Table of Contents - Issue
Recent articles
-
 Prevalence and Risk Factors of Hepatitis B Virus Infection among a Cohort of Primary Health Care Workers in NigeriaAuthor: Orji Ikechukwu AnthonyDOI: 10.21522/TIJPH.2013.11.01.Art001
Prevalence and Risk Factors of Hepatitis B Virus Infection among a Cohort of Primary Health Care Workers in NigeriaAuthor: Orji Ikechukwu AnthonyDOI: 10.21522/TIJPH.2013.11.01.Art001Prevalence and Risk Factors of Hepatitis B Virus Infection among a Cohort of Primary Health Care Workers in Nigeria
Abstract:
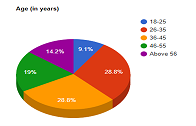
Hepatitis B Virus (HBV) infection is one of the most infectious diseases globally. Nigeria is among the endemic countries for HBV, with a National prevalence of 11%. The Primary Healthcare Center (PHC) is critical for interrupting the transmission of HBV infection. Consequently, the baseline information concerning the prevalence, associated risk factors, and vaccination status of the health workers for HBV is required for the system strengthening, hence, the need for this study. To determine the prevalence of HBV among health workers in PHCs in AMAC, Abuja. 2. To identify the risk factors associated with HBV infection amongst this cohort. A hospital-based cross-sectional descriptive study involving 168 randomly selected PHC health workers. Data was collected with a structured questionnaire, and participants were screened for HBsAg. Data were analyzed using SPSS version 21.0 with results significant at p-value < 0.05. 168 respondents participated in the study, 65.5% were females, and the mean age was 34 +/- 9 years. The full vaccination rate was 44%, while the prevalence of HBV infection was 4.8%. The history of dental procedure was the only significant predictor of HBV infection, and those who had the dental procedure were thrice more likely to be infected with HBV than their counterparts (OR: 3.077). The prevalence of HBV in this study is low, per, National prevalence, but high for this cohort of health workers with a considerable Hepatitis B vaccination rate. There is a need to strengthen health workers' HBV screening and vaccination in addition to improving infection prevention and control in dental clinics/surgeries.
Keywords: HBV Infection, Health-worker, Primary Healthcare Center, Prevalence, Risk Factors.Prevalence and Risk Factors of Hepatitis B Virus Infection among a Cohort of Primary Health Care Workers in Nigeria
References:
[1] World Health Organization. Guidelines for the prevention, care, and treatment of persons with chronic hepatitis B infection [internet]. 2015 [cited Feb 2021]. Available from www.who.int/hepatitis/publications/hepatitis-b-guidelines/en/.
[2] World Health Organization. Global alert response: Hepatitis B [internet]. 2014 [cited Feb 2021]. Available from http://www.who.int/csr/disease/hepatitis/whocdscsrlyo20022/en/index2.html.
[3] Mukhtar I. G, Yakasai, B.W, Muhammad S. M, Salisu A. I. 2018. Prevalence of hepatitis b virus surface antigen and hepatitis c virus antibody among prospective blood donors at Murtala Muhammad specialist hospital, kano, Nigeria. Journal of Pure and Applied Sciences. 4 (1): 170-176. Available from https://www.researchgate.net/publication/329591929.
[4] World Health Organization. Global hepatitis report, 2017 [internet]. 2017 [cited Feb 2021]. Available from www.who.int/hepatitis/publications/global-hepatitis-report2017/en/.
[5] World Health Organization. Hepatitis B, Key Facts [internet]. 2019 [cited Feb 2021]. Available from www.who.int/news-room/fact-sheets/detail/hepatitis-b.
[6] Schad V.A. Global prevalence of hepatitis B virus (HBV) infection in 2016 estimated [internet]. 2018 [cited Feb 2021]. Available from https://www.infectiousdiseaseadvisor.com/home/advisor-channels/hepatitis-advisor/global-prevalence-of-hepatitis-b-virus-infection-in-2016-estimated/.
[7] Abutu A. Nigeria’s complicated hepatitis burden. The lancet. Gastroenterology & hepatology. 2018; 3 (10): 669. Available from DOI: doi.org/10.1016/S2468-1253 (18)30279-.
[8] Orji I. A, & Okoli U. T. Prevalence of Hepatitis-B infection among Pregnant Women in a Primary Healthcare Centre in Abuja, Nigeria. Texila International Journal of Public Health. 2016; 4 (4): Art. 57. Available from DOI: 10.21522/TIJPH.2013.04.04.
[9] Anaedobe CG, Fowotade A, Omoruyi CE, Bakare RA. 2015. Prevalence, socio-demographic features, and risk factors of Hepatitis B virus infection among pregnant women in Southwestern Nigeria. Pan African Medical Journal. 20: 406. Available from www.panafrican-med-journal.com/content/article/20/406/full/ doi:10.11604/pamj.2015.20.406.6206.
[10] Yakasai IB, Ayuba R, Abubakar IS, Ibrahim SA. 2012 Jan-Dec; Sero-prevalence of Hepatitis B Virus Infection and its Risk factors among Pregnant Women Attending Antenatal Clinic at Aminu Kano Teaching Hospital, Kano, Nigeria. Journal of Basic and Clinical Reproductive Sciences. 1 (1 & 2). Available from www.jbcrs.org DOI: 10.4103/2278-960X.104297.
[11] Esan A.J, Omisakin C.T, Ojo-Bola T, Wooden M.F, Fasakin K.A, Ogunleye A. A. 2014; Sero- Prevalence of Hepatitis B and Hepatitis C Virus Co-Infection among Pregnant Women in Nigeria. American Journal of Biomedical Research. 2 (1): 11-15. Available from http://pubs.sciepub.com/ajbr/2/1/3.
[12] Desalegn Z, Mihret A, Beyene H.B, Yilma M, Seid Y, Tamiru W, et al. 2016; Survey of Hepatitis B virus infection and risk factors among pregnant women at public hospital in Ethiopia. International Journal of Biomedical Research. 7(7): 450-456. Available from DOI: 10.7439/ijbr.
[13] Tanga AT, Teshome MA, Hiko D, Fikru C, Jilo GK. 2019; Sero-prevalence of hepatitis B virus and associated factors among pregnant women in Gambella hospital, South-western Ethiopia: facility based cross-sectional study. BMC Infectious Diseases. 19: 602 Available from https://doi.org/10.1186/s12879-019-4220-z.
[14] Osman A.M.M, Mirghani O.A, Gasim G.I, Adam I. 2014; Hepatitis B Virus, Hepatitis C Virus, and Human Immunodeficiency Virus Infections among Pregnant Women in Central Sudan. Sudan Journal of Medical Sciences. 9 (2): 91-96.
[15] Coste M., De Sèze M., Diallo A., et al. 2019; Burden and impacts of chronic hepatitis B infection in rural Senegal: study protocol of a cross-sectional survey in the area of Niakhar (AmBASS ANRS 12356). BMJ Open. 9: e030211. Available from doi:10.1136/ bmjopen-2019-030211.
[16] Rabiu KA, Akinola OI, Adewunmi AA, Omololu OM, Ojo TO. 2010 Aug; Risk factors for hepatitis B virus infection among pregnant women in Lagos, Nigeria. Acta Obstetrician Et Gynecologica Scandinavica. 89: 1024–1028. Available from https://www.researchgate.net/publication/45268763. DOI: 10.3109/00016349.2010.482580.
[17] Glen S. Sample size in statistics (How to find it): Excel, Cochran’s formula, general tips. From Statistics HowTo.com: Elementary statistics for the rest of us [internet]. 2020 [cited March 2021]. Available from https://www.statisticshowto.com/probability-and-statistics/find-sample-size/.
[18] Ola SO, Odaibo GN, Olaleye OD, et al. 2012; Hepatitis B and E viral infections among Nigerian healthcare workers. Afr J Med Sci. 41: 387–391.
[19] Mueller A, Stoetter L, Kalluvya S, Stich A, Majinge C, Weissbrich B, Kasang C. 2015 Sep 23; Prevalence of hepatitis B virus infection among health care workers in a tertiary hospital in Tanzania. BMC Infect Dis. 15:386. doi: 10.1186/s12879-015-1129-z. PMID: 26399765; PMCID: PMC4581415.
[20] Alqahtani JM, Abu-Eshy SA, Mahfouz AA, et al. Sero-prevalence of hepatitis B and C virus infections among health students and health care workers in the Najran region, southwestern Saudi Arabia: the need for national guidelines for health students. BMC Pub Health 2014; 14: 577.
[21] Bonani P and Bonnacorssi G. Vaccination against hepatitis B in health care workers. Vaccine 2001; 19: 2389–2394.
[22] Kateera F, Walker TD, Mutesa L, et al. 2015; Hepatitis B and C seroprevalence among health care workers in a tertiary hospital in Rwanda. Trans R Soc Trop Med Hyg. 109: 203–208.
[23] Orji CJ, Chime OH, Ndibuagu EO. 2020; Vaccination status and prevalence of hepatitis B virus infection among health-care workers in a tertiary health institution, Enugu State, Nigeria. Proceedings of Singapore Healthcare. 29(2): 119-125. doi:10.1177/2010105820923681.
[24] Elzouki AN, Elgamay SM, Zorgani A, et al. 2014; Hepatitis B and C status among health care workers in the five main hospitals in eastern Libya. Infect Pub Health 7: 534–541.
[25] Rybacki M, Piekarska A, Wiszniewska M, et al. 2013; Hepatitis B and C infection: is it a problem in Polish healthcare workers? Int J Occup Med Environ Health 26: 430–439.
[26] Ciorlia LA, Zanetta DM. 2005 Oct; Hepatitis B in healthcare workers: prevalence, vaccination, and relation to occupational factors. Braz J Infect Dis. 9(5):384-9. doi: 10.1590/s1413-86702005000500005. Epub 2006 Jan 6. PMID: 16410889.
[27] Hussein N.R. 2018; Risk factors of hepatitis B virus infection among blood donors in Duhok city, Kurdistan Region, Iraq. Caspian J Intern Med. 9(1):22-26. doi:10.22088/cjim.9.1.22.
[28] Molla S, Munshea A & Nibret E. 2015; Seroprevalence of hepatitis B surface antigen and anti HCV antibody and its associated risk factors among pregnant women attending maternity ward of Felege Hiwot Referral Hospital, northwest Ethiopia: a cross-sectional study. Virol J. 12: 204. https://doi.org/10.1186/s12985-015-0437-7.
[29] Tiruye G, Shiferaw K, Tadesse F. 2018; Seroprevalence of Hepatitis B Virus Infection and Associated Factors among Pregnant Women Attended Antenatal Care Services in Harar City, Eastern Ethiopia. J Women's Health Care, 7: 436. doi:10.4172/2167-0420.1000436 P.
[30] Olayinka AT, Oyemakinde A, Balogun MS, Ajudua A, Nguku P, Aderinola M, Egwuenu-Oladejo A, Ajisegiri SW, Sha'aibu S, Musa BO, Gidado S, Nasidi A. 2016 Oct 5; Seroprevalence of Hepatitis B Infection in Nigeria: A National Survey. Am J Trop Med Hyg. 95(4):902-907. doi: 10.4269/ajtmh.15-0874. Epub 2016 Aug 15. PMID: 27527630; PMCID: PMC5062798.
[31] Umare A, Seyoum B, Gobena T, Haile Mariyam T. 2016; Hepatitis B Virus Infections and Associated Factors among Pregnant Women Attending Antenatal Care Clinic at Deder Hospital, Eastern Ethiopia. PLoS One. 11(11): e0166936. https://doi.org/10.1371/journal.pone.0166936.
[32] Mahboobi N, Porter SR, Karayiannis P, Alavian SM. 2013 Mar; Dental treatment as a risk factor for hepatitis B and C viral infection. A review of recent literature. J Gastrointestin Liver Dis. 22(1):79-86. PMID: 23539395.
Viewed PDF 1163 86 -
Factors Associated with the Low Facilities Visit: The Real Expectations of Patients in Cameroonian’s ContextAuthor: Georges BonabeDOI: 10.21522/TIJPH.2013.11.01.Art002
Factors Associated with the Low Facilities Visit: The Real Expectations of Patients in Cameroonian’s Context
Abstract:
The health district of Mfou is one of the 29 health districts for the Central region of Cameroon. In 2014, the attendance rate of its facilities was 41%, lower than the 80% norm of the Togolese Ministry of Health in 2013. Questioning the factors associated with this low attendance necessitated the identification of links and associations between it and social demographic factors, health satisfaction, and the perception of facilities by the population. To identify factors associated with low attendance in the Mfou Health District. This is a quanti-qualitative, descriptive cross-sectional study that took place from June 15 to September 22, 2018, in the 32 health facilities in the Mfou Health District. The data collection was based on medical consultation records for 84231 enrolled persons, 372 questionnaires administered to patients in health facilities, and 5 patients who underwent interviews. The data analysis was carried out using CSPro 6.2, Survey CTO Collect v2.41, and SPSS 21 software and the manual operation of the audio content of the interviews. This study shows that the attendance rate of health facilities in the health district of Mfou remains low: 39% in 2015 and 42% in 2017. The factors associated with low attendance at health facilities are the lack of health insurance, the rural environment, the poor quality of reception, the low dynamism of community health workers, the high cost of care and services, the need to have a family relative or an acquaintance working in the Hospital and going to the Hospital only when the illness seems serious with a (P˂ 5%). The low attendance of health facilities in the Mfou health district remains a major public health concern. This is associated with many factors for which the involvement of communities is necessary and their inclusion in the development of health policies.
Keywords: Factors Associated with Low Attendance of Health Facilities, Health Facilities, and Health Districts.
Factors Associated with the Low Facilities Visit: The Real Expectations of Patients in Cameroonian’s Context
References:
[1] Heinmüller R, Dembélé YA, Jouquet G, Haddad S, Ridde V. Soins gratuits avec une ONG ou par l’État au Mali–effets sur la fréquentation des centres de santé par les enfants de 0 à 4 ans. Accès aux soins, Financement de la santé et Performance. 2012 :21.
[2] Africa Progress Panel Policy Brief Maternal Health: Investing in the Lifeline of Healthy Societies & Economies. 2010.
[3] Samuel B. Le cadre stratégique de lutte contre la pauvreté et les trajectoires de la planification au Burkina Faso. Sociétés politiques comparées. 2009 ;16.
[4] Ikelle R. Ville-Management 7. La qualité de gestion et d’attractivité de l’hôpital de District de Bonassama à Douala. 2007.
[5] ECD Ebolowa: Summary of Ebolowa Health District activities for the year 2010. 2010.
[6] ECD Mfou: Executive Team of Mfou Health District Mfou District Health Action Plan For the year 2015. 2015.
[7] Ministry of Health of Togo: Main health indicators. 2013.
[8] Britten N. Qualitative research: qualitative interviews in medical research. BMJ. 1995;311(6999):251-3.
[9] Creswell JW. Research Design Qualitative, Quantitative, and Mixed Methods Approaches Second Edition Sages Publications. Inc; 2003.
[10] Fall I, Seck I, Wone I, Ba-Fall K, Faye A, Ndiaye P, et al. Monitoring et évaluation des programmes de santé en Afrique subsaharienne. Méde Trop. 2005;65(2):184.
[11] Boutin-Mostefa B. et al. Réorganisation de la structure des urgences adultes. Catégoriser et prioriser : 2 mots pour une r(évolution). Dossier CHRU Montpellier. 2008.
[12] Lunjwire K. Le comportement de la population de Goma dans la recherche des soins, Etude des cas de la diarrhée, ville de Goma, ULPGL. 2007: p 64.
[13] USAID: United States Agency for International Development. Changer le comportement des agents de santé communautaires. 2017.
[14] Brundtland G. Combattre la pauvreté en améliorant la santé. Un nouvel axe pour l’OMS. Actualité et dossier en santé publique. 2000; 30:61-4.
[15] Or Z, Com-Ruelle L. La qualité de soins en France : comment la mesurer pour l’améliorer ? J d’écon méd. 2008 ;26(6) :371-85.
[16] Izandengera A. Facteurs déterminant la faible utilisation des services des soins curatifs dans la zone de sante de Karisimbi. Goma/RD Congo ; ISTM/GOMA. 2011
[17] Lavy V, Quigley JM. Willingness to pay for the quality and intensity of medical care. Low-income households in Ghana. 1993.
[18] Dor A, Van Der Gaag J. The demand for medical care in developing countries: quantity rationing in rural Cote d’Ivoire: The World Bank; 1988.
[19] Moliner P, Guimelli C. Les représentations sociales. Fondements historiques et développements récents : Presses universitaires de Grenoble ; 2015.
[20] Charaudeau P. A communicative conception of discourse. Discourse studies. 2002;4(3):301-18.
[21] Moscovici S. On social representations In JP Forgas. Social cognition. 1981:181-209.
[22] Mbainadjina I. Etude socioéconomique sur le coût et accessibilité des populations aux soins de santé au Tchad. 2006.
[23] Magne C. Etude des facteurs entravant la bonne fréquentation des structures sanitaires en milieu rural. Cas du CMA de Kongso Bafoussam III. Ecole des infirmiers diplômés d’état de Bafoussam, Cameroun. 2012.
[24] Sadio A, Diop F. Utilisation et demande de services de santé au Sénégal. Health Financing and Sustainability (HFS) Project, Abt Associates Inc, Bethesda, MD(Draft). 1994.
[25] Graine-auvergne-rhone-alpes.org. [online] Available at: http://graine-auvergne-rhone-alpes.org/DOC/Publications/AccompChangement/01-theorie_comportement_planifie-VF.pdf [Accessed 24 Oct. 2018].
[26] Viau R. L’évaluation source de motivation ou de démotivation ? Québec français. 2002(127) :77-9.
Viewed PDF 968 44 -
 Retained Foreign Body, Still a Reality and Consequence of Non-use of the WHO Surgical Safety Check Lists in Tropical SurgeryAuthor: Leku BADOI: 10.21522/TIJPH.2013.11.01.Art003
Retained Foreign Body, Still a Reality and Consequence of Non-use of the WHO Surgical Safety Check Lists in Tropical SurgeryAuthor: Leku BADOI: 10.21522/TIJPH.2013.11.01.Art003Retained Foreign Body, Still a Reality and Consequence of Non-use of the WHO Surgical Safety Check Lists in Tropical Surgery
Abstract:
Adhesions are a major cause of acute abdomen in previously operated patients. The presence of a retained foreign body in the abdomen is a leading factor in the development of post-operative adhesion. It is, therefore important to take all necessary measures to avoid retained foreign bodies in the abdomen, as this increases the risk of developing post-operative adhesions and complications. A 32yr old female with a relevant past surgical history of an emergency laparotomy indicated for a ruptured ectopic pregnancy presented as an emergency 3 months after the above surgery at a tropical regional hospital with signs of generalized peritonism, following a brief history of sudden onset of lower abdominal pains. A diagnosis of bowel obstruction was made. Resuscitation was done, followed by an emergency exploratory laparotomy. It revealed the presence of a retained foreign body (gauze in our case), surrounded by multiple adhesion around the ileo-cecal junction with 2 meters of ischemic small bowel. Adhesion lysis was done, foreign body was extracted, the ischemic bowel was resected, and an end-to-end anastomosis was performed using Lambert’s technique. The patient had a smooth recovery. Implementing the effective use of the WHO surgical checklists before incision and before closing the abdomen will prevent foreign body retention, hence reducing post-operative complications.
Keywords: Adhesions, Bowel obstruction, Retained foreign body.Retained Foreign Body, Still a Reality and Consequence of Non-use of the WHO Surgical Safety Check Lists in Tropical Surgery
References:
[1] Luijendijk, R. W., de Lange, D. C., Wauters, C. C., Hop, W. C., Duron, J. J., Pailler, J. L., Camprodon, B. R., Holmdahl, L., van Geldorp, H. J., & Jeekel, J. (1996). Foreign material in postoperative adhesions. Annals of surgery, 223(3), 242–248. https://doi.org/10.1097/00000658-199603000-00003.
[2] “WHO surgical safety checklist and implementation manual”. World Health Organization. 2010-12-08. Archived from the original on July 2, 2008. Retrieved 2015-04-23.
[3] Mock, Charles N.; Donkor, Peter; Gawande, Atul; Jamieson, Dean T.; Kruk, Margaret E.; Debas, Haile T. (2015). “1. Essential surgery: key messages of this volume”. In Debas, Haile T.; Peter, Donkor; Gawande, Atul; Jamison, Dean T.; Kruk, Margaret E. (eds.). Disease Control Priorities, Third Edition (Volume 1): Essential Surgery. Vol. 1 (3rd ed.). Washington : World Bank Publications. p. 13. ISBN 978-1-4648-0346-8.
[4] “Decade of improved outcomes for patients thanks to Surgical Safety Checklist”. www.england.nhs.uk. Retrieved 5 February 2021.
[5] “WHO | WHO Surgical Safety Checklist”. WHO. Archived from the original on July 10, 2017. Retrieved 5 February 2021.
[6] Treadwell, Jonathan R; Lucas, Scott; Tsou, Amy Y (April 2014). “Surgical checklists: a systematic review of impacts and implementation”. BMJ Quality & Safety. 23 (4): 299–318. Doi:10.1136/bmjqs-2012-001797. ISSN 2044-5415. PMC 3963558. PMID 23922403.
[7] WHO Guidelines for Safe Surgery 2009. World Health Organization Press. 2009. p. 6. ISBN 978-92-4-159855-2. Archived from the original on November 7, 2017.
[8] Haynes, Alex B.; Weiser, Thomas G.; Berry, William R.; Lipsitz, Stuart R.; Breizat, Abdel-Hadi S.; Dellinger, E. Patchen; Herbosa, Teodoro; Joseph, Sudhir; Kibatala, Pascience L.; Lapitan, Marie Carmela M.; Merry, Alan F. (2009-01-29). “A Surgical Safety Checklist to Reduce Morbidity and Mortality in a Global Population”. New England Journal of Medicine. 360 (5): 491–499. doi:10.1056/NEJMsa0810119. ISSN 0028-4793. PMID 19144931.
[9] GlobalSurg Collaborative (2016). “Mortality of emergency abdominal surgery in high-, middle- and low-income countries”. British Journal of Surgery. 103 (8): 971–988. doi:10.1002/bjs.10151. hdl:20.500.11820/7c4589f5-7845-4405-a384-dfb5653e2163. PMID 27145169. S2CID 20764511.
[10] GlobalSurg Collaborative (2019). “Pooled analysis of WHO Surgical Safety Checklist use and mortality after emergency laparotomy” (PDF). British Journal of Surgery. 106 (2) : 103–112. Doi:10.1002/bjs.11051. PMC 6492154. PMID 30620059.
[11] GlobalSurg Collaborative (2019). “Pooled analysis of WHO Surgical Safety Checklist use and mortality after emergency laparotomy” (PDF). British Journal of Surgery. 106 (2) : 103–112. Doi:10.1002/bjs.11051. PMC 6492154. PMID 30620059.
[12] Ellis, H., Moran, B. J., Thompson, J. N., Parker, M. C., Wilson, M. S., Menzies, D., McGuire, A., Lower, A. M., Hawthorn, R. J., O’Brien, F., Buchan, S., & Crowe, A. M. (1999). Adhesion-related hospital readmissions after abdominal and pelvic surgery: a retrospective cohort study. Lancet (London, England), 353(9163), 1476–1480. https://doi.org/10.1016/S0140-6736(98)09337-4.
[13] Wilson, I., & Walker, I. (2009). The WHO Surgical Safety Checklist: the evidence. Journal of perioperative practice, 19(10), 362–364. https://doi.org/10.1177/175045890901901002.
[14] Gawande, A. A., Studdert, D. M., Orav, E. J., Brennan, T. A., & Zinner, M. J. (2003). Risk factors for retained instruments and sponges after surgery. The New England journal of medicine, 348(3), 229–235. https://doi.org/10.1056/NEJMsa021721.
[15] Rowlands A. (2012). Risk factors associated with incorrect surgical counts. AORN journal, 96(3), 272–284. https://doi.org/10.1016/j.aorn.2012.06.012.
[16] González-Quintero, V. H., & Cruz-Pachano, F. E. (2009). Preventing adhesions in obstetric and gynecologic surgical procedures. Reviews in obstetrics & gynecology, 2(1), 38–45.
[17] Ergul, E., & Korukluoglu, B. (2008). Peritoneal adhesions: facing the enemy. International journal of surgery (London, England), 6(3), 253–260. https://doi.org/10.1016/j.ijsu.2007.05.010.
[18] Ten Broek, R. P., Strik, C., Issa, Y., Bleichrodt, R. P., & van Goor, H. (2013). Adhesiolysis-related morbidity in abdominal surgery. Annals of surgery, 258(1), 98–106. https://doi.org/10.1097/SLA.0b013e31826f4969.
[19] Wan, W., Le, T., Riskin, L., & Macario, A. (2009). Improving safety in the operating room: a systematic literature review of retained surgical sponges. Current opinion in anaesthesiology, 22(2), 207–214. https://doi.org/10.1097/ACO.0b013e328324f82d.
[20] Ulsenheimer K. (2007). Belassene Fremdkörper--aus der Sicht des Juristen [Retained foreign bodies from the point of view of the jurist]. Der Chirurg; Zeitschrift fur alle Gebiete der operativen Medizen, 78(1), 28–34. https://doi.org/10.1007/s00104-006-1280-6.
[21] Fouelifack, F. Y., Fouogue, J. T., Fouedjio, J. H., & Sando, Z. (2013). A case of abdominal textiloma following gynecologic surgery at the Yaounde Central Hospital, Cameroon. The Pan African medical journal, 16, 147. https://doi.org/10.11604/pamj.2013.16.147.3201.
[22] Mefire, A. C., Tchounzou, R., Guifo, M. L., Fokou, M., Pagbe, J. J., Essomba, A., & Malonga, E. E. (2009). Retained sponge after abdominal surgery: experience from a third world country. The Pan African Medical Journal, 2, 10.
[23] Greenberg, C. C., Regenbogen, S. E., Lipsitz, S. R., Diaz-Flores, R., & Gawande, A. A. (2008). The frequency and significance of discrepancies in the surgical count. Annals of surgery, 248(2), 337–341. https://doi.org/10.1097/SLA.0b013e318181c9a3.
[24] Serghini, I., El Fikri, A., Salim Lalaoui, J., Zoubir, M., Boui, M., & Boughanem, M. (2011). Textilome abdominal : à propos d’un cas. The Pan African Medical Journal, 9.
[25] Târcoveanu, E., Dimofte, G., Georgescu, S., Vasilescu, A., Lupaşcu, C., Bradea, C., & Van Hee, R. (2011). Laparoscopic retrieval of gossypibomas--short series and review of literature. Acta chirurgica Belgica, 111(6), 366–369. https://doi.org/10.1080/00015458.2011.11680774.
[26] Smith DA, Kashyap S, Nehring SM. Bowel Obstruction. [Updated 2022 Jun 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441975/.
[27] Kopka, L., Fischer, U., Gross, A. J., Funke, M., Oestmann, J. W., & Grabbe, E. (1996). CT of retained surgical sponges (textilomas): pitfalls in detection and evaluation. Journal of computer assisted tomography, 20(6), 919–923. https://doi.org/10.1097/00004728-199611000-00009.
[28] Lauwers, P. R., & Van Hee, R. H. (2000). Intraperitoneal gossypibomas: the need to count sponges. World journal of surgery, 24(5), 521–527. https://doi.org/10.1007/s002689910084.
[29] van Steensel, S., van den Hil, L., Schreinemacher, M., Ten Broek, R., van Goor, H., & Bouvy, N. D. (2018). Adhesion awareness in 2016: An update of the national survey of surgeons. PloS one, 13(8), e0202418. https://doi.org/10.1371/journal.pone.0202418.
[30] Ten Broek, R. P., Strik, C., Issa, Y., Bleichrodt, R. P., & van Goor, H. (2013). Adhesiolysis-related morbidity in abdominal surgery. Annals of surgery, 258(1), 98–106. https://doi.org/10.1097/SLA.0b013e31826f4969.
Viewed PDF 1067 23 -
 The Use of Herbal Health Products and Home-Based Remedies for Protection Against Covid-19Author: Olalekan FagbolaDOI: 10.21522/TIJPH.2013.11.01.Art004
The Use of Herbal Health Products and Home-Based Remedies for Protection Against Covid-19Author: Olalekan FagbolaDOI: 10.21522/TIJPH.2013.11.01.Art004The Use of Herbal Health Products and Home-Based Remedies for Protection Against Covid-19
Abstract:
Natural medicinal products and home-based remedies have been in use for centuries by people across the world. Tradition, belief, cultural practice, and previous experience are associated with the use of herbal products. The trend is observed to be on the increase since covid-19 Pandemic hit the global stage. In the early days of the Pandemic, people protected themselves by practicing measures that would safeguard them from getting infected with the deadly virus. This study evaluated prevalence, risks, harms, benefits, and other issues associated with using herbs and home-based remedies to prevent and treat Covid-19. It highlights various measures of prevention and treatment practiced by employees and customers of a Regional Corporation by capturing the demographic characteristics, reasons, and associated factors for using alternative medical products. A descriptive cross-sectional survey in a hybrid online was carried out from February 2022 to April 2022. Data of independent and dependent variables was collected using a well-structured hybrid (online and paper and pencil) questionnaire. Prevalence of steam inhalation was 51%, essential oils, including menthol crystal vapour inhalation, was 61%, herbal supplements was 20.6%, and natural health products was 100% (n = 286). Non-allopathic medicinal products, home-based remedies, and other preventive health measures were on the increase in prevalence during covid-19 Pandemic. Large studies are required to assess the efficacy and safety of herbal supplements and home-based remedies to protect users from unnecessary dangers inherent in their use.
Keywords: Covid-19 pandemic, Herbal health supplements, Home-based remedies, Infection, Prevalence, Natural products, Regional corporation.The Use of Herbal Health Products and Home-Based Remedies for Protection Against Covid-19
References:
[1] Boozariet, M., and Hosseinzadeh, H. (2020). Natural products for Covid-19 prevention and treatment regarding to previous coronavirus infections and novel studies. Phytotherapy research: PTR. 35. 10.1002/ptr.6873. https://onlinelibrary.wiley.com/doi/10.1002/ptr.6873.
[2] Singla R, K., Xuefei, H., Hitesh, C., Christos, T., Shen L., Amjad, K, K., Bairong, S. (2021). Natural Products for the Prevention and Control of the Covid-19 Pandemic: Sustainable Bioresources: Journal=Frontiers in Pharmacology, Volume=12, Year=2021. ISSN=1663-9812. DOI=10.3389/fphar.2021.758159 https://www.frontiersin.org/articles/10.3389/fphar.2021.758159.
[3] Shahrajabian, M, H., Sun, W., and Cheng, Q. (2019) Clinical aspects and health benefits of ginger (Zingiberofficinale) in both trad-itional Chinese medicine and modern industry, Acta Agriculturae Scandinavica, Section B — Soil & Plant Science, 69:6, 546-556, DOI: 10.1080/09064710.2019.1606930 https://doi.org/10.1080/09064710.2019.1606930.
[4] Jafarzadeh, S., Abdorreza, N., Ali, S., Oladzadabbasabadi, N., & Jafari, S. (2021). Application of bio-nanocomposite films and edible coatings for extending the shelf life of fresh fruits and vegetables. Advances in Colloid and Interface Science. 10.1016/j.cis.2021.102405.
[5] Rusmini, R., Ningsih, MU., Emilyani, D. (2022). Ten Percent Red Ginger Gel Relieves Knee Joint Pain in the Elderly with Osteoarthritis. Open Access Maced J Med Sci. 2022 Apr 14; 10(B):1164-1169. https://doi.org/10.3889/oamjms.2022.889.
[6] Ozkur, M., Benlier, N., Takan, I., Vasileiou, C., Georgakilas, A. G., Pavlopoulou, A., Cetin, Z., & Saygili, E. I. (2022). Ginger for Healthy Ageing: A Systematic Review on Current Evidence of Its Antioxidant, Anti-Inflammatory, and Anticancer Properties. Oxidative medicine and cellular longevity, 2022, 4748447. https://doi.org/10.1155/2022/4748447.
[7] Unuofin, J, O., Masuku Nelisiwe Prenate, M, N., Paimo, O. K., Lebelo, S. L. Ginger from Farmyard to Town: Nutritional and Pharmacological Applications JOURNAL, Frontiers in Pharmacology. VOLUME 12, 2021, ISSN1663-9812 DOI: 10.3389/fphar.2021.779352 https://www.frontiersin.org/articles/10.3389/fphar.2021.779352.
[8] Vasconcellos, J., Conte-Junior, C., Silva, D. et al. Comparison of total antioxidant potential, and total phenolic, nitrate, sugar, and organic acid contents in beetroot juice, chips, powder, and cooked beetroot. Food SciBiotechnol 25, 79–84 (2016). https://doi.org/10.1007/s10068-016-0011-0.
[12] Richard S. Rivlin (2021). Historical Perspective on the Use of Garlic, The Journal of Nutrition, Volume 131, Issue 3, March 2001, Pages 951S–954S, https://doi.org/10.1093/jn/131.3.951S.
[13] Francisco, V., Figueirinha, A., Neves, B. M., García-Rodríguez, C., Lopes, M. C., Cruz, M. T., & Batista, M. T. (2011). Cymbopogoncitratus as source of new and safe anti-inflammatory drugs: bio-guided assay using lipopolysaccharide-stimulated macrophages. Journal of ethnopharmacology, 133(2), 818–827. https://doi.org/10.1016/j.jep.2010.11.018.
[14] Boukhatem, M. N., Ferhat, M. A., Kameli, A., Saidi, F., & Kebir, H. T. (2014). Lemon grass (Cymbopogoncitratus) essential oil as a potent anti-inflammatory and antifungal drugs. The Libyan journal of medicine, 9, 25431. https://doi.org/10.3402/ljm.v9.25431.
[15] Bankole, S. A. and Joda, A. (2004). African Journal of Biotechnology Vol. 3 (1), pp. 52-59, January 2004 Available online at http://www.academicjournals.org/AJB ISSN 1684–5315 © 2004 Academic Journals. https://tspace.library.utoronto.ca/bitstream/1807/3492/1/jb04008.pdf.
[16] Ross S. M. (2016). Echinacea purpurea: A Proprietary Extract of Echinacea purpurea Is Shown to be Safe and Effective in the Prevention of the Common Cold. Holistic nursing practice, 30(1), 54–57. https://doi.org/10.1097/HNP.0000000000000130.
[17] Karsch-Völk, M., Barrett, B., Kiefer, D., Bauer, R., Ardjomand-Woelkart, K., & Linde, K. (2014). Echinacea for preventing and treating the common cold. The Cochrane database of systematic reviews, 2(2), CD000530. https://doi.org/10.1002/14651858.CD000530.pub3.
[18] Hewlings, S. J., & Kalman, D. S. (2017). Curcumin: A Review of Its Effects on Human Health. Foods (Basel, Switzerland), 6(10), 92. https://doi.org/10.3390/foods6100092.
