Table of Contents - Issue
Recent articles
-
 Causes of Reduced Revenue Generation in Federal Staff Hospital (Fsh) Laboratory; Annex 111 Federal Capital Territory, AbujaAuthor: Bassey, G. MDOI: 10.21522/TIJPH.2013.10.04.Art001
Causes of Reduced Revenue Generation in Federal Staff Hospital (Fsh) Laboratory; Annex 111 Federal Capital Territory, AbujaAuthor: Bassey, G. MDOI: 10.21522/TIJPH.2013.10.04.Art001Causes of Reduced Revenue Generation in Federal Staff Hospital (Fsh) Laboratory; Annex 111 Federal Capital Territory, Abuja
Abstract:
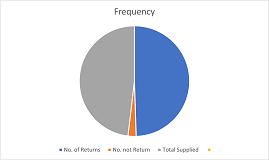
The healthcare delivery system has been criticized for its “culture of blame” in which culpability for failure has been attributed to the human elements of the system: The Study was designed to identify and ascertain reasons for low-revenue generation in Federal staff hospital (FSH) laboratory; annex 111, Abuja and to proffer solutions, as well as deliver health care that minimizes risks and harm to service users, including avoiding preventable injuries and reducing medical errors. According to World Health Organization (WHO), a well-functioning healthcare system requires a financing mechanism, well trained and adequately paid workforce, reliable Information on which to base decisions and policies, and well-maintained health facilities to deliver quality services and technologies. Out of a total number of two hundred (200) respondents interviewed using questionnaires, hundred and sixty (160) were received using the random sampling method. 41% of the respondents believed that there are no barriers to accessing the facility, 48.0% indicated a Lack of Knowledge, and 11.0% said proximity. The year 2017/2018 to 2019 report showed a tremendous improvement. Revenue generated and the number of patients for the year 2018 was to the tune of twenty-nine million, nine hundred and seventy-six thousand, six hundred and sixty naira only (₦29,976,660.00) and twelve thousand, seven hundred and twenty-six patients (12,726) respectively. In comparing the year 2017/2018, respectively, this Study concluded that for overall improvement of the quality and performance in the healthcare environment, there is a need for the development of new inter-organizational patterns of care delivery and complex multitier governance structures.
Keywords: Federal staff hospital (FSH) laboratory, Health care, Knowledge. Preventable injuries, World Health Organization (WHO).Causes of Reduced Revenue Generation in Federal Staff Hospital (Fsh) Laboratory; Annex 111 Federal Capital Territory, Abuja
References:
[1] Carter JY:(1999), Role of laboratory services in health care, The present status in Eastern Africa and recommendations for future. East Afr Med J,73(70) (editorial).
[2] W.C. Cockerham, (2008) B.P. Hinote, in International Encyclopedia of Public Health.
[3] Gemson, G. S., & Kyamru, J. I. (2013). Theory and practice of research methods for the health and social sciences (Rev ed). Jalingo: Livingstone Education Publishing Enterprise (Nig).
[4] Global One Logistics, LLC. (2010). Retrieved from http://www.theymustthinkwerecrazy.com/.
[5] Robert M. Califf, (2018), Principles and Practice of Clinical Research (Fourth Edition).
[6] International Development Research Centre. (2018, July 19). Getting the healthcare basics right for pregnant women in Nigeria. https://www.idrc.ca/en/research-in-action/getting-healthcare-basics-right-pregnant-women-Nigeria.
[7] Rocha, V. (2019), How telehealth can get healthcare to more people. Retrieved June 4, 2020, from weforum.org.
[8] Kassu A, Aseffa A:(1999) Laboratory services in health center within Amhara region, north Ethiopia. East Afr Med J.76(5):239-242.
[9] Abdosh B: (2006) The quality of hospital services in Eastern Ethiopia: patient’s perspective. Ethiop J Health Dev.2006,20(3) :199-200.
[10] TsankovaG. Georgieva E., Kaludova, V, Ermenlieva N. :(2014) Patients Satisfaction with laboratory services at selected medical diagnostic laboratories in Varna. J IMAB. ;20(2):500-501.
[11] Jeffrey R. Balser, William W. Stead, in The Transformation of Academic Health Centers, 2015
[12] Aregbesola, B. S. (2018). Prioritizing Health for the Benefit of the Populace – A Perspective from Nigeria., Global Health, Social Issues, June 15.
[13] Hoyle, David (2005). ISO 9000 Quality Systems Handbook, Fifth Edition. Butterworth-Heinemann. p. 686. ISBN 978-0-7506-6785-2.
[14] http://www.drsforamerica.org/learn/policy-center/healthcare-delivery-system.
[15] Laszeray, Tech, (2019), The importance of quality management systems. 12315 York Delta Drive, North Royalton, OH 44133, inquiry@laszeray.440-517-7822.
[16] Tricker, Ray (2005). ISO 9001:2000 Audit Procedures, Second Edition. Butterworth-Heinemann. p. 320. ISBN 978-0-7506-6615-2.
[17] Dobb, Fred (2004). ISO 9001:2000 Quality Registration Step-by-Step, Third Edition. Butterworth-Heinemann. p. 292. ISBN 978-0-7506-4949-0.
[18] Hoveland I, (2005.) Successful communication: a toolkit for researchers and civil society organizations. Rapid research and policy development; https://www.odi.org/publications/155-successfulcommunication.
[19] Ochei, O.J., Kolhatkar., (2007), Medical Laboratory Science, Theory and Practice, Tata McGraw-Hill Publishing Company Limited, New Delhi, page 111-151.
[20] Hassemer DJ:(2003), Wisconsin State laboratory of Hygiene’s role in clinical laboratory improvement. Wis Med J.102 (6):56-59.
[21] Oja PI, Kouri TT,Pakarinen AJ:(2006), From customer satisfaction survey to corrective actions in laboratory services in a University hospital .Int J Qual Health Care.18(6): 422-428 10.1093/intqhc/mz1050.
Viewed PDF 971 46 -
 Factors Contributing to Lost to Follow up on People Living with HIV, Bor State HospitalAuthor: John Aban Chol NyijokDOI: 10.21522/TIJPH.2013.10.04.Art002
Factors Contributing to Lost to Follow up on People Living with HIV, Bor State HospitalAuthor: John Aban Chol NyijokDOI: 10.21522/TIJPH.2013.10.04.Art002Factors Contributing to Lost to Follow up on People Living with HIV, Bor State Hospital
Abstract:
Long-term regular follows up of ART clients is an important component of HIV care, treatment, and prevention. Clients who are lost to follow-up while on treatment compromise their own health leading to poor treatment outcomes, which has a negative impact on HIV control programs. This study aimed to determine the factors contributing to the lost to follow-up (LTFU) of HIV clients on ARVs at the ART clinic, Bor state hospital. A retrospective cohort study of 60 people living with HIV from 576 clients who are lost to follow-up and attending an ART clinic service between Jan. 2015 - Dec. 2019 was undertaken. LTFU was defined as not taking an ARVs drug refill for a period of three months or longer from the last attendance for refill and not yet classified as ‘died’ or ‘transferred out. A total of 1993 clients enrolled at the HIV ART clinic, a total of 576 clients (29.0%) were defined as LTFU from enrolled clients, and 1417 clients (71.0%) were actively being followed up and on ART in the HIV ART clinic. Overall, these data suggested that LTFU in this study was high in patients who were married, low level of education, stigma-related factors, unemployment among clients, and clinical stages I &II were associated with LTFU in this study.
Keywords: Anti-retroviral therapy, ART, factors contributed to lost to follow up, HIV, lost to follow up, PLHIV, South Sudan.Factors Contributing to Lost to Follow up on People Living with HIV, Bor State Hospital
References:
[1] atilda K, Esther B, Joy K, et al. Loss to Follow-Up among HIV Positive Pregnant and Lactating Mothers on Lifelong Anti-retroviral Therapy for PMTCT in Rural Uganda.
[2] Bryan E. Shepherd, Meridith B, Lara M. E. Vaz, et al. Impact of Definitions of Loss to Follow-up on Estimates of Retention, Disease Progression, and Mortality: Application to an HIV Program in Mozambique, American Journal of Epidemiology, Volume 178, Issue 5, 1 September 2013, Pages 819–828, https://doi.org/10.1093/aje/kwt030.
[3] Chi BH, Yiannoutsos CT, Westfall AO, et al. (2011) Universal Definition of Loss to Follow-Up in HIV Treatment Programs: A Statistical Analysis of 111 Facilities in Africa, Asia, and Latin America. PLoS Med 8(10): e1001111. https://doi.org/10.1371/journal.pmed.1001111.
[4] Opio, D., Semitala, F.C., Kakeeto, A. et al. Loss to follow-up and associated factors among adult people living with HIV at public health facilities in Wakiso district, Uganda: a retrospective cohort study. BMC Health Serv Res 19, 628 (2019). https://doi.org/10.1186/s12913-019-4474-6.
[5] Faraz A, Gideon M, Joseph S. et al. Identifying and Reengaging Patients Lost to Follow-Up in Rural Africa: The “Horizontal” Hospital-Based Approach in Uganda. Global Health: Science and Practice March 2019, 7(1):103-115; https://doi.org/10.9745/GHSP-D-18-00394.
[6] Williams H, Filbert F, Brouno P. et al. Lost to follow up and clinical outcomes of HIV adult patients on anti-retroviral therapy in care and treatment centers in Tanga City, north-eastern Tanzania. Tanzania Journal of Health Research Doi: http://dx.doi.org/10.4314/thrb.v14i4.3 Volume 14, Number 4, October 2012.
[7] MOH. Fact sheet on the Uganda Population HIV Impact Assessment [Internet]. WHO | Regional Office for Africa. 2017 [cited 2018 Aug 21]. Available from: https://www.afro.who.int/publications/fact-sheet-ugandapopulation-hiv-impact-assessment.
[8] Bior, Awak Deng. HIV/AIDS: A Threat to National Security in South Sudan. Sudd Institute, 2014, www.jstor.org/stable/resrep11027 Accessed 26 July 2020.
[9] Opio, D., Semitala, F.C., Kakeeto, A. et al. Loss to follow-up and associated factors among adult people living with HIV at public health facilities in Wakiso district, Uganda: a retrospective cohort study. BMC Health Serv Res 19, 628 (2019). https://doi.org/10.1186/s12913-019-4474-6.
[10] Kiwanuka J, Mukulu Waila J, Muhindo Kahungu M, et al. Determinants of loss to follow-up among HIV positive patients receiving anti-retroviral therapy in a test and treat setting: A retrospective cohort study in Masaka, Uganda. PLoS One. 2020; 15(4): e0217606. Published 2020 Apr 7. doi: 10.1371/journal.pone.0217606.
[11] Geng EH, Bangsberg DR, Musinguzi N, et al. Understanding reasons for and outcomes of patients lost to follow-up in anti-retroviral therapy programs in Africa through a sampling-based approach. J Acquir Immune Defic Syndr. 2010; 53(3):405-411. doi:10.1097/QAI.0b013e3181b843f0.
[12] Vervölgyi, E., Kromp, M., Skipka, G. et al. Reporting of loss to follow-up information in randomised controlled trials with time-to-event outcomes: a literature survey. BMC Med Res Methodol 11, 130 (2011). https://doi.org/10.1186/1471-2288-11-130.
[13] Frédérique C, Kathrin Z, Olivia K, et al. Outcomes of Patients Lost to Follow-up in African Antiretroviral Therapy Programs: Individual Patient Data Meta-analysis, Clinical Infectious Diseases, Volume 67, Issue 11, 1 December 2018, Pages 1643–1652, https://doi.org/10.1093/cid/ciy347.
[14] Zürcher K, Mooser A, Anderegg N, et al. Outcomes of HIV-positive patients lost to follow-up in African treatment programmes. Trop Med Int Health. 2017; 22(4):375-387. doi:10.1111/tmi.12843In.
[15] Kaplan S, Nteso KS, and Ford N, et al. Loss to follow-up from anti-retroviral therapy clinics: A systematic review and meta-analysis of published studies in South Africa from 2011 to 2015. South Afr J HIV Med. 2019; 20(1):984. Published 2019 Dec 18. doi:10.4102/sajhivmed. v20i1.984in 16 –.
[16] Goggin K, Hurley EA, Staggs VS, et al. Rates and Predictors of HIV-Exposed Infants Lost to Follow-Up during Early Infant Diagnosis Services in Kenya. AIDS Patient Care STDS, 33(8):346-353, 01 Aug 2019.
[17] World Health Organisation (2008), Mortality of Patients Lost to follow-up in Antiretroviral Treatment Programs in Resource limited setting. System review and Meta-Analysis. Available at (www.plosone.org/./info:doi/2F10.137).
[18] World Health Organisation (2008), Lost opportunity to complete CD4+ Lymphocytes testing among patients who tested positive for HIV in South Africa. Lost Opportunities to initiate HIV Care in South Africa. Available at (www.who.int/bulletin/volumes/88/9/09-068981.pdf).
[19] Center for Disease Control and Prevention CDC (2015), How HIV passed from one person to another. Available at (www.cdc.gov/hiv/./qa/transimissi).
[20] PLHIV (2010), Publication for People Living with HIV/AIDS. Available at (www.nephark.org).
[21] Rebecca Hodes, nam-aidmap(2010). Lost to follow-up health system failure, not patients to blame. 8th International AIDS Conference, 29th July 2010. Available at (www.aidsmap.com/loss-to-follow-up-he).
[22] Wikipedia, the free encyclopedia (2011), HIV in general. Available at (http://en.wikipedia.org/wiki/Hiv).
[23] Joint United Nations Program on HIV/AIDS (2006, 2010, 2011). Overview of the global AIDS Epidemic. UN Report on the Global AIDS epidemic. Available at (www.unaids.org/globalreport/global).
[24] International HIV/AIDS charity (2011). Averting HIV/AIDS. Available at (www.avert.org/world-aids-day.htm).
[25] Geng EH, Bangsberg DR, MUSNGUZIN (2009). Understanding reasons for and outcomes of patients lost to follow-up in anti-retroviral therapy programs in Africa through a sampling-based approach. J Acquir Immune Defic. Syndr. 2009 Sept.10.
[26] Lessels, R.J.; Mutevendzi, P.C.; Cooke, G.S.; Nowel M.L.; Retention in HIV Care for individuals not yet eligible for anti-retroviral therapy: rural KwanZulu-Natal, South Africa. J Acquir Immune Defic. Syndr 2010.
[27] Paula Braitsein (2010). XVIII International AIDS Conference of 2010. Available at (www.aids2010.org/).
[28] Cohort profile: The International epidemiological databases to evaluate AIDS (IeDEA) in Sub-Saharan Africa. Int J. Epidemiol (2011): dyr080vldy08.
[29] Amref ART hub (2011). Definition of LTFU in Pre-ART and ART. Amref ART knowledge Hub. Available at (www.hub.amref.org/index.php).
[30] Dr. Benjamin H.C.; Ronald A.C.; Albert M.; Andrew O.; Westfall.; Wilbrand M.; Mohammed L.; Lloyd B.M.; Stenttet V.; Jeffrey S.A.; A.M J Epidemiol.2010 April 15;171(8):924-931. Published online 2010 March. 10. d0i:10.1093 /aje/kw9008.
[31] Gilles V.C.; Nathan F.; Katherine H.; Eric G.; Shaheed M.; David C.; Andrew B.: PLOS ONE (2011). vol.6, issue 2; Published online 2011. Public library of science pg 9 doi: 10.1371/journal.pone.0014684. Available at (www.embase.com).
Viewed PDF 911 85 -
 Utilization of Community-Based Health Insurance among Residence of Katsina State, NigeriaAuthor: Yahaya Shamsuddeen SuleimanDOI: 10.21522/TIJPH.2013.10.04.Art003
Utilization of Community-Based Health Insurance among Residence of Katsina State, NigeriaAuthor: Yahaya Shamsuddeen SuleimanDOI: 10.21522/TIJPH.2013.10.04.Art003Utilization of Community-Based Health Insurance among Residence of Katsina State, Nigeria
Abstract:
Enrollment into any form of insurance is very low in Katsina State, with most people paying out of pocket for health care. The utilization of community-based health insurance will provide financial risk protection and improve health outcomes. The objective of the study is to compare differences in Utilization between community-based health insurance member households and non-member households and to identify factors associated with the utilization. A comparative cross-sectional descriptive study was conducted among household heads in Katsina State, Nigeria. Targeted participants were selected using multistage sampling techniques. Primary data was generated using Open Data Kit (ODK), which was later downloaded and exported to SPSS version 20® for statistical analysis. Mean, and standard deviation from the mean (Mean ± SD) were used to study population characteristics towards utilization of CHI. The statistical significance level of analyzed variables were accepted at P≤0.05. The mean age of respondents was 46.82±13 and 44±12.5 years for CBHI enrolled and non-ensured groups, respectively. Heads of the households were predominantly males and currently married, with 97.3% and 93.3% for CBHI members compared to 82.7% and 99.3% of non-member households, respectively. The enrolled CBHI group utilizes PHC services more than the non-enrolled group(p<0.05) with age, marital status, education, number of children, and distance to health facilities all associated with Utilization. Utilization of CBHI was higher among enrolled groups than non-enrolled groups. Many factors, such as age, marital status, education level, and Payment of transportation to the facility, affect utilization of these services. We recommend CBHI be expanded, poor and vulnerable groups are given special consideration, and people not enrolled should be encouraged to join.
Keywords: Community, Comparative, Health, Insurance, Utilization.Utilization of Community-Based Health Insurance among Residence of Katsina State, Nigeria
References:
[1] Carrin, G. (2003). Community-based Health Insurance Schemes in Developing Countries; facts, problems, and perspectives. World Health Organization, Geneva.
[2] The World Health Report; Health System Financing; The Path to Universal Coverage, 2010, http://www.who.int/whr/2010/whr10_en.pdf Accessed 2 nd August 2020.
[3] WHO 2020 Community-Based Health insurance Scheme. https://www.who.int/news-room/factsheets/detail/community-based-health-insurance2020.
[4] Onwujekwe.O, Valenyi. E. Feasibility of voluntary health insurance in Nigeria. 2006. The World Bank.
[5] National Bureau of Statistics (NBS) and United Nations Children’s Fund (UNICEF). 2017 Multiple Indicator Cluster Survey 2016-17, Survey Findings Report. Abuja, Nigeria; National Bureau of Statistics and United Nations Children’s Fund.
[6] Nasiru, L., Mohammed, T.S., Hassan, A., Shamsuddeen, Y (2021). Health Care Access and Utilization among Households in Katsina State North-western, Nigeria. International Journal of Tourism and Hotel Management; 2641-6948.
[7] Yahaya S.S, Mustapha M, , Lawal N , Runka JY. Knowledge of Community Based Health Insurance among Residence of Katsina State, Nigeria; A Comparative Cross-Sectional Study. Texila International Journal of Academic Research Special Edition Apr 2022.
[8] Araoye MO. Research Methodology with Statistics for Health and Social Sciences, first edition. Nathadex publishers Ilorin, 2004;25- 120.
[9] Gnawali DP, Pokhrel S, Sié A, Sanon M, De Allegri M, Souares A, Dong H, Sauerborn R. The effect of community-based health insurance on the utilization of modern health care services; evidence from Burkina Faso. Health Policy. 2009 May;90(2-3);214-22. doi; 10.1016/j.healthpol.2008.09.015. Epub 2008 Nov 25. PMID; 19036467.
[10] Asmamaw Atnafu Tsegaye Gebremedhin. Community-Based Health Insurance Enrollment and Child Health Service Utilization in Northwest Ethiopia; A Cross-Sectional Case Comparison Study. Clinico Economics and Outcomes Research 2020;12.
[11] Atnafu A, Gebremedhin T. Community-Based Health Insurance Enrolment and Child Health Service Utilization in Northwest Ethiopia; A Cross-Sectional Case Comparison Study. Clinicoecon Outcomes Res. 2020 Aug 10;12;435-444. doi; 10.2147/CEOR.S262225. PMID; 32848434; PMCID; PMC7428314.
[12] Sarah Alkenbrack, Magnus Lindelow. The impact of community-based health insurance on utilization and out-of-pocket expenditures in Lao People’s Democratic Republic. Health Econ. 2015 Apr;24(4);379-99.
[13] Bayked EM, Kahissay MH,Workneh BD. Factors affecting the uptake of community-based health insurance in Ethiopia; a systematic review. Int J Sci Rep 2021;7(9);459-67. (5) (PDF) Factors affecting community based health insurance utilization in Ethiopia; A systematic review. Available from: https;//www.researchgate.net/publication/340193552_Factors_affecting_community_based_health_insurance_utilization_in_Ethiopia_A_systematic_review [accessed May 20 2022].
Viewed PDF 2167 73 -
 Assessment of the Nutritional Status of Babies with Neonatal Jaundice in GhanaAuthor: Frederick AdiibokaDOI: 10.21522/TIJPH.2013.10.04.Art004
Assessment of the Nutritional Status of Babies with Neonatal Jaundice in GhanaAuthor: Frederick AdiibokaDOI: 10.21522/TIJPH.2013.10.04.Art004Assessment of the Nutritional Status of Babies with Neonatal Jaundice in Ghana
Abstract:
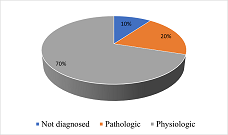
Neonatal jaundice is a public health concern responsible for a relatively high rate of infant morbidity and mortality. Therefore, it is prudent to put in place effective risk-reduction strategies and detect and treat new born jaundice effectively. Optimum nutrition has been shown to be crucial to health and well-being. This study, therefore, sought to investigate the nutritional status of babies that report to three referral hospitals in Ghana (Korle-bu Teaching Hospital, Greater Accra Regional Hospital and the Tamale Teaching hospital). It was a multi-center nested, case-control study involving 120 cases and 120 controls of neonates in the three referral hospitals in Ghana. The study revealed that babies with neonatal jaundice in Ghana mostly have a normal nutritional status, even though they lose about 5% of their birth weight. More mothers of healthy babies (88.3%) did exclusive breastfeeding, compared with mothers of babies with neonatal jaundice (76.7%). It was also revealed that the three referral hospitals implemented the Baby Friendly Hospital Initiative’s ten steps to successful breastfeeding as a measure to prevent suboptimal feeding, which could lead to an increase in bilirubin levels. Assessment and interventions to prevent weight loss should therefore be paramount for babies with neonatal jaundice.
Keywords: Malnutrition, Neonatal jaundice.Assessment of the Nutritional Status of Babies with Neonatal Jaundice in Ghana
References:
[1] Wickström, R., Skiöld, B., Petersson, G., Stephansson, O., Altman, M. (2018). Moderate neonatal hypoglycemia and adverse neurological development at 2-6 years of age. European Journal of Epidemiology, 33, 1011–1020.
[2] American Academy of Pediatrics (2004). Management of hyperbilirubinemia in the new-born infant 35 or more weeks of gestation. Subcommittee on Hyperbilirubinemia. Pediatrics, 114(1), 297-316.
[3] Hoynes, H., Schanzenback, D.W. & Almond, D. (2016). Long-run impacts of childhood access to the safety net. American Economic Review, 106(4), 903-934.
[4] Radhakrishnan, K. (2015). Vitamin D deficiency in children: Is your child getting enough? U.S. News & World Report. Retrieved from: http://health.usnews.com/health-news/patient-advice/articles/2015/11/06/vitamin-d-deficiency-in-children.
[5] Benson, S.L.J., Thompson, M. (2016). Nutrition assessment. Academy of Nutrition and Dietetics Pocket Guide to Neonatal Nutrition, 2nd Edn. Chicago. Pp. 1-31.
[6] Leppanen, M., Lapinleimu, H., Lind, A., et al. (2014). Antenatal and postnatal growth and 5-year cognitive outcome in very preterm infants. Pediatrics, 133(1), 63-70. doi: 10.1542/peds.2013-1187.
[7] Corkins, M.R. (2017). Why is diagnosing pediatric malnutrition important? Nutrition Clinical Practice, 32(1), 15-18. doi: 10.1177/0884533616678767.
[8] Mehta S, Kumar P, Narang A. (2005). A randomized controlled trial of fluid supplementation in term neonates with severe hyperbilirubinemia. Journal of Pediatrics, 147(6), 781-785.
[9] Weng, Y., Chiu, Y., Cheng, S. (2012). Breast Milk Jaundice and Maternal Diet with Chinese Herbal Medicines. Evidence-Based Complementary and Alternative Medicine. Retrieved from https://www.hindawi.com/journals/ecam/2012/150120/ on 18th April 2017.
[10] Wilde, V.K. (2021). Breastfeeding Insufficiencies: Common and Preventable Harm to Neonates. Cureus, 13(10), e18478. doi:10.7759/cureus.18478.
[11] Metcoff, J. (1994). Clinical assessment of nutritional status at birth. fetal malnutrition and SGA are not synonymous. Pediatric Clinical North America, 41(5), 875-91.
[12] Althomali, R., Aloqayli, R., Alyafi, B., Nono, A., Alkhalaf, S., Aljomailan, A., et al. (2018). Neonatal jaundice causes and management. International Journal of Community Medicine and Public Health, 5, 4992-6.
[13] Academy of Breastfeeding Medicine (ABM) (2017). ABM Clinical Protocol #22: Guidelines for Management of Jaundice in the Breastfeeding Infant 35 Weeks or More of Gestation. Vol., 12, No. 5. DOI: 10.1089/bfm.2017.29042.vjf.
[14] Koletzko, B. (2015). Pediatric Nutrition in Practice; World Review Nutrition Dietetics: Basel, Karger. Volume 113, pp. 139–146.
[15] Hunt, L., Ramos, M., Helland, Y., Lamkin, K. (2020). Decreasing neonatal jaundice readmission rates through implementation of a jaundice management guide. BMJ Open Qual, 9, 1.
[16] Bolajoko, O. Olusanya, M., Kaplan, T., Hansen W. R, (2018). Neonatal hyperbilirubinaemia: a global perspective. Lancet Child Adolescent Health 4642(18), 30139-1 Retrieved on 4th June 2021 from http://www.thelancet.com/child-adolescent.
[17] Pagana, K.D., Pagana, T.J., Pagana, T.N. (2019). Mosby’s Diagnostic and Laboratory Test Reference. 14th ed. Mo: Elsevier, St. Loius.
[18] Escobar, G., Gonzales, M., Armstrong, M.A., Folck, B.F., Xiong, B., Newman, T.B. (2002). Rehospitalisation for neonatal dehydration: A nested case-control study. Arch Pediatric Adolescent Medicine, 156, 155-161.
[19] Boo N.Y. and Lee, H.T. (2002). Randomized controlled trial of oral versus intravenous fluid supplementation on serum bilirubin level during phototherapy of term infants with severe hyperbilirubinaemia. Journal of Paediatric Child Health, 38(2), 151-155.
[20] Thornton, P.S., Stanley, C.A., De Leon, D.D, et al. Recommendations from the pediatric endocrine society for evaluation and management of persistent hypoglycemia in neonates, infants, and children. Journal of Pediatrics, 2015;167:238–245.
Viewed PDF 1194 40 -
 Managing Municipal Solid Waste Issues; Sources, Composition, Disposal, Recycling, and Volarization, Chililabombwe District, ZambiaAuthor: Gift SakanyiDOI: 10.21522/TIJPH.2013.10.04.Art005
Managing Municipal Solid Waste Issues; Sources, Composition, Disposal, Recycling, and Volarization, Chililabombwe District, ZambiaAuthor: Gift SakanyiDOI: 10.21522/TIJPH.2013.10.04.Art005Managing Municipal Solid Waste Issues; Sources, Composition, Disposal, Recycling, and Volarization, Chililabombwe District, Zambia
Abstract:
Solid waste continues to pose important challenges to our environment on a daily basis. Insufficient solid waste management systems and equipment have contributed to the alteration to the ecosystems, including water, air, and soil pollution that infringes on the health of the general public that is associated with health ailments like cholera and other food and water borne diseases. Chililabombwe district’s face has continued to be dented with the unkempt environment with littered solid waste that has become a stinging and widespread challenge, especially in the urban areas of the district. Solid waste (SW) collection and working disposal systems are the major problems of the urban environment in most developing countries worldwide. MSW management solutions are financially dependable for the technical viable, socially inclement, and legally accepted. Solid waste management remained the biggest challenge that all the local authorities in Zambia and many developing countries in Africa. Commercialization or valorization of organic food waste was one of the important research areas that could combat the increased solid waste in the environmental causing environmental degradation. The objective of this study was to address matters that would respond positively to the waste management crisis in the district. As waste continues to be accumulated, with its high generation, more technologies are sought in the area of treatment and exploitation of organic and municipal waste through composting and anaerobic digestion in the management of waste. The lack of technologies and machinery has equally downplayed the essence of waste management in the Chililabombwe district.
Keywords: Anaerobic, Digestion, Landfill, Organic, Solid wastes, Valorization.Managing Municipal Solid Waste Issues; Sources, Composition, Disposal, Recycling, and Volarization, Chililabombwe District, Zambia
References:
[1] Ayomoh M, Oke S, Adedeji W and Charles-Owaba O (2008) An approach to tackling the environmental and health impacts of municipal solid waste disposal in developing countries. Journal of Environmental Management 88(1); 108–114.
[2] McDougall, F., White, P., Franke, M., & Hindle, P. (2011). Integrated Solid Waste Management, A Life-Cycle Inventory. London; Blackwell Science.
[3] Environmental Management Act (No.12 of 2011 section 56(1)(a)(b) &(c) of the Laws of Zambia.
[4] GRZ. (2017). Environmental Management and Coordination (Waste management Regulations). Lusaka; GRZ.
[5] BlaserF.Schluep.M.2012E-waste. Economic Feasibility of e-Waste Treatment in Tanzania Final Version, March 2012. EMPA Switzerland & UNIDO.
[6] Wilson D.C et al.,2010Comparative Analysis of Solid Waste Management. In Cities Around the World. Paper Delivered at the UK Solid Waste Association, Nov.2010.
[7] Okot-OkumuJ.NyenjeR.2011 Municipal solid waste management under decentralisation in Uganda.” Habitat International 35, 537.
[8] Sarkhel, P. & S. Banerjee. 2009. Municipal solid waste management, source-separated waste, and stakeholder’s attitude; a contingent valuation study. Environment, Development, and Sustainability.
[9] Macawife, J. & G. S. Su. 2009. Local government officials’ perceptions and attitudes towards solid waste management in Dasmarinas, Cavite, Philippines. Journal of Applied Sciences in Environmental Sanitation 4; 63-69.
[10] Sharholy, M., Ahmad, K., Mahmood, G., and Trivedi, R.C. (2008) Municipal Solid Waste Management in Indian Cities. Waste Management, 28, 459-467. https://dx.doi.org/10.1016/j.wasman.2007.02.008.
[11] Antipolis S (2000) Syria profile. In Policies and Institutional Assessment of Solid Waste Management in Five Countries. Blue Plan Regional Activity Centre, Valbonne, France.
[12] Al-Khatib IA, Arafat HA, Basheer T et al. (2007) Trends and problems of solid waste management in developing countries; a case study in seven Palestinian districts. Waste Management 27(12); 1910–1919.
[13] Bandara NJ, Hettiaratchi JPA, Wirasinghe S and Pilapiiya S 2007 Relation of waste generation and composition to socio-economic factors; a case study. Environmental Monitoring and Assessment 135(1–3); 31–39.
[14] Al-Khatib IA, Monou M, Zahra ASFA, Shaheen HQ and Kassinos D (2010) Solid waste characterization, quantification, and management practices in developing countries. A case study; Nablus district–Palestine. Journal of Environmental Management 91(5); 1131–1138.
[15] C. Zurbrugg, S. Drescher, I. Rytz, A. H. M. M. Sinha, and I. ¨ Enayetullah, “Decentralised composting in Bangladesh, a win-win situation for all stakeholders,” Resources, Conservation and Recycling, vol. 43, no. 3, pp. 281–292, 2005.
[16] Mbewe, R., & Mundia, Y. (2012). National Study on Health Care waste, Ministry of Health. Lusaka; CBoH.
[17] Asase M, Yanful EK, Mensah M, Stanford J and Amponsah S (2009) Comparison of municipal solid waste management systems in Canada and Ghana; a case study of the cities of London, Ontario, and Kumasi, Ghana. Waste Management 29 (10); 2779–2786.
[18] Nthambi, M. (2013). An Economic Assessment of Household Solid Waste Management Options; The Case of Kibera Slum, Nairobi City, Kenya. Nairobi; University of Nairobi.
[19] Al-Yousfi B (2004) Sound Environmental Management of Solid Waste – the Landfill Bioreactor. United Nations Environmental Programme – Regional Office for West Asia, Manama, Bahrain
[20] Nyang’echi, G. N. (2012). Management of Solid and Liquid wastes. A Manual for Environmental Health Workers. African Medical Research Foundation.
[21] GRZ. (2011). Ministry of Planning, National Development and Vision 2030 Progress Report. Lusaka; GRZ.
[22] Almasri R, Muneer T and Cullinane K (2011) The effect of transport on air quality in urban areas of Syria. Energy Policy 39(6); 3605–3611.
[23] L. Dahlén Household Waste Collection Factors and Variations, Department of Civil, Mining and Environmental Engineering Division of Waste Science.
[24] Calo F and Parise M (2009) Waste management and problems of groundwater pollution in karst environments in the context of a post-conflict scenario; the case of Mostar (Bosnia Herzegovina). Habitat International 33(1); 63–72.
[25] Batool SA and Ch MN (2009) Municipal solid waste management in Lahore city district, Pakistan. Waste Management 29(6); 1971–1981.
[26] U.S. Environmental Protection Agency, Wastes – Non-Hazardous Waste – Municipal Solid Waste, 1200 Pennsylvania Ave., N. W. Washington, DC 20460, U.S.A. (2013).
[27] S. H. Swan, “Environmental phthalate exposure in relation to reproductive outcomes and other health endpoints in humans,” Environmental Research, vol. 108, no. 2, pp. 177–184, 2008.
[28] M. P. Velez, T. E. Arbuckle, and W. D. Fraser, “Female exposure ´ to phenols and phthalates and time to pregnancy; The Maternal-Infant Research on Environmental Chemicals (MIREC) study,” Fertility and Sterility, vol. 103, no. 4, pp. 1011.e2–1020.e2, 2015.
[29] I.A. Al-Khatib M. Monou S.F. Abdul Q.S. Hafez K. Despo Solid waste characterization, quantification, and management practices in developing countries. A case study Nablus district – Palestine 2010.
[30] Mashamba, S. M. (2015). Slum Development; A Manifestation on the failed public housing delivery system, Lusaka; Department of Physical Planning and Housing, Zambia.
[31] Laner, D., Fellner, J., Brunner, & P.H. (2009a). Flooding of municipal solid waste landfills - An environmental hazard? Science of the Total Environment, 407, 3674–3680. https://doi.org/10.1016/j.scitotenv.2009.03.006.
[32] Chalmin P and Gaillochet C (2009) From Waste to Resource, an Abstract of World Waste Survey 2009. Cyclope, Veolia Environmental Services, Edition Economica, Aubervilliers, France.
[33] Chowdhury M (2009) Searching quality data for municipal solid waste planning. Waste Management 29(8); 2240–2247.
[34] Kumar, H. D. (2008). Environmental Pollution and Waste Management. MD Publications Ltd.
[35] Larkin, G. R. (2014). Public-private partnerships in economic development; A review of theory and practice. Economic Development Review, 7-9.
[36] Williams, P.W., ed., 1993, Karst Terrains, Environmental Changes and Human Impact; Cremingen-Destedt, Germany, Catena Supplement no. 25, 268 p.
Viewed PDF 1495 73 -
 Systemic Effects on Access to and Utilization of Quality Contraceptive Services by Women of Reproductive age During Covid-19 Pandemics in Oyo State, NigeriaAuthor: Esther OyewoDOI: 10.21522/TIJPH.2013.10.04.Art006
Systemic Effects on Access to and Utilization of Quality Contraceptive Services by Women of Reproductive age During Covid-19 Pandemics in Oyo State, NigeriaAuthor: Esther OyewoDOI: 10.21522/TIJPH.2013.10.04.Art006Systemic Effects on Access to and Utilization of Quality Contraceptive Services by Women of Reproductive age During Covid-19 Pandemics in Oyo State, Nigeria
Abstract:
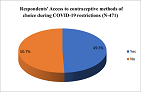
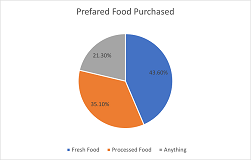
The indirect health impacts include diversion or depletion of resources to provide routine care and decreased access to routine care resulting from an inability to travel due to restriction, fear, or other factors. This paper presents the findings of a cross-sectional quantitative study exploring systemic effects on access to and utilization of quality contraceptive services by women of reproductive age during the Covid-19 pandemic in Oyo State, Nigeria. A purposive sampling technique was used to select 471 users of users of MNCH services (postnatal clinic and family planning services and immunization uptakes) that responded to 43 structured questionnaires that included socio-demographical characteristics, knowledge of contraceptive products and service availability, contraceptive supplies, access and utilization, health system opportunities and challenges amidst Covid-19 pandemics. Of the 471 respondents, the mean age of respondents was 29.63± 3.29years, with (34.2%) within 26-30 years age group. Majorly self-employed/business (74.9%), (91.1%) Yorubas ethnicity. Only 49.2% accessed contraceptive services during restrictions; due to overwhelming fear of Covid-19 by (31.7%), and disruption of services (31.1%). Others mentioned cost, restriction in movement, and difficulty in seeing caregivers. With 65.4% of the total respondents currently obtained a method with easy in restrictions. The Chi-square test, on the relationship between respondents’ access to and utilization of contraceptive services with systemic factors shows a significant relationship with p =0.004 during the pandemic. It becomes highly imperative that the family planning program be redesigned to improve the health system as part of the preparedness measures to address gaps due to the Covid-19 restrictions.
Keywords: Access and Utilization, Contraceptives, Covid-19 Pandemic, Effects, Systemic.Systemic Effects on Access to and Utilization of Quality Contraceptive Services by Women of Reproductive age During Covid-19 Pandemics in Oyo State, Nigeria
References:
[1] Zulu JM, et al, 2015. Innovation in health service delivery: integrating community health assistants into the health system at the district level in Zambia. BMC Health Serv Res. 2015;15(1):1.
[2] Schneider H, Lehmann U, 2016. From Community Health Workers to Community Health Systems: Time to Widen the Horizon? Health Syst Reform;2(2):112–8.
[3] Vinit Sharma et al., 2020Why the Promotion of Family Planning Makes More Sense Now Than Ever Before? First Published August 5, 2020, https://doi.org/10.1177/0972063420935545.
[4] Purdy C, 2020. Opinion: How will Covid-19 affect global access to contraceptives—and what can we do about it? Devex, https://www.devex.com/news/sponsored/opinion-how-will-covid-19-affect-global-access-to-contraceptives-and-what-can-we-do-about-it-96745.
[5] Marie Stopes International,2020. Stories from the frontline: in the shadow of the Covid-19 pandemic, https://www.mariestopes.org/covid-19/stories-from-the-frontline.
[6] International Planned Parenthood Federation, 2020. Covid-19 pandemic cuts access to sexual and reproductive healthcare for women around the world, 2020, https://www.ippf.org/news/covid-19-pandemic-cuts-access-sexual-and-reproductive-healthcare-women-around-world.
