposal monitoring. Connaught Hospital also met 56% of these requirements. The study showed a significant correlation between hospital bed capacity and the average patient volume (p < 0.05), with higher bed capacities resulting in higher patient volume. In addition, the correlation analysis revealed a significant association between effective monitoring mechanisms and the presence of an antibiotic stewardship program (p < 0.05). Furthermore, the availability of laboratory departments significantly influenced microbiological culture and sensitivity testing capabilities (p < 0.05), with a higher number of departments resulting in more efficient microbiological testing for antibiotic resistance. This study highlights the importance of enhancing the systems and structures of hospitals, to effectively combat AMR.
Keywords : Antimicrobial, Resistance, Structures, Systems, University Teaching Hospital.A Cross-Sectional Study Evaluating the Contribution of Systems and Structures to Tackling Antimicrobial Resistance (AMR) in Three Selected University Teaching Hospital Complexes in Sierra Leone: An Analysis of Key Factors
References:
[1] World Health Organization. Worldwide country situation analysis : response to antimicrobial resistance [Internet]. Geneva : World Health Organization ; 2015 [cited 2021 Dec 9]. 42 p. Available from : https://apps.who.int/iris/handle/10665/163468.
[2] Prestinaci F, Pezzotti P, Pantosti A. Antimicrobial resistance : a global multifaceted phenomenon. Pathog Glob Health. 2015 Oct ;109(7) :309–18.
[3] Tacconelli E, Sifakis F, Harbarth S, Schrijver R, van Mourik M, Voss A, et al. Surveillance for control of antimicrobial resistance. The Lancet Infectious Diseases. 2018 Mar 1 ;18(3) : e99–106.
[4] Antimicrobial Resistance Collaborators. Global burden of bacterial antimicrobial resistance en 2019 : à systematic analysis. Lancet. 2022 Jan 18 ; S0140-6736(21)02724-0.
[5] Antibiotic resistance [Internet]. [Cited 2021 Jun 28]. Available from : https://www.who.int/news-room/fact-sheets/detail/antibiotic-resistance.
[6] Sartelli M, Weber DG, Ruppé E, Bassetti M, Wright BJ, Ansaloni L, et al. Antimicrobials : à global alliance for optimizing their rational use in intra-abdominal infections (AGORA). World Journal of Emergency Surgery. 2016 Jul 15 ;11(1) :33.
[7] Zhang Z, Hu Y, Zou G, Lin M, Zeng J, Deng S, et al. Antibiotic prescribing for upper respiratory infections among children in rural China : a cross-sectional study of outpatient prescriptions. Glob Health Action. 2017 May 2 ;10(1) :1287334.
[8] Rochford C, Sridhar D, Woods N, Saleh Z, Hartenstein L, Ahlawat H, et al. Global governance of antimicrobial resistance. The Lancet. 2018 May 19 ;391(10134) :1976–8.
[9] Mhondoro M, Ndlovu N, Bangure D, Juru T, Gombe NT, Shambira G, et al. Trends in antimicrobial resistance of bacterial pathogens in Harare, Zimbabwe, 2012–2017 : a secondary dataset analysis. BMC Infectious Diseases. 2019 Aug 27 ;19(1) :746.
[10] Kanu JS, Khogali M, Hann K, Tao W, Barlatt S, Komeh J, et al. National Antibiotic Consumption for Human Use in Sierra Leone (2017–2019) : A Cross-Sectional Study. Tropical Medicine and Infectious Disease. 2021 Jun ;6(2) :77.
[11] Volpi C, Shehadeh F, Mylonakis E. Correlation of antimicrobial prescription rate and county income in medicare part D. Medicine (Baltimore). 2019 May 31 ;98(22) : e15914.
[12] Kanu JS, Khogali M, Hann K, Tao W, Barlatt S, Komeh J, et al. National Antibiotic Consumption for Human Use in Sierra Leone (2017–2019) : A Cross-Sectional Study. Tropical Medicine and Infectious Disease. 2021 Jun ;6(2) :77.
[13] Lakoh S, John-Cole V, Luke RDC, Bell N, Russell JBW, Mustapha A, et al. Antibiotic use and consumption in Freetown, Sierra Leone : A baseline report of prescription stewardship in outpatient clinics of three tertiary hospitals. IJID Reg. 2023 Feb 20 ;7 :43–51.
[14] Kanu JS, Khogali M, Hann K, Tao W, Barlatt S, Komeh J, et al. National Antibiotic Consumption for Human Use in Sierra Leone (2017–2019) : A Cross-Sectional Study. Tropical Medicine and Infectious Disease. 2021 Jun ;6(2) :77.
[15] WHO consolidated guidelines on tuberculosis - NCBI Bookshelf [Internet]. [Cited 2023 Aug 14]. Available from : https://www.ncbi.nlm.nih.gov/books/NBK588564/.
[16] World Health Organization. Worldwide country situation analysis : response to antimicrobial resistance [Internet]. Geneva : World Health Organization ; 2015 [cited 2021 Dec 9]. 42 p. Available from : https://apps.who.int/iris/handle/10665/163468.
[17] Human Resources for Health Country Profile. 2016.
[18] Premji SS, Hatfield J. Call to Action for Nurses/Nursing. Biomed Res Int. 2016 ;2016 :3127543.
[19] Kurth AE, Jacob S, Squires AP, Sliney A, Davis S, Stalls S, et al. Investing in Nurses is a Prerequisite for Ensuring Universal Health Coverage. J Assoc Nurses AIDS Care. 2016 ;27(3) :344–54.
[20] Moyo P, Moyo E, Mangoya D, Mhango M, Mashe T, Imran M, et al. Prevention of antimicrobial resistance in sub-Saharan Africa : What has worked ? What still needs to be done ? Journal of Infection and Public Health. 2023 Apr 1 ;16(4) :632–9.
[21] D’Arcy N, Ashiru-Oredope D, Olaoye O, Afriyie D, Akello Z, Ankrah D, et al. Antibiotic Prescribing Patterns in Ghana, Uganda, Zambia and Tanzania Hospitals : Results from the Global Point Prevalence Survey (G-PPS) on Antimicrobial Use and Stewardship Interventions Implemented. Antibiotics. 2021 Sep ;10(9) :1122.
[22] Tiwari A, Kurittu P, Al-Mustapha AI, Heljanko V, Johansson V, Thakali O, et al. Wastewater surveillance of antibiotic-resistant bacterial
pathogens : A systematic review. Frontiers in Microbiology [Internet]. 2022 [cited 2023 Jul 25] ;13. Available from : https://www.frontiersin.org/articles/10.3389/fmicb.2022.977106.[23] Iera J, Seghieri C, Tavoschi L, Isonne C, Baccolini V, Petrone D, et al. Early Warning Systems for Emerging Profiles of Antimicrobial Resistance in Italy : A National Survey. International Journal of Environmental Research and Public Health. 2023 Jan ;20(9) :5623.
[24] IJERPH | Free Full-Text | Early Warning Systems for Emerging Profiles of Antimicrobial Resistance in Italy : A National Survey [Internet]. [Cited 2023 Jul 25]. Available from : https://www.mdpi.com/1660-4601/20/9/5623.
[25] Kersh EN, Pham CD, Papp JR, Myers R, Steece R, Kubin G, et al. Expanding U.S. Laboratory Capacity for Neisseria gonorrhoeae Antimicrobial Susceptibility Testing and Whole-Genome Sequencing through the CDC’s Antibiotic Resistance Laboratory Network. J Clin Microbiol. 2020 Mar 25 ;58(4) : e01461-19.
[26] Umutesi G, Velin L, Muwanguzi M, Faktor K, Mugabo C, Rukundo G, et al. Strengthening Antimicrobial Resistance Diagnostic Capacity in Rural Rwanda : A Feasibility Assessment. Ann Glob Health. 2021 ;87(1) :78.