[19] Ramadasan Kuttan, P., Bhanumathy, K., and Nirmala, M.C. George (1985). Potential anticancer activity of turmeric (Curcuma longa), Cancer Letters, Volume 29, Issue 2,1985, Pages 197-202, ISSN 0304-3835, https://doi.org/10.1016/0304-3835(85)90159-4.
[20] Sanati, S., Razavi, B. M., & Hosseinzadeh, H. (2018). A review of the effects of Capsicum annuum L. and its constituent, capsaicin, in metabolic syndrome. Iranian journal of basic medical sciences, 21(5), 439–448. https://doi.org/10.22038/IJBMS.2018.25200.6238.
[21] Cichewicz, R. H., & Thorpe, P. A. (1996). The antimicrobial properties of chile peppers (Capsicum species) and their uses in Mayan medicine. Journal of ethnopharmacology, 52(2), 61–70. https://doi.org/10.1016/0378-8741(96)01384-0.
[23] Kumar, A., Baitha, U., Aggarwal, P., &Jamshed, N. (2016). A fatal case of menthol poisoning. International journal of applied & basic medical research, 6(2), 137–139. https://doi.org/10.4103/2229-516X.179015.
[24] Pereira, E. J., Sim, L., Driver, H., Parker, C., & Fitzpatrick, M. (2013). The effect of inhaled menthol on upper airway resistance in humans: a randomized controlled crossover study. Canadian respiratory journal, 20(1), e1–e4. https://doi.org/10.1155/2013/383019.
[25] Ogunsalu, C., Barton, E, Fagbola, O., Johnson L, Ajike, S., Johnson, L., Ogunsalu, D., and Judy, K. (2022. Menthol Crystal Vapor Inhalation in the Prevention and Remission of Early Diagnosed Covid-19 Patients: Evidence-Based. J Dent Oral Sci. 2022;4(1):1-17. DOI: https://doi.org/10.37191/Mapsci-2582-3736-4(1)-112.
[26] Gibbs J. E. (2019). Essential oils, asthma, thunderstorms, and plant gases: a prospective study of respiratory response to ambient biogenic volatile organic compounds (BVOCs). Journal of asthma and allergy, 12, 169–182. https://doi.org/10.2147/JAA.S193211.
[27] Burfield, (200). Safety of essential oils, International Journal of Aromatherapy,Volume 10, Issues 1–2, 2000, Pages 16-29, ISSN 0962-4562, https://doi.org/10.1016/S0962-4562(00)80005-3.
[28] Chowdhury, M., Alif, Y. A., Alam, S., Emon, N. U., Richi, F. T., Zihad, S., Taki, M., & Rashid, M. A. (2022). Theoretical effectiveness of steam inhalation against SARS-CoV-2 infection: updates on clinical trials, mechanism of actions, and traditional approaches. Heliyon, 8(1), e08816. https://doi.org/10.1016/j.heliyon.2022.e08816.
[29] La Marca, et al (2020. Thermal inactivation of SARS Covid-2 virus: Are steam inhalations a potential treatment? Life Sciences. 265. 118801. 10.1016/j.lfs.2020.118801. https://www.researchgate.net/publication/347093201_Thermal_inactivation_of_SARS_Covid-2_virus_Are_steam_inhalations_a_potential_treatment.
[30] Bello, I, B., Akinnawo, E, O., Akpunne, B, O., Mopa-Egbunu, A. (2022). Knowledge of Covid-19 and preventive measures on self-medication practices among Nigerian undergraduates, Cogent Arts & Humanities, 9:1, 2049480, DOI: 10.1080/23311983.2022.2049480. https://doi.org/10.1080/23311983.2022.2049480.
[31] Nuertey, B, D., Addai, J., Kyei-Bafour, P., Bimpong Km A., Adongo, V., Boateng, L., Mumuni, K., Dam, K, M., Udofia, , ., Seneadza N, H., Calys-Tagoe, B, L., Tette, A., Yawson, E., Soghoian, S., Helegbe, H., Vedanthan R. (2022). Home-Based Remedies to Prevent Covid-19-Associated Risk of Infection, Admission, Severe Disease, and Death: A Nested Case-Control Study. Evidence-Based complementary and Alternative Medicine, vol. 2022, Article ID 4559897, 9 pages, 2022. https://doi.org/10.1155/2022/4559897.
[32] Vimalanathan, S. (2014). Anti-influenza virus activity of essential oils and vapors. American Journal of Essential Oils and Natural Products. 2. 47-53. (PDF) Anti-influenza virus activity of essential oils and vapors (researchgate.net).
[33] Chaachouay, N., Douira, A., & Zidane, L. (2021). Covid-19, prevention, and treatment with herbal medicine in the herbal markets of Salé Prefecture, North-Western Morocco. European journal of integrative medicine, 42, 101285. https://doi.org/10.1016/j.eujim.2021.101285.
[35] Villena-Tejada M, Vera-Ferchau I, Cardona-Rivero A, Zamalloa-Cornejo R, Quispe-Florez M, Frisancho-Triveño Z (2021) Use of medicinal plants for Covid-19 prevention and respiratory symptom
htreatment during the Pandemic in Cusco, Peru: A cross-sectional survey. PLoS ONE 16(9): e0257165. https://doi.org/10.1371/journal.pone.0257165.[36] Yimenu, D. K., Jejaw, A., Haylu, E., Kassahun, S., & Kifle, Z. D. (2022). Knowledge, Attitude, and Practice Towards Facemask Use Amid the Coronavirus 2019 Pandemic Among Public Transport Drivers in Gondar Town, A Cross-Sectional Study. INQUIRY: The Journal of Health Care Organization, Provision, and Financing. https://doi.org/10.1177/00469580221096285.
[37] Wubet, G, M., Zimamu, L, Y. (2022). Knowledge, attitude, and practice towards facemask use amid the Covid-19 Pandemic among public transport drivers in Debre-Tabor town, Ethiopia. J Community Med Health Solut. 2022; 3: 001-010. DOI: 10.29328/journal.jcmhs.1001013.
[38] Habersaat, K.B., Betsch, C., and Danchin, M. (2020). Ten considerations for effectively managing the Covid-19 transition. Nat Hum Behav, 4, 677-687. https://doi.org/10.1038/s41562-020-0906-x.
[39] Chiu, N. C., Chi, H., Tai, Y. L., Peng, C. C., Tseng, C. Y., Chen, C. C., Tan, B. F., & Lin, C. Y. (2020). Impact of Wearing Masks, Hand Hygiene, and Social Distancing on Influenza, Enterovirus, and All-Cause Pneumonia During the Coronavirus Pandemic: Retrospective National Epidemiological Surveillance Study. Journal of medical Internet research, 22(8), e21257. https://doi.org/10.2196/21257.
[40] Al-Wutayd, O., Mansour, A, E., and Aldosary, A.H. (2021. Handwashing knowledge, attitudes, and practices during the Covid-19 Pandemic in Saudi Arabia: A non-representative cross-sectional study. Sci Rep 11, 16769 (2021).https://doi.org/10.1038/s41598-021-96393-6.
Viewed PDF 1322 36 -
 Development of a South-South Clinical Research Capacity Strengthening: Institutional Partnership Platform between Cameroon and South AfricaAuthor: Yayah Emerencia NgahDOI: 10.21522/TIJPH.2013.11.01.Art005
Development of a South-South Clinical Research Capacity Strengthening: Institutional Partnership Platform between Cameroon and South AfricaAuthor: Yayah Emerencia NgahDOI: 10.21522/TIJPH.2013.11.01.Art005Development of a South-South Clinical Research Capacity Strengthening: Institutional Partnership Platform between Cameroon and South Africa
Abstract:
Collaborative partnerships are key components to reinforce biomedical and clinical research capacity and are characterized by enormous challenges though important in promoting the institutional exchange of ideas and capacities that potentially fill knowledge and research gaps. An observational analysis was conducted from 2014 to 2022 between the Faculty of Medicine and Health Sciences, Stellenbosch University, South Africa, and the Centre for the Study of Communicable Diseases (CSCCD), Faculty of Medicine and Biomedical Science, University of Yaoundé I, Cameroon. Despite constraints, affiliations with institutes from developed economies are often established within the framework of North-South collaborations. Since 2014, a strong bilateral South-South research partnership between the two institutions has been developed and consolidated for sustainable coexistence. In this paper, we report on qualitative research within our leading collaborative scientists involved in major institutional research, our views on South-South collaboration, and the factors that consolidate our decision-making about joining and participating actively in research networks.
Keywords South-South collaboration, Stellenbosch University, South Africa, University of Yaoundé 1, Cameroon.Development of a South-South Clinical Research Capacity Strengthening: Institutional Partnership Platform between Cameroon and South Africa
References:
[1] Chendi BH, Okomo Assoumou MC, Jacobs GB, Yekwa EL, Lyonga E, Mesembe M, Eyoh A, Ikomey GM. Rate of viral load change and adherence of HIV adult patients treated with Efavirenz or Nevirapine antiretroviral regimens at 24 and 48 weeks in Yaoundé, Cameroon: a longitudinal cohort study. BMC Infect Dis. 2019 Feb 26; 19 (1):194. doi: 10.1186/s12879-019-3824-7.
[2] Donne J. Devotions Upon Emergent Occasions and Seuerall Steps in my Sicknes - Meditation XVII, 1624.
[3] ilbert D, Ikomey GM, Njenda D, Gichana J, Katusiime MG, Ndze VN, Zeier M, Mesember M, Fokunang C, Assoumou MCO, Tebeu P, Atangana PA and Jacobs GB. Oncogenic Human Papillomavirus genotypes 16 and 18 prevalence among women with normal cervical cytology and neoplasia in Cameroon: A Systematic Review. The journal of medicine and health sciences Health Sciences and Diseases. 18;3. 2017. www.hsd-fmsb.org.
[4] uiedem E, Ikomey GM, Nkenfou C, Walter PE, Mesembe M, Chegou NN, Jacobs GB, Okomo Assoumou MC. Chronic obstructive pulmonary disease (COPD): neutrophils, macrophages and lymphocytes in patients with anterior tuberculosis compared to tobacco related COPD. BMC Res Notes. 2018 Mar 27;11 (1):192. doi: 10.1186/s13104-018-3309-6.
[5] acobs GB and Ikomey GM. Biomedical research and capacity building: Bilateral collaboration between research institutes in South Africa and Cameroon. SAMJ. 2016. 106; 10.
[6] Ikomey GM, Assoumou MCO, Gichana JO, Njenda D, Mikasi SG, Mesembe M, Lyonga E and Jacobs GB. Observed HIV drug resistance associated mutations amongst naïve immunocompetent children in Yaoundé, Cameroon. Germs. 2017 Dec 5;7(4):178-185. doi: 10.18683/germs.2017.1124.
[7] Joel G. Sprunger. The Benefits of Engaging in Collaborative Research Relationships: November 30, 2017.
[8] Munung NS, Mayosi BM and de Vries J. Equity in international health research collaborations in Africa: Perceptions and expectations of African researchers. PLoS One. 2017 Oct 16; 12(10): e0186237. doi: 10.1371/journal.pone.0186237.
[9] National Academies of Sciences, Engineering, and Medicine. 2018. Data Matters: Ethics, Data, and International Research Collaboration in a Changing World: Proceedings of a Workshop. Washington, DC: The National Academies Press. doi: http://doi.org/10.17226/25214.
[10] Nachega JB, Uthman OA, Ho YS, et al. Current status and future prospects of epidemiology and public health training and research in the WHO African region. Int J Epidemiol 2012 ;41(6):1829-1846. DOI :10.1093/ije/dys189.
[11] Uthman OA, Wiysonge CS, Ota MO, et al. Increasing the value of health research in the WHO African Region beyond 2015 – reflecting on the past, celebrating the present and building the future: A bibliometric analysis. BMJ Open 2015;5(3): e006340. DOI:10.1136/bmjopen-2014-006340.
[12] World Health Organisation (WHO) global health report, 2018. https://www.who.int/gho/publications/world_health_statistics/en/ - Date accessed 03 August 2019.
[13] Agar J. Science in the 20th Century and Beyond. Cambridge: Polity Press; 2012.
[14] Sonnenwald D. H. Scientific collaboration. Annual review of information science and technology. 2007; 41(1): 643–681.
[15] Ad Hoc Committee on Health Research Relating to Future Intervention Options. Investing in Health Research and Development. Geneva: World Health Organisation; 1996.
[16] Council on Health Research for Development (COHRED). International Conference on Health Research for Development, Bangkok, 2001. Available: www.conference2000.ch.
[17] Bull S, Cheah P, Denny S, Jao I, Marsh V, Merson L, et al. Ethics and best practices for sharing individual-level health research data from low- and middle-income settings. Journal of Empirical Research on Human Research Ethics. 2015; 10(3): 302–313. pmid:26297751.
[18] Carpenter-Song E, Whitley R. Behind the Scenes of a Research and Training Collaboration: Power, Privilege, and the Hidden Transcript of Race. Culture, Medicine, and Psychiatry. 2013; 37(2): 288–306. pmid:23580139.
[19] Crane J. Scrambling for Africa? Universities and global health. The Lancet. 2011; 377(9775): 1388–1390. pmid:21074254.
[20] Crane JT. Scrambling for Africa: AIDS, expertise, and the rise of American Global Health Science. Ithaca: Cornell University Press; 2013.
[21] Gerrets RP. Globalizing international health: The cultural politics of ‘partnership’ in Tanzanian malaria control. New York: New York University Press; 2010.
[22] Macdonald H, Spiegel AD. ‘Distraction from the real difficulties’: ethical deliberations in international health research. Anthropology Southern Africa. 2013; 36. Issue 3/4:146–154.
[23] Benjamin R. ‘A Lab of Their Own’: Genomic sovereignty as postcolonial science policy. Policy and Society. 2009; 28(4): 341–355.
[24] Dunbar K. How scientists rseally reason: Scientific reasoning in real-world laboratories. In Sternberg RJ, Davidson J, editors. Mechanisms of Insight. Cambridge, MA: MIT Press. 1995. pp. 365–395.
[25] Christian S, Mosavel M, van Stade D. Ethical challenges in the design and conduct of locally relevant international health research. Social Science & Medicine. 2007; 64 (9): 1960–1969. pmid:17321657.
[26] Council on Health Research for Development (COHRED). Where there is no lawyer: guidance for fairer contract negotiation in collaborative research partnerships; 2013. Available: http://www.cohred.org/wp-content/uploads/2012/04/Fair-Research-Contracting-Guidance-Booklet-e-version.pdf doi: https://doi.org/10.1242/dev.085035 23362346.
[27] World Conferences on Research Integrity. Montreal Statement on Research Integrity in Cross-Boundary Research Collaborations’; 2013. Available: http://www.researchintegrity.org/Statements/Montreal%20Statement%20English.pdf.
[28] Council on Health Research for Development (COHRED). The COHRED Fairness Index for international collaborative partnerships; 2015. Available: http://cfi.cohred.org/cohred-fairness-index/.
[29] Parker M. Ethical problems and genetics practice. Cambridge: Cambridge University Press; 2012. https://doi.org/10.1017/CBO9781139107792.
[30] Kingori P. Experiencing everyday ethics in context: Frontline data collectors’ perspectives and practices of bioethics. Social Science and Medicine. 2013: 98: 361–370. pmid:24210881.
[31] Parker MKP. Good and Bad Research Collaborations: Researchers’ Views on Science and Ethics in Global Health Research. PLoS ONE; 2016; 11 (10): e0163579. https://doi.org/10.1371/journal.pone.0163579.
Viewed PDF 1370 54 -
 Knowledge and Practices of Female Traditional Healthcare Givers to Mothers on Referral System for Care and Immunization against Childhood Killer Diseases in Hard-to-Reach Areas of Adamawa State - NigeriaAuthor: Takwi, RelesterDOI: 10.21522/TIJPH.2013.11.01.Art006
Knowledge and Practices of Female Traditional Healthcare Givers to Mothers on Referral System for Care and Immunization against Childhood Killer Diseases in Hard-to-Reach Areas of Adamawa State - NigeriaAuthor: Takwi, RelesterDOI: 10.21522/TIJPH.2013.11.01.Art006Knowledge and Practices of Female Traditional Healthcare Givers to Mothers on Referral System for Care and Immunization against Childhood Killer Diseases in Hard-to-Reach Areas of Adamawa State - Nigeria
Abstract:
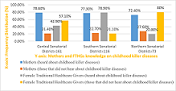
Female Traditional Healthcare Givers’ (FTHGs) knowledge, attitude, and practice on maternal and infant survival from pregnancy, delivery, and after birth has been a contextual matter throughout the globe, especially where the incidence of infant mortality rate is high. This often poses questions as to why, what happened, and where women of childbearing go for health seeking when pregnant, at birth, and after delivery? The impact of FTHGs activities to mothers and infants on their education and referral of mothers and children for treatment and immunization was studied in the three Senatorial Districts of Adamawa State. Self-structured questionnaires with both open and closed-ended responses and oral interviews were used for the purpose of the study and analyzed electronically on SPSS version 25.0. Approaches to improve the knowledge and practice of Female Traditional Healthcare Givers include seminars and workshops by Non-Governmental Organizations’, Antenatal Care at government health facilities, and health professionals’ effort in-home visits and formal education. These have improved FTHGs knowledge, skills, and acceptance of immunization programme against childhood killer diseases in most of the Senatorial District communities. Maternal and infant morbidity and mortality has experienced a great reduction in the process as FTHGs made referrals to health facilities on cases needing treatment and immunization. This underlies the need for training in epidemiological findings to prevent the incidence of infant morbidity and mortality since education is the key to a healthy live.
Keywords: Childhood killer diseases, Epidemiological, Female Traditional Health care Givers, Healthcare, Immunization, Infant morbidity, Mortality, and Referral.Knowledge and Practices of Female Traditional Healthcare Givers to Mothers on Referral System for Care and Immunization against Childhood Killer Diseases in Hard-to-Reach Areas of Adamawa State - Nigeria
References:
[1] Preedy, V.R. and Watson, R.R. (2010). The Impact of Infectious Diseases on the Development of Africa. Handbook of Disease Burdens and Quality of Life Measures. 2010 : 1171–1188. doi: 10.1007/978-0-387-78665-0_66.
[2] Mojoyinola, J.K., and Olaleye, B. A. (2012). Physical and Psychological Factors Influencing Maternal Non-Compliance with Immunization Schedule. Available at http://www.Continental Journal of Nursing Science. 4(2): 37-51.
[3] Masten A.S., Cicchetti, D. (2010). Developmental Cascades: Developmental Psychopathology (psychopathol) Development and Psychopathology; 22(3) 491 – 495.
[4] Breiner, S. (2016). Parenting Knowledge, Attitudes and Practices. Parenting Matters: Supporting Parents of Children ages 0-8. Hard copy Version at National Academic Press. Available at https://www.ncbi.nlm.nih.govlbookslNBK402020 Retrieved on 7th September 2020.
[5] Jones T.L, Prinz R.J. (2015). Potential roles of Parental self – efficacy in parents and child adjustment. A review. Clinical Psychology Review, 25(3): 341 – 363.
[6] Ajzen, J and Fishbien, k.M. (1980). Understanding Attitudes and predicting social behaviour. Englewood cliffs; N.J: Prentice – Hall. Available at https:// researchgate.net/publication/276847036 Retrieved on 5th June 2020.
[7] Fishbein, M., Triands, H.C., Kanfer, F.H., Becker, M., Stadt, M.E. (2001). Factors influencing behaviours and behaviour change. Evaluation and the Health Professions. Using Intervention Theory to Factors Influencing Behaviour Change. Project Respect. Sage Journals, 24(4) 36 – 384.
[8] Struthers, R., Eschiti, V. and Patchell, B. (2004). Traditiona04indigenous healing: Part I. Complementary Therapies in Nursing and Midwifery, 10(3):1419. DOI: 10.1016/j.ctnm.2004.05.001.
[9] Ekor, M. (2013). The growing use of herbal medicines: issues relating to adverse reactions and challenges in monitoring safety. Frontiers in Pharmacology. 4:177.
[10] Adatara, P., Strumpher, J. and Ricks, E. (2020). Exploring the reasons why women prefer to give birth at home in rural northern Ghana: a qualitative study. BMC Pregnancy Childbirth. 20:500. doi: 10.1186/s12884-020-03198-y.
[11] Imoh, G. (2013). Communication for Social Mobilization. An Evaluative Study of the Immunization Campaign in Nigeria. Journal of Humanities and Social Sciences Available at http://(IOSR-JHSS), 13(6): 78-88 Retrieved on 7th April 2022.
[12] Shehu, D., Norizon, A. G. and Bozkurt, V. (2015). A System review on Factors Affecting Community Participation towards Polio Immunization in Nigeria, Mediterranean Journal of Social Sciences. 6(2): -408-415 Retrieved on 30th March 2022.
[13] Birhanu, S., Anteneh, A., Kibie, Y., andJejaw,A. (2016) Knowledge, Attitude and Practice of Mothers towards Immunization of Infants in Health Centres at Addis Ababa Ethiopia. American Journal of Health Research 4(1):6 Available at Doi: 10.11648/j.ajhr.20160401.12.
[14] World Bank (2020). Poverty Overview. Available at https://www.worldbank.org Retrieved on 9th June 2020.
[15] UN (2009). Achieving global public health agenda. United Nations Publications. Available at: https://www.un.org/en/ecosoc/docs/pdfs/achieving_global_public_ health_agenda.pdf Accessed on September 23rd, 2022.
[16] Omotara, B.A., Okujagu, T.F., Gbodossou, E. (2012). Assessment of Knowledge, Attitude and Practice of Stakeholders towards Immunization in Borno State Nigeria. A Qualitative Approach Journal of Community Medicine and Health Education.2:181. Available at http://Doi:10.4172/2161- 0711.1000181 Retrieved on 29th March 2022.
[17] Lemeshow, S., Hosmer, D.W., Klar, J. (2003) and WHO, (2005). Determination of Sample Size. Malaysian Journal of Medical Sciences. Formula Calculating Population Sample Size. Available at https://apps.who.int/iris/bitstream/handl/10665/41607/ Retrieved n 13th July 2020.
[18] Al-Ayed, I.H. (2010). Mothers’ knowledge of child health matters: Are we doing enough?
[19] Journal of Family and Community Medecine.17(1): 22–28. doi: 10.4103/13191683.68785.
[20] Bello, K and Daniel, A. D. (2017) Knowledge and Attitude of Mothers towards childhood Immunization in Bauchi Local Government, Bauchi State – Nigeria. Available at http://www.semanticscholar.org/paper/knowledgeandattitude-ofmothers-towards-childhood-Bello_Daniel/9eddfc7e5831856952661068dbcfOcOc5097fe#citing-par Retrieved on 6th April 2020.
[21] Oku A., Oyo-Ita, A., Glenton, C., Leoin, S. (2017). Perceptions and experiences of Childhood vaccination communication strategies. Journal Public health. 3:222-224.
[22] Akingbulu, O. (2019) United Nation Women, in Partinership with P&G and Afrigrants Trained 250 Women…by UNICEF Communication Officer. Available at Nigeria.un.org Retrieved on 3rd April 2020.
[23] Adatara, P.’ Afaya, A.; Baku, E. A.; Salia, S. M. and Asempah A. (2018) Perspective of Traditional Birth Attendants on their Experiences and Roles in Maternal Healthcare in Rural Areas of Northern Ghana. International Journal of Reproductive Medicine, 3(1):22-32.
[24] Hernandez, S.; Oliveira, J.B. and Shirazin, T. (2017) How a Training Program is Transforming the Role of Traditional Birth Attendants from cultural
Practitioners to Unique Health-care-Providers. A Community Case Study in Rural Guatemala Available at https://doi.org/10.3389/fpubh.2017.oo111 Retrieved on 7th April 2022.[25] Sarmento D.R. (2014). Traditional Birth Attendance in A Health System: What are Roles, Benefits and Challenges: A Case Study of incorporated TBA in Timor-Leste Available at apfmj.biomedcentral.com>articles Retrieved on 30th March 2022.
[26] World Bank, (2020). Poverty Overview. Available at https://www.worldbank.org Available on 9th June 2020.
[27] Herval, A.M.; Gomes, V.E.; Oliveira, D.P.D.; Vargas, A.M.D. (2019) Health Education Strategies Targeting Maternal and Child Health. https://www.ncbi.nim.nih.gov/pmc/articles/PMC6616517/ Retrieved on 7th April 2022.
Viewed PDF 935 33 -
 Prevalence of Tuberculosis among Presumptive Tuberculosis Patients Offered HIV Testing Services in Federal Capital Territory, Abuja NigeriaAuthor: Tangkat Friday HosleDOI: 10.21522/TIJPH.2013.11.01.Art007
Prevalence of Tuberculosis among Presumptive Tuberculosis Patients Offered HIV Testing Services in Federal Capital Territory, Abuja NigeriaAuthor: Tangkat Friday HosleDOI: 10.21522/TIJPH.2013.11.01.Art007Prevalence of Tuberculosis among Presumptive Tuberculosis Patients Offered HIV Testing Services in Federal Capital Territory, Abuja Nigeria
Abstract:
Tuberculosis is a communicable disease caused by Mycobacterium tuberculosis, considered a major risk to global health security. This study determined the prevalence, treatment outcomes, and factors associated with tuberculosis among 737 presumptive tuberculosis patients in Federal Capital Territory Abuja, Nigeria from 1st April 2019 to 30th May 2021 through retrospective cross-sectional study and multi-stage sampling. From Non-Municipal Area Councils, Bwari was selected while from Health Facilities, General Hospital Bwari and Gwarimpa were selected from Bwari and Abuja Municipal Area Council respectively by simple random sampling and data abstractions were done and analyzed using Statistical Package for Social Sciences version 23.0 Software. The prevalence of tuberculosis amongst the patients was 19.4%. The tuberculosis treatment outcome showed that 66.4% were cured, 14.7% completed treatment, 7.0% failed treatment, 5.6% lost to follow-up and 0.7% removed from the Register. The prevalence of tuberculosis in the Bwari Area Council was 8.2%. The association between Area Council of Resident and tuberculosis was significant (p = 0.001). Patients that reside in Bwari Area Council were 0.078 times less likely to have tuberculosis compared to those who reside in Abuja Municipal Area Council and, Area Council of Residence was a predictor of tuberculosis (aOR = 0.001; 95% C.I. = 0.043 - 0.141). The prevalence of tuberculosis amongst patients with Human Immunodeficiency Virus was 29.6%. The association was significant (p = 0.001) but not a predictor of tuberculosis (aOR = 0.840; 95% C.I. = 0.617 - 1.810).
Keywords: Human Immunodeficiency Virus, Presumptive, Tuberculosis.Prevalence of Tuberculosis among Presumptive Tuberculosis Patients Offered HIV Testing Services in Federal Capital Territory, Abuja Nigeria
References:
[1] Tiewsoh, J. A., Antony, B., & Boloor, R. (2020). HIV-TB co-infection with clinical presentation, diagnosis, treatment, outcome, and its relation to CD4 count, a cross-sectional study in a tertiary care hospital in coastal Karnataka. Journal of Family Medicine and Primary Care, 9(2), 1160. https://doi.org/10.4103/jfmpc.jfmpc_950_19.
[2] KNCV Tuberculosis Foundation. (n.d.). What is tuberculosis? - KNCV - Tuberculosefonds. Retrieved March 30, 2021, from https://www.kncvtbc.org/en/about-tb/.
[3] World Health Organization. (2020). Global tuberculosis report 2020: executive summary. https://apps.who.int/iris/bitstream/handle/10665/337538/9789240016095-eng.pdf.
[4] ALNAP. (2020). Global Tuberculosis Report 2020 | ALNAP. Retrieved April 10, 2021, from https://www.alnap.org/help-library/global-tuberculosis-report-2020.
[5] World Health Organization. (2020). Global Tuberculosis Report 2020 | HIV/AIDS Data Hub for the Asia-Pacific Region. Retrieved April 10, 2021, from https://www.aidsdatahub.org/resource/global-tuberculosis-report-2020.
[6] Floyd, K., Glaziou, P., Zumla, A., & Raviglione, M. (2018). The global tuberculosis epidemic and progress in care, prevention, and research: an overview in year 3 of the End TB era. The Lancet Respiratory Medicine, 6(4), 299–314. https://doi.org/10.1016/S2213-2600(18)30057-2.
[7] USAID. (2009). Standard Operating Procedures for Implementation of TB Activities at HIV/AIDS Service Delivery Sites Collaborative TB/HIV Services. Retrieved April 17, 2021, from https://challengetb.org/publications/tools/tb_hiv/SOPCollaborativeTBHIVServices.pdf.
[8] World Health Organization. (2020). Tuberculosis. Retrieved March 30, 2021, from https://www.who.int/news-room/fact-sheets/detail/tuberculosis.
[9] Centers for Disease Control and Prevention. (2016). Basic TB Facts | TB | CDC. Retrieved March 30, 2021, from https://www.cdc.gov/tb/topic/basics/default.htm.
[10] National Health System. (2019). Tuberculosis (TB) - Causes - NHS. https://www.nhs.uk/conditions/tuberculosis-tb/causes/.
[11] The Global Fund. (2021). Tuberculosis - The Global Fund to Fight AIDS, Tuberculosis and Malaria. Retrieved April 10, 2021, from https://www.theglobalfund.org/en/tuberculosis/.
[12] World Health Organization. (2018). HIV/AIDS | WHO | Regional Office for Africa. Retrieved April 11, 2021, from https://www.afro.who.int/health-topics/hivaids.
[13] Measure evaluation. (n.d.). Frameworks Module 250706.ppt — Measure Evaluation. Retrieved March 31, 2021, from https://www.measureevaluation.org/resources/training/capacity-building-resources/phn/course-modules/week-1/Frameworks Module 250706.ppt/view.
[14] Federal Ministry of Health Nigeria. (2010). National Tuberculosis and Leprosy Control Programme: Workers’ manual – Revise 5th Edition 1. Retrieved April 2, 2021, from https://www.who.int/hiv/pub/guidelines/nigeria_tb.pdf.
[15] Adebisi, Y. A., Agumage, I., Sylvanus, T. D., Nawaila, I. J., Ekwere, W. A., Nasiru, M., Okon, E. E., Ekpenyong, A. M., & Lucero-Prisno III, D. E. (2019). Burden of Tuberculosis and Challenges Facing Its Eradication in West Africa. International Journal of Infection, 6(3). https://doi.org/10.5812/iji.92250.
[16] Ologunde, C. A., Anidiobu, C. O., Oluwasusi, V. O., & Ilesanmi, T. M. (2021). Prevalence of Tuberculosis and Human Immunodeficiency Virus (HIV) in Ikere-Ekiti, Ekiti State Southwestern Nigeria. South Asian Journal of Research in Microbiology, 9(1), 1–5. https://doi.org/10.9734/sajrm/2021/v9i130198.
[17] Hassan, A., Olukolade, R., Ogbuji, Q., Onyemocho, A., Okwuonye, L., Igbabul, S., Okechukwu, J., Kusimo, O., Osho, A., Osinowo, K., & Ladipo, O. (2016). Evaluation of Tuberculosis Treatment Outcome of TB/HIV Co-Infection: A Four-Year Retrospective Cohort Study in HIV-Prevalent Setting of North Central Nigeria. Journal of Tuberculosis Research, 04(03), 122–133. https://doi.org/10.4236/jtr.2016.43015.
[18] Dye, C., Harries, A. D., Maher, D., Hosseini, S. M., Nkhoma, W., & Salaniponi, F. M. (2006). Tuberculosis. In Disease and Mortality in Sub-Saharan Africa. The International Bank for Reconstruction and Development / The World Bank. http://www.ncbi.nlm.nih.gov/pubmed/21290646.
[19] Centers for Disease Control and Prevention. (2020). Global Health - Newsroom - Tuberculosis. Retrieved April 10, 2021, from https://www.cdc.gov/globalhealth/newsroom/topics/tb/index.html.
[20] Nwokoro, U. U., Dahiru, T., Olorukooba, A., Daam, C. K., Waziri, H. S., Adebowale, A., Waziri, N. E., & Nguku, P. (2020). Determinants of perinatal mortality in public secondary health facilities, Abuja municipal area council, Federal Capital Territory, Abuja, Nigeria. Pan African Medical Journal, 37(114), 1–12. https://doi.org/10.11604/pamj.2020.37.114.17108.
[21] Hamisu, A. W., Etapelong, S. G., Ayodeji, I. H., Furera, Z., Ningi, N., Jimoh, A., Fiona, B., Banda, R., Tegegne, S. G., Ajogwu, A., Nwachukwu, J., John, D., Abdurrahman, S., Ahmed, F., Adesola, L., Teresa, N., Adesola, O., Rahmat, A., Elizabeth, A., & Lydia, T. (2020). Assessment of the contribution of community active surveillance to covid-19 case detection in the Federal Capital Territory, Abuja, Nigeria. African Journal of Biology and Medical Research, 3(2), 98–110. www.abjournals.org.
[22] Ifeadike, C., Ironkwe, O., Nnebue, C., Nwabueze, S., Ubajaka, C., Adogu, P. O. U., & Emelumadu, O. (2012). Prevalence and pattern of bacteria and intestinal parasites among food handlers in the Federal Capital Territory of Nigeria. Nigerian Medical Journal, 53(3), 166. https://doi.org/10.4103/0300-1652.104389.
[23] Kamweli, M., Id, A., Kwaga, J., Okolocha, E., & Mba, N. (2019). Prevalence and risk factors for multi-drug resistant Escherichia coli among poultry workers in the Federal Capital Territory, Abuja , Nigeria Prevalence and risk factors for multi-drug resistant Escherichia coli among poultry workers in the Federal Capit. November. https://doi.org/10.1371/journal.pone.0225379.
[24] National Tuberculosis and Leprosy Control Programme. (2019). 2019 Annual TB Report. https://www.health.gov.ng/doc/Draft-2019-NTBLCP-Annual-report-22032020.pdf.
[25] Dememew, Z. G., Jerene, D., Datiko, D. G., Hiruy, N., Tadesse, A., Moile, T., Bekele, D., Yismawu, G., Melkieneh, K., Reshu, B., & Suarez, P. G. (2020). The yield of community-based tuberculosis and HIV among key populations in hotspot settings of Ethiopia: A cross-sectional implementation study. PLoS ONE, 15(5), e0233730. https://doi.org/10.1371/journal.pone.023373.
[26] Ejeh, F. E., Undiandeye, A., Okon, K., Kazeem, H. M., & Kudi, A. C. (2020). Isolation and Immunological Detection of Mycobacterium Tuberculosis from HIV and Non-HIV Patients in Benue State, Nigeria. Ethiopian Journal of Health Sciences, 30(1), 55–64. https://doi.org/10.4314/ejhs.v30i1.8.
[27] Inyinbor, H. E., Omosigho, P. O., Akobi, O. A., Gideon, Emumwen, E., Ogedengbe, S. O., Shehu, Kudu Mohammed, Abdullahi1, M. N., Aliyu2, N. J., Oshinsanya1, T. T., Favour, A., Emumwen4, E., & . (2020). Prevalence of Pulmonary Tuberculosis in Bida, North Central Nigeria: A fiveYear Retrospective Study. J Med Lab Sci, 30(4), 26–34.