[7] Falcone R E, Detty A. 2015. “The Next Pandemic: Hospital Response.” Emergency Medical Reports 36 (26): 1–16.
[8] International Federation of Gyanecology and Obsteric, 2020. Covid-19 Contraception and Family Planning: Contraceptive and Family Planning services and supplies are CORE components of essential health services, and access to these services is a fundamental human right.
[9] Guanjian Li, Dongdong Tang et al., 2020: Impact of the Covid-19 Pandemic on Partner Relationships and Sexual and Reproductive Health: Cross-Sectional, Online Survey Study, Published on 6.8.2020 in Vol 22, No 8 (2020).
[10] Kavita Nanda, et al, 2020. Contraception in the Era of Covid-19, Glob Health Sci Pract. 2020 Jun 30; 8(2): 166–168. Published online 2020 Jun 30. Doi: 10.9745/GHSP-D-20-00119 PMCID: PMC7326510, PMID: 32312738.
[11] Weinberger M, Hayes B, et al., 2020: Doing things differently: what it would take to ensure continued access to contraception during Covid-19. Glob Health Sci Pract, 8, pp. 169-175.
[12] Modupe Taiwo, et al, 2020. Gendered Impact of Covid-19 on the Decision-Making Power of Adolescents in Northern Nigeria, Save the Children Nigeria.
[13] Kantorová V, et al.,2020 Estimating progress towards meeting women’s contraceptive needs in 185 countries: A Bayesian hierarchical modelling study. PloS Med 17(2): e1003026. https://journals.plos.org/plosmedicine/articleid=10.1371/journal.pmed.1003026.
[14] United Nations, Department of Economic and Social Affairs, Population Division, 2019. Family Planning and the 2030 Agenda for Sustainable Development. New York: United Nations.
[15] WHO, 2007. Maternal mortality in 2005; Estimates Developed by WHO, UNICEF, UNFPA, and The World Bank, WHO, Geneva 2007.
[16] Lule E, et al., 2007. Fertility regulation behavior and their costs: contraception and unintended pregnancies in Africa and Eastern Europe and Central Asia. Washington: World Bank; 2007.
[17] Kayode Afolabi, 2020. Sustaining FP & Sexual Reproductive Reproductive Health Services Delivery amidst Covid-19 Pandemic, Director/Head RH Division, Federal Ministry of Health.
[18] Aishat Bukola Usman, Olubunmi Ayinde, et al, 2020. Epidemiology of Corona Virus Disease 2019 (Covid-19) Outbreak Cases in Oyo State, Southwest Nigeria March -April 2020. DOI:10.21203/rs.3.rs-29502/v1.
[19] National Population Commission (NPC) [Nigeria] and ICF. 2019. Nigeria Demographic and Health Survey 2018. Abuja, Nigeria, and Rockville, Maryland, USA A: NPC and ICF.
[20] Ezugwu EC, Nkwo PO, Agu PU, Ugwu EO, Asogwa AO, 2014. Contraceptive use among HIV-positive women in Enugu, southeast Nigeria. Int J Gynaecol Obstet 2014; 126:14-7.
[21] USAID, 2020. Monitoring Covid-19’s Effects on Family Planning: What Should We Measure?
[22] FP2020, Measurement, no date, http://progress.familyplanning2020.org/measurement.
[23] Michelle Weinberger et al, 2020: Doing Things Differently: What It Would Take to Ensure Continued Access to Contraception During Covid-19. Global Health: Science and Practice, 8(2):169-175; https://doi.org/10.9745/GHSP-D-20-00171.
[24] Sorpreso ICE, et al, 2015. Sexually vulnerable women: could long-lasting reversible contraception be the solution? Rev Bras Ginecol E Obstet.; 37:395–396.
[25] Taylor Riley et al., 2020. Estimates of the Potential Impact of the Covid-19 Pandemic on Sexual and Reproductive Health in Low- and Middle-Income Countries, International Perspectives on Sexual and Reproductive Health, A journal of peer-reviewed research, volume 46, page 73-76.
Viewed PDF 1134 25 -
 Results of Unintentional Injuries among Preschool Children Enrolled in Day-care Centers from Selected Villages around Gaborone, BotswanaAuthor: Kedibonye Tsaone Mmachere MarekaDOI: 10.21522/TIJPH.2013.10.04.Art007
Results of Unintentional Injuries among Preschool Children Enrolled in Day-care Centers from Selected Villages around Gaborone, BotswanaAuthor: Kedibonye Tsaone Mmachere MarekaDOI: 10.21522/TIJPH.2013.10.04.Art007Results of Unintentional Injuries among Preschool Children Enrolled in Day-care Centers from Selected Villages around Gaborone, Botswana
Abstract:
This study employed a descriptive cross-sectional study qualitative and quantitative designs to gather data through structured interviews, questionnaires over a certain period in time in the past (retrospective) and the present (concurrent), and then analyze the results. The study was undertaken in the selected villages around Gaborone Botswana, situated in the south of the country. Its final focus was to publish the research results from a research survey done on unintentional injuries among preschool children enrolled in day-care centers from selected villages around Gaborone, Botswana. The population consisted of 47-day care centers in the selected villages around Gaborone which are all situated in Mogoditshane/Thamaga Subdistrict. A sample of 45 care centers was drawn using Yamane formula. Data were then collected through auditing, structured interviews, and questionnaires. The Statistical Package for Social Sciences (SPSS) program was used to analyze the data. The summary of the results of the current study show that: i) Males are more likely to get injured than females ii) Older children are more likely to sustain UI (iii) UI are sustained in the late afternoons iv) UI are more likely to be sustained in the early and late part of the week v) Season or term of study is not a factor of UI vi) Amount of time spent at school is a factor of UI (Davis, Godfrey & Rankin 2013).The findings indicate that there are factors that can have a negative influence on the occurrence of unintentional injuries in day care centers. It is suggested that a supportive teaching programme in the form of a workshop for service providers, teachers and parents should be designed, that will support the system of unintentional injury prevention program for preschool children in day care centers in order to prevent unintentional injuries in the selected villages around Gaborone, Botswana.
Keywords: Contributing factors to unintentional injuries, Day care centers / pre-schools/ preprimary units, Interventions on unintentional injury prevention, Unintentional injuries, Unintentional injuries prevention, the Prevalence of unintentional injuries in childcare settings.Results of Unintentional Injuries among Preschool Children Enrolled in Day-care Centers from Selected Villages around Gaborone, Botswana
References:
[1] Daycare centers and pre-schools under the Fair Labor Standards Act (FLSA) http://www.dol.gov/agencies/whd/fact-sheet/46-flsa-daycare(2009).
[2] Hoffnung, M., Hoffnung, R. J., Seifert, K. L., Burton Smith, R., & Hine, A. (2010). Childhood (1st ed.). Milton, Old: John Wiley & Sons Australia.
[3] Phelan KJ,Khoury J, Kalkwarf HJ,Lanphear BP.Trends and patterns of playground injuries in United States children and adolescents (20010. Ambulatory Pediatrics 2001; 1(4):227-33. https://doi.org/10.1177%2F003335490512000111.
[4] Macarthur Colin, Hu Xiaohan, Wesson David E &Parkin Patricia C. (2000). Risk factors for severe injuries associated with falls from playground equipment. Analysis and prevention, 32(3):377-82. doi: 10.1016/s0001-4575(99)00079-2.
[5] Gong1 Hairong, Guoping Lu, Jian Ma1, Jicui Zheng, Fei Hu1, Jing Liu1, Jun Song, Shenjie Hu1, Libo Sun1, Yang Chen1, Li Xie, Xiaobo Zhang, Leilei Duan6 and Hong Xu (2021) Causes and Characteristics of Children Unintentional Injuries in Emergency Department and Its Implications for Prevention Public Health PMC8374066. doi: 10.3389/fpubh.2021.669125.
[6] CDC (2013). Centers for Disease Control and Prevention. Injury, Violence, and Safety. Available at http://www.cdc.gov/InjuryViolenceSafety/.
[7] Unitentional injuries. Rhode Island department https://health.ri.gov/injury/ (n.d.).
[8] Mónica, R.-C. (2009). Unintentional Childhood injuries in Sub- Saharan Africa: An overview of risk and protective factors. Journal of Health care for the poor and undeserved, 20(4 Suppl):51-67 DOI:10.1353/hpu.0.0226.
[9] Yamane, Taro (1973) Statistics’, an introductory analysis, 2nd edition, New York: Harper International Edition jointly published by. Harper & Row.
[10] Davis Christopher S 1, Godfrey Sarah E, Rankin Kristin M (2013) Unintentional injury in early childhood: its relationship with childcare setting and provider. Maternal and Child Health Journal. 17(9):1541-9. doi: 10.1007/s10995-012-1110-z.
[11] Hashikawa A, Newton M.F, Stevens M, Cunningham R. M (2013) Unintentional injuries in childcare centers in the United States: A systematic review Journal of Child Health Care 19(1). DOI: 10.1177/1367493513501020.
[12] Chang A, Lugg M, Nebedum M, (1989) Injuries among pre-school children enrolled in daycare centers. Pediatrics (1989) 83 (2): 272–277. https://doi.org/10.1542/peds.83.2.272.
[13] Sacks Smith JD,Kaplan KM, Lambert DA,Sattin RW, Sikes( 1989) RK The epidemiology of J injuries in Atlanta daycare centers. JAMA, 01262(12):1641-1645 DOI: 10.1001/jama.1989.03430120095028 PMID: 2769919.
[14] Alkon A, Genevro JL, Kaiser PJ, Schann PJT, Chesney JM, Boyce M (1994) Injuries in childcare centers: Rates, severity, and etiology. Pediatrics 94(6 Pt 2):1043-6.
[15] Lee, E.J., & Bass, C. (1990). Survey of accidents in a university daycare center. Journal of Pediatric Health Care 4(1):18-23. doi: 10.1016/0891-5245(90)90035-5.
[16] Macarthur Colin, Hu Xiaohan, Wesson David E &Parkin Patricia C. (2000). Risk factors for severe injuries associated with falls from playground equipment. Analysis and prevention, 32(3):377-82. doi: 10.1016/s0001-4575(99)00079-2.
[17] Alkon A, Genevro JL, Tschann JM, et al. (1999) The epidemiology of injuries in 4 childcare centers. Archives of Pediatrics and Adolescent Medicine 153(12):1248-54. doi: 10.1001/archpedi.153.12.1248.
[18] Hyder Adnan, Peden Margaret, Krug Etienne ( 2009) Child injuries and violence: The new challenge for child health Bulletin of the World Health Organisation 86(6):420 DOI:10.2471/BLT.08.054767.
[19] Davis, C.S., Godfrey, S.E., & Rankin, K.M. (2012). Unintentional injury in early childhood: Its relationship with childcare setting and provider. Maternal Child Health Journal, NLM Unique ID: 9715672. 17(9):1541-9. doi: 10.1007/s10995-012-1110-z.
[20] Petridou Eleni Th, Sibert J, Dedoukou J Xi, Skalkidis I. (2002). Injuries in public and private playgrounds: The relative contribution of structural,equipment and human factors. Acta Paediatrics, 2002; 91(6):691-7. doi: 10.1080/080352502760069133.
[21] Teck Hoc Toh,Lee Wong. (2006). Playground injuries in Singaporean children with special reference to falls from monkey-bars. https://www.researchgate.net/publication/287080444.
[22] Lee, E.J., & Bass, C. (1990). Survey of accidents in a university daycare center. Journal of Pediatric Health Care, 4(1):18-23 doi: 10.1016/0891- 5245(90)90035-5.
[23] Maundeni, T. (2013), Early Childhood Care and Education in Botswana: A Necessity That Is Accessible to Few Children. Creative Education, 04(07):54-59 DOI:10.4236/ce.2013.47A1008 http://www.scirp.org/journal/ce.
Viewed PDF 897 32 -
 Knowledge, Attitude and Practice toward Nutrition among Communities in Southern Senatorial Zone of Borno StateAuthor: Ibrahim Musa NgosheDOI: 10.21522/TIJPH.2013.10.04.Art008
Knowledge, Attitude and Practice toward Nutrition among Communities in Southern Senatorial Zone of Borno StateAuthor: Ibrahim Musa NgosheDOI: 10.21522/TIJPH.2013.10.04.Art008Knowledge, Attitude and Practice toward Nutrition among Communities in Southern Senatorial Zone of Borno State
Abstract:
Nutrition is a key element of health promotion, prevention, and management of diseases. The study was aimed at assessing the nutritional knowledge, attitude, and practice of communities and to determine factors influencing the nutritional knowledge, attitudes, and practices of these communities. A cross-sectional study was conducted among 10 communities. Multistage sampling was used to select the sample size of 1000 individuals. The study utilized both primary and secondary data through journals and administration of a self-developed structured interviewer questionnaire and focus group discussions. The data was analyzed using statistical package for social science (SPSS v20). Results were presented using descriptive statistics and Chi-square. The findings of the study revealed that communities have little or no knowledge about nutrition despite the availability of different sources of nutritional information, majority of communities have a negative attitude towards the importance of nutrition because of their Cultural beliefs. Moreso, majority communities do not prepare balanced family meals. The result from chi-square analysis shows that age and source of nutritional knowledge are the main factors influencing nutritional knowledge and education level, marital status, and sources of family income are the main factors influencing nutritional practices among communities. Base on the findings of the study it was recommended among others that there is need to increased public awareness and enlightenment to improve the attitude and practice of communities, community leaders and health workers to promote good dietary habits and consumption of good indigenous food to motivate practice among communities.
Keywords: Attitude, Communities, Knowledge, Nutrition, Practice.Knowledge, Attitude and Practice toward Nutrition among Communities in Southern Senatorial Zone of Borno State
References:
[1] World Health Organization (2019) World Health Statistics: monitoring health for sustainable development goals: ISBN 978-92-4-156570-7.
[2] Givens D.I (2018) Dairy foods, red meat and processed meat in the diet: implications for health at key life stages. Animal12, 1709– 1721. Cambridge University Press.
[3] Triches, R. & Giugliani, E. (2005). Obesity, eating habits and nutritional knowledge among school children. Revista de Saúde Pública. 39:541-547.
[4] Ihab, A., Jalil, R., Manan, W., Wan N., Wan S., Mohd S., Zalilah & Abdullah, M. (2013). Nutritional Outcomes Related to Household Food Insecurity among Mothers in Rural Malaysia. Journal of health, population, and nutrition. 31: 480-9.
[5] Mirmiran, P., Azadbakht, L., & Azizi F. (2007) Dietary behaviour of Tehranian adolescents does not accord with their nutritional knowledge. Journal Public Health Nutrition 10(9):897-901.
[6] Kigaru, D.M.D., Loechl, C., Moleah, T. (2015) Nutrition knowledge, attitude and practices among urban primary school children in Nairobi City, Kenya: a KAP study. BMC Nutrition 1(44). https://doi.org/10.1186/s40795-015-0040-8.
[7] Kalu, R.E and Etim, K.E (2018) Factors Associated with Malnutrition among Underfive Children in Developing Countries: A Review. Global journal of pure and applied sciences 24: 69-74 ISSN 1118-0579 DOI: https://dx.doi.org/10.4314/gjpas.v24i1.8.
[8] Berti C, Cetin I, and Agostoni C. (2016) Pregnancy and infants’ outcome: nutritional and metabolic implications. Crit Rev Food Science Nutrition. 56:82-91.
[9] Uddin M.T., Islam M.N. & Uddin MJ (2008) A survey on knowledge of nutrition of physicians in Bangladesh: evidence from Sylhet data. South East Asian Journal Medical Education. 2:14–17.
[10] Vahyala A.T., Minnessi G.K. and Kabiru U. (2016). The effects of Boko Haram insurgency on food security status of some selected local government areas in Adamawa State, Nigeria. Sky Journal of Food Science 5(3): 012 – 018.
[11] Nahikian-Nelms, M. (1997) Influential Factors of Caregiver Behavior at Mealtime: A Study of 24 Child Care Programs. Journal of the American Dietetic Association, (97), 505-509.
[12] Bakhtiar M.D., Masud-ur-Rahman M.D., Kamruzzaman Nargis Sultana M.D and Shaikh S.S. (2021) Determinants of nutrition knowledge, attitude and practices of adolescent sports trainee: A cross-sectional study in Bangladesh. Heliyon Journal 7(1):1-11.
[13] Jeinie, M.H.B.; Guad, R.M.; Hetherington, M.M.; Gan, S.H.; Aung, Y.N.; Seng,W.Y.; Lin, C.L.S.; George, R.; Sawatan,W.; Nor, N.M. (2021) Comparison of Nutritional Knowledge, Attitudes and Practices between Urban and Rural Secondary School Students: A Cross-Sectional Study in Sabah, East Malaysia. Foods. 10, 2037. https://doi.org/10.3390/foods10092037.
[14] Fasola O, Abosede O, Fasola F.A. (2018). Knowledge, attitude and practice of good nutrition among women of childbearing age in Somolu Local Government, Lagos State. Journal Public Health African. 9(1):793.
[15] Charles S.R., Ismail S., Ahmad N., Ying L.P, Abubakar N.I. (2016) Knowledge, Attitude, and Practice of Adolescent Girls towards Reducing Malnutrition in Maiduguri Metropolitan Council, Borno State, Nigeria: Cross-Sectional Study. Nutrients. ;12(6):1681.
[16] Likert, R. (1932). A technique for measurement of attitudes. Archives of Psychology, 140, 5-55.
[17] Kassahun, C.W., Mekonen, A.G. (2017) Knowledge, attitude, practices and their associated factors towards diabetes mellitus among non-diabetes community members of Bale Zone administrative towns, South East. Journal of Medical Science 12(1):34-37.
[18] Uba, M. N., Alih, F. I., Kever, R.T. & Lola, N. (2015). Knowledge, attitude and practice of nurses toward pressure ulcer prevention in University of Maiduguri Teaching Hospital, Borno State, North-Eastern, Nigeria. International Journal of Nursing and Midwifery, 7(4), 54-60.
[19] Kaur, K., Grover, K., & Kaur, N. (2016). Assessment of Nutrition Knowledge of Rural Mothers and Its Effectiveness in Improving Nutritional Status of Their Children. Indian Research Journal of Extension Education, 15, 90-98.
[20] Farjana R.B, Joti Lal B., Kazi Abul K. (2021) Knowledge, Attitude and Practices Regarding Nutrition among Adolescent Girls in Dhaka City: A Cross-sectional Study. Nutrition Food Science International Journal. 10(4): 555795. DOI: 10.19080/NFSIJ.2021.10.555795.
[21] Sulaiman S., Muhammad G.A, Muhammad A.S., Abubakar H., and Abubakar S.M. (2020). Assessment of nutritional status, knowledge, attitude, and practices of infant and young child feeding in Kumbotso local government area, Kano State, Nigeria. Pakistan Journal Nutrition 19: 444-450.
[22] French, S. A., Wall, M., & Mitchell, N. R. (2010). Household income differences in food sources and food items purchased. The international journal of behavioral nutrition and physical activity, 7, 77. https://doi.org/10.1186/1479-5868-7-77.a.
Viewed PDF 1510 131 -
 Estimating the Biological Age and the Magnitude of Lifestyle Determinants of Ageing among Nigerian AdultsAuthor: Abiodun Bamidele AdelowoDOI: 10.21522/TIJPH.2013.10.04.Art009
Estimating the Biological Age and the Magnitude of Lifestyle Determinants of Ageing among Nigerian AdultsAuthor: Abiodun Bamidele AdelowoDOI: 10.21522/TIJPH.2013.10.04.Art009Estimating the Biological Age and the Magnitude of Lifestyle Determinants of Ageing among Nigerian Adults
Abstract:
Considering the various limitations of using chronological age, biological age estimation is becoming increasingly recognized as one of the novel public health and clinical strategies for preventing and controlling the rising global prevalence of noncommunicable diseases (NCDs) and for achieving healthy ageing. The objectives of this study are to estimate the biological age and compare it to the chronological age of Nigerian adults. Also, to score the magnitude of some of the lifestyle determinants of biological age among the study population. This cross-sectional study uses simple random sampling technique to select 82 Nigerian adults for the study, while standardized instruments were used to collect data. The P value for the study was set at 0.05 level of significance. The result of the study noticed poor mean Mediterranean Diet Adherence (MDAQ) score of 7.0 ± 2.28 and mean International Physical Activity (IPAQ) score of 1.3 ± 0.51. There was also suboptimal mean Pittsburgh Sleep Quality Index (PSQI) score of 5.9 ± 3.01, mean Perceive Stress Scale-4 (PSS-4) score of 6.3 ± 2.79, and mean Social Connectedness Scale (SCS) score of 15.2 ± 4.13. Furthermore, the estimated biological age of the respondents (45.9 years, ±10.31), was higher than their chronological age (43.2 years, ±8.92). The study concluded that the magnitudes of the lifestyle determinants of ageing are high enough to result in accelerated biological ageing among the study population. Such development, if not mitigated, may result in a significant increase in the prevalence of NCDs and premature deaths in the near future.
Keywords: Accelerated Ageing, Biological Age, Chronological Age, Lifestyle determinants of ageing, Health Promotion Intervention.Estimating the Biological Age and the Magnitude of Lifestyle Determinants of Ageing among Nigerian Adults
References:
[1] Pathath A.W., 2017, Theories of Aging. International Journal of Indian Psychology, 4 (3), 15 – 22. https://DOI:10.25215/0403.142.
[2] Jia L., Zhang W., and Chen X., 2017, Common methods of biological age estimation. Clinical Interventions in Aging, 12, 759–772.
[3] Cavallasca J., 2017, Measuring aging: what is your physiological age? Date of access: 2/4/2021. http://www.longlonglife.org/en/transhumanism-longevity/aging/measure-of-aging/measuring-aging-physiological-age/.
[4] Jiang S., and Guo Y., 2020, Epigenetic Clock: DNA Methylation in Aging. Stem Cells International, 2020, 1 – 9. https://doi.org/10.1155/2020/1047896.
[5] Kim S., and Jazwinski S.M., 2015, Quantitative measures of healthy aging and biological age. Healthy Aging Res., 4, 1 – 25. http://doi:10.12715/har.2015.4.26.
[6] Rollandi G.A., Chiesa A., Sacchi N., Castagnetta M., Puntoni M., Amaro A., et al., 2019, Biological Age versus Chronological Age in the Prevention of Age Associated Diseases, OBM Geriatrics, 3(2), 1 – 14, https://doi:10.21926/obm.geriatr.1902051.
[7] Kim S., Myers L., Wyckoff J., Cherry K.E., and Jazwinski S.M., 2017, The frailty index outperforms DNA methylation age and its derivatives as an indicator of biological age. GeroScience, 39, 83 – 92. https://DOI10.1007/s11357-017-9960-3.
[8] Waters D., 2020, This biological age calculator shows how old your body is. Date of access: 4/6/2021. https://www.womanandhome.com/health-and-wellbeing/biological-age-calculator-20430/.
[9] Kresovich J.K., Xu Z., O’Brien K.M., Weinberg C.R., Sandler D.P., and Taylor J.A., 2019, Methylation-Based Biological Age and Breast Cancer Risk. J Natl Cancer Inst., 1, 111(10), 1051-58. https://doi:10.1093/jnci/djz020.
[10] Waters D., 2020, This biological age calculator shows how old your body is. Date of access: 4/6/2021. https://www.womanandhome.com/health-and-wellbeing/biological-age-calculator-20430/.
[11] Federal Ministry of Health of Nigeria, 2015, National Strategic Plan of Action on Prevention and Control of Non-Communicable Diseases. Date of access: 21/7/2021 https://www.medbox.org/document/nigeria-national-strategic-plan-of-action-on-prevention-and-control-of-non-communicable-diseases#GO.
[12] World Health Organization, 2018, Non-communicable Diseases Country profiles 2018. Date of access: 21/7/2022. https://www.who.int/nmh/publications/ncd-profiles-2018/en/.
[13] Thompson A.E., Anisimowicz Y., Miedema B., Hogg W., Wodchis W.P., & Aubrey-Bassler K., 2016, The influence of gender and other patient characteristics on health care-seeking behaviour: a QUALICOPC study, BMC Family Practice, 17, 38. https://DOI:10.1186/s12875-016-0440-0.
[14] Lim M.T., Lim Y.M.F., Tong S.F., and Sivasampu S., 2019, Age, sex and primary care setting differences in patients’ perception of community healthcare seeking behaviour towards health services, PLoS ONE 14(10), e0224260. https://doi.org/10.1371/journal.pone.0224260.
[15] de Wit J.B.F., Peeters M., and Koning I., 2022, Risk Behaviour and Health Outcomes of Adolescents and Young Adults. Date of access: 20/7/2022. https://www.frontiersin.org/research-topics/5907/risk-behaviour-and-health-outcomes-of-adolescents-and-young-adults.
[16] Hilz R., & Wagner M., 2018, Marital Status, Partnership and Health Behaviour: Findings from the German Ageing Survey (DEAS). Comparative Population Studies, 43, 65-98. https://DOI:10.12765/CPoS-2018-08en.
[17] Fuchs M., 2021, Want to add healthy years to your life? Here’s what new longevity research says. Date of access: 9/8/2021. https://www.washingtonpost.com/lifestyle/wellness/longevity-research-diet-exercise-tips/2021/10/10/edb5cdc2-2856-11ec-9de8-156fed3e81bf_story.html
[18] Abuduxike G., Aşut Ö, Vaizoğlu S.A., and Cali S., 2020, Health-Seeking Behaviors and its Determinants: A Facility-Based Cross-Sectional Study in the Turkish Republic of Northern Cyprus. Int J Health Policy Manag, x(x), 1–10. https://Doi:10.15171/ijhpm.2019.106.
[19] International Diabetes Federation, 2021, IDF Diabetes Atlas 10th edition. Date of access: 20/7/2022. https://diabetesatlas.org/idfawp/resource-files/2021/07/IDF_Atlas_10th_Edition_2021.pdf.
[20] Federal Ministry of Health of Nigeria, 2021, National Guideline on The Prevention, Control and Management of Diabetes Mellitus. Date of access: 21/7/2022. https://www.health.gov.ng/doc/National%20Guideline%20for%20the%20prevention,%20control%20and%20management%20of%20Diabetes%20Mellitus%20in%20Nigeria%20(3).pdf.
[21] World Health Organization, 2011, Global Status Report on Non-Communicable Diseases 2010. Date of access: 21/7/2022. https://apps.who.int/iris/bitstream/handle/10665/44579/9789240686458_eng.pdf?sequence=1&isAllowed=y.
[22] Furman D., Campisi J., Verdin E., Carrera-Bastos P., Targ S., Franceschi C., et al., 2019, Chronic inflammation in the etiology of disease across the life span. Nature Medicine, 25, 1822 – 1832. https://doi.org/10.1038/s41591-019-0675-0.
[23] Akarolo-Anthony S.N., Willett W.C., Spiegelman D., and Adebamowo C.A. Obesity epidemic has emerged among Nigerians. BMC Public Health 2014, 14:455. http://www.biomedcentral.com/1471-2458/14/455.
[24] Chukwuonye I.I., Chuku A., John C., Ohagwu K.A., Imoh M.E., Isa S.E., et al., 2013, Prevalence of overweight and obesity in adult Nigerians – a systematic review. Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy, 6, 43–47.
[25] Södergren M., 2013, Lifestyle predictors of healthy ageing in men. Maturitas., 75(2), 113-7. https://DOI:10.1016/j.maturitas.2013.02.011.
[26] Adelowo A.B., 2021, Analyzing the Magnitude of Global Epidemiological Transition in Sub-Saharan Africa: A Need to Review the Current Healthcare Management Approach. Texila International Journal of Public Health, 9 (3); 204 – 212. https://DOI:10.21522/TIJPH.2013.09.03.Art018.
[27] Adelowo A.B., 2022, A Scoping Review of Cardio-Metabolic Syndrome: A Critical Step in Mitigating the Rising Global Burden of Cardiovascular Diseases and Diabetes Mellitus. Int J Diabetes Metab Disord, 7(1): 80-86. https://doi.org/10.33140/IJDMD.07.01.13.
[28] Federal Ministry of Health of Nigeria, 2014, National Nutritional Guideline on Non-Communicable Disease Prevention, Control and Management. Date of access: 13/12/2016. http://www.health.gov.ng/doc/NutritionalGuideline.pdf.
[29] Agu AU, Esom EA, Chime SC, Anyaeji PS, Anyanwu GE, and Obikili EN., 2021, Impact of sleep patterns on the academic performance of medical students of College of Medicine, University of Nigeria. Int J Med Health Dev, 26, 31-6.
[30] Onoh I., 2017, World Sleep Day: How sleep deprivation threatens Lagosians’ wellbeing – Expert. Date of access: 4/8/2022. https://www.environewsnigeria.com/world-sleep-day-sleep-deprivation-threatens-lagosians-wellbeing-expert/.
[31] Adelowo A.B, 2020, Sleep: An Insight into the Neglected Component of a Healthy Lifestyle. Nigerian School of Health Journal, 32 (1), 75-87.
[32] Wilson D., Driller M., Johnston B., and Gill N., 2021, The effectiveness of a 17-week lifestyle intervention on health behaviors among airline pilots during COVID-19. J Sport Health Sci, 10, 333 – 40. https://doi.org/10.1016/j.jshs.2020.11.007.
[33] Iyizoba N., 2017, Nigeria: Managing Stress in World’s Most Stressful Country. AllAfrica, 2017. Date of access: 5/8/20222. https://allafrica.com/stories/201709140833.html.
[34] ThisDay, 2021, Nigeria: The Stress of Living in Lagos. AllAfrica, 2021. Date of access: 5/8/2022. https://allafrica.com/stories/202106280283.html.
[35] Onigbogi C.B., and Banerjee S., 2019, Prevalence of Psychosocial Stress and Its Risk Factors among Health-care Workers in Nigeria: A Systematic Review and Meta-Analysis. Niger Med J.60(5), 238–244. https://doi:0.4103/nmj.NMJ_67_19.
[36] Ogbujah C, 2014, African Cultural Values and Inter-communal Relations: The Case with Nigeria. Developing Country Studies 2014: 4 (24): 208-17.
[37] Onuoha F., 2015, Onuoha Frank: Locating African Values in Twenty–First Century Economics. ASFL, 2018. Date of access: 5/8/2022. https://www.africanliberty.org/2015/09/09/onuoha-frank-locating-african-values-in-twenty-first-century-economics/.
[38] Sibani C.M., 2018, Impact of Western Culture on Traditional African Society: Problems and Prospects. International Journal of Religion and Human Relations 2018; 10 (1): 56 – 72.
[39] Watson K.,2019, Everything You Need to Know About Premature Ageing. Date of access: 24/11/2020. https://www.healthline.com/health/beauty-skin-care/premature-aging#tips-for-prevention.
[40] Sandoiu A., 2017, Sedentary lifestyle speeds up biological aging, study finds. Date of access: 21/6/2021. https://www.medicalnewstoday.com/articles/315347#Sedentary-women-biologically-older-by-8-years.
[41] Irwin M.R.,2014, Sleep and inflammation in resilient aging. Interface Focus, 4 (20140009), 1 – 7. http://dx.doi.org/10.1098/rsfs.2014.0009.
[42] He M., Deng X., Zhu Y., Huan L., and Niu W., 2020, The relationship between sleep duration and all-cause mortality in the older people: an updated and dose-response meta-analysis. BMC Public Health, 20 (1179), 1 – 18. https://doi.org/10.1186/s12889-020-09275-3.
[43] Korab A., 2021, Everyday Habits That Age You Faster, According to Science: Look younger and be healthier with this essential advice. Date of access: 21/2/2021. https://www.eatthis.com/news-health-habits-age-science/.
[44] Franklin B.A, and Cushman M., 2011, Recent Advances in Preventive Cardiology and Lifestyle Medicine. Circulation, 123, 2274 – 2283.
[45] Miller J., 2011, The Fountain of Youth: The Quest for Biological Immortality. Date of access: 8/5/2021. http://www.slideshare.net/Justin2226/human-longevity-by-justin-miller.
[46] Whitbourne S.K., 2012, What’s Your True Age? You may be a lot younger than you think. Date of access: 8/4/2021. https://www.commonlit.org/texts/what-s-your-true-age.
Viewed PDF 1103 19 -
 Assessment of Utilization of Standing Order in the Management of Patients by Community Health Extension Workers in Ekiti State, NigeriaAuthor: Rasheed Adeyemi AdepojuDOI: 10.21522/TIJPH.2013.10.04.Art010
Assessment of Utilization of Standing Order in the Management of Patients by Community Health Extension Workers in Ekiti State, NigeriaAuthor: Rasheed Adeyemi AdepojuDOI: 10.21522/TIJPH.2013.10.04.Art010Assessment of Utilization of Standing Order in the Management of Patients by Community Health Extension Workers in Ekiti State, Nigeria
Abstract:
Engagement and training of community health extension workers was the strategy adopted by Nigeria to solve the problem of the dearth of skilled health workers at the primary health care level. This group of health workers were trained to use standing orders in the management of the patient at this level of care. The purpose of this study is to investigate the extent of utilization of standing order among community health extension workers. The research was cross-sectional in nature, and it used a self-applied structured questionnaire. The questionnaire was distributed between March and April 2022. There were 265 respondents with age ranges between 23 and 58 years, and the majority (86.7%) were females. 98.1% possessed a copy of the standing order, and 88.5% and 9.9% kept their standing orders in health facilities and home, respectively. 62.3% used it regularly, 19.6% occasionally, 8.3% sometimes and 9.8% rarely used it. Reasons given for not using standing orders included- waste of time, patients who think I am not competent, and not containing new drugs. Regular utilization of standing order is low, and there is a need to educate the community extension workers on the importance of standing order at the primary health care level.
Keywords: Standing order, Standardization, Utilization.Assessment of Utilization of Standing Order in the Management of Patients by Community Health Extension Workers in Ekiti State, Nigeria
References:
[1] Ibrahim D.O: Assessment of the Use of National Standing Orders in the Treatment of Minor Ailments among Community Health Practitioners in Ibadan Municipality. International Journal of Scientific and Research Publications, 2016; 6(10): 50-54.
[2] James Macinko, Barbara Starfield and Temitope Erinosho: The Impact of Primary Healthcare on Population Health in Low- and Middle-Income Countries. J Ambulatory Care Manage, 2009; 32(2): 150-171.
[3] Taiwo Akinyede Obembe, Kayode Omoniyi Osungbade, and Christianah Ibrahim: Appraisal of primary health care services in federal capital territory, Abuja, Nigeria: How committed are health workers. The Pan African Medical Journal, 2017; 28: 134.
[4] Bolaji Shamson Aregbeshola and Samina Mohsin Khan: Primary Health Care in Nigeria: 24 years after Olikoye-Ransome Kuti’s Leadership. Frontiers in Public Health, 2017; 5:48/.
[5] Alenoghena I., Aigbiremolen A.O., Abejegha C. and Eboreime E: Primary health care in Nigeria: Strategies and constraints in implementations. International Journal of Community Research, 2014; 3(3): 74-79.
[6] Abdulraheem I.S., Olapipo A.R. and Amodu M.O: Primary health care services in Nigeria: Critical issues and strategies for enhancing the use by the rural communities. Journal of Public Health and Epidemiology, 2012; 4(1): 5-13.
[7] Gideon E.D.O: Perspective on Primary Health Care in Nigeria: Past, Present, and Future. Centre for Population and Environmental Development, 2014; Series No 10.
[8] Seye Abimbola, Titilayo Olanipekun, Uchenna Igbokwe, Joel Negin, Stephen Jan, Alexandra Martiniuk, Nnenna Ihebuzor, and Muyi Aina: How decentralization influences retention of primary health workers in rural Nigeria. Global Health Action, 2015; 8:26616.
[9] Seye Abimbola, Titilope Olanipekun, Marta Schaaf, Joel Negin, Stephen Jan and Alexandra L.C. Martinuik: Where there is no policy: governing the posting and transfer of primary health care workers in Nigeria. The International Journal of Health Planning and Management, 2017; 32: 492-508.
[10] Olayinka Akanke Abosede and Olugbenga Fola Sholeye: Strengthening the Foundation for Sustainable Primary Health Care Services in Nigeria. Primary Health Care, 2014; 4(3).
[11] Primary health care systems (PRIMASYS): case study from Nigeria. Geneva: World Health Organization; 2017. Licence: CCBY-NC-SA 3.0 IGO.
[12] Tamara Kredo, Susanne Bernhardsson, Taryn Young, Quinette Louw, Eleanor Ochodo and Karen Grimmer: Guide to clinical practice guidelines: the current state of play. International Journal of Quality in Health Care, 2016; 28(1): 122-128.
[13] Irving R. Tabershaw and Margaret S. Hargreaves: Functions of Standing Orders for the Nurses in Industry. American Journal of Public Health, 1947; 37: 1430- 1434.
[14] Guerrero GP, Beccaria LM, and Trevizan MA: Standard operating procedure: Use in nursing care in hospital services. Rev Latino-am Enfermagem, 2008; 16(6): 966-972
[15] Walter RR, Gehlen MH, Ilha S, Zamberlan C, Barbosa de Freitas HM, and Pereira FW: Standard operation procedure in the nursing context: the nurses’ perception. Rev Fund Care Online. 2016 out/dez; 8(4): 5095-5100. DOI: http.dx.doi, org:10.9789/21755361. 2016.v8i4.5095-5100.
[16] Fatima Riskat Rahji: Knowledge, Perception and Utilization of integrated Management of Childhool Illnesses among Health care Workers in selected Primary Health Care Facilities in Ibadan, Nigeria. Nursing and Midwifery Council of Nigeria, 2018.
[17] Oyewole MF: Utilization of Primary Health Care Services Among Rural Dwellers in Oyo State. Nigeria Journal of Rural Sociology, 2018; 18(1): 106-111.
[18] Seye Abimbola, Titilope Olanipekun, Marta Schaaf, Joel Negin, Stephen Jan, and Alexandra L.C. Martinuik: Where there is no policy: governing the posting and transfer of primary health care workers in Nigeria. The International Journal of Health Planning and Management, 2017; 32: 492-508.
[19] V Lukali and C Michelo: Factors associated with Irrational Drug use at a District Hospital in Zambia: Patient Record-Based Observation. Medical Journal of Zambia, 2015; 42(1): 25-30.
[20] Mekonnen Sisay, Getnet Mengistu, Bereket Molla, Firehiwot Amare, and Tesfaye Gabriel: Evaluation of rational drug use based on World Health Organization core drug use indicators in selected public hospitals in eastern Ethiopia: a cross sectional study. BMC Health Services Research, 2017; 17:161. DOI.10.1186/s12913-017-2097-3.
[21] Basheer A.Z. Chedi, Ibrahim Abudu-Aguye and Helen O. Kwanashie: Drug use pattern in out-patient children: a comparison between primary and secondary health care facilities in Northern Nigeria. African Journal of Pharmacy and Pharmacology, 2015; 9(4): 74-81.
[22] Bosse G, Schmidbauer W, Spies CD, Sorensen M, Francis RCE, Bubser F, Krebs M and Kerner T: Adherence to Guidelines –based Standard Operating Procedures in Pre-hospital Emergency Patient with Chronic Obstructive Pulmonary Diseases. The Journal of International Medical Research, 2011; 39: 267-276.