Viewed PDF 818 19 -
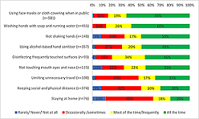 Predicting the Adoption of COVID-19 Public Health Preventive Measures in Ethiopia: Application of Health Belief ModelAuthor: Luwaga LilianeDOI: 10.21522/TIJPH.2013.11.03.Art026
Predicting the Adoption of COVID-19 Public Health Preventive Measures in Ethiopia: Application of Health Belief ModelAuthor: Luwaga LilianeDOI: 10.21522/TIJPH.2013.11.03.Art026Predicting the Adoption of COVID-19 Public Health Preventive Measures in Ethiopia: Application of Health Belief Model
Abstract:
In the face of coronavirus disease pandemic, adherence to public health measures largely influences their effectiveness in containing the spread. Four specific objectives guided this study: (i) Assess whether individuals are adhering to the COVID-19 preventive measures promoted by Ethiopian government; (ii) Examine the heterogeneity in adoption of preventive measures in Ethiopia; (iii) Identify the factors affecting adherence to preventive measures-based health belief model; and (iv) Examine the moderating effects of socio-economic factors on the relationship between adherence to preventive measures and HBM factors. The study relied on a nationally representative cross-sectional survey commissioned by the World Health Organization in 2021 for Ethiopia. Data was collected from 895 individuals aged 18 years of age or older. Analysis applied several methods including the Multiple Correspondence Analysis, Univariate analysis, hierarchical cluster analysis, cluster analysis and multiple regression analysis. Using face masks and washing hands were the most frequently practiced preventive measures. The regression analysis indicated that perceived severity, perceived barriers, and cues to action showed a significant association with adherence at p >0.05. Furthermore, socio-economic factors have a moderating role on adherence to preventive measures and HBM factors. Effective promotion and adoption of preventive measures require addressing individuals' perceptions of severity and benefits while minimizing barriers and providing clear cues to action. Additionally, specific preventive measures that require ongoing effort and habit development may face challenges in adoption. Tailoring interventions can help overcome these challenges and encourage the widespread adoption of preventive measures to curtail the spread.
Keywords: Coronavirus disease - 2019, Prevention, Health belief model.Predicting the Adoption of COVID-19 Public Health Preventive Measures in Ethiopia: Application of Health Belief Model
References:
[1] Jebril, Nadia., (2020). World Health Organization declared a pandemic public health menace: A systematic review of the coronavirus disease 2019 “COVID-19”, up to 26th March 2020. Available at SSRN 3566298.
[2] WHO. first case of COVID-19 Confirmed in Ethiopia. 2020 [cited 2021 2/19/23021]; Available from: https://www.afro.who.int/news/first-case-Covid-19-confirmed-ethiopia.
[3] Chan, K.H. and K.-Y. Yuen, COVID-19 epidemic: disentangling the re-emerging controversy about medical facemasks from an epidemiological perspective. International Journal of Epidemiology, 2020. 49(4): p. 1063-1066.
[4] Morawska, L. and D.K. Milton, it is time to address airborne transmission of coronavirus disease 2019 (COVID-19). Clinical Infectious Diseases, 2020. 71(9): p. 2311-2313.
[5] Tadesse, S. and W. Muluye, The impact of COVID-19 pandemic on education systems in developing countries: a review. Open Journal of Social Sciences, 2020. 8(10): p. 159-170.
[6] Yan, E., et al., Predicting public adherence to Covid-19 preventive measures: A cross-sectional study in Hong Kong. International Journal of Environmental Research and Public Health, 2021. 18(23): p. 12403.
[7] Gebreheat, G., et al., Adherence to COVID-19 preventive measures and associated factors in Ethiopia: A systematic review and meta-analysis. PLoS One, 2022. 17(10): p. e0275320.
[8] de Bruin, Y.B., et al., Initial impacts of global risk mitigation measures taken during the combatting of the COVID-19 pandemic. Safety Science, 2020: p. 104773.
[9] Azene, Z.N., et al., Correction: Adherence towards COVID-19 mitigation measures and its associated factors among Gondar City residents: A community-based cross-sectional study in Northwest Ethiopia. PloS one, 2021. 16(8): p. e0256954.
[10] Tamirat, T. and L. Abute, Adherence towards COVID‐19 prevention measures and associated factors in Hossana town, South Ethiopia, 2021. International Journal of Clinical Practice, 2021. 75(12): p. e14530.
[11] Desalegn, Z., et al., COVID-19 and the public response: Knowledge, attitude, and practice of the public in mitigating the pandemic in Addis Ababa, Ethiopia. PloS one, 2021. 16(1): p. e0244780.
[12] Abeya, S.G., et al., Adherence to COVID-19 preventive measures and associated factors in Oromia regional state of Ethiopia. PloS one, 2021. 16(10): p. e0257373.
[13] Jones, C.L., et al., The health belief model as an explanatory framework in communication research: exploring parallel, serial, and moderated mediation. Health communication, 2015. 30(6): p. 566-576.
[14] Seid, M.A. and M.S. Hussen, Knowledge, and attitude towards antimicrobial resistance among final year undergraduate paramedical students at University of Gondar, Ethiopia. BMC infectious diseases, 2018. 18: p. 1-8.
[15] Adli, I., et al., Knowledge, attitude, and practice related to the COVID-19 pandemic among undergraduate medical students in Indonesia: A nationwide cross-sectional study. PLoS One, 2022. 17(1): p. e0262827.
[16] Harris, D., et al., The effect of COVID-19 and government response measures on poor and vulnerable groups in urban areas in Ethiopia. London, UK: Oxford Policy Management, 2020.
[17] Shewasinad Yehualashet, S., et al., Predictors of adherence to COVID-19 prevention measure among communities in North Shoa Zone, Ethiopia based on health belief model: A cross-sectional study. PloS one, 2021. 16(1): p. e0246006.
[18] Kebede, Y., et al., Knowledge, perceptions, and preventive practices towards COVID-19 early in the outbreak among Jimma university medical center visitors, Southwest Ethiopia. PloS one, 2020. 15(5): p. e0233744.
[19] Lau, L.L., et al., Knowledge, attitudes, and practices of COVID-19 among income-poor households in the Philippines: A cross-sectional study. Journal of Global Health, 2020. 10(1).
[20] Talic, S., et al., Effectiveness of public health measures in reducing the incidence of COVID-19, SARS-CoV-2 transmission, and COVID-19 mortality: systematic review and meta-analysis. BMJ, 2021. 375.
[21] Ayouni, I., et al., Effective public health measures to mitigate the spread of COVID-19: a systematic review. BMC Public Health, 2021. 21(1): p. 1-14.
[22] Dwipayanti, N.M.U., D.S. Lubis, and N.P.A. Harjana, Public perception and hand hygiene behavior during COVID-19 pandemic in Indonesia. Frontiers in Public Health, 2021. 9: p. 543.
[23] Singanayagam, A., et al., Community transmission and viral load kinetics of the SARS-CoV-2 delta (B. 1.617. 2) variant in vaccinated and unvaccinated individuals in the UK: a prospective, longitudinal, cohort study. The lancet Infectious Diseases, 2022. 22(2): p. 183-195.
[24] Mansilla Domínguez, J.M., et al., Risk perception of COVID− 19 community transmission among the Spanish population. International Journal of Environmental Research and Public Health, 2020. 17(23): p. 8967.
[25] Mannan, D.K.A. and K.M. Farhana, Knowledge, attitude, and acceptance of a COVID-19 vaccine: A global cross-sectional study. International Research Journal of Business and Social Science, 2020. 6(4).
[26] Abdelhafiz, A.S., et al., Knowledge, perceptions, and attitude of Egyptians towards the novel coronavirus disease (COVID-19). Journal of Community Health, 2020. 45: p. 881-890.