[28] Ajide, B., Chuku, A., Lawson, L., Orole, K., & and Adogo, L. (2020). Prevalence of Mycobacterium tuberculosis in North Central Nigeria. Nigerian Journal of Microbiology, 34(2), 5325–5332. http://www.nsmjournal.org.ng/2020-34-2/12.pdf.
[29] Ekeke, N., Aniwada, E., Chukwu, J., Nwafor, C., Meka, A., Alphonsus, C., Ezeakile, O., Ajayi, A., Soyinka, F., Bakpa, F., Uwanuruochi, V., Aniekwensi, E., & Eze, C. (2020). Screening diabetes mellitus patients for tuberculosis in southern nigeria: A pilot study. Advances in Respiratory Medicine, 88(1), 6–12. https://doi.org/10.5603/ARM.2020.0072.
[30] Gebretsadik, D., Ahmed, N., Kebede, E., Mohammed, M., & Belete, M. A. (2020). Prevalence of Tuberculosis by Automated GeneXpert Rifampicin Assay and Associated Risk Factors Among Presumptive Pulmonary Tuberculosis Patients at Ataye District Hospital, Northeast Ethiopia. Infection and Drug Resistance, 13, 1507–1516. https://doi.org/10.2147/IDR.S248059.
[31] Ugwu, K. O., Agbo, M. C., & Ezeonu, I. M. (2021). Prevalence of tuberculosis, drug-resistant tuberculosis and HIV/TB co-infection in Enugu, Nigeria. African Journal of Infectious Diseases, 15(2), 24–30. https://doi.org/10.21010/ajid.v15i2.5.
[32] Tola, A., Minshore, K. M., Ayele, Y., & Mekuria, A. N. (2019). Tuberculosis Treatment Outcomes and Associated Factors among TB Patients Attending Public Hospitals in Harar Town, Eastern Ethiopia: A Five-Year Retrospective Study. Tuberculosis Research and Treatment, 2019, 1–11. https://doi.org/10.1155/2019/1503219.
[33] Teferi, M. Y., Didana, L. D., Hailu, T., Woldesenbet, S. G., Bekele, S., & Mihret, A. (2021). Tuberculosis treatment outcome and associated factors among tuberculosis patients at Wolayta Sodo Teaching and Referral Hospital, Southern Ethiopia: a retrospective study. Journal of Public Health Research, 10(3). https://doi.org/10.4081/JPHR.2021.2046.
[34] Tanue, E. A., Nsagha, D. S., Njamen, T. N., & Clement Assob, N. J. (2019). Tuberculosis treatment outcome and its associated factors among people living with HIV and AIDS in Fako Division of Cameroon. PLOS ONE, 14(7), e0218800. https://doi.org/10.1371/JOURNAL.PONE.0218800.
[35] Narasimhan, P., Wood, J., Macintyre, C. R., & Mathai, D. (2013). Risk Factors for Tuberculosis. 2013, 11. https://doi.org/10.1155/2013/828939.
[36] Abdulkader, M., Van Aken, I., Niguse, S., Hailekiros, H., & Spigt, M. (2019). Treatment outcomes and their trend among tuberculosis patients treated at peripheral health settings of Northern
Ethiopia between 2009 and 2014: A registry-based retrospective analysis. BMC Research Notes, 12(1), 1–5. https://doi.org/10.1186/S13104-019-4824-9/FIGURES/1.[37] Mamo, A., Mama, M., Solomon, D., & Mohammed, M. (2021).
Treatment Outcomes and Predictors Among Tuberculosis Patients at Madda Walabu University Goba Referral Hospital, Southeast Ethiopia
. Infection and Drug Resistance, 13, 4763–4771. https://doi.org/10.2147/IDR.S285542.[38] Getahun, B., Ameni, G., Medhin, G., & Biadgilign, S. (2013). Treatment outcome of tuberculosis patients under directly observed treatment in Addis Ababa, Ethiopia. The Brazilian Journal of Infectious Diseases, 17(5), 521–528. https://doi.org/10.1016/J.BJID.2012.12.010.
[39] Io, O., Ti, C., & Em, O. (2021). Detection of HIV and Mycobacterium tuberculosis among University Students in Port Harcourt, Nigeria 1. MedRxiv, 2021.03.06.21253050. https://doi.org/10.1101/2021.03.06.21253050.
[40] Moglad, E. H. O., Ahmed, D. A. O., Awad AL-Kareem, S. M. M., Elgoraish, A. G., Ali, H. T. O., & Altayb, H. N. (2020). Prevalence of human immunodeficiency virus among pulmonary tuberculosis patients: A cross-sectional study. Microbiology and Immunology, 64(12), 810–814. https://doi.org/10.1111/1348-0421.12856.
[41] Mesfin YM, Hailemariam D, Biadgilign S, Kibret KT (2014) Association between HIV/AIDS and Multi-Drug Resistance Tuberculosis: A Systematic Review and Meta-Analysis. PLoS ONE 9(1): e82235. doi: 10.1371/journal.pone.0082235.
Viewed PDF 1238 44 -
 A Study on Knowledge of Health Workers on Vaccine Storage, Distribution, and Cold Chain Management in YemenAuthor: Victor SuleDOI: 10.21522/TIJPH.2013.11.01.Art008
A Study on Knowledge of Health Workers on Vaccine Storage, Distribution, and Cold Chain Management in YemenAuthor: Victor SuleDOI: 10.21522/TIJPH.2013.11.01.Art008A Study on Knowledge of Health Workers on Vaccine Storage, Distribution, and Cold Chain Management in Yemen
Abstract:
The success of the Expanded Programme on Immunization (EPI) over the years is attributed to the immunization supply chain, effective logistics systems, and the health professionals who run them. Gaps in knowledge and practices still exist in developing countries and countries with conflict. Due to the paucity of information regarding the subject in humanitarian settings, this study was carried out. This descriptive cross-sectional study was carried out among health workers at the four levels of the healthcare system in 6 governorates in Yemen. A total of 536 health workers provided responses to the online questionnaire between February and May 2022. The study showed that 515(96.1%) and 521(97.2%) of the respondents, respectively, knew the recommended temperature range for storage of Rota and pentavalent vaccines at the health facility. Most respondents, 415(77.4%) and 413(77.0%) knew the recommended storage temperature for measles and BCG, respectively, and 466(86.9%) knew they could be stored at a negative temperature when the need arises. Over two-thirds of respondents only receive vaccines 411(76.7%), and 124(23.1%) receive and distribute vaccines. Vaccine distribution included the use of refrigerated vehicles (15.2%), cold boxes (32.8%), and vaccine carriers (41.6%), both with conditioned ice packs. Despite the protracted and complex humanitarian situation in Yemen, Health workers demonstrated good knowledge and practices of vaccine storage, distribution, and cold chain management, which contributed to the sustenance of immunization services. There is a need for required investment in a cost-effective and sustainable last-mile vaccine distribution approach to ensure equitable availability of vaccines at health facilities and prevent any missed opportunity.
Keywords: Cold chain, Distribution, Vaccine storage, Knowledge.A Study on Knowledge of Health Workers on Vaccine Storage, Distribution, and Cold Chain Management in Yemen
References:
[1] Osei, E., Ibrahim, M., & Kofi Amenuvegbe, G., 2019, Effective Vaccine Management: The Case of a Rural District in Ghana. Advances in preventive medicine, 2019, 5287287. https://doi.org/10.1155/2019/5287287.
[2] WHO., & UNICEF., 2016, WHO/UNICEF joint statement: Achieving immunization targets with the comprehensive effective vaccine management (cEVM) framework https://apps.who.int/iris/bitstream/handle/10665/254717/WHO-IVB-16.09-eng.pdf.
[3] World Health Organization. (WHO)., 2017, Guideline for establishing or improving primary and intermediate vaccine stores. https://apps.who.int/iris/bitstream/handle/10665/67807/WHO_V-B_02.34_eng.pdf.
[4] Centre for Disease Control and Prevention. (CDC)., 2021, Vaccine Storage and Handling Toolkit https://www.cdc.gov/vaccines/hcp/admin/storage/toolkit/storage-handling-toolkit.pdf.
[5] Nwankwo, B., Joga, S.J., Olorukooba, A.A. et al., 2018, Knowledge, attitude, and practice of cold chain management among primary health care workers in Giwa, Northwestern Nigeria. Arch Med Surg 2018; 3:71-6. https://www.archms.org/text.asp?2018/3/2/71/254575.
[6] Mohammed, S.A., Workneh, B.D., & kahissay, M.H., 2021, Knowledge, attitude and practice of vaccinators and vaccine handlers on vaccine cold chain management in public health facilities, Ethiopia: Cross-sectional study. PLoS ONE 16(2): e0247459. https://doi.org/10.1371/journal.pone.0247459.
[7] Zayer, J., & Chiad, I., 2020, Evaluation of Application of Effective Vaccine Management in Wassit Governorate, Iraq. International journal of pharmaceutical quality assurance. 11. 242-246. https://www.researchgate.net/publication/348780491_Evaluation_of_Application_of_Effective_Vaccine_Management_in_Wassit_Governorate_Iraq.
[8] Al Abri, S., Al-Rawahi, B., Abdelhady, D., & AL abaidani, Idris., 2018, Effective vaccine management and Oman’s healthcare system’s challenge to maintain high global standards. Journal of Infection and Public Health. 11. 10.1016. https://www.researchgate.net/publication/325210133_Effective_vaccine_management_and_Oman’s_healthcare_system’s_challenge_to_maintain_high_global_standards/citation/download.
[9] Gebretnsae, H., Hadgu, T., Ayele, B. et al., 2022, Knowledge of vaccine handlers and status of cold chain and vaccine management in primary health care facilities of Tigray region, Northern Ethiopia: Institutional based cross-sectional study. PLOS ONE. 17. e0269183. 10.1371/journal.pone.0269183.https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0269183.
[10] Ministry of Public Health & Population, Yemen., 2016, Comprehensive Multi-year Plan (cMYP) 2016-2020.
[11] Charan, J., & Biswas, T., 2013, How to calculate sample size for different study designs in medical research? Indian journal of psychological medicine, 35(2), 121–126. https://doi.org/10.4103/0253-7176.116232.
[12] World Health Organization (WHO)., 2005, Vaccine Management Assessment. http://apps.who.int/iris/bitstream/handle/10665/69616/WHO_IVB_05.02_eng.pdf?sequence=1.
[13] Ameen H.A., Salaudeen A.G., Bolarinwa O.A. et al., 2014, Vaccine Storage and Handling Practices among routine immunization service providers in a metropolitan city of North-Central Nigeria. Journal of Community Medicine and Primary Health Care. 26 (2) 18–28. https://www.ajol.info/index.php/jcmphc/article/view/125356.
[14] Feyisa, D., Ejeta, F., Aferu, T. et al., 2022, Adherence to WHO vaccine storage codes and vaccine cold chain management practices at primary healthcare facilities in Dalocha District of Silt’e Zone, Ethiopia. Trop Dis Travel Med Vaccines 8, 10. https://doi.org/10.1186/s40794-022-00167-5.
[15] Mohammed, S.A., Workneh, B.D., & kahissay, M.H., 2021, Knowledge, attitude and practice of vaccinators and vaccine handlers on vaccine cold chain management in public health facilities, Ethiopia: Cross-sectional study. PLoS ONE 16(2): e0247459. https://doi.org/10.1371/journal.pone.0247459.
[16] Daud, Norwati., 2014, Knowledge, Attitude and Adherence to Cold Chain among General Practitioners in Kelantan, Malaysia. https://internalmedicine.imedpub.com/knowledge-attitude-and-adherence-to-cold-chain-amonggeneral-practitioners-in-kelantan-malaysia.php?aid=6257.
[17] Woldamichael, B., Bekele, D., & Esmael, A., 2018, Cold Chain Status and Knowledge of Vaccine Providers at Primary Health Care of Units Bale Zone, Southeast Ethiopia: Cross-sectional Study. Immunome Research. 14,152. https://www.readcube.com/articles/10.4172/1745-7580.1000152.
[18] Zeyneba, J. Y., Habtamu, Y.N., Behailu, T. D. et al., 2019, Knowledge of Health Professionals on Cold Chain Management and Associated Factors in Ezha District, Gurage Zone, Ethiopia, Scientifica, vol. 2019, Article ID 6937291, 7 pages. https://doi.org/10.1155/2019/6937291.
[19] Ebile Akoh, W., Ateudjieu, J., Nouetchognou, J.S. et al., 2016, The expanded program on immunization service delivery in the Dschang health district, west region of Cameroon: a cross sectional survey. BMC Public Health 16, 801. https://doi.org/10.1186/s12889-016-3429-7.
[20] Mavimbe, J.C., Bjune, G., 2007, Cold chain management: Knowledge and practices in primary health care facilities in Niassa, Mozambique. Ethiopian Journal of Health Development, 21(2): 130-135. https://www.ajol.info/index.php/ejhd/article/view/10040.
[21] WHO., & UNICEF., 2016, WHO-UNICEF Effective Vaccine Store Management Initiative: Modules 1-4. https://apps.who.int/iris/bitstream/handle/10665/68993/WHO_IVB_04.16-20.pdf?sequence=1.
[22] PATH Optimize., Aug.2013, Preventing in cold boxes and vaccine carrier. https://media.path.org/documents/TS_opt_handout_freeze_safe.pdf.
[23] Haidari, L. A., Brown, S. T., Wedlock, P., Connor, D. L., Spiker, M., & Lee, B. Y., 2017. When are solar refrigerators less costly than on-grid refrigerators: A simulation modeling study. Vaccine, 35(17), 2224–2228. https://doi.org/10.1016/j.vaccine.2016.11.103.
[24] WHO., & UNICEF., 2015, Introducing solar powered vaccine refrigerator and freezer system: A guide for managers in national immunization programmes https://apps.who.int/iris/bitstream/handle/10665/195778/9789241509862_eng.pdf.
[25] Grasso, M., Ripabelli, G., Sammarco, M. L., Manfredi Selvaggi, T. M., & Quaranta, A, 1999, Vaccine storage in the community: a study in central Italy. Bulletin of the World Health Organization, 77(4), 352–355. https://pubmed.ncbi.nlm.nih.gov/10327715/.
[26] Yakum, M.N., Ateudjieu, J., Walter, E.A. et al. Vaccine storage and cold chain monitoring in the Northwest region of Cameroon: a cross sectional study. BMC Res Notes 8, 145 (2015). https://doi.org/10.1186/s13104-015-1109-9.
[27] UNICEF Supply Division., July 2018, Cold Chain Equipment - Solar Direct Drive and Mains Powered Refrigerator Systems: Product Profiles, Availability, and Guidance UNICEF Supply Division. https://www.unicef.org/supply/sites/unicef.org.supply/files/2019-06/cold-chain-equipment-sdd-drive-and-mains-powered-refrigerators.pdf .
[28] Ministry of Public Health & Population, Yemen. (2020). Application for Country led service bundle under Cold Chain Equipment Optimization Platform (CCEOP) Application.
[29] UNICEF Supply., 2015, Using the Sun to Keep Vaccines Cool: A collaboration to develop an environmentally-friendly, affordable, battery-free
refrigeration system: Solar Direct Drive Technology https://www.unicef.org/innovation/stories/using-sun-keep-vaccines-cool.[30] WHO., & UNICEF., 2017, Evidence brief Solar power refrigerator and Freezer https://apps.who.int/iris/bitstream/handle/10665/254715/WHO-IVB-17.01-eng.pdf;sequence=1.
[31] Department of Health., National Immunization Program Manila, Philippines., 2018, Vaccines, Cold Chain and Logistics Management Manual of Operations 5th edition. https://doh.gov.ph/sites/default/files/publications/NIP-MOP-Booklet%2010.pdf.
Viewed PDF 1388 75 -
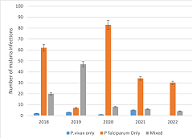 Efficacy of Plasmoquine for the Treatment of Plasmodium Vivax and Plasmodium FalciparumAuthor: Mahadi Abdujabar IssaDOI: 10.21522/TIJPH.2013.11.01.Art009
Efficacy of Plasmoquine for the Treatment of Plasmodium Vivax and Plasmodium FalciparumAuthor: Mahadi Abdujabar IssaDOI: 10.21522/TIJPH.2013.11.01.Art009Efficacy of Plasmoquine for the Treatment of Plasmodium Vivax and Plasmodium Falciparum
Abstract:
This study is a response to the challenge of malaria infections, which remain a major public health in South Africa. Reports of malarial outbreaks in the country have been predominant in KwaZulu-Natal, Mpumalanga, and Limpopo provinces. Currently, combination therapy referred to artemisinin-based combination treatments (ACTs) has been recommended both by the World Health Organization and the National Department of Health of South Africa. However, due to widespread reports of artemisinin resistance, other alternative treatment options were explored. The aim of the study was thus to establish the efficacy of plasmoquine as an alternative treatment option among malaria patients in Johannesburg, the economic capital of South Africa, found in the Gauteng Province. The study adopted a quantitative approach, and a purposive retrospective investigation was adopted. Patient data from 2018-2022 was analyzed to determine the incidence of malaria in the study location and the efficacy of treatment with plasmoquine. The results of this study, therefore, indicate that P. falciparum is still the main cause of malaria in the study area. A total of 322 patient files were included in the study, with P. falciparum determined to be the main cause of infection over the four-year data assessed. Furthermore, plasmoquine was determined to be effective in treating malaria among 298 of the study population, with only 24 (7.5%) experiencing the development of vomiting after the treatment course. The findings of the study offer government makes policymakers the opportunity to develop policies that enhance the re-introduction of plasmoquine to combat malaria in South Africa.
Keywords: Artemisinin-based combination treatments; Artemisinin resistance, Malaria; Plasmoquine.Efficacy of Plasmoquine for the Treatment of Plasmodium Vivax and Plasmodium Falciparum
References:
[1] Domingues, W., Dos Santos, E. H., Yamamoto, L., Di Santi, S. M., Kanunfre, K. A., & Okay, T. S. (2022). Single-round multiplex PCR with species-specific mitochondrial primers of P. falciparum, P. vivax/P. simium and P. malariae/P. brasilianum: Comparison with standard techniques. Journal of Microbiological Methods, 193, 106398.
[2] Akilimali, A., Bisimwa, C., Aborode, A. T., Biamba, C., Sironge, L., Balume, A., ... & Fajemisin, E. A. (2022). Self-medication and Anti-malarial Drug Resistance in the Democratic Republic of the Congo (DRC): A silent threat. Tropical Medicine and Health, 50(1), 1-5.
[3] Weiss, D. J., Bertozzi-Villa, A., Rumisha, S. F., Amratia, P., Arambepola, R., Battle, K. E., & Gething, P. W. (2021). Indirect effects of the Covid-19 pandemic on malaria intervention coverage, morbidity, and mortality in Africa: a geospatial modelling analysis. The Lancet Infectious Diseases, 21(1), 59-69.
[4] Macharia, P. M., Giorgi, E., Noor, A. M., Waqo, E., Kiptui, R., Okiro, E. A., & Snow, R. W. (2018). Spatio-temporal analysis of Plasmodium falciparum prevalence to understand the past and chart the future of malaria control in Kenya. Malaria journal, 17(1), 1-13.
[5] White, N. J. (2019). Triple artemisinin-containing combination anti-malarial treatments should be implemented now to delay the emergence of resistance. Malaria journal, 18(1), 1-3.
[6] Carman (1935)
[7] Gilles HM. Management of severe malaria: a practical handbook. 2nd Edition. Geneva: World Health Organization, 2000.
[8] van der Pluijm, R. W., Amaratunga, C., Dhorda, M., & Dondorp, A. M. (2021). Triple artemisinin-based combination therapies for malaria–a new paradigm? Trends in parasitology, 37(1), 15-24.
[9] Wicht, K. J., Small-Saunders, J. L., Hagenah, L. M., Mok, S., & Fidock, D. A. (2022). Mutant PfCRT Can Mediate Piperaquine Resistance in African Plasmodium falciparum With Reduced Fitness and Increased Susceptibility to Other Antimalarials. The Journal of Infectious Diseases.
[10] McLean, A. R., Indrasuta, C., Khant, Z. S., Phyo, A. K., Maung, S. M., Heaton, J., ... & Smithuis, F. M. (2021). Mass drug administration for the acceleration of malaria elimination in a region of Myanmar with artemisinin-resistant falciparum malaria: a cluster-randomised trial. The Lancet Infectious Diseases, 21(11), 1579-1589.
[11] Naing, C., Whittaker, M. A., Htet, N. H., Aye, S. N., & Mak, J. W. (2019). Efficacy of anti-malarial drugs for treatment of uncomplicated falciparum malaria in Asian region: A network meta-analysis. Plos one, 14(12), e0225882.
[12] Njau, J., Silal, S. P., Kollipara, A., Fox, K., Balawanth, R., Yuen, A., ... & Moonasar, D. (2021). Investment case for malaria elimination in South Africa: a financing model for resource mobilization to accelerate regional malaria elimination. Malaria journal, 20(1), 1-16.
[13] Martineau, P., Behera, S., Nonaka, M., Jayanthi, R., Ikeda, T., Minakawa, N., ... & Mabunda, Q. (2022). Predicting malaria outbreaks from sea surface temperature variability up to 9 months ahead in Limpopo, South Africa, using machine learning. Frontiers in public health, 10.
[14] Craig et al. (2004), Malaria Research Programme, Medical Research Council, Durban, South Africa
[15] Raman, J., Morris, N., Frean, J., Brooke, B., Blumberg, L., Kruger, P., ... & Moonasar, D. (2016). Reviewing South Africa’s malaria elimination strategy (2012–2018): progress, challenges, and priorities. Malaria journal, 15(1), 1-11.
[16] Cui, L., Yan, G., Sattabongkot, J., Cao, Y., Chen, B., Chen, X.s & Zhou, G. (2012). Malaria in the Greater Mekong Subregion: heterogeneity and complexity. Acta tropica, 121(3), 227-239
[17] Nosten, F., & White, N. J. (2007). Artemisinin-based combination treatment of falciparum malaria. Defining and Defeating the Intolerable Burden of Malaria III: Progress and Perspectives: Supplement to Volume 77 (6) of American Journal of Tropical Medicine and Hygiene.
[18] World Health Organization. (2016). Eliminating malaria in the Greater Mekong Subregion: United to end a deadly disease (No. WHO/HTM/GMP/2016.12). World Health Organization.
[19] National Department of Health: Pretoria: South African National Department of Health. 2019. Malaria elimination strategic plan for South Africa 2019-2023.
[20] World Health Organization: Geneva: World Health Organization; 2017. A framework for malaria elimination.
Viewed PDF 1204 27 -
 Epidemiological Characteristics of Frailty and Ageing: Case Study of Elderly Hospice Care Sites in BurundiAuthor: Pierre KwizeraDOI: 10.21522/TIJPH.2013.11.01.Art010
Epidemiological Characteristics of Frailty and Ageing: Case Study of Elderly Hospice Care Sites in BurundiAuthor: Pierre KwizeraDOI: 10.21522/TIJPH.2013.11.01.Art010Epidemiological Characteristics of Frailty and Ageing: Case Study of Elderly Hospice Care Sites in Burundi
Abstract:
Frailty and ageing are bound together, and frailty is linked with reduced capacity and low ability to survive adverse health outcomes. While ageing is glowing globally, in Burundi, a lot has been done to protect and improving the lives of old people, however, multiple challenges persist and limit them from benefiting from their human rights. We, therefore, thought to assess for factors influencing their quality of life, and then to discuss about measures to be taken to ensure ageing in good health. A descriptive cross-sectional study was done in three hospice care sites in Burundi and 57 participants were interviewed using a questionnaire between 16 February and 28th March 2022. Data were analyzed using the Computer Software Statistical Product and Service Solutions (SPSS 20.0). The relationship was considered significant when the P-value was less than the level of significance (<0.05) at 95% confidence interval. The research found that social status is linked with physical frail (p=0.029), and marital status was associated with the apparition of physical signs of frailty (p=0.005); In addition, 47.32 % with the underlining condition were without medication, 90% attended to a clinic 2 times and plus while 28.07% were admitted, 50.87% complained about the limited access to medicine and medical care and 61.40% complained about the variety and the quality of food. These factors can impact ageing in good health, and we recommend that comprehensive support for elderly people be in place and future research compare home-based support and support from hospice care.
Keywords: Access, Ageing, Frailty, Healthcare, Support.Epidemiological Characteristics of Frailty and Ageing: Case Study of Elderly Hospice Care Sites in Burundi
References:
[1] Kenneth, R., 2005, What would make a definition of frailty successful: age and ageing. Oxford University Press on behalf of the British Geriatrics Society, 34: 432–434, https://academic.oup.com/ageing/article/34/5/432/40406?login=true.
[2] Emma, G., L., 2019, Frailty in Tanzania: a longitudinal mixed methods study. Newcastle University, Doctor of Philosophy, Institute of Health, and Society, https://theses.ncl.ac.uk/jspui/handle/10443/4917.
[3] David, R. L., Eilann, C. S., Joan, C. L., Miranda, L. R. W., Mary, P. & Nancy, P. G., 2018, Understanding functional and social risk characteristics of frail older adults: a cross-sectional survey study. NIH, National Library of Medicine, National Center for Biotechnology Information, 19(1):170, https://pubmed.ncbi.nlm.nih.gov/30340530/.
[4] Eva, T., 2008, Ageing, disability and frailty. NIH, National Library of Medicine, National Center for Biotechnology Information, 52 Suppl 1:6-11, https://pubmed.ncbi.nlm.nih.gov/18382070/.
[5] AgeUK, Understanding Frailty, last updated 21/07/2020, https://www.ageuk.org.uk/our-impact/policy-research/frailty-in-older-people/understanding-frailty/.
[6] UNDP, Ageing, Older Persons and the 2030 Agenda for Sustainable Development, 12/07/2017, https://www.undp.org/publications/ageing-older-persons-and-2030-agenda-sustainable-development.
[7] WHO, Ageing and Health, 01/10/2022., https://www.who.int/news-room/fact-sheets/detail/ageing-and-health.
[8] Republique Du Burundi, Rapport des Projections Démographiques 2008-2030, ministère des Finances et de la Planification Economique, Institut de Statistiques et d’Etudes Economiques du Burundi (ISTEEBU) Bujumbura, 11/12/2021, https://www.isteebu.bi/wp-content/uploads/2020/04/Projection-de-la-population-bdi-2008-2030.pdf.
[9] REPUBLIQUE DU BURUNDI, Plan National de Développement du Burundi (PND BURUNDI) 2018-2027, 23/3/2022, https://www.presidence.gov.bi/strategies-nationales/plan-national-de-developpement-du-burundi-pnd-burundi-2018-2027/.
[10] Republique Du Burundi, Document de Politique Nationale de Protection Sociale au Burundi, 12/04/2022, https://www.refworld.org/pdfid/609ed3e74.pdf.
[11] Republique Du Burundi, Protection Sociale au Burundi, 21/5/2022, https://cnps.gov.bi/quest-ce-que-la-protection-sociale/.
[12] Republique Du Burundi, ministère de l’Intégration Nationale, des Affaires Sociales, des Droits de la Personne Humaine et du Genre, Secrétariat Exécutif Permanent de la Commission Nationale de Protection Sociale (SEP/CNPS), 2016, Etude de Base sur le Programme de Financement de l’Accès aux Soins de Santé pour les Personnes Agées au Burundi, Rapport définitif, Réalisé par I.C.G.C, page 23.
[13] Republique Du Burundi, Commission Nationale de protection Sociale/Secrétariat Exécutif Permanent (SEP/CNPS), 2019, Livret Synthèse de la restitution de l’Etude sur la Situation des Personnes Agées dans les Provinces de Gitega, Muramvya et Mwaro, rapport définitif.
[14] UN, HelpAge International, Ageing, Older Persons and the 2030 Agenda for Sustainable Development, 17/2/2022, https://www.un.org/development/desa/dspd/wp-content/uploads/sites/22/2017/08/Ageing-Older-Persons-and-2030-Agenda_Issues-Brief-low-resolution-.pdf.
[15] Republique Du Burundi, ministère de l’Intégration Nationale, des Affaires Sociales, des Droits de la Personne Humaine et du Genre, Stratégie de la Protection Sociale au Burundi, 03/02/2022, https://www.ilo.org/dyn/natlex/docs/ELECTRONIC/110614/137626/F444053803/BDI-110614.pdf.
[16] Lieve, J., Hoeyberghs, J. M. G. A., Schols, D. V., Nico, D. W. et al, 2019, Psychological frailty and quality of life of community dwelling older people: a qualitative study. Applied Research in Quality of Life, 15, 1395–1412 (2020), https://link.springer.com/article/10.1007/s11482-019-09735-y.
[17] Magdalena, S., Jerzy, S. & Katarzyna, W. T., 2020, Determinants of multidimensional and physical frailty and their individual components: interactions between frailty deficits, observational study. NIH, National Library of Medicine, National Center for Biotechnology Information, 21, 17(22):8656, https://pubmed.ncbi.nlm.nih.gov/33233408/.
[18] Bruno, B., Oscar, R., & Tiago, C., 2018, Assessing the social dimension of frailty in old age: A systematic review, Archives of Gerontology and Geriatrics, 78, 101-113, https://doi.org/10.1016/j.archger.2018.06.005.
[19] Fried, L. P., et al, 2001, Frailty in older adults: evidence for a phenotype. NIH, National Library of Medicine, National Center for Biotechnology Information, 56(3):M146-56, https://pubmed.ncbi.nlm.nih.gov/11253156/.
[20] Gobbens, R. J. J.& van, A. M. A. L. M., 2014, The prediction of quality of life by physical, psychological, and social components of frailty in community-dwelling older people. Quality of Life Research, 23, 2289–2300, https://doi.org/10.1007/s11136-014-0672-1.
[21] UNHCR, RefWorld, Burundi: At what age are people considered elderly, treatment of the elderly by society and the authorities, including those who are political militants, 26/02/2018, https://www.refworld.org/cgi-bin/texis/vtx/rwmain?docid=5acf85d74.
[22] WORLD HEALTH RANKINGS, Live Longer Live Better, Burundi, 16/03/2022, https://www.worldlifeexpectancy.com/burundi-life-expectancy.
[23] Buchman, A. S., Wilson, R. S., Bienias, J. L. & Bennett, D. A, 2009, Change in frailty and risk of death in older persons. Experimental Ageing Research, pages 61–82, https://doi.org/10.1080/03610730802545051.
[24] Fereshteh, M. & François, B., 2021, Frailty as a Moderator of the relationship between social isolation and health outcomes in community-dwelling older adults. Environmental Research and Public Health, 18(4): 1675; https://doi.org/10.3390/ijerph18041675.
[25] Caterina, T. et al, 2016, Marital status and frailty in older people: gender differences in the Progetto Veneto Anziani, longitudinal study. Journal of Women’s Health, 25, 6, https://doi.org/10.1089/jwh.2015.5592.
[26] Mina, K., Phyo, K. M., Christopher, M. N. & Alison, D. M. A., 2017, Review of frailty syndrome and its physical, cognitive, and emotional domains in the elderly. Geriatrics, 2(4), 36; https://doi.org/10.3390/geriatrics2040036.
[27] Kota, T. et al, 2018, Ageing-related anorexia and its association with disability and frailty. NIH, National Library of Medicine, National Center for Biotechnology Information, (5):834-843, https://pubmed.ncbi.nlm.nih.gov/30109778/.
[28] Tino, P. Alexander, W., Hannah, M. Z., Sigrid, F. & Hubertus, A., 2021, Impact of common dizziness associated symptoms on dizziness handicap in older adults. Frontiers in Neurology, 12, 801-499, https://doi.org/10.3389/fneur.2021.801499.
[29] Löhler, J. & al, 2019, Hearing impairment in old age: detection, treatment, and associated Risks. Dtsch Arztebl International, 116(17), 301–310, https://doi.org/10.3238/arztebl.2019.0301.
[30] Van, D. B. et al, 2015, Palliative care for older people: A public health perspective. Oxford Academy accessed 11 Nov. 2022, https://doi.org/10.1093/acprof:oso/9780198717614.001.0001.
[31] Michelle, C. O., Pamela, R. B. & Carmen, A. P., 2017, Blood pressure in older adults: The Importance of Frailty. Springer Link, (7): 55, https://doi.org/10.1007/s11906-015-0564-y.
[32] Mit, P., Gorik, O., Sally, H. & Andrew, D., 2004, Burundi: a population deprived of basic health care. British Journal of General Practice, 54(505): 634–635, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1324857/.
[33] Aoife, L. et al., 2021, The impact of frailty screening of older adults with multidisciplinary assessment of those at-Risk during emergency hospital attendance on the quality, safety and cost-effectiveness of care (SOLAR): a randomized controlled trial. Trials, 22: 581 (2021), https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-021-05525-w.
[34] WHO, Clinical Consortium on Healthy Ageing (frailty and intrinsic capacity), 23/04/2022, https://apps.who.int/iris/bitstream/handle/10665/272437/WHO-FWC-ALC-17.2-eng.pdf.
[35] UN General Assembly, Department of Economic and Social Affairs Ageing. International Year of Older Persons 1999, (Principles for older persons), 24/04/2022, https://www.un.org/development/desa/ageing/resources/international-year-of-older-persons-1999/principles.html.
Viewed PDF 1475 40 -
 Implementing a Community-Based Participatory Approach to Promote Health Facility Delivery among Women of Reproductive Age in Kanamai Area, Kilifi CountyAuthor: Johnson S. ManyiwaDOI: 10.21522/TIJPH.2013.11.01.Art011
Implementing a Community-Based Participatory Approach to Promote Health Facility Delivery among Women of Reproductive Age in Kanamai Area, Kilifi CountyAuthor: Johnson S. ManyiwaDOI: 10.21522/TIJPH.2013.11.01.Art011Implementing a Community-Based Participatory Approach to Promote Health Facility Delivery among Women of Reproductive Age in Kanamai Area, Kilifi County
Abstract:
Maternal utilization has been low over the years in Kenya. Approaches to establish safe motherhood through promotion of health facility have been equally fronted. This study applied certain aspects of community education approach encompassing group discussion and community dialogue to provide a clear insight of how the approach is a vital tool. Community based cross sectional study was conducted in Kanamai sub-location, Kilifi County to recruit 232 women selected by simple random sampling technique. The data were collected using pre-tested semi-structured questionnaires and the collected data was coded, entered, cleaned, and analysed using R for Windows (version 4.0.3). Sixty-nine percent (69%) of women advocated for the delivery at the designated health facilities. Independent factors that were found to influence health facility based delivery in this study were being employed (OR = 12.42, 95% CI: 6.25 - 24.70, p<0.0001), having given birth to 3-4 children, (OR = 2.56, 95% CI: 6.25 - 24.70, p=0.0062) and rating of both group discussion (OR = 0.15, 95% CI: 0.03 -0.66, p=0.0041) and community dialogue (OR = 0.21, 95% CI: 0.08 - 0.59, p=0.0013) to be low. Leading by the example set by the government of offering free maternal services, engaging the key stakeholders through approaches such as group discussion and community dialogue could go a long way in increasing delivery in the health facilities thus tremendously lowering mortality rate for both the baby and the mother which could otherwise occur when the mother doesn’t get services of a specialized personnel.