[23] Al-Mounawara Yaya: Reducing Under-five Childhood Mortality using IMCI/e-IMCI: Implementation Approaches in Nigeria. A Master’s Paper submitted to the faculty of the University of North Carolina at Chapel Hill in partial fulfilment of the requirements for the degree of master’s in public health in the Global Public Health Program at The Gillings School of Global Public Health, 2017.
[24] Grace Komuhangi, Nwana Uchechukwu Kevin, Ilori Oluwole Felex and Lydia Kabiri: Factors Associated with Compliance with Infection Control Guidelines in the Management of Labour by Healthcare Workers at Mulago Hospital, Uganda. Open Journal of Nursing, 2019; 9(7): 697- 723. doi: 10.4236/ojn.2019.97054
[25] Sarah Lodel, Christoph Ostgathe, Maria Heckel, Karin Oechsle and Susanne Gahr: Standard Operating Procedures (SOP) for Palliative Care in German Comprehensive Cancer Centres – an evaluation of implementation status. MBC Palliative Care, 2020; 19(62).
[26] Lamin E.S. Jaiteh, Stefan A Helwig, Abubacarr Jagne, Andreas Ragoschle-Schumm, Catherine Sarr, Silke Walter Martin Lesmeister, Dipl-Phys Matthias Manitz, Sebastian Blab, Sarah Weis, Verena Schlund, Neneh Bah, Jil Kauffmann, Mathias Fousse, Sabina Kangankan, Asmell Ramos Cabrera,
Kai Kronfeld, Christian Ruckes, Dipl-Math Yang Liu, Ousman Nyan, and Klaus Fassbender: Standard operating procedures improve acute neurologic care in a sub-Saharan African setting. Neurology, 2017; 89: 144-152. DOI 10.1212/WNL.0000000000004080.[27] Hongxia Zhang, Zonghong Zhu, Xiaoyan Wang, Xiaofeng Wang, Limin Fan, Ranran Wu, and Chenjing Sun: Application Effect of the Standard Operation Procedures in the Prevention of Venous Thromboembolism. Journal of Healthcare Engineering, 2022. https://doi.org/10.1155/2022/5019898.
[28] David M.O. Omoit, George O. Otieno and Kenneth K. Rucha: Measuring the Extent of Compliance to Standard Operating Procedures for Documentation of Medical Records by Healthcare Workers in Kenya. Public Health Research, 2020; 10(2): 78-86. doi: 10.5923/j.phr.20201002.06.
Viewed PDF 1116 46 -
 Vaccine Management Knowledge and Practice of Health workers in YemenAuthor: Victor SuleDOI: 10.21522/TIJPH.2013.10.04.Art011
Vaccine Management Knowledge and Practice of Health workers in YemenAuthor: Victor SuleDOI: 10.21522/TIJPH.2013.10.04.Art011Vaccine Management Knowledge and Practice of Health workers in Yemen
References:
[1] Osei, E., Ibrahim, M., & Kofi Amenuvegbe, G., 2019, Effective Vaccine Management: The Case of a Rural District in Ghana. Advances in preventive medicine, 2019, 5287287. https://doi.org/10.1155/2019/5287287.
[2] Pollard, A.J., Bijker, E.M., 2021, A guide to vaccinology: from basic principles to new developments. Nat Rev Immunol 21, 83–100, https://doi.org/10.1038/s41577-020-00479-7.
[3] World Health Organization. Regional Office for Africa., 2017, Mid-Level Management Course for EPI Managers: Block III: Logistics: Module 8: Vaccine management, https://apps.who.int/iris/handle/10665/260479.
[4] Ameen, H., Salaudeen, A.G., Musa, O. et al., Predictors of vaccine management practices among primary healthcare workers (PHCWs) in Ilorin, North Central Nigeria. Research Journal of Health Sciences, 4. 2016-148. https://www.researchgate.net/publication/305495236_Predictors_of_vaccine_management_practices_among_primary_healthcare_workers_PHCWs_in_Ilorin_North_Central_Nigeria.
[5] WHO., & UNICEF., 2016, WHO/UNICEF joint statement: Achieving immunization targets with the comprehensive effective vaccine management (cEVM) framework. https://apps.who.int/iris/handle/10665/254717.
[6] Wasiu, O.A., & Oluwatosin, A.A., 2020, Knowledge and practice of vaccination logistics management among primary health care workers in Nigeria: Orcid Icon Pages 1490-1495. https://doi.org/10.1080/21645515.2020.1827609.
[7] Mohammed, S.A., Workneh, B.D., & kahissay, M.H., 2021, Knowledge, attitude and practice of vaccinators and vaccine handlers on vaccine cold chain management in public health facilities, Ethiopia: Cross-sectional study. Plos One 16(2): e0247459. https://doi.org/10.1371/journal.pone.0247459.
[8] Ministry of Public Health & Population, Yemen., 2016, Comprehensive Multi-year Plan (cMYP) 2016-2020.
[9] United Nation Children Fund (UNICEF)., Sept. 2022, Yemen draft country program document. https://www.unicef.org/executiveboard/documents/Yemen-draft-country-programme-document-srs-2022.
[10] Charan, J., & Biswas, T., 2013, How to calculate sample size for different study designs in medical research? Indian Journal of Psychological Medicine, 35(2), 121–126. https://doi.org/10.4103/0253-7176.116232.
[11] World Health Organization (WHO)., 2005, Vaccine Management Assessment. http://apps.who.int/iris/bitstream/handle/10665/69616/WHO_IVB_05.02_eng.pdf?sequence=1.
[12] Feyisa, D., Ejeta, F., Aferu, T. et al., 2022, Adherence to WHO vaccine storage codes and vaccine cold chain management practices at primary healthcare facilities in Dalocha District of Silt’e Zone, Ethiopia. Trop Dis Travel Med Vaccines 8, 10. https://doi.org/10.1186/s40794-022-00167-5.
[13] World Health Organization., 2016, Global Routine Immunization Strategies and Practices (GRISP): a companion document to the Global Vaccine Action Plan (GVAP). https://apps.who.int/iris/handle/10665/204500.
[14] Daud, Norwati., 2014, Knowledge, Attitude and Adherence to Cold Chain among General Practitioners in Kelantan, Malaysia. https://internalmedicine.imedpub.com/knowledge-attitude-and-adherence-to-cold-chain-amonggeneral-practitioners-in-kelantan-malaysia.php?aid=6257.
[15] Gebretnsae, H., Hadgu, T., Ayele, B. et al., 2022, Knowledge of vaccine handlers and status of cold chain and vaccine management in primary health care facilities of Tigray region, Northern Ethiopia: Institutional based cross-sectional study. Plos One. 17. e0269183. 10.1371/journal.pone.0269183. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0269183.
[16] Woldamichael, B., Bekele, D., & Esmael, A., 2018, Cold Chain Status and Knowledge of Vaccine Providers at Primary Health Care of Units Bale Zone, Southeast Ethiopia: Cross-sectional Study. Immunome Research. 14,152. https://www.readcube.com/articles/10.4172/1745-7580.1000152.
[17] Zeyneba, J. Y., Habtamu, Y.N., Behailu, T. D. et al., 2019, Knowledge of Health Professionals on Cold Chain Management and Associated Factors in Ezha District, Gurage Zone, Ethiopia, Scientifica, vol. 2019, Article ID 6937291, 7 pages. https://doi.org/10.1155/2019/6937291.
[18] Ebile Akoh, W., Ateudjieu, J., Nouetchognou, J.S. et al., 2016, The expanded program on immunization service delivery in the Dschang health district, west region of Cameroon: a cross sectional survey. BMC Public Health 16, 801. https://doi.org/10.1186/s12889-016-3429-7.
[19] Mavimbe, J.C., Bjune, G., 2007, Cold chain management: Knowledge and practices in primary health care facilities in Niassa, Mozambique. Ethiopian Journal of Health Development, 21(2): 130-135. https://www.ajol.info/index.php/ejhd/article/view/10040.
[20] Ameen H.A; Salaudeen A.G; Bolarinwa O.A. et al., 2014, Vaccine Storage and Handling Practices among routine immunization service providers in a metropolitan city of North-Central Nigeria. Journal of Community Medicine and Primary Health Care. 26 (2) 18–28. https://www.ajol.info/index.php/jcmphc/article/view/125356.
[21] PATH Optimize., Aug.2013, Preventing in cold boxes and vaccine carrier. https://media.path.org/documents/TS_opt_handout_freeze_safe.pdf.
[22] Bogale, H.A., Amhare, A.F., & Bogale, A.A., 2019, Assessment of factors affecting vaccine cold chain management practice in public health institutions in east Gojam zone of Amhara region. BMC Public Health 19, 1433. https://doi.org/10.1186/s12889-019-7786-x.
[23] Ministry of Public Health & Population, Yemen., July 2013, Effective Vaccine Management Assessment (EVM) report.
[24] Milstein J., 2010, Vaccine Vial Monitor (VVM) Availability and Use in the African, Eastern Mediterranean, Southeast Asian, and Western Pacific Regions. Ferney: PATH, World Health Organization; https://media.path.org/documents/TS_opt_vvm_avail_use.pdf.
[25] Kartoglu, U., Ozgüler, N. K., Wolfson, L. J., & Kurzatkowski, W., 2010, Validation of the shake test for detecting freeze damage to adsorbed vaccines. Bulletin of the World Health Organization, 88(8), 624–631. https://doi.org/10.2471/BLT.08.056879.
[26] Das, B., Bora, P., 2019, Effect of mobile-based supportive supervision on cold chain point management and routine immunization service delivery. International Journal of Medical Science and Public Health, 8 (1). 1-5. https://www.bibliomed.org/?mno=302642932.
[27] Iwu, C. J., Ngcobo, N., McCaul, M. et al., 2020, Vaccine stock management in primary health care facilities in OR Tambo District, Eastern Cape, South Africa. Vaccine, 38(25), 4111–4118. https://doi.org/10.1016/j.vaccine.2020.04.019.
[28] Ministry of Public Health & Population, Yemen. (2019). Immunization forecast for 2020.
[29] Ministry of Public Health & Population, Yemen. (2020). Immunization forecast for 2021.
[30] Ministry of Public Health & Population, Yemen. (2021). Immunization forecast for 2022.
[31] United Nation Children Funds (UNICEF)., July 2022, Immunization regional snapshots. Immunization regional snapshots - UNICEF DATA.
[32] Ministry of Public Health & Population, Yemen., 2019, Quarterly Vaccine stock take report for 2019.
[33] Ministry of Public Health & Population, Yemen., 2020, Quarterly Vaccine stock take report for 2020.
[34] Ministry of Public Health & Population, Yemen., 2019, Routine Immunization data for 2019.
[35] Ministry of Public Health & Population, Yemen., 2020, Routine Immunization data for 2020.
[36] Ministry of Public Health & Population, Yemen., 2021, Routine Immunization data for 2021.
[37] Widsanugorn, O., Suwattana, O., Harun-Or-Rashid, M., & Sakamoto, J., 2011, Healthcare workers’ knowledge and practices regarding expanded program on immunization in Kalasin, Thailand. Nagoya Journal of Medical Science, 73(3-4), 177–185. https://pubmed.ncbi.nlm.nih.gov/21928699/.
[38] Sinha, A., Verma, A., Chandrakar, A. et al., 2017, Evaluation of cold chain and logistics management practice in Durg district of Chhattisgarh: pointer from Central India. International Journal of Community Medicine and Public Health, 4(2). 390. https://www.ijcmph.com/index.php/ijcmph/article/view/582.
Viewed PDF 1230 70 -
 Investigating the Effects of Occupational Stress on Nurses Working in Referral Hospitals in Botswana to Reduce Health RiskAuthor: Tabby MaphangelaDOI: 10.21522/TIJPH.2013.10.04.Art012
Investigating the Effects of Occupational Stress on Nurses Working in Referral Hospitals in Botswana to Reduce Health RiskAuthor: Tabby MaphangelaDOI: 10.21522/TIJPH.2013.10.04.Art012Investigating the Effects of Occupational Stress on Nurses Working in Referral Hospitals in Botswana to Reduce Health Risk
Abstract:
The incidence of work stress among nurses is a persistent issue. This qualitative study was carried out to examine the problems that nurses experience in providing basic health care at Botswana referral hospitals. The study was presented as a qualitative research approach. Three referral hospitals: Princess Marina Hospital, Nyangabwe Referral Hospital, and Sabrana Psychiatric Hospital were chosen for this study. Ten management officers from the three referral hospitals with the necessary and appropriate experience were purposefully sampled in order to generate the required data via questionnaires and interviews. An inductive thematic data analysis was then used, the researchers attentively examined the data to uncover common themes and patterns that appear frequently. The intended study objectives were obtained by focusing on the preceding sampled data from management officers in referral hospitals: to identify challenges faced by nurses in the delivery of basic health care services and to recommend strategies that can be used to address challenges faced by nurses in the delivery of basic health care services. The overall findings of this study emphasized three themes that developed from the interviews: the obstacles faced by nurses in the delivery of essential health care services, which are: a lack of manpower, a lack of staff and accommodation, low wages, and a terrible working environment. The researchers finished by providing a conceptual model that may be employed as an intervention technique in the workplace to help with occupational stress.
Keywords: Occupational Stress, Stressors, Stress, Nurses.Investigating the Effects of Occupational Stress on Nurses Working in Referral Hospitals in Botswana to Reduce Health Risk
References:
[1] Alomani, Q., 2016, Causes and Effects of Occupational Stress in Nursing. Proceedings of 17th Iastem International Conference, Istanbul Turkey.
[2] American Board of Occupational Health Nursing, 2016, Occupational health nursing profession, Hinsdale, ABOHN, 3–28.
[3] Aditi, V., Rishu, R., 2020, Occupational Stress among Nurses: A Factorial Study with Special Reference to Indore City, Journal of Health Management, 22(1)67-77.
[4] Banovcinova, L., & Baskova, M., 2014, Sources of Work-related Stress and their Effect on Burnout in Midwifery, Procedia - Soc Behav Sci; 132:248–54.
[5] David, H., 1995, Mental Health and the Built Environment, New York, Routledge.
[6] Dagget, T., Molla, A., Belachew, T., 2016, Job related stress among nurses working in Jimma Zone public hospitals, Southwest Ethiopia: A cross sectional study. BMC Nurs. 2016; 15(1):1–11.
[7] Dobnik, M., Maletič, M., Skela-Savič, B., 2018, Work-Related Stress Factors in Nurses at Slovenian Hospitals-A Cross-Sectional Study, Slovenian Journal of Public Health, 2018;57(4):192–200.
[8] Gebeyehu, S., Zeleke, B., 2019, Workplace stress and associated factors among healthcare professionals working in public health care facilities in Bahir Dar City, Northwest Ethiopia. BMC Res Notes; 12(1):1–5.
[9] Hamim, N., 2015, Workload and Work Stress on Caring Behavior in nurse on Nursing Services, Int J Hum Resour Stud, 5(3):148.
[10] Jelastopulu, E., Tsouvaltzidou, T., Vangeli, E., Messolora, F., Detorakis, J., Alexopoulos, E., 2013, Self-reported Sources of Stress, Job Satisfaction and Quality of Care in Professional Hospital Nurses in West-Greece, Nurs Heal. 1(1):1–9.
[11] Rasool, E.A., Nasrin, Elahi, E.M., Masoud, F. K., 2017, How Do the Nurses Cope with Job Stress? A Study with Grounded Theory Approach, Journal of Caring Sciences, 6(3), 199211.
[12] Jose, T.T., Bhat, S.M., A, 2015, Descriptive Study on Self-Esteem among Nurses Working in Selected Hospitals of Udupi and Mangalore Districts Karnataka, India. Int J Nurs Educ. 7(3):154.
[13] Kawano, Y, 2008, Association of job-related stress factors with psychological and somatic symptoms among Japanese hospital nurses: Effect of departmental environment in acute care hospitals. J Occup Health, 50(1):79–85.
[14] Kokoroko, E., Sanda, M.A., 2019, Effect of Workload on Job Stress of Ghanaian OPD Nurses: The Role of Coworker Support. Saf Health Work, 8(3):142.
[15] Jasmina, S., 2018, Stress Factors among Nurses at the Primary and Secondary Level of Public Sector Health Care: The Case of Slovenia, Macedonian Journal of Medical Sciences, 6(2): 416–422.
[16] Muraleeswaran, R., Akilendran, K., 2016, An Assessment of level of work – Related Stress Among Nursing Officers at District General Hospital Vavuniya in Sri Lanka. Int J Sci Res Publ, 6(3):177–80.
[17] Mushonga, B., Dube-Mawerewere, V., 2017, Factors that contribute to burnout syndrome among critical care nurses in Intensive Care Units, Botswana. Int J Nurs Sci, 7(4):91–5.
[18] Prisca, E.N., 2020, Assisting Psychiatric Nurses in Managing Work Stress and Decreasing Callouts and Absenteeism. ProQuest LLC.
[19] Yueh-Chi, T.1., Chieh-Hsing, L., 2012, Factors and symptoms associated with work stress and health-promoting lifestyles among hospital staff: a pilot study in Taiwan. BMC Health Serv Res, 12(162):199.
[20] Yuan, D., Gazi, A.I., Rahman, A., 2022, Occupational stress and health risk of employees working in the garments sector of Bangladesh: An empirical study. Frontiers in Public Health, 12(1):1–5.
Viewed PDF 1115 35 -
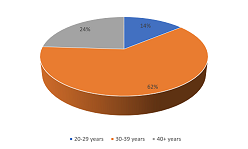 Prevalence of Cervical Cancer in Enugu State: A Critical Review of 5-year Hospital Data in Enugu State, Southeast NigeriaAuthor: Ajegbo Uzoma ChidinmaDOI: 10.21522/TIJPH.2013.10.04.Art013
Prevalence of Cervical Cancer in Enugu State: A Critical Review of 5-year Hospital Data in Enugu State, Southeast NigeriaAuthor: Ajegbo Uzoma ChidinmaDOI: 10.21522/TIJPH.2013.10.04.Art013Prevalence of Cervical Cancer in Enugu State: A Critical Review of 5-year Hospital Data in Enugu State, Southeast Nigeria
Abstract:
Cervical cancer is one of the most common cancers that affect women worldwide. In developing countries, cancers are detected late due to limited access to preventative measures and late treatment options leading to higher death rates in these countries. The study was undertaken to determine the cervical cancer prevalence to aid in planning grass root level programs to reduce the morbidity and mortality from the disease. This study is a hospital-based retrospective design that reviewed reported screening test results of CCa cases in five screening centres identified in Enugu state. Reported data sets were analysed and one-sample t-test analysis of statistical significance was determined. A pooled total of 27 333 patients were screened using pap smear and 3528 tested positive for cervical cancer was reported over the five years period giving a prevalence rate of 13%. The mean age of the positive cases was 38.82 ± 8.15 years. The majority of the cases (62%) were recorded among the age group 30 – 39 years. The yearly rates included 14% prior to 2016, 12%, 9%, 20%, 13% and 10% for 2016, 2017, 2018, 2019 and 2020 respectively. T-test analysis showed a significant difference in testing rate when compared to previous study t = 5.7, p = .002. The prevalence of this study is high when as reported in previous studies. Therefore, a targeted awareness and enlightenment of the public on cervical cancer screening is highly recommended to ensure early detection which guarantees good treatment outcomes.
Keywords: Cervical Cancer; Enugu State, Nigeria, Prevalence, Screening test.Prevalence of Cervical Cancer in Enugu State: A Critical Review of 5-year Hospital Data in Enugu State, Southeast Nigeria
References:
[1] Ferlay J, Ervik M, Lam F, Colombet M, Mery L, Piñeros M, Znaor A, Soerjomataram I, Bray F (2018). Global Cancer Observatory: Cancer Today. Lyon, France: International Agency for Research on Cancer. Available from: https://gco.iarc.fr/today.
[2] Global Cancer Observatory: Cancer Today. Lyon, France: International Agency for Research on Cancer. Available from: https://gco.iarc.fr/today, Accessed [11 May 2022].
[3] Frazer, H. (2006) “Human papillomavirus vaccine,” International Journal of Gynecology & Obstetrics, vol. 94, pp. 381–388, 2006.
[4] Ugwu, E. O., Obi, S. N., Ezechukwu, P. C., Okafor, I. I., & Ugwu, A. O. (2013). Acceptability of human papillomavirus vaccine and cervical cancer screening among female health-care workers in Enugu, Southeast Nigeria. Nigerian Journal of clinical practice, 16(2), 249-252.
[5] Akanbi, O. A., Iyanda, A., Osundare, F., & Opaleye, O. O. (2015). Perceptions of nigerian women about human papilloma virus, cervical cancer, and HPV Vaccine. Scientifica, 2015.
[6] World Health Organization. Human papillomavirus (HPV) and cervical cancer. https://www.who.int/news-room/fact-sheets/detail/human-papillomavirus-(HPV)-and-cervical-cancer (Accessed 19th May 2022).
[7] Devarapalli, P., Labani, S., Nagarjuna, N., Panchal, P., & Asthana, S. (2018). Barriers affecting uptake of cervical cancer screening in low- and middle-income countries: A systematic review. Indian Journal of Cancer, 55(4), 318.
[8] Escoffery, C., Rodgers, K.C., Kegler, M.C., Haardörfer, R., Howard, D.H., Liang, S., Pinsker, E., Roland, K.B., Allen, J.D., Ory, M.G. and Bastani, R., 2014. A systematic review of special events to promote breast, cervical, and colorectal cancer screening in the United States. BMC public health, 14(1), pp.1-13.
[9] Racey CS, Withrow DR, Gesink D (2013). Self-collected HPV testing improves participation in cervical cancer screening: A systematic review and meta-analysis. Can J Public Health 2013; 104:159-66. 15.
[10] Madzima TR, Vahabi M, Lofters A (2017). Emerging role of HPV self-sampling in cervical cancer screening for hard-to-reach women: Focused literature review. Can Fam Physician 2017; 63:597-601.
[11] Albrow R, Blomberg K, Kitchener H, Brabin L, Patnick J, Tishelman C, et al. Interventions to improve cervical cancer screening uptake amongst young women: A systematic review. Acta Oncol 2014; 53:445-51.
[12] Sabatino, S.A., Lawrence, B., Elder, R., Mercer, S.L., Wilson, K.M., DeVinney, B., Melillo, S., Carvalho, M., Taplin, S., Bastani, R. and Rimer, B.K., 2012. Effectiveness of interventions to increase screening for breast, cervical, and colorectal cancers: nine updated systematic reviews for the guide to community preventive services. American Journal of Preventive Medicine, 43(1), pp.97-118.
[13] Crawford J, Ahmad F, Beaton D, Bierman AS. Cancer screening behaviors among South Asian immigrants in the UK, US, and Canada: A scoping study. Health Soc Care Community 2016; 24:123-53.
[14] McFarland DM, Gueldner SM, Mogobe KD (2016). Integrated review of barriers to cervical cancer screening in Sub-Saharan Africa. Journal of Nursing Scholarship, 48(5), 490-498.
[15] Lim JN, Ojo AA (2017). Barriers to utilization of cervical cancer screening in Sub Sahara Africa: A systematic review. Eur J Cancer Care (Engl) 2017;26. doi: 10.1111/ecc. 12444.
[16] Lu M, Moritz S, Lorenzetti D, Sykes L, Straus S, Quan H (2012). A systematic review of interventions to increase breast and cervical cancer screening uptake among Asian women. BMC Public Health 2012; 12:413.
[17] World Health Organization Screening for Cervical Cancer https://www.who.int/activities/screening-for-cervical-cancer accessed 30/01/2021.
[18] Agorye Ingwu, J. (2016). Knowledge and Screening Practices of Cervical Cancer among Pregnant Women Attending Antenatal Clinic in Tertiary Hospitals in Enugu, South-Eastern Nigeria. Journal of Cancer and Tumor International, 4(2), 1-9. https://doi.org/10.9734/JCTI/2016/27118.
[19] Schnatz P. F., Markelova N. V., Holmes D., Mandavilli S. R., and O’Sullivan D. M. (2008), “The prevalence of cervical HPV and cytological abnormalities in association with reproductive factors of rural Nigerian women,” Journal of Women’s Health, vol. 17, no. 2, pp. 279–285, 2008.
[20] Jeong S, Saroha E, Knight J, Roofe M, Jolly PE 2011. Determinants of adequate follow-up of an abnormal Papanicolaou result among Jamaican women in Portland, Jamaica. Cancer Epidemiol 2011; 35:211-6. 11.
[21] Hoque M, Hoque E, Kader SB. (2018) Evaluation of cervical cancer screening program at a rural community of South Africa. East Afr J Public Health 2008; 5:111-6. 12. Human papillomavirus (HPV) and cervical cancer.
[22] Uzochukwu, B., Onwujekwe, O., Soludo, E., Nkoli, E., & Uguru, N. (2009). The District Health System in Enugu state, Nigeria: an analysis of policy development and implementation. Enugu, Nigeria: Consortium for Research on Equitable Health Systems.
[23] WHO (2022) Cancer. Available at: https://www.who.int/health-topics/cancer#tab=tab_1 (Accessed 13th May 2022).
[24] Oketch SY, Kwena Z, Choi Y, Adewumi K, Moghadassi M, Bukusi EA, Huchko MJ. 2019. Perspectives of women participating in a cervical cancer screening campaign with community-based HPV self-sampling in rural western Kenya: a qualitative study. BMC Womens Health. 2019 Jun 13;19(1):75. doi: 10.1186/s12905-019-0778-2. PMID: 31196175.
[25] Udigwe, G. O. (2006). Knowledge, attitude, and practice of cervical cancer screening (pap smear) among female nurses in Nnewi Southeastern Nigeria. Nigerian Journal of clinical practice, 9(1), 40-43.
[26] Joseph, A., Olisaemeka, E. P., Chukwudi, O. R., Igwe, N. M., Agwu, M. R., & Egbuji, C. C. (2015). Frequency and pattern of gynecological cancers in a federal teaching hospital, Abakaliki, Nigeria. Journal of Basic and Clinical Reproductive Sciences, 4(2), 54-57.
[27] Chukwuali, L. I., Onuigbo, W. I., & Mgbor, N. C. (2003). Cervical Cancer Screening in Enugu, Nigeria. Tropical Journal of Obstetrics and Gynaecology, 20(2), 109-112.
[28] Dim C. C., Ezegwui H. U., Ikeme A. C., Nwagha U. I. & Onyedum C. C. (2011) Prevalence of cervical squamous intraepithelial lesions among HIV-positive women in Enugu, South-eastern Nigeria, Journal of Obstetrics and Gynaecology, 31:8, 759-762, DOI: 10.3109/01443615.2011.598967
[29] Daniel, G. O., Musa, J., Akindigh, T. M., Shinku, F., Shuaibu, S. I., Kwaghe, B., ... & Sagay, A. (2020). Prevalence and predictors of precancerous cervical lesions among HIV‐positive women in Jos, north‐central Nigeria. International Journal of Gynecology & Obstetrics, 151(2), 253-259.
[30] Ukah, C. O., & Nwofor, A. M. (2017). Cancer incidence in south-east Nigeria: a report from Nnewi cancer registry. Orient Journal of Medicine, 29(1-2), 48-55.
[31] Ajah, L. O., Ezeonu, P. O., Ozonu, N. C., Iyoke, C. A., Nkwo, P. O., & Ajah, M. I. (2015). A five-year review of cervical cytology in Abakaliki, Nigeria. Am J Cancer Prev, 3(2), 23-6.
[32] Ekwedigwe, K.C., Ezeonu, P.O., Edegbe, F., Esike, C., Agbata, A.T., Ukaegbe, C.I., Anozie, O.B., Asiegbu, O.G. and Isikhuemen, M., 2018. Prevalence and Pattern of Abnormal Pap Smear among Pregnant Women Attending Antenatal Clinic in a Missionary Hospital in Abakaliki, Southeast Nigeria. Open Journal of Obstetrics and Gynecology, 8(8), pp.728-740.
[33] Kani, Y. A., Muhammad, Y., Binji, A., Iliya, S., Adejumo, R., & Kamilu, I. M. (2020). Prevalence of cervical cancer-A 6-year Retrospective Study in Jigawa State, Nigeria. World Journal of Biology Pharmacy and Health Sciences, 4(1), 008-013.
[34] Gage, J. C., Ajenifuja, K. O., Wentzensen, N. A., Adepiti, A. C., Eklund, C., Reilly, M., ... & Schiffman, M. (2012). The age‐specific prevalence of human papillomavirus and risk of cytologic abnormalities in rural Nigeria: Implications for screen‐and‐treat strategies. International Journal of cancer, 130(9), 2111-2117.
[35] Nejo, Y. T., Olaleye, D. O., & Odaibo, G. N. (2018). Prevalence and risk factors for genital human papillomavirus infections among women in Southwest Nigeria. Archives of Basic and Applied Medicine, 6(1), 105.
[36] Kachalla, N. A., Isa, H., Bashir, M., & Yunana, S. Prevalence of Human Papilloma Virus among women of childbearing Age in Yola Adamawa State, Nigeria. UJMR, Volume 6 Number 2, December 2021, pp 24 – 29.
[37] Ezechi, O.C., Ostergren, P.O., Nwaokorie, F.O. et al. The burden, distribution, and risk factors for cervical oncogenic human papillomavirus infection in HIV-positive Nigerian women. Virol J 11, 5 (2014). https://doi.org/10.1186/1743-422X-11-5.
[38] Akarolo-Anthony, S.N., Al-Mujtaba, M., Famooto, A.O. et al. HIV associated high-risk HPV infection among Nigerian women. BMC Infect Dis 13, 521 (2013).
[39] Okolo, C., Franceschi, S., Adewole, I., Thomas, J.O., Follen, M., Snijders, P.J., Meijer, C.J. and Clifford, G.M., 2010. Human papillomavirus infection in women with and without cervical cancer in Ibadan, Nigeria. Infectious agents and cancer, 5(1), pp.1-4.
[40] Adegbesan Omilabu, M., Okunade, K., & Omilabu, S. (2014). Oncogenic human papillomavirus infection among women attending the cytology clinic of a tertiary hospital in Lagos, South-West Nigeria. Int J Res Med Sci, 2(2), 625.
[41] Mohammed, M. M. (2015). Prevalence of Cervical Human Papillomavirus Infection Among Women Presenting or Cervical Cancer Screening in Gombe North-Eastern Nigeria. Faculty of Pathology.
[42] Auwal, I. K., Aminu, M., Atanda, A. T., Tukur, J., & Sarkinfada, F. (2013). Prevalence and risk factors of high-risk human papillomavirus infections among women attending gynecology clinics in Kano, Northern Nigeria. Bayero Journal of pure and applied sciences, 6(1), 67-71.
[43] De Vuyst, H., Steyaert, S., Van Renterghem, L., Claeys, P., Muchiri, L., Sitati, S., Vansteelandt, S., Quint, W., Kleter, B., Van Marck, E. and Temmerman, M., 2003. Distribution of human papillomavirus in a family planning population in Nairobi, Kenya. Sexually transmitted diseases, pp.137-142.
[44] Salih, M.M., Safi, M.E., Hart, K. et al. Genotypes of human papillomavirus in Sudanese women with cervical pathology. Infect Agents Cancer 5, 26 (2010). https://doi.org/10.1186/1750-9378-5-26.
[45] Didelot-Rousseau, M.N., Nagot, N., Costes-Martineau, V., Valles, X., Ouedraogo, A., Konate, I., Weiss, H.A., Van de Perre, P., Mayaud, P. and Segondy, M., 2006. Human papillomavirus genotype distribution and cervical squamous intraepithelial lesions among high-risk women with and without HIV-1 infection in Burkina Faso. British Journal of Cancer, 95(3), pp.355-362.
[46] Leroy V, Ladner J, De Clercq A, Meheus A, Nyiraziraje M, Karita E, Dabis F (1999): Cervical dysplasia and HIV type 1 infection in African pregnant women: a cross-sectional study, Kigali, Rwanda. The Pregnancy and HIV Study Group (EGE). Sex Transm Infect 1999, 75(2):103–106.
[47] Yakub, M. M., Fowotade, A., Anaedobe, C. G., Manga, M. M., Bakare, R. A., & Abimiku, B. A. (2019). Human papillomavirus correlates of high-grade cervical dysplasia among HIV-Infected women at a major treatment center in Nigeria: a cross-sectional study. The Pan African Medical Journal, 33.
[48] Moodley J, Constant D, Hoffman M, Salimo A, Allan B (2009): Human papillomavirus prevalence, viral load, and pre-cancerous lesions of the cervix in women initiating highly active antiretroviral therapy in South Africa: a cross-sectional study. BMC Cancer 2009, 9(1):275.
[49] Blossom DB, Beigi RH, Farrell JJ, Mackay W, Qadadri B, Brown DR, Rwambuya S, Walker CJ, Kambugu FS, Abdul-Karim FW: Human papillomavirus genotypes associated with cervical cytologic abnormalities and HIV infection in Ugandan women. J Med Virol 2007, 79(6):758–765.
[50] Parham GP, Sahasrabuddhe VV, Mwanahamuntu MH, Shepherd BE, Hicks ML, Stringer EM, Vermund SH (2006): Prevalence and predictors of squamous intraepithelial lesions of the cervix in HIV-infected women in Lusaka, Zambia. Gynecol Oncol 2006, 103(3):1017–1022.
[52] Morhason-Bello Imran O., Kareem Yusuf Olushola, Adewole Isaac F. (2020). Modeling for Predictors of Knowledge Score on Etiology and Prevention Strategies for Cervical Cancer Among Women of Reproductive Age in Ibadan. JCO Global Oncology. 2020; (6): 892.
Viewed PDF 1718 101 -
 Community Health Posts Impact on Adult Male Access to HIV Services in Lusaka, ZambiaAuthor: Mwayabo Jean Claude KazadiDOI: 10.21522/TIJPH.2013.10.04.Art014
Community Health Posts Impact on Adult Male Access to HIV Services in Lusaka, ZambiaAuthor: Mwayabo Jean Claude KazadiDOI: 10.21522/TIJPH.2013.10.04.Art014Community Health Posts Impact on Adult Male Access to HIV Services in Lusaka, Zambia
Abstract:
Achieving HIV epidemic control is an ultimate goal for Zambia. To achieve this goal there is need to close services access gaps. Adult men are less likely to utilize existing health facility-based HIV services and they account for a significant proportion of new HIV infections with risk to onward HIV transmission in the community. Almost two-thirds of males (65.1%) and 79.2% of females aged 15-59 years reported ever having been tested for HIV and having received their results. Over two-thirds (67.1%) of HIV-positive males 25-29 years of age reported being unaware of their HIV status. Twenty-five percent of the national pandemic is in Lusaka. This non-experimental, descriptive mixed-methods study shows increase in number of adult males accessing services at community health posts and the impact of community health posts on improving adult male access to HIV services, including improved retention to HIV services and viral load suppression. The attitude or customer care of health care workers and the location of the community health posts played a bigger role in improving adult male access to HIV services, by creating a better, trusted environment and by bringing the services closer to where these males work or live. The community health post improved also the inequality in accessing HIV services for adult males, as this is one of the key factors to achieving the end of HIV pandemic.
Keywords: Community Health Post, Control, Epidemic, HIV, Impact, and Inequality, Male Adult.Community Health Posts Impact on Adult Male Access to HIV Services in Lusaka, Zambia
References:
[1] United Nations AIDS. (2020). UNAIDS DATA Report 2020. UNAIDS, (pp. 4-26). https://www.unaids.org/sites/default/files/media_asset/2020_aids-data-book_en.pdf. Accessed in April 2020.
[2] Zambia Central Statistical Office (2013). Population and Demographic Projections 2011 - 2035. Central Statistical Office. https://www.zamstats.gov.zm/phocadownload/Zambia%20Census%20Projection%202011%20-%202035.pdf. Accessed on August 4th, 2020.
[3] Population-Based HIV Impact Assessment. (2016). Zambia Population-Based HIV Impact Assessment Report. (pp. 6-129). https://phia.icap.columbia.edu/wp-content/uploads/2019/03/ZAMPHIA-Final-Report__2.26.19.pdf. Accessed on August 5th, 2020.
[4] Country Operational Plan. (2018). Strategic Direction Summary. PEPFAR Zambia. https://www.pepfar.gov/documents/organization/285848.pdf. Accessed on August 6th, 2020.
[5] World Health Organization. (2016). Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection. World Health Organization. https://www.who.int/hiv/pub/arv/arv-2016/en/. Accessed on August 6th, 2020.
[6] World Health Organization. (2017). Treat all: Policy adoption and implementation status in countries. World Health Organization. https://www.who.int/publications/i/item/treat-all-policy-adoption-and-implementation-status-in-countries. Accessed on August 7th, 2020.
[7] United Nations AIDS. (2019). Zambia Country factsheet. UNAIDS. http://aidsinfo.unaids.org/. Accessed on August 06, 2020.
[8] Sweat M, Morin S, Celentano D, Mulawa M, Singh B, Mbwambo J, et al. (2011). Community-based intervention to increase HIV testing and case detection in people aged 16–32 years in Tanzania, Zimbabwe, and Thailand (NIMH Project Accept, HPTN 043): a randomised study. The Lancet Infectious Diseases. 11(7):525-32.
[9] Medley AM, Hrapcak S, Golin RA, Dziuban EJ, Watts H, Siberry GK, et al. (2018). Strategies for Identifying and Linking HIV-Infected Infants, Children, and Adolescents to HIV Treatment Services in Resource Limited Settings. JAIDS Journal of Acquired Immune Deficiency Syndromes. 78: S98-S106.
[10] Govindasamy D, Meghij J, Negussi EK, Baggaley RC, Ford N, Kranzer K. (2014). Interventions to improve or facilitate linkage to or retention in pre-ART (HIV) care and initiation of ART in low- and middle-income settings – a systematic review. Journal of the International AIDS Society. 17(1):19032.
[11] Yeganeh N, Simon M, Mindry D, et al. (2017). Barriers and facilitators for men to attend prenatal care and obtain HIV voluntary counseling and testing in Brazil. PLoS One. 12(4): e0175505.
[12] Saldana, J. (2012). The coding manual for qualitative research, 2nd edition. Thousand oaks, CA: SAGE.
[13] Lincoln YS, Guba EG. (1985). Naturalistic inquiry. Beverly Hills: Sage.
[14] Guba, E., Lincoln, Y. (1989). Fourth generation evaluation. Newbury Park, CA:Sage.
[15] Brewer K. R. W., Hanif M. (1983). Sampling with unequal probabilities. Spring-verlag, New-York.
[16] Gari S, Martin-Hilber A, Malungo JR, Musheke M, Merten S. (2014). Sex differentials in the uptake of antiretroviral treatment in Zambia. AIDS Care;26(10):1258-62. doi: 10.1080/09540121.2014.897911. PMID: 24666201.
[17] Gonzalez, Monica M. (2016). The coding manual for qualitative research: a review. The Qualitative Report, vol. 21, no. 8, (pp. 1546+). Link.gale.com/apps/doc/A463514474/AONE?u=anon~a46004e3&sid=googleScholar&xid=0220d70d. Accessed 26 Aug. 2020.
