Table of Contents - Issue
Recent articles
-
 Disorders of Blood Gases, Electrolytes, Magnesium, Albumin and Calcium Metabolism in SARS-CoV-2-infected PatientsAuthor: Ajibola AdisaDOI: 10.21522/TIJPH.2013.10.01.Art001
Disorders of Blood Gases, Electrolytes, Magnesium, Albumin and Calcium Metabolism in SARS-CoV-2-infected PatientsAuthor: Ajibola AdisaDOI: 10.21522/TIJPH.2013.10.01.Art001Disorders of Blood Gases, Electrolytes, Magnesium, Albumin and Calcium Metabolism in SARS-CoV-2-infected Patients
Abstract:
Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2)-infection is characterized by several malfunctions, including severe pulmonary disorders. Other metabolic consequences of SARS-CoV-2-infection have not been clearly defined. The present study assessed the status of blood gases, calcium metabolism, and electrolytes in SARS-CoV-2-infected individuals. One hundred and thirty-four newly diagnosed SARS-CoV-2-infected patients (age ranged 65-82years) attending Mullingar Regional Hospital, Republic of Ireland, participated in this study. They all had pulmonary disorders, pyrexia, body pains, etc. SARS-CoV-2 was confirmed in all patients using the RT-PCR molecular test method. The data of another 121 plasma samples of apparently normal, non-SARS-CoV-2-infected individuals taken before the emergence of Covid-19 served as controls. Levels of partial pressure of oxygen (pO2), saturated oxygen (SatO2), partial pressure of carbon dioxide (pCO2), and ionized calcium (Ca2+) were determined in all participants using the potentiometric method in RAPIDPOINT 500 Blood Gases System. Plasma vitamin-D was determined by immune enzymatically technique using DXi 800 Access Immunoassay System. Total calcium, phosphate, albumin, magnesium, and electrolytes were determined by the photometric method using Beckman Au680- Chemistry Analyzer. The results showed significantly (p<0.05) higher levels of pCO2 and HCO3- in COVID-19-patients compared to controls. Significantly(p<0.05) lower levels of pO2, SatO2, pH, K+, albumin, total-calcium, Ca2+, magnesium, and vitamin-D were observed in COVID-19 patients compared to controls. Corrected calcium, PO4-, Na+, and Cl- levels did not show significant (p>0.05) changes in the COVID-19-patients compared to controls. Abnormal blood gases, acidosis, hypomagnesaemia, hypoalbuminemia, hypovitaminosis D and calcium metabolic disorders could be features of COVID-19-disease.
Disorders of Blood Gases, Electrolytes, Magnesium, Albumin and Calcium Metabolism in SARS-CoV-2-infected Patients
References:
[1] Oudit GY, Kassiri Z, Jiang C, et al. 2009. Sars-Coronavirus modulation of myocardial ACE2 expression and inflammation in patients with SARS. Eur J Clin Invest. 39:618–25.
[2] Guo Y , Qing-Dong Cao, Zhong-Si Hong, Yuan-Yang Tan, Shou-Deng Chen, Hong-Jun Jin, Kai-Sen Tan, De-Yun Wang, Yan Yan 2020. The origin, transmission, and clinical therapies on coronavirus disease 2019 (Covid-19) outbreak - an update on the status. Mil Med Res. 13;7(1):11. doi: 10.1186/s40779-020-00240-0.
[3] Letko M, Marzi A, Munster V. 2020. Functional assessment of cell entry and receptor usage for SARS-CoV-2 and other lineage B beta coronaviruses. Nat Microbiol. 5:562–9.
[4] Boermeester MA, van Leeuwen PAM, Coyle SM, et al., 1995. Interleukin-1 receptor blockade in patients with sepsis syndrome: evidence that interleukin-1 contributes to the release of interleukin-6, elastase phospholipase A2, and to the activation of the complement, coagulation, and fibrinolytic systems, Arch Surg, vol. 130; 739-48.
[5] Santos RA, Ferreira AJ, Simoes ESA. 2008. Recent advances in the angiotensin converting enzyme 2-angiotensin (1-7)-Mas axis. Exp Physiol. 93 (5):519–27.