Keywords: Advocacy, Delivery, Community Education Group Discussion, Community Dialogue.Implementing a Community-Based Participatory Approach to Promote Health Facility Delivery among Women of Reproductive Age in Kanamai Area, Kilifi County
References:
[1] Indira, N., Shaver, T., Clark, P.A, Cordero, D., & Faillace, S., 2004, Entry into this World: Who Should Assist? Birth Attendants and Newborn Health. Published by the Basic Support for Institutionalizing Child Survival Project (BASICS II) for the United States Agency for International Development. Arlington, Virginia.
[2] Wanjira, C., Mwangi, M., Mathenge, E., Mbugua, G. & Ng’ang’a, Z., 2011, Delivery Practices and Associated factors among Mothers Seeking Child welfare Services in selected Health Facilities in Nyandarua South District, Kenya. BMC, Public Health, 11-360. https://doi.org/10.1186/1471-2458-11-360.
[3] World Health Organization & United Nations Children’s Fund (UNICEF)., 2010. Countdown to 2015-decade report (2000-2010) with country profiles: taking stock of maternal, newborn and child survival. World Health Organization. https://apps.who.int/iris/handle/10665/44346.
[4] World Health Organization, International Confederation of Midwives & Fédération internationale de Gynécologie et d’Obstétrique., 2004, Making pregnancy safer: the critical role of the skilled attendant: a joint statement by WHO, ICM and FIGO. World Health Organization. https://apps.who.int/iris/handle/10665/42955.
[5] Narahari, P., Chittaranjan, Adanu R., 2015, The unfinished agenda of women’s reproductive health. International Journal of Gynecology & Obstetrics. 131. S1-S2. 10.1016/j.ijgo.2015.04.025.
[6] UNICEF., 2008, Maternal and Newborn health. https://www.unicef.org/health/maternal-and-newborn-health.
[7] UNICEF., 2009, State of the World’s Children Report. https://www.unicef.org/reports/state-worlds-children-2009.
[8] Apple, MW., & Beane, JA., 1995, Democratic schools. Alexandria, VA: Association for Supervision and Curriculum Development.
[9] Gardner, H., 1991, The Unschooled Mind. How Children Think and How Schools Should Teach. New York: Basic Books.
[10] Kenya National Bureau of Statistics, Ministry of Health/Kenya, National AIDS Control Council/Kenya, Kenya Medical Research Institute, National Council for Population and Development/Kenya, and ICF International. 2015, Kenya Demographic and Health Survey 2014. Rockville, MD, USA: Kenya National Bureau of Statistics, Ministry of Health/Kenya, National AIDS Control Council/Kenya, Kenya Medical Research Institute, National Council for Population and Development/Kenya, and ICF International.
[11] Owiti, A., Oyugi, J., & Essink, D. 2018, Utilization of Kenya’s free maternal health services among women living in Kibera slums: a cross-sectional study. The Pan African medical journal, 30, 86. https://doi.org/10.11604/pamj.2018.30.86.15151.
[12] HERA., 2013, Health Partners Ghana. Evaluation of the free maternal health care initiative in Ghana, Accra & Reet.
[13] Zhao, Q., Kulane, A., Gao, Y. & Xu, B., 2009, Knowledge and attitude on maternal health care among rural-to-urban migrant women in Shanghai, China. BMC Womens Health, 9(5). https://doi.org/10.1186/1472-6874-9-5.
[14] Ahmed, N., & Abdel-Rahman, N., 2008, Demographic and socio-economic characteristics of nomadic population/Sudan fifth census. Khartoum. (non-published report).
[15] Bell, J., Sian, L., & Curtis, A., 2003, Trends in Delivery Care in Six Countries. DHS Analytical Studies No. 7. Calverton, Maryland, USA: ORC Macro and the International Research Partnership for Safe Attendance for Everyone (SAFE).
[16] Campbell, O., Graham, W., 2006, Strategies for reducing maternal mortality: getting on with what works. Lancet, 368: 1284-1299. doi: 10.1016/S0140-6736(06)69381-1. PMID: 17027735.
[17] Oestergaard, M.Z., Inoue, M., Yoshida, S., Mahanani, W.R., Gore, F.M., Cousens, S., Lawn, J.E., & Mathers, C.D., 2011, United Nations Inter-Agency Group for Child Mortality Estimation and the Child Health Epidemiology Reference Group. Neonatal mortality levels for 193 countries in 2009 with trends since 1990: a systematic analysis of progress, projections, and priorities. PLoS Med. 8(8): e1001080. doi: 10.1371/journal.pmed.1001080. Epub 2011 Aug 30. PMID: 21918640; PMCID: PMC3168874.
[18] Moore, M., Alex, B., & George, I., 2011, Utilization of Health Care Services by Pregnant mothers during Delivery. A community Based Study in Nigeria. Journal of Medicine and Medical Science. 2(5), 864-867. PMID: 22066284.
[19] Pradhan, A., Aryal, R.H., Regmi, G., Ban, B. & Govindasamy, P., 1996, Nepal Family. Health Survey 1996. Kathmandu, Ministry of Health, Nepal; New Era; Macro International.
[20] Babalola, S., & Fatusi, A., 2009, Determinants of use of maternal health services in Nigeria-looking beyond individual and household factors. Bio Med Central Pregnancy and Childbirth, 9 (43), 1471-2393. https://doi.org/10.1186/1471-2393-9-43.
[21] Gabrysch, S., & Campbell, O.M., 2009, Still too far to walk: Literature review of the determinants of delivery service use. BMC Pregnancy Childbirth 9(34), 1471-2393. https://doi.org/10.1186/1471-2393-9-34.
[22] Manyiwa, J.S., Yuko O.W. & Opiyo, B.O., 2018, Major Predisposing Factors to Utilization of Traditional Birth Attendants by Expectant Mothers in Mombasa County, Kenya. Texila International Journal of Public Health, 6(3), 2520-3134. DOI: 10.21522/TIJPH.2013.06.03. Art016.
[23] Miltenburg S.A., van Pelt S., de Bruin W., & Shields-Zeeman L., 2019, Mobilizing community action to improve maternal health in a rural district in Tanzania: lessons learned from two years of community group activities. Glob Health Action. 2019;12(1),1621590. Doi: 10.1080/16549716.2019.1621590. PMID: 31190635; PMCID: PMC6566771.
Viewed PDF 802 21 -
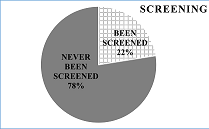 Assessment of Knowledge and Attitude towards Cervical Cancer Screening among Women in Reproductive Age in Chawama Compound, Lusaka, ZambiaAuthor: Voster NyirendaDOI: 10.21522/TIJPH.2013.11.01.Art012
Assessment of Knowledge and Attitude towards Cervical Cancer Screening among Women in Reproductive Age in Chawama Compound, Lusaka, ZambiaAuthor: Voster NyirendaDOI: 10.21522/TIJPH.2013.11.01.Art012Assessment of Knowledge and Attitude towards Cervical Cancer Screening among Women in Reproductive Age in Chawama Compound, Lusaka, Zambia
Abstract:
Cervical cancer is a cancer of the cervix, the organ connecting the uterus and the vagina. It is predominantly caused by human papilloma virus (HPV), which is a sexually transmittable infection-causing pathogen. The purpose of this study was to assess the knowledge and attitudes toward cervical cancer screening among women of the reproductive age group in the Chawama compound Lusaka district. A descriptive cross-sectional research design was used to collect data. The researcher used a questionnaire that included both structured and open-ended questions. Results: Results of this study showed knowledge 59 (73.75%) out of 80 respondents had good knowledge on cervical cancer. The study also revealed that (22%) 18 out of 80 respondents have been screened for cervical cancer, and (78%) 62 out of 80 respondents had never been screened for cervical cancer. The respondents who agreed that cultural beliefs could hinder women from going for cervical cancer were, 18 (22%) out of 80, and 62 (78%) out of 80 denied that cultural beliefs cannot hinder women from going for cervical cancer screening. There is therefore needed to create proper awareness and sensitization of cervical cancer screening as well as improve cervical cancer screening services.
Keywords: Attitude, Cervical cancer, Cervical cancer screening, Knowledge.Assessment of Knowledge and Attitude towards Cervical Cancer Screening among Women in Reproductive Age in Chawama Compound, Lusaka, Zambia
References:
[1] Altaian, R., and Sarg, M.J., (2000). The Cancer Dictionary- Revised Edition. Checkmark Books, facts on file Inc. New York.
[2] Black, M. J. and Hawks, H.J, (2005). Medical-Surgical Nursing, Clinical Management for Positive Outcomes. 7th Edition, Elsevier, USA.
[3] Centers for disease control CDC (2013), Cervical cancer screening among women aged 18-30 years, united states US Department of health and human services. 2013/61c51:1038- 1042.
[4] Gulanick, M., & Myers, J. L. (2017). Nursing care plans: diagnoses interventions, & outcomes. 9th edition. St. Louis, Missouri: Mosby, an imprint of Elsevier Inc.
[5] Monahan, D.F., Sands, K.J., Neighbours, M., Marek, F.J and Green, J.C., (2007). Phipp’s Medical Surgical Nursing- Health and Illness perspectives Europe, Middlde East and Africa edition. 8th Edition, Mosby, St Louis.
[6] World Health Organization, (2018). Cervical Cancer, Human Papilomavirus and HPV Vaccines: Key Points to Policy - Makers and Health Professionals. WHO/RHR/08.14, Geneva, Switzerland.
[7] Mkumba, G. (2006). A study to assess the safety, acceptability, feasibility of implementation of a cervical cancer screening program using Visual Inspection with Acetic acid in Zambia, http://www.cidrz.org/cervical-cancer-screening.
[8] Parkin, D.M. (2010). Global Cancer Statistics in the Year 2000. Lancet Oncol. 2:533-543.
[9] Balogun, M., Odukoya, O. and Ujomu, P. (2012). Knowledge of cervical cancer and its risk factors among women residing in two urban slums in Lagos, Nigeria. Nig Med Pract.
[10] Macha, S. (2008). Cervical Cancer Screening. Published by CIDRZ, Lusaka.
[11] Ministry of Health (2016). National Cancer Control Strategic Plan.
[12] Xinhua News, (2011). More Zambian Women Undergo Cervical Cancer Screening. Available on www.highbeam.com/doc/lP2-28029094.htm.
[13] Central Statistics Office (2015). Zambia Demographic Health Survey. Government Printers, Lusaka.
[14] Adanu, R. (2002). Cervical Cancer Knowledge and Screening in Accra. Ghana Journal of Women’s Health and Gender-Based Medicine. 11 (6); 487-8.
[15] Walraven, G. (2003). Prevention of Cervical Cancer in Africa, a Daunting Task? African Journal of Reproductive Health. Volume 7:2, 7-12.
[16] Ashford. L, and Collymore. Y. (2005). Prevention of Cervical Cancer Worldwide, Population Reference Bureau, Washington.
[17] Aniebue, P.U. and Aniebue, U.U. (2010). Knowledge and Practice of Cervical Cancer Screening among Female Undergraduate Students in a Nigerian University. Springer 2010.
[18] Sanghvi, H., Lacoste, M., and McCormick, (2005). Preventing Cervical Cancer in Low-Resource Settings: from research to Practice. Conference report, Bangkok, Thailand.
[19] Wong, C. (2009). International Union for Health Promotion and Education-Cervical Cancer Prevention and Control in Zambia Professional Development Exchange Program. Lusaka, Zambia.
[20] Leyva, M., Byrd. T. and Tarwater.P, (2006). Attitude towards Cervical Cancer Screening. California Journal of Health Promotion. Volume 4, issue 2, 13- 14.
Viewed PDF 1056 53 -
Pictorial Representation on Non-Steroidal Anti-Inflammatory Drugs Product Package and its Influence on Self Medication among Adults in Alimosho LGA, Lagos State, NigeriaAuthor: Dunoi Onwuemezie AfamDOI: 10.21522/TIJPH.2013.11.01.Art013
Pictorial Representation on Non-Steroidal Anti-Inflammatory Drugs Product Package and its Influence on Self Medication among Adults in Alimosho LGA, Lagos State, Nigeria
Abstract:
The purpose of this study is to determine the influence of pictorial representation on product packs of NSAIDs on their self-medication among adults in Alimosho Local Government Area (LGA) of Lagos State. The study is a descriptive inferential cross-sectional study that involved the collection of data from adults and secondary data from a regulatory authority. The data collected from questionnaires administered to adults who were randomly selected across the LGA was analyzed to evaluate the association between pictorial representation on product packs and the practice of self-medication. A time series analysis was conducted with secondary data obtained from the National Agency for Food and Drug Administration and Control (NAFDAC), Nigeria’s medicine regulatory agency, to determine the possible changes or trends that may have occurred with the availability of NSAIDs with pictorial representation. The respondents who participated in the research were adults who were 18 years and above. Of the 652 respondents, 50.8% were males, and 49.2% were females. Demographic profiles, Information sources, and pictorial influence on product packs of NSAID were tested for association with self-medication. Among respondents, 80.6% admitted that they are self-medicated, and 50.6% of them responded that pictorial representation influenced their decision to purchase NSAIDs. A binary logistic regression was performed to ascertain the association between demographic profile and the influence of pictorial representation on product packs of NSAIDs. The overall model was statistically significant, χ2 (9) = 33.097, p< 0.005. The model explained 1.05% (Nagelkerke R2) of the variance in a pictorial representation and correctly classified 62.3% of cases.
Keywords: Alimosho, Attitude, Knowledge, NSAID, Perception, Self-medication.Pictorial Representation on Non-Steroidal Anti-Inflammatory Drugs Product Package and its Influence on Self Medication among Adults in Alimosho LGA, Lagos State, Nigeria
References:
[1] Bennadi, D. 2013 Self-medication: A current challenge. Journal of Basic and Clinical Pharmacy, 5(1), 19. https://doi.org/10.4103/0976-0105.128253.
[2] Esan D.T. 2018 “Assessment of Self-Medication Practices and Its Associated Factors among Undergraduates of a Private University in Nigeria”, Journal of Environmental and Public Health, vol. 2018, Article ID 5439079, 2018. https://doi.org/10.1155/2018/5439079.
[3] Shafie, M., Eyasu, M., Muzeyin, K., Worku, Y., and Martín-Aragón, S. 2018 Prevalence, and determinants of self-medication practice among selected households in Addis Ababa community. PloS one, 13(3), e0194122. https://doi.org/10.1371/journal.pone.0194122.
[5] NAFDAC 2019 Drug and related product labelling regulations 2019 https://www.nafdac.gov.ng/wp-content/uploads/Files/Resources/Regulations/All_Regulations/Drug-and-Related-Product-Labelling-Regulations-2019.pdf.
[6] NAFDAC 2021 Drug And Related Products Labelling Regulations, 2021 https://www.nafdac.gov.ng/wp-content/uploads/Files/Resources/Regulations/Regulations_2021/Drug-and-Related-Product-Labelling-Regulations-2021.pdf (Accessed 27 May 2022).
[7] ALG (n.d) Alimosho Local Government Area in Metro Lagos https://www.citypopulation.de/php/nigeria-metrolagos.php?cid=NGA025003.
[8] LSG 2013 Lagos State Government Digest of Statistics 2013 http://mepb.lagosstate.gov.ng/wp-content/uploads/sites/29/2017/01/2013-Digest-ofStatistics.pdf.
[9] Wejnert, C., Pham, H., Krishna, N., Le, B., and DiNenno, E. 2012 Estimating design effect and calculating sample size for respondent-driven sampling studies of injection drug users in the United States. AIDS and behavior, 16(4), 797–806. https://doi.org/10.1007/s10461-012-0147-8.
[10] Charan J., and Biswas T. 2013 How to calculate sample size for different study designs in medical research, Indian journal of psychological medicine, 35(2), 121–126. https://doi.org/10.4103/0253-7176.116232.
[11] CSPro 2022 Census and Survey Processing System (CSPro) Online Available https://www.census.gov/data/software/cspro.html (Accessed April 2021).
[13] Bruce N., et al. 2008 Quantitative research methods for health research: a practical interactive guide to epidemiology and statistics. Chichester, UK: Wiley.
[14] Boelsterli U. 2002 Mechanisms of NSAID-induced hepatotoxicity: focus on Nimesulide. Drug Safety, 25(9):633-648. DOI: 10.2165/00002018-200225090-00003. PMID: 12137558.
[15] Masubuchi Y., Yamada S., Horie T. 2000 Possible mechanisms of hepatocyte injury induced by diphenylamine and its structurally related NSAIDS. J Pharmacol Exp Ther, 292:982–987.
[16] Motola D., Vaccheri A., Silvani M. C., et al. 2004 Pattern of NSAID use in the Italian general population: a questionnaire-based survey. European Journal of Clinical Pharmacology, 60(10):731–8.
[17] Ek, S. 2013 Gender differences in health information behaviour: a Finnish population-based survey Online available at: http://heapro.oxfordjournals.org/content/early/2013/08/28/heapro.dat063.full.pdf+html (Accessed 01 October, 2022).
[18] Bidmon, S. and Terlutter, R. 2015 Gender Differences in Searching for Health Information on the Internet and the Virtual Patient-Physician Relationship in Germany: Exploratory Results on How Men and Women Differ and Why Journal of Medical Internet Research 2015, Volume 17, No 6: e156 (Accessed 01 October 2022).
[19] NAFDAC 2020 NAFDAC Green Book https://greenbook.nafdac.gov.ng/ (Accessed 11 October 2022).
[20] Asakitikpi, A. E. 2019 Healthcare Coverage and Affordability in Nigeria: An Alternative Model to Equitable Healthcare Delivery. In (Ed.), Universal Health Coverage. Intech Open. https://doi.org/10.5772/intechopen.85978.
[21] Bart J. and Por M. et al. 2012 Addressing access barriers to health services: an analytical framework for selecting appropriate interventions in low-income Asian countries, Health Policy, and Planning, 27(4):288–300, https://doi.org/10.1093/heapol/czr038.
[22] McLeod S. 2019 What’s the difference between qualitative and quantitative research? https://www.simplypsychology.org/qualitative-quantitative.html.
[23] Akinyuli, D. 2010 The Challenges Faced by NAFDAC in the National Regulatory Process as it relates to Essential Drugs for the prevention of Maternal and Newborn Deaths in Nigeria Tropical Journal Obstetrics and Gynaecology, Vol 27 (1), April 2010 file:///C:/Users/user/Downloads/85148-Article%20Text-208263-1-10-20130201.pdf.
Viewed PDF 875 22 -
 Are Primary Health Care Workers in Ikere Local Government Area of Ekiti State Making Diagnosis or Classification of Diseases before Giving Treatment?Author: Rasheed Adeyemi AdepojuDOI: 10.21522/TIJPH.2013.11.01.Art014
Are Primary Health Care Workers in Ikere Local Government Area of Ekiti State Making Diagnosis or Classification of Diseases before Giving Treatment?Author: Rasheed Adeyemi AdepojuDOI: 10.21522/TIJPH.2013.11.01.Art014Are Primary Health Care Workers in Ikere Local Government Area of Ekiti State Making Diagnosis or Classification of Diseases before Giving Treatment?
Abstract:
Diagnosis is the establishment of a disease condition affecting an individual by a clinician. It is the end result of a process in which a clinician synthesis various combinations of symptoms and signs exhibited by a patient to make a list of possible disease conditions afflicting the patient. This study aimed to ascertain whether Primary Health Care Workers In the Ikere Local Government of Ekiti State were making diagnoses or classifications of diseases before giving treatments. The purpose of this study was to ascertain whether Primary Health Care Workers In the Ikere Local Government of Ekiti State were making diagnoses or classifications of diseases before giving treatments. The study was a retrospective cross-sectional in nature and used secondary data from eight (8) primary health centers within the Local Government, comprising of two (2) Comprehensive and six (6) Basic Health Centers. A total of 513 out-patient cards were examined in the eight selected health facilities. Data was collected and analysed using SPSS version 2.0. Attempt at making a diagnosis were made in 206(40.2%), while no diagnosis were made in 307 (59.6%). 40 different diagnoses were made with malaria alone, 113 (54%) been the most diagnosed. Other diagnoses included wound 17 (8.1%), road traffic accident 10 (4.8%), malaria in combination with typhoid 8 (3.8%), malaria with peptic ulcer and malaria with infection at 2 (1%) each, dysentery, and typhoid 4 (1.9%) each. The uses of physical examination and laboratory investigation as well as diagnosis/ classification before treatment, were low.
Keywords: Classification, Diagnosis, Primary health care, Primary health care workers.Are Primary Health Care Workers in Ikere Local Government Area of Ekiti State Making Diagnosis or Classification of Diseases before Giving Treatment?
References:
[1] Abdulraheem I.S, Olapipo A.R and Amodu M.O:Primary health care servoces in Nigeria: critical issues and strategies for enhancing the use by the rural communities. Journal of Public Health and Epidemiology, 2012; 4(1): 5-13.
[2] Adama Ekenna, Ijeoma Uchenna Itanyi, Ugochukwu Nwokoro, Lisa R Hirschhorn and Benjamin Uzochukwu: How ready is the system to deliver primary healthcare: Results of primary health facility assessment in Enugu State, Nigeria. Health Policy and Planning, 2020; 35(suppl1): 97-106.
[3] Baerheim A: The diagnosis process in general practice: has it a two-phase structure? Family practice, 2001; 18(3): 243-245.
[4] Chukwuemeka Kenechukwu Jude, Agozie Ubesie Chukwunedum and Kunle Obidike Egbuna: Under-five malnutrition in South-Eastern metropolitan city. Afri Health Sci. 2019; 19(4): 3078-3084. https://dx.doi.org/10.4314/ahs.v19i4.29.
[5] Daniel H Kress, Yanfang Su and Hong Wang: Assessment of Primary Health Care System Performance in Nigeria: Using the Primary health care Performance Indicator Conceptual Framework. Health Systems & Reforms. 2016; 2(4): 302-318, DOI:10.1080/23288604.2016.1234861.
[6] Find: Assessment of Diagnostic Gaps and Relevant Digital Health Solutions. 2020.find https://dx.org/wp-uploads/2020/11/NIGERIA_Executive–summary_20201109_v1.0.pdf.
[7] Francis Koce, Gurch Randhawa and Bertha Ochieng: Understanding healthcare self-referral in Nigeria from the service users’ perspective: a qualitative study of Niger state. BMC Health Services Research, 2019; 19:209. https://doi.org/10.1186/s12913-019-4046-9.
[8] Hardeep Singh, Gordon D Schiff, Mark L Graber, Igho Onakpoya and Matthew J Thompson: The global burden of diagnostic errors in primary care. BMJ Qual Saf, 2017; 26: 484-494 doi:10.1136/bmjqs-2016-005401.
[9] H.C Okeke, P Bassey, O.A Oduwole and A Adindu: Clients characteristic and satisfaction with the quality of primary health-care services in Calabar, Nigeria. Calabar J Health Sci, 2019; 3(1):1-8.
[10] Carter JY, Lema OE, Wangai MW, Munafu CG, Rees PH, Nyamongo JA: Laboratory testing improves diagnosis and treatment outcomes in primary health care facilities. Afr J Lab Med. 2012;1(1), Art. #8, 6 pages. https://dx.doi.org/10.4102/ajlm.v1i1.8.
[11] Jonathan S Ilgen, Kevin W Eva, and Glenn Regehr: What’s in a Label? Is Diagnosis the Start or the end of Clinical Reasoning? J Gen Intern Med, 2016; 31(4):435–7. DOI:10.1007/s11606-016-3592-7.
[12] Menizibeya Osain Welcome: The Nigerian health system: Need for integrating adequate medical intelligent and surveillance system. J Pharm Bioallied Sci, 2011; 3(4): 470-478. Doi:10.4103/0975-7406.90100.
[13] Well M, Goldstein L N: How and why Peadiatric Weight Estimation System Fail – A Body Composition Study. Cureus, 2020; 12(3) e7198.DOI: 10.7759/cureus.7198.
[14] Oche Prince I and Ndukwu Geraldine: The Prevalence of Malaria amongst Adults in Remote Primary Health Care Facility in South-South Nigeria. Texila International Journal of Academic research, 2014. ISSN: 2520-3088. DOI: 10.21522/TIJAR.2014.07.02.Art010.
[15] Olawunmi AOlagundoye, Omobolanle O Akinwunmi, Esther T Onafeso, Ihuoma Henshaw, Adewunmi Odujoko, Mutiat A Oladipo-Badmus, Fosade T Amosun and Ibijoke O Ajimobi: Comparative assessment of the of the primary care system: A survey of family physicians’ perspective at tertiary health facility and a new family medicine training facility in the Lagos State health system. J Family Med Prim care, 2020; 9:871-6.
[16] Oyewole MF: Utilization of Primary Health Care Services among Rural Dwellers in Oyo State. Nigeria Journal of Rural Sociology, 2018; 18(1): 106-111.
[17] Peter Hucklbroiche: ‘‘Disease Entity’’ as the Key Theoretical Concept of Medicine. Journal of Medicine and Philosophy,2014; 39: 609-633. DOI:10.1093/jmp/jhu040.
[18] Primary health care systems (PRIMASYS): case study from Nigeria. Geneva: World Health Organization; 2017. Licence: CCBY-NC-SA 3.0 IGO.
[19] Robert Edwin Rakel: Diagnosis. https://www.britannica.com/science/diagnosis.
[20] Talal Asif, Amena Mohiuddin, Badar Hasan and Rebecca R Pauly: Importance of Thorough Physical Examination: A lost Art. Cureus, 2017; 9(5): e1212. DOI 107759/cureus.1212.
[21] Victoria Wurcel, Americo Cicchetti, Louis Garrison, Michelle M. A Kip, Hendrik Koffijberg, Anne Kolbe, Mariska M. G Leeflang, Tracy Merlin, Jorge Mestre-Ferrandiz, Wija Oortwijn, Cor Oosterwijk, Sean Tunis and Bernarda Zamora: The value of Diagnostic Information in Personalized Healthcare: A Comprehensive Concept to Facilitate
Bringing This Technology into Healthcare System.Public Health Genomics, 2019; 22: 8-15. DOI: 10.1159/000501832.Viewed PDF 1228 31 -
 Predictors of Adverse Events Following Immunization Reporting amongst Healthcare Workers in Jigawa State, Northern Nigeria, 2022Author: Belinda Vernyuy UbaDOI: 10.21522/TIJPH.2013.11.01.Art015
Predictors of Adverse Events Following Immunization Reporting amongst Healthcare Workers in Jigawa State, Northern Nigeria, 2022Author: Belinda Vernyuy UbaDOI: 10.21522/TIJPH.2013.11.01.Art015Predictors of Adverse Events Following Immunization Reporting amongst Healthcare Workers in Jigawa State, Northern Nigeria, 2022
Abstract:
An adverse event following immunization (AEFI) is any untoward medical occurrence that follows immunization and does not necessarily have a causal relationship with the usage of the vaccine. Reporting of AEFI is suboptimal amongst healthcare workers (HWs). This study aimed to determine predictors of HW’s reporting of AEFI. A descriptive cross-sectional study was conducted among HWs in selected health facilities (HFs) in Jigawa State using an open data kit self-administered questionnaire to collect data on socio-demographic characteristics, training, knowledge, and their practices on AEFI reporting. Analysis was conducted using Statistical Package for Social Sciences (SPSS) for frequencies, proportions, and associations using bivariate analysis and multivariate analysis using logistic regression to determine predictors of AEFI reporting with statistical significance set at p<0.05 and 95% confidence interval. Of the 400 respondents, 280 (70%) respondents had good knowledge of AEFI, 328(82%) sends routine AEFI reports and of 212 (53%) who recently encountered an AEFI, 174 (82.1%) exhibited some good reporting practices. Female gender (AOR 0.46, p=0.035), full-time employees (AOR 0.227, p=0.019), a recent encounter with an AEFI (AOR 3.087, p=0.007) and being trained on AEFI (AOR 5.54, p=0.011), reporting to elicit training (AOR 2.70, p=0.031) were predictors of routine reporting from health facility and reporting an encountered AEFI respectively. Overall, gender, employment status, being trained, and recent AEFI encounter to elicit training were predictors of AEFI reporting. To improve reporting of AEFI, there is a need to engage and train health workers on AEFI surveillance.
Keywords: Adverse events following immunization, Knowledge, Practice, Predictors, Reporting.Predictors of Adverse Events Following Immunization Reporting amongst Healthcare Workers in Jigawa State, Northern Nigeria, 2022
References:
[1] Deoja, G., Shanmuganathan, P., Kumarappan, M., 2018, Safety surveillance and causality assessment of adverse event following immunization in children - A vaccine vigilance study. Natl J Physiol Pharm Pharmacol, 8(9), 1209, https://www.njppp.com/.
[2] WHO, Explorations of inequality: Childhood immunization, Accessed: 3 May 2022. https://www.who.int/data/health-equity/report_2018_immunization.
[3] WHO, Immunization and conflict, Accessed: 3 May 2022. https://www.unicef.org/immunization/immunization-and-conflict.
[4] WHO, Vaccines and immunization, Accessed: 23 April 2022. https://www.who.int/health-topics/vaccines-and-immunization.
[5] Al Awaidy, S., Bawikar, S., Prakash, K. P., Al Rawahi, B., Mohammed, A. J., 2010, Surveillance of adverse events following immunization: 10 years’ experience in Oman. EMHJ - East Mediterr Health J, 16 (5) 474-480, https://apps.who.int/iris/handle/.
[6] Ekwueme, O. C., 2009, Adverse events following immunization: Knowledge and experience of mothers in immunization centres in Enugu State, Nigeria. Int J Med Health Dev, 14(1), https://doi.org/.
[7] Joshi, N., Prajapati, H., Solanki, K., Sukhlecha, A., Trivedi, H., Gajera, M., et al., 2013, Pattern of adverse events following immunization in an Indian teaching hospital. Int J Med Sci Public Health, 2(1), 62-68, https://doi.org/.
[8] Sadoh, A. E., Nwaneri, D. U., Ogboghodo, B. C., Sadoh, W. E., 2018, Comparison of adverse events following pentavalent and diphtheria‐tetanus‐pertussis vaccines among Nigerian children. Pharmacoepidemiol Drug Saf, 27(1), 119–122, https://doi.org/.
[9] Williams, S. E., Edwards, K. M., Baxter, R. P., LaRussa, P. S., Halsey, N. A., Dekker, C. L., et al., 2013, Comprehensive Assessment of Serious Adverse Events Following Immunization by Health Care Providers. J Pediatr, 162(6), 1276-1281, https://doi.org/.
[10] Zvanaka, S., Tsitsi, J., Chonzi, P., Shambira, G., Gombe, N. T., Tshimanga, M., 2016, Evaluation of the adverse events following immunizations surveillance system in Harare City, Zimbabwe, 2016: a descriptive cross-sectional study. Pan Afr Med J, 28(1), https://doi.org/.
[11] Mohammed, L. A., Aliyu, A. A., Maiha, B. B., Isa, A., 2018, Knowledge, perception and reporting attitude of adverse effects following immunization among primary healthcare workers in sabon gari local government area Zaria, Kaduna State, Nigeria. Niger J Basic Clin Sci, 15(1), 81, https://doi.org/.
[12] Alvarez-Pasquín, M. J., Heijbel, H., Yarwood, J., Damme, P. V., Partners, V., 2009, VACSATC (Vaccine safety: attitudes, training and communication): Why such a project? Eurosurveillance, 14(16), 19181, https://doi.org/.
[13] Kuçuku, M., 2012, Role of Pharmacovigilance on Vaccines Control. J Rural Med, 27(1), 42–45, https://doi.org/.
[14] Freed, G. L., Clark, S. J., Hibbs, B. F., Santoli, J. M., 2004, Parental vaccine safety concerns: The experiences of pediatricians and family physicians. Am J Prev Med, 26(1), 11–14, https://doi.org/.
[15] Masika, C. W., Atieli, H., Were, T., 2016, Knowledge, Perceptions, and Practice of Nurses on Surveillance of Adverse Events following Childhood Immunization in Nairobi, Kenya. BioMed Res Int. 2016, 3745298–10, https://doi.org/.
[16] Swarnkar, M., Baig, V. N., Soni, S. C., Shukla, U. S., Ali, J., 2016, Assessment of Knowledge and Practice About Immunization Among Health Care Providers. Natl J Community Med, 7(04), 281–285, https://www.njcmindia.org/.
[17] Aderibigbe, S., Osagbemi, G., Bolarinwa, O., 2010, Adverse event following immunization in a Nigerian tertiary health institution. Am J Sci Ind Res, 1, 496–499, https://doi.org/.
[18] Ogunyemi, R., Odusanya, O., 2016, A survey of knowledge and reporting practices of primary healthcare workers on adverse experiences following immunisation in alimosho local government area, Lagos, Nigeria. Postgrad Med J, 23 (79), https://www.npmj.org/.
[19] Gbenewei, E., Nomhwange, T., Taiwo, L., Ayodeji, I., Yusuf, K., Jean Baptiste, A. E., et al., 2011, Adverse events following immunization: Findings from 2017/2018 measles vaccination campaign, Nigeria AEFI reporting in 2017/2018 measles vaccination campaign. Vaccine. 39, C82–C88, https://doi.org/.
[20] Mehmeti, I., Nelaj, E., Simaku, A., Tomini, E., Bino, S., 2017, Knowledge, practice and approaches of health professionals to adverse events following immunization and their reporting in Albania. Heliyon, 3(6), https://doi.org/.
[21] WHO, Vaccine Safety Basics, Accessed: 21 December 2020. https://vaccine-safety-training.org/investigation.html.
[22] McClenathan, B. M., Edwards, K. M., 2019, Vaccine safety: An evolving evidence‐based
science. Br J Clin Pharmacol, 85(12), 2649–2651, https://doi.org/.[23] Principi, N., Esposito, S., 2016, Adverse events following immunization: real causality and myths. Expert Opin Drug Saf, 15(6), 825–835, https://doi.org/.
[24] Lwanga, S. K., Lemeshow, S., 1991, Sample size determination in health studies: a practical manual, World Health Organization. https://apps.who.int/iris/handle/.
[25] Umar, A., Sufiyan, M., Tukur, D., Onoja-Alexander, M., Amadu, L., Bashir, S., 2020, Knowledge of Adverse Events Following Immunization Reporting Tool and System Among Primary Healthcare Workers in Jigawa State, Infect Control Hosp Epidemiol, 41(S1), https://doi.org/.