[18] Berge Y. G., & Tille Y. (2009). Sampling with Unequal Probabilities. Handbook of Statistics 29, part a, 39-54.
[19] Hanif, M., & Brewer, K. R. W. (1980). Sampling with Unequal Probabilities without Replacement: A Review. International Statistical Review / Revue Internationale de Statistique, 48(3), 317–335. https://doi.org/10.2307/1402944.
[20] Beuving, J., & de Vries, G. (2015). On naturalistic inquiry: Key issues and practices. In Doing Qualitative Research: The Craft of Naturalistic Inquiry (pp. 27–46). Amsterdam University Press. https://doi.org/10.2307/j.ctt130h8g7.7.
[21] Beuving, J., & de Vries, G. (2015). Looking at society: Observing, participating, interpreting. In Doing Qualitative Research: The Craft of Naturalistic Inquiry (pp. 65–88). Amsterdam University Press. https://doi.org/10.2307/j.ctt130h8g7.9.
[22] Ammon N, Mason S, Corkery JM. (2018). Factors impacting antiretroviral therapy adherence among human immunodeficiency virus-positive adolescents in sub-Saharan Africa: a systematic review. Public Health.; 157:20– 31.
Viewed PDF 1249 54 -
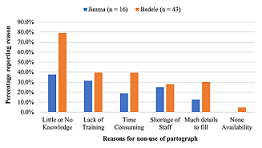 Factors Associated with partographs Utilization in Jimma and Bedele Zones, Oromia Regional State, EthiopiaAuthor: Polite DubeDOI: 10.21522/TIJPH.2013.10.04.Art015
Factors Associated with partographs Utilization in Jimma and Bedele Zones, Oromia Regional State, EthiopiaAuthor: Polite DubeDOI: 10.21522/TIJPH.2013.10.04.Art015Factors Associated with partographs Utilization in Jimma and Bedele Zones, Oromia Regional State, Ethiopia
Abstract:
Use of partographs during labor is a key intervention but it is not widely used due to various factors. This is one of the quality thematic areas incentivized by PBF. Hence the aim of our study was to determine these factors associated with utilization of partograph in Jimma and Buno-Bedelle zone. Our study adopted a cross-section design with independent control. The data collection was retrospective interview of 239 health workers who conducted deliveries in Q3 2021 (July – September 2021) in health facilities from both Buno-Bedele (control) and Jimma (intervention) zones. Bivariate analysis was performed using chi-squared tests. Multivariate analysis was performed using logistic regression analysis. All data analysis was conducted in STATA 15. The proportion of health workers using partographs was higher in Jimma (86.5%) compared to Bedele (64.4%), with a p-value less than 0.001. The finding of this study indicated that the major reasons for non-use of partographs were little/no knowledge, lack of training and shortage of staff and time consuming. Knowledge of partograph, availability of partograph and training on partograph have a positive impact on use of partographs as shown by the statistically significant adjusted odds ratios (AORs) in Table 4. Midwives were also found to be more likely to use partographs compared to nurses. This study revealed that PBF contributed to availability of partographs, improved knowledge score and training on partograph utilization in Jimma. PBF have also improved the use pf partographs for monitoring labour and understanding of action lines in early diagnosis of complications during labour.
Keywords: Factors, Partographs, Performance based financing, Utilization and Completeness.
Factors Associated with partographs Utilization in Jimma and Bedele Zones, Oromia Regional State, Ethiopia
References:
[1] WHO. Trends in maternal mortality 2000 to 2017: estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division. Geneva: World Health Organization, 2019.
[2] Countdown to 2015-decade report (2000–10): taking stock of maternal, newborn, and child survival. Bhutta, Z. A., Chopra, M., Axelson, H., Berman, P., Boerma, T., Bryce, J., & Wardlaw, T. 2015, The lancet, 375(9730), pp. 2032-2044.
[3] Global, regional, and national levels of maternal mortality, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Kassebaum, N. J., Barber, R. M., Bhutta, Z. A., Dandona, L., Gething, P. W., Hay, S. I., & Ding, E. L. 2016, The Lancet, 388(10053)., pp. 1775-1812.
[4] The use and perceived barriers of the partograph at public health institutions in East Gojjam Zone, Northwest Ethiopia. Zelellw, D., Tegegne, T. 1, s.l.: Annals of global health, 2018, Vol. 84. 198.
[5] Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN Maternal Mortality Estimation Inter-Agency Group. Alkema, L., Chou, D., Hogan, D., Zhang, S., Moller, A. B., Gemmill, A., ... & Inter, U. N. M. M. E. 10017, s.l.: The lancet, 2016, Vol. 387. 462-474.
[6] FMOH, EPHI. National maternal death surveillance and response annual report 2008 EFY. s.l.: Federal Democratic Republic of Ethiopia Ministry of Health (FMOH) EPHI, 2017.
[7] Indicators, K. Mini Demographic and Health Survey. s.l.: EPHI and ICF, 2019.
[8] Level of partograph utilization and its associated factors among obstetric caregivers at public health facilities in East Gojam Zone, Northwest Ethiopia. Zelellw, D. A., & Tegegne, T. K. 2018, PloS one, 13(7).
[9] Magnitude of partograph use and factors that affecting its utilization among obstetric caregivers in public health institutions of West Showa Zone. Oromia Regional state, Ethiopia. Willi, W. 2015.
[10] Effect of partograph use on outcomes for women in spontaneous labour at term and their babies. Lavender, T., Cuthbert, A., & Smyth, R. M. 2018, Cochrane database of systematic reviews, (8).
[11] Maternal mortality from obstructed labor: a MANDATE analysis of the ability of technology to save lives in sub-Saharan Africa. Harrison, M. S., Griffin, J. B., McClure, E. M., Jones, B., Moran, K., & Goldenberg, R. L. 09, s.l.: American Journal of Perinatology., 2016, Vol. 33. 873-881.
[12] The use of the partograph in labor monitoring: a cross-sectional study among obstetric caregivers in General Hospital, Calabar, Cross River State, Nigeria. Asibong, U., Okokon, I. B., Agan, T. U., Oku, A., Opiah, M., Essien, E. J., & Monjok, E. s.l.: International Journal of Women’s Health, 2014, Vol. 6. 873.
[13] Partograph utilization as a decision-making tool and associated factors among obstetric care providers in Ethiopia: a systematic review and meta-analysis. Ayenew, A. A., & Zewdu, B. F. 2020, Systematic reviews, 9(1), pp. 1-11.
[14] Assessment of partograph utilization and associated factors among obstetric care givers at public health institutions in central zone, Tigray, Ethiopia. Hailu, T., Nigus, K., Gidey, G., Hailu, B., & Moges, Y. 2018, BMC research notes, 11(1)., pp. 1-6.
[15] Partograph utilization and associated factors among obstetric care providers in North Shoa Zone, Central Ethiopia: a cross sectional study. Wakgari, N., Amano, A., Berta, M., & Tessema, G. A. 2015, African health sciences, 15(2), pp. 552-559.
[16] Magnitude of partograph use and associated factors among obstetric care givers in public health institution in Sidama Zone, Southern Ethiopia. Eshetu, K., Hussen, E., & Dulla, D. 6, s.l.: Diversity and Equality in Health and Care., 2017, Vol. 14.
[17] Effect of partogram use on outcomes for women in spontaneous labour at term. Lavender, T., Hart, A., Smyth, R.M. s.l.: Cochrane Database Syst Rev., 2013, Vol. 7.
[18] Effect of Partogram Use on Outcomes for Women in Spontaneous Labour at Term: RHL Commentary. Soni, B. L. Geneva: World Health Organization, 2009, The WHO Reproductive Health Library.
[19] Partograph revisited. N., Magon. 1, 2011, Int J Clin Cases Investig, Vol. 3.
[20] Partograph Utilization and Factors Associated with Poor Perinatal Outcomes in Wolaita Sodo University Referral Hospital, Southern Ethiopia. Chemeda, G., Teklewold, B., & Daka, K. s.l.: Journal of Health, Medicine, and Nursing., 2019, Vol. 63.
[21] Health professional’s knowledge and use of the partograph in public health institutions in eastern Ethiopia: a cross-sectional study. Mezmur, H., Semahegn, A., Tegegne, B. S. 1, s.l.: BMC pregnancy and childbirth., 2017, Vol. 17. 1-7.
[22] Partograph in management of labour. World Health Organization maternal health and safe motherhood programme. WHO. s.l.: Lancet, 1994, Vol. 343. 1399-1404.
[23] Obstetric care in low-resource settings: what, who, and how to overcome challenges to scale up? Hofmeyr, G. J., Haws, R. A., Bergström, S., Lee, A. C., Okong, P., Darmstadt, G. L., ... & Lawn, J. E. 2009, International Journal of Gynecology & Obstetric (107)., pp. 21-45.
[24] Contemporary patterns of spontaneous labor with normal neonatal outcomes. Zhang, J., Landy, H. J., Branch, D. W., Burkman, R., Haberman, S., Gregory, K. D., & Reddy, U. M. 2010, Obstetrics, and gynecology,116(6)., p. 1281.
[25] A Practical Guide: The Partograph Part I, Principles and Strategy WHO. World Health Organisation. Division of Family Health. Labour, W. P. P. s.l.: Maternal Health and Safe Motherhood Practical Guide: WHO/FHE/MSM/93.8., 1994, Safe Motherhood Practical Guide: WHO/FHE/MSM/93.8.
[26] Low utilization of partograph and its associated factors among obstetric care providers in governmental health facilities at West Shoa Zone, Central Ethiopia. Bedada, K. E., Huluka, T. K., & Bulto, G. A. 2020, International Journal of Reproductive Medicine.
[27] Utilization of Partograph and its associated factors among midwives working in public health institutions, Addis Ababa City Administration, Ethiopia. Hagos, A. A., Teka, E. C., & Degu, G. 2017, BMC pregnancy and childbirth, 20(1), pp. 1-9.
[28] Incidence, causes and outcome of obstructed labor in jimma university specialized hospital. . Fantu, S., Segni, H., & Alemseged, F. 2010, Ethiopian Journal of Health Sciences, 20(3).
[29] The partograph for the prevention of obstructed labor. Clinical obstetrics and gynecology, 52(2), 256-269. Mathai, M. 2009, Clinical obstetrics, and gynecology, 52(2)., pp. 256-269.
[30] Assessment of knowledge and utilization of the partograph among health professionals in Amhara region. Abebe, F., Birhanu, D., Awoke, W., Ejigu, T. 2, 2013, Ethiopia Science Journal of Clinical Medicine, Vol. 2, pp. 26 - 42.
[31] Partograph utilization and associated factors among obstetric care providers in North Shoa Zone, Central Ethiopia: a cross sectional study. Wakgari, N., Amano, A., Berta, M., & Tessema, G. A. 2, s.l.: African Health Sciences, 2015, Vol. 15. 552-559.
[32] A cross-sectional study of partograph utilization as a decision-making tool for referral of abnormal labour in primary health care facilities of Bangladesh. Khan, A. N. S., Billah, S. M., Mannan, I., Mannan, I. I., Begum, T., Khan, M. A., & Graft-Johnson, J. D. 2018, Plos one, 13(9).
[33] Knowledge and utilization of the partograph: A cross-sectional survey among obstetric care providers in urban referral public health institutions in northwe and southwest Cameroon. Sama, C. B., Takah, N. F., Danwe, V. K., Melo, U. F., Dingana, T. N., & Angwafo III, F. F. 2017, Plos one 12(2).
[34] Knowledge and utilization of the partograph among obstetric care givers in southwest Nigeria. African Journal of Reproductive Health. Fawole, A. O., Hunyinbo, K. I., & Adekanle, D. A. 2008, African Journal of Reproductive Health, 12(1), pp. 22-29.
[35] Knowledge and utilization of the partograph among midwives in the Niger Delta Region of Nigeria. Opiah, M. M., Ofi, A. B., Essien, E. J., & Monjok, E. 2012, African Journal of Reproductive Health, 16(1), pp. 125-132.
[36] Utilization of the partograph and its associated factors among obstetric care providers in the Eastern zone of Tigray, Northern Ethiopia. Gebreslassie, G. W., Weldegeorges, D. A., Assefa, N. E., Gebrehiwot, B. G., Gebremeskel, S. G., Tafere, B. B., ... & Welesamuel, T. G. 2019, The Pan African Medical Journal (34).
[37] Partograph Utilization and Associated Factors among Obstetric Care Providers Working in Public Health Facilities of Wolaita Zone. Markos, M., Arba, A., & Paulos, K. 2020, Journal of Pregnancy.
[38] Partograph utilization and associated factors among obstetric care providers at public health facilities in Hadiya Zone, Southern Ethiopia. Haile, Y., Tafese, F., Weldemarium, T. D., & Rad, M. H. 2020, Journal of Pregnancy 2020.
[39] Knowledge and utilization of partograph among health care professionals in public health institutions of Bale zone, Southeast Ethiopia. Markos, D., & Bogale, D. 2016, Public health (137), pp. 162-168.
[40] Knowledge and utilization of partograph among obstetric care givers in public health institutions of Addis Ababa, Ethiopia. Yisma, E., Dessalegn, B., Astatkie, A., & Fesseha, N. 2013, BMC Pregnancy and Childbirth, 13(1), pp. 1-9.
[41] Partograph utilization as a decision-making tool and associated factors among obstetric care providers in Ethiopia: a systematic review and meta-analysis. Ayenew, A. A., & Zewdu, B. F. 2020, Systematic Reviews, 9(1)., p. 251.
[42] Looking into the performance-based financing black box: evidence from an impact evaluation in the health sector in Cameroon. de Walque, Damien, et al. 6, 2021, Health Policy and Planning, Vol. 36.
[43] Communities of practice: the missing link for knowledge management on implementation issues in low-income countries? Meessen, Bruno, et al. 8, 2011, Vol. 16.
[44] Performance-based financing: the same is different. Meessen, Bruno, et al. 2017, Health Policy and Planning.
[45] Output-based payment to boost staff productivity in public health centres: contracting in Kabutare District, Rwanda. Meessen, Bruno, Kashala, Jean-Pierre I and Musango, Laurent. 2007, Bulletin of the World Health Organization, pp. 108-115.
[46] Effects of pay for performance in health care: A systematic review of systematic reviews. Eijkenaar, Frank, et al. 2-3, 2013, Health Policy, Vol. 110.
[47] Effect on maternal and child health services in Rwanda of payment to primary health-care providers for performance: an impact evaluation. Basinga, P., et al. 2011, The Lancet, pp. 1421-1428.
[48] Paying for performance’ in Rwanda: Does it pay off? Kalk, A., Paul, F. A. and Grabosch, E. 2010, Tropical Medicine & International Health, pp. 182-190.
[49] Performance-based financing for better quality of services in Rwandan health centres: 3-year experience. Rusa, Louis, et al. 7, 2009, Tropical Medicine & International Health, Vol. 14.
[50] A Conditional Cash Transfer Program in the Philippines Reduces Severe Stunting. Kandpal, Eeshani, et al. 9, 2016, The Journal of Nutrition, Vol. 146.
[51] Can performance-based financing be used to reform health systems in developing countries? Ireland, Megan, Paul, Elisabeth and Dujardin, Bruno. 9, 2011, Bulletin of the World Health Organization, Vol. 89.
[52] Taking Results-Based Financing from Scheme to System. Shroff, Zubin Cyrus, et al. 2, 2017, Health Systems & Reform, Vol. 3.
[53] Why there is so much enthusiasm for performance-based financing, particularly in developing countries. Soeters, Robert and Vroeg, Piet. 9, 2011, Bulletin of the World Health Organization, Vol. 89.
[54] The national free delivery policy in Nepal: early evidence of its effects on health facilities. Witter, S., et al. 2, 2011, Health Policy and Planning, Vol. 26.
[55] Studying the link between institutions and health system performance: a framework and an illustration with the analysis of two performance-based financing schemes in Burundi. Bertone, M. P. and Meessen, B. 8, 2013, Health Policy and Planning, Vol. 28.
[56] Does training on performance-based financing make a difference in performance and quality of health care delivery? Health care provider’s perspective in Rungwe Tanzania. Manongi, Rachel, et al. 1, 2014, BMC Health Services Research, Vol. 14.
[57] Performance-based financing with GAVI health system strengthening funding in rural Cambodia: a brief assessment of the impact. Matsuoka, S., et al. 4, 2014, Vol. 29.
[58] A realist review to assess for whom, under what conditions and how pay for performance programmes work in low- and middle-income countries. Singh, Neha S., et al. 2021, Social Science & Medicine, Vol. 270.
[59] The Quality of Care. Donabedian, A. 12, 1988, JAMA, Vol. 260.
[60] Impact of Performance-Based Financing (PBF) Program on Utilization and Completeness of Partographs in Jimma. Dube, P., et al. 3, 2022, Texila International Journal of Academic Research, Vol. 9, pp. 83-95.
[61] Use of the partogram by doctors and midwives at Odi District Hospital, Gauteng, South Africa. Maphashaa, O. M., Govender, I., Motloba, D. P., & Barua, C. 2017, South African Family Practice, 59(2), pp. 82-86.
[62] Use and completion of partograph during labour is associated with a reduced incidence of birth asphyxia: a retrospective study at a peri-urban setting in Ghana. Anokye, R., Acheampong, E., Anokye, J., Budu-Ainooson, A., Amekudzie, E., Owusu, I., ... & Mprah, W. K. 2019, Journal of Health, Population and Nutrition, 38(1)., pp. 1-8.
[63] Partograph use among Midwives in the Gambia. Badjie, B., Kao, C. H., Gua, M. L., & Lin, K. C. 2013, African Journal of Midwifery and Women’s Health, 7(2), pp. 65-69.
[64] Assessment of partogram use during labour in rujumbura health Sub district, Rukungiri district, Uganda. Ogwang, S., Karyabakabo, Z., & Rutebemberwa, E. 2009, African Health Sciences, 9(2).
[65] Use of the partogram by doctors and midwives at Odi District Hospital, Gauteng, South Africa. . Maphashaa, O. M., Govender, I., Motloba, D. P., & Barua, C. 2017, South African Family Practice, 59(2)., pp. 82-86.
[66] Helping midwives in Ghana to reduce maternal mortality. Floyd, L. 2013, African Journal of Midwifery and Women’s Health, 7(1), pp. 34-38.
[67] Care/Engender Health, Fistula. Improving partograph use in Uganda through coaching and mentoring. New York: Fistula Care., 2013.
[68] An exploration of the unintended consequences of performance-based financing in 6 primary healthcare facilities in Burkina Faso. Turcotte-Tremblay, A.M., Gali Gali, I.A., Ridde, V. 2, 2022, International Journal Health Policy Management., Vol. 11. 145–159.
[69] Partograph utilization and associated factors among graduating health professional students in Asella Referal and Teaching Hospital, Ethiopia, 2016. Bekele, D., Beyene, K., Hinkosa, L., & Shemsu, M. N. 2, s.l.: STM Journal., 2016, Vol. 6.
[70] Partograph utilization and associated factors among obstetric care givers in governmental health institutions of Jigjiga and Degehabur towns, Somali region, Ethiopia: A cross-sectional study. Ayehubizu, L.M., Tibebeu, A.T., Fetene, M.T., Yohannes, S.H., Yadita, Z.S. 3, s.l.: Plos One, 2022, Vol. 17.
Viewed PDF 1162 57 -
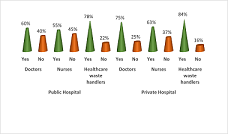 Assessment of Healthcare Waste Management Strategies in Selected Hospitals in Abuja, NigeriaAuthor: Agbanusi Uchechukwu JonathanDOI: 10.21522/TIJPH.2013.10.04.Art016
Assessment of Healthcare Waste Management Strategies in Selected Hospitals in Abuja, NigeriaAuthor: Agbanusi Uchechukwu JonathanDOI: 10.21522/TIJPH.2013.10.04.Art016Assessment of Healthcare Waste Management Strategies in Selected Hospitals in Abuja, Nigeria
Abstract:
Improper healthcare waste management practices, capable of contributing to poor human health and negative environmental impacts, inundate Abuja hospitals. Therefore, the purpose of this study is to assess risk perceptions and awareness among healthcare workers handling hospital waste in Abuja, Nigeria. In this study, mixed methods design of quantitative approach using cross-sectional study and qualitative approach using descriptive case study were applied to explore the risk perceptions and awareness of healthcare waste handlers within the four selected (two public and two private) hospitals in Abuja. Coding and analysis of the quantitative and qualitative data helped in triangulation, which improved the quality of work. Major trends found through investigations, include that: most Abuja hospitals were fraught with poor healthcare waste management practices; healthcare waste attendants handling hospital waste in Abuja seldom appreciate the danger involved; there exists risky exposures of hospital waste to human health; coupled with negative environmental impacts. Summary of interpretation for the study points at improper healthcare waste management practices.
Keywords: Environmental impacts, Healthcare waste management, Healthcare workers, Human health, planned behaviour theory, Risk perception, social care, Waste Management Theory.Assessment of Healthcare Waste Management Strategies in Selected Hospitals in Abuja, Nigeria
References:
[1] Path 2009 Achieving effective sharps waste management in GAVI host countries. A proposed approach with estimates of cost 2006 http://.www.Path.org/files/TS_ach_eff_swm.pdf.
[2] Tudor, Terry (2005). Towards the development of a standardised measurement unit for healthcare waste generation. Journal of Resources, Conservation and Recycling. DOI - 10.1016/j.resconrec.2006.06.007.
[3] Ferreira A.P., Veiga MM (2003). Hospital waste operational procedures: A case study in Brazil. Waste Manage. Res., 21: 377-382.
[4] Da Silva CE, Hoppe AE, Ravanello MM, Mello N (2005). Medical waste Management in the south of Brazil. Waste Manage. 25: 600-605.
[5] WHO (1985). Management of waste from hospitals and other health care establishments.
[6] Report on a WHO meeting, Bergen, 28 June–1 July 1983. Copenhagen, World Health Organization Regional Office for Europe (EURO Reports and Studies, No. 97).
[7] Gai, R.; Xu, L.; Li, H.; Zhou, C.; He, J.; Yoshihisa, S.; Wei, T.; Chushi, K. Investigation of healthcare waste management in Binzhou District, China. Waste Manag. 2010, 30, 246–250.
[8] Sapkota, B.; Kumar Gupta, G.; Mainali, D. Impact of intervention on healthcare waste management practices in a tertiary care governmental hospital of Nepal. BMC Public Health 2014, 14, 1005.
[9] Tabash, M.I.; Hussein, R.A. Mahmoud, A.H.; El-Borgy, M.D.; Abu-Hamad, B.A. Impact of an intervention programme on knowledge, attitude, and practice of healthcare staff regarding pharmaceutical waste management, Gaza, Palestine. Public Health 2016, 138, 127-137.
[10] Stanley H. O. Okpara K. E. Chukwujekwu D. C. Agbozu I. E. Nyenke C. U. 2011 Health care waste management in Port Harcourt Metropolis American Journal of Scientific and Industrial Research 25769773.
[11] Abah S. O. Ohimain E. I. 2010 Assessment of Dumpsite Rehabilitation Potential using the Integrated Risk Based Approach: A case study of Eneka, Nigeria. WorldAppl ju. Sci. J., 8 4 436 442.
[12] Keiski, Pongrácz and Phillips (2004). Evolving the Theory of Waste Management: Defining key concepts}, Conference proceedings.
[13] Ajzen, Icek (1985). “From Intentions to Actions: A Theory of Planned Behavior”. In Kuhl, Julius; Beckmann, Jürgen (eds.). Action Control: From Cognition to Behavior. Springer. pp. 11–39. ISBN 978-3-642-69748-7.
[14] Icek Ajzen. Theory of planned behavior. Organizational behavior and human decision processes 50 (2), 179-211, 1991. 88632,1991.
[15] Adegbita, M. A., Nwafor, S. O., Afon, A., Abegunde, A. A., & Bamise, C. T. (2010).
[16] Assessment of dental waste management in a Nigerian tertiary hospital. Waste. manag. Res., 28, 769-777.
[17] Olubukola BO (2009). Comparative Analysis of Health Care Waste Management Practice in Two General Hospitals in Nigeria. Available at http://www.eco-web.com/edi/index.htm.
[18] Phengxay S. Okumura J. Miyoshi M. Sakisaka K. Kuroiwa C. Phengxay M. 2005 Healthcare Waste Management in Lao PDR: A case study, Waste. Manage. Res., 23 571 581.
[19] Patton, M. Q. (1999). Enhancing the Quality and Credibility of Qualitative Analysis. Health Services Research, 34, 1189-1208.
[20] Bassey B. E. Benka-Coker M. O. Aluyi H. S. A. 2006 Characterization and management of solid medical wastes in the Federal Capital Territory, Abuja Nigeria African Health Sciences, 6 1 58 63.
[21] World Bank (2020) “Solid Waste Management.” Retrieved September 2020.
[22] Nmere, Obasi & Okolo, Victor & Okechukwu, James & Alio, Felix & Anetoh, John. (2020). Influence of public relations’ media public enlightenment campaign and community participation strategies on waste management. Problems and Perspectives in Management. 18. 82-96. 10.21511/ppm.18(1).2020.08.
Viewed PDF 1061 46 -
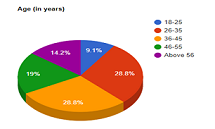 Self-Prescribed Pharmacological Drugs Used for Covid-19 Prevention and Treatment in the Current PandemicAuthor: Olalekan FagbolaDOI: 10.21522/TIJPH.2013.10.04.Art017
Self-Prescribed Pharmacological Drugs Used for Covid-19 Prevention and Treatment in the Current PandemicAuthor: Olalekan FagbolaDOI: 10.21522/TIJPH.2013.10.04.Art017Self-Prescribed Pharmacological Drugs Used for Covid-19 Prevention and Treatment in the Current Pandemic
Abstract:
The practice of using pharmacological drugs not prescribed by qualified medical practitioners is a worrying trend especially in the ongoing Covid-19 pandemic. It is a global issue that has attracted the attention of physicians and various stakeholders in the health care systems in developing and developed countries. Such practice is associated with overdosage, allergic reaction, infection resistant to antibiotic, wrong diagnosis, delay in seeking treatment at health facilities and drug addiction. This study assessed the prevalence of self-prescribed antibiotics, analgesics, vitamins, and minerals by a cross section of burgesses in the Prices Town Regional Corporation (PTRC) in South Trinidad to treat and prevent Covid-19 infection. A descriptive cross-sectional survey in online and paper and pencil questionnaire formats was conducted from February 2022 to April 2022 on 286 self-selected participants from a population of 1000 residents. Data entry and analysis conducted after merging them using Google Charts. Prevalence of Ivermectin was 9.44%, Zithromax 3.15, Steroids 3.5% Panadol 33.6%, Vitamins C 63.3%, Zinc 60.8%, D3 55.2 %, and B Complex 11.9%. Multivariate analysis performed on dependent and independent variables showed that the use of self-prescribed medication was significantly associated with age group 26-35 years (COR 0.15, p0.00129, 95% CI 0.04, 0.51 at significance level of p≤0.05) and marital status of being separated from spouses (COR 2.48, p0.0229, 95% CI 1.02, 6.06, significance level of p≤0.05). More females practiced self-medication compared to males. The researcher recommends health education to curb the practice.
Keywords: Prevalence, Treatment, Self-prescribed antimicrobials, Analgesic, Vitamins, Covid-19, Pandemic, Infection.Self-Prescribed Pharmacological Drugs Used for Covid-19 Prevention and Treatment in the Current Pandemic
References:
[1] Nasir, M., Talha, K. A., Chowdhury, A.S. M., Zahan, T., Rawshan, Perveen, R. A. (2020). Prevalence, Pattern and Impact of Self Medication of Anti-infective Agents During Covid-19 Outbreak in Dhaka City. 10.21203/rs.3.rs-57011/v1. file:///C:/Users/Fagbola/Downloads/Prevalence_Pattern_and_Impact_of_Self_Medication_o.pdf].
[2] Sankaranarayanan, R. (2017). Can we classify cross- sectional studies into analytical studies? Retrieved from: https://www.researchgate.net/post/Dear-all-Can-we-classify-cross-sectional-studies-into-analytical-studies/589dea50eeae39590619ad32/citation/download.
[5] Wegbom, A. I, Edet, C. K., Raimi, O., Fagbamigbe, A. F., and Kiri. VA., (2021) Self-Medication Practices and Associated Factors in the Prevention and/or Treatment of Covid-19 Virus: A Population-Based Survey in Nigeria. Front. Public Health. https://doi.org/10.3389/fpubh.2021.606801.
[7] Adebisi, Y.A., Jimoh, N.D., and Ogunkola, I. O. (2021). The use of antibiotics in Covid-19 management: a rapid review of national treatment guidelines in 10 African countries. Trop Med Health 49, 51 (2021). https://doi.org/10.1186/s41182-021-00344-w.
[8] Locquet, Médéa; Diep, Anh Nguyet; Beaudart, Charlotte; Dardenne, Nadia; Brabant, Christian; Bruyère, Olivier; Donneau, A. Françoise. (2021). A systematic review of prediction models to diagnose Covid-19 in adults admitted to healthcare centers. Arch Public Health; 79(1): 105, 2021 Jun 18. DOI: 10.1186/s13690-021-00630-3.
[9] Popp, M., Stegemann, M., Riemer, M., Metzendorf, M-I., Romero, C. S., Mikolajewska, A., Kranke, P., Meybohm, P., Skoetz, N., and Weibel, S. (2021). Antibiotics for the treatment of Covid-19. Cochrane Database of Systematic Reviews 2021, Issue 10. Art. No.: CD015025. DOI: 10.1002/14651858.CD015025.
[10] Tekeba, A., Ayele, Y., Negash, B., & Gashaw, T. (2021). Extent of and Factors Associated with Self-Medication among Clients Visiting Community Pharmacies in the Era of Covid-19: Does It Relieve the Possible Impact of the Pandemic on the Health-Care System? Risk management and healthcare policy, 14, 4939–4951. https://doi.org/10.2147/RMHP.S338590.
[11] Del-Toro-Rubio, M., Bohórquez-Moreno, C., Díaz-Pérez, A., and Barrios-Puerta, Z. (2020). Factors associated with self-medication in adolescents in the rural area of Cartagena, Colombia. Arch Med (Manizales) 2020; 20(2):356-363. https://doi.org/10.30554/archmed.20.2.3697.2020.
[12] Abdelwahed RNK, Jassem M, Alyousbashi A. Self-Medication Practices, Prevalence, and Associated Factors among Syrian Adult Patients: A Cross-Sectional Study. J Environ Public Health. 2022 Jun 28; 2022:9274610. doi: 10.1155/2022/9274610. PMID: 35800339; PMCID: PMC9256391.
[13] Hughes, C. M., McElnay, J. C., & Fleming, G. F. (2001). Benefits and risks of self-medication. Drug safety, 24(14), 1027–1037. https://doi.org/10.2165/00002018-200124140-00002.
[14] WHO (2000). World Health Organization Guidelines for the Regu latory Assessment of Medicinal Products for use in Self-Medication. https://apps.who.int/iris/bitstream/handle/10665/66154/WHO_EDM_QSM_00.1_eng.pdf.
[15] Topinková, E., Baeyens, J.P., Michel, JP. et al. (2012). Evidence-Based Strategies for the Optimization of Pharmacotherapy in Older People. Drugs Aging 29, 477–494 (2012). https://doi.org/10.2165/11632400-000000000-00000.
[16] Montastruc, J. L., Bagheri, H., Geraud, T., & Lapeyre-Mestre, M. (1997). Pharmacovigilance de l’automédication [Pharmacovigilance of self-medication]. Therapie, 52(2), 105–110. https://pubmed.ncbi.nlm.nih.gov/9231503/.
[17] Fair, R. J., & Tor, Y. (2014). Antibiotics and bacterial resistance in the 21st century. Perspectives in medicinal chemistry, 6, 25–64. https://doi.org/10.4137/PMC.S14459.
[18]Banić Tomišić, Z. (2011). The Story of Azithromycin. Kemija u industriji/Journal of Chemists and Chemical Engineers. 60. 603-617. https://www.researchgate.net/publication/286136408_The_Story_of_Azithromycin/citation/download.
[19] Hauk L. (2014). AAP releases guideline on diagnosis and management of acute bacterial sinusitis in children one to 18 years of age. American family physician, 89(8), 676–681.https://pubmed.ncbi.nlm.nih.gov/24784128/.
[20] Oldenburg CE, Pinsky BA, Brogdon J, et al. Effect of Oral Azithromycin vs Placebo on Covid-19 Symptoms in Outpatients With SARS-CoV-2 Infection: A Randomized Clinical Trial. JAMA. 2021;326(6):490–498. doi:10.1001/jama.2021.11517. https://jamanetwork.com/journals/jama/fullarticle/2782166.
[21] Dorobisz, K., Dorobisz, T., Janczak, D., & Zatoński, T. (2021). Doxycycline in the Coronavirus Disease 2019 Therapy. Therapeutics and clinical risk management, 17, 1023–1026. https://doi.org/10.2147/TCRM.S314923.
[22] Chivese, T., Omran A.H., Musa, G. H., Al-Wattary, N., Badran, S., Soliman, N., Ahmed T.M., Matizanadzo, J., Mohamed M. M., Thalib, E. L., and Suhail A.R. (2021). Efficacy of chloroquine and hydroxychloroquine in treating Covid-19 infection: A meta-review of systematic reviews and an updated meta-analysis, Travel Medicine and Infectious Disease, Volume 43, 2021, 02135, ISSN 1477-8939, https://doi.org/10.1016/j.tmaid.2021.102135.
[26] Caly. L., Druce J.D., Catton, M.G., Jans, D.A., Wagstaff, K.M. The FDA-approved drug ivermectin inhibits the replication of SARS-CoV-2 in vitro. Antiviral Research, Volume 178, 2020,104787, ISSN 0166 3542, https://doi.org/10.1016/j.antiviral.2020.104787. (https://www.sciencedirect.com/science/article/pii/S0166354220302011).
[28] Babalola, O. E., Bode, C. O., Ajayi, A. A., Alakaloko, F. M., Akase, I. E., Otrofanowei, E., Adeyemo, A. O., and Omilabu, S. (2021) change to 2022. Ivermectin shows clinical benefits in mild to moderate covid-19: a randomized controlled double blind dose response study in Lagos. medRxiv 2021.01.05.21249131; doi: https://doi.org/10.1101/2021.01.21249131.
[29] Baracaldo-Santamaría, D., Pabón-Londoño, S., & Rojas-Rodriguez, L. C. (2022). Drug safety of frequently used drugs and substances for self-medication in Covid-19. Therapeutic advances in drug safety, 13, 20420986221094141. https://doi.org/10.1177/20420986221094141.
[35] Manjani, L., Desai, N., Kohli, A., Arya, R., Woods, C., and Desale, S. (2021). Effects of acetaminophen on outcomes in patients hospitalized with Covid-10. Presented at: CHEST 2021; October 17-20, 2021; Orlando, FL/Virtual. Abstract A1072. https://journal.chestnet.org/article/S0012-3692(21)02443-0/fulltext#relatedArticles.
[36] Sestili P, Fimognari, C. (2020). Paracetamol‐Induced Glutathione Consumption: Is There a Link with Severe Covid‐19 Illness? Front Pharmacol. 2020;11: 579944. 10.3389/fphar.2020.579944 https://www.frontiersin.org/articles/10.3389/fphar.2020.579944/full.
[37] Pandolfi, S., Simonetti, V., Ricevuti, G., & Chirumbolo, S. (2021). Paracetamol in the home treatment of early Covid-19 symptoms: A possible foe rather than a friend for elderly patients? Journal of medical virology, 93(10), 5704–5706. https://doi.org/10.1002/jmv.27158.
[38] Kelleni M. T. (2022). NSAIDs and Kelleni’s protocol as potential early Covid-19 treatment game changer: could it be the final countdown? Inflammopharmacology, 30(1), 343–348. https://doi.org/10.1007/s10787-021-00896-7.
[39] Wijaya, I., Andhika, R., Huang, I., Purwiga, A., & Budiman, K. Y. (2021). The effects of aspirin on the outcome of Covid-19: A systematic review and meta-analysis. Clinical epidemiology and global health, 12, 100883. https://doi.org/10.1016/j.cegh.2021.100883.
[40] Voruganti, D., Bassareo, P. P. and Calcaterra, G. (2022). Does aspirin save lives in patients with Covid-19? Heart 2022; 108:88-89. https://heart.bmj.com/content/108/2/88.citation-tools.
[41] Mosleh, G., Badr, P., Zaeri, M., & Mohagheghzadeh, A. (2021). Potentials of Antitussive Traditional Persian Functional Foods for Covid-19 Therapy†. Frontiers in pharmacology, 12, 624006. https://doi.org/10.3389/fphar.2021.624006.
[42] Zhang, D. H., Zhang, X., Peng, B., Deng, S. Q., Wang, Y. F., Yang, L., Zhang, K. Z., Ling, C. Q., & Wu, K. L. (2020). Network pharmacology suggests biochemical rationale for treating Covid-19 symptoms with a Traditional Chinese Medicine. Communications biology, 3(1), 466. https://doi.org/10.1038/s42003-020-01190-y.
[43] Esam Z. (2020). Protective potential of expectorants against Covid-19. Medical hypotheses, 142, 109844. https://doi.org/10.1016/j.mehy.2020.109844.
[48] Jurowski, K., Szewczyk, B., Nowak, G., & Piekoszewski, W. (2014). Biological consequences of zinc deficiency in the pathomechanisms of selected diseases. Journal of biological inorganic chemistry: JBIC: a publication of the Society of Biological Inorganic Chemistry, 19(7), 1069–1079. https://doi.org/10.1007/s00775-014-1139-0.
[50] Tan, B., Chew, N., Lee, G., Jing, M., Goh, Y., Yeo, L., Zhang, K., Chin, H. K., Ahmad, A., Khan, F. A., Shanmugam, G. N., Chan, B., Sunny, S., Chandra, B., Ong, J., Paliwal, P. R., Wong, L., Sagayanathan, R., Chen, J. T., Ng, A., Sharma, V. K. (2020). Psychological Impact of the Covid-19 Pandemic on Health Care Workers in Singapore. Annals of internal medicine, 173(4), 317–320. https://doi.org/10.7326/M20-1083.
[51] Ragan, I., Hartson, L., Pidcoke, H., Bowen, R., & Raymond P. (2020). Pathogen reduction of SARS-CoV-2 virus in plasma and whole blood using riboflavin and UV light. doi: https://doi.org/10.1101/2020.05.03.074971.
[52] Mikkelsen, K., Stojanovska, L., Prakash, M., & Apostolopoulos, V. (2017). The effects of vitamin B on the immune/cytokine network and their involvement in depression. Maturitas, 96, 58–71. https://doi.org/10.1016/j.maturitas.2016.11.012.
[53] Shakoor, H., Feehan, J., Al Dhaheri, A., Ali, H., Platat, C., Ismail, L., Apostolopoulos, V., Stojanovska, L. (2020). Immune-boosting role of vitamins D, C, E, zinc, selenium, and omega-3 fatty acids: Could they help against Covid-19? Maturitas. 143. 10.1016/j.maturitas.2020.08.003.