[27] Chan, E.Y.Y., et al., Sociodemographic predictors of health risk perception, attitude and behavior practices associated with health-emergency disaster risk management for biological hazards: the case of COVID-19 pandemic in Hong Kong, SAR China. International Journal of Environmental Research and Public Health, 2020. 17(11): p. 3869.
[28] Cha, S.E., X. Ku, and I. Choi, Post COVID-19, still wear a face mask? Self-perceived facial attractiveness reduces mask-wearing intention. Frontiers in Psychology, 2023. 14.
[29] Zewdie, A., et al., The health belief model’s ability to predict COVID-19 preventive behavior: A systematic review. Sage Open Medicine, 2022. 10: p. 20503121221113668.
[30] Oldeweme, A., et al., The role of transparency, trust, and social influence on uncertainty reduction in times of pandemics: empirical study on the adoption of COVID-19 tracing apps. Journal of Medical Internet Research, 2021. 23(2): p. e25893.
[31] Papageorge, N.W., et al., Socio-demographic factors associated with self-protecting behavior during the COVID-19 pandemic. Journal of Population Economics, 2021. 34: p. 691-738.
[32] Dryhurst, S., et al., Risk perceptions of COVID-19 around the world. Journal of Risk Research, 2020. 23(7-8): p. 994-1006.
[33] Roozenbeek, J., et al., Susceptibility to misinformation about COVID-19 around the world. Royal Society open science, 2020. 7(10): p. 201199.
[34] Kim, Y.-I., et al., Infection and rapid transmission of SARS-CoV-2 in ferrets. Cell host & microbe, 2020. 27(5): p. 704-709. e2.
[35] Farooq, A., S. Laato, and A.N. Islam, Impact of online information on self-isolation intention during the COVID-19 pandemic: cross-sectional study. Journal of Medical Internet research, 2020. 22(5): p. e19128.
[36] Prati, G. and L. Pietrantoni, the relation of perceived and received social support to mental health among first responders: a meta‐analytic review. Journal of Community Psychology, 2010. 38(3): p. 403-417.Viewed PDF 979 37 -
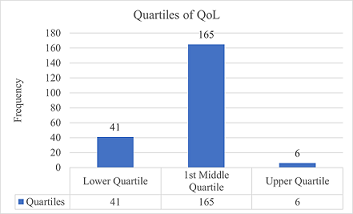 The Impact of Musculoskeletal Pain on the Quality of Life of Farmers in the Volta Region of GhanaAuthor: Armstrong CudjoeDOI: 10.21522/TIJPH.2013.11.03.Art027
The Impact of Musculoskeletal Pain on the Quality of Life of Farmers in the Volta Region of GhanaAuthor: Armstrong CudjoeDOI: 10.21522/TIJPH.2013.11.03.Art027The Impact of Musculoskeletal Pain on the Quality of Life of Farmers in the Volta Region of Ghana
Abstract:
The incidence of musculoskeletal (MSK) pain among farmers in Ghana is high. In the Volta Region, where the proposed research was conducted, MSK pain is among the top three most reported cases at the Ho Teaching Hospital. While the number of cases is known and treated at the hospital, the root causes are not. The proposed study investigated the effects of MSK pain on the quality of life (QoL) of farmers in the Region, to determine whether the age and sex of farmers in the Volta Region have any relationship with QoL, and to determine whether their knowledge about MSD and QoL was adequate to inform on its management. A total of 212 farmers were selected for the study without any particular order. Cross-sectional surveys were conducted to obtain the demographic and socioeconomic status of the participants. Both qualitative and quantitative statistical methods were used to determine the impact of MSK pain on QoL, the relationship between age/sex and QoL and if the farmers in the Volta Region think they have enough knowledge about their MSDs and are confident in managing them. The study found that the QoL among the farmers was very low. The farmers' QoL was below the average grouped quality of life and about 26.5% can be said to be clearly above the average grouped quality of life. MSK pains have had a huge toll on the quality of life of Volta Region farmers affecting about 73.5% of the respondent farmers.
Keywords: DALY, HRQoL, NMQ, MSK-HQ, MSK, Musculoskeletal pain, Quality of Life, Farmers in Ghana.The Impact of Musculoskeletal Pain on the Quality of Life of Farmers in the Volta Region of Ghana
References:
[1] Al-Sari, U. A., Tobias, J., & Clark, E. (2016). Health-related quality of life in older people with osteoporotic vertebral fractures: a systematic review and meta-analysis. Osteoporosis International 27(10), 2891–2900. https://doi.org/10.1007/s00198-016-3648-x.
[2] Beaudart, C., Biver, E., Bruyère, O., Cooper, C., Al-Daghri, N., Reginster, J. Y., & Rizzoli, R. (2018). Quality of life assessment in musculo-skeletal health. Aging Clinical and Experimental Research, 30(5), 413–418. https://doi.org/10.1007/s40520-017-0794-8.
[3] Walsh NE, Brooks P, Hazes JM, Walsh RM, Dreinhöfer K, Woolf AD, Akesson K, Lidgren L; Bone and Joint Decade Task Force for Standards of Care for Acute and Chronic Musculoskeletal Pain. Standards of care for acute and chronic musculoskeletal pain: the Bone and Joint Decade (2000-2010). Arch Phys Med Rehabil. 2008 Sep;89(9):1830-45. doi: 10.1016/j.apmr.2008.04.009. PMID: 18760171.
[4] Racine EF, Laditka SB, Dmochowski J, Alavanja MC, Lee DC, Hoppin JA. Farming activities and carrying and lifting: the Agricultural Health Study. J Phys Act Health. 2012 Jan;9(1):39-47. doi: 10.1123/jpah.9.1.39. PMID: 22232503; PMCID: PMC3257835.
[5] Wolf AM, Siadaty MS, Crowther JQ, Nadler JL, Wagner DL, Cavalieri SL, Elward KS, Bovbjerg VE. Impact of lifestyle intervention on lost productivity and disability: improving control with activity and nutrition. J Occup Environ Med. 2009 Feb;51(2):139-45. doi: 10.1097/JOM.0b013e3181965db5. PMID: 19209034; PMCID: PMC2688905.
[6] Williams, A, et al. “Musculoskeletal conditions may increase the risk of chronic disease: a systematic review and meta-analysis of cohort studies.” BMC Med 16.167 (2018).
[7] World Vision, Sustaining farming and livelihoods in Volta region, (2021). https://www.wvi.org/stories/ghana/sustaining-farming-and-livelihoods-volta-region.
[8] C H Roux, F Guillemin, S Boini, F Longuetaud, N Arnault, S Hercberg, S Brianc¸on, 2004, Impact of musculoskeletal disorders on quality of life: an inception cohort study:Annals of the Rheumatic Diseases 2005;64:606-611.
[9] Sergio Vargas-Prada, David Coggon, 2015, Psychological and psychosocial determinants of musculoskeletal pain and associated disability, Best Practice & Research Clinical Rheumatology, Volume 29, Issue 3, 2015, Pages 374-390, ISSN 1521-6942, https://doi.org/10.1016/j.berh.2015.03.003. (https://www.sciencedirect.com/science/article/pii/S1521694215000066).
[10] Erick, P., & Smith, D. (2011). A systematic review of musculoskeletal disorders among school teachers. BMC Musculoskeletal Disorders, 12(260), 1-11.
[11] Jaiswal, N., & Mesaria, S. (2015). Musculoskeletal disorders among teachers residing in various nations: a review. Research Journal of Recent Sciences, 4(2015), 23-27.
[12] Chacha, B., & Zani, A. (2015). The impact of Free Primary Education on pupil-teacher ratio in Kuria East Constituency, Kenya. IOSR Journal of Humanities And Social Science, 20(5), 1-12.
[13] Wang’eri, T., & Okello, L. (2014). Role overload, teacher-pupil-ratio, school type, years of teaching experience, gender and burn out as factors related to work stress among primary school teachers in Kasarani Division, Nairobi County, Kenya. Global Journal of Human-Social Science Linguistics & Education, 14(1), 54-64.