[6] Zhang R, Wu Y, Zhao M, Liu C, Zhou L, Shen S, Liao S, Yang K, Li Q, Wan H. 2009. Role of HIF-1alpha in the regulation of ACE and ACE2 expression in hypoxic human pulmonary artery smooth muscle cells. Am J Physiol Lung Cell Mol. Physiol. 297(4): L631–40.
[7] Aya Bassatne, Maya Basbous, Marlene Chakhtoura, Ola El Zein, Maya Rahme, Ghada El-Hajj Fuleihan 2021. The link between Covid-19 and VItamin D (VIVID): A systematic review and meta-analysis. Metabolism. 119:154753.
[8] Guan WJ, Ni ZY, Hu Y, et al. 2020. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 382: 1708–20.
[9] Klok FA, Kruip M, van der Meer NJM, et al. 2020. Incidence of thrombotic complications in critically ill ICU patients with Covid-19. Thromb Res. Published online April 10. Doi: 10.1016/j.thromres.2020.04.013.
[10] Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, et al. 2020 Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized with Covid-19 in the New York City Area. JAMA. https://doi.org/10.1001/jama.2020.6775 PMID: 32320003.
[11] Myers LC, Parodi SM, Escobar GJ, Liu VX 2020. Characteristics of Hospitalized Adults with Covid-19 in an Integrated Health Care System in California. JAMA.
https://doi.org/10.1001/jama.2020.7202 PMID: 32329797.
[12] Assandri R, Buscarini E, Canetta C, Scartabellati A, Viganò G, Montanelli A., 2020. Laboratory Biomarkers Predicting Covid-19 Severity in the Emergency Room. Arch Med Res. 51 (6):598-599. doi: 10.1016/j.arcmed.2020.05.011.
[13] Hinojosa-Velasco A, Bobadilla-Montes de Oca VP, García-Sosa LE, Mendoza-Durán JD, Pérez-Méndez MJ, Eduardo Dávila-González, Dolores G Ramírez-Hernández, Jaime García-Mena, Zárate-Segura P, Reyes-Ruiz JM, Bastida-González F., 2020 A Case Report of Newborn Infant with Severe Covid-19 in Mexico: Detection of SARS-CoV-2 in Human Breast Milk and Stool. Int J Infect Dis. 26; S1201-9712(20)30684-6. doi: 10.1016/j.ijid.2020.08.055. Online ahead of print.
[14] Singhal T. 2020. A Review of Coronavirus Disease-2019 (Covid-19). Indian J Pediatr. 87(4):281-286. doi: 10.1007/s12098-020-03263-6. Epub 2020.
[15] Petrilli CM, Jones SA, Yang J, Rajagopalan H, O’Donnell L, Chernyak Y, et al. 2020. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study. BMJ. 369: m1966. https://doi.org/10.1136/bmj.m1966 PMID: 32444366.
[16] Xie J, Covassin N, Fan Z, Singh P, Gao W, Li G, et al. 2020. Association Between Hypoxemia and Mortality in Patients with Covid-19. Mayo Clin Proc. 95: 1138–1147. https://doi.org/10.1016/j.mayocp. 2020.04.006 PMID: 32376101.
[17] Mejı´a F, Medina C, Cornejo E, Morello E, Va´squez S, Alave J, et al. 2020. Oxygen saturation as a predictor of mortality in hospitalized adult patients with Covid-19 in a public hospital in Lima, Peru. PLoS One 15(12): e0244171. https://doi.org/10.1371/journal.pone.0244171.
[18] Eltzschig HK, Carmeliet P. 2011. Hypoxia and inflammation. N Engl J Med. 364: 656–665. https://doi.org/10.1056/NEJMra0910283 PMID: 21323543.
[19] Persechini A., Moncrief N.D., Kretsinger R.H 1989. The EF-hand family of calcium-modulated proteins. Trends Neurosci. 12: 462–467 [PubMed] [Google Scholar].