[56] Schlueter, A. K., & Johnston, C. S. (2011). Vitamin C: Overview and Update. Journal of Evidence-Based Complementary & Alternative Medicine, 49–57. https://doi.org/10.1177/1533210110392951.
[58] Pisoschi, A.M., et al. (2021) Oxidative Stress Mitigation by Antioxidants—An Overview on Their Chemistry and Influences on Health Status. European Journal of Medicinal Chemistry, 209, Article ID: 112891. https://doi.org/10.1016/j.ejmech.2020.112891.
[59] Science, M., Maguire, J. L., Russell, M. L., Smieja, M., Walter, S. D., & Loeb, M. (2013). Low serum 25-hydroxyvitamin D level and risk of upper respiratory tract infection in children and adolescents. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America, 57(3), 392–397. https://doi.org/10.1093/cid/cit289.
[60] Aglipay, M., Birken, C. S., Parkin, P. C., Loeb, M. B., Thorpe, K., Chen, Y., Laupacis, A., Mamdani, M., Macarthur, C., Hoch, J. S., Mazzulli, T., Maguire, J. L., & TARGet Kids! Collaboration (2017). Effect of High-Dose vs Standard-Dose Wintertime Vitamin D Supplementation on Viral Upper Respiratory Tract Infections in Young Healthy Children. JAMA, 318(3), 245–254. https://doi.org/10.1001/jama.2017.8708.
[63] Olayemi J, Olayinka B, Musa I. (2010). Evaluation of Antibiotic Self-Medication Pattern Amongst Undergraduate Students of Ahmadu Bello University (Main Campus), Zaria. Journal Applied Sciences and Engineering Technology, 2(1): 35-38. https://maxwellsci.com/print/rjaset/v2-35-38.pdf.
[65] Amaha. M. H., Alemu, B.M, and Atomsa, G. E. (2019) Self-medication practice and associated factors among adult community members of Jigjiga town, Eastern Ethiopia. PLoS ONE 14(6): e0218772. https://doi.org/10.1371/journal.pone.0218772.
[66] Alshammari F, Alobaida A, Alshammari A, Alharbi A, Alrashidi A, Almansour A, Alremal A and Khan KU (2021) University Students’ Self-Medication Practices and Pharmacists’ Role: A Cross-Sectional Survey in Hail, Saudi Arabia. Front. Public Health 9:779107. doi: 10.3389/fpubh.2021.779107.
[67] Zeru N, Fetene D, Geberu DM, Melesse AW, Atnafu A. Self-Medication (2020): Practice and Associated Factors Among University of Gondar College of Medicine and Health Sciences Students: A Cross-Sectional Study. Patient Prefer Adherence. 2020; 14:1779-1790
https://doi.org/10.2147/PPA.S274634.[68] Makowska, M., Boguszewski, R., Nowakowski, M., & Podkowińska, M. (2020). Self-Medication-Related Behaviors and Poland’s Covid-19 Lockdown. International Journal of Environmental Research and Public Health, 17(22), 8344. MDPI AG. Retrieved from http://dx.doi.org/10.3390/ijerph17228344.
[69] Shaamekhi, H. R., Asghari Jafarabadi, M., & Alizadeh, M. (2019). Demographic determinants of self-medication in the population covered by health centers in Tabriz. Health promotion perspectives, 9(3), 181–190. https://doi.org/10.15171/hpp.2019.26.
[70] Demissie, F., Ereso, K., & Paulos, G. (2022). Self-Medication Practice with Antibiotics and Its Associated Factors Among Community of Bule-Hora Town, Southwest Ethiopia. Drug, healthcare, and patient safety, 14, 9–18. https://doi.org/10.2147/DHPS.S325150.
[71] Bello, I, B., Akinnawo, E, O., Akpunne, B, O., Mopa-Egbunu, A. (2022). Knowledge of Covid-19 and preventive measures on self-medication practices among Nigerian undergraduates, Cogent Arts & Humanities, 9:1, 2049480, DOI: 10.1080/23311983.2022.2049480. https://doi.org/10.1080/23311983.2022.2049480.
Viewed PDF 936 15 -
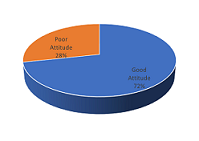 Knowledge, Attitude, and Practice of Cervical Cancer Among Women of Childbearing Age in Enugu State, Southeast NigeriaAuthor: Ajegbo Uzoma ChidinmaDOI: 10.21522/TIJPH.2013.10.04.Art018
Knowledge, Attitude, and Practice of Cervical Cancer Among Women of Childbearing Age in Enugu State, Southeast NigeriaAuthor: Ajegbo Uzoma ChidinmaDOI: 10.21522/TIJPH.2013.10.04.Art018Knowledge, Attitude, and Practice of Cervical Cancer Among Women of Childbearing Age in Enugu State, Southeast Nigeria
Abstract:
Cervical cancer (CCa) is the fourth most frequent cancer in women worldwide, and the second most common cancer in women living in developing countries. The study was done to determine the knowledge, attitude, and practice of CCa prevention strategies among women of childbearing age in Enugu State, Nigeria. A descriptive cross-sectional study of 450 eligible women in Enugu State who were selected by proportionate stratified random sampling method. Data were collected electronically using KoboCollect app. Chi-square and bivariate logistic regression model for statistical significance association estimates at 95% C I and, P < 0.05 were done. The mean knowledge score was 3.38 ± 5.009 out of 29 points, with only 5.1% of the respondents classified as having good knowledge. Muslims/traditionalists were 9.6 times more likely than Christians to have good CCa knowledge (95% CI OR= 2.037 – 45.394). Respondents with secondary education were 8 times less likely than those with tertiary education to have good CCa knowledge (95% CI OR 0.034 – 0.415). Majority (71.6%) of the respondents were classified as having a good attitude. Respondents with good CCa knowledge were 4.4 times more likely to have right CCa prevention attitude compared to those with poor knowledge (95% CI OR= 0.053 – 0.985). 3.8% and 8.2% of the respondents have ever screened for CCa and received HPV immunization respectively. Although the knowledge and practice were very low, the CCa prevention attitude was good. Therefore, we recommend targeted awareness and enlightenment of the public about CCa to achieve optimal timely detection and treatment.
Keywords: Cervical Cancer (CCa); Enugu State, KAP, Women of Childbearing Age; Southeast; Nigeria.Knowledge, Attitude, and Practice of Cervical Cancer Among Women of Childbearing Age in Enugu State, Southeast Nigeria
References:
[1] Eke N., Ezeama, C., Eke, C., Eleje G., Akabuike, J. and Ezebialu, I. (2010) ‘Knowledge of Cervical Cancer and its Screening Amongst Female Workers in Nnewi, Nigeria’, Afrimedic Journal, Vol. 1 (1), pp. 31-36.
[2] BMC Cancer, Comprehensive Knowledge About Cervical Cancer Is Low Among Women In Northwest Ethiopia, Published: 02 January 2013 https://bmccancer.biomedcentral.com/articles/10.1186/1471-2407-13-2#author-information accessed 20/01/2021.
[3] Tsu VD, Levin CE: Making the case for cervical cancer prevention: what about equity. Reproductive Health Matter. 2008, 16 (32): 104-112. 10.1016/S0968-8080(08)32411-2.
[4] Ogunbode OO, Ayinde OA (2005). Awareness of Cervical Cancer and Screening in a Nigerian Female Market Population. Annals of African Medicine. 2005;4(4):160.
[5] Adanu RM: Cervical cancer knowledge and screening in Accra, Ghana. J Wom Health Gend Base Med. 2002, 11 (6): 487-488. 10.1089/152460902760277822.
[6] Getahun, F., Mazengia, F., Abuhay, M., & Birhanu, Z. (2013). Comprehensive knowledge about cervical cancer is low among women in Northwest Ethiopia. BMC cancer, 13(1), 1-7.
[7] Twinomujuni C, Nuwaha F, Babirye JN (2015). Understanding the Low level of cervical cancer screening in Masaka Uganda using the ASE model: a community-based survey. PLoS One. 2015;10(6): e0128498.
[8] Mukama, T., Ndejjo, R., Musabyimana, A., Halage A, Musoke D (2017). Women’s knowledge and attitudes towards cervical cancer prevention: a cross sectional study in Eastern Uganda. BMC Women’s Health 17, 9 (2017). Mutyaba T, Mmiro F, Weiderpass E (2006). Knowledge, attitudes, and practices on cervical cancer screening among the medical workers of Mulago Hospital, Uganda. BMC Med Educ. 2006; 6:13.
[9] Lyimo FS, Beran TN (2012). Demographic, knowledge, attitudinal, and accessibility factors associated with uptake of cervical cancer screening among women in a rural district of Tanzania: three public policy implications. BMC Public Health. 2012;12(1):22.
[10] Lim J, Ojo A (2016). Barriers to utilization of cervical cancer screening in Sub Sahara Africa: a systematic review. Eur J Cancer Care. 2016.
[11] Moser K, Patnick J, Beral V. Inequalities in reported use of breast and cervical screening in Great Britain: analysis of cross-sectional survey data. BMJ. 2009;338: b2025.
[12] Ebu, N. I., Mupepi, S. C., Siakwa, M. P., & Sampselle, C. M. (2015). Knowledge, practice, and barriers toward cervical cancer screening in Elmina, Southern Ghana. International journal of women’s health, 7, 31.
[13] Sudenga SL, Rositch AF, Otieno WA, Smith JS (2013). Brief report: knowledge, attitudes, practices and perceived risk of cervical cancer among Kenyan women. Int J Gynecol Cancer. 2013 Jun;23(5):895–899.
[14] Balogun MR, Odukoya OO, Oyediran MA, Ujomi PU. Cervical cancer awareness and preventive practices: a challenge for female urban slum dwellers in Lagos, Nigeria. Afr J Reprod Health.2012 Mar;16(1):75–82.
[15] Igwilo AI, Igwilo UU, Hassan F, Idanwekhai M, Igbinomwanhia O, Popoola AO (2010). The knowledge, attitude, and practice of the prevention of cancer of the cervix in Okada Community. Asian Journal of Medical Sciences. 2012;4(3):95–98.
[16] Olubodun, T., Odukoya, O. O., & Balogun, M. R. (2019). Knowledge, attitude, and practice of cervical cancer prevention, among women residing in an urban slum in Lagos, Southwest, Nigeria. Pan African Medical Journal, 32(1).
[17] Wright KO, Aiyedehin O, Akinyinka MR, Ilozumba O (2014). Cervical cancer: community perception and preventive practices in an urban neighborhood of Lagos (Nigeria) ISRN Preventive Medicine. 2014; 2014:950534.
[18] Nwozor CM, Oragudosi AL (2013). Awareness and uptake of cervical cancer screening among women in Onitsha, South-East, Nigeria. Greener Journal of Medical Sciences. 2013;3(8):283–288.
[19] Ugwu, E. O., Obi, S. N., Ezechukwu, P. C., Okafor, I. I., & Ugwu, A. O. (2013). Acceptability of human papilloma virus vaccine and cervical cancer screening among female health-care workers in Enugu, Southeast Nigeria. Nigerian journal of clinical practice, 16(2), 249-252.
[20] Agboola, A. and Bello, O. (2021) ‘The determinants of knowledge of cervical cancer, attitude towards screening and practice of cervical cancer prevention amongst antenatal attendees in Ibadan, Southwest Nigeria’, ecancer medical science, Vol. 1, pp.1-12.
[21] Ojiyi E, Dike EI (2008). Knowledge and Practice of cervical Cancer Screening at Imo State University Orlu. Port Harcourt Med J. 2008; 2:145 150.
[22] Feyi-Waboso, P. A., Kamanu, C., & Aluka, C. (2005). Awareness and risk factors for cervical cancer among women in Aba, south-eastern Nigeria. Tropical Journal of Obstetrics and gynaecology, 22, 25-26.
[23] Obiechina, N. J. A., & Mbamara, S. U. (2009). Knowledge attitude and practice of cervical cancer screening among sexually active women in Onitsha, southeast Nigeria. Nigerian Journal of Medicine, 18(4).
[24] Eze, J. N., Umeora, O. U., Obuna, J. A., Egwuatu, V. E., & Ejikeme, B. N. (2012). Cervical cancer awareness and cervical screening uptake at the Mater Misericordiae Hospital, Afikpo, Southeast Nigeria. Annals of African medicine, 11(4), 238.
[25] John-Akinola, Y. O., Oluwasanu, M. M., & Oladepo, O. (2021). Urban Poor Community Settings’ Knowledge and Screening Practices for Cervical Cancer in Ibadan, Nigeria. JCO Global Oncology, 7, 1024-1031.
[26] Udigwe, G. O. (2006). Knowledge, attitude, and practice of cervical cancer screening (pap smear) among female nurses in Nnewi Southeastern Nigeria. Nigerian journal of clinical practice, 9(1), 40-43.
[27] Ezem, B. U. (2007). Awareness and uptake of cervical cancer screening in Owerri, South-Eastern Nigeria. Annals of African medicine, 6(3), 94.
[28] Aboyeji PA, Ijaiya MA, Jimoh AA. Knowledge, attitude and practice of cervical smear as a screening procedure for cervical cancer in Ilorin, Nigeria. Tropical Journal of Obstetrics and Gynaecology 2004; 21:114-117.
[29] Ayinde AE, Adewale IF, Babarinsa IA. Trends in cervical smear screening in Ibadan, Nigeria. A four-year review. West Afr J Med 1998; 19:25-30 Ayinde O, Omigbodun A. Knowledge, attitude, and practices related to prevention of cancer of the cervix among female health workers in Ibadan. Journal of Obstetrics and Gynecology, Vol. 23 (1), pp. 59- 62.
[30] Akujobi, C. N., Ikechebelu, J. I., Onunkwo, I., & Onyiaorah, I. V. (2008). Knowledge, attitude and practice of screening for cervical cancer among female students of a tertiary institution in Southeastern Nigeria. Nigerian Journal of Clinical Practice, 11(3), 216-219.
[31] Olaniyan OB, Agboghoroma OC, Ladepo OP (2000). Knowledge and Practice of Cervical Screening among Female Health Workers in Government Hospitals in Abuja Metropolis Nigeria. Trop J Obstet Gynaecol 2000; 17(11):18 20.
[32] Anikwe Chidebe Christian, Osuagwu Philip Chidubem, Ikeoha Cyril Chijioke, Dimejesi Okechukwu B Ikechukwu, Okorochukwu Bartholomew Chukwunonye (2021). Cervical Cancer: Assessment of Its Knowledge, Utilization of Services and Its Determinant Among Female Undergraduate Students in a Low Resource Setting. International Quarterly of Community Health Education. 2021; 0272684X21.
[33] Asiedu Mercy N., Agudogo Júlia S., Dotson Mary E., Skerrett Erica, Krieger Marlee S., Lam Christopher T., Agyei Doris, Amewu Juliet, Asah-Opoku Kwaku, Huchko Megan, Schmitt John W., Samba Ali, Srofenyoh Emmanuel, Ramanujam Nirmala (2020). A novel speculum-free imaging strategy for visualization of the internal female lower reproductive system. Scientific Reports. 2020; 10(1).
[35] Yahya Anisah, Ismail Zubair Hadi, Bawa Umma Suleiman (2020). Awareness and utilization of cervical cancer screening services among primary health care providers in Zaria. Annals of African Medical Research. 2020; 2(2).
[36] Seow A, Wong ML, Smith WC, Lee HP (1995). Beliefs and Attitudes as Determinants of Cervical Cancer Screening: A Community-Based Study in Singapore. Preventive Medicine. 1995; 24(2):134- 41.
[37] Anyebe EE, Opaluwa SA, Muktar HM, Phili P F (2014). Knowledge and practice of cervical cancer screening amongst nurses in Ahmadu Bello University Teaching Hospital Zaria. Research on Humanities and Social Sciences Vol.4 (27), pp. 33- 40.
[38] Esin MN, Bulduk S, Ardic A Beliefs About Cervical Cancer Screening Among Turkish Married Women. J Cancer Educ. 2011 Feb 19.
[39] Gharoro EP, Ikeanyi EN. (2006) An Appraisal of the Level of Awareness and Utilization of the Pap smear as a Cervical Cancer Screening Test among Female Health Workers in a Tertiary Health Institution. International Journal of Gynecological Cancer 2006; 16:1063–1068.
[40] Oluwole, E. O., Mohammed, A. S., Akinyinka, M. R., & Salako, O. (2017). Cervical cancer awareness and screening uptake among rural women in Lagos, Nigeria. Journal of Community Medicine and Primary Health Care, 29(1), 81-88.
[41] Okunowo, A. A., Daramola, E. S., Soibi-Harry, A. P., Ezenwankwo, F. C., Kuku, J. O., Okunade, K. S., & Anorlu, R. I. (2018). Women’s knowledge of cervical cancer and uptake of Pap smear testing and the factors influencing it in a Nigerian tertiary hospital. Journal of cancer Research and Practice, 5(3), 105-111.
[42] Yahya A, Mande A (2019). Awareness and knowledge of cervical cancer and its screening methods among women attending primary healthcare centers in Zaria, North‑Western, Nigeria. Trop J Obstet Gynaecol. 2019; 36:271–276.
[43] Ingwu J 2017. Knowledge and screening practices of cervical cancer among pregnant women attending antenatal clinic in tertiary hospitals in Enugu, South-Eastern knowledge, and screening practices of cervical cancer among pregnant women attending antenatal clinic in ter. J Cancer Tumor Int. 2017;4(2):1–9.
[44] Idowu, A., Olowookere, S.A., Fagbemi, A.T. and Ogunlaja, O.A., 2016. Determinants of cervical cancer screening uptake among women in Ilorin, North Central Nigeria: a community-based study. Journal of cancer epidemiology, 2016.
[48] McFarland DM, Gueldner SM, Mogobe KD (2016). Integrated review of barriers to cervical cancer screening in Sub-Saharan Africa. Journal of Nursing Scholarship, 48(5), 490-498.
[49] Tebeu PM, Major AL, Rapiti E, Petignat P, Bouchardy C (2007). The Attitude and Knowledge of
Cervical Cancer by Cameroonian women: A Clinical Survey Conducted in Maroua, the capital of Far North Province of Cameroon. International Journal of Gynecological Cancer 2007.[51] Aniebue, P., Onwasigwe, C., Ndu, A., Ezeoke, U. and Aniebue, U. (2001) ‘Perception, Attitude and Practice of Cancer Screening among female doctors and nurses in Enugu’, International Journal of Medicine and Health Development, Vol. 6(2), pp. 78-80.
[52] Ogochukwu, T. N., Akabueze, J., Ezeome, I. V., Aniebue, U. U., & Oranu, E. O. (2017). Vaccination against human Papilloma virus in adolescent girls: mother’s knowledge, attitude, desire, and practice in Nigeria. J Infect Dis Preve Med, 5(151), 2.
[53] Awodele, O., Adeyomoye, A. A. A., Awodele, D. F., Kwashi, V., Awodele, I. O., & Dolapo, D. C. (2011). A study on cervical cancer screening amongst nurses in Lagos University Teaching Hospital, Lagos, Nigeria. Journal of Cancer Education, 26(3), 497-504.
[54] Sherris J, Castro W, Lewin C, Dzuba I, Arossi S. The Case for Investing in Cervical Cancer Prevention. Cervical Cancer Prevention Issues in Depth no. 3. Alliance for Cervical Cancer Prevention (ACCP) 2004, Seattle. Available at www.path.org/ files/RH_accp_case.pdf.
[55] Aniebue, P. N., & Aniebue, U. U. (2010). Awareness and practice of cervical cancer screening among female undergraduate students in a Nigerian university. Journal of Cancer Education, 25(1), 106-108.
Viewed PDF 1298 64 -
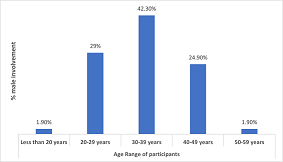 Factors Influencing Male Involvement in the Prevention of Mother-to-Child Transmission of HIV: The Missing Component in Test and Start in Kumba Health DistrictAuthor: Athanasius Fang EbuaDOI: 10.21522/TIJPH.2013.10.04.Art019
Factors Influencing Male Involvement in the Prevention of Mother-to-Child Transmission of HIV: The Missing Component in Test and Start in Kumba Health DistrictAuthor: Athanasius Fang EbuaDOI: 10.21522/TIJPH.2013.10.04.Art019Factors Influencing Male Involvement in the Prevention of Mother-to-Child Transmission of HIV: The Missing Component in Test and Start in Kumba Health District
Abstract:
Prevention of Mother to child Transmission (PMTCT) programs has been proven to be effective in reducing the risk of HIV transmission from mother to child. Men participation in PMTCT programs is likely to increase women’s uptake of PMTCT services. Unfortunately, men involvement in this intervention has been very minimal. Thus, identifying the factors that influences male involvement in the PMTCT programs is imperative. The study was a hospital and community base quantitative cross-sectional survey of 200 pregnant women attending antenatal clinic ANC/PMTCT clinic and 200 men in the Kumba Health District community using structured questionnaire. Ethical clearance was obtained from Faculty of health sciences University of Buea. Each health area in the district represented a stratum. Women were sampled at the clinics and men in the community. Written consent was obtained from all participants. Data was analyzed using SPSS version 26 at 95% confident interval and P<0.05 for statistical significance. Result. 52(13%) of male respondents had attended PMTCT services in the district with their partners which is far below the 80% standard set by the ministry of Public Health of Cameroon. Of the 200 male respondents 94(47%) had heard about PMTCT programs (p=0.001). Knowledge on HIV transmission through breast feeding (P=0.001) were highly significant, likewise level of education (P=0.003) and employment of participants (P=0.001). Despite the successful implementation of the Test and START in Kumba Health District, eliminating MTCT of HIV remains a major challenge.
Keywords. ANC, ARV, HIV, Male Involvement, MTCT, PMTCT.Factors Influencing Male Involvement in the Prevention of Mother-to-Child Transmission of HIV: The Missing Component in Test and Start in Kumba Health District
References:
[1] Unaids. Prevention gap report. Annual. Geneva-Switzerland: UNAIDS, UNAIDS; 2016 https://www.unaids.org/sites/default/files/media_asset/2016-prevention-gap-report_en.pdf.
[2] World Health Oganisation. Global AIDS Response Progress Reporting. Annual. Geneva: WHO, HIV/AIDS; 2021. Report No.: ISBN 978 92 4 150934 3 (WHO) https://www.unaids.org/sites/default/files/media_asset/JC2702_GARPR2015guidelines_en.pdf.
[3] UNAIDS. GLOBAL HIV STATISTICS. FACT SHEET. Geneva: UNAIDS, UNAIDS; 2021. https://www.unaids.org/en/resources/fact-sheet.
[4] CDC/PEPFAR. Cameroon Country Operational Plan COP 2021: Strategic Summary. Annual. Yaounde: CDC, HIV; 2021. https://www.state.gov/wp-content/uploads/2021/09/Cameroon_SDS_Final-Public_Aug-11-2021.pdf.
[5] World Health Organisation. Current issues. Annual. Geneva: WHO, HIV/AIDS; 2021 November https://www.who.int/health-topics/hiv-aids#tab=tab_1.
[6] UNAIDS. Understanding Fast-Track: Accelerating Action to End to end the AIDS Epidemic by 2030. Annual. UNAIDS, HIV; 2021 October. https://www.unaids.org/sites/default/files/media_asset/201506_JC2743_Understanding_FastTrack_en.pdf.
[7] Nsagha DS, Gregory HEE, Claude NS, Marcelin NN, Boniface N. The Role of the Male Partner in the Prevention of Mother to Child Transmission of HIV in Cameroon. American Journal of Epidemiology and Infectious Disease. 2014; 2(2): 52-59. http://pubs.sciepub.com/ajeid/2/2/1/index.html.
[8] Southwest Regional Technical Group. PMTCT Report. Annual. Kumba: Kumba Health District, PMTCT; 2021.
[9] Brittain K. Male partner involvement during pregnancy: The missing component in PMTCT adherence in Khayelitsha? Master of Public Health Thesis. Cape Town: University of Cape Town, Epidemiology; 2014. https://core.ac.uk/download/pdf/185413517.pdf.
[10] Katz DA, Kiarie JN, John-Stewart GC, et al. Male perspectives on incorporating men into antenatal HIV counseling and testing. Pub Med [PMC free article]. 2009; 6(2). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2765726/.
[11] Theuring S, Mbezi P, Luvanda H, et al. Male involvement in PMTCT services in Mbeya Region, Tanzania. Pub Med [PMC free article]. 2009; 8(2). https://pubmed.ncbi.nlm.nih.gov/19308720/.
[12] Makoni A, Chemhuru M, Chimbetete C, Gombe N, Mungeti M, Bangwe D, et al. Factors associated with male involvement in the prevention of mother to child transmission of HIV, Midlands Province, Zimbabwe, 2015 - a case control study. BMC Public Health BMC sries. 2016 April; 4(213). https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-016-2939-7
[13] Zubairu Iliyasu , Isa S Abubakar , Hadiza S Galadanci , Muktar H Aliyu. Birth preparedness, complication readiness and fathers’ participation in maternity care in a northern Nigerian community. Afr J Reprod Health. 2010 March; 14(1): 21-32. https://pubmed.ncbi.nlm.nih.gov/20695136/.
[14] Godlove N Nkuoh,, Dorothy J Meyer , Pius M Tih , Joseph Nkfusai. Barriers to men’s participation in antenatal and prevention of mother-to-child HIV transmission care in Cameroon, Africa. J Midwifery Womens Health. 2010 August; 55(4): 363-9. https://pubmed.ncbi.nlm.nih.gov/20630363/.
[15] Matongo L, Hang’andua A, Nzala HB, Malebe T. Exploring determinants of male involvement in PMTCT programs in Chibombo district of central province of Zambia. Asian Journal of Multidisciplinary Studies. 2014 September; 2(12). http://dspace.unza.zm/bitstream/handle/123456789/4013/Matongo%20HL.pdf?sequence=1&isAllowed=y.
[16] Alinane Linda Nyondo, Angela Faith Chimwaza , Adamson Sinjani Muula. Stakeholders’ perceptions on factors influencing male involvement in prevention of mother to child transmission of HIV services in Blantyre, Malawi. BMC Public Health volume. 2014 July; 291(14): 2-12. https://bmcpublichealth.biomedcentral.com/articles/10.1186/1471-2458-14-691.
[17] Byamugisha R TJSNTT. Determinants of male involvement in the prevention of mother-to-child transmission of HIV programme in Eastern Uganda: a cross-sectional survey. Reprod Health. 2010 February; 7(12). https://reproductive-health-journal.biomedcentral.com/articles/10.1186/1742-4755-7-12.
[18] Abuhay Y, AL, &FN. Male involvement in prevention of mother to child transmission of HIV and associated factors among males in Addis Ababa, Ethiopia. American Journal of Health Research. 2014 February; 2(6): 338-343. https://www.sciencepublishinggroup.com/journal/paperinfo.aspx?journalid=656&doi=10.11648/j.ajhr.20140206.13.
[19] Amsalu ATG, &AAA. Level of male partner involvement and associated factors in prevention of mother to child transmission of HIV/AIDS services in Debremarkos town, Northwest Ethiopia. African Journal of AIDS and HIV Research. 2013 December; 1(2). https://www.semanticscholar.org/paper/Level-of-male-partner-involvement-and-associated-in-Amsalu-Tiruneh/d4b24a5ee8551f04e9f719ac80aed23a07d3115c.
[20] Marelign Tilahun, Shikur Mohamed. Male Partners involvement in the Prevention of Mother-To-Child Transmission oo HIV and associated factors in Arba Minch Town and Arba Minch Woreda, Southern Ethiopia. BioMed Research International. 2015 October; 4(12): 7-15. https://bmcresnotes.biomedcentral.com/articles/10.1186/s13104-020-05023-3.
[21] Daniel Ww. Biostatistics: A Foundation for Analysis in the Health Sciences. Ninth ed. Jacobs J, editor. Danvers: Laurie Rosatone; 2009. https://faculty.ksu.edu.sa/sites/default/files/145_stat_-_textbook.pdf.
[22] Kalembo FW, Zgambo M, Mulaga AN, et al. Association between male partner involvement and the uptake of prevention of mother-to-child transmission of HIV (PMTCT) interventions in Mwanza district, Malawi: a retrospective cohort study. Pub Med [PMC free article]. 2013; 16(5). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3680434/.
[23] Mbezi PB. Factors affecting the levels of male involvement in the prevention of mother to child transmission of HIV in Mbeya City. Master’s Thesis. Mbeya: Muhimbili University of Health and Applied Sciences, Tanzania., Public Health; 2010.
[24] Morfaw F, Mbuagbaw L, Thabane L, et al. Male involvement in prevention programs of mother to child transmission of HIV: a systematic review to identify barriers and facilitators. Syst Rev. Pub Med [PMC free article]. 2013 January; 5(2): 46-53. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3599633/.
[25] Said M. Factors influencing Prevention of Mother to Child Transmission (PMTCT) outcomes in the Rundu District of Namibia. Master’s Thesis. Stellenbosch: University of Stellenbosch, South Africa., Public Health; 2014.
[26] Osman RJ, U, AU, MHA, Adpa AS, &MK. Barriers to male involvement in uptake of Prevention-of-Mother-to-Child-Transmission (PMTCT) of HIV in Sub-Saharan Africa. IOSR Journal of Nursing and Health Sciences. 2012 July; 3(5). http://iosrjournals.org/iosr-jnhs/papers/vol3-issue5/Version-1/A03510107.pdf.
[27] Auvinen J KJ. Male involvement and prevention of mother-to-child transmission of HIV in Sub-Saharan Africa: an integrative review. Bentham Science. 2013 August; 11(2): 169 - 177. https://www.eurekaselect.com/article/50061.
[28] Adeleke O. Male partner involvement in the prevention of mother-to-child transmission (PMTCT) of HIV Pogram in Mthatha, South Africa. Master Thesis. Mthatha: University of Stellenboch, South Africa, Public Health; 2013. https://scholar.sun.ac.za/handle/10019.1/80259.
[29] Kevin Koo, Jennifer D. Makin, Brian W. C. Forsyth. Barriers to male-partner participation in programs to prevent mother-to-child HIV transmission in South Africa. AIDS Educ Prev. 2013 February; 25(1): 14–24. https://pubmed.ncbi.nlm.nih.gov/23387948/.
[30] Dunlap J, Foderingham N, Bussell S, Wester CW, Audet CM, Muktar H Aliyu. Male involvement for the prevention of mother-to-child HIV transmission: A brief review of initiatives in East, West, and Central Africa. Current HIV/AIDS Reports. 2014 June; 11(2): 109-118. https://europepmc.org/article/med/24633806.
[31] Kalembo FW ZMMAea. Association between male partner involvement and the uptake of prevention of mother-to-child transmission of HIV (PMTCT) interventions in Mwanza district, Malawi: a retrospective cohort study. Plos one. 2013 June; 8(6): 5-12. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3680434/.
[32] Rebecca John Osman, Regine Unkels, Umar Aliyu, Habiba A, Otonoku K. Mathew. Barriers to male involvement in uptake of Prevention-of-Mother-to-Child-Transmission (PMTCT) of HIV in Sub-Saharan Africa. IOSR Journal of Nursing and Health Sciences. 2014 July; 3(5): 01-07. https://iosrjournals.org/iosr-jnhs/papers/vol3-issue5/Version-1/A03510107.pdf.
[33] Michael Reece, Ariane Hollub , Mabel Nangami , Karin Lane. Assessing male spousal engagement with prevention of mother-to-child transmission (pMTCT) programs in western Kenya. AIDS Care. 2010 June; 22(2): 43-50. https://pubmed.ncbi.nlm.nih.gov/20461572/.
[34] Ramon L, Cui, R.R, Muessig K. E, Thirumurthy, H, Tucker, J. D. Incentivizing HIV/STI testing a systematic review of the literature. AIDS Behav. 2014 November; 18(1): 5-12. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3966986/.
[35] Chanuan Uakarn, Kajohnsak Chaokromthong , Nittaya Sintao. Sample Size Estimation using Yamane and Cochran and Krejcie and Morgan and Green Formulas and Cohen Statistical Power Analysis by G*Power and Comparisons. Apheit International Journal. 2021 December; 10(2): 79-80.
Viewed PDF 1134 22 -
 Acceptability of HIV Test and Treat among Women and Men Seeking Health Care at Monze Mission HospitalAuthor: Chilabi KasongoDOI: 10.21522/TIJPH.2013.10.04.Art020
Acceptability of HIV Test and Treat among Women and Men Seeking Health Care at Monze Mission HospitalAuthor: Chilabi KasongoDOI: 10.21522/TIJPH.2013.10.04.Art020Acceptability of HIV Test and Treat among Women and Men Seeking Health Care at Monze Mission Hospital
Abstract:
The HIV test and treat strategy removes many barriers that interrupt HIV intervention. The Test and Treat campaign is an important strategy such that it promotes the general public access various promotive, preventive and treatment services. The aim of the study was to determine the acceptability of HIV Testing and Treatment and factors that influence acceptance among women and men seeking health care at Monze Mission Hospital. A cross-sectional study design was used at Monze Mission Hospital in Monze district. The findings from 171 patients showed that 72% (12) participants knew the meaning of HIV test and treat policy compared to 28% (48) that seemed not to know. The general distribution of HIV test acceptability among participants shows that the majority of the participants in this study had accepted to be tested for their HIV status. The study shows that 87% of the study participants accepted to be tested for HIV. The study shows that acceptability for HIV test and treat as per UNAIDS 2020 target i.e achieving 90/90/90 has not been achieved. This could be due to less sensitization as 28% of participants never knew the meaning of the policy. Other factors could be lacking awareness, 31% of the participants were not aware of care, treatment, and support services availability for HIV positive people at the hospital. To achieve acceptability of HIV test and treatment, we need to consider educational programs to strengthen or increase sensitization on the meaning and benefits of the program.
Keywords: Acceptability to HIV; test; treat; men and women.Acceptability of HIV Test and Treat among Women and Men Seeking Health Care at Monze Mission Hospital
References:
[1] Nweze, Justus & Emmanuel, Eke & Nweze, Emeka. (2017). HIV/AIDS in sub-Saharan Africa: Current status, challenges, and prospects. Asian Pacific Journal of Tropical Disease. 7. 239-256.
[2] UNAIDS (2018). HIV and AIDS in Zambia: Test and treat showing results in Uganda and Zambia.
[3] Kapata N, Chanda-Kapata P, Grobusch M, O’Grady J, Schwank S, Bates M, et al. Scale-up of TB and HIV programme collaborative activities in Zambia±a 10-year review. Tropical Medicine & International Health. 2012; 17(6):760±6.
[4] National AIDS Counsel (2015). Zambia Country Report: Monitoring the declaration of commitment on HIV and AIDS and the universal access.
[5] Thierman S, Chi BH, Levy JW, Goldenberg RL, Stringer JS, Sinkala M (2006). Individual-level predictors for HIV testing among antenatal attendees in Lusaka, Zambia.
[6] Musheke M, Bond V, Merten S (2013). Couple experiences of provider-initiated couple HIV testing in an antenatal clinic in Lusaka, Zambia: lessons for policy and practice. BMC health services research. 2013; 13 (1):97.
[7] Siame, (2017), HIV testing mandatory: https://Zambia.co.zm/news/headlines/2017/08/16/hiv-testing-mandatory/,
[8] WHO, (2019). Innovative WHO HIV testing recommendations aim to expand treatment coverage. Geneva, Switzerland.
[9] Ware NC, Wyatt MA, Geng EH, Kaaya SF, Agbaji OO, Muyindike WR, et al. (2013). Toward an understanding of disengagement from HIV treatment and care in sub-Saharan Africa: a qualitative study.
[10] UNAIDS (2019). Global AIDS update 2019. Geneva, Switzerland.
[11] Monze Education Fund and Guide to Monze (2020). www.monze.com/placeshospital.html accessed on 13/10/2022 at 11:40.
[12] Ministry of Health (2018): Government pleased with Monze Mission Hospital School of Nursing’s contribution https://www.lusakatimes.com/2018/02/12/governmen - Search (bing.com).
[13] Cambridge Dictionaries online, (2016) https://dictionary.cambridge.org/dictionary/english/knowledge.
[14] Banda, J.M. (2012) Willingness to Accept HIV Testing among Caretakers with a Child Attending the University Teaching Hospital in Lusaka, Zambia. Medical Journal of Zambia, 39. http://www.ajol.info.
[15] CSO (2015) Zambia Demographic Health Survey (ZDHS). Lusaka.
[16] Akanem, E.E. and Gbadegesin, A. (2004) Voluntary Counselling and Testing (VCT) for Human Immunodeficiency Virus: A Study on Acceptability by Nigerian Women Attending Antenatal Clinics. African Journal of Reproductive Health, 8, 91-100. http://bioline.org.br.
[17] Delhi (2008), acceptance of HIV testing among women attending ante natal care in South- Western Uganda: risk factors and reasons for test refusal. AIDS CARE;20(6). www.tandfonline.com/doi/abs/10.1080/09540120701693990.
[18] sharma, T., Kalra, J., Dhasmana, D., & Basera, H. (2014). Poor adherence to treatment: A major challenge in diabetes. Journal, Indian Academy of Clinical Medicine, 15(1), 26–29.
[19] Gatty, Nithin & Unnikrishnan, Bhaskaran & Thapar, Rekha & Mithra, Prasanna & Kulkarni, Vaman & Holla, Ramesh & Bhagawan, Darshan & Kumar, Avinash. (2015). Stigmatization and Discrimination toward People Living with HIV/AIDS in a Coastal City of South India. Journal of the International Association of Providers of AIDS Care. https://www.researchgate.net/publication/272077985_Stigmatization_and_Discrimination_toward_People_Living_with_HIVAIDS_in_a_Coastal_City_of_South_India.
[20] Tabbish S. (2001), Hospital and Health Services Administration Principles and Practice; Oxford University Press. 699.
[21] Bohner, Gerd & Wänke, Michaela. (2002). Attitudes and Attitude Change. 10.4324/9781315784786. Attitudinal Influences on Transfer of Training: A Systematic Literature Review (researchgate.net).
Viewed PDF 910 15 -
 A Reappraisal of Various Animal Models used in Periodontology with Future Perspectives and AlternativesAuthor: Sameena ParveenDOI: 10.21522/TIJPH.2013.10.04.Art021
A Reappraisal of Various Animal Models used in Periodontology with Future Perspectives and AlternativesAuthor: Sameena ParveenDOI: 10.21522/TIJPH.2013.10.04.Art021A Reappraisal of Various Animal Models used in Periodontology with Future Perspectives and Alternatives
Abstract:
Periodontitis is an inflammatory infectious disease that occurs when the supporting tissues of the teeth are infected by a mix of gram-positive bacteria (GPB), and anaerobic bacteria. Periodontitis must be treated as soon as possible to avoid more injury and worsening of the condition. Prior to evaluating new treatments, animal studies are used in conjunction with in vitro studies in periodontitis research. Even though cultured cells can be used to examine physiological processes that occur in periodontitis development, the complex host response that is at the root of the illness is impossible to replicate in vitro. Mice, rats, rabbits, hamsters, nonhuman primates, dogs, and pigs have all been used to imitate human periodontitis, each with its own set of benefits and drawbacks. Animals have played an important part in researching periodontal diseases and developing effective treatments. There is a limitation in the usage of large animals due to their housing problems. Animals for periodontitis are selected based on their resemblance with that human structure and functioning. The usage of these animals will aid in the better and more precise replication of human disease. This will improve the disease’s prognosis and treatment outcome. As a result, the medications utilized can provide a better indication of the effect they will have on the human body based on the effects they have on animal models. Therefore, it is critical to use appropriate animals in periodontal research in order to develop improved treatments for these disorders. Thus, animal models play a crucial role in periodontal research.