[14] Bodhare T, Valsangkar S, Bele S. (2011), An epidemiological study of work-related musculoskeletal disorders among construction workers in karimnagar, andhra pradesh. Indian J Community Med. 2011 Oct;36(4):304-7. doi: 10.4103/0970-0218.91420. PMID: 22279263; PMCID: PMC3263153.
[15] World Health Organisation, Musculoskeletal Health (2022). https://www.who.int/news-room/fact-sheets/detail/musculoskeletal-conditions.
[16] Middleswort, M. (2016). The definition and causes of musculoskeletal disorders (MSDs). Retrieved June 14, 2016, from Ergonomics Plus: http://ergo-plus.com/musculoskeletal-disorders-msd/.
[17] GBD 2019 Diseases and Injuries Collaborators. “Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the global burden of disease study 2019.” Lancet 396 (2020): 1204-1222.
[18] da Costa, BR and ER Vieira . “Risk factors for work-related musculoskeletal disorders: a systematic review of recent longitudinal studies.” Am J Ind Med 53 (2010): 285-323.
[19] Ul-Haq, Z., Mackay, D. F., & Pell, J. P. (2014). Association between physical and mental health-related quality of life and adverse outcomes; A retrospective cohort study of 5,272 Scottish adults. BMC Public Health, 14(1), 1–10. https://doi.org/10.1186/1471-2458-14-1197.
[20] National Commission for Civic Education (2021). Population and Housing Census provisional results, 2021 Population and Housing Census provisional results - Volta Region | NCCE Ghana.
[21] Siedlecki, Sandra L. PhD, RN, APRN-CNS, FAAN. Understanding Descriptive Research Designs and Methods. Clinical Nurse Specialist 34(1):p 8-12, 1/2 2020. | DOI: 10.1097/NUR.0000000000000493.
[22] Sample size calculator, http://www.raosoft.com/samplesize.html.
[23] Crawford, J. (2007). The Nordic Musculoskeletal Questionnaire. Occupational Medicine (Lond), 57(4), 300-01.
[24] Norton, S., Ellis, B., Suárez, B. S., Schwank, S., Fitzpatrick, R., Price, A., & Galloway, J. (2019). Validation of the Musculoskeletal Health Questionnaire in inflammatory arthritis: A psychometric evaluation. Rheumatology (United Kingdom), 58(1), 45–51. https://doi.org/10.1093/rheumatology/key240.
[25] Chartered Society of Physiotherapy (2023), The implementation of and improvement in the musculoskeletal health questionnaire (MSK-HQ) scores at a MSK Outpatient Department, https://www.csp.org.uk/innovations/implementation-improvement-musculoskeletal-health-questionnaire-msk-hq-scores-msk#:~:text=The%20MSK%2DHQ%20is%20a,a%20better%20MSK%2DHQ%20status.
[26] Joanne O. Crawford, The Nordic Musculoskeletal Questionnaire, Occupational Medicine, Volume 57, Issue 4, June 2007, Pages 300–301, https://doi.org/10.1093/occmed/kqm036.
[27] J-Pal, 2023, Data Cleaning and Management, https://www.povertyactionlab.org/resource/data-cleaning-and-management
[28] Investopedia, 2023, Descriptive Statistics: Definition, Overview, Types, Example, https://www.investopedia.com/terms/d/descriptive_statistics.asp.
[29] Roshani K. Prematunga, 2012, Correlational analysis, Australian Critical Care, Volume 25, Issue 3, 2012, Pages 195-199, ISSN 1036-7314, https://doi.org/10.1016/j.aucc.2012.02.003. (https://www.sciencedirect.com/science/article/pii/S1036731412000410).
[30] SAGE Publications, 2010, Qualitative Data, Analysis, and Design, https://www.sagepub.com/sites/default/files/upm-binaries/43144_12.pdf.
[31] Barneo-Alcántara, M., Díaz-Pérez, M., Gómez-Galán, M., Carreño-Ortega, Á., Callejón-Ferre, Á.J. (2021). Musculoskeletal Disorders in Agriculture: A Review from Web of Science Core Collection. Agronomy 11, 201. https://doi.org/10.3390/agronomy11102017.
[32] Shuler, K.A, Zeng, P., Danforth, M.E. (2012). Upper limb ethereal change with the transition to agriculture in the southeastern United States: A view from Moundville and the central Tombigbee River valley. Homo, 63, 413–434.
[33] Eshed, V., Gopher, A., Galili, E., & Hershkovitz, I. (2004). Musculoskeletal stress markers in Natufian hunter-gatherers and Neolithic farmers in the levant: The upper limb. Am. J. Phys. Anthr. 123 (303–315)
[34] Peterson, J. (2010). Domesticating gender: Neolithic patterns from the southern Levant. J. Anthr. Archaeol.29, 249–264.
[35] Vega-Fernández G, Lera L, Leyton B, Cortés P, Lizana PA. Musculoskeletal Disorders Associated With Quality of Life and Body Composition in Urban and Rural Public School Teachers. Front Public Health. 2021 Jun 1;9:607318. doi: 10.3389/fpubh.2021.607318. PMID: 34141698; PMCID: PMC8203816.
[36] Strømnes LA, Ree H, Gjesdal K, Ariansen I. Sex Differences in Quality of Life in Patients With Atrial Fibrillation: A Systematic Review. J Am Heart Assoc. 2019 Apr 16;8(8):e010992. doi: 10.1161/JAHA.118.010992. PMID: 30957624; PMCID: PMC6507196.
[37] Zakerian, S. A., Monazzam, M. R., Dehghan, S. F., Mohraz, M. H., Safari, H., & Asghari, M. (2013). Relationship between knowledge of ergonomics and workplace conditions with musculoskeletal disorders among nurses: A questionnaire survey. World Appl Sci J, 24(2), 227-33.
Viewed PDF 1113 41 -
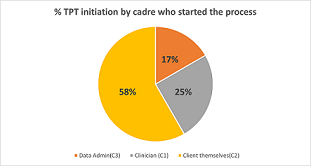 Scaling Up the Uptake of Tuberculosis Preventative Therapy among HIV Positive Clients at Okahao Clinic, Northern Namibia; A Quality Improvement Capstone ProjectAuthor: Caeser MagumbaDOI: 10.21522/TIJPH.2013.11.03.Art028
Scaling Up the Uptake of Tuberculosis Preventative Therapy among HIV Positive Clients at Okahao Clinic, Northern Namibia; A Quality Improvement Capstone ProjectAuthor: Caeser MagumbaDOI: 10.21522/TIJPH.2013.11.03.Art028Scaling Up the Uptake of Tuberculosis Preventative Therapy among HIV Positive Clients at Okahao Clinic, Northern Namibia; A Quality Improvement Capstone Project
Abstract:
Globally over 10.4 million people fell ill with TB, of which 1.7 million died from the disease in 2016. And in the same year, 40% of HIV deaths were due to TB. 95% of TB deaths occur in low- and middle-income countries, and Namibia has one of the highest case notification rates (CNR) of TB in the world. Tuberculosis Presumptive Therapy (TPT) treats latent TB infection, and this reduces the likelihood that active TB disease will develop. Whereas Namibia adopted TPT use for PLHIV in 2005, the national coverage has remained low and was estimated to be 35% in June 2018, and specifically at 42% for Okahao, ART Clinic. We therefore designed a quality improvement project to scale up the uptake of TPT at this clinic. We used both quantitative and qualitative methods. We conducted health education sessions daily for 15 minutes, and patients were taught about TPT. Three categories of clients were registered according to those who suggested TPT initiation. Category one (C1) were those where a clinician suggested TPT, Category two (C2) by the client themselves and category three (C3) by data administrators. We analyzed data using simple excel spread sheets as either trend graphs or pie charts. Category two had more clients started on TPT (n=1,609, 58.3%). TPT coverage within the backlog cohort improved from 42% to 94%, and for the new cohort, coverage increased from 81% to 100%. 13 clients (64%) reported skin related manifestations as side effects. Daily health education about TPT in HIV care settings improves uptake.