[26] Sani, U. M., Oche, M. O., Raji, M. O., Ango, U. M., Jiya, N. M., 2019, Knowledge, Attitude and Reporting Practices on Adverse Events Following Immunization among Routine Immunization Service Providers in Health Facilities of Sokoto State, Nigeria. Int J Trop Dis Health, 2019, 1–14, https://doi.org/.
[27] Ogunyemi, R., Odusanya, O., 2016, A survey of knowledge and reporting practices of primary healthcare workers on adverse experiences following immunisation in alimosho local government area, Lagos, Nigeria. Postgrad Med J, 23 (79), https://doi.org/.
[28] Yamoah, P., Bangalee, V., Oosthuizen, F., 2019, Knowledge and Perceptions of Adverse Events Following Immunization among Healthcare Professionals in Africa: A Case Study from Ghana. Vaccines Basel, 7(1), 28, https://doi.org/.
[29] The Global Vaccine Safety Initiative (GVSI), Accessed: 23 April 2022. https://www.who.int/initiatives/the-global-vaccine-safety-initiative.
Viewed PDF 1081 41 -
 Barriers to HIV Testing among Clients of Female Sex Workers an Assessment of Ogoja Local Government AreaAuthor: Simon J, AgadaDOI: 10.21522/TIJPH.2013.11.01.Art016
Barriers to HIV Testing among Clients of Female Sex Workers an Assessment of Ogoja Local Government AreaAuthor: Simon J, AgadaDOI: 10.21522/TIJPH.2013.11.01.Art016Barriers to HIV Testing among Clients of Female Sex Workers an Assessment of Ogoja Local Government Area
Abstract:
Frequent engagement of men in sexual encounters with female sex workers (FSWs) while not using condoms places them at high risk for Human Immunodeficiency Virus (HIV) infection. HIV testing has been noted to be among the necessary methods to stop HIV transmission and acquisition. However, it’s illustrious that not all men voluntarily test for Human Immunodeficiency Virus (HIV), take a look at how to stop Human immunodeficiency virus (HIV) transmission and/or acquisition. This study aimed to spot barriers to accessing Human immunodeficiency virus (HIV) testing services among men. World Health Organization square measure shoppers of female sex workers (clients) in Ogoja Cross River North, South-South Nigeria. A comprehensive search of recent literature uncovered a fancy array of social, Personal, and behavioural barriers, as well as knowledge/awareness of the Human immunodeficiency virus (HIV) infection’s existence, perception of human immunodeficiency (HIV) risk, stigma from care suppliers or family/partners/friends, distrust of care providers/systems. The purpose of this study is to explore possible barriers to HIV counseling and testing uptake among clients of Female Sex Workers in the Ogoja Local Government area of Cross River State, Nigeria, and to see possible ways of mitigating the barriers to epidemic control. This study was conducted in Ogoja Cross River State, Nigeria, with a sample size of 100 male clients of female sex workers, via random sampling technique through an online survey system known as Mwater for data collection. Frequency counts and percentages were used for data analysis. Vital findings of the study conclude: stigma and trust impact uptake of HIV test among male clients of female sex workers.
Keywords: Acquired immunodeficiency syndromes, Barriers, Female sex workers, Human immunodeficiency virus, Human immunodeficiency virus testing, Male.Barriers to HIV Testing among Clients of Female Sex Workers an Assessment of Ogoja Local Government Area
References:
[1] Medicinenet (2020): Infectious Disease: Are These Historical Illnesses Coming Back? Retrieved from: https://www.medicinenet.com/diseases_conditions_making_comeback/article.htm.
[2] Wikipedia (2022): Sex worker Retrieved on https://en.wikipedia.org/wiki/Sex_worker.
[3] Meyer KB, Pauker SG., 1987; Screening for HIV: can we afford the false positive rate? N Engl J Med. 317:238-241.
[4] Centres for Disease Control., 1989; Interpretation and use of the Western blot assay for serodiagnosis of human immunodeficiency virus type 1 infection. MMWR Morb Mortal Wkly Rep.;38(Suppl 7):S1-S7.
[5] Case KK, Ghys PD, Gouws E, Eaton JW, Borquez A, Stover J, et al., 2012; Understanding the modes of the transmission model of new HIV infection and its use in prevention planning. Bull World Health Organ. 90:831–8A.
[6] Shaw SY, Bhattacharjee P, Isac S, Deering KN, Ramesh BM, Washington R, et al. A., 2013; cross-sectional study of sexually transmitted pathogen prevalence and condom use with commercial and non-commercial sex partners among clients of female sex workers in southern India. Sex Transm Dis. 40(6):482–9.
[7] Couture MC, Soto JC, Akom E, Labbe AC, Joseph G, Zunzunegui MV., 2008; Clients of female sex Workers in Gonaives and St-Marc, Haiti characteristics, sexually transmitted infection prevalence, and risk factors. Sex Transm Dis. 35(10):849–55.
[8] Xu JJ, Wang N, Lu L, Pu Y, Zhang GL, Wong M, et al., 2008; HIV and STIs in clients and female sex Workers in Mining Regions of Gejiu City, China. Sex Transm Dis. 35(6):558–65.
[9] Jin X, Smith K, Chen RY, Ding G, Yao Y, Wang H, et al., 2010; HIV prevalence and risk behaviors among male clients of female sex workers in Yunnan, China. J Acquir Immune Def Syn. 53(1):131–5.
[10] Nguyen NT, Nguyen HT, Trinh HQ, Mills SJ, Detels R., 2009; Clients of female sex workers as a bridging population in Vietnam. AIDS Behav. 13(5):881–91.
[11] Volkmann T, Wagner KD, Strathdee SA, Semple SJ, Ompad DC, Chavarin CV, et al., 2014; Correlates of self-efficacy for condom use among male clients of female sex Workers in Tijuana, Mexico. Arch Sex Behav. 43(4):719–27.
[12] Suryawanshi D, Bhatnagar T, Deshpande S, Zhou W, Singh P, Collumbien M., 2013; Diversity among clients of female sex Workers in India: comparing risk profiles and intervention impact by the site of solicitation. Implications for the vulnerability of less visible female sex workers. PLoS One. 8(9):e73470.
[13] Miller GA, Mendoza W, Krone MR, Meza R., 2004; Clients of female sex Workers in Lima, Peru: a bridge population for sexually transmitted disease/HIV transmission? Sex Transm Dis. 31(6):337–42.
[14] Ramanathan S, Nagarajan K, Ramakrishnan L, Mainkar MK, Goswami P, Yadav D, et al., 2014; Inconsistent condom use by male clients during anal intercourse with occasional and regular female sex workers (FSWs): survey findings from southern states of India. BMJ Open. 4(e005166):1–8.
[15] Kementrian Kesehatan RI. Laporan Situasi Perkembangan., 2016; HIV/AIDS & PIMS ddiseases Indonesia, Tahun Jakarta: Kementrian Kesehatan RI. 16 (4)18-28 Available at: http://www.aidsindonesia.or.id/ck_uploads/files/Final%20Laporan%20HIV%20AIDS%20TW%204%202016.pdf
[16] Fonner VA, Denison J, Kennedy CE, O’Reilly K, Sweat M., 2014; Voluntary counselling and testing (VCT) for changing HIV-related risk behavior in developing countries. Cochrane Database Syst Rev. 9:1–28.
[17] Painter TM., 2001; Voluntary counselling and testing for couples:na high-leverage intervention for HIV/AIDS prevention in sub-Saharan Africa. Soc Sci Med. 53:1397–411.
[18] Cohen MS, Chen YQ, McCauley M., 2011; Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 365(6):493–505.
[19] WHO., 2015; Consolidated guidelines on HIV testing services. Geneva: World Health Organization.
[20] Niccolai LM, Odinokova VA, Safiullina LZ., 2012; Clients of street-based female sex workers and potential bridging of HIV/STI in Russia: results of a pilot study. AIDS Care. 24(5):665–72.
[21] Fleming PJ, Barrington C, Perez M, Donastorg Y, Kerrigan D., 2015; Strategies for recruiting steady male partners of female sex workers for HIV research. AIDS Behav. 19(2):362–8.
[22] Patterson TL, Goldenberg S, Gallardo M., 2009; Correlates of HIV, sexually transmitted infections, and associated high-risk behaviors among male clients of female sex workers in Tijuana, Mexico. AIDS. 23(13):1765–71.
[23] Darling K.E., Diserens EA, N’Garambe C. A., 2012; cross-sectional survey of attitudes to HIV risk and rapid HIV testing among clients of sex workers in Switzerland. Sex Transm Infect. 88(6):462–4.
[24] UNAIDS. 90-90-90., 2014; an ambitious treatment target to help end the AIDS epidemic. Geneva: Joint United Nations Programme on HIV/AIDS.
[25] Lahuerta M, Torrens M, Sabidó M, Batres A, Casabona J., 2013; Sexual risk behaviours and barriers to HIV testing among clients of female sex workers in Guatemala: a qualitative study. Cult Health Sex. 15(7):759–73.
[26] Siu GE, Wight D, Seeley JA., 2014; Masculinity, social context, and HIV testing: an ethnographic study of men in Busia district, rural eastern Uganda. BMC Public Health. 14(33):1-11.
[27] Levesque J-F, Harris MF, Russell G., 2013; Patient-centred access to health care: conceptualizing
access at the interface of health systems and populations. Int J Equity Health. 12(18):1–9.[28] Fauk NK, Mwanri L., 2015; Inequalities in addressing the HIV epidemic: the story of the Indonesia Ojek community. Int J Hum Rights Healthcare. 8(3):144–59.
[29] Fauk NK, Mwanri L., 2014; Economic and environmental determinants of Ojek’s susceptibility to HIV infection. Int J Appl Pharm Sci BioMed Sci. 3(1):291–300.
[30] Lobiondo-Wood G, Haber J., 2010 Nursing research: methods and critical appraisal for evidence-based practice. St Louis, MO: Mosby. 3(2) 263-300.
[31] Corbin J, Strauss A., 1990; Grounded theory research: procedures, canons, and evaluative criteria. Qual Sociol. 13(1):1–21.
[32] Ritchie J, Spencer L., 1994; Qualitative data analysis for applied policy research. In: Bryman A, Burgess RG, editors. Analyzing qualitative data. London: Routledge; 1994; p. 173–94.
[33] Fauk NK, Mwakinyali SE, Putra S, Mwanri L., 2017; The socio-economic impacts of AIDS on families caring for AIDS-orphaned children in Mbeya rural district, Tanzania. Int J Hum Rights Healthcare. 10(2):132–45.
[34] Ritchie J, Spencer C., 1994; Qualitative data analysis for applied policy research. In: Bryman A, Burgess RG, editors. Analyzing qualitative data. London: New York Routledge; p. 173–94.
[35] Pope C, Ziebland S, Mays N., 2000; Qualitative research in health care: analysing qualitative data. BMJ. 320(7227):114–6.
[36] Fauk NK, Mery MS, Sigilipoe MA, Putra S, Mwanri L., 2017; Culture, social networks and HIV transmission among men who have sex with men in Indonesia. PLoS One. 12(6):1–14.
[37] Smith J, Firth J., 2011; Qualitative data analysis: the framework approach. Nurse Res. 18(2):52–62.
Viewed PDF 1064 38 -
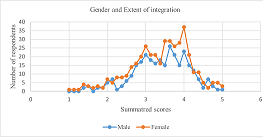 Extent of Integration of Social Determinants of Health in Clinical Practice in Hospitals in UgandaAuthor: Higenyi EmmanuelDOI: 10.21522/TIJPH.2013.11.01.Art017
Extent of Integration of Social Determinants of Health in Clinical Practice in Hospitals in UgandaAuthor: Higenyi EmmanuelDOI: 10.21522/TIJPH.2013.11.01.Art017Extent of Integration of Social Determinants of Health in Clinical Practice in Hospitals in Uganda
Abstract:
The study determined the extent to which health workers in hospitals in Uganda integrate social determinants into clinical practice. This will provide a baseline for improvement interventions and act as a starting point for elucidating the factors influencing the integration of social determinants into clinical practice. This was a multi-method cross-sectional study conducted at 12 hospitals in Uganda. Data was collected between September and November 2021 involving 1042 health workers, 21 key informants, 2119 medical records, and six focus groups. The extent of integration was measured using an eight-item Likert scale for health workers (Cronbach’s alpha of 0.794, inter-item correlation 0.15 to 0.5;) 24-item Likert scale for key informants (Cronbach’s alpha was 0.973, inter-item correlation 0.18 to 0.936), and medical records. The study was approved by the research and ethics committee of Makerere University School of Health Sciences and by the Texila American University Faculty and registered by the National Council of Science and Technology. The aggregate extent of integration was 66%, computed as the average health workers score (66%), key informants score (65%), and medical records score (66%). There were variations across hospitals and social demographics of health workers. The extent of integration of social determinants into clinical practice was successfully determined. Further investigations are required to explain the variations across hospitals. The study did not take into consideration carry-over effects from health workers working in non-hospital healthcare settings.
Keywords: Social determinants; Clinical practice; Integration; Factors; Hospitals; Uganda.Extent of Integration of Social Determinants of Health in Clinical Practice in Hospitals in Uganda
References:
[1] Han, D. S., Sang-Soo Bae, Kim, D.-H., & Choi, Y.-j. 2017, Origins and Evolution of Social Medicine and Contemporary Social Medicine in Korea. Preventive Medicine and Public Health, 50(3), 141-147. doi: 10.3961/jpmph.16.106. https://koreascience.kr/article/JAKO201718836709557.pdf.
[2] Anne A., A. 2018, Screening for social determinants of health in clinical care: moving from the margins to the mainstream. Public Health Review, 39(19). doi: https://doi.org/10.1186/s40985-018-0094-7. https://publichealthreviews.biomedcentral.com/articles/10.1186/s40985-018-0094-7.
[3] Samantha A and Elizabeth H 2018, Beyond Health Care: The Role of Social Determinants in Promoting Health and Health Equity. Date of Access: 30/07/22. https://www.kff.org/disparities-policy/issue-brief/beyond-health-care-the-role-of-social-determinants-in-promoting-health-and-health-equity/.
[4] Andermann, A. 2016, Taking action on the social determinants of health in clinical practice: a framework for health professionals. CMAJ, 188(17-18). doi:10.1503/cmaj.160177. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5135524/.
[5] Phillips, J., Richard, A., Mayer, K. M., Shilkaitis, M., Fogg, L. F., & Vondracek, H. 2020, Integrating the Social Determinants of Health into Nursing Practice: Nurses' Perspectives. Nursing Scholarship. Retrieved November 15, 2020, from https://sigmapubs.onlinelibrary.wiley.com/doi/full/10.1111/jnu.12584.
[6] National Academies of Sciencies, Engineering and Medicne. (2019). Integrating Social Care into the Delivery of Health Care: Moving Upstream to Improve the Nation’s Health. Washington, DC: The National Academies Press. doi: https://doi.org/10.17226/25467.
[7] American Academy of Family Physicians. (2018). Addressing Social Determinants of Health in Primary Care team-based approach for advancing health equity. The Everyone Project. Date Accessed: 7/31/22. https://www.aafp.org/dam/AAFP/documents/patient_care/everyone_project/team-based-approach.pdf.
[8] WHO. (2008). Social determinants of health. Date Accessed: 29/08/2020, https://www.who.int/social_determinants/thecommission/finalreport/key_concepts/en.
[9] J. Michael O.,2008. Macrosocial Determinants of Population Health: Edited by Sandro Galea. American Journal of Epidemiology, 167(12). https://doi.org/10.1093/aje/kwn059. https://academic.oup.com/aje/article/167/12/1518/88508.
[10] Allie F., 2020. Applying Social Determinants of Health to Improve Care Coordination. Date Accessed: 26/05/2020; https://hitconsultant.net/2020/05/26/applying-social-determinants-of-health-to-improve-care-coordination/#.YYiJWmBBw2w.05/26/2020.
[11] Labib G, Gerald V. G., David Z., Anne A., 2018. Physician experiences and barriers to addressing the social determinants of health in the Eastern Mediterranean Region: a qualitative research study. BMC Health Services Research (2018) 18:614. https://doi.org/10.1186/s12913-018-3408-z.
[12] Deloitte. (2017). Social determinants of health: How are hospitals and health systems investing in and addressing social needs? https://www2.deloitte.com/content/dam/Deloitte/us/Documents/life-sciences-health-care/us-lshc-addressing-social-determinants-of-health.pdf.
[13] Arvin G., Brian J., Barry Z., 2013, Addressing Social Determinants of Health within the Patient-Centred Medical Home. Date Accessed: 07/07/2019, https://www.pcpcc.org/resource/addressing-social-determinants-health-within-patient-centered-medical-home.
[14] Popay J, Kowarzik U, Mallinson S, Mackian S, Barker J. 2007. Social problems, primary care and pathways to help and support addressing health inequalities at the individual level. Part II: lay perspectives. J Epidemiology Community Health.;61(11) doi: 10.1136/jech.2007.061945.
[15] Cecilia O. 2021. Government Rushes to Procure More Hospital Beds. The New Vision, 07 July https://www.newvision.co.ug/articledetails/108087.
[16] Mohamad A. P., 2013. Sample size calculation in medical studies. Gastrology and Hepatology from Bed to Bench, 6(1) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4017493/.
[17] Jarmusz, S. V. 2019. News and Insights: Data insights. (S. v. Jarmusz, Editor) Retrieved from mgma.com: https://www.mgma.com/data/data-stories/screening-for-social-determinants-of-health-(sdoh).
[18] Ministry of Health, 2018. Annual Health Sector Performance Report http://library.health.go.ug/sites/default/files/resources/AHSPR%202017_18%20FY.pdf.
[19] UCLA Centre for Health Policy Research 2004. Section 4: Key informant Interviews. https://healthpolicy.ucla.edu/programs/health-data/trainings/Documents/tw_cba23.pdf.
[20] Paul E. S. 1992. Summated Rating Scale Construction: An Introduction Sage University Papers Series. Quantitative Applications in the Social Sciences; No. 07-082. https://home.ubalt.edu/tmitch/645/articles/Summated%20Rating%20Scales.pdf.
[21] Anol B., 2012. Social Science Research: Principles, Methods, and Practices. https://courses.lumenlearning.com/suny-hccc-research-methods/chapter/chapter-6-measurement-of-constructs/
[22] Uganda Bureau of Statistics, 2019. Annual Labour Force Survey 2018/19. https://www.ubos.org/wp-content/uploads/publications/05_20212018-19_ALFS_Report_FINAL.pdf.
[23] WEMOS Health Limited, 2019 Uganda’s Human Resources For Health: Paradoxes And Dilemmas. Country Report Uganda. https://www.wemos.nl/wp-content/uploads/2019/11/Wemos_Country-report-Uganda-2019_Ugandas-Human-resources-for-health_Paradoxes-and-dilemmas.pdf.
[24] Office of International Religious Freedom. 2019. Report on International Religious Freedom: Uganda. https://www.state.gov/reports/2019-report-on-international-religious-freedom/uganda/#:~:text=According%20to%20the%20most%20recent,14%20percent%2.
[25] Ministry of Health 2007. Uganda Health Workforce Study: Satisfaction and Intent to Stay Among Current Health Workers. https://Intrahealth.org/sites/ihweb/files/files/media/uganda-health-workforce-study-satisfaction-and-intent-to-stay-among-current-health-workers/exe.
[26] Politi, B. J., Arena, V. C., Schwerha, J., & Sussman. 2004. Occupational Medical History Taking: How Are Today’s Physicians Doing? A Cross-Sectional Investigation of the Frequency of Occupational History Taking by Physicians in a Major U.S. Teaching Center. Journal of Occupational and Environmental Medicine, 46(6), https://journals.lww.com/joem/Abstract/2004/06000/Occupational_Medical_History_Taking__How_Are.9.aspx.
[27] Dauner, K.N., Loomer, L. A, 2021. qualitative assessment of barriers and facilitators associated with addressing social determinants of health among members of a health collaborative in the rural Midwest. BMC Health Serv Res 21, 867 (2021). https://doi.org/10.1186/s12913-021-06859-6.
[28] WHO (2022). WHO called to return to the Declaration of Alma-Ata. https://www.who.int/teams/social-determinants-of-health/declaration-of-alma-ata.
[29] Eder M., Henninger M., Durbin S. Iacocca M. O. Martin A; Gottlieb, L. M., Lin J. S., 2021.Screening and Interventions for Social Risk Factors: Technical Brief to Support the US Preventive Services Task Force. Journal of The American Medical Association, 326 (4) DOI10.1001/jama.2021.12825.
[30] Joshua R. V., Julia Adler-Milstein, Laura M. G., et al., 2022. The American Journal of Managed Care, January 2022, 8 (1). Assessment of Structured Data
Elements for Social Risk Factors. https://www.ajmc.com/view/assessment-of-structured-data-elements-for-social-risk-factors.[31] ECDC Technical Report, 2018. Social determinants and risk factors in tuberculosis surveillance in the EU/EEA. https://www.ecdc.europa.eu/sites/default/files/documents/Social-determinants-and-risk-factors-for-TB.pdf.
[32] Ruth A. Hackett and Andrew Steptoe, 2017. Type 2 diabetes mellitus and psychological stress — a modifiable risk factor Article in Nature Reviews Endocrinology · June 2017 DOI: 10.1038/nrendo.2017.64). https://www.researchgate.net/publication/318080827_Type_2_diabetes_mellitus_and_psychological_stress_-_a_modifiable_risk_factor.
[33] Soto, C.M., Kleinman, K.P. & Simon, S.R. Quality, and correlates of medical record documentation in the ambulatory care setting. BMC Health Serv Res 2, 22 (2002). https://doi.org/10.1186/1472-6963-2-22. https://bmchealthservres.biomedcentral.com/articles/10.1186/1472-6963-2-22.
[34] Tasew, H., Mariye, T. & Teklay, G.,2019. Nursing documentation practice and associated factors among nurses in public hospitals, Tigray, Ethiopia. BMC Res Notes 12, 612 (2019). https://doi.org/10.1186/s13104-019-4661-xNursing documentation practice and associated factors among nurses in public hospitals, Tigray, Ethi. https://bmcresnotes.biomedcentral.com/articles/10.1186/s13104-019-4661-x.
Viewed PDF 1157 33 -
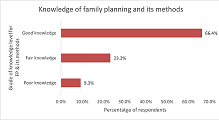 Prevalence and Knowledge of Family Planning among Women of Reproductive Age Group in Primary Healthcare Centers in Abuja, NigeriaAuthor: Orji Ikechukwu ADOI: 10.21522/TIJPH.2013.11.01.Art018
Prevalence and Knowledge of Family Planning among Women of Reproductive Age Group in Primary Healthcare Centers in Abuja, NigeriaAuthor: Orji Ikechukwu ADOI: 10.21522/TIJPH.2013.11.01.Art018Prevalence and Knowledge of Family Planning among Women of Reproductive Age Group in Primary Healthcare Centers in Abuja, Nigeria
Abstract:
The contraceptive prevalence rate (CPR) is a key indicator for measuring improvements in access to reproductive health. In Nigeria, the average CPR remains low at 17%, with wide variability in the knowledge of family planning (FP) methods across the states and communities. Thus, this study set out to 1. Determine the Contraceptive prevalence rate among women of the reproductive age groups (WRAGs) in Primary Healthcare Centers (PHCs) in Abuja. 2. Assess the knowledge of family planning and its methods among WRAGs in PHCs in Abuja. This is a descriptive cross-sectional study conducted among WRAG in two PHCs in Abuja. A simple random method was used to select 400 WRAGs, and the information from participants was captured with a pre-tested structured questionnaire. SPSS version 21.0 was used for data analysis, the hypothesis was tested with chi-square, and the results were significant at p-value < 0.05. The study analyzed 375 valid and complete questionnaires; the mean age was 30 ± 6.29 years, and 90.7% of respondents had at-least secondary school education. The CPR was 36%, and the most common FP methods were male condoms (11.6%), injectable birth control (5.4%), female condoms (4.7%), and implants (4.0%). About 66% of participants had good knowledge of FP methods, and this was associated with increased uptake of contraceptives. The CPR found in this study is considerably higher than the Nigeria national average. The finding aligns with the reported good knowledge of family planning and high literacy level. Furthermore, good knowledge of FP methods was significantly associated with increased contraceptive uptake.
Keywords: Abuja, Contraceptive prevalence, Knowledge of family planning, Primary healthcare centers, Women of reproductive age group.Prevalence and Knowledge of Family Planning among Women of Reproductive Age Group in Primary Healthcare Centers in Abuja, Nigeria
References:
[1] Akgun S, Bakar C. Üreme. sağlığı epidemiyolojisi: Türkiye’de doğurganlık ve aile planlaması. Turkish Journal of Obstetrics and Gynecology. 2006; 3:9-18.
[2] Ahmed S, Li Q, Liu L, Tsui AO. Maternal deaths averted by contraceptive use: An analysis of 172 countries. Lancet. 2012; 380:111-125. DOI: 10.1016/S0140-6736(12)60478-4. PMID: 22784531 A.
[3] Susheela S, Jacqueline D. Adding It Up: Costs and Benefits of Family Planning Services. Guttmacher Institute: New York; 2012.
[4] Moazzam A, Armando S, Asma R, Mario F, Marleen T. A global research agenda for family planning: Results of an exercise for the setting of research priorities. Bulletin of the World Health Organization. 2014; 92:93-98. DOI: 10.2471/BLT.13.122242.
[5] Cleland J, Conde-Agudelo A, Peterson H, Tsui A. Contraception, and health. Lancet. 2012; 380:149-156. DOI: 10.1016/S0140-6736(12)60609-6. PMID: 22784533.
[6] Family Planning 2020. Washington, DC: Family Planning 2020; 2012. Available at: http://www.familyplanning2020.org.
[7] Canning D, Schultz TP. The economic consequences of reproductive health and family planning. Lancet. 2012; 380:165-171. DOI: 10.1016/S0140-6736(12)60827-7. PMID: 22784535.
[8] United Nations, Department of Economic and Social Affairs, and Population Division. 2017b. World population/publications/pdf/family/WFP2017_Highlights.pdf.
[9] UNDESA. World Family Planning. United Nations. 2017;43. Available at: https://www.un.org/en/development/desa/population/publications/pdf/family/WFP2017_Highlights.pdf pmid:28327096.
[10] Paschal Awingura Apanga and Matthew Ayamba Adam Factors influencing the uptake of family planning services in the Talensi District, Ghana. Pan Afr Med J. 2015 Jan 5; 20:10. doi: 10.11604/pamj.2015.20.10.5301. eCollection 2015.
[11] Amadou Barrow. A Survey on Prevalence and Knowledge of Family Planning among Women of Childbearing Age in the Provincial Settings of the Gambia: A Descriptive Cross-Sectional Study. Hindawi Advances in Preventive Medicine. 2020; 2020, Article ID 8862290, 12 pages https://doi.org/10.1155/2020/886229.
[12] Geno Obwoya, Justin & Wulifan, Joseph & Kalolo, Albino. Factors Influencing Contraceptives Use among Women in the Juba City of South Sudan. International Journal of Population Research. 2018. 1-7. 10.1155/2018/6381842.
[13] Cavallaro FL, Benova L, Macleod D, Faye A, Lynch CA. Examining trends in family planning among harder-to-reach women in Senegal 1992-2014. Sci Rep. 2017 Jan 20; 7:41006. doi: 10.1038/srep41006. PMID: 28106100; PMCID: PMC5247687.
[14] National Population Commission. Nigerian Demographic and Health Survey 2018. Available at: https://nationalpopulation.gov.ng/ndhs-2018-key-finding.
[15] Muhammad AP. Family Planning 2020 Commitment. 2017. Available at: http://ec2-54-210-230-186.compute-1.amazonaws.com/wp-content/uploads/2016/10/Govt.-of-Nigeria FP2020-Commitment-2012.pdf.
[16] Ogboghodo EO, Adam VY, Wagbatsoma VA. Prevalence and Determinants of Contraceptive Use among Women of Child-Bearing Age in a Rural Community in Southern Nigeria. Journal of Community Medicine and Primary Health Care. 2017;29 (2).
[17] Akamike IC, Madubueze UC, Okedo-Alex IN, Anyigor CJ, Azuogu BN, Umeokonkwo CD, & Mbachu CO. Perception, pattern of use, partner support and determinants of uptake of family planning methods among women in rural communities in Southeast Nigeria. Contraception and Reproductive Medicine. 2020;5:14. https://doi.org/10.1186/s40834-020-00120-x.
[18] Adeyemi A, Olugbenga-Bello AI, Adeoye O, Salawu M, Aderinoye A, Agbaje MA, et al. Contraceptive prevalence and determinants among women of reproductive age group in Ogbomoso, Oyo State, Nigeria. Open Access Journal of Contraception. 2016;2016(7) pp33-41b. https://doi.org/10.2147/OAJC.S94826.
[19] Alege SG, Matovu JK, Ssensalire S, Nabiwemba E. Knowledge, sources, and use of family planning methods among women aged 15-49 years in Uganda: a cross-sectional study. Pan Afr Med J. 2016 May 10;24:39. doi: 10.11604/pamj.2016.24.39.5836. PMID: 27583102; PMCID: PMC4992376.
[20] Birabwa C, Chemonges D, Tetui M, Baroudi M, Namatovu F, Akuze J. et al. Knowledge and Information Exposure About Family Planning Among Women of Reproductive Age in Informal Settlements of Kira Municipality, Wakiso District, Uganda. Front. Glob. Womens Health, 25 May 2021. https://doi.org/10.3389/fgwh.2021.650538.
[21] Upadhayay A, Shah SK, Thapa DK, T.S. S, Ghimire R, Dahal HR. Knowledge, Attitude and Practice of Family Planning Method Among Married Women of Reproductive Age Group in Earth Quake Displaced Population of Sindupalchok Disrtict, Nepal. American Journal of Public Health Research, 2017;5(1), pp1-5. doi: 10.12691/ajphr-5-1-1.
[22] Lincoln J, Mohammadnezhad M, Khan S. Knowledge, Attitudes, and Practices of Family Planning Among Women of Reproductive Age in Suva, Fiji in 2017. J Women’s Health Care. 2018; 7: 431. doi:10.4172/2167-0420.1000431.
[23] Azuogu B, Akamike I, Okedo-Alex I, Adeke A, Agu A, Akpa C. et al. Knowledge, Attitude and Perceived Partner and Socio-cultural Support for Family Planning among Women of Reproductive Age in a Rural Community in Ebonyi State, Nigeria. Journal of Epidemiological Society of Nigeria. 2020;3(2), 17 - 28. https://doi.org/10.46912/jeson.28.
[24] Anate BC, Balogun MR, Olubodun T, Adejimi AA. Knowledge and utilization of family planning among rural postpartum women in Southwest Nigeria. J Family Med Prim Care. 2021; 10:730-7.
[25] Akinwale DO, Okafor AN, Akinbade OM, Ojo CI. Determinants of Modern Contraceptives Utilization among Women of Reproductive Age in Rural Community, Osun State, Nigeria. International Journal of Caring Sciences. May-August 2020;13(2) Page 1173.
[26] Oluwole EO, Kuyinu YA, Goodman OO, Odugbemi BA, Akinyinka MR. Factors Influencing the Uptake of Modern Family Planning Methods among Women of Reproductive Age in A Rural Community in Lagos State. International Journal of Tropical Disease & Health. 2015;11(3). pp1-11. https://doi.org/10.9734/IJTDH/2016/20373.
[27] Okech TC, Wawire NW, Mburu TK. Contraceptive use among women of reproductive age in Kenya’s city slums. Int J Bus Soc Sci. 2011;2:22–43.
[28] World Health Organization. Unsafe Abortion: Global and Regional Estimates of the Incidence of Unsafe Abortion and Associated Mortality in 2004. WHO, Geneva: 2004.
[29] Akani C, Enyindah C, Babatunde S. Emergency contraception: knowledge and perception of female undergraduates in the Niger Delta of Nigeria. Ghana Med J. 2008;42:68–70.
[30] UN World Population Prospects (2019 Revision) - United Nations population estimates and projections; 2021 World Population Review Nigeria Population. 2021. Available at: https://worldpopulationreview.com/countries/nigeria-population.
[31] Fadeyibi O, Alade M, Adebayo S, Erinfolami T, Mustapha F, Yaradua S. Household Structure and Contraceptive Use in Nigeria. Front Glob Womens Health. 2022;3:821178. doi:10.3389/fgwh.2022.821178.
[32] United Nations. World Contraceptive Use 2022. Available at: https://www.un.org/development/desa/pd/data/world-contraceptive-use.
[33] Afolabi BM, Ezedinachi ENU, Arikpo I, Ogunwale A, Ganiyu DF, Abu RA, et al. Knowledge, non‑use, use and source of information on contraceptive methods among women in various stages of reproductive age in rural Lagos, Southwest Nigeria. Open Access J Contracept. 2015;6:65–75.
[34] Osaro BO, Tobin‑West CI, Mezie‑Okoye MM. Knowledge of modern contraceptives and their use among rural women of childbearing age in Rivers State Nigeria. Ann Trop Med Public Health. 2017;10:1043‑8.
[35] Durowade KA, Omokanye LO, Elegbede OE, Adetokunbo S, Olomofe CO, Ajiboye AD, et al. Barriers to contraceptive uptake among women of reproductive age in a semi‑urban community of Ekiti State, Southwest Nigeria. Ethiop J Health Sci. 2017;27:121‑8.
[36] Usman S, Olabisi K, Ibiwumi I, Oluwole O, Adewale O, Ayooluwa A. Family planning practices among rural community women in Nigeria. Journal of Experimental and Integrative Medicine. 2016;6. 88. 10.5455/jeim.120716.or.155.
[37] Aninyei L, Onyesom I, Ukuhor H, Uzuegbu UE, Ofili M, Anyanwu EB. Knowledge attitude to modern family planning methods in Abraka communities, Delta State, Nigeria. East African journal of public health. 2008;5. 10-2. 10.4314/eajph.v5i1.38970.
[38] Akamike IC, Okedo-Alex IN, Madubueze UC, Umeokonkwo CD. Does community mobilisation improve awareness, approval, and uptake of family planning methods among women of reproductive age in Ebonyi State? Experience from a quasi-experimental study. Pan African Medical Journal. 2019; 33:17. doi:10.11604/pamj.2019.33.17.17401.
[39] National Population Commission ICF. Nigeria Demographic and Health Survey. (2018). Abuja: Nigeria and Rockville, Maryland.