Keywords: Animal models; Bacteria; In vitro; Periodontitis; Treatment.A Reappraisal of Various Animal Models used in Periodontology with Future Perspectives and Alternatives
References:
[1] Oz, H.S., Puleo, D.A., 2011, Animal models for periodontal disease. J Biomed Biotechnol., 2011:754857.
[2] Nazir, M., Al-Ansari, A., Al-Khalifa, K., Alhareky, M., Gaffar, B., Almas, K., 2020, Global Prevalence of Periodontal Disease and Lack of Its Surveillance. Scientific World Journal, 2146160.
[3] Relvas, M., López-Jarana, P., Monteiro, L., Pacheco, J.J., Braga, A.C., Salazar, F., 2022, Study of Prevalence, Severity and Risk Factors of Periodontal Disease in a Portuguese Population. J Clin Med., 11(13),3728.
[4] Reynolds, I., Duane, B., 2018, Periodontal disease has an impact on patients’ quality of life. Evidence-based dentistry, 19(1),14-5.
[5] Tonetti, M.S., Bottenberg, P., Conrads, G., Eickholz, P., Heasman, P., Huysmans, M.C., López, R., Madianos, P., Müller, F., Needleman, I., Nyvad B., 2017, Dental caries and periodontal diseases in the ageing population: call to action to protect and enhance oral health and well‐being as an essential component of healthy ageing–Consensus report of group 4 of the joint EFP/ORCA workshop on the boundaries between caries and periodontal diseases. Journal of clinical periodontology, 44, S135-44.
[6] Pasupuleti, M.K., Molahally, S.S., Salwaji S., 2016, Ethical guidelines, animal profile, various animal models used in periodontal research with alternatives and future perspectives. Journal of Indian Society of Periodontology, 20(4),360.
[7] How, K.Y., Song, K.P., Chan K.G., 2016, Porphyromonasgingivalis: an overview of periodontopathic pathogen below the gum line. Frontiers in microbiology, 9(7), 53.
[8] Cekici, A., Kantarci, A., Hasturk, H., Van Dyke, T.E., 2014, Inflammatory and immune pathways in the pathogenesis of periodontal disease. Periodontology 2000, 64(1), 57-80.
[9] Zhou, L.N., Bi, C.S., Gao, L.N., An, Y., Chen, F., Chen, F.M., 2019, Macrophage polarization in human gingival tissue in response to periodontal disease. Oral diseases, 25(1), 265-73.
[10] Ausenda, F., Rasperini, G., Acunzo, R., Gorbunkova, A., Pagni, G.,2019, New perspectives in the use of biomaterials for periodontal regeneration. Materials, 12(13), 2197.
[11] Xu, X.Y., Li, X., Wang, J., He, X.T., Sun, H.H., Chen, F.M.,2019, Concise review: periodontal tissue regeneration using stem cells: strategies and translational considerations. Stem cells translational medicine, 8(4), 392-403.
[12] Struillou, X., Boutigny, H., Soueidan, A., Layrolle, P.,2010, Experimental animal models in periodontology: a review. The open dentistry journal, 4, 37.
[13] Martínez-García, M., Hernández-Lemus, E., 2021, Periodontal inflammation and systemic diseases: an overview. Frontiers in physiology, 1842.
[14] Gonzalez, OA., Nagarajan, R., Novak, M.J, Orraca, L., Gonzalez‐Martinez, JA., Kirakodu, S.S., Ebersole, J.L., 2016, Immune system transcriptome in gingival tissues of young nonhuman primates. Journal of periodontal research, 51(2), 152-63.
[15] Dannan, A., Alkattan, F., 2007, Animal models in periodontal research: A mini review of the literature. The Internet Journal of Veterinary Medicine, 5(1), 5.
[16] Liang, Y., Luan, X., Liu, X., 2020, Recent advances in periodontal regeneration: A biomaterial perspective, Bioactive materials, 5(2), 297-308.
[17] Sulijaya, B., Rahdewati, H., Sunarto, H., Soeroso, Y., 2019, An. Maximizing Periodontal Defect Creation and Experimental Design in Non-Human Primate Model Study. An Updated Review Article Journal of International Dental and Medical Research, 12(2), 733-7.
[18] Kantarci, A., Hasturk, H., Van, Dyke., T.E., 2015, Animal models for periodontal regeneration and peri‐implant responses. Periodontology 2000, 68(1), 66-82.
[19] Shanbhag, S., Pandis, N., Mustafa, K., Nyengaard, J.R., Stavropoulos, A., 2017, Alveolar bone tissue engineering in critical‐size defects of experimental animal models: a systematic review and meta‐analysis. Journal of tissue engineering and regenerative medicine,11(10), 2935-49.
[20] Li, D., Feng, Y., Tang, H., Huang, L., Tong, Z., Hu, C., Chen, X., Tan, J.,2020, A simplified and effective method for generation of experimental murine periodontitis model. Frontiers in Bioengineering and Biotechnology, 25(8),444.
[21] Marchesan, J., Girnary, MS., Jing, L., Miao, M.Z., Zhang, S., Sun, L., Morelli, T., Schoenfisch, M.H., Inohara, N., Offenbacher, S., Jiao, Y.,2018, An experimental murine model to study periodontitis. Nature protocols,13(10), 2247-67.
[22] Bhattarai, G., Poudel, SB., Kook, S.H, Lee, J.C.,2016, Resveratrol prevents alveolar bone loss in an experimental rat model of periodontitis. Acta biomaterialia,1(29),398-408.
[23] Courbon, G., Rinaudo-Gaujous, M., Blasco-Baque, V., Auger, I., Caire, R., Mijola, L., Vico, L., Paul, S., Marotte, H., 2019, Porphyromonasgingivalis experimentally induces periodontitis and an anti-CCP2-associated arthritis in the rat. Annals of the rheumatic diseases, 78(5), 594-9.
[24] Offenbacher, S., Jiao, Y., Kim, SJ., Marchesan, J., Moss, K.L., Jing, L., Divaris, K., Bencharit, S., Agler, C.S., Morelli, T., Zhang, S.,2018, GWAS for Interleukin-1β levels in gingival crevicular fluid identifies IL37 variants in periodontal inflammation. Nature communications, 9(1), 1-7.
[25] Fawzy, El-Sayed., K.M, Doerfer., C.E., 2017, Animal models for periodontal tissue engineering: a knowledge-generating process. Tissue Engineering Part C: Methods, 23(12), 900-25.
[26] Donos, N., Park, J.C., Vajgel, A., de, Carvalho, Farias, B., Dereka, X., 2018, Description of the periodontal pocket in preclinical models: limitations and considerations. Periodontology 2000, 76(1), 16-34.
[27] Jati, A.S., Furquim, L.Z., Consolaro, A., 2016, Gingival recession: its causes and types, and the importance of orthodontic treatment. Dental press journal of orthodontics, 21,18-29.
[28] Preshaw, P.M., 2015, Detection and diagnosis of periodontal conditions amenable to prevention. BMC oral health, 15(1),1-1.
[29] Dahlén, G., Charalampakis, G., Abrahamsson, I., Bengtsson, L., Falsen, E., 2012, Predominant bacterial species in subgingival plaque in dogs. Journal of periodontal research, 47(3), 354-64.
[30] Nicholls, V.M., Townsend, N., 2016, Dental disease in aged horses and its management. Veterinary Clinics: Equine Practice, 32(2), 215-27.
[31] Tyrrell, K.L., Citron, D.M., Jenkins, J.R., Goldstein, E.J., 2002, Periodontal bacteria in rabbit mandibular and maxillary abscesses. J Clin Microbiol., 40(3):1044-7.
[32] Banu, S.R., J., 2018, A Review Role of Animal Models in Periodontal Research. Asian Journal of Pharmaceutical and Clinical Research, 11(7),47-51.
[33] Schou, S., Holmstrup, P., Kornman, KS., 1993, A review of the literature non-human primates used in studies of periodontal disease pathogenesis. J Periodontol, 64,497-508.
[34] Priyanka, M., Jaiganesh, D.R.,2013, Periodontally accelerated osteogenic orthodontics. Int J Pharm PharSci, 5,49-51.
[35] Giannobile, W.V., Finkelman, R.D., Lynch, S.E., 1994, Comparison of canine and non-human primate animal models for periodontal regenerative therapy: results following a single administration of PDGF/IGF-I. J Periodontol, 65(12),1158–68.
[36] Sculean, A., Karring, T., Theilade, J., Lioubavina, N., 1997, The regenerative potential of oxytalanfibers. an experimental study in the monkey. J Clin Periodontol, 24(12),932–6.
[37] Kostopoulos, L., Karring, T., 2004, Susceptibility of GTR-regenerated periodontal attachment to ligature-induced periodontitis. J Clin Periodontol, 31(5), 336–40.
[38] Karatzas, S., Zavras, A., Greenspan, D., Amar, S., 1999, Histologic observations of periodontal wound healing after treatment with perioglas in nonhuman primates. Int J Periodontics Rest Dent, 19(5),489–99.
[39] Donos, N., Sculean, A., Glavind, L., Reich, E., Karring, T., 2003, Wound healing of degree III furcation involvements following guided tissue regeneration and/or Emdogaina histologic study. J Clin Periodontol, 30(12),1061–8.
[40] Trejo, P.M., Bonaventura, G., Weng, D., Caffesse, RG., Bragger, U., Lang, N.P., 2006, Effect of mechanical and antiseptic therapy on peri-implant mucositis: an experimental study in monkey. Clin Oral Implants Res, 17(3),294–304.
[41] Sculean, A., Donos, N., Brecx, M., Reich, E., Karring, T.,2000, Treatment of intrabony defects with guided tissue regeneration and enamel-matrix-proteins an experimental study in monkeys. J Clin Periodontol, 27(7), 466–72.
[42] Pieri, FA., Souza, M.C., Vermelho, L.L., Vermelho, ML., Perciano, P.G., Vargas, F.S., Borges, A.P., da Veiga-Junior, V.F., Moreira, M.A., 2011, Use of β-caryophyllene to combat bacterial dental plaque formation in dogs. BMC Veterinary Research, 12(1),1-8.
[43] Yimam, M., Brownell, L., Do, S.G., Lee, Y.C., Kim, D.S., Seo, K., Jeong, M., Kim, S., Jia, Q., 2019, Protective effect of UP446 on ligature-induced periodontitis in beagle dogs. Dentistry Journal, 7(2),33.
[44] Hamp, S.E., Hamp, M., Olsson, S.E., Lindberg, R., Schauman, P.,1997, Radiography of spontaneous periodontitis in dogs. J Periodontal Res, 32(7), 589–97.
[45] Haney, J.M., Zimmerman, G.J., Wikesjo, U.M., 1995, Periodontal repair in dogs: evaluation of the natural disease model. J Clin Periodontol, 22(3), 208–13.
[46] Miranda, L.A., Gomes, S.C., Soares, I.J., Oppermann, R.V., 2006, A resin-modified glass ionomer cement barrier for treating degree II furcation defects: a pilot study in dogs. Acta Odontol Scand, 64(1),37–41.
[47] Schwarz, F., Herten, M., Sager, M., Bieling, K., Sculean, A., Becker, J., 2007, Comparison of naturally occurring and ligature-induced peri-implantitis bone defects in humans and dogs. Clin Oral Implants Res 18(2),161–70.
[48] Lin, P., Niimi, H., Ohsugi, Y., Tsuchiya, Y., Shimohira, T., Komatsu, K., Liu, A., Shiba, T., Aoki, A., Iwata, T., Katagiri, S., 2021, Application of Ligature-Induced Periodontitis in Mice to Explore the Molecular Mechanism of Periodontal Disease. International Journal of Molecular Sciences, 22(16), 8900.
[49] Jacob, S.P, Nath, S., 2013, Rat gingival model for testing drugs influencing inflammation. IeJSME, 7(2),8-16.
[50] Huang, K.K., Shen, C., Chiang, C.Y., Hsieh, Y.D., Fu, E., 2005, Effects of bone morphogenetic protein-6 on periodontal wound healing in a fenestration defect of rats. J Periodontal Res, 40(1),1–10.
[51] Eslami, B., Behnia, H., Javadi, H., Khiabani, K.S., Saffar, A.S., 2003, Histopathologic comparison of normal and hyperplastic condyles. Oral Surg Oral Med Oral Pathol Oral RadiolEndod, 96(6),711–7.
[52] Graves, D.T., Fine, D., Teng, Y.T., Van, Dyke., T.E., Hajishengallis, G., 2008, The use of rodent models to investigate host–bacteria interactions related to periodontal diseases. Journal of clinical periodontology, 35(2), 89-105.
[53] Lallam-Laroye, C., Escartin, Q., Zlowodzki, A.S., et al., 2006, A. Periodontitis destructions are restored by synthetic glycosaminoglycan mimetic. J Biomed Mater Res, 79(3), 675–83.
[54] Baron, R., Saffar, J.L., 1978, A quantitative study of bone remodeling during experimental periodontal disease in the golden hamster. J Periodontal Res, 13(4), 309–15.
[55] Thumbigere, Math., V, Rebouças., P, Giovani., P.A., Puppin-Rontani, R.M., Casarin, R., Martins, L., Wang, L., Krzewski, K., Introne, W.J., Somerman, M.J., Nociti, Jr., FH., 2018, Periodontitis in Chédiak-Higashi syndrome: An altered immunoinflammatory response. JDR clinical & translational research, 3(1), 35-46.
[56] Hammer, A.S., Andersen, T.H., Eriksen, T., Kortegaard, H.E., Dietz, H.H., Chriél, M., 2005, Radiographic evaluation of destructive periodontal disease in blue mink in relation to age and blood morphology. Canadian journal of veterinary research, 69(2),128.
[57] Johnson-Delaney, C.A., 2016, Exotic Animal Practice. Anatomy and disorders of the oral cavity of ferrets and other exotic companion carnivores. Veterinary Clinics,19(3),901-28.
[58] Harper, D.S, Mann, P.H., Regnier S., 1990, Measurement of dietary and dentifrice effects upon calculus accumulation rates in the domestic ferret. J Dent Res, 69,447-50.
[59] Weinberg, M.A., Bral, M., 1999, Periodontol Laboratory animal models in periodontology. J Clin, 26(6), 335–40.
[60] Tyrrell, K.L., Citron, D.M., Jenkins, J.R, Goldstein, E.J., Periodontal bacteria in rabbit mandibular and maxillary abscesses. J Clin Microbiol, 40, 1044-7.
[61] Oortgiesen, D.A., Meijer, G.J., Bronckers, A.L., Walboomers, X.F., Jansen, J.A., 2010, Fenestration defects in the rabbit jaw: An inadequate model for studying periodontal regeneration. Tissue Eng Part C Methods, 16, 133-40.
[62] Priyanka, M., Ramamurthy, J., 2015, Tissue engineering in periodontal regeneration. Res J Pharm Bio Chem Sci, 69,78-82.
[63] Ranganatha, N., Kuppast, I.J., 2012, A review on alternatives to animal testing methods in drug development. Int J Pharm Pharm Bio Sci, 4,28-32.
[64] Holmes, M., Thomas, R., Hamerow, H., 2021, Periodontal disease in sheep and cattle: Understanding dental health in past animal populations. International Journal of Paleopathology, 1(33),43-54.
[65] Wang, S., Liu, Y., Fang, D., Shi, S., 2007, The miniature pig: A useful large animal model for dental and orofacial research. Oral Dis, 13,530-7.
[66] Polejaeva, I.A., Chen, S.H., Vaught, T.D, Page, R.L, Mullins, J, Ball, S., et al., 2000, Cloned pigs produced by nuclear transfer from adult somatic cells. Nature, 407,86-90.
[67] Fawzy, El-Sayed, K.M., Dörfer, C.E., 2017, Animal Models for Periodontal Tissue Engineering: A Knowledge-Generating Process. Tissue Eng Part C Methods, 23(12), 900-925.
Viewed PDF 970 12 -
 An Epidemiological Survey of Non-municipal Drinking Water Supplies Among Rural Communities in the Blue and John Crow Mountain Ranges, Jamaica, December 2021- June 2022Author: Karlene AtkinsonDOI: 10.21522/TIJPH.2013.10.04.Art022
An Epidemiological Survey of Non-municipal Drinking Water Supplies Among Rural Communities in the Blue and John Crow Mountain Ranges, Jamaica, December 2021- June 2022Author: Karlene AtkinsonDOI: 10.21522/TIJPH.2013.10.04.Art022An Epidemiological Survey of Non-municipal Drinking Water Supplies Among Rural Communities in the Blue and John Crow Mountain Ranges, Jamaica, December 2021- June 2022
Abstract:
The unavailability of safe running water is a major problem faced by many residents of rural Jamaica; the use of unsafe drinking water for domestic purposes is also a major public health challenge in developing countries due its contribution to the global burden of disease reported annually. The aim of the research was to assess the microbiological and physiochemical quality parameters of non-municipal drinking water from springs and tributaries within the Blue and John Crow mountains. The study methodology used was sampling through field work and laboratory testing for microbiological water quality parameters using standard procedures. The research is a cross-sectional survey that was conducted over a seven-month period. Fourteen samples of water were collected from the water sources and in the homes of the residents. Five water parameters were assessed against national and internal water quality index. In one hundred percent of the samples the total coliforms levels exceeded the established safe limit as established by the Ministry of Health Jamaica. The initial hypothesis of the research was supported by the findings. The consumption and use of non-municipal water throughout the communities of the Blue and John Crow Mountain bears a significant risk for public health.
Keywords: Unsafe drinking water, Rural communities, Potable water, Water quality index.An Epidemiological Survey of Non-municipal Drinking Water Supplies Among Rural Communities in the Blue and John Crow Mountain Ranges, Jamaica, December 2021- June 2022
References:
[1] Water System Planning: Estimating Water Needs. (2022, August 26). Water System Planning: Estimating Water Needs. Retrieved November 3, 2022, from https://extension.psu.edu/water-system-planning-estimating-water-needs.
[2] Global WASH Fast Facts | Global Water, Sanitation and Hygiene | Healthy Water | CDC. (2022, May 31). Global WASH Fast Facts | Global Water, Sanitation and Hygiene | Healthy Water | CDC. Retrieved November 3, 2022, from https://www.cdc.gov/healthywater/global/wash_statistics.html.
[3] Project, B. (2016, November 1). Water Quality in Jamaica. The Borgen Project. Retrieved November 3, 2022, from https://borgenproject.org/water-quality-in-jamaica/.
[4] Householders Urged to Purify Stored Water – Jamaica Information Service. (2022, November 2). Householders Urged to Purify Stored Water – Jamaica Information Service. Retrieved November 3, 2022, from https://jis.gov.jm/householders-urged-to-purify-stored-water.
[5] Caribbean epidemiology Center. (n.d.). Epidemics Investigated. https://www.paho.org/spc-crb/dmdocuments/history-of-carec/Epidemics%20investigated.pdf.
[6] Westmoreland chief health inspector urges precaution against leptospirosis. (2020, June 23). Westmoreland Chief Health Inspector Urges Precaution Against Leptospirosis | News | Jamaica Gleaner. Retrieved November 3, 2022, from https://jamaica-gleaner.com/article/news/20200623/westmoreland-chief-health-inspector-urges-precaution-against-leptospirosis.
[7] Super User. (n.d.). Blue and John crow mountains. https://www.blueandjohncrowmountains.org/do/bird-watching.
[8] Drinking-water. (2022, March 21). Drinking-water. Retrieved November 3, 2022, from https://www.who.int/news-room/fact-sheets/detail/drinking-water.
[9] Goal 6 | Department of Economic and Social Affairs. (2023, May 1). Goal 6 | Department of Economic and Social Affairs. Retrieved November 3, 2022, from https://sdgs.un.org/goals/goal.
[10] Dinka, M.O (2017). Safe Drinking Water: Concepts, Benefits, Principles and Standards [Unpublished doctoral dissertation].
[11] Haile Reda, A. (2015). Assessment of physicochemical quality of spring water in Arbaminch, Ethiopia. Journal of Environmental Analytical Chemistry, 02(05). https://doi.org/10.4172/2380-2391.1000157.
[12] National Environment and Planning agency. (2009). water_quality_standard_freshwater.pdf. https://www.nepa.gov.jm/new/legal_matters/policies_standards/docs/standards/water_quality_standard_freshwater.pdf.
[13] Water quality indicators. (2022, July 7). Environment | Department of Environment and Science, Queensland. https://environment.des.qld.gov.au/management/water/health-indicators.
[14] Ameen, H. A. (2019, October 14). Spring water quality assessment using water quality index in villages of Barwari Bala, Duhok, Kurdistan Region, Iraq. Applied Water Science, 9(8). https://doi.org/10.1007/s13201-019-1080-z.
[15] Coliform Bacteria and Drinking Water. (2016). https://doh.wa.gov/sites/default/files/legacy/Documents/Pubs//331-181.pdf.
[16] Guidelines for drinking-water quality, 4th edition, incorporating the 1st addendum. (2017, April 24). Guidelines for Drinking-water Quality, 4th Edition, Incorporating the 1st Addendum. Retrieved November 3, 2022, from https://www.who.int/publications/i/item/9789241549950.
[17] Abdallah. (2010). Assessment Of Drinking Water Quality According to WQI Based on Turbidity in Rabak Town White Nile State Sudan 2010.
[18] Fewtrell, L., et al. (2005) Water, sanitation, and hygiene interventions to reduce diarrhea in less developed countries: A systematic review and meta-analysis. The Lancet Infectious Diseases, 5, 42. doi:10.1016/S1473-3099(04)01253.
[19] Clasen, Thomas Frank; (2006) Household-based water treatment for the prevention of diarrheal disease. PhD thesis, London School of Hygiene & Tropical Medicine. DOI: https://doi.org/10.17037/PUBS.00682347.
[20] Geremew, A., et al. (2018) Point-of-use water chlorination among urban and rural households with under-five-year children: A comparative study in Kersa health and demographic surveillance site, Eastern Ethiopia. Journal of Water, Sanitation and Hygiene for Development, 8(3), 468-480. https://doi.org/10.2166/washdev.2018.173.
[21] Gallagher, C. D., & Dietrich, A. M. (2010). TDS and temperature affect consumer taste preferences. Opflow, 36(12), 20-22. https://doi.org/10.1002/j.1551-8701.2010.tb03058.x.
[22] Campbell, B. (2022, July 22). What are Tannins in water? Water Quality Products. https://www.wqpmag.com/home/article/21014398/what-are-tannins-in-water.
[23] Assurity Consulting. (2019, June 1). Explore drinking water quality: Pseudomonas aeruginosa. Assurity Consulting Ltd. https://www.assurityconsulting.co.uk/knowledge/guides/what-is-important-to-know-about-drinking-water-quality-pseudomonas-aeruginosa.
[24] Gautam, R. K., et al. (2014). Chapter 1. Contamination of heavy metals in aquatic media: Transport, toxicity, and technologies for remediation. Heavy Metals in Water, 1-24. https://doi.org/10.1039/9781782620174-00001.
[25] A guide to drinking water treatment and sanitation for Backcountry and travel use. (2022, October 19). Centers for Disease Control and Prevention. https://www.cdc.gov/healthywater/drinking/travel/backcountry_water_treatment.html.
[26] Potable water. (n.d.). Water Education Foundation. https://www.watereducation.org/aquapedia-background/potable-water.
[27] Water. (2017, 7). WHO | Regional Office for Africa. https://www.afro.who.int/health-topics/water.
[28] Fasihi, S., et.al. (2021). Effect of alkaline drinking water on bone density of postmenopausal women with osteoporosis. Journal of Menopausal Medicine, 27(2), 94. https://doi.org/10.6118/jmm.20036.
[29] Magro, M., et.al. (2016). Alkaline water and longevity: A murine study. Evidence-Based
[30] Saanvi. (2021, October 12). Alkaline water: Possible side effects of drinking high PH water. Styles At Life.
[31] Kumpel, E. (2017). Environmental solid matrices - Determination of total dissolved solids (TDS) in water and eluates. Seasonal Variation in Drinking and Domestic Water Sources and Quality in Port Harcourt, Nigeria. https://doi.org/10.3403/30133766u.
[32] World Health Organization. (1997). Guidelines for drinking-water quality.
[33] Jabbar‐Lopez, Z. (2020). The effect of water hardness on atopic eczema, skin barrier function: A systematic review, meta‐analysis. Clinical & Experimental Allergy, 51(3), 430-451. https://doi.org/10.1111/cea.13797.
[34] Gobalarajah, K., Subramaniam, P., Jayawardena, U. A., Rasiah, G., Rajendra, S., & Prabagar, J. (2020). Impact of water quality on chronic kidney disease of unknown etiology (CKDu) in Thunukkai division in Mullaitivu district, Sri Lanka. BMC Nephrology, 21(1). https://doi.org/10.1186/s12882-020-02157-1.
[35] Bothe, G., et. al. (2015). Efficacy and safety of a natural mineral water rich in magnesium and sulphate for bowel function: A double-blind, randomized, placebo-controlled study. European Journal of Nutrition, 56(2), 491-499. https://doi.org/10.1007/s00394-015-1094-8.
[36] Vizioli, B., Hantao, L. W., & Montagner, C. C. (2022). Disinfection byproducts in emerging countries.
[37] Moore, G., & Walker, J. (2014). Presence and control of legionella pneumophila and pseudomonas aeruginosa Biofilms in hospital water systems. Biofilms in Infection Prevention and Control, 311-337. https://doi.org/10.1016/b978-0-12-397043-5.00017-7.
[38] Gebresilasie, K. G., et.al. (2021). Assessment of some physicochemical parameters and heavy metals in hand-dug well water samples of Kafta Humera Woreda, Tigray, Ethiopia. International Journal of Analytical Chemistry, 2021, 1-9. https://doi.org/10.1155/2021/8867507.
Viewed PDF 979 31 -
 Socioeconomic Impacts of Risks Associated with Pre-eclampsia during Pregnancy in Imo StateAuthor: Godwin Chukwuemeka Amarikwa-ObiDOI: 10.21522/TIJPH.2013.10.04.Art023
Socioeconomic Impacts of Risks Associated with Pre-eclampsia during Pregnancy in Imo StateAuthor: Godwin Chukwuemeka Amarikwa-ObiDOI: 10.21522/TIJPH.2013.10.04.Art023Socioeconomic Impacts of Risks Associated with Pre-eclampsia during Pregnancy in Imo State
Abstract:
Preeclampsia risk is a global pandemic that poses a serious threat to global health. It is recognized as a chronic and debilitating disease that is associated with significant complications. As a result, it significantly reduces life expectancy, can cause multi-system morbidities, increases healthcare costs, and ultimately results in the premature death of both the mother and the fetus. All forms of preeclampsia carry unacceptable human, societal, and financial costs for Imo State, regardless of income. Therefore, in Imo State, Southeast Nigeria, this study looked into the socioeconomic effects of the risks associated with pre-eclampsia during pregnancy. This study employed both descriptive and analytical study designs. Data gathering techniques included target, stratified sampling, and random sampling. A total of 3690 people from around the state made up the sample size. Questionnaires were used as the research tool for data collection. Tables and charts with the generated data were created. Statistically descriptive:. The significant difference between the perception of risk variables by individuals and patients was measured using chi-square. Regarding the socioeconomic effects of preeclampsia risks, respondents were generally in agreement that these risks can result in job loss, with 56.19%, or 1190 out of 2700 responses, saying “Yes,” 12.84%, or 272 out of 2700 responses, saying “No,” and 656 out of 2700 respondents, or 30.97% of the responses, saying “No idea.” However, there was a very high significant variation among their responses. Additionally, they agreed that preeclampsia risks can result in subpar performance at work. Preeclampsia risks had a negative socioeconomic influence on the patients’.
Keywords: Impacts, Imo State , Pre-eclampsia ,Risks, Socioeconomic.Socioeconomic Impacts of Risks Associated with Pre-eclampsia during Pregnancy in Imo State
References:
[1] Vidaeff A, Pettker CM, Simhan H. (2019) Gestational Hypertension and Preeclampsia ACOG PRACTICE BULLETIN. Clinical Management Guidelines for Obstetrician-Gynecologists. Am Coll. Obstet Gynecol. 133(1):1–25 7.3. Williams PJ and Broughton Pipkin F (2011) The genetics of pre-eclampsia and other hypertensive disorders of pregnancy. Best Pract Res Clin Obstet Gynaecol. 25: 405-417.
[2] Trogstad L, Magnus P, Stoltenberg C (2011).. Pre-eclampsia: Risk factors and causal models. Best Pract Res Clin Obstet Gynaecol 25(3):329-42.
[3] Williams PJ and Broughton Pipkin F (2011) The genetics of pre-eclampsia and other hypertensive disorders of pregnancy. Best Pract Res Clin Obstet Gynaecol. 25: 405-417
[4] Belay A.S., Wudad T. (2019). Prevalence and associated factors of pre-eclampsia among pregnant women attending antenatal care at Mettu Karl referral hospital, Ethiopia: cross-sectional study. Journal of Clinical Practice, 25(1):14.
[5] World Health Organisation’ (2011). WHO recommendations for prevention and treatment of preeclampsia and eclampsia. Available at: https://www.who.int/reproductivehealth/publications/maternal_perinatal_health/9789241548335/en/ (Accessed: 8 January 2021).
[6] Bellamy, L, Casas, J, Hingorani, AD, Williams, DJ. Pre-eclampsia and risk of cardiovascular disease and cancer in later life: systematic review and meta-analysis. British Medical Journal. 2007; 335:974–985.
[7] Birhanu MY, Temesgen H, Demeke G, Assemie MA, Alamneh AA, Desta M, Toru M, Ketema DB, Bischof P, Martelli M, Campana A, Itoh Y, Ogata Y, Nagase H. (1995) Importance of matrix metalloproteinases in human trophoblast invasion. Early Pregnancy 263-269.
[8] Stevens W, Shih T, Incerti D, Ton TGN, Lee HC, Peneva D, (2017) Short-term costs of preeclampsia to the United States health care system. Am J Obstet Gynecol. ;217(3):237–248.e16.
[9] Nnodim, J., Emmanuel, N., Hope, O., Nwadike, C., Ukamaka, E., Christian, O. (2017). Membrane potential, serum calcium and serum selenium decrease in pre-eclampsia subjects in Owerri. Universa Medicina, 36(2), 88–93.
[10] Siddiqui A, Deneux-Tharaux C, Luton D, Schmitz T, Mandelbrot L, Estellat C (2020) Maternal obesity and severe pre-eclampsia among immigrant women: a mediation analysis. Sci Rep.;10(1):1–9.
[11] Ajah L.O., Ozonu N.C., Ezeonu P.O., Lawani L.O., Obuna J.A., Onwe E.O. (2016). The Feto-Maternal Outcome of Preeclampsia with Severe Features and Eclampsia in Abakaliki, South-East Nigeria. Journal of Clinical Diagnostics and Research, 10(9): QC18–QC21.
[12] Amaral LM, Wallace K, Owens M, LaMarca B (2017). Pathophysiology and Current Clinical Management of Preeclampsia. Curr Hypertens Rep. 19(8):616.
[13] Gray KJ, Kovacheva VP, Mirzakhani H, Bjonnes AC, Almoguera B, Wilson ML, Ingles SA, Lockwood Hakonarson H, McElrath TF, Murray JC, Norwitz ER, Karumanchi SA, Bateman BT (2018), Gene-Centric Analysis of Preeclampsia Identifies Maternal Association at PLEKHG1 Hypertension, ;72(2):408-416.
[14] Morton CH, Seacrist MJ, VanOtterloo LR, Main EK. (2019) Quality improvement opportunities identified through case review of pregnancy-related deaths from preeclampsia/eclampsia. J Obstet Gynecol Neonatal Nurs. 48(3):275–87.
[15] Berhan Y., Endeshaw G. (2015). Clinical and Biomarkers Difference in Prepartum and Postpartum Eclampsia. Ethiopian Public Health Journal, 25(3):257–66.
[16] Das S, Das R, Bajracharya R, Baral G, Jabegu B, Odland JØ, (2019) Incidence and risk factors of pre-eclampsia in the paropakar maternity and women’s hospital, Nepal: A retrospective study. Int J Environ Res Public Health. 16(19):1–8.
[17] Ebrahimi A, Sayad B, Rahimi Z. (2020) COVID-19 and psoriasis: biologic treatment and challenges. J Dermatolog Treat. J Dermatolog Treat; 1–5.
[18] Aziza.com.ng (2022). Imo State History, Local Government Area, and Senatrial Zones/Districts. Available at: https://www.aziza.com.ng/read/2019/10/imo-state-and-local-government-area/ (Accessed: 9 January 2022).
[19] Lucas, A. O. and Gilles, H. M. (2003): Short textbook of public health medicine for the tropics. Revised 4th edition. Hodder Arnold, London, UK pp 30-51.
[20] Farmer, A.; Wade, A. and Goyder, E. (2007): Impact of self-monitoring of blood glucose in the management of patients with non-insulin treated diabetes: open parallel group randomised trial. BMJ.;335:132.
[21] Payne, R. W., Murray, D. A., Hardings, S. A. Baird, D. B. and Soutar, D. M. (2007). GenStat for windows (12th Edition). VSN International Ltd, Hemel Hempstead.
[22] Wandabwa J., Doyle P., Kiondo P., Campbell O., Maconichie N., Welishe G. (2010). Risk factors for severe pre-eclampsia and eclampsia in Mulago Hospital, Kampala, Uganda. East African Medical Journal, 87(10):415–24.
Viewed PDF 983 27 -
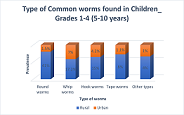 Prevalence of Worm Infestation and Associated Risk Factors among Rural and Urban Lower Primary School Going Children in Kasama District, Northern Province, ZambiaAuthor: Ernest Chama MutaleDOI: 10.21522/TIJPH.2013.10.04.Art024
Prevalence of Worm Infestation and Associated Risk Factors among Rural and Urban Lower Primary School Going Children in Kasama District, Northern Province, ZambiaAuthor: Ernest Chama MutaleDOI: 10.21522/TIJPH.2013.10.04.Art024Prevalence of Worm Infestation and Associated Risk Factors among Rural and Urban Lower Primary School Going Children in Kasama District, Northern Province, Zambia
Abstract:
Regardless of the many health promotion communications and public health interventions that the Government of the Republic of Zambia continues to provide to its citizens via the Ministry of Health that are directed at the prevention and reduction of worm infestation in Kasama District, Northern Province of Zambia, a lot of lower primary school going children still continue to miss school attendance in order to access health services due to worm infestation cases which have continued to be on the increase in both rural and urban areas. The high levels of poverty and other related risk factors in such resource-limited areas have put many of these children at increased risk of worm infestation. Thus, this study investigated the relationship between those risk factors and the prevalence of worm infestation in both rural and urban areas with respect to area of residency of the children. The study used retrospective quantitative methods in eliciting information from data sources from six health facilities in Northern Province covering a 2year period (2018-2020). Consequently, 120 children were identified and included in the study. Thereafter, data were analyzed using a statistical package for the social sciences (SPSS v19). Findings indicate; low socio-economic status and areas of residency were the main contributing risk factors in rural than urban areas. Therefore, recommendations on the country’s policies towards mass deworming programs and basic hygiene in lower primary school going children were availed to government after completing the study.
Keywords: Residency, Primary School Children, Prevalence, Worm Infestations, Zambia.Prevalence of Worm Infestation and Associated Risk Factors among Rural and Urban Lower Primary School Going Children in Kasama District, Northern Province, Zambia
References:
[1] Mwale, K., & Siziya, S. (2015). Intestinal Infestations in Under-Five Children in Zambia. International Journal of MCH and AIDS, 4(2), 40–46. https://pubmed.ncbi.nlm.nih.gov/27622006.
[2] King, C. H. (2010). Parasites and poverty: The case of schistosomiasis. Acta Tropica, 113(2), 95–104. https://doi.org/https://doi.org/10.1016/j.actatropica.2009.11.012.
[3] Kumar, H., Jain, K., & Jain, R. (2014). A study of prevalence of intestinal worm infestation and efficacy of anthelminthic drugs. Medical Journal, Armed Forces India, 70(2), 144–148. https://doi.org/10.1016/j.mjafi.2013.12.009.
[4] Bundy, D. A. P., Walson, J. L., & Watkins, K. L. (2013). Worms, wisdom, and wealth: why deworming can make economic sense. Trends in Parasitology, 29(3), 142–148. https://doi.org/https://doi.org/10.1016/j.pt.2012.12.003.
[5] Ugbomoiko, U. S., Dalumo, V., Ofoezie, I. E., & Obiezue, R. N. N. (2009). Socio-environmental factors and ascariasis infection among school-aged children in Ilobu, Osun State, Nigeria. Transactions of The Royal Society of Tropical Medicine and Hygiene, 103(3), 223–228. https://doi.org/10.1016/j.trstmh.2008.12.014.
[6] Gunawardena, G. S. A., Karunaweera, N. D., & Ismail, M. M. (2004). Socio–economic and behavioural factors affecting the prevalence of Ascaris infection in a low-country tea plantation in Sri Lanka. Annals of Tropical Medicine & Parasitology, 98(6), 615–621. https://doi.org/10.1179/000349804225021299.
[7] Ganguly, S., Barkataki, S., Karmakar, S., Sanga, P., Boopathi, K., Kanagasabai, K., Kamaraj, P., Chowdhury, P., Sarkar, R., Raj, D., James, L., Dutta, S., Sehgal, R., Jha, P., & Murhekar, M. (2017). High prevalence of soil-transmitted helminth infections among primary school children, Uttar Pradesh, India, 2015. Infectious Diseases of Poverty, 6(1), 139. https://doi.org/10.1186/s40249-017-0354-7.
[8] Feachem, R. G., Guy, M. W., Harrison, S., Iwugo, K. O., Marshall, T., Mbere, N., Muller, R., & Wright, A. M. (1983). Excreta disposal facilities and intestinal parasitism in urban Africa: Preliminary studies in Botswana, Ghana, and Zambia. Transactions of The Royal Society of Tropical Medicine and Hygiene, 77(4), 515–521. https://doi.org/10.1016/0035-9203(83)90128-1.
[9] Walana, W., Aidoo, E. N. K., & Tay, S. C. K. (2014). Prevalence of hookworm infection: a retrospective study in Kumasi. Asian Pacific Journal of Tropical Biomedicine, 4, S158–S161. https://doi.org/https://doi.org/10.12980/APJTB.4.2014APJTB-2013-0014.
[10] Kunwar, R., Acharya, L., & Karki, S. (2016). Decreasing prevalence of intestinal parasitic infections among school-aged children in Nepal: a systematic review and meta-analysis. Transactions of The Royal Society of Tropical Medicine and Hygiene, 110(6), 324–332. https://doi.org/10.1093/trstmh/trw033.