Keywords: TB Presumptive Therapy (TPT), Uptake, HIV positive, Quality improvement project.Scaling Up the Uptake of Tuberculosis Preventative Therapy among HIV Positive Clients at Okahao Clinic, Northern Namibia; A Quality Improvement Capstone Project
References:
[1] R. Wood and L-G Bekker. (2014) Isoniazid preventive therapy for tuberculosis in South Africa: An assessment of the local evidence base. South Africa Medical Journal 104(3):174-177. DOI: 10.7196/SAMJ.7968.
[2] Danyuttapolchai J, Kittimunkong S, Nateniyom S, Painujit S, Klinbuayaem V, Maipanich N, et al. (2017) Implementing an isoniazid preventive therapy program for people living with HIV in Thailand. PLoS ONE 12(9): e0184986. https://doi.org/10.1371/journal.pone.0184986.
[3] Ayele et al. (2015) Effect of isoniazid preventive therapy on tuberculosis or death in persons with HIV: a retrospective cohort study. BMC Infectious Diseases 15:334 DOI 10.1186/s12879-015-1089-3.
[4] N. P. Spyridis, P. G. Spyridis et al. (2007) The Effectiveness of a 9-Month Regimen of Isoniazid Alone versus 3- and 4-Month Regimens of Isoniazid plus Rifampin for Treatment of Latent Tuberculosis Infection in Children: Results of an 11-Year Randomized Study. Clinical Infectious Diseases; 45:715–22
[5] S. M. Hermans, A. D. Grant, et al. (2016) The timing of tuberculosis after isoniazid preventive therapy among gold miners in South Africa: a prospective cohort study. BMC Medicine 14:45 DOI 10.1186/s12916-016-0589-3.
[6] Namibia Population6-Based HIV Impact Assessment, 2016-2017: https://phia.icap.columbia.edu/wpcontent/uploads/2018/10/NAMPHIA-pdf.
[7] Namibia7 National Guideline for Antiretroviral Therapy 2016: https://aidsfree.usaid.gov/sites/default/files/na_national_guidelines_art.Pdf.
[8] C. Padmapriyadarsini8, M. Das, et al. (2018) Is Chemoprophylaxis for Child Contacts of Drug-Resistant TB Patients Beneficial? A Systematic Review. Tuberculosis Research and Treatment, Article ID 3905890, 8 pages. https://doi.org/10.1155/2018/3905890.
[9] Thomas R. Frieden9, Harold W. Jaffe, et al. (2011) Recommendations for Use of an Isoniazid-Rifapentine Regimen with Direct Observation to Treat Latent Mycobacterium Tuberculosis Infection. CDC Morbidity and Mortality Weekly Report 60:48.
[10] Lauren Hart10. (2011) Isoniazid Preventive Therapy for the Prevention of Tuberculosis in People Living with HIV/AIDS. Moving Evidence into Action.www.FHI360.org.
[11] Gavin J. Churchyard, Katherine L. Fielding, et al. (2014) A Trial of Mass Isoniazid Preventive Therapy for Tuberculosis Control. The New England Journal of Medicine 370:17, 1661-1663.
[12] J. E. Golub, S. Cohn et al. (2015) Long-term Protection from Isoniazid Preventive Therapy for Tuberculosis in HIV-Infected Patients in a Medium-Burden Tuberculosis Setting: The TB/HIV in Rio (THRio) Study. Clinical Infectious Diseases 60:4, 639-645.
[13] Basenero A, Kaliba S (2020); Using a Quality Improvement Collaborative Approach to Improve Tuberculosis prevention therapy coverage in the Kavango region, Namibia.
[14] Temprano ANRS 12136 Study Group. A trial of early antiretrovirals and isoniazid preventive therapy in Africa. N England J Med. 2015.
Viewed PDF 776 20 -
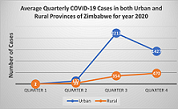 COVID-19 Infections and Deaths between Rural and Urban Provinces of Zimbabwe, 2020: A Spatial Variations AnalysisAuthor: Blessing SilwanganiDOI: 10.21522/TIJPH.2013.11.03.Art029
COVID-19 Infections and Deaths between Rural and Urban Provinces of Zimbabwe, 2020: A Spatial Variations AnalysisAuthor: Blessing SilwanganiDOI: 10.21522/TIJPH.2013.11.03.Art029COVID-19 Infections and Deaths between Rural and Urban Provinces of Zimbabwe, 2020: A Spatial Variations Analysis
Abstract:
Zimbabwe continues to record new COVID-19 cases as is the case in other countries. Although the Ministry of Health in Zimbabwe continues to publish daily situation reports (SitRep), and regular surveillance updates, no review of existing data has been done to establish the regional trends of the disease over time. This desk review study seeks to analyze the trends (province by province) of the COVID-19 in Zimbabwe for year 2020 in order to establish if spatial variations in infection rates and deaths exist. Ultimately, the aim is to come up with appropriate context-specific prevention and control measures. The study also seeks to establish whether or not there is a difference in COVID-19 infection rates and deaths between urban and rural provinces of Zimbabwe. A historical research design that made use of available secondary data on COVID-19 in Zimbabwe was used. COVID-19 statistics for year 2020 as provided by the Zimbabwe Ministry of Health and Child Care were accessed from the website and reviewed. A hypothesis test to determine if there was a difference in COVID-19 attack rates between urban and rural provinces of Zimbabwe was also done. An independent samples t-test using Microsoft excel was done on cumulative COVID-19 cases data for the entire year 2020. The study revealed that spatial variations in COVID-19 infections and deaths between urban and rural provinces of Zimbabwe existed. Urban provinces recorded more COVID-19 cases in 2020 compared to rural provinces.
Keywords: COVID-19, Infection rate, Psychological distress, Spatial, Variations, Vaccine hesitancy.COVID-19 Infections and Deaths between Rural and Urban Provinces of Zimbabwe, 2020: A Spatial Variations Analysis
References:
[1] Murewanhema, G., Burukai, T., Mazingi, D., Maunganidze, F., Mufunda, J., Munodawafa, D., & Pote, W., 2020, A descriptive study of the trends of COVID-19 in Zimbabwe from March-June 2020: policy and strategy implications. Pan African Medical Journal. 2020 Nov 9;37(Suppl 1):33. doi: 10.11604/pamj.supp.2020.37.33.25835. PMID: 33456657; PMCID: PMC7796830, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7796830/.
[2] World Health Organization. Coronavirus disease (COVID-19) situation report 162. 2020. Jun 30, Accessed 9 September 2023 from https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports.
[3] World Health Organization. Coronavirus disease (COVID-19) situation report 163. 1 July 2020, https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200701-covid-19-sitrep-163.pdf.
[4] Government of Zimbabwe, Ministry of Health and Child Care, COVID 19 Daily Updates retrieved from http://www.mohcc.gov.zw/index.php?option=com_phocadownload&view=category&id=15&Itemid=741&limitstart=20.
[5] Zimbabwe COVID-19 Situation Report, Issue No 10 31032020 Issue No 10 Zimbabwe COVID-19 Sitrep.pdf.
[6] Murewanhema, G., & Makurumidze, R., 2020, Essential health services delivery in Zimbabwe during the COVID-19 pandemic: perspectives and recommendations. Pan Afr Med J. 2020 Aug 11;35(Suppl 2):143. doi: 10.11604/pamj.supp.2020.35.143.25367. PMID: 33193958; PMCID: PMC7608772.