Viewed PDF 976 35 -
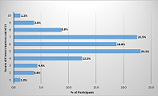 Assessment of Knowledge and Attitude towards Coronavirus Disease 2019 Vaccines among Students in Zambia - A Case Study of the University of ZambiaAuthor: Richard HaakondeDOI: 10.21522/TIJPH.2013.11.01.Art019
Assessment of Knowledge and Attitude towards Coronavirus Disease 2019 Vaccines among Students in Zambia - A Case Study of the University of ZambiaAuthor: Richard HaakondeDOI: 10.21522/TIJPH.2013.11.01.Art019Assessment of Knowledge and Attitude towards Coronavirus Disease 2019 Vaccines among Students in Zambia - A Case Study of the University of Zambia
Abstract:
Equitable access to safe and efficacious vaccines is essential to the fight against Covid-19. Low vaccine acceptance poses a challenge to controlling the Covid-19 pandemic. Young people are key in the fight against Covid-19, as they are a majority in most African populations. A cross-sectional study was used to assess the knowledge and attitude toward Covid-19 vaccines among university students in Zambia. This study comprised a total of 160 respondents with an average age of 21.0 + 3.6 years, ranging from 18 to 46 years. The study was done between January and February 2022. Random sampling was used for participant enrollment, and an interviewer-administered questionnaire was used for data collection. Spearman’s Rank Correlation test and Binary Logistic Regression were performed to establish relationships among the study variables. The study revealed a knowledge score of 61.3%, and a Covid-19 vaccine acceptance score of 28.0%. Knowledge was also found to be associated with Covid-19 vaccine acceptance (p<0.05). Covid-19 vaccine acceptance showed an association with history of having a relative or close friend who had Covid-19 infection (OR=2.041, C.I. 95%, 1.010-4.127; p<0.05), as well as knowledge (OR=1.275, C.I. 95%, 1.045-1.556; p<0.05). The results showed good knowledge of Covid-19 vaccines among students. The attitude was however found to be negative, as indicated by a vaccine acceptance score of 28.0%. Evidence-based health education on the importance of Covid-19 vaccination is needed to counter myths and conspiracy beliefs about the disease to improve vaccine uptake.
Keywords: Vaccines; Covid-19; Acceptance; Attitude; Knowledge; Zambia.Assessment of Knowledge and Attitude towards Coronavirus Disease 2019 Vaccines among Students in Zambia - A Case Study of the University of Zambia
References:
[1] Zhu, N., Zhang, D., Wang, W., Li, X., Yang, B., Song, J., & Tan, W. (2020). A novel coronavirus from patients with pneumonia in China, 2019. New England Journal of Medicine. https://www.nejm.org/doi/full/10.1056/nejmoa2001017.
[2] Cucinotta, D., Vanelli, M. (2020). WHO Declares Covid-19 a Pandemic. Acta Biomed. Mar 19;91(1):157-160. doi: 10.23750/abm. v91i1.9397. PMID: 32191675; PMCID: PMC7569573. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6357666/.
[3] World Health Organization. (2022, August 18a). Coronavirus Disease (Covid-19) Dashboard. Retrieved from https://covid19.who.int/table.
[4] Africa Centre for Disease Control and Prevention. (2021, August 17a). Coronavirus Disease (Covid-19) Dashboard. Retrieved from http://africacdc.org/covid-19.
[5] Mwai, P. (2021, October 1). Covid-19 vaccinations: More than 50 nations have missed a target set by the WHO. BBC Reality Check. Retrieved from https://www.bbc.com/news/56100076.
[6] Elhadi, M., Alsoufi, A., Alhadi, A., Hmeida, A., Alshareea, E., Dokali, M., ... & Msherghi, A. (2021). Knowledge, attitude, and acceptance of healthcare workers and the public regarding the Covid-19 vaccine: a cross-sectional study. BMC Public Health, 21(1), 1-21. https://link.springer.com/article/10.1186/s12889-021-10987-3.
[7] World Health Organization (2021, April 16c). WHO Africa /Zambia Launches the Covid–19 Vaccination. Retrieved from https://www.afro.who.int/news/zambia-launches-covid-19-vaccination.
[8] Barello, S., Nania, T., Dellafiore, F., Graffigna, G., & Caruso, R. (2020). ‘Vaccine hesitancy among university students in Italy during the Covid-19 pandemic. European Journal of Epidemiology, 35(8), 781-783. https://link.springer.com/article/10.1007/s10654-020-00670-z.
[9] Pourhoseingholi, M. A., Vahedi, M., & Rahimzadeh, M. (2013). Sample size calculation in medical studies. Gastroenterology and hepatology from bed to the bench, 6(1), 14–17. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4017493/.
[10] Mulenga, L. B., Hines, J. Z., Fwoloshi, S., Chirwa, L., Siwingwa, M., Yingst, S., ... & Malama, K. (2021). Prevalence of SARS-CoV-2 in six districts in Zambia in July 2020: a cross-sectional cluster sample survey. The Lancet Global Health, 9(6), e773-e781. https://www.sciencedirect.com/science/article/pii/S2214109X2100053X.
[11] The University of Zambia Official Website. (2021) Retrieved from https://www.unza.zm.
[12] Ab Hamid, M. R., Sami, W., & Sidek, M. M. (2017, September). Discriminant validity assessment: Use of Fornell & Larcker criterion versus HTMT criterion. In Journal of Physics: Conference Series (Vol. 890, No. 1, p. 012163). IOP Publishing. https://iopscience.iop.org/article/10.1088/1742-6596/890/1/012163/pdf.
[13] Sallam, M., Dababseh, D., Eid, H., Hasan, H., Taim, D., Al-Mahzoum, K., Al-Haidar, A., Yaseen, A., Ababneh, N. A., Assaf, A., Bakri, F. G., Matar, S., & Mahafzah, A. (2021). Low Covid-19 Vaccine Acceptance Is Correlated with Conspiracy Beliefs among University Students in Jordan. International journal of environmental research and public health, 18(5), 2407. https://www.mdpi.com/1660-4601/18/5/2407/pdf.
[14] Islam, M. S., Siddique, A. B., Akter, R., Tasnim, R., Sujan, M. S. H., Ward, P. R., & Sikder, M. T. (2021). Knowledge, attitudes, and perceptions towards Covid-19 vaccinations: a cross-sectional community survey in Bangladesh. medRxiv. https://link.springer.com/article/10.1186/s12889-021-11880-9.
[15] Gallè, F., Sabella, E. A., Roma, P., De Giglio, O., Caggiano, G., Tafuri, S., ... & Napoli, C. (2021). Knowledge and Acceptance of Covid-19 Vaccination among Undergraduate Students from Central and Southern Italy. Vaccines, 9(6), 638. https://www.mdpi.com/2076-393X/9/6/638/pdf?version=1623327543.
[16] Sallam, M. (2021). Covid-19 vaccine hesitancy worldwide: a concise, systematic review of vaccine acceptance rates. Vaccines, 9(2), 160. https://www.mdpi.com/2076-393X/9/2/160/pdf.
[17] Bai, W., Cai, H., Liu, S., Liu, H., Qi, H., Chen, X., & Xiang, Y. T. (2021). Attitudes toward Covid-19 vaccines in Chinese college students. International Journal of Biological Sciences, 17(6), 1469. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8071773/.
[18] Abebe, H., Shitu, S., & Mose, A. (2021). Understanding Covid-19 Vaccine Knowledge, Attitude, Acceptance, and Determinates of Covid-19 Vaccine Acceptance Among Adult Population in Ethiopia. Infection and Drug Resistance, 14, 2015. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8179743/.
Viewed PDF 1037 30 -
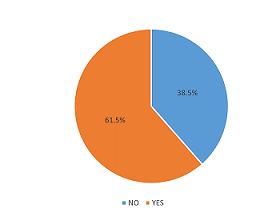 Effect of Access to Immunization Information on Vaccine Acceptance amongst Parents/Caregivers Visiting Health Facilities in Wushishi Local Government Area, Niger StateAuthor: Otojareri KADOI: 10.21522/TIJPH.2013.11.01.Art020
Effect of Access to Immunization Information on Vaccine Acceptance amongst Parents/Caregivers Visiting Health Facilities in Wushishi Local Government Area, Niger StateAuthor: Otojareri KADOI: 10.21522/TIJPH.2013.11.01.Art020Effect of Access to Immunization Information on Vaccine Acceptance amongst Parents/Caregivers Visiting Health Facilities in Wushishi Local Government Area, Niger State
Abstract:
Globally, vaccines are the most cost-effective medical intervention to prevent death and disease. The objectives of this study were to assess the effect of access to immunization information on vaccine acceptance amongst parents/caregivers visiting the major health facilities within Wushishi Local Government Area, Niger State. A semi-structured interviewer-administered questionnaire was used for this study. The result of the study showed a mean age of respondents was 26.88 years. 96.5% of the respondents were females, 45.5% had no formal education, 30.7% were unemployed, and 35.5% were of Hausa ethnicity. 65.1% of respondents obtain information on routine immunization within 12 months before the study. 54.5% had satisfactory knowledge of immunization, while 71.5% exhibited a favorable attitude toward immunization. The major source of information was health workers. Those who had access to information were more likely to have good knowledge of immunization (X62=127.246, DF=1, p=0.001) and a more favorable attitude towards immunization (X62=14.155, DF=1, p=0.001). This study has demonstrated that access to information on immunization greatly affects the knowledge and, consequently, the attitude of parents toward making a positive decision to accept vaccination. Efforts should be made to understand the content and effect of information sources on knowledge and attitudes toward vaccination by relevant stakeholders involved in the implementation of immunization programs.
Keywords: Access to immunization, Access to immunization information, Vaccine acceptance.Effect of Access to Immunization Information on Vaccine Acceptance amongst Parents/Caregivers Visiting Health Facilities in Wushishi Local Government Area, Niger State
References:
[1] Njidda, U. M. (2017). Assessment of Parents Knowledge towards the Benefits of Child Immunization in Maiduguri, Borno State, Nigeria. Nursing & Care Open Access Journal, 3(2). https://doi.org/10.15406/ncoaj.2017.03.00067.
[2] Feemster, K. A. (2020). Building vaccine acceptance through communication and advocacy. Human Vaccines and Immunotherapeutics, 16(5), 1004–1006. https://doi.org/10.1080/21645515 .2020.1746603.
[3] Handy, L. K., Maroudi, S., Powell, M., Nfila, B., Moser, C., Japa, I., Monyatsi, N., Tzortzi, E., Kouzeli, I., Luberti, A., Theodoridou, M., Offit, P., Steenhoff, A., Shea, J. A., & Feemster, K. A. (2017). The impact of access to immunization information on vaccine acceptance in three countries. PLoS ONE, 12(8), 1–16. https://doi.org/10.1371/journal.pone.0180759.
[4] Adebisi, Y. A., Alaran, A. J., Bolarinwa, O. A., Akande-Sholabi, W., & Lucero-Prisno, D. E. (2021). When it is available, will we take it? Social media users’ perception of hypothetical covid-19 vaccine in nigeria. Pan African Medical Journal, 38. https://doi.org/10.11604/pamj. 2021.38.230.27325.
[5] Zhao, Q., Sun, X., Xie, F., Chen, B., Wang, L., Hu, L., & Dai, Q. (2021). Impact of COVID-19 on psychological wellbeing. International Journal of Clinical and Health Psychology, 21(3), 4–9. https://doi.org/10.1016/j.ijchp.2021.100252.
[6] Torre, G. La, Scalingi, S., Garruto, V., Siclari, M., Chiarini, M., & Mannocci, A. (2017). Knowledge , Attitude, and Behaviours towards Recommended Vaccinations among Healthcare Workers. 6–8. https://doi.org/10.3390/healthcare5010013.
[7] Adeyanju, G. C., Sprengholz, P., Betsch, C., & Essoh, T. A. (2021). Caregivers’ willingness to vaccinate their children against childhood diseases and human papillomavirus: A cross-sectional study on vaccine hesitancy in Malawi. Vaccines, 9(11). https://doi.org/10.3390/vaccines9111231.
[8] Hmr, A., Glenton, C., & Lewin, S. (2017). qualitative evidence ( Review ). https://doi.org/10.1002/14651858.CD011787.pub2.www.cochranelibrary.com.
[9] Sondagar, C., Xu, R., MacDonald, N. E., & Dubé, E. (2020). Vaccine acceptance: How to build and maintain trust in immunization. Canada Communicable Disease Report, 46(5), 155–159. https://doi.org/10.14745/ccdr.v46i05a09.
[10] Obasohan, P. E., Mustapha, M. A., Makada, A., & Obasohan, D. N. (2018). Evaluating the reasons for partial and non-immunization of children in Wushishi local government area, Niger state, Nigeria: Methodological comparison. African Journal of Reproductive Health, 22(4), 113–122. https://doi.org/10.29063/ajrh2018/v22i4.12.
[11] Hogue, M. D., & Meador, A. E. (2016). Vaccines and Immunization Practice. Nursing Clinics of North America, 51(1), 121–136. https://doi.org/10.1016/j.cnur.2015.10.005.
[12] Durán-Méndez, A., Jardínez-Vera, A. C., Jiménez-Muñoz, E., & Peón, A. N. (2021). A brief history of vaccines and an overview of their benefits. Revista de La Sociedad Española de Beneficencia, 2(1), 1–6. https://doi.org/10.46295/2:1.vachi
[13] Filia, A., Bella, A., Ancona, F. D., Fabiani, M., Giambi, C., Rizzo, C., Ferrara, L., Pascucci, M. G., & Rota, M. C. (2019). Childhood vaccinations : knowledge , attitudes and practices of paediatricians and factors associated with their confidence in addressing parental concerns , Italy , 2016. Eurosurveillance, 24(6). https://doi.org/10.2807/1560-7917.ES.2019.24.6.1800275.
[14] Taiwo, L., Idris, S., Abubakar, A., Nguku, P., Nsubuga, P., Gidado, S., Okeke, L., Emiasegen, S., & Waziri, E. (2017). Factors affecting access to information on routine immunization among mothers of under 5 children in Kaduna state Nigeria, 2015. Pan African Medical Journal, 27, 1–8. https://doi.org/10.11604/pamj.2017.27.186.11191.
[15] Lewandowska, A., Lewandowski, T., Rudzki, G., & Rudzki, S. (n.d.). Opinions and Knowledge of Parents Regarding Preventive Vaccinations of Children and Causes of Reluctance toward Preventive Vaccinations.
[16] Larson Williams, A., Mitrovich, R., Mwananyanda, L., & Gill, C. (2019). Maternal vaccine knowledge in low- and middle-income countries—and why it matters. Human Vaccines and Immunotherapeutics, 15(2), 283–286. https://doi.org/10.1080/21645515.2018.1526589.
[17] Jones, A. M., Omer, S. B., Bednarczyk, R. A., Halsey, N. A., Moulton, L. H., & Salmon, D. A. (2012). Parents’ Source of Vaccine Information and Impact on Vaccine Attitudes, Beliefs, and Nonmedical Exemptions. Advances in Preventive Medicine, 2012 (February 2004), 1–8. https://doi.org/10.1155/2012/932741.
[18] Adedokun, S. T., Uthman, O. A., Adekanmbi, V. T., & Wiysonge, C. S. (2017). Incomplete childhood immunization in Nigeria: A multilevel analysis of individual and contextual factors. BMC Public Health, 17(1), 1–10. https://doi.org/10.1186/s12889-017-4137-7.
[19] GebreEyesus, F., Amlak, T., Tarekegn, T., Shiferaw, B., Mewahegn, M., Emeria, O., Agerie, A., & Chanie, D. (2021). Knowledge , Attitude , and Practices of Parents About Immunization of Infants and Its Associated. Dovepress, 12(223), 223–238. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8121275/pdf/phmt-12-223.pdf
[20] Sallam, M. (2021). Worldwide Vaccine Hesitancy. Vaccines, 1–14. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7920465/.
Viewed PDF 1042 43 -
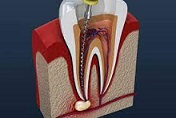 Application of Stem Cells in EndodonticsAuthor: Satish VishwanathaiahDOI: 10.21522/TIJPH.2013.11.01.Art021
Application of Stem Cells in EndodonticsAuthor: Satish VishwanathaiahDOI: 10.21522/TIJPH.2013.11.01.Art021Application of Stem Cells in Endodontics
Abstract:
The discovery of stem cells in dental pulp has expanded our understanding concerning the various mechanisms that play a substantial role in the maintenance of dental pulp homeostasis to improve health and also regarding the pulp response to injury. Stems cells play a pivotal role in the physiology of the dental pulp tissue throughout the entire lifespan of the tooth. The ideology that these cells are intimately associated with regulating pulp angiogenesis as a response to cariogenic challenges is also inferred. In recent times, we are witnessing an increasing number of passionate individuals showing enthusiasm in the field of regenerative endodontics as stem cells exhibit potential benefits in dental pulp tissue engineering. The article here focuses predominantly on stem cells—the dental stem cells and non-dental stem cells which play an active part in benefitting pulpal necrosis tooth, the cardinal objective of these cells in the field of endodontic therapy, and the current, as well as the future role, stem cells could play in the clinical practice of endodontics eventually.
Keywords: Dental stem cells, Pulpal necrosis, Stem cells, Regenerative.Application of Stem Cells in Endodontics
References:
[1] Fischbach, G. D., Fischbach, R., L., 2004, Stem cells: science, policy, and ethics. The Journal of clinical investigation, 114(10):1364-1370.
[2] Ashri, N. Y., Ajlan, S. A., & Aldahmash, A. M., 2015, Dental pulp stem cells. Biology and use for periodontal tissue engineering. Saudi medical journal, 36(12), 1391–1399.
[3] Almeida, P. N., Cunha, K. S., 2016, Dental stem cells and their application in Dentistry: a literature review. Revista Brasileira de Odontologia, 73(4):331.
[4] Rao M. S., 2004, Stem sense: a proposal for the classification of stem cells. Stem cells and development, 13(5), 452–455.
[5] Rai, S., Kaur, M., & Kaur, S., 2013, Applications of stem cells in interdisciplinary dentistry and beyond: an overview. Annals of medical and health sciences research, 3(2), 245–254.
[6] Lin, L. M., & Kahler, B., 2017, A review of regenerative endodontics: current protocols and future directions. Journal of Istanbul University Faculty of Dentistry, 51(3 Suppl 1), S41–S51.
[7] De Ugarte, D. A., Morizono, K., Elbarbary, A., Alfonso, Z., Zuk, P. A., Zhu, M., Dragoo, J. L., Ashjian, P., Thomas, B., Benhaim, P., Chen, I., Fraser, J., & Hedrick, M. H., 2003, Comparison of multi-lineage cells from human adipose tissue and bone marrow. Cells, tissues, organs, 174(3), 101–109.
[8] Takahashi, K., & Yamanaka, S., 2006, Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell, 126(4), 663–676.
[9] Caplan A. I., 1991, Mesenchymal stem cells. Journal of Orthopaedic Research: official publication of the Orthopaedic Research Society, 9(5), 641–650.
[10] Bluteau, G., Luder, H. U., De Bari, C., & Mitsiadis, T. A., 2008, Stem cells for tooth engineering. European cells & materials, 16, 1–9.
[11] Mitsiadis, T. A., Orsini, G., & Jimenez-Rojo, L., 2015, Stem cell-based approaches in dentistry. European cells & materials, 30, 248–257.
[12] Huang, Y. H., Yang, J. C., Wang, C. W., Lee, S. Y., 2010, Dental stem cells and tooth banking for regenerative medicine. J ExpClin Med, 2(3):111-117.
[13] Ravindran, S., Huang, C. C., & George, A., 2014. Extracellular matrix of dental pulp stem cells: applications in pulp tissue engineering using somatic MSCs. Frontiers in physiology, 4, 395.
[14] Alongi, D. J., Yamaza, T., Song, Y., Fouad, A. F., Romberg, E. E., Shi, S., Tuan, R. S., & Huang, G. T., 2010, Stem/progenitor cells from inflamed human dental pulp retain tissue regeneration potential. Regenerative medicine, 5(4), 617–631.
[15] Xiong, J., Gronthos, S., & Bartold, P. M., 2013, Role of the epithelial cell rests of Malassez in the development, maintenance, and regeneration of periodontal ligament tissues. Periodontology 2000, 63(1), 217–233.
[16] Cai, J., Zhang, Y., Liu, P., Chen, S., Wu, X., Sun, Y., Li, A., Huang, K., Luo, R., Wang, L., Liu, Y., Zhou, T., Wei, S., Pan, G., & Pei, D., 2013, Generation of tooth-like structures from integration-free human urine induced pluripotent stem cells. Cell regeneration (London, England), 2(1), 6.
[17] Laird, D. J., De Tomaso, A. W., & Weissman, I. L.,2005, Stem cells are units of natural selection in a colonial ascidian. Cell, 123(7), 1351–1360.
[18] Chrepa, V., Henry, M. A., Daniel, B. J., & Diogenes, A., 2015, Delivery of Apical Mesenchymal Stem Cells into Root Canals of Mature Teeth. Journal of dental research, 94(12), 1653–1659.
[19] Huang, G. T., Yamaza, T., Shea, L. D., Djouad, F., Kuhn, N. Z., Tuan, R. S., & Shi, S., 2010, Stem/progenitor cell-mediated de novo regeneration of dental pulp with newly deposited continuous layer of dentin in an in vivo model. Tissue engineering. Part A, 16(2), 605–615.
[20] Zhang, X., Li, H., Sun, J., Luo, X., Yang, H., Xie, L., Yang, B., Guo, W., & Tian, W., 2017, Cell-derived micro-environment helps dental pulp stem cells promote dental pulp regeneration. Cell proliferation, 50(5), e12361.
[21] Sanz, J. L., Guerrero-Gironés, J., Pecci-Lloret, M. P., Pecci-Lloret, M. R., & Melo, M., 2021, Biological interactions between calcium silicate-based endodontic biomaterials and periodontal ligament stem cells: A systematic review of in vitro studies. International Endodontic Journal, 54(11), 2025–2043.
[22] Srisuwan, T., Tilkorn, D. J., Al-Benna, S., Abberton, K., Messer, H. H., & Thompson, E. W., 2013, Revascularization and tissue regeneration of an empty root canal space is enhanced by a direct blood supply and stem cells. Dental traumatology: official publication of International Association for Dental Traumatology, 29(2), 84–91.
[23] Friedlander, L. T., Cullinan, M. P., & Love, R. M., 2009, Dental stem cells and their potential role in apexogenesis and apexification. International Endodontic Journal, 42(11), 955–962.
[24] Kottoor., J, 2013, Biomimetic endodontics: barriers and strategies. Health Sciences, 2(1):JS007.
[25] Ding, R. Y., Cheung, G. S., Chen, J., Yin, X. Z., Wang, Q. Q., & Zhang, C. F., 2009, Pulp revascularization of immature teeth with apical periodontitis: a clinical study. Journal of endodontics, 35(5), 745–749.
[26] Gandhi, A., Gandhi, T., 2011, Madan N. Dental pulp stem cells in endodontic research: a promising tool for tooth tissue engineering. RSBO. 8(3):335-40.
[27] Harikumar., Kavitha, A., Jayaprada, J., Shetty, S.R.,2010, Regenerative Endodontics. Ind J Dent Adv, 2(2):203-209.
[28] Shi, S., Bartold, P. M., Miura, M., Seo, B. M., Robey, P. G., & Gronthos, S., 2005, The efficacy of mesenchymal stem cells to regenerate and repair dental structures. Orthodontics & craniofacial research, 8(3), 191–199.
[29] Arora, V., Arora, P., & Munshi, A. K., 2009, Banking stem cells from human exfoliated deciduous teeth (SHED): saving for the future. The Journal of clinical pediatric dentistry, 33(4), 289–294.
[30] Goldstein, G., Slizys, I. S., & Chase, M. W., 1961, Studies on fluorescent antibody staining. I. Non-specific fluorescence with fluorescein-coupled sheep anti-rabbit globulins. The Journal of experimental medicine, 114(1), 89–110.
[31] Baranwal, K., A, 2015, Regenerative Stem Cells for Endodontic Tissue Engineering: Past, Present and Future. Ann ProsthodontRestor Dent, 1(1):20-5.
Viewed PDF 893 35 -
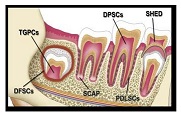 Application of Stem Cells in Pediatric DentistryAuthor: Prabhadevi C MaganurDOI: 10.21522/TIJPH.2013.11.01.Art022
Application of Stem Cells in Pediatric DentistryAuthor: Prabhadevi C MaganurDOI: 10.21522/TIJPH.2013.11.01.Art022Application of Stem Cells in Pediatric Dentistry
Abstract:
A stem cell is a master of all cells in the body, which can divide and regrow with regeneration and vascularization. The deciduous teeth, which are not infected and vital with pulp stem cells, help in the formation of adult stem cells. The extracted stem cells from human exfoliated deciduous teeth (SHED) and immature dental pulp stem cells can be harvested as stem cells that form dental tissue regeneration SHED, osteogenic potential 40%, and neurogenic potential either by in vivo or in vitro method. The article here focuses mainly on the stem cell classification of dental stem cells, their characterization, therapeutic application, application in the deciduous tooth procedure, banking of SHED, and recent innovative methods for banking SHED. This review was done to highlight the integral role of pedodontists in educating patients about stem cell banking services and must become a part of such services.
Keywords: Human exfoliated deciduous teeth, Immature dental pulp stem cells, Pedodontist, Pediatric dentistry, Stem cells.Application of Stem Cells in Pediatric Dentistry
References:
[1] Stem Cells: Past, Present, and the Future https://stemcellres.biomedcentral.com/articles/10.1186/s13287-019-1165-5.
[2] Stem Cells: https://medlineplus.gov/stemcells.html.
[3] Miura, M., Gronthos, S., Zhao, M., Lu, B., Fisher, L. W., Robey, P. G., & Shi, S., 2003, SHED: stem cells from human exfoliated deciduous teeth. Proceedings of the National Academy of Sciences of the United States of America, 100(10), 5807–5812.
[4] Kerkis, I., Kerkis, A., Dozortsev, D., Stukart-Parsons, G. C., Gomes Massironi, S. M., Pereira, L. V., Caplan, A. I., & Cerruti, H. F., 2006, Isolation and characterization of a population of immature dental pulp stem cells expressing OCT-4 and other embryonic stem cell markers. Cells, tissues, organs, 184(3-4), 105–116.
[5] Popuri S. K., 2018, Concerns of a Pediatric Dentist in Dental Stem Cells: An Overview. The Open Dentistry Journal, 12, 596–604.
[6] Kerkis, I., & Caplan, A. I., 2012, Stem cells in dental pulp of deciduous teeth. Tissue Engineering. Part B, Reviews, 18(2), 129–138.
[7] Saber S. E., 2009, Tissue engineering in endodontics. Journal of Oral Science, 51(4), 495–507.
[8] Cordeiro, M. M., Dong, Z., Kaneko, T., Zhang, Z., Miyazawa, M., Shi, S., Smith, A. J., & Nör, J. E., 2008, Dental pulp tissue engineering with stem cells from exfoliated deciduous teeth. Journal of Endodontics, 34(8), 962–969.
[9] Bansal, R., & Jain, A., 2015, Current overview on dental stem cells applications in regenerative dentistry. Journal of Natural Science, biology, and medicine, 6(1), 29–34.
[10] de Mendonça Costa, A., Bueno, D. F., Martins, M. T., Kerkis, I., Kerkis, A., Fanganiello, R. D., Cerruti, H., Alonso, N., & Passos-Bueno, M. R., 2008, Reconstruction of large cranial defects in nonimmunosuppressed experimental design with human dental pulp stem cells. The Journal of Craniofacial Surgery, 19(1), 204–210.
[11] Papaccio, G., Graziano, A., d’Aquino, R., Graziano, M. F., Pirozzi, G., Menditti, D., De Rosa, A., Carinci, F., & Laino, G., 2006, Long-term cryopreservation of dental pulp stem cells (SBP-DPSCs) and their differentiated osteoblasts: a cell source for tissue repair. Journal of Cellular Physiology, 208(2), 319–325.
[12] Rosa, V., Dubey, N., Islam, I., Min, K. S., & Nör, J. E., 2016, Pluripotency of Stem Cells from Human Exfoliated Deciduous Teeth for Tissue Engineering. Stem Cells International, 2016, 5957806.
[13] Arora, V., Arora, P., & Munshi, A. K., 2009, Banking stem cells from human exfoliated deciduous teeth (SHED): saving for the future. The Journal of Clinical Pediatric Dentistry, 33(4), 289–294.
[14] Telles, P. D., Machado, M. A., Sakai, V. T., & Nör, J. E., 2011, Pulp tissue from primary teeth: new source of stem cells. Journal of Applied Oral Science: Revista FOB, 19(3), 189–194.
[15] Friedlander, L. T., Cullinan, M. P., & Love, R. M., 2009, Dental stem cells and their potential role in apexogenesis and apexification. International Endodontic Journal, 42(11), 955–962.
[16] Caruso, S., Sgolastra, F., & Gatto, R., 2014, Dental pulp regeneration in paediatric dentistry: the role of stem cells. European Journal of Paediatric Dentistry, 15(2), 90–94.
[17] Chrepa, V., Pitcher, B., Henry, M. A., & Diogenes, A., 2017, Survival of the Apical Papilla and Its Resident Stem Cells in a Case of Advanced Pulpal Necrosis and Apical Periodontitis. Journal of Endodontics, 43(4), 561–567.
[18] Tsai, A. I., Hong, H. H., Lin, W. R., Fu, J. F., Chang, C. C., Wang, I. K., Huang, W. H., Weng, C. H., Hsu, C. W., & Yen, T. H., 2017, Isolation of Mesenchymal Stem Cells from Human Deciduous Teeth Pulp. BioMed Research International, 2017, 2851906.
[19] Yin, Z., Wang, Q., Li, Y., Wei, H., Shi, J., & Li, A., 2016, A novel method for banking stem cells from human exfoliated deciduous teeth: lentiviral TERT immortalization and phenotypical analysis. Stem Cell Research & Therapy, 7, 50.
[20] Narang, S., & Sehgal, N., 2012, Stem cells: A potential regenerative future in dentistry. Indian Journal of Human Genetics, 18(2), 150–154.
Viewed PDF 931 43 -
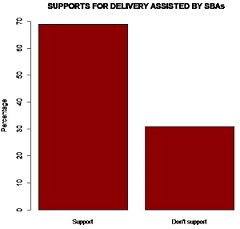 The Role of Organized Public Forums in Improving Uptake of Skilled Birth Attendants among Women of Reproductive Age in Kilifi County, KenyaAuthor: Johnson S ManyiwaDOI: 10.21522/TIJPH.2013.11.01.Art023
The Role of Organized Public Forums in Improving Uptake of Skilled Birth Attendants among Women of Reproductive Age in Kilifi County, KenyaAuthor: Johnson S ManyiwaDOI: 10.21522/TIJPH.2013.11.01.Art023The Role of Organized Public Forums in Improving Uptake of Skilled Birth Attendants among Women of Reproductive Age in Kilifi County, Kenya
Abstract:
The skilled and competent attendant is vital in curbing maternal and infant mortality. Promoting the utilization of maternal health services supervised by skilled health professionals greatly aids in bridging the gap in accessing maternal health services such as immunization and postnatal care services. This lack of skilled attendance is one of the major factors responsible for the rising maternal and infant mortality. Thus, there’s still needed to encourage these women to seek out the services of skilled health professionals during childbirth. This study is aimed at investigating the use of an organized public forums approach in influencing the uptake of skilled birth attendants (SBAs) among women of reproductive age in the Kanamai Area, Kilifi County. The study was conducted at Kanamai Area, Kilifi County. A cross-sectional survey was carried out using semi-structured questionnaires as tools of data collection. Simple random sampling was used to recruit the study participants. All analyses were done using R for Windows (version 4.0.3). Both descriptive and inferential analyses were done. Descriptive statistics were used to generate frequency and percentages, while chi-square was used to draw inferences. Association was considered significant if 𝑃 < 0.05. Some of the notable significant factors gathered through our public forum engagement influencing support for delivery assisted by skilled birth attendants (SBAs) were education level, occupation, and parity. There’s a need for the concerned agencies to embrace the use of public forums and other relevant approaches so as to sought out and promote the rate of health services utilization.
Keywords: SBAs, Childbirth, Utilization, Health Facilities, Public Forum.The Role of Organized Public Forums in Improving Uptake of Skilled Birth Attendants among Women of Reproductive Age in Kilifi County, Kenya
References:
[1] World Health Organization. 2019. Trends in maternal mortality 2000 to 2017: estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division: executive summary. World Health Organization. https://apps.who.int/iris/handle/10665/327596.
[2] World Health Organization, International Confederation of Midwives & Fédération internationale de Gynécologie et d’Obstétrique. 2004. Making pregnancy safer: the critical role of the skilled attendant: a joint statement by WHO, ICM and FIGO. World Health Organization. https://apps.who.int/iris/handle/10665/42955.
[3] Bongaarts, J., WHO., UNICEF., & UNFPA., 2016, World Bank Group, & United Nations population division trends in maternal mortality: 1990 to 2015 Geneva: World Health Organization, 2015. Popul Dev Rev.;42(4):726.
[4] Crowe, S., Utley, M., Costello, A., & Pagel, C., 2012, How many births in sub-Saharan Africa and South Asia will not be attended by a skilled birth attendant between 2011 and 2015? BMC Pregnancy Childbirth 12(4). https://doi.org/10.1186/1471-2393-12-4.
[5] Ross, JA., & Blanc, AK., 2012. Why aren’t there more maternal deaths? A decomposition analysis. Maternal and Child Health Journal, 16(2), 456–463. https://doi.org/10.1007/s10995-011-0777-x
[6] UNICEF. Delivery care. 2021. https://data.unicef.org/topic/maternal-health/delivery-care/.
[7] Yaya, S., & Ghose, B., 2019, Global Inequality in Maternal Health Care Service Utilization: Implications for Sustainable Development Goals. Health equity, 3(1), 145–154. https://doi.org/10.1089/heq.2018.0082.
[8] Centers for Disease Control and Prevention., 2006, Recommendations to improve preconception health and health care—United States: A report of the CDC/ATSDR Preconception Care Work Group and the Select Panel on Preconception Care. MMWR. 55(RR-06):1–23.
[9] Bajpai N, Dholakia R, & Towle M., 2013, Increasing the availability of Skilled birth attendance in Rural India Mumbai. India. Columbia Global Centers | South Asia, Columbia University. globalcenters.columbia.edu/southasia/.
[10] Kenya National Bureau of Statistics (KNBS) and ICF Macro. 2010. Kenya Demographic and Health Survey 2008-09. Calverton, Maryland: KNBS and ICF Macro.
[11] MoH. Kenya Reproductive, Maternal, Newborn, Child, and Adolescent Health (Rmncah) Investment Framework, 2016, Nairobi, Ministry of Health.
[12] Kenya National Bureau of Statistics (KNBS, 2019). 2019 Kenya Population and Housing Census. Volume I: Population by County and Sub County. Kenya National Bureau of Statistics.
[13] Krejcie and Morgan (1970) Sample determination Table.
[14] Kathuri, N, J, & Pals D. A. (1993). Major causes of outmigration in Mukurueni, Nyeri County.
[15] Chou, D., Daelmans, B., Jolivet, RR., Kinney, M., & Say L., 2015, Ending preventable maternal and new-born mortality and stillbirths. BMJ. 351. doi: https://doi.org/10.1136/bmj.h4255.
[16] MoH. Transforming Health: Accelerating Attainment of Universal Health Coverage. Kenya Health Sector Strategic and Investment Plan 2014–2018 (KHSSP 2014–2018). Edited by Ministry of Health Kenya. Nairobi: Ministry of Health; 2014.