[20] Yang W., Lee H.W., Hellinga H., Yang J.J. 2002. Structural analysis, identification, and design of calcium-binding sites in proteins. Proteins. 47:344–356 [PubMed] [Google Scholar].
[21] Xingjuan Chen, Ruiyuan Cao, Wu Zhong 2019. Host Calcium Channels and Pumps in Viral Infections. Cells. Dec 30;9(1):94. doi: 10.3390/cells9010094.
[22] Zhou Y., Yang W., Kirberger M., Lee H.W., Ayalasomayajula G., Yang J.J. 2006. Prediction of EF-hand calcium-binding proteins and analysis of bacterial EF-hand proteins. Proteins. 65:643–655 [PubMed] [Google Scholar].
[23] Xi Zhou; Dong Chen Lan Wang; Yuanyuan Zhao; Lai Wei; Zhishui Chen; Bo Yang 2020. Low serum calcium: a new, important indicator of COVID-19 patients from mild/moderate to severe/critical. Biosci Rep. 40 (12): BSR20202690. https://doi.org/10.1042/BSR20202690.
[24] Hanley B, Lucas SB, Youd E, Swift B, Osborn M. 2020. Autopsy in suspected COVID-19 cases. Journal of Clinical Pathology 73:239–242.
[25] Miyazawa, M. 2020. Immunopathogenesis of SARS-CoV-2-induced pneumonia: lessons from influenza virus infection. Inflamm Regener 40, 39. https://doi.org/10.1186/s41232-020-00148-1.
[26] Wu Z, McGoogan JM. 2020. Characteristics of and Important Lessons from the Coronavirus Disease 2019 (Covid-19) Outbreak in China: Summary of a Report of 72 314 Cases from the Chinese Center for Disease Control and Prevention. JAMA. https://doi.org/10.1001/jama.2020.2648 PMID: 32091533
[27] Andrew M Luks, Erik R Swenson 2020. Pulse Oximetry for Monitoring Patients with Covid-19 at Home. Potential Pitfalls and Practical Guidance. Ann Am Thorac Soc. 17(9):1040-1046 doi: 10.1513/AnnalsATS.202005-418FR.
[28] Zhang R, et al. 2009. Role of HIF-1α in the regulation ACE and ACE2 expression in hypoxic human pulmonary artery smooth muscle cells. Am. J. Physiol. Lung Cell. Mol. Physiol. 297: L631–L640 [PubMed] [Google Scholar].
[29] Jahani M, Dokaneheifard S, Mansouri K. 2020. Hypoxia: a key feature of Covid-19 launching activation of HIF-1 and cytokine storm. J. Inflamm. 17:33 [PMC free article] [PubMed] [Google Scholar].
[30] Ward PA, Fattahi F, Bosmann M. 2016. New insights into molecular mechanisms of immune complex-induced injury in the lung. Front. Immunol. 7:86 [PMC free article] [PubMed] [Google Scholar].
[31] Stenmark KR, Tuder RM, El Kasmi KC. 2015. Metabolic reprogramming and inflammation act in concert to control vascular remodeling in hypoxic pulmonary hypertension. J. Appl. Physiol. 119:1164–1172 [PMC free article] [PubMed] [Google Scholar].
[32] Pugliese SC, et al. 2017. A time- and compartment-specific activation of lung macrophages in hypoxic pulmonary hypertension. J. Immunol. 198:4802–4812 [PMC free article] [PubMed] [Google Scholar].
[33] Morne C Bezuidenhout, Owen J Wiese, Desiree Moodley, Elizna Maasdorp, Mogamat R Davids, Coenraad Fn Koegelenberg, Usha Lalla, Aye A Khine-Wamono, Annalise E Zemlin, Brian W Allwood. 2021. Correlating arterial blood gas, acid-base and blood pressure abnormalities with outcomes in Covid-19 intensive care patients. Ann Clin Biochem. 58(2):95-101. doi: 10.1177/0004563220972539 Epub 2020 Nov 20.