[11] Abossie, A., & Seid, M. (2014). Assessment of the prevalence of intestinal parasitosis and associated risk factors among primary school children in Chencha town, Southern Ethiopia. BMC Public Health, 14(1), 166. https://doi.org/10.1186/1471-2458-14-166.
[12] Ashtiani, M. T. H., Monajemzadeh, M., Saghi, B., Shams, S., Mortazavi, S. H., Khaki, S., Mohseni, N., Kashi, L., & Nikmanesh, B. (2011). Prevalence of intestinal parasites among children referred to Children’s Medical Center for 18 years (1991–2008), Tehran, Iran. Annals of Tropical Medicine & Parasitology, 105(7), 507–513. https://doi.org/10.1179/1364859411Y.0000000040.
[13] Kahisay, M., Birhanie, M., & Derso, A. (2021). Prevalence and Intensity of Schistosoma mansoni Infection and Its Associated Risk Factors Among Patients with and without HIV at Chuahit Health Center, Dembia District, Northwest Ethiopia. Research and Reports in Tropical Medicine, 12, 25–32. https://doi.org/10.2147/RRTM.S292899.
[14] Prevalence & risk factors for soil transmitted helminth infection among school children in south India. The Indian Journal of Medical Research, 139(1), 76–82. https://pubmed.ncbi.nlm.nih.gov/24604041.
[15] Mulatu, G., Zeynudin, A., Zemene, E., Debalke, S., & Beyene, G. (2015). Intestinal parasitic infections among children under five years of age presenting with diarrhoeal diseases to two public health facilities in Hawassa, South Ethiopia. Infectious Diseases of Poverty, 4(1), 49. https://doi.org/10.1186/s40249-015-0081-x.
[16] Nishiura, H., Imai, H., Nakao, H., Tsukino, H., Changazi, M. A., Hussain, G. A., Kuroda, Y., & Katoh, T. (2002). Ascaris lumbricoides among children in rural communities in the Northern Area, Pakistan: prevalence, intensity, and associated socio-cultural and behavioral risk factors. Acta Tropica, 83(3), 223–231. https://doi.org/https://doi.org/10.1016/S0001-706X(02)00116-X.
[17] Sitotaw, B., Mekuriaw, H., & Damtie, D. (2019). Prevalence of intestinal parasitic infections and associated risk factors among Jawi primary school children, Jawi town, north-west Ethiopia. BMC Infectious Diseases, 19(1), 341. https://doi.org/10.1186/s12879-019-3971-x.
[18] Talukdar, K., & Baruah, R. (2015). Health status of primary school children: a community based cross sectional study in rural areas of Kamrup district, Assam. Journal of Evolution of Medical and Dental Sciences, 4, 2093+. https://link.gale.com/apps/doc/A471274605/HRCA?u=anon~8c8b55ae&sid=googleScholar&xid=e994453c.
[19] Walson, J. L., Stewart, B. T., Sangaré, L., Mbogo, L. W., Otieno, P. A., Piper, B. K. S., Richardson, B. A., & John-Stewart, G. (2010). Prevalence and Correlates of Helminth Co-infection in Kenyan HIV-1 Infected Adults. PLOS Neglected Tropical Diseases, 4(3), e644.
[20] Davis, S. M., Worrell, C. M., Wiegand, R. E., Odero, K. O., Suchdev, P. S., Ruth, L. J., Lopez, G., Cosmas, L., Neatherlin, J., Njenga, S. M., Montgomery, J. M., & Fox, L. M. (2014). Soil-transmitted helminths in pre-school-aged and school-aged children in an urban slum: a cross-sectional study of prevalence, distribution, and associated exposures. The American Journal of Tropical Medicine and Hygiene, 91(5), 1002–1010. https://doi.org/10.4269/ajtmh.14-0060.
Viewed PDF 1119 32 -
 Use of Aerobic Exercise as an Adjunct to Conventional Therapy in the Management of an Older Adult with Chronic Low Back Pain in Nigeria: A Case ReportAuthor: Kolo M. AliyuDOI: 10.21522/TIJPH.2013.10.04.Art025
Use of Aerobic Exercise as an Adjunct to Conventional Therapy in the Management of an Older Adult with Chronic Low Back Pain in Nigeria: A Case ReportAuthor: Kolo M. AliyuDOI: 10.21522/TIJPH.2013.10.04.Art025Use of Aerobic Exercise as an Adjunct to Conventional Therapy in the Management of an Older Adult with Chronic Low Back Pain in Nigeria: A Case Report
Abstract:
Treatment preferences utilized by most physical therapists on adults with LBP in Nigeria often do not adhere to global clinical practice guidelines, which include aerobic exercise. This case report describes the utilization of aerobic exercise within a conventional multimodal treatment approach in the management of chronic LBP for an older adult living in Nigeria. Baseline measures of NPRS, ODI, RPE, and lumbar range of movement were taken at the initial visit. Subsequently, the intervention combined a walking aerobic exercise both overground and, on the treadmill, with other therapies (e.g., directional preference exercises, strengthening exercises) for 16 sessions over four weeks. Following 16 sessions, clinically meaningful improvements in pain, disability, lumbar range of motion, and rate of perceived exertion were observed. The patient complied, reported no side effects, and had positive feedback regarding the intervention. The utilization of aerobic exercises within a conventional multimodal treatment approach is safe and could be useful for the management of chronic LBP in older adults.
Keywords: Aerobic exercise, Conventional management, Clinical practice guidelines, Low back pain, Physical therapy, Walking exercise.Use of Aerobic Exercise as an Adjunct to Conventional Therapy in the Management of an Older Adult with Chronic Low Back Pain in Nigeria: A Case Report
References:
[1] World Health Organization Scientific Group, 2003, The burden of musculoskeletal conditions at the start of the new millennium. Geneva, Switzerland: World Health Organization, https://apps.who.int/iris/handle/10665/42721.
[2] Ries J. D., 2018, Rehabilitation for individuals with dementia: Facilitating success. Curr Geriatr Rep, 7(11):59–70. doi:10.1007/s13670-018-0237-1.
[3] Awosan K. J., Yikawe S.S., Oche O.M., Oboirien M., 2017, Prevalence, perception, and correlates of low back pain among healthcare workers in tertiary health institutions in Sokoto, Nigeria. Ghana Med J, 51(4):164-174 doi:10.4314/GMJ.V51I4.4.
[4] Ogden C.L., Carroll M.D., Curtin L.R., McDowell M.A., Tabak C.J., Flegal K.M., 2006, Prevalence of overweight and obesity in the United States, 1999–2004. JAMA, 295(13):1549–1555. doi:10.1001/jama.295.13.1549.
[5] Patel H., Alkhawam H., Madanieh R., Shah N., Kosmas C.E., Vittorio T.J., 2017, Aerobic vs anaerobic exercise training effects on the cardiovascular system. World J Cardiol, 9(2):134. doi:10.4330/wjc.v9.i2.134.
[6] Ayanniyi O., Lasisi O.T., Adegoke B., Oni-Orisan M.O., 2007, Management of low back pain: Attitudes and treatment preferences of physiotherapists in Nigeria. Afri J Biomed Res, 10:41-49. doi:10.4314/ajbr.v10i1.48970.
[7] Dagenais S., Caro J., Haldeman S., 2008, A systematic review of low back pain cost of illness studies in the United States and internationally. Spine J, 8:8–20. doi:10.1016/j.spinee.2007.10.005.
[8] Battie M.C., Cherkin D.C., Dunn R., Ciol M.A., Wheeler K.J., 1994, Managing low back pain. attitudes and treatment preferences of physical therapists. Phys Ther, 74(3):219- 226. doi:10.1093/ptj/74.3.219.
[9] Oppong-Yeboah B., May S., 2014, Management of low back pain in Ghana: A survey of self-reported practice. Physiother Res Intl, 19(4):222-230. doi:10.1002/pri.1586.
[10] Foster N.E., Thompson K.A., Baxter G.D., Allen J., 1999, Management of non-specific low back pain by physiotherapists in Britain and Ireland. A descriptive questionnaire of current clinical practice Spine, 24(13):1332-42. doi:10.1097/00007632-199907010-00011.
[11] George S.Z., Fritz J.M., Silfies S.P., et al., 2021, Interventions for the management of acute and chronic low back pain: Revision 2021. J Orthop Sports Phys Ther, 51(11): CPG1-CPG60. doi:10.2519/jospt.2021.0304.
[12] Finley C.R., Chan D.S., Garrison S., et al., 2018, What are the most common conditions in primary care? Systematic review. Can Fam Physician, 64:832-840. Published 2018. Accessed July 16, 2022
[13] Haldeman S., Nordin M., Chou R., et al., 2018, The global spine care initiative: World spine care executive summary on reducing spine‑related disability in low‑ and middle‑income communities. Eur Spine J, 27(Suppl 6);27:776–785. doi:10.1007/s00586-018-5722-x.
[14] Safiri S., Kolahi A.A., Cross M., et al., 2021, Prevalence, deaths, and disability-adjusted life years due to musculoskeletal disorders for 195 countries and territories 1990–2017. Arthritis Rheumatol, 73:702-714. doi:org/10.1002/art.41571.
[15] Cook C., Learman K., Showalter C., O’Halloran B., 2015, The relationship between chief complaint
and comparable sign in patients with spinal pain: An exploratory study. Man Ther, 20(3):451-5. doi:10.1016/j.math.2014.11.007.[16] Egwu M.O., Ojeyinka A.A., Olaogun M.O., 2007, The effect of vertical oscillatory pressure (vop) on youths and elderly adult low back pain (lbp) intensity and lumbo-sacral mobility. J Jpn Phys Ther Assoc, 10(1):17-26. doi:10.1298/jjpta.10.17.
[17] Pesonen J., Shacklock M., Rantanen P., et al., 2021, Extending the straight leg raise test for improved clinical evaluation of sciatica: Reliability of hip internal rotation or ankle dorsiflexion. BMC Musculoskeletal Disord, 22(1):1-8. doi:10.21203/rs.3.rs-200428/v1.
[18] Fairbank J.C., Pynsent P.B., 2000, The Oswestry disability index. Spine. 25(22):2940-2952. doi:10.1097/00007632-200011150-00017.
[19] U.S. Department of Health and Human Services, 2018, Physical activity guidelines for Americans. 2nd edition. Washington, DC: U.S. Department of Health and Human Services.
[20] Morris J.N., Hardman A.E., 1997, Walking to health. Sports Med. 23(5):306-332. doi:10.2165/00007256-199723050-00004.
[21] Liu M.Q., Anderson F.C., Schwartz M.H., Delp S.L., 2008, Muscle contributions to support and progression over a range of walking speeds. J Biomech, 41(15):3243-52. doi:10.1016/j.jbiomech.2008.07.031.
[22] Uzawa H., Davis S., 2018, Outcome measures for adherence to home exercises among patients with chronic low back pain: A systematic review. J Phys Ther Sci, 30(4):649-653. doi:10.1589/jpts.30.649.
[23] Morris J.N., Hardman A.E., 1997, Walking to health. Sports Med, 23(5):306-332. doi:10.2165/00007256-199723050-00004.
Viewed PDF 972 23 -
 Prevalence of Human Immunodeficiency Virus among Presumptive Tuberculosis Patients Offered HIV Testing Services in Federal Capital Territory, Abuja NigeriaAuthor: Tangkat Friday HosleDOI: 10.21522/TIJPH.2013.10.04.Art026
Prevalence of Human Immunodeficiency Virus among Presumptive Tuberculosis Patients Offered HIV Testing Services in Federal Capital Territory, Abuja NigeriaAuthor: Tangkat Friday HosleDOI: 10.21522/TIJPH.2013.10.04.Art026Prevalence of Human Immunodeficiency Virus among Presumptive Tuberculosis Patients Offered HIV Testing Services in Federal Capital Territory, Abuja Nigeria
Abstract:
Human Immunodeficiency Virus has a prevalence of 1.4% in Nigeria, 2.0% in North Central Nigeria and, 1.4% among adults in Abuja. This study determined prevalence and predictors of Human Immunodeficiency Virus among 737 presumptive tuberculosis patients in Federal Capital Territory Abuja Nigeria from 1st April 2019 to 30th May 2021 through retrospective cross-sectional study and multi-stage sampling. From Non-Municipal Area Councils, Bwari was selected while from Health Facilities, General Hospital Bwari and Gwarimpa were selected from Bwari and Abuja Municipal Area Council respectively by simple random sampling and data abstractions were done and analyzed using Statistical Package for Social Sciences version 23.0 Software. The prevalence of Human Immunodeficiency Virus amongst patients with known status was 29.0%, unknown status 1.9% while their cumulative prevalence was 30.7%. The prevalence of Human Immweredeficiency Virus amongst patients with tuberculosis was 1.1%. Factors associated with Human Immunodeficiency Virus were Area Council (p = 0.001), age (p = 0.001) and gender (p = 0.001). For predictors, residency in Bwari was 0.196 times less likely compared to residency at AMAC, Abuja and, place of Residence was a predictor (aOR = 0.001; 95% C.I. = 0.130-295). The age group 31-40 years were 2 times more likely compared to other age groups and, age it was predictor (aOR = 0.019; 95% C.I. = 1.125-3.852). and male gender gender were 0.601 time less likely compared to females and, gender is a predictor (aOR = 0.021; 95% C.I. = 0.391-0.925).
Keywords: Human Immunodeficiency Virus, Presumptive, Tuberculosis.Prevalence of Human Immunodeficiency Virus among Presumptive Tuberculosis Patients Offered HIV Testing Services in Federal Capital Territory, Abuja Nigeria
References:
[1] Nigerian AIDS Control Agency. (2020). About HIV/AIDS - NACA Nigeria. Retrieved April 11, 2021, from https://naca.gov.ng/about-hivaids/.
[2] World Health Organization. (n.d.). HIV/AIDS. Retrieved April 11, 2021, from https://naca.gov.ng/about-hiv-aids/.
[3] World Health Organization. (2018). HIV/AIDS | WHO | Regional Office for Africa. Retrieved April 11, 2021, from https://www.afro.who.int/health-topics/hivaids.
[4] World Health Organization. (n.d.). HIV/AIDS. Retrieved April 11, 2021, from https://www.who.int/health-topics/hiv-aids#tab=tab_1.
[5] UNAIDS. (2020). Global HIV & AIDS statistics — 2020 fact sheet | UNAIDS. Retrieved April 12, 2021, from https://www.unaids.org/en/resources/fact-sheet.
[6] International Labour Organization. (n.d.). HIV/AIDS in Africa (Africa). Retrieved April 11, 2021, from https://www.ilo.org/africa/areas-of-work/hiv-aids/lang--en/index.htm.
[7] Birdthistle, I., Schaffnit, S. B., Kwaro, D., Shahmanesh, M., Ziraba, A., Kabiru, C. W., Phillips-Howard, P., Chimbindi, N., Ondeng’E, K., Gourlay, A., Cowan, F. M., Hargreaves, J. R., Hensen, B., Chiyaka, T., Glynn, J. R., & Floyd, S. (2018). Evaluating the impact of the DREAMS partnership to reduce HIV incidence among adolescent girls and young women in four settings: A study protocol. BMC Public Health, 18(1). https://doi.org/10.1186/s12889-018-5789-7.
[8] Centers for Disease Control and Prevention. (2020). Global Health - Newsroom - Tuberculosis. Retrieved April 10, 2021, from https://www.cdc.gov/globalhealth/newsroom/topics/tb/index.html.
[9] UNAIDS. (2019). New survey results indicate that Nigeria has an HIV prevalence of 1.4% | UNAIDS. Retrieved April 11, 2021, from https://www.unaids.org/en/resources/presscentre/pressreleaseandstatementarchive/2019/march/20190314_nigeria.
[10] NAIIS. (2019). Key findings. Retrieved April 12, 2021, from https://naiis.ng/resource/factsheet/NAIIS National Summary Sheet.pdf.
[11] NACA. (2019). Nigeria prevalence rate - NACA Nigeria. Retrieved April 12, 2021, from https://naca.gov.ng/nigeria-prevalence-rate/.
[12] Slogrove, A. L., Schomaker, M., Davies, M. A., Williams, P., Balkan, S., Ben-Farhat, J., Calles, N., Chokephaibulkit, K., Duff, C., Eboua, T. F., Kekitiinwa-Rukyalekere, A., Maxwell, N., Pinto, J., Seage, G., Teasdale, C. A., Wanless, S., Warszawski, J., Wools-Kaloustian, K., Yotebieng, M.,Leroy, V. (2018). The epidemiology of adolescents living with perinatally acquired HIV: A cross-region global cohort analysis. Plos Medicine, 15(3). https://doi.org/10.1371/journal.pmed.1002514.
[13] World Health Organization. (2020). Tuberculosis. Retrieved March 30, 2021, from https://www.who.int/news-room/fact-sheets/detail/tuberculosis.
[14] World Health Organization. (n.d.). Tuberculosis (TB) | WHO | Regional Office for Africa Organization. Retrieved April 11, 2021, from https://www.afro.who.int/health-topics/tuberculosis-tb.
[15] World Health Organization. (n.d.). Tuberculosis (TB) | WHO | Regional Office for Africa Organization. Retrieved April 11, 2021, from https://www.afro.who.int/health-topics/tuberculosis-tb.
[16] Federal Ministry of Health Nigeria. (2010). National Tuberculosis and Leprosy Control Programme: Workers’ manual – Revise 5th Edition 1. Retrieved April 2, 2021, from https://www.who.int/hiv/pub/guidelines/nigeria_tb.pdf.
[17] Hassan, A., Olukolade, R., Ogbuji, Q., Onyemocho, A., Okwuonye, L., Igbabul, S., Okechukwu, J., Kusimo, O., Osho, A., Osinowo, K., & Ladipo, O. (2016). Evaluation of Tuberculosis Treatment Outcome of TB/HIV Co-Infection: A Four-Year Retrospective Cohort Study in HIV-Prevalent Setting of North Central Nigeria. Journal of Tuberculosis Research, 04(03), 122–133. https://doi.org/10.4236/jtr.2016.43015.
[18] Dye, C., Harries, A. D., Maher, D., Hosseini, S. M., Nkhoma, W., & Salaniponi, F. M. (2006). Tuberculosis. In Disease and Mortality in Sub-Saharan Africa. The International Bank for Reconstruction and Development / The World Bank. http://www.ncbi.nlm.nih.gov/pubmed/21290646.
[19] Nwokoro, U. U., Dahiru, T., Olorukooba, A., Daam, C. K., Waziri, H. S., Adebowale, A., Waziri, N. E., & Nguku, P. (2020). Determinants of perinatal mortality in public secondary health facilities, Abuja municipal area council, Federal Capital Territory, Abuja, Nigeria. Pan African Medical Journal, 37(114), 1–12. https://doi.org/10.11604/pamj.2020.37.114.17108.
[20] Federal Capital Territory. (2019). Federal Capital Territory (FCT) Health Sector Resource Mobilisation Plan (2018–2022). http://www.healthpolicyplus.com/ns/pubs/17373-17676_NigeriaFCTRMP.pdf.
[21] Hamisu, A. W., Etapelong, S. G., Ayodeji, I. H., Furera, Z., Ningi, N., Jimoh, A., Fiona, B., Banda, R., Tegegne, S. G., Ajogwu, A., Nwachukwu, J., John, D., Abdurrahman, S., Ahmed, F., Adesola, L., Teresa, N., Adesola, O., Rahmat, A., Elizabeth, A., & Lydia, T. (2020). Assessment of the contribution of community active surveillance to covid-19 case detection in the Federal Capital Territory, Abuja, Nigeria. African Journal of Biology and Medical Research, 3(2), 98–110. www.abjournals.org.
[22] Kamweli, M., Id, A., Kwaga, J., Okolocha, E., & Mba, N. (2019). Prevalence and risk factors for multi-drug resistant Escherichia coli among poultry workers in the Federal Capital Territory , Abuja , Nigeria Prevalence and risk factors for multi-drug resistant Escherichia coli among poultry workers in the Federal Capit. November. https://doi.org/10.1371/journal.pone.0225379.
[23] Kyaw, K. W. Y., Kyaw, N. T. T., Kyi, M. S., Aye, S., Harries, A. D., Kumar, A. M. V., Oo, N. L., Satyanarayana, S., & Aung, S. T. (2020). HIV testing uptake and HIV positivity among presumptive tuberculosis patients in Mandalay, Myanmar, 2014-2017. Plos One, 15(6), e0234429. https://doi.org/10.1371/journal.pone.0234429.
[24] Kumar, A. M., Gupta, D., Kumar, A., Gupta, R. S., Kanchar, A., Rao, R., Shastri, S., Suryakanth, M. D., Rangaraju, C., Naik, B., Guddemane, D. K., Bhat, P., Nair, A. S., Harries, A. D., & Dewan, P. (2016). HIV testing among patients with presumptive tuberculosis: How do we implement it in a routine programmatic setting? Results of a large operational research from India. PLoS ONE, 11(5), e0156487. https://doi.org/10.1371/journal.pone.0156487.
[25] Dlodlo, R. A., Hwalima, Z. E., Sithole, S., Takarinda, K. C., Tayler-Smith, K., & Harries, A. D. (2015). Are HIV-positive presumptive tuberculosis patients without tuberculosis getting the care they need in Zimbabwe? Public Health Action, 5(4), 217–221. https://doi.org/10.5588/pha.15.0036.
[26] Wasihun, A. G., Dejene, T. A., & Hailu, G. G. (2020). Frequency of MTB and rifampicin resistance MTB using Xpert-MTB/RIF assay among adult presumptive tuberculosis patients in Tigray, Northern Ethiopia: A cross sectional study. PLoS ONE, 15(11 November), e0240361. https://doi.org/10.1371/journal.pone.0240361.
[27] MacPherson, P., Lebina, L., Motsomi, K., Bosch, Z., Milovanovic, M., Ratsela, A., Lala, S., Variava, E., Golub, J. E., Webb, E. L., & Martinson, N. A. (2020). Prevalence and risk factors for latent tuberculosis infection among household contacts of index cases in two South African provinces: Analysis of baseline data from a cluster-randomised trial. PLOS ONE, 15(3), e0230376. https://doi.org/10.1371/Journal.Pone.0230376.
[28] Gelaw, B., Tigabu, A., Tadesse, T., Tegegne, Z., Hailu, W., Mahmud, E., Sisay, T., & Sendeku, W. (2021). Mycobacterium tuberculosis and HIV co-infection among presumptive tuberculosis cases and asthmatic patients at university of gondar hospital, northwest ethiopia. Clinical Laboratory, 67(1), 1–8. https://doi.org/10.7754/Clin.Lab.2020.200458.
[29] NACA. (2020). About HIV/AIDS - NACA Nigeria. Retrieved April 11, 2021, from https://naca.gov.ng/about-hivaids/.
[30] Okonko, I. O., Ejike, I. U., Innocent-Adiele, C., & Cookey, T. I. (2020). HIV coinfections with tuberculosis among HIV-1 infected individuals in old cross river state, Nigeria. Journal of Immunoassay and Immunochemistry, 41(3), 245–256. https://doi.org/10.1080/15321819.2020.1717527.
[31] Ibrahim, M. A., Abdulkadir, B., Y. Y. Riko, Farida, A. T., Mujahid, H., Ezekiel, B. K., Usman, A., Ahmad, M. A., Isah, M. G. and Murtala, S. (2020). A Survey on Tuberculosis and HIV Co-Infection among Presumptive Tuberculosis Patients within Zuru Emirate Council, Kebbi State, Nigeria. Nigerian Journal of Microbiology, 34(2), 5380–5389. http://www.nsmjournal.org.ng/2020-34-2/19.pdf.
[32] Nutor, J.J., Duah, H.O., Agbadi, P. et al. (2020). Spatial analysis of factors associated with HIV infection in Malawi: indicators for effective prevention. BMC Public Health 20, 1167. https://doi.org/10.1186/s12889-020-09278-0.
[33] Anoubissi JdD, Gabriel EL, Kengne Nde C, Fokam J, Tseuko DG, Messeh A, et al. (2019) Factors associated with risk of HIV-infection among pregnant women in Cameroon: Evidence from the 2016 national sentinel surveillance survey of HIV and syphilis. Plos One 14(4): e0208963. https://doi.org/10.1371/journal.pone.0208963.
Viewed PDF 1077 16 -
 Assessment of Injection Safety Practice in Health Care Settings: a Case from the GambiaAuthor: Robert NinsonDOI: 10.21522/TIJPH.2013.10.04.Art027
Assessment of Injection Safety Practice in Health Care Settings: a Case from the GambiaAuthor: Robert NinsonDOI: 10.21522/TIJPH.2013.10.04.Art027Assessment of Injection Safety Practice in Health Care Settings: a Case from the Gambia
Abstract:
Unsafe injection practices transmit bloodborne pathogens on a large scale worldwide and thus the Ministry of Health was assisted in conducting an assessment of injection safety in the Gambia in 2021. Interviews and observation of injection practices in all of the public health facilities and a sample of private health facilities including NGO. A total of 81 health facilities had been involved. Sterilisation of injection material observed in 3 facilities (3.7%) for therapeutic injection. Vaccinations, used either AD syringe (83.7%) or disposable syringes (16.3%). Re-used injection equipment without sterilisation in facilities was 8.6%. Proportion of health facilities in lack of AD syringes is 6.3%. 87.3% of the health facilities the availability of AD syringes was over than 50 units. Lack of disposable syringes was 17.3% of the health facilities. In 46 health facilities (56.8%), the availability of disposable syringes was over 20 units. Lack of safety box in facilities was 50.6% (n=41). Needle stick injuries have been observed in 79.7% (n=74) of the health facilities. A proportion of 70.9% of vaccinators and 52.1% of curative injection providers reported experiencing at least one needle-stick injury. Lack of safety boxes and waste disposable facilities, unsafe behaviours and poor sharp waste management lead to unsafe injection practices in the Gambia, exposing patients, health care workers and community to bloodborne infections. A coordinated strategy, training of health workers, and encouraging of the proper disposal of sharp required to prevent injection-associated infections in the Gambia.
Keywords: AD syringes, Injection, Needles, Safety boxes.Assessment of Injection Safety Practice in Health Care Settings: a Case from the Gambia
References:
[1] Naik A, Gharat V, Bansal RK. An Assessment of Injection Practices in Urban Health Centers of Surat City: Are the Health Care Workers Safe? National Journal of Community Medicine. 2012;3(01):125–8.
[2] Yan YW, Yan J, Zhang GP, Gao ZL, Jian HX. Prevalence of injections and knowledge of safe injections among rural residents in Central China. Singapore Medical Journal. 2007;48(8):769.
[3] Hutin YJ, Hauri AM, Armstrong GL. Use of injections in healthcare settings worldwide, 2000: literature review and regional estimates. Bmj. 2003;327(7423):1075.
[4] Hardon AP, van Staa A. Injection practices on the developing world: Results and recommendations from field studies in Uganda and Indonesia. 1995.
[5] Daly AD, Nxumalo MP, Biellik RJ. An assessment of safe injection practices in health facilities in Swaziland. South African Medical Journal. 2004;94(3):194–7.
[6] Pepin J, Abou Chakra CN, Pepin E, Nault V, Valiquette L. Evolution of the global burden of viral infections from unsafe medical injections, 2000–2010. PloS one. 2014;9(6):e99677.
[7] Water S, Organization WH. Safe health-care waste management: policy paper. World Health Organization; 2004.
[8] Ibrahim S, Salem N, Soliman S. Assessment of Safe Injection Practices and Needlestick Injury Among Nursing Students At Mansoura University. Mansoura Nursing Journal. 2021;8(1):59–76.
[9] Luby S. Injection safety. Emerging Infectious Diseases. 2001;7(3 Suppl):535.
[10] Hauri AM, Armstrong GL, Hutin YJ. The global burden of disease attributable to contaminated injections given in health care settings. International Journal of STD & AIDS. 2004;15(1):7–16.
[11] Matsubara C, Sakisaka K, Sychareun V, Phensavanh A, Ali M. Anxiety, and perceived psychological impact associated with needle stick and sharp device injury among tertiary hospital workers, Vientiane, Lao PDR. Industrial health. 2020;2019–0088.
[12] Simonsen L, Kane A, Lloyd J, Zaffran M, Kane M. Unsafe injections in the developing world and transmission of bloodborne pathogens: a review. Bulletin of the World Health Organization. 1999;77(10):789.
[13] Hutin Y, Hauri A, Chiarello L, Catlin M, Stilwell B, Ghebrehiwet T, et al. best infection control practices for intradermal, subcutaneous, and intramuscular needle injections. Bulletin of the World Health Organization. 2003; 81:491–500.
[14] Network SIG. Report of the SIGN2010 meeting. In: Annual meeting of the Safe Injection Global Network Dubai, United Arab Emirates. 2010. p. 9–11.
[15] Kotwal A. Innovation, diffusion and safety of a medical technology: a review of the literature on injection practices. Social science & medicine. 2005;60(5):1133–47.
[16] Kane A, Lloyd J, Zaffran M, Simonsen L, Kane M. Transmission of hepatitis B, hepatitis C and human immunodeficiency viruses through unsafe injections in the developing world: model-based regional estimates. Bulletin of the World Health Organization. 1999;77(10):801.
[17] Simonsen L, Kane A, Lloyd J, Zaffran M, Kane M. Unsafe injections in the developing world and transmission of bloodborne pathogens: a review. Bulletin of the World Health Organization. 1999;77(10):789.
[18] World Health Organization. Revised injection safety assessment tool: tool C - revised [Internet]. World Health Organization; 2008 [cited 2022 Nov 9]. Report No.: WHO/EHT/08.08. Available from: https://apps.who.int/iris/handle/10665/330070.
[19] Sahu D, Gandhi N. Assessment of safe injection practices in a tertiary care hospital: a cross-sectional study from Chhattisgarh. National Journal of Community Medicine. 2015;6(04):500–3.
[20] Statistics GB of. The Gambia 2013 Population and Housing Census Preliminary Results. Gambia Bureau of Statistics Serre Kunda, The Gambia; 2013.
[21] Abdul-Lateef SJ, Sulaiman MH, Jasim MS. Assessment of injection safety practice among nurses at primary health care centers in Mosul. Organization. 2000; 2:5.
[22] Al Awaidy S, Zayed B, Ramadan M, Hsairi M. Assessment of safe injection practices in health facilities in Oman. Eastern Mediterranean Health Journal. 2018;24(4):351–9.
Viewed PDF 981 26 -
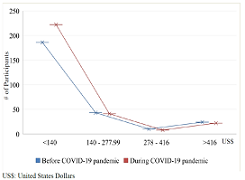 Impact of the Covid-19 Pandemic on Care of Patients with Diabetes Mellitus at Kitwe Teaching Hospital in 2021Author: Webster CheweDOI: 10.21522/TIJPH.2013.10.04.Art028
Impact of the Covid-19 Pandemic on Care of Patients with Diabetes Mellitus at Kitwe Teaching Hospital in 2021Author: Webster CheweDOI: 10.21522/TIJPH.2013.10.04.Art028Impact of the Covid-19 Pandemic on Care of Patients with Diabetes Mellitus at Kitwe Teaching Hospital in 2021
Abstract:
Coronavirus disease 2019 (Covid-19) pandemic tested the resilience of the health care system in many countries including Zambia. At the peak, disruption of the global supply chain affected availability of essential commodities needed to manage many health ailments like diabetes mellitus (DM). The study was aimed to understand the challenges faced by DM patients in accessing specialist services at KTH DM specialist clinic during the Covid-19 pandemic in 2021. A cross sectional descriptive study was conducted with a total of 293 participants (109 males and 184 females) recruited using a designed structured questionnaire and results analyzed using Microsoft Office Excel 2016 and the Statistical Package for Social Sciences (SPSS) version 16.0 software. The mean age was 54.0 ± 13.0 years old with 78(26.6%) being below the age of 45 years. 197(67.2%) were married and 157(53.6%) had primary education or less. 216(73.7%) and 222(75.8%) were earning <US$5.00 per day before and during Covid-19 pandemic respectively while the majority were spending one fifth of their earned income on medication from private pharmacies alone. 231(78.8%) had T2DM while 149(50.8%) had high plasma glucose levels; high BMI, high waist circumference and hypertension 184(62.8%). The study suggested that disruption of outpatient services led to patients presenting with high plasma glucose levels, poorly controlled weight (high BMI and high waist circumference). Commonest complications included hypertension and peripheral neuropathy. There is a need to devise a more pragmatic and resilient healthcare system in future to minimize the effects of any pandemic should they arise.
Keywords: Covid-19, Diabetes medication, Diabetes mellitus, Essential healthcare services, Hypertension, Lifestyle modification.Impact of the Covid-19 Pandemic on Care of Patients with Diabetes Mellitus at Kitwe Teaching Hospital in 2021
References:
[1] R. (chair) et al. Williams, IDF Diabetes Atlas 9th. 2019.
[2] American Diabetes Association, “Standards of Medical Care in Diabetes—2022 Abridged for Primary Care Providers,” Clin. Diabetes, vol. 40, no. 1, pp. 10–38, Jan. 2022, doi: 10.2337/cd22-as01.
[3] A. Ramachandran, C. Snehalatha, E. Latha, M. Manoharan, and V. Vijay, “Impacts of urbanisation on the lifestyle and on the prevalence of diabetes in native Asian Indian population,” Diabetes Res. Clin. Pract., vol. 44, no. 3, pp. 207–213, Jun. 1999, doi: 10.1016/S0168-8227(99)00024-8.
[4] T. I. A. SØrensen, “The changing lifestyle in the world: Body weight and what else?” in Diabetes Care, 2000, vol. 23, no. SUPPL. 2.
[5] N. G. Forouhi and N. J. Wareham, “Epidemiology of diabetes,” Medicine (Baltimore)., vol. 38, no. 11, pp. 602–606, Nov. 2010, doi: 10.1016/j.mpmed.2010.08.007.
[6] S. Mallapaty, “Evidence suggests the coronavirus might trigger diabetes,” Nature, pp. 16–17, 2020.
[7] S. Peric and T. M. Stulnig, “Diabetes and Covid-19,” Wien. Klin. Wochenschr., vol. 132, no. 13–14, pp. 356–361, Jul. 2020, doi: 10.1007/s00508-020-01672-3.
[8] L. Marchand, M. Pecquet, and C. Luyton, “Type 1 diabetes onset triggered by Covid-19,” Acta Diabetol., vol. 57, no. 10, pp. 1265–1266, Oct. 2020, doi: 10.1007/s00592-020-01570-0.
[9] S. Lou Bailey et al., “Diabetes mellitus in Zambia and the Western Cape province of South Africa: Prevalence, risk factors, diagnosis and management,” Diabetes Res. Clin. Pract., vol. 118, pp. 1–11, 2016, doi: 10.1016/j.diabres.2016.05.001.
[10] Zambia Statistical Agency, “The Zambia Statistical Agency (ZamStats).” https://www.zamstats.gov.zm (accessed May 20, 2021).
[11] IMF, World Economic Outlook: Recovery During a Pandemic, no. May. 2021.
[12] African Development Bank (AfDB) Group, “Zambia Economic Outlook,” 2021. https://www.afdb.org/en/countries-southern-africa-zambia/zambia-economic-outlook (accessed May 20, 2021).
[13] Zambia Ministry of Finance, “Annual Economic Report - 2019,” Lusaka, 2020. [Online]. Available: https://www.mof.gov.zm/?wpfb_dl=264.
A. Sharma, P. Gupta, and R. Jha, “Covid-19: Impact on Health Supply Chain and Lessons to Be Learnt,” J. Health Manag., vol. 22, no. 2, pp. 248–261, Jun. 2020, doi: 10.1177/0972063420935653.
[14] V. Haldane et al., “Health systems resilience in managing the Covid-19 pandemic: lessons from 28 countries,” Nat. Med., vol. 27, no. 6, pp. 964–980, Jun. 2021, doi: 10.1038/s41591-021-01381-y.
[15] A. Sagan et al., “Covid-19 and Health Systems Resilience: Lessons Going Forward,” Eurohealth (Lond)., vol. 26, no. 2, pp. 20–24, 2020, [Online]. Available: https://apps.who.int/iris/bitstream/handle/10665/336290/Eurohealth.
[16] A. Desta et al., “Impacts of Covid-19 on essential health services in Tigray, Northern Ethiopia: A pre-post study,” PLoS One, vol. 16, no. 8, p. e0256330, Aug. 2021, doi: 10.1371/journal.pone.0256330.
[17] M. Zakoji and T. Sundararaman, “Emerging good practices and lessons learnt to maintain essential health services during the Covid-19 pandemic,” WHO South-East Asia J. Public Heal., vol. 10, no. 3, p. 26, 2021, doi: 10.4103/2224-3151.309868.
[18] Z. Aranda et al., “Disruptions in maternal health service use during the Covid-19 pandemic in 2020: Experiences from 37 health facilities in low-income and middle-income countries,” BMJ Glob. Heal., vol. 7, no. 1, pp. 1–10, 2022, doi: 10.1136/bmjgh-2021-007247.
[19] K. Blanchet et al., “Protecting essential health services in low-income and middle-income countries and humanitarian settings while responding to the Covid-19 pandemic,” BMJ Glob. Heal., vol. 5, no. 10, pp. 1–9, 2020, doi: 10.1136/bmjgh-2020-003675.
[20] World Health Organization, “Covid-19 continues to disrupt essential health services in 90% of countries,” 2021. https://www.who.int/news/item/23-04-2021-covid-19-continues-to-disrupt-essential-health-services-in-90-of-countries (accessed May 20, 2021).
[21] World Health Organization, “Nearly 1 in 5 Covid-19 deaths in the African region linked to diabetes,” 2020. https://www.afro.who.int/news/nearly-1-5-covid-19-deaths-african-region-linked-diabetes (accessed May 20, 2021).
[22] A. Huang et al., “Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China,” Lancet, vol. 395, no. 10223, pp. 497–506, Feb. 2020, doi: 10.1016/S0140-6736(20)30183-5.
[23] A. Flyvbjerg, “Pathogenesis of Microvascular Complications,” in Textbook of Diabetes, Chichester, UK: John Wiley & Sons, Ltd, 2016, pp. 541–553.
[24] M. Khamaisi, G. L. King, K. Park, and Q. Li, “Pathogenesis of Microvascular Complications,” in Diabetes Complications, Comorbidities and Related Disorders, 2nd ed., Springer, Cham, 2020, pp. 161–201.
[25] M. J. Fowler, “Microvascular and Macrovascular Complications of Diabetes,” Clin. Diabetes, vol. 26, no. 2, pp. 77–82, Apr. 2008, doi: 10.2337/diaclin.26.2.77.
[26] Diabetes Control and Complications Trial Research Group, “Effect of intensive diabetes treatment on the development and progression of long-term complications in adolescents with insulin-dependent diabetes mellitus: Diabetes Control and Complications Trial,” J. Pediatr., vol. 125, no. 2, pp. 177–188, Aug. 1994, doi: 10.1016/S0022-3476(94)70190-3.
[27] UK Prospective Diabetes Study (UKPDS) Group, “Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34),” Lancet, vol. 352, no. 9131, pp. 854–865, Sep. 1998, doi: 10.1016/S0140-6736(98)07037-8.