[17] Moore, M., Alex, B., & George, I., 2011, Utilization of Health Care Servicesby Pregnant mothers during Delivery. A community Based Study in Nigeria. East Afr J Public Health. 8(1):49-51. PMID: 22066284.
[18] Abebe, F., Berhane, Y. & Girma, B., 2012, Factors associated with home delivery in Bahirdar, Ethiopia: A case control study. BMC Res Notes 5, 653. https://doi.org/10.1186/1756-0500-5-653.
[19] Agarwal, S., Sethi, V., Srivastava, K., Jha, P. K., & Baqui, A. H., 2010, Birth preparedness and complication readiness among slum women in Indore city, India. Journal of Health, Population, and Nutrition, 28(4), 383–391. https://doi.org/10.3329/jhpn.v28i4.6045.
[20] Lawn J, Lule N. & Kerber K., 2005, Achieving the Millennium Development Goal of Improving
Maternal Health: Determinants, Interventions and Challenges. Health, Nutrition and Population (HNP) discussion paper. World Bank, Washington, DC. © World Bank. https://openknowledge.worldbank.org/handle/10986/13744.[21] Mbugua, S., & Kerry, LD., 2018, Maternal Health Indicators in High-Priority Counties of Kenya: Levels and Inequities. DHS Further Analysis Reports No. 110. Rockville, Maryland, USA: ICF.
[22] Singh, P.K., Rai, R.K., Alagarajan, M., & Singh, L. (2012). Determinants of Maternity Care services Utilization among Married adolescents in Rural India. Plos One 7(2): e31666.doi: 10.1371/journal.pone.003166.
[23] Pathak, PK., Singh, A., & Subramaman, SV., 2010, Economic Inequalities in Maternal health care: prenatal and Skilled Birth Attendance in India, 1992-2006. PLoS ONE 5. https://doi.org/10.1371/journal.pone.0013593.
[24] Khan, YP., Munim, S., & Bhutta, ZA., 2009, Maternal health and survival in Pakistan: issues and options. Journal of Obstetrics and Gynecology. 31(10):920-929. doi: 10.1016/S1701-2163(16)34321-3. PMID: 19941721.
[25] Gabrysch, S., & Campbell, O.M., 2009, Still too far to walk: Literature review of the determinants of delivery service use. BMC Pregnancy Childbirth 9(34). https://doi.org/10.1186/1471-2393-9-34.
Viewed PDF 916 17 -
 Effect of Interpersonal Communication Training Program on Knowledge, Attitude, and Reinforcing/Support Skills of Anti-retroviral Therapy Providers in Gombe State HospitalsAuthor: Suraj Abdulkarim ADOI: 10.21522/TIJPH.2013.11.01.Art024
Effect of Interpersonal Communication Training Program on Knowledge, Attitude, and Reinforcing/Support Skills of Anti-retroviral Therapy Providers in Gombe State HospitalsAuthor: Suraj Abdulkarim ADOI: 10.21522/TIJPH.2013.11.01.Art024Effect of Interpersonal Communication Training Program on Knowledge, Attitude, and Reinforcing/Support Skills of Anti-retroviral Therapy Providers in Gombe State Hospitals
Abstract:
Evidence from the developed world suggests that healthcare practitioners with greater Interpersonal communication (IPC) skills have better health outcomes after IPC training. There is less evidence from developing nations. This study examined the impact of an IPC training program on the knowledge, attitude, and reinforcing/supporting skills of ART practitioners at public ART hospitals in Gombe state, Nigeria. The study used a quasi-experimental design with two groups and two stages, as well as a multi-stage sampling approach. The knowledge disposition, attitude, and reinforcing and supporting IPC skills of 120 ART practitioners from six randomly selected hospitals were assessed. Then three weeks later, a 2-day IPC training using a self-administered structured questionnaire was carried out. SPSS Software (v. 22) was used to perform descriptive and inferential analyses on the data. At baseline, the Chi-Square test indicated no association between the groups on any of the demographic factors. The pre-intervention mean knowledge score was significantly higher (p = 0.019) in the experimental group than in the control group, although there were no significant differences in attitude (p=0.32) or reinforcing and support skills (p=0.786). After the IPC skills training program, significant differences were noticed between the experimental and control groups in terms of knowledge (p=.000) and attitude (p=0.006), but not in terms of reinforcing and support skills (p=.119). Training in interpersonal communication skills influences the knowledge and attitude of ART health providers in Gombe State. As a result, in-service IPC training is suggested for ART Health Providers in the State.
Keywords: Anti-retroviral therapy (ART), Interpersonal communication (IPC), Reinforcing and supporting skills.Effect of Interpersonal Communication Training Program on Knowledge, Attitude, and Reinforcing/Support Skills of Anti-retroviral Therapy Providers in Gombe State Hospitals
References:
[1] Siamian, H., Bagheri-Nesami, H., Darvish, .RN, Reza, F.N., Akbari, H., Balaghafari, H., Vahdei, M., 2014, Assessment of interpersonal communication skills among sari health centers’ staff. Mater Sociomed, 26(5), 324-32,8. https://pubmed.ncbi.nlm.nih.gov/25568632/.
[2] Brown L. D., De Negri B., Hernandez, O., Dominguez L, Sanchack JH, Roter D., 2000, An evaluation of the impact of training Honduran health care providers in interpersonal communication. International Journal for Quality in Health Care, 12(6), 495-501, https://pubmed.ncbi.nlm.nih.gov/11202603/.
[3] Skovdal, M., Wringe, A., Seeley, J., 2017, Using theories of practice to understand HIV-positive persons varied engagement with HIV services: a qualitative study in six Sub-Saharan African countries. Sexually Transmitted Infections, 93(3), 44-55., https://pubmed.ncbi.nlm.nih.gov/28736396/.
[4] Roemer, M. I., Montoya-Aguilar, C., 1988., Quality assessment and assurance in primary health care. Geneva: WHO Offset Publication, https://apps.who.int/iris/handle/10665/40663.
[5] Loevinsohn, B. P., 1990, Health Education Interventions in Developing Countries: A Methodological Review of Published Articles. International Journal of Epidemiology, 19(4), 788-794, https://pubmed.ncbi.nlm.nih.gov/2084004/.
[6] Hall, J., Rote,r D., and Katz, N., 1988, Correlates of provider behavior: a meta-analysis. Medical Care 26(1), 657-675, https://pubmed.ncbi.nlm.nih.gov/3292851/.
[7] Stein, T., Frankel, R. M., Krupat, E., 2005, Enhancing clinician communication skills in a large healthcare organization: a longitudinal case study. Patient Education and Counseling, 58 (1), 4-12, https://pubmed.ncbi.nlm.nih.gov/15950831/.
[8] Stewart, M., Brown, J.B., Boon, H., Galajda ,J., Meredith, L., Sangster, M., 1999, Evidence on patient-doctor communication. Cancer Prevention and Control, 3(1), 25-30, https://pubmed.ncbi.nlm.nih.gov/10474749/.
[9] Levinson, W., Roter, D.L., Mullooly, J.P., Dull, V.T., Frankel, R.M., 1997, Physician-patient communication: the relationship with malpractice claims among primary case physicians and surgeons. J Am Med Assoc, 277(1), 553-559, https://pubmed.ncbi.nlm.nih.gov/9032162/.
[10] City Population., 2022., Gombe State in Nigeria. https://citypopulation.de/en/nigeria/admin/NGA016_gombe/.
[11] McGilton, K.S., Boscart, V., Fox, M., Sidani, S., Rochon, E., Sorin-Peters, R. A., 2009, Systematic review of the effectiveness of communication interventions for health care providers caring for patients in residential care settings. Worldviews Evid Based Nurs. 6 (1), 149–159, https://pubmed.ncbi.nlm.nih.gov/19523033.
[12] Dickson, D.A. 1989, Interpersonal communication in the health professions: A focus on training. Counselling Psychology Quarterly, 2(3):345-366, https://www.tandfonline.com/doi/abs/10.1080/09515078908256688.
[14] Abdullahi, S.A., Smelyanskaya, M., John, S., 2020, Providing TB and HIV outreach services to internally displaced populations in Northeast Nigeria: Results of a controlled intervention study. PLoS medicine, 17(9)14-21, https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1003218.
[15] Garland, M.E., 2006, Assessing the Impact of the Interpersonal Communication Course. “Master’s Thesis, University of Tennessee, https://trace.tennessee.edu/utk_gradthes/4488.
[16] Hibbard, J.H., 2003, Engaging health care consumers to improve the quality of care. Medical care. 199(1), I61-I70, https://www.researchgate.net/publication/10935728_Engaging_Health_Care_Consumers_to_Improve_the_Quality_of_Care.
[17] Kagan C, Evans J, Kay B. Manual of Interpersonal Skills for Nurses: An Experiential approach. J Nurse Edu. 2002; 123(5):32- 38, https://old.amu.ac.in/emp/studym/100016913.pdf.
[18] Garland, M.E., 2006, Assessing the Impact of the Interpersonal Communication Course. “Master’s Thesis, University of Tennessee, https://trace.tennessee.edu/utk_gradthes/4488.
[19] Brown, B., Crawford, P., Carter, R., 2006, Evidence-based Health Communication: Interpersonal communication. Jadvnurse, 29(1), 53-60, https://www.researchgate.net/publication/286459012_Evidence_based_health_communication.
[20] Bérengère, N., Lori, B,, Orlando, H., Julia, R,, Debra, R., 2000, Quality Assurance Methodology Refinement Series. Improving Interpersonal Communication Between Health Care Providers and Clients, online 102(12), 43-49. http://qam.ipcbhpac.org/content/168/6/721.
Viewed PDF 994 30 -
 Factors Influencing Integration of Social Determinants of Health into Clinical Practice in Hospitals in UgandaAuthor: Higenyi EmmanuelDOI: 10.21522/TIJPH.2013.11.01.Art025
Factors Influencing Integration of Social Determinants of Health into Clinical Practice in Hospitals in UgandaAuthor: Higenyi EmmanuelDOI: 10.21522/TIJPH.2013.11.01.Art025Factors Influencing Integration of Social Determinants of Health into Clinical Practice in Hospitals in Uganda
Abstract:
The overall objective of this study was to assess the factors influencing the extent of integration of social determinants of health (SDH) into clinical practice in hospitals in Uganda. This was cross-sectional. Data was collected from 1042 health workers using a self-administered questionnaire. The factors influencing integration were elucidated using multiple regression modeling. The final model of the influencing factors contained the factor domains health worker confidence, hospital environment, health worker attitude, adoption level for strategies of integration, disease characteristics, and accreditation to the Nurses and Midwives Council. The study successfully elucidated the model for factors influencing the integration of social determinants into clinical practice. The findings have educational, practice, administrative, and policy implications. The multi-method approach was used to limit social desirability bias among health workers; however, the study did not adjust for carry-over effects arising from health workers who were also practicing in private clinics and medical centres.
Keywords: Clinical practice; Factors, Integration; Social determinants.Factors Influencing Integration of Social Determinants of Health into Clinical Practice in Hospitals in Uganda
References:
[1] Andermann, A. 2016. Taking action on the social determinants of health in clinical practice: a framework for health professionals. CMAJ, 188(17-18). doi:10.1503/cmaj.160177.
[2] James R. H, Delia B, Carlton A. E, Michelle A, Mark P, and John D. H. P, 2011. The Social Determinants of Tuberculosis: From Evidence to Action. Am J Public Health, 101(4): 654–662. Doi: 10.2105/AJPH.2010.199505.
[3] Elizabeth L. Tung, M. E. Peek, Marco A. R, Joyce P. Y, and Anna V, 2021. Association of Neighborhood Disadvantage with Racial Disparities In Covid-19 Positivity In Chicago. doi: 10.1377/hlthaff.2021.00695 Health Affairs 40, NO. 11 (2021): 1784–1791. https://www.healthaffairs.org/doi/pdf/10.1377/hlthaff.2021.00695.
[4] Hugh A, and Laura M. G, 2019. Meanings and Misunderstandings: A Social Determinants of Health Lexicon for Health Care Systems. https://www.milbank.org/quarterly/articles/meanings-and-misunderstandings-a-social-determinants-of-health-lexicon-for-health-care-systems/.
[5] Sara P and Sandro G, 2008. Epidemiology and the Macrosocial Determinants of Health. Journal of Public Health Policy 29, 275–289. doi:10.1057/jphp.2008.15.
[6] WHO, 2008. Social determinants of health. Retrieved August 29, 2020, from who.int: https://www.who.int/social_determinants/thecommission/finalreport/key_concepts/en.
[7] National Academies of Sciencies, Engineering and Medicne, 2019) Integrating Social Care into the Delivery of Health Care: Moving Upstream to Improve the Nation’s Health. Washington, DC: The National Academies Press. doi: https://doi.org/10.17226/25467.
[8] Michael J. O,2008. Macrosocial Determinants of Population Health: Edited by Sandro Galea. American Journal of Epidemiology, Volume 167 (12), Pages 1518–1519, https://doi.org/10.1093/aje/kwn059. https://academic.oup.com/aje/article/167/12/1518/88508.
[9] Raphael D, B. J. 2015 Understanding action on the social determinants of health: a critical realist analysis of in-depth interviews with staff of nine Ontario public health units. BMC Res Notes.8:105. Doi: 10.1186/s13104-015-1064-5. PMID: 25885537; PMCID: PMC4404559.
[10] Joshua R. Vest, PhD, MPH, Julia Adler-Milstein, Laura M. Gottlieb, et al., 2022. The American Journal of Managed Care, January 2022, Volume 28 (1). Assessment of Structured Data Elements for Social Risk Factors.
[11] American Academy of Family Physicians. (2019). About/Policies. Accessed July 04, 2019, from www.aafp.org: https://www.aafp.org/about/policies/all/social-determinants.html.
[12] Shekelle, P.G., Begashaw, M.M., Miake-Lye, I.M. et al, 2022. Effect of interventions for non-emergent medical transportation: a systematic review and meta-analysis. BMC Public Health 22, 799 (2022). https://doi.org/10.1186/s12889-022-13149-1.
[13] Richard Resnick October 20, 2021. What Social Determinants of Health Affect Medication Adherence. https://blog.cureatr.com/how-social-determinants-of-health-affect-medication-adherence.
[14] Han, D. S., Sang-Soo Bae, Kim, D.-H., & Choi, Y.-j. (2017, May). Origins and Evolution of Social Medicine and Contemporary Social Medicine in Korea. Preventive Medicine and Public Health, 50(3), 141-147. doi: 10.3961/jpmph.16.106.
[15] Samantha Artiga, a. E. 2018. Beyond Health Care: The Role of Social Determinants in Promoting Health and Health Equity. Retrieved from https://www.kff.org/disparities-policy/issue-brief/beyond-health-care-the-role-of-social-determinants-in-promoting-health-and-health-equity/.
[16] Andermann, A. 2018. Screening for social determinants of health in clinical care: moving from the margins to the mainstream. Public Health Review, 39(19). doi: https://doi.org/10.1186/s40985-018-0094-7.
[17] Garg, A., Jack, B., & Zuckerman, B., 2013. (A. M. Association, Producer) Retrieved July 05, 2019, https://www.pcpcc.org/resource/addressing-social-determinants-health-within-patient-centered-medical-home.
[18] Popay J, K. U, Mallinson S, M. S, Barker J. Social problems, primary care and pathways to help and support addressing health inequalities at the individual level. Part II: lay perspectives. J Epidemiol Community Health; 61(11):972-7. doi: 10.1136/jech.2007.061945. PMID: 17933955; PMCID: PMC2465618
[19] Allie F, 2020. Applying Social Determinants of Health to Improve Care Coordination. https://hitconsultant.net/2020/05/26/applying-social-determinants-of-health-to-improve-care-coordination/#.YYiJWmBBw2w.05/26/2020.
[20] Sara H., 2017. Using Social Determinants of Health in Patient-Centered Care. https://patientengagementhit.com/news/using-social-determinants-of-health-in-patient-centered-care.
[21] American Academy of Family Physicians. (2018). Addressing Social Determinants of Health in Primary Care team-based approach for advancing health equity. The EveyOne Project. https://www.aafp.org/dam/AAFP/documents/patient_care/everyone_project/team-based-approach.pdf.
[22] Cecilia O. 2021. Government Rushes to Procure More Hospital Beds. The New Vision, 07 July https://www.newvision.co.ug/articledetails/108087.
[23] Mohamad A. P., M. V. 2013. Sample size calculation in medical studies. Gastrology and Hepatology from Bed to Bench, 6(1), 14-17. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4017493/.
[24] Jarmusz, S. v. 2019, News and Insights: Data insights. (S. v. Jarmusz, Editor). https://www.mgma.com/data/data-stories/screening-for-social-determinants-of-health-(sdoh).
[25] Robert J. W., 2014. Reporting and Interpreting Scores Derived from Likert-type Scales. Journal of Agricultural Education, 55(5), 30-47. doi: 10.5032/jae.2014.05030.
[26] Paul E. Spector. 1992. Summated Rating Scale Construction: An Introduction Sage University Papers Series. Quantitative Applications in the Social Sciences; No. 07-082.
[27] Anol Bhattacherjee, 2012. Social Science Research: Principles, Methods, and Practices. https://courses.lumenlearning.com/suny-hccc-research-methods/chapter/chapter-6-measurement-of-constructs/.
[28] Uganda Bureau of Statistics, August 2019. Annual Labour Force Survey 2018/19. https://www.ubos.org/wp-content/uploads/publications/05_20212018-19_ALFS_Report_finaL.pdf.
[29] WEMOS Health Limited, 2019 Uganda’s Human Resources for Health: Paradoxes And Dilemmas. Country Report Uganda. https://www.wemos.nl/wp-content/uploads/2019/11/Wemos_Country-report-Uganda-2019_Ugandas-Human-resources-for-health_Paradoxes-and-dilemmas.pdf.
[30] Office Of International Religious Freedom. 2019 Report on International Religious Freedom: Uganda. https://www.state.gov/reports/2019-report-on-international-religious-freedom/uganda/#:~:text=According%20to%20the%20most%20recent,14%20percent%2.
[31] MoH 2007. Uganda Health Workforce Study: Satisfaction and Intent to Stay Among Current Health Workers. Intrahealth.org/sites/ihweb/files/files/media/uganda-health-workforce-study-satisfaction-and-intent-to-stay-among-current-health-workers/exe.
[32] Phillips, J., Richard, A., Mayer, K. M., Shilkaitis, M., Fogg, L. F., & Vondracek, H. 2020, Integrating the Social Determinants of Health into Nursing Practice: Nurses’ Perspectives. Nursing Scholarship. Retrieved November 15, 2020, from https://sigmapubs.onlinelibrary.wiley.com/doi/full/10.1111/jnu.12584.
[33] Arch G. M., Zhigang X, Sandhya Y., Maribeth W., Amy V. B., Young-Rock Hong, 2020. Physician Cultural Competency Training and Impact on Behavior: Evidence From the 2016 National Ambulatory Medical Care Survey. Fam Med. 2020;52(8):562-569, doi: 10.22454/FamMed.2020.163135.
[34] Pettersson S, Holstein J, Jirwe M, Jaarsma T, Klompstra L., 2021. Cultural competence in healthcare professionals, specialised in diabetes, working in primary healthcare-A descriptive study. https://www.diva-portal.org/smash/get/diva2:1574741/Fulltext01.pdf. doi: 10.1111/hsc.13442. Epub 2021 Jun 18. PMID: 34145649.
[35] Braun BL, Fowles JB, Solberg LI, Kind EA, Lando H, Pine D: Smoking-related attitudes and clinical practices of medical personnel in Minnesota. American Journal of Preventive Medicine. 2004, 27: 316-322. 10.1016/j.amepre.2004.07.010.
[36] Borrelli B, Hecht J, Papandonatos G, Emmons K, Tatewosian L, Abrams D, 2001: Smoking-cessation counseling in the home - Attitudes, beliefs, and behaviours of home healthcare nurses. Amercian Journal of Preventive Medicine. 21: 272-277. 10.1016/S0749-3797(01)00369-5.
[37] Taka mine, L., Forman, J., Damschroder, L.J. et al. Understanding providers’ attitudes and key concerns toward incorporating CVD risk prediction into clinical practice: a qualitative study. BMC Health Serv Res 21, 561 (2021). https://doi.org/10.1186/s12913-021-06540-y.
[38] EUFIC, 2014. Behaviour Change Models and Strategies https://www.eufic.org/en/healthy-living/article/motivating-behaviour-change.
Viewed PDF 971 29 -
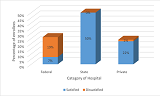 Assessment of the Impact of Health Maintenance Organizations on Access, Utilization, and Quality of Service among National Health Insurance Authority Enrollees in Kano, Kano State NigeriaAuthor: Gidado YusufDOI: 10.21522/TIJPH.2013.11.01.Art026
Assessment of the Impact of Health Maintenance Organizations on Access, Utilization, and Quality of Service among National Health Insurance Authority Enrollees in Kano, Kano State NigeriaAuthor: Gidado YusufDOI: 10.21522/TIJPH.2013.11.01.Art026Assessment of the Impact of Health Maintenance Organizations on Access, Utilization, and Quality of Service among National Health Insurance Authority Enrollees in Kano, Kano State Nigeria
Abstract:
Effort by government in Nigeria to provide effective ways of accessing quality and affordable healthcare service has been contentious with high cost of health care service delivery. The ineffective management of health care funds over the years was observed as key contributor to the rising cost of healthcare services. The need for the establishment of health maintenance organizations (HMOs) whose responsibility as purchasers, was to manage health care services with health facilities providers under the National Health Insurance Authority Scheme (NHIA). However, this research seeks to assess the impact of healthcare purchasers in Kano state Nigeria, as regards knowledge, utilization, and satisfaction of enrollees whose healthcare services they manage. The study utilized analysis of enrollees, HMOs and desk officers under the scheme. Quantitative and qualitative methods using interviewer administered questionnaire and Key stakeholders’ interview was used. Data were recorded in Microsoft Excel 2010 and analyzed using SPSS version 23.0. NVIVO version 12 with verbatim transcription was used for thematic analysis of qualitative data. Chi-square used to test degree of association and Logistic regression utilized to predict factors for the determinants. Results were presented as tables and charts. Statistical significance p-value <0.05 at confidence level of 95% was considered significant. Thus, analysis of the general demographic outcomes showed a significant association between HMOs and enrollees’ level of knowledge, utilization and satisfaction (p<0.05). Conversely, analysis of federal, state and private run facilities separately, revealed varying outcome as regards the three determinants, with the state-run hospitals mostly affected in terms of enrollee’s outcome.
Keywords: Desk officers, Health Maintenance Organizations, Knowledge, National Health Insurance Authority, Satisfaction, Utilization.Assessment of the Impact of Health Maintenance Organizations on Access, Utilization, and Quality of Service among National Health Insurance Authority Enrollees in Kano, Kano State Nigeria
References:
[1] Kutzin J., 2001, A descriptive framework for country-level analysis of health care financing arrangements. Health policy (Amsterdam, Netherlands), 56(3)171–204. https://doi.org/10.1016/s0168-8510(00)00149-4.
[2] Pozgar, G., 2016, Legal and Ethical Issues for Health Professionals (4th ed.). Burlington, MA: Jones & Bartlett Learning. Date of Access: 23/6/2021, https://samples.jblearning.com/9781284036794/9781284069761_FMxx_Cropped.pdf
[3] Odeyemi, I. A., and Nixon, J., 2013, Assessing equity in health care through the national health insurance schemes of Nigeria and Ghana: a review-based comparative analysis. International journal for equity in health, 12, Article number 9. https://doi.org/10.1186/1475-9276-12-9.
[4] Chen, A., and Goldman, D., 2016, Health care spending: Historical trends and new directions. Annual Review of Economics, 8, 291-319. doi:10.1146/annureveconomics-080315-015317.
[5] Zohrevandi, B., & Tajik, H., 2014, A Survey of Patients’ Satisfaction in Emergency Department of Rasht Poursina Hospital. Emergency (Tehran, Iran), 2(4), 162–165.
[6] Doris, D.S., 2022, Health in Nigeria -statistics and facts. Date of Access: 20/11/22, https://www.statista.com.
[7] Lars, K., 2022, Density of physicians in west Africa 2020 by country. Date of Access: 20/11/22, https://www.statista.com/statistics/1122671/density-of-medical-doctors-in-west-africa-by-country/.
[8] Simona.V., 2021, Government’s healthcare expenditure in Nigeria 2019-2021. Date of Access: 2/7/21, https://www.statista.com/aboutus/our-research-commitment/ 1914/ simona-varrella.
[9] Uzochukwu, B. S., Ughasoro, M. D., Etiaba, E., Okwuosa, C., Envuladu, E., and Onwujekwe, O. E., 2015, Health care financing in Nigeria: Implications for achieving universal health coverage. Nigerian journal of clinical practice, 18(4), 437–444. https://doi.org/10.4103/1119-3077.154196.
[10] Elizabeth, E.D., 2020, A Health Care Management Organization’s Internal Controls Strategy for Managed Care” Walden Dissertations and Doctoral Studies. 9345. https://scholarworks.waldenu.edu/dissertations/9345.
[11] Wao, H., and Onwuegbuzie, A.J., 2011, A Mixed Research Investigation of Factors Related to Time to the Doctorate in Education. International Journal of Doctoral Studies, 6, 115-134.
[12] Molina, A.J.F., and Fetters, M.D., 2018, Future Special Issues at the Journal of Mixed Methods Research. Journal of Mixed Methods Research,12(4),369–370, https://doi.org/10.1177/1558689818800897.
[13] Sánchez, H.A., and Alcón, S.E., 2011, Pragmatic gains in the study abroad context: Learners’ experiences and recognition of pragmatic routines, Journal of Pragmatics, 146,54-71.
[14] Federal Republic of Nigeria., 2009, National Population Commission Official Gazette. National Population Commission, Abuja. No.2 Vol.96.
[15] Kano State Ministry of Health, Kano SACA, IHVN and FHI 360., 2013, Kano State-wide Rapid Health Facility Assessment, Nigeria: Kano State Ministry of Health, Kano State Agency for the Control of AIDS, IHVN and FHI 360.
[16] James, E.B., 2001, Organizational research: Determining appropriate sample size in survey research.
[17] Daramola, O.E., Adesina, C.T., Abu, J.M., and Akande, T.M., 2019, Health Services Utilization Patterns among Enrollees of the National Health Insurance Scheme at a Tertiary Health Facility in Federal Capital Territory (FCT) – Abuja, Nigeria.
[18] Elo, S., Kaariainen, M., Kanste, O., Polkki, T., Utriainen, K., and Kyngas, H., 2014, Qualitative content analysis: A focus on trustworthiness. Sage Open, 4(1), 1-10. doi:10.1177/2158244014522633.
[19] Saunders, M.N.K., and Rohon, C., 2014, There’s no madness in my method: Explaining how your coaching research findings are built on firm foundations. Coaching: An International Journal of Theory, Research and Practice, 7, 74-83. doi:10.1080/17521882.2014.889185.
[20] Woods, M., Paulus, T., Atkins, D. P., and Macklin, R., 2016, Advancing Qualitative Research Using Qualitative Data Analysis Software (QDAS)? Reviewing Potential Versus Practice in Published Studies using ATLAS.ti and NVivo, 1994–2013.Social Science Computer Review, 34(5),597–617, https://doi.org/10.1177/ 0894439 3155963 11.
[21] Teusner, A., 2016, Insider research, validity issues, and the OHS professional: one person’s journey. International Journal of Social Research Methodology, 19, 85 - 96.
[22] Nelson, A.M., 2016, Methodology for examining attributes of African Americans in the Department of Defence Senior Executive Service Corp. Journal of Economic Development, Management, IT, Finance and Marketing, 8, 48-68.
[23] Anney, V., 2014, Ensuring the quality of the findings of qualitative research: Looking at trustworthiness criteria. Journal of Emerging Trends in Educational Research and Policy Studies, 5, 272-281.
[24] Lagarde, M., and Palmer, N., 2011, The impact of user fees on access to health services in low- and middle-income countries. The Cochrane database of systematic reviews, (4), CD009094, https://doi.org/10.1002/14651858.CD009094.
[25] Mohammad, A., 2013.Evaluation Study of Rashtriya Swasthya Bima Yojana in Shala and Kangra Districts in Himachal Pradesh. Date of Access: 9/11/2022, http://www.rsby.gov.in/Documents.aspx?ID=14.
[26] Patel, J., Shah, J., Agarwal, M., Kedia, G., 2013, Post Utilization Survey of RSBY beneficiaries in civil hospital, Ahmedabad: A cross sectional study. International Journal of Medical Science and Public Health. 2(4):1109-12.
[27] Iliyasu, Z., Abubakar, I.S., Abubakar, S., Lawan, U.M.., and Gajida, A.U., 2010, Patients’ satisfaction with services obtained from Aminu kano teaching hospital, Kano, Northern Nigeria. Journal of Scientific Research, 11, 1.
[28] Apeloko, O.D., 2017, Health Insurance Scheme (NHIS) in Nigeria: An Empirical Survey. International Journal of Politics and Good Governance. (8):1–25.
[29] 29. Ele, G.N., Ochu, U., Odili, V., Okechukwu, R., Ogbonna, B., 2016, Evaluation of the Benefits, Quality of Services and Challenges to the Nigerian National Health Insurance Scheme among Enrollees in a Tertiary Teaching Hospital in Southeast Nigeria. Journal of Advance Medical Pharmaceutical Science. 10;9(3):1–11.
[30] Osuchukwu, N.C., Osonwa, K.O., Eko, J.E., Uwanede, C.C., Abeshi, S.E., Offiong, D.A., 2013, Evaluating the Impact of National Health Insurance Scheme on Health Care Consumers in Calabar Metropolis, Southern Nigeria. Int J Learning Develop. Vol 3(4):30-45.
Viewed PDF 1082 49 -
 Quality of Life of People Living with HIV and AIDS on Art from a Tertiary Hospital in North KeralaAuthor: Jesha MundodanDOI: 10.21522/TIJPH.2013.11.01.Art027
Quality of Life of People Living with HIV and AIDS on Art from a Tertiary Hospital in North KeralaAuthor: Jesha MundodanDOI: 10.21522/TIJPH.2013.11.01.Art027Quality of Life of People Living with HIV and AIDS on Art from a Tertiary Hospital in North Kerala
Abstract:
Quality of life (QoL) refers to how well we live. Some people say the quality of life is about wealth and owning things, while others may define it in terms of physical, mental, and emotional well-being. A cross-sectional study on the quality of life of people living with HIV and AIDS attending ART-Clinic Calicut, a tertiary care unit in North Kerala where patients can check their CD4 count and get antiretroviral treatment free of cost. The study was conducted from over a period of 6 months with the help of two sets of questionnaires, part 1 to interview the subject on Socio-demography, Family details, Personal habits, Risk behavior, Disease-related details and part 2 for assessing quality of life by WHOQoL-HIV instrument. The sample size was calculated to be 310. The current study shows a good overall quality of life. The study shows a better score for the physical domain, psychological domain, independence domain, social relationship domain, and Environment domain but a lower score for spirituality/ religion/ personal belief domain. Social support given to PLHA was found to be an independent determinant that significantly improves Overall QoL and all its domains. The absence of HIV infection among children significantly improves all domains of QoL. The absence of opportunistic infection significantly improves all domains except the Physical domain which shows improvement but is not significant. All factors that improve Overall QoL were found to be improving all six domains of QoL.
Keywords: Quality of life, QoL, People living with HIV and AIDS, PLHA.Quality of Life of People Living with HIV and AIDS on Art from a Tertiary Hospital in North Kerala
References:
[1] WHO QOL-HIV Group. 2003. Preliminary development of the World Health Organization’s Quality of Life HIV Instrument (WHOQOL-HIV): analysis of the pilot version. Social Science and Medicine; 57: 1259–1275.
[2] International Institute for Population Sciences. 2007. National Family Health Survey-3 (2005-06).
[3] United Nations. 2001. Gender and HIV/AIDS (special session). 25-27 June 2001, New York.
[4] William C, Sarie Human, John A Rudo, Maria Rosa et al. 2009. Exploring HIV Stigma and quality of life for persons living with HIV infection. Journal of Association of Nurses in AIDS Care. 20(3):161-168.
[5] Subramanian T, Gupta MD, Dorairaj VS, Periaman V, Mathai AK. 2009. Psychosocial impact and quality of life of people living with HIV/AIDS in Chennai, South India. AIDS CARE. 21(4):473-481.
[6] Census of India (2011). State wise data on literacy. Kerala Literacy Rate.
[7] Census of India (2011). Work participation of females. Census data, Kerala.
[8] KSACS. 2011. Summary Report. Behavioral Surveillance Survey, Kerala, India.
[9] NACO. 2006. Socioeconomic impact of HIV/AIDS in India. Study done in six high prevalence states, Andhra Pradesh, Karnataka, Maharashtra, Nagaland, Manipur. Available on: Data.undp.org.in/hivreport/India_Report of UNDP.
[10] Saseedharan Pallikadavath et al. 2001. HIV/AIDS in rural India: Focus group discussion on Context and health care needs. Pune. available on socstas.soton.ac.uk.
[11] Global Adult Tobacco Survey. 2011. HIV estimates by detailed status of smoking, according to region/states/UTS. India. (2009-2010).
[12] NACO. 2011. annual report. (2010-’11) Available on: AnnualReport, 2010-2011-TEXTCS.indd (naco.org).
[13] KSACS. 2007. sentinel surveillance data, 2007. HIV prevalence in high-risk population.
[14] Robert W Burgoyne, Darell HS. 2008. Prolongation and quality of life for HIV infected adults treated with highly active antiretroviral therapy, a balancing act. Journal of Antimicrobial Chemothrapy. 61(469): 469-473.
[15] NACO. 2009. Training manual on intensified TB/HIV package for medical officers. TBC. available on www. Tbcindia.org.
[16] T.Mahalakshmi , KC Mofolorunsho, KG Osaybome. 2011. Quality of life of people living with HIV infection in Puducherry, India. Indian Journal of Community Medicine. 36(3).
[17] Lamkang AS, Joshi PC, Singh MM. 2009. Assessing the quality of life and needs of HIV/AIDS patients in Manipur, India. Journal of Communicable Disease. 41(4):221-227.
[18] Karl Peltzer et al. 2008. Health related factors in a sample of HIV infected South Africans. Human Science Research Council.
[19] Kristi Routel, Heti Pisarev, Hella Mail, Anneli Uskula. 2009. Factors influencing the quality of life of people living with HIV in Estonia. Journal of International AIDS Society. S12-13.
[20] Imam MH, Karim MR, Ferdous C Akhther. 2011. Health related quality of life among people living with HIV in Bangladesh. Bangladesh Medical Research Council Bulletin. 37:1-6.
[21] P.S Chandra Veena Satyanarayana, Satish Chandra, Satish Mahendra. 2009. Do men and women with HIV differ in their quality of life? A study from South India. AIDS Behaviour. 13:110-117.