[7] World Health Organization. Guidance Document for a Differentiated Response to COVID-19 Outbreak in Urban and Rural settings 2021 Retrieved from https://www.afro.who.int/sites/default/files/Covid-19/Techinical%20documents/Guidance%20Document%20for%20a%20Differentiated%20Response%20to%20COVID-19%20Outbreak%20in%20Urban%20and%20Rural%20settings.pdf.
[8] Black, J.M & Ubbes, V.A., 2009, Historical Research: A Thematic Analysis of Convention and Conference Themes for Selected Professional Health Education Associations from 1975 to 2009, International Electronic Journal of Health Education, 2009;12:33-47 https://www.researchgate.net/publication/233858380_Historical_Research_A_Thematic_Analysis_of_Convention_and_Conference_Themes_for_Selected_Professional_Health_Education_Associations_from_1975_to_2009.
[9] Desmet, K., & Wacziarg, R., 2020, Understanding Spatial Variation in COVID-19 across the United States National Bureau of Economic Research ,1050 Massachusetts, MA 02138 June 2020, https://www.nber.org/system/files/working_papers/w27329/revisions/w27329.rev0.pdf.
[10] Turner-Musa, J., Ajayi, O., & Kemp, L., 2020, Examining social determinants of health, stigma, and COVID-19 disparities. Healthcare. 2020 Jun 12;8(2):168, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7349778/.
[11] Santibañez, S., Bellis, K.S., Bay, A., Chung, C.L., Bradley, K., Gibson, D., et al., 2019, Strengthening rural states’ capacity to prepare for and respond to emerging infectious diseases, 2013–2015. Southern Medical Journal. 2019 Feb;112(2):101–5. pmid:30708375, https://pubmed.ncbi.nlm.nih.gov/30708375/.
[12] Sun, Y., & Monnat, S.M., 2022, Rural-urban and within-rural differences in COVID-19 vaccination rates. J Rural Health. 2022 Sep;38(4):916-922. doi: 10.1111/jrh.12625. Epub 2021 Sep 23. PMID: 34555222; PMCID: PMC8661570, https://pubmed.ncbi.nlm.nih.gov/34555222/.
[13] The obstacles to combat against COVID-19 pandemic and the remedies: Bangladesh scenario Journal of Public Health Research. Doi: https://journals.sagepub.com/doi/full/10.4081/jphr.2021.26271.
[14] Aabed, K., & Lashin, M.M.A., 2021, An analytical study of the factors that influence COVID-19 spread. Saudi J Biol Sci. 2021 Feb;28(2):1177-1195. doi: 10.1016/j.sjbs.2020.11.067. Epub 2020 Nov 26. PMID: 33262677; PMCID: PMC7690266, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7690266/.
[15] Cuadros, D.F., Branscum, A.J., Mukandavire, Z., Miller, F.D., MacKinnon, N., 2021, Dynamics of the COVID-19 epidemic in urban and rural areas in the United States. Ann Epidemiol. 2021 Jul; 59:16-20. doi: 10.1016/j.annepidem.2021.04.007. Epub 2021 Apr 22. PMID: 33894385; PMCID: PMC8061094, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8061094/.
[16] Karim, S.A., & Chen, H.F., 2021, Deaths From COVID-19 in Rural, Micropolitan, and Metropolitan Areas: A County-Level Comparison. J Rural Health. 2021 Jan;37(1):124-132. doi: 10.1111/jrh.12533. Epub 2020 Nov 6. PMID: 33155723, https://pubmed.ncbi.nlm.nih.gov/33155723/.
[17] Ezeh, A., Oyebode, O., Satterthwaite, D., Chen, Y. F., Ndugwa, R., Sartori, J., & Lilford, R. J., 2017, The history, geography, and sociology of slums and the health problems of people who live in slums. The lancet, 389(10068), 547– 558, https://pubmed.ncbi.nlm.nih.gov/27760703/.
[18] Liu, T., Gong, D., Xiao, J., Hu, J., He, G., Rong, Z., & Ma, W., 2020, Cluster infections play important roles in the rapid evolution of COVID-19 transmission: A systematic review. Int J Infect Dis. 2020 Oct; 99:374-380. doi: 10.1016/j.ijid.2020.07.073. Epub 2020 Aug 5. PMID: 32768702; PMCID: PMC7405860, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7405860/.
[19] Zhang, Y., Zhang, A., & Wang, J., 2020, Exploring the roles of high-speed train, air, and coach services in the spread of COVID-19 in China. Transp Policy (Oxf). 2020 Aug; 94:34-42. doi: 10.1016/j.tranpol.2020.05.012. Epub 2020 May 26. PMID: 32501380; PMCID: PMC7248624, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7248624/.
[20] Hu, M., Lin, H., Wang, J., Xu, C., Tatem, A.J., Meng, B., Zhang, X., Liu, Y., Wang, P., Wu, G., Xie, H., & Lai, S., 2021, Risk of Coronavirus Disease 2019 Transmission in Train Passengers: An Epidemiological and Modeling Study. Clin Infect Dis. 2021 Feb 16;72(4):604-610. doi: 10.1093/cid/ciaa1057. PMID: 32726405; PMCID: PMC7454391, https://pubmed.ncbi.nlm.nih.gov/32726405/.
[21] Feng, Y., Zhang, Y., Ding, X., Fan, Y., & Ge, J., 2023, Multi-scale risk assessment and mitigations comparison for COVID-19 in urban public transport: A combined field measurement and modeling approach. Build Environ. 2023 Aug 15; 242:110489. doi: 10.1016/j.buildenv.2023.110489. Epub 2023 Jun 2. PMID: 37333517; PMCID: PMC10236904, https://pubmed.ncbi.nlm.nih.gov/37333517/.
[22] Bwerinofa I.J, Mahenehene J, Manaka M, et al. What is ‘community resilience’? Responding to COVID- 19 in rural Zimbabwe. BMJ Global Health 2022;7: e009528. doi:10.1136/bmjgh-2022-009528.
[23] Factors influencing parents’ hesitancy to vaccinate their children aged 5–11 years old against COVID-19: results from a cross-sectional study in Malaysia. https://doi.org/10.3389/fpubh.2023.1091015.
[24] Factors influencing the acceptability of COVID-19 vaccination: A cross-sectional study from Malaysia. Vacunas Journal. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8407950/; https://www.sciencedirect.com/science/article/pii/S1576988721000479#.
[25] COVID-19 Vaccine Hesitancy and Confidence in the Philippines and Malaysia: A Cross-sectional Study of Sociodemographic Factors and Digital Health Literacy. PLOS Global Public Health. October 17, 2022.
[26] COVID-19 Vaccine Hesitancy in Rural and Urban Communities: A global survey. Frontiers in Public Health. September 26, 2022. https://doi.org/10.3389/fpubh.2022.958668.
[27] Knowledge, Attitude and Practices Toward Coronavirus Disease (COVID- 19) in Southeast and South Asia: A Mixed Study Design Approach. Frontiers in Public Health. June 21, 2022. https://doi.org/10.3389/fpubh.2022.875727.
[28] Digital health literacy for COVID-19 vaccination and intention to be immunized: a cross sectional multi-country study among the general adult population Frontiers in Public Health. Frontiers in Public Health, 16 September 2022Sec. Public Health Education and Promotion; https://doi.org/10.3389/fpubh.2022.998234.
[29] The potential association of COVID-19 and Psychological Distress and Anxiety in Iran International Journal of Epidemiology and Health Sciences December 2022;3: http://www.ijehs.com/article_254985_6a8c46f2c5c2024a15dac171ed8d66cd.pdf.
[30] Factors Associated with Psychological Distress Among Myanmar Residents During Covid-19 Pandemic Crises. Journal of Public Health Research. Doi: https://journals.sagepub.com/doi/full/10.4081/jphr.2021.2279
[31] Depression and anxiety in Malaysian population during third wave of the COVID-19 pandemic. https://doi.org/10.1016/j.cegh.2021.100868.