[34] Lippi, G, South, AM, Henry, BM. 2020. Electrolyte imbalances in patients with severe coronavirus disease 2019 (Covid-19). Ann Clin Biochem. 57:262-5.
https://doi.org/10.1177/0004563220922255 Search in Google Scholar
[35] Zhou Y, Teryl K. Frey, and Jenny J. Yang 2009. Viral calciomics: Interplays between Ca2+ and virus. Cell Calcium. 46(1): 1–17.
[36] Ruiz M.C., Cohen J., Michelangeli F 2000. Role of Ca2+ in the replication and pathogenesis of rotavirus and other viral infections. Cell Calcium. 28:137–149 [PubMed] [Google Scholar].
[37] Di Filippo, L, Formenti, AM, Rovere-Querini, P, Carlucci, M, Conte, C, Ciceri, F, et al. 2020. Hypocalcemia is highly prevalent and predicts hospitalization in patients with Covid-19. Endocrine. 68:475–8. https://doi.org/10.1007/s12020-020-02383-5 Search in Google Scholar.
[38] Antoniak S, Nigel Mackman., 2014. Multiple roles of the coagulation protease cascade during virus infection. Blood. 123 (17): 2605–2613. https://doi.org/10.1182/blood-2013-09-526277.
[39] Ryan MF 1991. The role of magnesium in clinical biochemistry: an overview. Ann Clin Biochem. 28:19–26 [PubMed] [Google Scholar].
[40] Swaminathan R 2003. Magnesium Metabolism and its Disorders. Clin Biochem Rev. 24(2): 47–66.
[41] Chuan-Feng Tang, Hong Ding, Rui-Qing Jiao, Xing-Xin Wu, and Ling-Dong Kong. 2020.. Possibility of magnesium supplementation for supportive treatment in patients with COVID-19. Eur J Pharmacol. 5; 886: 173546. doi: 10.1016/j.ejphar.2020.173546.
[42] Jacob S. Stevens, Andrew A. Moses, Thomas L. Nickolas, Syed Ali Husain, and Sumit Mohan. 2021, Increased Mortality Associated with Hypermagnesemia in Severe Covid-19 Illness. Kidney360. 2 (7) 1087-1094; Doi: https://doi.org/10.34067/KID.0002592021.
[43] Laure-Cranford AG, Krust MS, Riviere Y, Rey-Cuille MA, Montagnier L, Hovanessian AG. 1991. The cytopathic effect of HIV is associated with apoptosis. Virology. 185: 829-839.
[44] Rundk Hwaiz, Mohammed Merza, Badraldin Hamad, Shirin HamaSalih, Mustafa Mohammed, Harmand Hama 2021. Evaluation of hepatic enzymes activities in Covid-19 patients. Int Immunopharmacol. 2021; 97:107701. doi: 10.1016/j.intimp. 107701. Epub 2021 Apr 21.
[45] Yu, D., Du, Q., Yan, S. et al. 2021. Liver injury in Covid-19: clinical features and treatment management. Virol J 18, 121. https://doi.org/10.1186/s12985-021-01593-1.
[46] Xu Y, Yang H, Wang J, Li X, Xue C, Niu C, Liao P. 2021. Serum Albumin Levels are a Predictor of Covid-19 Patient Prognosis: Evidence from a Single Cohort in Chongqing, China. Int J Gen Med. 14:2785-2797 https://doi.org/10.2147/IJGM.S312521.