[28] Z. He and G. L. King, “Microvascular complications of diabetes,” Endocrinol. Metab. Clin. North Am., vol. 33, no. 1, pp. 215–238, Mar. 2004, doi: 10.1016/j.ecl.2003.12.003.
[29] G. Rayman et al., “Guidelines for the management of diabetes services and patients during the COVID‐19 pandemic,” Diabet. Med., vol. 37, no. 7, pp. 1087–1089, Jul. 2020, doi: 10.1111/dme.14316.
[30] A. Kazi and L. Blonde, Classification of diabetes mellitus, vol. 21, no. 1. 2001.
[31] M. A. B. Khan, M. J. Hashim, J. K. King, R. D. Govender, H. Mustafa, and J. Al Kaabi, “Epidemiology of Type 2 Diabetes – Global Burden of Disease and Forecasted Trends,” J. Epidemiol. Glob. Health, vol. 10, no. 1, p. 107, 2019, doi: 10.2991/jegh.k.191028.001.
[32] H. A. van Dam, F. G. van der Horst, L. Knoops, R. M. Ryckman, H. F. J. M. Crebolder, and B. H. W. van den Borne, “Social support in diabetes: a systematic review of controlled intervention studies,” Patient Educ. Couns., vol. 59, no. 1, pp. 1–12, Oct. 2005, doi: 10.1016/j.pec.2004.11.001.
[33] J. L. Strom and L. E. Egede, “The Impact of Social Support on Outcomes in Adult Patients with Type 2 Diabetes: A Systematic Review,” Curr. Diab. Rep., vol. 12, no. 6, pp. 769–781, Dec. 2012, doi: 10.1007/s11892-012-0317-0.
[34] K. Y. Chan, W. Cockshaw, K. Smith, E. Holmes-Truscott, F. Pouwer, and J. Speight, “Social support and self-care outcomes in adults with diabetes: The mediating effects of self-efficacy and diabetes distress. Results of the second diabetes MILES – Australia (MILES-2) study,” Diabetes Res. Clin. Pract., vol. 166, p. 108314, Aug. 2020, doi: 10.1016/j.diabres.2020.108314.
[35] K. D. Adam et al., “Factors affecting diabetes knowledge in Type 2 diabetic veterans,” Diabetologia, vol. 46, no. 8, pp. 1170–1178, Aug. 2003, doi: 10.1007/s00125-003-1161-1.
[36] F. Fernanda et al., “Relationship between knowledge, attitude , education and duration of disease in individuals with diabetes mellitus,” Acta Paul Enferm, vol. 25, no. 2, pp. 284–290, 2012.
[37] M. Delamater, “Improving Patient Adherence,” Clin. Diabetes, vol. 24, no. 2, pp. 71–77, Apr. 2006, doi: 10.2337/diaclin.24.2.71.
[38] A. Kalungia, M. Mwale, I. S. Sondashi, B. Mweetwa, P. Yassa, and G. Kadimba, “Availability of Essential Antihypertensive and Antidiabetic Medicines in Public Health Facilities in Lusaka District, Zambia,” Med. J. Zambia, vol. 44, no. 3, pp. 140–148, 2017.
[39] H. Kaiser, L. Hehman, B. C. Forsberg, W. M. Simangolwa, and J. Sundewall, “Availability, prices and affordability of essential medicines for treatment of diabetes and hypertension in private pharmacies in Zambia,” PLoS One, vol. 14, no. 12, p. e0226169, Dec. 2019, doi: 10.1371/journal.pone.0226169.
[40] amnath S. Ramanathan, “Correlation of duration, hypertension and glycemic control with microvascular complications of diabetes mellitus at a tertiary care hospital,” Integr. Mol. Med., vol. 4, no. 1, 2017, doi: 10.15761/IMM.1000272.
[41] S. Zoungas et al., “Association of HbA1c levels with vascular complications and death in patients with type 2 diabetes: evidence of glycaemic thresholds,” Diabetologia, vol. 55, no. 3, pp. 636–643, Mar. 2012, doi: 10.1007/s00125-011-2404-1.
[42] T.-C. Li et al., “Glycemic control paradox: Poor glycemic control associated with higher one-year and eight-year risks of all-cause hospitalization but lower one-year risk of hypoglycemia in patients with type 2 diabetes,” Metabolism, vol. 64, no. 9, pp. 1013–1021, Sep. 2015, doi: 10.1016/j.metabol.2015.05.004.
[43] L. Perreault et al., “Sex Differences in Diabetes Risk and the Effect of Intensive Lifestyle Modification in the Diabetes Prevention Program,” Diabetes Care, vol. 31, no. 7, pp. 1416–1421, Jul. 2008, doi: 10.2337/dc07-2390.
[44] M. A. M. Jacobs-van der Bruggen et al., “Cost-Effectiveness of Lifestyle Modification in Diabetic Patients,” Diabetes Care, vol. 32, no. 8, pp. 1453–1458, Aug. 2009, doi: 10.2337/dc09-0363.
[45] S. Carlsson, N. Hammar, and V. Grill, “Alcohol consumption and type 2 diabetes,” Diabetologia, vol. 48, no. 6, pp. 1051–1054, Jun. 2005, doi: 10.1007/s00125-005-1768-5.
Viewed PDF 1080 27 -
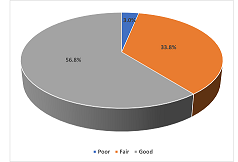 Perception of Health Workers on Reporting of Adverse Events Following Immunization in Jigawa State, Nigeria, 2022Author: Uba Belinda VernyuyDOI: 10.21522/TIJPH.2013.10.04.Art029
Perception of Health Workers on Reporting of Adverse Events Following Immunization in Jigawa State, Nigeria, 2022Author: Uba Belinda VernyuyDOI: 10.21522/TIJPH.2013.10.04.Art029Perception of Health Workers on Reporting of Adverse Events Following Immunization in Jigawa State, Nigeria, 2022
Abstract:
An adverse event following immunization (AEFI) is any untoward medical occurrence which follows immunization, and which does not necessarily have a causal relationship with the usage of the vaccine. Reporting of AEFI is suboptimal amongst healthcare workers (HCWs). This study aimed to determine health workers’ perception on AEFI reporting. A descriptive cross-sectional study was conducted among health workers in selected health facilities in Jigawa State. We used an Open data kit (ODK) based self-administered questionnaire to collect data on socio demographic characteristics, knowledge, and perception of respondents on AEFI. Data was analyzed using Statistical Package for Social Sciences (SPSS), for frequencies, associations and factors affecting HCWs perception of AEFI reporting at 5% significance (p-value<0.05) and 95% confidence interval. Perception was graded as: poor<50%, fair 50–70% and good ≥70%. Of the 400 respondents, 227(56.8%) had good perception. Building public trust in immunization (94.8%), to enable proper diagnosis and management (94.0%), elicit training needs (94.0%) and reduce consequences of AEFI on health workers (86.0%) were the main reasons for reporting AEFI. The barriers to reporting AEFI were time constraints (51.6%), poor feedback (48.8%) and fear of consequences (41.0%). AEFI knowledge (AOR 2.312, p=0.018) and receipt of feedback on reported AEFIs (AOR 0.45, p=0.026) were independent predictors of good perception of AEFI. Only 57% of health workers had a good perception of AEFI. To improve reporting of AEFI, there is need to train heath workers and strengthen feedback mechanism of AEFI surveillance system.
Keywords: Adverse events following immunization, Health providers, Perception, Surveillance.Perception of Health Workers on Reporting of Adverse Events Following Immunization in Jigawa State, Nigeria, 2022
References:
[1] World Health Organization (WHO), Health Equity, Accessed: 3 May 2022. https://www.who.int/data/health-equity/report_2018_immunization.
[2] Amarasinghe A., 2016, World Health Organization, Global Advisory Committee on Vaccine Safety. Global manual on surveillance of adverse events following immunization. http://apps.who.int/iris/bitstream/10665/206144/1/9789241507769_eng.pdf Accessed 29 December 2020.
[3] McClenathan B. M., Edwards K. M., 2019, Vaccine safety: An evolving evidence‐based science. Br J Clin Pharmacol, 85(12):2649–2651.
[4] Mark K., 2022, Children’s Vaccine Program: The Case for Childhood Immunization; (5).
[5] World Health Organization, Vaccines, and immunization, Accessed: 23 April 2022. https://www.who.int/health-topics/vaccines-and-immunization.
[6] World Health Organization, Vaccine Safety Basics, Accessed 21 December 2020. https://vaccine-safety-training.org/investigation.html.
[7] World Health Organization, 2008, Reaching Every District Approach. http://www.who.int/bulletin/volumes/86/3/07-042127/en/.
[8] World Health Organization, Adverse events following immunization, Accessed 29 December 2020. https://www.who.int/vaccine_safety/initiative/tech_support/Part-3.pdf?ua=1.
[9] The Global Vaccine Safety Initiative (GVSI), Accessed 23 April 2022. https://www.who.int/initiatives/the-global-vaccine-safety-initiative.
[10] Lei J., Balakrishnan M.R., Gidudu J. F., Zuber P. L. F., 2018, Use of a new global indicator for vaccine safety surveillance and trends in adverse events following immunization reporting 2000-2015 | Elsevier Enhanced Reader, doi: 10.1016/j.vaccine. 02.012.
[11] World Health Organisation, 2011, Global Vaccine Action Plan 2011-2020.
[12] Siddiqui M., Salmon D. A., Omer S. B., 2013, Epidemiology of vaccine hesitancy in the United States. Hum Vaccines Immunother, 9(12):2643–2648.
[13] Akanmori B. D., Traore T., Balakrishnan M., Maure C., Zuber P., Mihigo R., 2018, Vaccine Safety and Pharmacovigilance in the African Region: Recent updates. J Immunol Sci. specialissue (1). https://www.immunologyresearchjournal.com/articles/vaccine-safety-and-pharmacovigilance-in-the-african-region-recent-updates.html. Accessed 23 April 2022.
[14] Orji C.J., Chime O. H., Ugwuonah C., 2020, Incidence and Pattern of Adverse Events Following Immunization in the 2017/2018 Measles Vaccination Campaign in Nigeria. Online J Health Allied Sci OJHAS,18(4). http://hinaring.summon.serialssolutions.com/2.0.0/link/0/.
[15] Gbenewei E., Nomhwange T., Taiwo L., Ayodeji I, Yusuf K., Jean Baptiste A. E., et al., 2021, Adverse events following immunization: Findings from 2017/2018 measles vaccination campaign, Nigeria AEFI reporting in 2017/2018 measles vaccination campaign. Vaccine, 39:C82–C88.
[16] Mehmeti I., Nelaj E., Simaku A., Tomini E., Bino S., 2017, Knowledge, practice, and approaches of health professionals to adverse events following immunization and their reporting in Albania. Heliyon, 3(6): e00331–e00331.
[17] Mohammed L. A., Aliyu A. A., Maiha B. B., Isa A., 2018, Knowledge, perception, and reporting attitude of adverse effects following immunization among primary healthcare workers in sabon gari local government area Zaria, Kaduna State, Nigeria. Niger J Basic Clin Sci15(1):81.
[18] Ogunyemi R., Odusanya O., 2016, A survey of knowledge and reporting practices of primary healthcare workers on adverse experiences following immunisation in alimosho local government area, Lagos. Niger Postgrad Med J, 23:79.
[19] Umar A., Sufiyan M., Tukur D., Onoja-Alexander M., Amadu L., Bashir S., 2020, Knowledge of Adverse Events Following Immunization Reporting Tool and System Among Primary Healthcare Workers in Jigawa State. Infect Control Hosp Epidemiol, 41(S1):s308–s308.
[20] M Oche O., 2020, Knowledge, Attitude and Reporting Practices on Adverse Events Following Immunization among Routine Immunization Service Providers in Health Facilities of Sokoto State, Nigeria. International Journal of Tropical Disease & Health.
[21] Sani U. M., Oche M. O., Raji M. O., Ango U. M., Jiya N. M., 2019, Knowledge, Attitude and Reporting Practices on Adverse Events Following Immunization among Routine Immunization Service Providers in Health Facilities of Sokoto State. Nigeria. Int J Trop Dis Health,1–14.
[22] Laryea E. B., Frimpong J. A., Noora C. L., Tengey J., Bandoh D., Sabblah G., et al., 2022, Evaluation of the adverse events following immunization surveillance system, Ghana 2019. PLOS ONE, 17(3):e0264697.
[23] Ogunyemi A., 2016, Survey of knowledge and reporting practices of primary healthcare workers on adverse experiences following immunisation in alimosho local government area, Lagos. Accessed 21 December 2020. https://www.npmj.org/article.asp?issn=1117-1936 volume 23; issue 2.
[24] Yamoah P., Bangalee V., Oosthuizen F., 2019, Knowledge and Perceptions of Adverse Events Following Immunization among Healthcare Professionals in Africa: A Case Study from Ghana. Vaccines Basel, 7(1):28.
[25] World Health Organization, Adverse events following immunization (AEFI), Accessed: 5 April 2022. https://www.who.int/teams/regulation-prequalification/regulation-and-safety/pharmacovigilance/health-professionals-info/aefi.
[26] National Primary Health Care Development Agency, 2018, Nigeria Field Guide on Surveillance of Adverse Events Following Immunization (AEFI) and Response.
Viewed PDF 1114 21 -
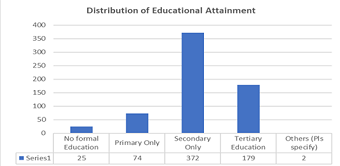 Self-Medication of Prescription Only Non-Steroidal Anti-Inflammatory Drugs among Households in Alimosho LGA, Lagos State, NigeriaAuthor: Dunoi Onwuemezie AfamDOI: 10.21522/TIJPH.2013.10.04.Art030
Self-Medication of Prescription Only Non-Steroidal Anti-Inflammatory Drugs among Households in Alimosho LGA, Lagos State, NigeriaAuthor: Dunoi Onwuemezie AfamDOI: 10.21522/TIJPH.2013.10.04.Art030Self-Medication of Prescription Only Non-Steroidal Anti-Inflammatory Drugs among Households in Alimosho LGA, Lagos State, Nigeria
Abstract:
The purpose of this study is to determine the knowledge, attitude, and practice of self-medication of NSAIDs among adults in Alimosho Local Government Area (LGA) of Lagos State. The study is descriptive inferential form cross-sectional study that involved collection of data from adults in the LGA. The data collected from questionnaires administered to adults who were randomly selected across the LGA was analyzed to evaluate the association between demographic characteristics and knowledge, attitude, and practice of self-medication. The respondents who participated in the research were adults who were 18 years and above. Of the 652 respondents 50.8% were males and while 49.2% were females. Demographic profile and Information sources were tested for association with self-medication. Among respondents, 80.6% admitted that they are self-medicated, and a binary logistic regression was performed to ascertain the effect of gender, age, marital status, and educational attainment on the likelihood of respondents engaging in self-medication. The overall logistic regression was statistically significant, χ2 (1) = 24.824, p< 0.005. The model explained 10.2% (Nagelkerke R2) of the variance in self-medication and correctly classified 80.4% of cases.
Keywords: Alimosho, Attitude, Knowledge, Lagos State, NAFDAC, NSAID, Perception, Self-medication.Self-Medication of Prescription Only Non-Steroidal Anti-Inflammatory Drugs among Households in Alimosho LGA, Lagos State, Nigeria
References:
[1] NAFDAC Green Book https://greenbook.nafdac.gov.ng/ (Accessed 11 October 2022).
[2] Batlouni M. (2010) Nonsteroidal anti-inflammatory drugs: cardiovascular, cerebrovascular, and renal effects. Arq Bras Cardiol. 2010;94(4):556-563.NAFDAC 2020.
[3] Boelsterli U. 2002 Mechanisms of NSAID-induced hepatotoxicity: focus on Nimesulide. Drug Safety, 25(9):633-648. DOI: 10.2165/00002018-200225090-00003. PMID: 12137558.
[4] Masubuchi Y., Yamada S., Horie T. 2000 Possible mechanisms of hepatocyte injury induced by diphenylamine and its structurally related NSAIDS. J Pharmacol Exp Ther. 292:982–987.
[5] NAFDAC 2019 Drug and related product labelling regulations 2019 https://www.nafdac.gov.ng/wp-content/uploads/Files/Resources/Regulations/All_Regulations/Drug-and-Related-Product-Labelling-Regulations-2019.pdf.
[6] NAFDAC 2021 Drug And Related Products Labelling Regulations, 2021 https://www.nafdac.gov.ng/wp-content/uploads/Files/Resources/Regulations/Regulations_2021/Drug-and-Related-Product-Labelling-Regulations-2021.pdf (Accessed 27 May 2022).
[7] ALG (n.d) Alimosho Local Government Area in Metro Lagos https://www.citypopulation.de/php/nigeria-metrolagos.php?cid=NGA025003.
[8] Wejnert, C., Pham, H., Krishna, N., Le, B., and DiNenno, E. 2012 Estimating design effect and calculating sample size for respondent-driven sampling studies of injection drug users in the United States. AIDS and behavior, 16(4), 797–806. https://doi.org/10.1007/s10461-012-0147-8.
[9] Charan J., and Biswas T. 2013 How to calculate sample size for different study designs in medical research, Indian journal of psychological medicine, 35(2), 121–126. https://doi.org/10.4103/0253-7176.116232.
[10] CSPro 2022 Census and Survey Processing System (CSPro) Online Available https://www.census.gov/data/software/cspro.html (Accessed March 2021).
[11] Bruce N., et al. 2008 Quantitative research methods for health research: a practical interactive guide to epidemiology and statistics. Chichester, UK: Wiley.
[12] Motola D., Vaccheri A., Silvani M. C., et al. 2004 Pattern of NSAID use in the Italian general population: a questionnaire-based survey. Eur J Clin Pharmacol,60(10):731–8.
[13] Shafie, M., Eyasu, M., Muzeyin, K., Worku, Y., & Martín-Aragón, S. 2018 Prevalence, and determinants of self-medication practice among selected households in Addis Ababa community. PloS one, 13(3), e0194122. https://doi.org/10.1371/journal.pone.0194122.
[14] Bidmon, S. and Terlutter, R. 2015 Gender Differences in Searching for Health Information on the Internet and the Virtual Patient-Physician Relationship in Germany: Exploratory Results on How Men and Women Differ and Why Journal of Medical Internet Research 2015, Volume 17, No 6: e156 (Accessed 01 October 2021).
[15] Ek, S. 2013 Gender differences in health information behaviour: a Finnish population-based survey Online available at: http://heapro.oxfordjournals.org/content/early/2013/08/28/heapro.dat063.full.pdf+html (Accessed 01 October, 2015).
[16] Esan D.T. 2018 “Assessment of Self-Medication Practices and Its Associated Factors among Undergraduates of a Private University in Nigeria”, Journal of Environmental and Public Health, vol. 2018, Article ID 5439079, 7 pages, 2018. https://doi.org/10.1155/2018/5439079.
[17] Bennadi, D. 2013 Self-medication: A current challenge. Journal of Basic and Clinical Pharmacy, 5(1), 19. https://doi.org/10.4103/0976-0105.128253.
[18] Kumari R., Kumar D., Bahl R., and Gupta 2012 Study of knowledge and practices of self-medication among medical students at Jammu. Journal of Medical Sciences, 15 (2):141-144.
[19] Gupta P., Bobhate P., and Shrivastava S. 2011 Determinants of self-medication practices in an urban slum community Asian Journal of Pharmaceutical and Clinical Research, 4 (3):54-57.
[20] Saha, A. et al. 2022 Risk factors associated with self-medication among the indigenous communities of Chittagong Hill Tracts, Bangladesh https://doi.org/10.1371/journal.pone.0269622.
[21] Asakitikpi, A. E. 2019. Healthcare Coverage and Affordability in Nigeria: An Alternative Model to Equitable Healthcare Delivery. In (Ed.), Universal Health Coverage. IntechOpen. https://doi.org/10.5772/intechopen.85978.
[22] Bart J. and Por M. et al. 2012 Addressing access barriers to health services: an analytical framework for selecting appropriate interventions in low-income Asian countries, Health Policy, and Planning, 27(4):288–300, https://doi.org/10.1093/heapol/czr038.
[23] McLeod S. 2019 What’s the difference between qualitative and quantitative research? https://www.simplypsychology.org/qualitative-quantitative.html.
[24] Cline R.J. and Haynes K. M. 2001 Consumer health information seeking on the Internet: the state of the art, Health Education Research, 16 (6):671–692, https://doi.org/10.1093/her/16.6.671.
[25] WHO, Royal Tropical Institute and University of Amsterdam. (2007). How to improve the use of medicines by consumers, Tercera edición. World Health Organization. https://apps.who.int/iris/handle/10665/69681.
Viewed PDF 859 25 -
 The Prevalence of Asymptomatic Malaria Amongst Nursery and Primary School Pupils in Bui, Northwest Cameroon: A Cross-Sectional StudyAuthor: Frederick Nchang ChoDOI: 10.21522/TIJPH.2013.10.04.Art031
The Prevalence of Asymptomatic Malaria Amongst Nursery and Primary School Pupils in Bui, Northwest Cameroon: A Cross-Sectional StudyAuthor: Frederick Nchang ChoDOI: 10.21522/TIJPH.2013.10.04.Art031The Prevalence of Asymptomatic Malaria Amongst Nursery and Primary School Pupils in Bui, Northwest Cameroon: A Cross-Sectional Study
Abstract:
Malaria is a public health concern worldwide, accounting for 31% of hospital consultations, 44% of hospitalisations, and 18% of deaths, and a cause of school absenteeism amongst pupils in Cameroon. The negative cognitive impact of malaria on pupils is a call for concern. This study aimed at determining the prevalence of asymptomatic malaria among pupils. A cross-sectional study was conducted from December 2015 to April 2016 in eight Nursery and Primary Schools in Bui. A total of 1,152 pupils were systematically screened for malaria using light microscopy. All anaemic and malaria positive cases were administered ferum folate/ferrous sulphate and artemether-lumefantrine for treatment. The prevalence of malaria and anaemia were 12% and 18.4%, respectively; anaemia accounted for 26.1% of all positive diagnostic tests. Malaria infection was significantly higher in adolescents aged 5–12 years (73.9%), as well as amongst males (51.4%). The proportion of pupils with asymptomatic malaria and anaemia was high. Age, sex, school, and community were associated with asymptomatic malaria as well as anaemia. Malaria intervention programmes should target asymptomatic malaria carriers for treatment to minimise transmission.
Keywords: Asymptomatic malaria, Bui, Cameroon, Prevalence, School Children.The Prevalence of Asymptomatic Malaria Amongst Nursery and Primary School Pupils in Bui, Northwest Cameroon: A Cross-Sectional Study
References:
[1] WHO. World malaria report 2021 [Internet]. World Health Organization; 2021. Available from: https://www.who.int/publications/i/item/9789240040496.
[2] Antonio-Nkondjio C, Ndo C, Njiokou F, Bigoga JD, Awono-Ambene P, Etang J, et al. Review of malaria situation in Cameroon: technical viewpoint on challenges and prospects for disease elimination. Parasit Vectors [Internet]. 2019 Oct 26 [cited 2022 Apr 12];12(1):501. Available from: https://doi.org/10.1186/s13071-019-3753-8.
[3] Ndong IC, van Reenen M, Boakye DA, Mbacham WF, Grobler AF. Trends in malaria admissions at the Mbakong Health Centre of the Northwest Region of Cameroon: a retrospective study. Malar J [Internet]. 2014 Aug 22 [cited 2022 Apr 12];13(1):328. Available from: https://doi.org/10.1186/1475-2875-13-328.
[4] Tangpukdee N, Duangdee C, Wilairatana P, Krudsood S. Malaria Diagnosis: A Brief Review. Korean J Parasitol [Internet]. 2009 Jun [cited 2022 Apr 4];47(2):93–102. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2688806/.
[5] Cho FN, Fru PN, Munguh SF, Cho BM, Jokwi PK, Fru CN, et al. Predictors of Ownership/Utilisation Indicators of Long-lasting Insecticide Nets in the Bamendankwe Health Area of Cameroon: A Cross-Sectional Study. Pan Afr J Life Sci. 2020 Dec 1;4.
[6] Fru PN, Cho FN, Tassang AN, Fru CN, Fon PN, Ekobo AS. Ownership and Utilisation of Long-Lasting Insecticidal Nets in Tiko Health District, Southwest Region, Cameroon: A Cross-Sectional Study. J Parasitol Res. 2021; 2021:8848091.
[7] Sato S. Plasmodium—a brief introduction to the parasites causing human malaria and their basic biology. J Physiol Anthropol [Internet]. 2021 Jan 7 [cited 2022 Apr 7]; 40:1. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7792015/.
[8] Tientche B, Fru-Cho J, Anong D, Ngouakam H, Nkuo-Akenji T. Assessment of Knowledge, Perception and Practices about Malaria in Some Rural Communities of Southwest Region, Cameroon. J Health Med Inform. 2020 Jan 1;11.
[9] Aschale Y, Mengist A, Bitew A, Kassie B, Talie A. Prevalence of malaria and associated risk factors among asymptomatic migrant laborers in West Armachiho District, Northwest Ethiopia. Res Rep Trop Med [Internet]. 2018 Jun 20 [cited 2022 Apr 15]; 9:95–101. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6047623/.
[10] Kwenti TE, Kwenti TDB, Njunda LA, Latz A, Tufon KA, Nkuo-Akenji T. Identification of the Plasmodium species in clinical samples from children residing in five epidemiological strata of malaria in Cameroon. Trop Med Health. 2017;45(14):1–8.
[11] MOH. Guidelines on malaria treatment in Cameroon; For Health Professionals. National Malaria Control Programme; 2019.
[12] Sumbele IUN, Nkain AJ, Ning TR, Anchang-Kimbi JK, Kimbi HK. Influence of malaria, soil-transmitted helminths, and malnutrition on haemoglobin level among school-aged children in Muyuka, Southwest Cameroon: A cross-sectional study on outcomes. PLOS ONE [Internet]. 2020 Mar 30 [cited 2022 Apr 12];15(3):e0230882. Available from: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0230882.
[13] WHO. Global technical strategy for malaria 2016-2030. United Kingdom: World Health Organization; 2015. 35 p.
[14] Antonio-nkondjio C, Kerah CH, Simard F, Awono-ambene P, Chouaibou M, Tchuinkam T, et al. Complexity of the Malaria Vectorial System in Cameroon: Contribution of Secondary Vectors to Malaria Transmission. J Med Entomol [Internet]. 2006 Nov 1 [cited 2022 Apr 17];43(6):1215–21. Available from: https://doi.org/10.1093/jmedent/43.6.1215.
[15] Ahmed A, Mulatu K, Elfu B. Prevalence of malaria and associated factors among under-five children in Sherkole refugee camp, Benishangul-Gumuz region, Ethiopia. A cross-sectional study. PloS One. 2021;16(2):e0246895.
[16] Nankabirwa J, Brooker SJ, Clarke SE, Fernando D, Gitonga CW, Schellenberg D, et al. Malaria in school-age children in Africa: an increasingly important challenge. Trop Med Int Health [Internet]. 2014 Nov [cited 2022 Apr 12];19(11):1294–309. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4285305/.
[17] Gari T, Loha E, Deressa W, Solomon T, Lindtjørn B. Malaria increased the risk of stunting and wasting among young children in Ethiopia: Results of a cohort study. PLOS ONE [Internet]. 2018 Jan 11 [cited 2022 Apr 12];13(1):e0190983. Available from: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0190983.
[18] Kojom Foko LP, Nolla NP, Nyabeyeu Nyabeyeu H, Tonga C, Lehman LG. Prevalence, Patterns, and Determinants of Malaria and Malnutrition in Douala, Cameroon: A Cross-Sectional Community-Based Study. BioMed Res Int [Internet]. 2021 Jul 13 [cited 2022 Apr 12];2021:e5553344. Available from: https://www.hindawi.com/journals/bmri/2021/5553344/.
[19] Mbohou CN, Foko LPK, Nyabeyeu HN, Tonga C, Nono LK, Kangam L, et al. Malaria screening at the workplace in Cameroon. PloS One. 2019;14(12):e0225219.
[20] Pandey A, Shingadia D. Treatment, and prevention of malaria in children. Paediatr Child Health [Internet]. 2022 Apr 7 [cited 2022 Apr 11]; Available from: https://www.sciencedirect.com/science/article/pii/S1751722222000373.
[21] Vorasan N, Pan-Ngum W, Jittamala P, Maneeboonyang W, Rukmanee P, Lawpoolsri S. Long-term impact of childhood malaria infection on school performance among school children in a malaria endemic area along the Thai Myanmar border. Malar J. 2015 Oct 9; 14:401.
[22] Lawpoolsri S, Sattabongkot J, Sirichaisinthop J, Cui L, Kiattibutr K, Rachaphaew N, et al. Epidemiological profiles of recurrent malaria episodes in an endemic area along the Thailand-Myanmar border: a prospective cohort study. Malar J. 2019 Apr 8;18(1):124.
[23] Danwang C, Khalil É, Achu D, Ateba M, Abomabo M, Souopgui J, et al. Fine scale analysis of malaria incidence in under-5: hierarchical Bayesian spatio-temporal modelling of routinely collected malaria data between 2012-2018 in Cameroon. Sci Rep. 2021 Jun 1;11(1):11408.
[24] Fokam EB, Dzi KTJ, Ngimuh L, Enyong P. The Effect of Long-Lasting Insecticide Bed Net Use on Malaria Prevalence in the Tombel Health District, South West Region-Cameroon. Malar Res Treat [Internet]. 2016 Jun 15 [cited 2022 Apr 12];2016: e3216017. Available from: https://www.hindawi.com/journals/mrt/2016/3216017/.
[25] Apinjoh T, Anchang J, Mugri R, Tangoh A, Nyingchu R, Chi H, et al. The Effect of Insecticide Treated Nets (ITNs) on Plasmodium falciparum Infection in Rural and Semi-Urban Communities in the Southwest Region of Cameroon. PloS One. 2015 Feb 25;10: e0116300.
[26] John Paul Tume S, Kimengsi J, Fogwe Z. Indigenous Knowledge and Farmer Perceptions of Climate and Ecological Changes in the Bamenda Highlands of Cameroon: Insights from the Bui Plateau. Climate. 2019 Dec 8; 7:1–18.
[27] Cho FN, Ngala H, Bongazi R, Kinsam R, Tata B, Aji D, et al. Effects of Soil Transmitted Helminths and Intestinal Protozoan Infections on Haemoglobin in School aged Children in Belo and Bui: A Cross-sectional Study. J Parasitol Res. 2021 Feb 1;2021.
[28] Wirkom V, Tata R, Agba M, Nwobu G, Ndze R, Onoja O, et al. Formol-Petrol Stool Concentration Method (Wirkom-Tata’s Stool Concentration Method): A Cheap Novel Technique for Detecting Intestinal Parasites in Resource-Limited Countries. Internet J Trop Med [Internet]. 2008 [cited 2022 Apr 12];5(1). Available from: https://scite.ai/reports/formol-petrol-stool-concentration-method-wirkom-tata-s-M6QMem.
[29] HFHC. Annual Report, 2016 [Internet]. Holy Family Health Centre, Djottin - Noni; 2016. Available from: http://tssfcameroon.org/health/.
[30] SEGH. Annual Report, 2016 [Internet]. Saint Elizabeth General Hospital Complex, Shisong; 2016. Available from: https://www.tssfcameroonhealth.de/hospitals-2/shisong-hospital/cardiac-center-shisong/.
[31] WHO. WHO guidelines for the treatment of malaria. World Health Organization; 2006. 266 p.
[32] WHO. WHO Guidelines for malaria. World Health Organization; 2021.
[33] Sumbele IUN, Sama SO, Kimbi HK, Taiwe GS. Malaria, Moderate to Severe Anaemia, and Malarial Anaemia in Children at Presentation to Hospital in the Mount Cameroon Area: A Cross-Sectional Study. Anemia [Internet]. 2016 [cited 2022 Apr 4]; 2016:5725634. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5118524/.
[34] Cheesbrough M. District Laboratory Practice in Tropical Countries. 2nd ed. Vol. 1. Cambridge: Cambridge University Press; 2009. 462 p.
[35] MOH. Health populations denominators 2018. Cameroon’s Ministry of Health; 2018.
[36] NIS. 2nd survey on the monitoring of public expenditures and the level of recipients’ satisfaction in the education and health sectors in Cameroon (PETS2),” in Health Component. Yaoundé: National Institute of Statistics; 2010. 1–116 p.
[37] Cheesbrough M. District Laboratory Practice in Tropical Countries. 2nd ed. Vol. 2. Cambridge: Cambridge University Press; 2006. 442 p.
[38] WHO. Manual of basic techniques for a health laboratory. 2nd ed. Geneva: World Health Organization; 2003. 398 p.
[39] WHO. Manual of basic techniques for a health laboratory, 2nd edition. Elliot J, editor. Bull World Health Organ [Internet]. 2004 Mar [cited 2022 Apr 12];82(3):229–229. Available from: https://iris.who.int/handle/10665/269104.
[40] WHO. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. Vitamin and Mineral Nutrition Information System [Internet]. World Health Organization; 2011. Available from: http://www.who.int/vmnis/indicators/haemoglobin.pdf.
[41] CDC. Laboratory diagnosis of malaria: Preparation of blood smears [Internet]. 2022 [cited 2022 Mar 27]. Available from: https://www.cdc.gov/dpdx/resources/pdf/benchAids/malaria/Malaria_procedures_benchaid.pdf.
[42] Shrestha B, Dunn L. The Declaration of Helsinki on Medical Research involving Human Subjects: A Review of Seventh Revision. J Nepal Health Res Counc. 2020 Jan 21;17(4):548–52.
[43] Worku L, Damtie D, Endris M, Getie S, Aemero M. Asymptomatic Malaria and Associated Risk Factors among School Children in Sanja Town, Northwest Ethiopia. Int Sch Res Not. 2014;2014:303269.
[44] Douamba Z, Dao NGL, Zohoncon TM, Bisseye C, Compaoré TR, Kafando JG, et al. Mother-to-Children Plasmodium falciparum Asymptomatic Malaria Transmission at Saint Camille Medical Centre in Ouagadougou, Burkina Faso. Malar Res Treat. 2014;2014:390513.
[45] Chiabi A, Djimafo ANM, Nguefack S, Mah E, Nguefack Dongmo F, Angwafo F. Severe malaria in Cameroon: Pattern of disease in children at the Yaounde Gynaeco-Obstetric and Pediatric hospital. J Infect Public Health [Internet]. 2020 Oct 1 [cited 2022 Apr 12];13(10):1469–72. Available from: https://www.sciencedirect.com/science/article/pii/S1876034120303932.
[46] Flavio A, Cedric Y, Nadia NAC, Payne VK. Malaria and Helminth Coinfection among Children at the Douala Gyneco-Obstetric and Pediatric Hospital. J Trop Med. 2021;2021:3702693.
[47] Emina JBO, Doctor HV, Yé Y. Profiling malaria infection among under-five children in the Democratic Republic of Congo. PloS One. 2021;16(5):e0250550.
[48] Kapesa A, Kweka EJ, Atieli H, Afrane YA, Kamugisha E, Lee MC, et al. The current malaria morbidity and mortality in different transmission settings in Western Kenya. PloS One. 2018;13(8):e0202031.
[49] Afoakwah C, Deng X, Onur I. Malaria infection among children under-five: the use of large-scale interventions in Ghana. BMC Public Health. 2018 Apr 23;18(1):536.
[50] Doudou MH, Mahamadou A, Ouba I, Lazoumar R, Boubacar B, Arzika I, et al. A refined estimate of the malaria burden in Niger. Malar J. 2012 Mar 27; 11:89.
[51] Wotodjo AN, Doucoure S, Gaudart J, Diagne N, Sarr FD, Faye N, et al. Malaria in Dielmo, a Senegal village: Is its elimination possible after seven years of implementation of long-lasting insecticide-treated nets? Plos One [Internet]. 2017 Jul 5 [cited 2022 Apr 12];12(7):e0179528. Available from: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0179528.
[52] Onyiah AP, Ajayi IO, Dada-Adegbola HO, Adedokun BO, Balogun MS, Nguku PM, et al. Long-lasting insecticidal net use and asymptomatic malaria parasitaemia among household members of laboratory-confirmed malaria patients attending selected health facilities in Abuja, Nigeria, 2016: A cross-sectional survey. PLOS ONE [Internet]. 2018 Sep 13 [cited 2022 Apr 12];13(9):e0203686. Available from: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0203686.
[53] Nyasa RB, Fotabe EL, Ndip RN. Trends in malaria prevalence and risk factors associated with the disease in Nkongho-mbeng; a typical rural setting in the equatorial rainforest of the South West Region of Cameroon. PloS One. 2021;16(5):e0251380.
[54] Sandie SM, Sumbele IUN, Tasah MM, Kimbi HK. Malaria parasite prevalence and Haematological parameters in HIV seropositive patients attending the regional hospital Limbe, Cameroon: a hospital-based cross-sectional study. BMC Infect Dis [Internet]. 2019 Nov 21 [cited 2022 Apr 12];19(1):988. Available from: https://doi.org/10.1186/s12879-019-4629-4.
[55] Robortella DR, Calvet AA, Amaral LC, Fantin RF, Guimarães LFF, França Dias MH, et al. Prospective assessment of malaria infection in a semi-isolated Amazonian indigenous Yanomami community: Transmission heterogeneity and predominance of submicroscopic infection. PloS One. 2020;15(3):e0230643.
[56] Quang HH, Chavchich M, Trinh NTM, Manh ND, Edstein MD, Martin NJ, et al. Cross-sectional survey of asymptomatic malaria in Dak Nong province in the Central Highlands of Vietnam for the malaria elimination roadmap. PLOS ONE [Internet]. 2021 Oct 20 [cited 2022 Apr 12];16(10): e0258580. Available from: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0258580.
[57] Tsegaye AT, Ayele A, Birhanu S. Prevalence, and associated factors of malaria in children under the age of five years in Wogera district, northwest Ethiopia: A cross-sectional study. PLOS ONE [Internet]. 2021 Oct 11 [cited 2022 Apr 12];16(10): e0257944. Available from: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0257944.
[58] Sama SO, Chiamo SN, Taiwe GS, Njume GE, Ngole Sumbele IU. Microcytic and Malarial Anaemia Prevalence in Urban Children ≤15 Years in the Mount Cameroon Area: A Cross-Sectional Study on Risk Factors. Anemia [Internet]. 2021 Apr 8 [cited 2022 Apr 4]; 2021:5712309. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8049821/.
[59] Tesema GA, Worku MG, Tessema ZT, Teshale AB, Alem AZ, Yeshaw Y, et al. Prevalence and
determinants of severity levels of anemia among children aged 6–59 months in sub-Saharan Africa: A multilevel ordinal logistic regression analysis. PLoS One [Internet]. 2021 Apr 23 [cited 2022 Apr 4];16(4): e0249978. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8064743/.[60] Ewusie JE, Ahiadeke C, Beyene J, Hamid JS. Prevalence of anemia among under-5 children in the Ghanaian population: estimates from the Ghana demographic and health survey. BMC Public Health [Internet]. 2014 Jun 19 [cited 2022 Apr 4]; 14:626. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4080691/.
Viewed PDF 1788 73