[32] A survey of psychological distress among Bangladeshi people during the COVID-19 pandemic: Clinical Epidemiology and Global Health. January 14, 2021. https://doi.org/10.1016/j.cegh.2020.100693.
[33] Mental health, risk perception, and coping strategies among healthcare workers in Egypt during the COVID-19 pandemic. February 27, 2023. Plos one https://doi.org/10.1371/journal.pone.0282264.
[34] Demographic and work-related factors associated with burnout, resilience, and quality of life among healthcare workers during the COVID-19 pandemic: A cross sectional study from Malaysia. Front. Public Health, 16 December 2022. Sec. Public Health Education and Promotion. https://doi.org/10.3389/fpubh.2022.1021495.
[35] Burnout, resilience and the quality of life among Malaysian healthcare workers during the COVID-19 pandemic Frontiers in Public Health, 30 November 2022. Sec. Public Health Education and Promotion. https://doi.org/10.3389/fpubh.2022.1021497.
[36] Impact of COVID-19 pandemic on mental health, risk perception and coping strategies among health care workers in Albania - evidence that needs attention. Clinical Epidemiology and Global Health Volume 12, October–December 2021, 100824. Doi: https://doi.org/10.1016/j.cegh.2021.100824.
[37] The immediate impact of COVID-19 on mental health and its associated factors among healthcare workers: A global perspective across 31 countries. Journal of Global Health. August 23, 2021. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7649521/.
[38] Palestinian Healthcare Workers Mental Health Challenges during COVID-19 Pandemic: A Cross-Sectional Study. Medical Research Archives. October 31, 2022. https://esmed.org/MRA/index.php/mra/article/view/3125.
Viewed PDF 882 27 -
 Microbial Contamination of Toothbrush and Methods to Overcome - A ReviewAuthor: Murukesan SDOI: 10.21522/TIJPH.2013.11.03.Art030
Microbial Contamination of Toothbrush and Methods to Overcome - A ReviewAuthor: Murukesan SDOI: 10.21522/TIJPH.2013.11.03.Art030Microbial Contamination of Toothbrush and Methods to Overcome - A Review
Abstract:
Numerous microbes found in household toothbrushes can lead to contamination of the oral cavity. These microorganisms can survive on the toothbrush for several days or weeks. Several studies have found a link between tooth decay and toothbrush bacterial residues. As a result, toothbrush disinfection is critical for toothbrush and oral hygiene maintenance. Furthermore, brush disinfection is required to prevent disease transmission, especially in children, the elderly, and high-risk patients, such as those with immunodeficiency or undergoing organ transplants or chemotherapy. This paper aims to analyse various methods of decontaminating toothbrushes. Numerous techniques have been discussed in the literature regarding decontamination of toothbrushes between uses. However, no single completely efficacious technique has been found to the said effect. Therefore, the search is still on for a rapidly effective, cost-effective, nontoxic, and easily implementable suitable alternative.
Keywords: Chemical, Contamination, Decontamination, Physical, Toothbrush.Microbial Contamination of Toothbrush and Methods to Overcome - A Review
References:
[1] Aarati, N., Ranganath, N. N., Soumya, B. G., Kishore, B., & Mithun, K.,2011, Evaluation of antibacterial and anticandidial efficacy of aqueous and alcoholic extract of neem (Azadirachta indica, An in vitro study. International Journal of Research in Ayurveda and Pharmacy, 2, 230–235.
[2] Abd-Ulnabi, R. M.,2012, Bacterial contamination of toothbrushes with comparison of healthy and dental patients. Basrah J. Sci., 30, 120–130.
[3] Ahmad, I., & Beg, A. Z.,2001, Antimicrobial and phytochemical studies on 45 Indian medicinal plants against multi-drug resistant human pathogens. Journal of Ethnopharmacology, 74(2), 113–123.
[4] Aldigs, E. K.,2013, Toothbrushes: A potential health risk. Egyptian Journal of Experimental Biology (Botany), 9, 259–263.
[5] Amin, M., Kazemi, M., & Rasaie, N.,2012, In vitro comparison of the effects of garlic juice and chlorhexidine mouthwash on oral pathogens. Jundishapur Journal of Microbiology, 5(2), 398–400.
[6] Amirabadi, F., & Sasannejad, S.,2016, Evaluation of the antimicrobial effects of various methods to disinfect toothbrushes contaminated with Streptococcus mutans. International Journal of Medical Research and Health Sciences, 5, 536–540.
[7] Anand, P. J., Athira, S., Chandramohan, S., Ranjith, K., Raj, V. V., & Manjula, V. D.,2016, January–February, Comparison of efficacy of herbal disinfectants with chlorhexidine mouthwash on decontamination of toothbrushes: An experimental trial. Journal of International Society of Preventive and Community Dentistry, 6(1), 22–27.
[8] Assari, A. S., Mohammed Mahrous, M., Ahmad, Y. A., Alotaibi, F., Alshammari, M., AlTurki, F., & AlShammari, T.,2022, January 11, Efficacy of different sterilization techniques for toothbrush decontamination: An ex vivo study. Cureus, 14(1), e21117.
[9] Balappanavar, A. Y., Nagesh, L., Ankola, A. V., Tangade, P. S., Kakodkar, P., & Varun, S.,2009, June 1, Antimicrobial efficacy of various disinfecting solutions in reducing the contamination of the toothbrush-A comparative study. Oral Health and Preventive Dentistry, 7(2), 137–145.
[10] Bélanger-Giguère, K., Giguère, S., & Bélanger, M.,2011, Disinfection of toothbrushes contaminated with Streptococcus mutans. American Journal of Dentistry, 24(3), 155–158.
[11] Bhat, P. K., Badiyani, B. K., Sarkar, S., Chengappa, S., & Bhaskar, N. N.,2012, Effectiveness of antimicrobial solutions on streptococcus mutans in used toothbrushes. World Journal Dent, 3, 6–10.
[12] Bhat, S. S., Hegde, K. S., & George, R. M.,2003, Microbial contamination of toothbrushes and their decontamination. Journal of the Indian Society of Pedodontics and Preventive Dentistry, 21(3), 108–112.
[13] Bunetel, L., Tricot-Doleux, S., Agnani, G., & Bonnaure-Mallet, M.,2000, In vitro evaluation of the retention of three species of pathogenic microorganisms by three different types of toothbrush. Oral Microbiology and Immunology, 15(5), 313–316. https://doi.org/10.1034/j.1399-302x.2000.150508.x
[14] Caudry, S. D., Klitorinos, A., & Chan, E. C.,1995, Contaminated toothbrushes and their disinfection. Journal. Canadian Dental Association, 61(6), 511–516.
[15] Chen, Y.-Y., Chiu, H.-C., & Wang, Y.-B.,2009, Effect of garlic extract on acid production and growth of streptococcus mutans. Journal of Food and Drug Analysis, 17(1), 59–63. https://doi.org/10.38212/2224-6614.2309
[16] Chibebe, J., Jr., & Pallos, D.,2001, Evaluation of sterilization of toothbrushes in a microwave oven (in vitro study, Rev. Biociênc, 7, 39–42.
[17] Cugini, M. A., Warren, P. R., & Cugini, M.,2006, May 1, The Oral-B Cross Action manual toothbrush: A 5-year literature review. Journal, 72(4), 323.
[18] da Silva, F. C., Kimpara, E. T., Mancini, M. N., Balducci, I., Jorge, A. O., & Koga-Ito, C. Y.,2008, Effectiveness of six different disinfectants on removing five microbial species and effects on the topographic characteristics of acrylic resin. Journal of Prosthodontics, 17(8), 627–633.
[19] Dalirsani, Z., Aghazadeh, M., Adibpour, M., Amirchaghm, M., Pakfetrat, A., Mozaffari, P. M., Mehdipour, M., & Zenooz, A. T.,2011, In vitro comparison of the antimicrobial activity of ten herbal extracts against Streptococcus mutans with chlorhexidine. Journal of Applied Sciences, 11(5), 878–882.