[47] Juyi Li , Meng Li, Shasha Zheng, Menglan Li, Minghua Zhang, Minxian Sun, Xiang Li, Aiping Deng , Yi Cai & Hongmei Zhang. Plasma albumin
levels predict risk for non-survivors in critically ill patients with Covid-19. Biomarkers in medicine vol. 14. 10; 826-837.Viewed PDF 1071 55 -
 Socio Demographic Profiles of Enuresis among Primary School ChildrenAuthor: Audu Hadiza MustaphaDOI: 10.21522/TIJPH.2013.10.01.Art002
Socio Demographic Profiles of Enuresis among Primary School ChildrenAuthor: Audu Hadiza MustaphaDOI: 10.21522/TIJPH.2013.10.01.Art002Socio Demographic Profiles of Enuresis among Primary School Children
Abstract:
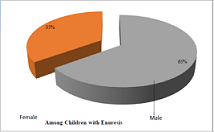
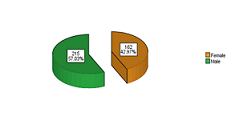
Enuresis is defined in many different ways, but the common thread to all involves a lack of bladder control after 5 years of age, an age when most children would be expected to have achieved bladder control. Nocturnal enuresis is best regarded as a condition with different etiologies. Many aetiological theories have been proposed, with the cause of nocturnal enuresis now regarded as heterogeneous. This was a cross-sectional, descriptive study of primary school children aged between 6-12 years. The study was conducted in Borno State in the northeastern part of Nigeria, West Africa. The sample size is 560, with 260(52.1%) males and 239 (47.9%) females. The ages of the respondents ranged from 6 to 12 years, with a mean age of 9.47 years and a Standard Deviation (SD) of ±1.85. Nine variables, namely age, gender, home environment, maternal education/occupation, paternal education/occupation, family size, and family history of enuresis among siblings at 95% CI were considered. The variables that have a significant relationship with enuresis when the chi 2 test was used were further subjected to logistic regression analysis. The children’s sex, age group, family history, fathers’ education, and occupation were found to have statistical significance in predicting bedwetting among children. Health educators and primary care health staff should obtain detailed history not to miss patients with enuresis, and parents should be informed about the psychological effects of Enuresis and to seek appropriate treatment for their children.
Socio Demographic Profiles of Enuresis among Primary School Children
References:
[1] Dhanidharka V. Primary nocturnal enuresis; where do we stand today? Indian Paediatrics. 2000; 37: 135-40.
[2] Gur E, Turhan P, Can G, Akkus S, Sever L, Guzelo S, et al. Enuresis; prevalence, Risk Factors, and Urinary pathology among school Children in Istanbul, Turkey; Paediatric International, Blackwell Publishers, Feb. 2004. 46(1):58-63(6).
[3] Akinyanju O, Agbato O, Ogunmekan AO, Okoye JU. Enuresis in sickle cell disease: prevalence studies. Journal of Tropical Paediatrics 1989; 35: 24-6.
[4] Winberg J, Bergstrom T, Jacobson B. Morbidity, age and sex distribution, recurrences, and renal scarring in symptomatic urinary tract infection in childhood. Kidney International (supplement) 1975; 4:101-6.
[5] American Psychiatric Association. Diagnosis and Statistical manual of Mental Diseases. (DSM-IV) Fourth Edition. Text Revision. Washington, DC.
[6] Lee SD, Sohn DW, Lee JZ, Park NC, Chung MK. An epidemiological study of Enuresis in Korean children. British Journal of Urology International, 2000; 85; (7):869-73.
[7] Yeung CK, Sreedhar B, Sihoe JY, Sit FY, Lau J. Differences in characteristics of nocturnal enuresis between children and adolescents, a critical appraisal from a large epidemiological study. British Journal of Urology International 2006; 97: 1069–73.
[8] Hagglof B, Andren O, Bergstrom E, Marklund L, Wendelius M. Self-esteem in children with nocturnal enuresis and urinary incontinence: improvement of self-esteem after treatment. European Urology 1998; 33 Supplement 3: 16–9.
[9] Mark SD, Frank JD. Nocturnal enuresis. British Journal of Urology. 1995:75:427-434.
[10] Butler R.J. Impact of nocturnal enuresis on children and young people. Scandinavian Journal of Urology and Nephrology. 2001:35(3):169-76.
[11] Enuresis-Psychology. Wikipedia.
http://psychology.wikia.com.
[12] Glicklich L. An historical account of enuresis. American Academy of Paediatrics. 1951; (8):859-870.
[13] Hazza I, Tarawneh H. Primary Nocturnal Enuresis among School children in Jordan. Saudi Journal of Kidney Diseases and Transplantation, 2002; 13: 478-480.
[14] Gurnus B, Vurgun N, Lekili M, Iscan A, Muezzinoglu T, Buyuksu C. Prevalence of nocturnal enuresis and accompanying factors in children aged 7-11 Years in Turkey. Acta Paediatric 1999; 88: (12): 1369-72. www.springerlink.com.