[22] Yogita Rai, Anusree Dutta, Anil K Gulati. 2008. Quality of life of HIV infected people across different stages of infection. Journal of Happiness Studies. 2(1): 61-69.
[23] Manoj Kumar, Saroj Verma, Dipti, Heena. 2009. Quality of life of patients with HIV infection. Indian Journal of Social Science Researchers. 26(2): 79-86.
[24] Elisabete Cristina, Ivon Franca, Fernonda Lopes. 2007. Quality of life of people with HIV/AIDS in Sao Paulo Brazil. Rev Sauda Publica. 41(2).
[25] Amare Deribew, Markas Tosfoye, Yohannes Hailmkhal, Neliya Negussu, Shalo Daba, Ajetne Woye, et al. 2009. Tuberculosis and HIV co-infection, its impact on quality of life. Health and Quality of Life Outcome. 7:105.
[26] A.A Fatiregum, KC Mofolorunsho, KG Osaybame. 2009. Quality of life of people living with HIV/AIDS in Koye State, Nigeria. Benin Journal of Postgraduate Medicine. 2(1).
[27] Venter E, Gericke GJ, Bekker PJ. 2009. Nutritional status, quality of life and CD4 cell count of adults living with HIV/AIDS in GaRankuwa area, South Africa. South African Journal of Clinical Nutrition. 22(3): 124-129.
[28] Zimpel Fbek. 2007.Quality of life in HIV positive Brazilians: application and validation of WHOQOL-HIVBrazilian version. AIDS CARE. 19:923-930.
[29] Kebeda Alera et al. 2010. Quality of life of people living with HIV/AIDS on highly active antiretroviral therapy in Ethiopia. African Journal of AIDS Research. 9(1):31-40.
[30] Naveet Wig, Raja lekshmi, Hemraj Pal, Vivek Chander Mohan, Sunil Kumar. 2006. The impact of HIV/AIDS on the quality of life: a cross sectional study in North India. Indian Journal of Medical Sciences. 60(1): 3-12.
[31] Abboud S, Noureddine S, Huijer HA, De Jong, Mokhbat J. 2010. Quality of life in people living with HIV/AIDS in Lebanon. AIDS CARE. 22(6):687-689.
[32] Xigoyan, Sato, Mari Kondo. 2011. Quality of life and related factors among people China. Journal of Nursing and Health Care of Chronic illness. 3(4): 513-520.
[33] Yang MH, Chen YM, Kuo BI, Wang KY. 2003. Quality of life and related factors for people living
with HIV/AIDS in Northern Taiwan. J Nurs Res. 11(3):217-26.[34] Basterdo Y. M., Kimberlin C. C. 2000. Relationship between quality of life of people, social support, and disease related factors in HIV infected persons in Venezuela. Aids Care. 12(5):673-84.
[35] Liu C., Johnson L, O Strow D, Silvester A, Visscher B, Jacobson LP.2006. Predictors for lower quality of life in HAART era among HIV infected men. Journal of AIDS. 42(4): 470-477.
[36] Wachtel T., Piette J, Mor V, Stein M, Flieshman J, Carpenter C. 1992. Quality of life in persons with HIV infection:measured by medical outcomes. Annals of Internal Medicine. 116(2): 129-37.
[37] Preau, Marie, Marcellin, Fabienne, Carrieri et al. 2007. Health related quality of life in French people living with HIV in 2003: National ANRS (EN 12-VESPA study. AIDS. 21(P): S19-27.
[38] Marziej Nojomi, Khalereh, Mitra. 2008. Health related quality of life in patients with HIV/AIDS. Archives Iranian Medicine. 11(6):608-612.
Viewed PDF 1064 35 -
 To Identify the Consequence of Social Distancing on the Social Affinity Needs in the Lives of the ElderlyAuthor: Babasaheb GhodkeDOI: 10.21522/TIJPH.2013.11.01.Art028
To Identify the Consequence of Social Distancing on the Social Affinity Needs in the Lives of the ElderlyAuthor: Babasaheb GhodkeDOI: 10.21522/TIJPH.2013.11.01.Art028To Identify the Consequence of Social Distancing on the Social Affinity Needs in the Lives of the Elderly
Abstract:
The present study aimed to examine the interrelatedness of three key variables: The social affinity needs of the elderly, the social needs of elderly individuals, and Social distance. To do this, a path analysis was conducted on a sample of elderly individuals. In conclusion, this study provides evidence of a complex relationship between social distance, social affinity needs and the social needs of the elderly. Social space has a positive relationship with both social affinity needs, and the social needs of the elderly, and social affinity needs have a positive relationship with the social needs of the elderly. This study provides valuable insights into the impact of social distancing on the social needs and social affinity needs of the elderly population. It highlights the need for interventions to support older adults during periods of social distancing. The previous two years were unpredictable. The epidemic has had a remarkable effect on all population subgroups. In response to the global spreading of the corona infection, the government devised social distance restrictions aimed at high-risk age groups. The indicated age group was those less than 65 years old. They are more susceptible to such a sickness due to age-related symptoms, lower antibodies, physical and psychological dependency upon one another, and especially lack of mobility. More than the danger of infection, the stigma connected to this circumstance significantly impacts the elderly. This generation faces increased mortality-related problems because of the comorbid condition.
Keywords: Elderly People, Pandemic, Social distancing, Vulnerable.To Identify the Consequence of Social Distancing on the Social Affinity Needs in the Lives of the Elderly
References:
[1] D. Democracy, the Market and the Forum. 2020. doi: 10.4324/9780203986820-27.
[2] D. Gujarati, “Title,” pp. 5–7, 2010, [Online]. Available: “Not just old and sick - The ‘will to health’ in later life,” Ageing Soc., vol. 29, no. 5, pp. 687–707, 2009, doi: 10.1017/S0144686X08008271.
[3] K. U. Mayer, “New directions in life course research,” Annu. Rev. Sociol., vol. 35, pp. 413–433, 2009, doi: 10.1146/annurev.soc.34.040507.134619.
[4] N. Lupu and J. Pontusson, “The structure of inequality and the politics of redistribution,” Am. Polit. Sci. Rev., vol. 105, no. 2, pp. 316–336, 2011, doi: 10.1017/S0003055411000128.
[5] F. Hong Kong Istanbul Karachi “Recensions / Reviews Recensions / Reviews,” pp. 201–203, 1995, [Online]. Available: doi: 10.1016/0047-2727(92)90024-A.
[6] L. Lawton, M. Silverstein, and V. Bengtson, “Affection, Social Contact, and Geographic Distance between Adult Children and Their Parents,” J. Marriage Fam., vol. 56, no. 1, p. 57, 1994, doi: 10.2307/352701.
[7] T. Line, J. Jain, and G. Lyons, “The role of ICTs in everyday mobile lives,” J. Transp. Geogr., vol. 19, no. 6, pp. 1490–1499, 2011, doi: 10.1016/j.jtrangeo.2010.07.002.
[8] L. Srole, “Social Integration and Certain Corollaries: An Exploratory Study,” Am. Sociol. Rev., vol. 21, no. 6, p. 709, 1956, doi: 10.2307/2088422.
[9] T. Faist, “Transnationalization in international migration: Implications for the study of citizenship and culture,” Ethn. Racial Stud., vol. 23, no. 2, pp. 189–222, 2000, doi: 10.1080/014198700329024.
[10] C. Phillipson, S. Yarker, L. Lang, P. Doran, M. Goff, and T. Buffel, “Covid-19, inequality and older people: Developing community-centred interventions,” Int. J. Environ. Res. Public Health, vol. 18, no. 15, 2021, doi: 10.3390/ijerph18158064.
[11] P. Higgs, M. Leontowitsch, F. Stevenson, and I. R. Jones, “Not just old and sick - The ‘will to health’ in later life,” Ageing Soc., vol. 29, no. 5, pp. 687–707, 2009, doi: 10.1017/S0144686X08008271.
[12] M. Harangi-Rákos, C. Pfau, É. B. Bába, B. A. Bács, and P. M. Kőmíves, “Lockdowns and Physical Activities: Sports in the Time of Covid,” Int. J. Environ. Res. Public Health, vol. 19, no. 4, 2022, doi: 10.3390/ijerph19042175.
[13] D. C. Giles, “Parasocial interaction: A review of the literature and a model for future research,” Media Psychol., vol. 4, no. 3, pp. 279–305, 2002, doi: 10.1207/S1532785XMEP0403_04.
[14] P. J. F. Gantillon, “'The adventurer.”,” Notes Queries, vol. s9-I, no. 26, p. 507, 1898, doi: 10.1093/nq/s9-I.26.507-c.
[15] J. Baars, “Aging: Learning to Live a Finite Life,” Gerontologist, vol. 57, no. 5, pp. 969–976, 2017, doi: 10.1093/geront/gnw089.
[16] W. Kymlicka, W. Kymlicka, and W. Kymlicka, “Recensions / Reviews Recensions / Reviews,” pp. 201–203, 1995, [Online]. Available: doi: 10.1016/0047-2727(92)90024-A.
[17] W. Kymlicka, W. Kymlicka, and W. Kymlicka, “Recensions / Reviews Recensions / Reviews,” pp. 201–203, 1995, [Online]. Available: doi: 10.1016/j.jtrangeo.2010.07.002.
[18] L. Kristov, P. Lindert, and R. McClelland, “Pressure groups and redistribution,” J. Public
Econ., vol. 48, no. 2, pp. 135–163, 1992, doi: 10.1016/0047-2727(92)90024-A.[19] J. DeFilippis and S. Saegert, “Five Faces of Oppression: Iris Marion Young,” Community Dev. Read., pp. 280–289, 2020, doi: 10.4324/9780203935569-42.
[20] Friedrich, “Russian Pronominal Usage.pdf.” 1969. [Online]. Available: http://mapageweb.umontreal.ca/tuitekj/cours/2611pdf/Friedrich-Russian-Pronominal.pdf.
Viewed PDF 876 24 -
 Assessment of the Knowledge of Hepatitis B Virus Infection in Primary Healthcare Centers in Abuja, NigeriaAuthor: Orji Ikechukwu ADOI: 10.21522/TIJPH.2013.11.01.Art029
Assessment of the Knowledge of Hepatitis B Virus Infection in Primary Healthcare Centers in Abuja, NigeriaAuthor: Orji Ikechukwu ADOI: 10.21522/TIJPH.2013.11.01.Art029Assessment of the Knowledge of Hepatitis B Virus Infection in Primary Healthcare Centers in Abuja, Nigeria
Abstract:
Hepatitis B virus (HBV) infection affects the liver and can lead to potentially life-threatening acute or chronic disease. The population with high HBV infection prevalence of
Keywords: Abuja, Hepatitis B virus Infection, Health-workers, Knowledge, Primary healthcare centers.8%, such as Nigeria, presents the highest risk of HBV transmission among health-workers. There is a need to disseminate knowledge of HBV infection and the risk of transmission to health-workers. In this baseline study, the team assessed the knowledge of HBV infection among health-workers in Primary Healthcare Centers (PHCs) in AMAC, Abuja. We conducted cross-sectional descriptive research that studied 168 randomly selected health-workers from 58 PHCs in AMAC, collected data with a pre-tested structured questionnaire, and analyzed it with SPSS version 21.0. The knowledge level of HBV symptoms and transmission ranged from 57.1% to 85.7%s and 84.5% to 91.7%, respectively. About 67% demonstrated good knowledge of HBV screening for pregnant women and 69% of Hepatitis B vaccination at birth. All the PHCs (100%) reported the unavailability of guidelines/protocols for HBV infection in pregnancy management and prevention. Furthermore, 51.2%, 53.7%, and 55.6% demonstrated poor knowledge of referral, PMTCT eligibility, and increased need for laboratory tests, respectively. Moreover, 60.2% showed poor awareness of treatment eligibility and 61.2% of choice of drug. Concluding, the respondents demonstrated good knowledge of HBV infection symptoms, transmission, screening for pregnant women, and vaccination schedules to prevent HBV infection. They showed a poor understanding of the referral of pregnant HBV seropositive women from the PHCs to secondary/tertiary hospitals, PMTCT, laboratory requirements for pregnant seropositive clients, and management of chronic HBV in pregnancy.
Assessment of the Knowledge of Hepatitis B Virus Infection in Primary Healthcare Centers in Abuja, Nigeria
References:
[1] World Health Organization. Hepatitis B, Key Facts [internet]. 2019 [cited Dec 2022]. Available at https://www.who.int/news-room/fact-sheets/detail/hepatitis-b.
[2] Abutu A. Nigeria’s complicated hepatitis burden. The lancet. Gastroenterology & hepatology. 2018; 3 (10): 669. Available from DOI: doi.org/10.1016/S2468-1253 (18)30279.
[3] Trépo C., Chan H.L., Lok A. Hepatitis B virus infection. Lancet. 2014; 384: 2053–2063.
[4] World Health Organization. Hepatitis B, Key Facts [internet]. 2019 [cited Dec 2022]. Available from www.who.int/news-room/fact-sheets/detail/hepatitis-b.
[5] Park K. Park’s textbook of preventive and social medicine, 22nd Ed. Jabalpur India, Bhanot publishers; 2013. 193-197p.
[6] World Health Organization. Guidelines for the prevention, care and treatment of persons with chronic hepatitis B infection [internet]. 2015 [cited Dec 2022]. Available from www.who.int/hepatitis/publications/hepatitis-b-guidelines/en/.
[7] World Health Organization. WHO Guidelines on Hepatitis B and C Testing. How to test for chronic hepatitis b infection – choice of serological assay and testing strategy [internet]. 2017 [cited Dec 2022]. Available from https://www.ncbi.nlm.nih.gov/books/NBK442276/.
[8] World Health Organization. Global Health Sector Strategy on Viral Hepatitis 2016–2021 towards Ending Viral Hepatitis [internet]. 2016 [cited Dec 2022]. Available from. Retrieved from https://apps.who.int/iris/bitstream/handle/10665/246177/WHO-HIV-2016.06-eng.pdf;jsessionid=E06F91F11D5557346E958E3F4020A864?sequence=1.
[9] Adekanle O., Ndububa D.A., Olowookere S.A., Ijarotimi O., Ijadunola K.T. Knowledge of Hepatitis B Virus Infection, Immunization with Hepatitis B Vaccine, Risk Perception, and Challenges to Control Hepatitis among Hospital Workers in a Nigerian Tertiary Hospital. Hindawi Publishing Corporation, Hepatitis Research and Treatment. 2015; Article ID 439867. Available from http://dx.doi.org/10.1155/2015/439867.
[10] Oyewusi C.O., Okanlawon F.A., Ndikom C.M. Knowledge and Utilization of Hepatitis B Infection Preventive Measures and Influencing Factors among Health Care Workers in Ibadan, Nigeria. International Journal of Caring Sciences. 2015 Jan -Apr; 8 (1): 164.
[11] Morowatishaifabad M.A., Zare Sakhvidi M.J., Gholianavval M., Masoudi Boroujeni D., Alavijeh M.M. Predictors of Hepatitis B Preventive Behavioral Intentions in Healthcare Workers. Saf Health Work. 2015;6(2):139-142. doi: 10.1016/j.shaw.2014.12.001
[12] NPHCDA. Minimum standard for primary health care in Nigeria. 2012. Available at https://hrf.health.gov.ng.
[13] Debes J.D., Kayandabila J. & Poemiller H. Knowledge of Hepatitis B Transmission Risks among Health Workers in Tanzania. Am. J. Trop. Med. Hyg. 2016; 94 (5) pp. 1100–1102 doi:10.4269/ajtmh.15-0797.
[14] Hassan M., Awosan K.J., Nasir S. et al. Knowledge, risk perception and hepatitis B vaccination status of healthcare workers in Usmanu Danfodiyo University Teaching Hospital, Sokoto, Nigeria. 2016; 8(4): 53–59. DOI: https://doi.org/10.5897/ JPHE2015.0795 10. Cvjetkovic SJ, Jeremic V.
[15] Dayyab F.M., Iliyasu G., Ahmad B.G., Bako A.T., Ngamariju S.S., Habib A.G. Hepatitis B vaccine knowledge and self-reported vaccination status among healthcare workers in a conflict region in northeastern Nigeria. Ther Adv Vaccines Immunother. 2020 Jan 16; 8:2515135519900743. doi: 10.1177/2515135519900743. PMID: 32002499; PMCID: PMC6966246.
[16] Ibitoye S.E. Knowledge and vaccination status for hepatitis B infection among health workers in Ibadan, Nigeria. African journal of medicine and medical sciences. 2020-08-07. https://ojshostng.com/index.php/ajmms/article/view/451.
[17] Adekanle O., Ndububa D.A., Olowookere S.A., Ijarotimi O., Ijadunola K.T. Knowledge of Hepatitis B Virus Infection, Immunization with Hepatitis B Vaccine, Risk Perception, and Challenges to Control Hepatitis among Hospital Workers in a Nigerian Tertiary Hospital. Hindawi Publishing Corporation, Hepatitis Research and Treatment. 2015; Article ID 439867. Available from http://dx.doi.org/10.1155/2015/439867.
[18] Oyewusi C.O., Okanlawon F.A., Ndikom C.M. Knowledge and Utilization of Hepatitis B Infection Preventive Measures and Influencing Factors among Health Care Workers in Ibadan, Nigeria. International Journal of Caring Sciences. 2015 Jan -Apr; 8 (1): 164.
[19] Yasobant S., Trivedi P., Saxena D., Puwar T., Vora K., Patel M. Knowledge of hepatitis B among healthy population: A community-based survey from two districts of Gujarat, India. J Family Med Prim Care. 2017 Jul-Sep;6(3):589-594. doi: 10.4103/2249-4863.222009. PMID: 29417014; PMCID: PMC5787961.
[20] Okwara E. C., Enwere O. O., Diwe C. K, Azike J. E., and Chukwulebe A. E., “Theatre and laboratory workers’ awareness of and safety practices against hepatitis B and C infection in a suburban university teaching hospital in Nigeria,” The Pan African Medical Journal, vol. 13, p. 2, 2012.
[21] Ayoub W.S. & Cohen E. Hepatitis B Management in the Pregnant Patient: An Update. J Clin Transl Hepatol. 2016 Sep 28; 4(3): 241–247. doi: 10.14218/JCTH.2016.00014.
[22] Chao, S.D., Cheung, C.M., Chang, E.T., Chang E.T., Pei A. Management of hepatitis B infected pregnant women: a cross-sectional study of obstetricians. BMC Pregnancy Childbirth 19, 275 (2019). https://doi.org/10.1186/s12884-019-2421-5.
Viewed PDF 1184 45 -
 Barriers and Facilitators to Integration of Social Determinants into Clinical Practice in Hospitals in UgandaAuthor: Higenyi EmmanuelDOI: 10.21522/TIJPH.2013.11.01.Art030
Barriers and Facilitators to Integration of Social Determinants into Clinical Practice in Hospitals in UgandaAuthor: Higenyi EmmanuelDOI: 10.21522/TIJPH.2013.11.01.Art030Barriers and Facilitators to Integration of Social Determinants into Clinical Practice in Hospitals in Uganda
Abstract:
Integration of social determinants into clinical practice is an emerging attractive phenomenon because of its potential benefits to the health system and patients however inadequate understanding of the barriers and facilitators poses immense challenges in designing programs and interventions aimed at enhancing integration of social determinants into clinical practice. This study investigated the barriers and facilitators to integration of social determinants into clinical practice in hospitals in Uganda. Data was collected from 21 key informants using a key informant guide that covered various aspects of integration of social determinants into clinical practice. The study identified barriers and facilitators at institutional and health-worker associated barriers. These barriers were at patient, departmental and community levels. There were similarities and differences in the barrier’s ad facilitators observed in this study and those articulated in literature. More so this study revealed some unique barriers and facilitators. The study confirmed existence of barriers and facilitators to integration of social determinants into clinical practice in hospitals in Uganda. Although in-depth interviews were conducted it was not possible to eliminate self-report bias
Keywords: Barriers, Facilitators, Social determinants, Integration, Hospitals.Barriers and Facilitators to Integration of Social Determinants into Clinical Practice in Hospitals in Uganda
References:
[1] Andermann, A., 2016. Taking action on the social determinants of health in clinical practice: a framework for health professionals. CMAJ, 188(17-18). doi:10.1503/cmaj.160177.
[2] Sara H., 2017. Using Social Determinants of Health in Patient-Centered Care. https://patientengagementhit.com/news/using-social-determinants-of-health-in-patient-centered-care.
[3] James R. Hargreaves, Delia Boccia, Carlton A. Evans, Michelle Adato, Mark Petticrew, and John D. H. Porter, 2011. The Social Determinants of Tuberculosis: From Evidence to Action. Am J Public Health, 101(4): 654–662. doi: 10.2105/AJPH.2010.199505.
[4] Hugh Alderwick and Laura M. Gottlieb, 2019. Meanings and Misunderstandings: A Social Determinants of Health Lexicon for Health Care Systems. https://www.milbank.org/quarterly/articles/meanings-and-misunderstandings-a-social-determinants-of-health-lexicon-for-health-care-systems/.
[5] Leo Lopez; Louis H. Hart; Mitchell H. Katz, 2021. Racial and Ethnic Health Disparities Related to Covid-19. JAMA. 2021;325(8):719-720. doi:10.1001/jama.2020.26443.
[6] Michael J. Oakes, 2008. Macrosocial Determinants of Population Health: Edited by Sandro Galea. American Journal of Epidemiology, Volume 167 (12), Pages 1518–1519, https://doi.org/10.1093/aje/kwn059, https://academic.oup.com/aje/article/167/12/1518/88508.
[7] Allie F., 2020. Applying Social Determinants of Health to Improve Care Coordination. https://hitconsultant.net/2020/05/26/applying-social-determinants-of-health-to-improve-care-coordination/#.YYiJWmBBw2w. 05/26/2020.
[8] Labib G., Gerald V. Gurp, David Z., Anne A., 2018. Physician experiences and barriers to addressing the social determinants of health in the Eastern Mediterranean Region: a qualitative research study. BMC Health Services Research (2018) 18:614. https://doi.org/10.1186/s12913-018-3408-z.
[9] WHO, 2008. Social determinants of health. Accessed 29/06/2020, from who.int: https://www.who.int/social_determinants/thecommission/finalreport/key_concepts/en.
[10] National Academies of Sciencies, Engineering and Medicne, 2019. Integrating Social Care into the Delivery of Health Care: Moving Upstream to Improve the Nation’s Health. Washington, DC: The National Academies Press. doi: https://doi.org/10.17226/25467.
[11] American Academy of Family Physicians, 2019. About/Policies. Accessed 04/07/2019, from www.aafp.org: https://www.aafp.org/about/policies/all/social-determinants.html.
[12] Richard R. 2021. How Social Determinants of Health Affect Medication Adherence. https://blog.cureatr.com/how-social-determinants-of-health-affect-medication-adherence.
[13] Samantha Artiga, a. E., 2018. Beyond Health Care: The Role of Social Determinants in Promoting Health and Health Equity. https://www.kff.org/disparities-policy/issue-brief/beyond-health-care-the-role-of-social-determinants-in-promoting-health-and-health-equity/.
[14] Rural Health Information Hub, 2020. Tools for success. Accessed 10/11/2020: https://www.ruralhealthinfo.org/toolkits/sdoh/1/frameworks.
[15] Andermann, A., 2018. Screening for social determinants of health in clinical care: moving from the margins to the mainstream. Public Health Review, 39(19). doi: https://doi.org/10.1186/s40985-018-0094-7.
[16] HIMSS, 2019. Resource Centre-Latest Resources. Retrieved from himss.org: https://www.himss.org/resources/social-determinants-health-can-zip-codes-influence-health-outcomes.
[17] Cecilia O. 2021. Government Rushes to Procure More Hospital Beds. The New Vision, 07 July https://www.newvision.co.ug/articledetails/108087.
[18] UCLA Centre for Health Policy Research, 2004. Section 4: Key informant Interviews. https://healthpolicy.ucla.edu/programs/health-data/trainings/Documents/tw_cba23.pdf.
[19] Dowhaniuk, N. Exploring country-wide equitable government health care facility access in Uganda. Int J Equity Health 20, 38 (2021). https://doi.org/10.1186/s12939-020-01371-5.
[20] Government of Uganda, 2017. Malnutrition in Uganda, Agriculture and Nutrition Fact Sheet. https://www.fantaproject.org/sites/default/files/resources/Uganda-Ag-Nutrition-FactSheet-Dec2017.pdf.
[21] Ssegujja, E., Mulumba, Y., Guttmacher, S. et al., 2021. The role and attributes of social networks in the provision of support to women after stillbirth: experiences from Uganda. BMC Women’s Health 21, 352 (2021). https://doi.org/10.1186/s12905-021-01498-9.
[22] Dauner, K.N., Loomer, L. A, 2021. Qualitative assessment of barriers and facilitators associated with addressing social determinants of health among members of a health collaborative in the rural Midwest. BMC Health Serv Res 21, 867 (2021). https://doi.org/10.1186/s12913-021-06859-6.
[23] Westerberg et, al 2009. Cross-sectional survey of hearing impairment and ear disease in Uganda. Journal of otolaryngology - head & neck surgery = Le Journal d’oto-rhino-laryngologie et de chirurgie cervico-faciale 37(6):753-8.
[24] The Republic of Uganda, 2015. The National Social Protection Policy. https://socialprotection.go.ug/wp-content/uploads/2016/07/National-Social-Protection-Policy-uganda.pdf.
[25] Hilary E. Rogers, 2014. Assessment Of the Capacity of Ugandan Health Facilities, Personnel, And Resources to Prevent And Control Noncommunicable Diseases.
Viewed PDF 893 26 -
 Prevalence of Hypertension among HIV/AIDS Patients Attending a Tertiary Hospital in North-East NigeriaAuthor: Roland I StephenDOI: 10.21522/TIJPH.2013.11.01.Art031
Prevalence of Hypertension among HIV/AIDS Patients Attending a Tertiary Hospital in North-East NigeriaAuthor: Roland I StephenDOI: 10.21522/TIJPH.2013.11.01.Art031Prevalence of Hypertension among HIV/AIDS Patients Attending a Tertiary Hospital in North-East Nigeria
Abstract:
The HIV disease and its several antiviral agents have over the years been showing some associations with hypertension. While the HIV programme in sub sub-Saharan Africa including Nigeria, which is largely donor driven, focuses on the provision of HIV care only, the evolving trend of hypertension in this population goes unrecognised and neglected. The objective of the study was to establish the burden of hypertension in the HIV population as an evolving unrecognised comorbidity calling for attention. The variables of age, marital status and ethnicity were evaluated and appear to have some bearings with hypertension. This was a retrospective, descriptive study conducted at Modibbo Adama University Teaching Hospital, Yola, Adamawa Nigeria through a review of past medical records of HIV patients attending the infectious disease clinic during a 10-year period. The retrieved data were entered into and analysed using the IBM SPSS version 20.0 statistical software. Prevalence was expressed in percentage. Bivariate analysis was performed using the Chi-square test for association between socio demographics and hypertension status. A value of p < 0.05 was considered significant Twenty-two per cent (22.1%) of the study population were found to be hypertensive. Older age, marital status and ethnicity were found to be significantly associated with hypertension among the HIV population (p<0.001). This finding draws attention to the high burden of hypertension among people living with HIV/AIDS. Health policy makers and other stakeholders should therefore design and implement a wholistic HIV programme that incorporates care for non-communicable diseases such as hypertension.
Keywords: Hypertension, HIV, prevalence.Prevalence of Hypertension among HIV/AIDS Patients Attending a Tertiary Hospital in North-East Nigeria
References:
[1] Okubadejo NU, Ozoh OB, Ojo OO, Akinkugbe AO, Odeniyi IA, Adegoke O, et al. Prevalence of hypertension and blood pressure profile amongst urban-dwelling adults in Nigeria: a comparative analysis based on recent guideline recommendations. Clin Hypertens. 2019 Dec;25(1).
[2] Bigna JJ, Tankeu AT, Kaze AD, Noubiap JJ, Nansseu JR. Prevalence and incidence of hypertension in the global HIV-infected population: A systematic review and meta-analysis protocol. BMJ Open. 2017;7(10):1–5.
[3] National Research Council. The Continuing Epidemiological Transition in Sub-Saharan Africa [Internet]. The Continuing Epidemiological Transition in Sub-Saharan Africa. 2012. Available from: http://www.ncbi.nlm.nih.gov/books/NBK114514/.
[4] Roth GA, Johnson C, Abajobir A, Abd-Allah F, Abera SF, Abyu G, et al. Global, Regional, and National Burden of Cardiovascular Diseases for 10 Causes, 1990 to 2015. J Am Coll Cardiol. 2017;70(1):1–25.
[5] Dimala CA, Atashili J, Mbuagbaw JC, Wilfred A, Monekosso GL. Prevalence of hypertension in HIV/AIDS patients on highly active antiretroviral therapy (HAART) compared with HAART-naïve patients at the Limbe Regional Hospital, Cameroon. PLoS One. 2016;11(2):1–11.
[6] Korem M, Wallach T, Bursztyn M, Maayan S, Olshtain-Pops K. High prevalence of hypertension in ethiopian and non-ethiopian HIV-infected adults. Int J Hypertens. 2018;2018.
[7] Ssinabulya I, Kayima J, Longenecker C, Luwedde M, Semitala F, Kambugu A, et al. Subclinical atherosclerosis among HIV-infected adults attending HIV/AIDS care at two large ambulatory HIV clinics in Uganda. PLoS One. 2014;9(2):1–9.
[8] Santos J, Palacios R, Castells E, González M, Ruiz J, Márquez M. Impact of highly active antiretroviral therapy on blood pressure in patients with HIV infection. A prospective study in a cohort of naive patients. Nutrition and Metabolic Disorders in HIV Infection. 2004;3(2):421–4.
[9] Bloomfield GS, Hogan JW, Keter A, Holland TL, Sang E, Kimaiyo S, et al. Blood pressure level impacts risk of death among HIV seropositive adults in Kenya: A retrospective analysis of electronic health records. BMC Infect Dis. 2014;14(1):1–10.
[10] Disease CA. Inflammation, Atherosclerosis, and coronary artery disease. 2005;1685–95.
[11] Jung O, Bickel M, Ditting T, Rickerts V, Welk T, Helm EB, et al. Hypertension in HIV-1-infected patients and its impact on renal and cardiovascular integrity. Nephrology Dialysis Transplantation. 2004;19(9):2250–8.
[12] Hendrix Sloane, Misuraca, & Moore A. genetic changes NIH Public Access. Bone. 2013;23(1):1–7.
[13] Tien PC, Choi AI, Zolopa AR, Benson C, Tracy R, Scherzer R, et al. Inflammation and mortality in HIV-infected adults: Analysis of the FRAM study cohort. J Acquir Immune Defic Syndr (1988). 2010;55(3):316–22.
[14] Dubé MP, Lipshultz SE, Fichtenbaum CJ, Greenberg R, Schecter AD, Fisher SD. Effects of HIV Infection and Antiretroviral Therapy on the Heart and Vasculature. Circulation. 2008;118(2):36–40.
[15] Manner IW, Trøseid M, Oektedalen O, Baekken M, Os I. Low Nadir CD4 Cell Count Predicts Sustained Hypertension in HIV-Infected Individuals. J Clin Hypertens. 2013;15(2):101–6.
[16] Isomaa B, Almgren P, Tuom T. Cardiovascular Morbidity and Mortality. Diabetes Care. 2001;24(4):683–9.
[17] Crane HM, van Rompaey SE, Kitahata MM. Antiretroviral medications associated with elevated blood pressure among patients receiving highly active antiretroviral therapy. Aids. 2006;20(7):1019–26.
[18] Farhangi MA, Keshavarz SA, Eshraghian M, Ostadrahimi A, Saboor-Yaraghi Dr. AA. White blood cell count in women: Relation to inflammatory biomarkers, haematological profiles, visceral adiposity, and other cardiovascular risk factors. J Health Popul Nutr. 2013;31(1):58–64.
[19] Rodolphe Thiébaut, Wafaa M El-Sadr, Nina Friis-Møller Rickenbach, Martin PR, Antonella, Monforte6 D, 7 LM, 8 EF, 9 OK, et al. Predictors of hypertension and changes of blood pressure in HIV-infected patients. Antivir Ther. 2005;10(7):811–23.
[20] Bosu WK, Aheto JMK, Zucchelli E, Reilly ST. Determinants of systemic hypertension in older adults in Africa: A systematic review. BMC Cardiovasc Disord. 2019;19(1).
[21] Girum T, Yasin F, Wasie A, Shumbej T, Bekele F, Zeleke B. The effect of “universal test and treat” program on HIV treatment outcomes and patient survival among a cohort of adults taking antiretroviral treatment (ART) in low-income settings of Gurage zone, South Ethiopia. AIDS Res Ther [Internet]. 2020;17(1):1–9. Available from: https://doi.org/10.1186/s12981-020-00274-3.
[22] Sample Size Calculator by Raosoft, Inc. [Internet]. Available from: http://www.raosoft.com/samplesize.html.
[23] Kwarisiima D, Balzer L, Heller D, Kotwani P, Chamie G, Clark T, et al. Population-based assessment of hypertension epidemiology and risk factors among HIV-positive and general populations in rural Uganda. PLoS One. 2016;11(5):1–11.
[24] Benzekri NA, Seydi M, Doye IN, Toure M, Sy MP, Kiviat NB, et al. Increasing prevalence of hypertension among HIV-positive and negative adults in Senegal, West Africa, 1994-2015. PLoS One. 2018;13(12):1–14.
[25] Peck RN, Shedafa R, Kalluvya S, Downs JA, Todd J, Suthanthiran M, et al. Hypertension, kidney disease, HIV, and antiretroviral therapy among Tanzanian adults: A cross-sectional study. BMC Med. 2014;12(1):1–11.
[26] Brennan AT, Jamieson L, Crowther NJ, Fox MP, George JA, Berry KM, et al. Prevalence, incidence, predictors, treatment, and control of hypertension among HIVpositive adults on antiretroviral treatment in public sector treatment programs in South Africa. PLoS One. 2018;13(10):1–19.
[27] Triant VA, Lee H, Hadigan C, Grinspoon SK. Increased acute myocardial infarction rates and cardiovascular risk factors among patients with human immunodeficiency virus disease. Journal of Clinical Endocrinology and Metabolism. 2007;92(7):2506–12.
[28] Tuoyire, D, & Ayeteh H. gender differences in the association between and hypertension in Ghana. J Biosoc Sci. 2019;51(3):313–34.
[29] Ramezankhani A, Azizi F, Hadaegh F. Associations of marital status with diabetes, hypertension, cardiovascular disease, and all-cause mortality: A long term follow-up study. PLoS One. 2019;14(4):1–15.
[30] Schwandt HM, Coresh J, Hindin MJ. Marital status, hypertension, coronary heart disease, diabetes, and death among African American women and men: Incidence and prevalence in the atherosclerosis risk in communities (ARIC) study participants. J Fam Issues. 2010;31(9):1211–29.
Viewed PDF 1090 51