[20] Dayoub, M. B., Rusilko, D., & Gross, A.,1977, Microbial contamination of toothbrushes. Journal of Dental Research, 56(6) (6, article 706), 706.
[21] Efstratiou, M., Papaioannou, W., Nakou, M., Ktenas, E., Vrotsos, I. A., & Panis, V.,2007, Contamination of a toothbrush with antibacterial properties by oral microorganisms. Journal of Dentistry, 35(4), 331–337.
[22] Fani, M. M., Kohanteb, J., & Dayaghi, M.,2007, Inhibitory activity of garlic (Allium sativum) extract on multidrug-resistant Streptococcus mutans. Journal of the Indian Society of Pedodontics and Preventive Dentistry, 25(4), 164–168.
[23] Glass, R. T.,1992, The infected toothbrush, the infected denture, and transmission of disease: A review. Compendium, 13(7), 592–598.
[24] Glass, R. T.,1992, Toothbrush types and retention of microorganisms: How to choose a biologically sound toothbrush. Journal – Oklahoma Dental Association, 82(3), 26–28.
[25] Gujjari, S. K., Gujjari, A. K., Patel, P. V., & Shubhashini, P. V.,2011, Comparative evaluation of ultraviolet and microwave sanitization techniques for toothbrush decontamination. Journal of International Society of Preventive and Community Dentistry, 1(1), 20–26.
[26] Ilić, D., Nikolić, V., Ćirić, A., Soković, M., Stanojković, T., Kundaković, T. et al.,2012, Cytotoxicity and antimicrobial activity of allicin and its transformation products. Journal of Medicinal Plants Research, 6, 59–65.
[27] Komiyama, E. Y., Back-Brito, G. N., Balducci, I., & Koga-Ito, C. Y.,2010, Evaluation of alternative methods for the disinfection of toothbrushes. Brazilian Oral Research, 24(1), 28–33.
[28] Lee, M. O.,2004, Bacteriological contamination of toothbrushes by dental plaque acidogenicity and related behaviors to toothbrush use. J. Korean Soc. Dent Hyg., 4, 255–263.
[29] Lee, S. G., Kang, B. R., Kim, H. S., Park, H. H., Park, H. R., Yoon, S. K., & Nam, S. H.,2017, Changes in the number of bacteria in a toothbrush according to the toothbrush management method. Biomedical Research, 28, 7306–7310.
[30] Makino, S. I., Cheun, H. I., Tabuchi, H., & Shirahata, T.,2000, Antibacterial activity of chaff vinegar and its practical application. Journal of Veterinary Medical Science, 62(8), 893–895.
[31] Mehta, A., Sequeira, P. S., & Bhat, G.,2007, Bacterial contamination and decontamination of toothbrushes after use. New York State Dental Journal, 73(3), 20–22.
[32] Mitrakul, K., Srisatjaluk, R. L., Srisukh, V., & Vongsawan, K.,2015, Efficacy of Citrus hystrix sprays in decontaminating Streptococcus mutans on childrens toothbrushes. Scienceasia, 41(1), 28–34.
[33] Nascimento, A. P., Watanabe, E., & Ito, I. Y.,2010, Toothbrush contamination by Candida spp. and efficacy of mouthrinse spray for their disinfection. Mycopathologia, 169(2), 133–138.
[34] Nelson-Filho, P., Isper, A. R., Assed, S., Faria, G., & Ito, I. Y.,2004, Effect of triclosan dentifrice on toothbrush contamination. Pediatric Dentistry, 26(1), 11–16.
[35] Pathak, A. K.,2012, Anti-candida activity of aqueous extracts of some herbals. Indian J. Fund Appl. Life Sci., 2, 1–6.
[36] Peker, I., Akca, G., Sarikir, C., Alkurt, M. T., & Celik, I.,2014, Effectiveness of alternative methods for toothbrush disinfection: An in vitro study. The Scientific World Journal, 2014, 726190.
[37] Prabhakar, A. R., Ahuja, V., & Basappa, N.,2009, Effect of curry leaves, garlic, and tea tree oil on streptococcus mutans and lactobacilli in children: A clinical and microbiological study. Bras Res Pediatr. Dent Int. Clin., 9, 259–263.
[38] Quirynen, M., de Soete, M., Pauwels, M., Goossens, K., Teughels, W., van Eldere, J., & van Steenberghe, D.,2001, Bacterial survival rate on tooth- and interdental brushes in relation to the use of toothpaste. Journal of Clinical Periodontology, 28(12), 1106–1114.
[39] Quirynen, M., De Soete, M., Pauwels, M., Gizani, S., Van Meerbeek, B., & van Steenberghe, D.,2003, Can toothpaste or a toothbursh with antibacterial tufts prevent toothbrush contamination? Journal of Periodontology, 74(3), 312–322.
[40] Salvia, A. C., Matilde, S., Rosa, F. C., Kimpara, E. T., Jorge, A. O., Balducci, I., & Koga-Ito, C. Y.,2013, Disinfection protocols to prevent cross-contamination between dental offices and prosthetic laboratories. Journal of Infection and Public Health, 6(5), 377–382.
[41] Sato, S., Pedrazzi, V., Guimarães Lara, E. H., Panzeri, H., Ferreira de Albuquerque, R. F., & Ito, I. Y.,2005, Antimicrobial spray for toothbrush disinfection: An in vivo evaluation. Quintessence International, 36(10), 812–816.
[42] Schlein, R. A., Kudlick, E. M., Reindorf, C. A., Gregory, J., & Royal, G. C.,1991, Toothbrushing and transient bacteremia in patients undergoing orthodontic treatment. American Journal of Orthodontics and Dentofacial Orthopedics, 99(5), 466–472.
[43] Sconyers, J. R., Crawford, J. J., & Moriarty, J. D.,1973, Relationship of bacteremia to toothbrushing in patients with periodontitis. Journal of the American Dental Association, 87(3), 616–622.
[44] Shin, A. R., & Nam, S. H.,2018, Antimicrobial effects of various methods for the disinfection of contaminated toothbrushes. Biomedical Research, 29(13), 2880–2884.
[45] Silva, M. M., Vergani, C. E., Giampaolo, E. T., Neppelenbroek, K. H., Spolidorio, D. M., & Machado, A. L.,2006, Effectiveness of microwave irradiation on the disinfection of complete dentures. International Journal of Prosthodontics, 19(3), 288–293.
[46] Sogi, S. H., Subbareddy, V. V., & Kiran, S. N.,2002, Contamination of toothbrush at different time intervals and effectiveness of various disinfecting solutions in reducing the contamination of toothbrush. Journal of the Indian Society of Pedodontics and Preventive Dentistry, 20(3), 81–85.
[47] Tomar, P., Hongal, S., Saxena, V., Jain, M., Rana, K., & Ganavadiya, R.,2014, Evaluating sanitization of toothbrushes using ultraviolet rays and 0.2% chlorhexidine solution: A comparative clinical study. Journal of Basic and Clinical Pharmacy, 6(1), 12–18.
[48] Turner, L. A., McCombs, G. B., Hynes, W. L., & Tolle, S. L.,2009, A novel approach to controlling bacterial contamination on toothbrushes: Chlorhexidine coating. International Journal of Dental Hygiene, 7(4), 241–245.
[49] Warren, D. P., Goldschmidt, M. C., Thompson, M. B., Adler-Storthz, K., & Keene, H. J.,2001, The effects of toothpastes on the residual microbial contamination of toothbrushes. Journal of the American Dental Association, 132(9), 1241–1245.
[50] Wetzel, W. E., Schaumburg, C., Ansari, F., Kroeger, T., & Sziegoleit, A.,2005, Microbial contamination of toothbrushes with different principles of filament anchoring. Journal of the American Dental Association, 136(6), 758–65.
Viewed PDF 1062 31