[15] Chang P, Chen WJ, Tsai WY, Chiu YN. An epidemiological study of nocturnal Enuresis in Taiwaneese children. British Journal of Urology International, 2001; 87:678-681.
[16] Bower WF, Moore KH, Shepherd RB, Adams RD. The epidemiology of childhood enuresis in Australia. British Journal of Urology. 1996; 78:602-6.
[17] Spee Van der Wekke J. Childhood Nocturnal Enuresis in the Netherlands. Urology international. 1998; 51: 1022-6.
[18] Chiozza MI, Bernardinelli L, Calone P. An Italian epidemiological multicentre study of nocturnal enuresis. British journal of urology. 1998; 81: 86-9.
[19] Rodriquez Fernandez LM, Marugan de Migulsanz JM, Lapena Lopez de Armentia S. Epidemiological study of nocturnal enuresis: analysis of associated factors. An esp. paediatrics. 1997; 46: 252-8.
[20] Hanafin S. Socio demographic factors associated with nocturnal enuresis. British journal of Nurses. 1998; 7; 403-8.
[21] Thiedke C. Nocturnal Enuresis. American Family Physician. 2003Apr; 67(7); 1509-10.
[22] Eapen V, Mabrouk A.M. Prevalence and correlates of nocturnal enuresis in United Arab Emirates. Saudi Medical Journal, 2003; Vol (24); 49-51.
[23] Butler RJ, Golding J, Northstone K. Nocturnal enuresis at 7.5 yrs old; prevalence and analysis of clinical signs. British Journal Urology International. 2005; 96:404-410.
[24] Dahl N. Arnell H, Hjalmas K, Jagervall M, Lackgren G, Stenberg A et, al. Primary nocturnal enuresis: linkage to chromosome 12q and evidence for genetic heterogeneity. American Journal of human Genetics. 1995;57.
[25] Eiberg H, Berendt I. Mohr, J. Assignment of dominant inherited nocturnal enuresis (ENUR1) to chromosome 13q. Nature & Genetics. 10: 354-356, 1995.
[26] Von Gontard A, Schaumburg H, Hollmann E, Eiberg H, Rittig S. The genetics of enuresis: A review. Journal of Urology, 2001; 166:2438-43.
[27] Arnell H, Hjalmas K. Jegard M, Lackgren G, Sternberg A, Bengtsson B, et, al. The genetics of primary nocturnal enuresis: Inheritance and suggestions of a second major gene on Chromosome 12q. Journal of medical genetics, 1997; 34: 360-315.
[28] Robert M, Averous M, Besset A, Carlander, B, Billiard M, Guiter J, Grasset D. Sleep polygraph studies using cystometry in twenty patients with enuresis. European Urology, 1993; 24(1), 97-102.
[29] Mayo ME, Burns MW. Urodynamic studies in children who wet. British Journal of Urology. 1990; 65:641-5.
[30] Marc C. Primary nocturnal enuresis: current concepts. American Family Physician 1999; 59: 1205-14, 1219-20.
[31] Rushton, H. Wetting, and functional voiding disorders. Urologic Clinics of North America, 1995 22(1), 75-93.
[32] Norgaard JP, Hansen JH, Nielsen JB, Rittig S, & Djurhuus JC. Nocturnal studies in enuretics, a Polygraphic study of sleep-EEG and bladder activity. Scandinavian Journal of Urology and Nephrology, 1989a; 125: 73-78.
[33] Wille S, Nocturnal enuresis: Sleep disturbance and behaviour patterns. Acta Paediatric, 1994; 83(7): 772-4.
[34] Mikkelson EJ, Rapoport JL. Enuresis: Psychopathology, sleep stage, and drug response. Urologic Clinics of North America, 1980; 7(2): 361-77.www.dryatnight.com.
[35] Kalo BB, Bella H. Enuresis: prevalence and associated factors among primary school children in Saudi Arabia. Acta Paediatric. 1996; 85:1217-22.
[36] Saddock BJ, Saddock VA. Kaplan & Sadock’s Synopsis of Psychiatry. 8th Edition. 1998; 1274-81. Lippincott Williams & Wilkins. New York.
[37] Brown M., Jacobs M, & Pelayo R. Adult obstructive sleep apnoea with secondary enuresis. Western Journal of Medicine, 1995; 163(5): 478-480.
[38] Weider DJ, Sateia MJ, West RP. Nocturnal enuresis in children with upper airway obstruction. Otolaryngology. Head Neck Surgery. 1991; 105: 427-32.
[39] Norgaard JP, Jonler M, Rittig S, & Djurhuus, J.C. A pharmacodynamic Study of Desmopressin in patients with nocturnal enuresis. Journal of Urology, 1995; 153: 1984-86.
[40] Norgaard JP, Rittig S, & Djurhuus JC. Nocturnal enuresis: An approach to treatment based on pathogenesis. Journal of Paediatrics, pub, Anthony Jannetti Inc, 1998 Dec; 18(4):259-73.
[41] Omigbodun OO. Psychosocial issues in child and adolescent psychiatric clinic population in Nigeria. Social Psychiatry, Psychiatric Epidemiology. 2004; Aug; 39(8):667-72.
[42] Werry JS, Cohrssen J. Enuresis an aetiological and therapeutic study. Journal of Paediatrics, 1965; 67: 423-31.bjsw.oxfordjounals.org/cgi.
[43] Schmitt BD, Nocturnal enuresis. Australian Paediatrics. Rev, 1997; 6, Jun; 18(6):183-91.
[44] Butler, R.J. Childhood nocturnal enuresis: Developing a conceptual framework. Clinical psychology. Review: 2004; 24(8): 909-31.
[45] Esperanca M, Gerrard, JW. Nocturnal enuresis: Comparison of the effect of Imipramine and dietary restriction on bladder capacity. Canadian Medical Association Journal, 1969 Dec; 13; 101(12): 65-68. www.pubmedcentralnih.gov.
[46] Djurhuus JC. Definitions of subtypes of enuresis. Scandinavian Journal of Urology Nephrology Supplement. 1999; 202:5-7.
[47] Haque M, Ellerstein NS, Grundy JH, Shelov SP, Weiss JC, McIntire MS, et al. Parental perceptions of enuresis: A collaborative study. American Journal of Disease In childhood, 1981; 35(9): 809-11.
[48] Osungbade KO, Oshiname FO. Prevalence and perception of nocturnal enuresis in children of a rural community in southwestern Nigeria. Tropical Doctor. 2003 Oct; 33(4): 234-6.
[49] Araoye OM. Sample size determination. Research methodology with statistics for health and social sciences. Ilorin: Nathadex Publishers; 2003. p 115-22.
[50] Kaufman J, Birmaher B, Brend I, Rao U, Ryan N. Kiddie-Sads, Present and lifetime version (KSADS-PL). Version 1.0 Pittsburgh: Department of psychiatry, University of Pittsburgh School of Medicine (UPMC) .1996. Retrieved from http://www.wpic.pitt.edu./ksads.
[51] Gureje O, Omigbodun OO, Gater R, Acha RA, Ikuwesan BA, Morris J. Psychiatric disorder in a paediatric primary care clinic. British Journal of Psychiatry. 1994; 165: 527-30.
[52] Azhir A, Frajzadegam Z, Adibi A, Hedayatpoor B, Fazel A, Divband A. An epidemiological Study of enuresis among primary school children in lsfahan, Iran. Published in Pub med. Saudi medical journal. 2006 Oct; 27(10); 1572-7.
[53] Etim U, Luka B. Girl Child Education Enrolment. World Bank Report, Oct; 2008.
Viewed PDF 1027 40 -
 Perception and Knowledge of Cancer and Cancer Screening among Staff of Military Hospital LagosAuthor: Abiola Ajoke Odeleye OladiranDOI: 10.21522/TIJPH.2013.10.01.Art003
Perception and Knowledge of Cancer and Cancer Screening among Staff of Military Hospital LagosAuthor: Abiola Ajoke Odeleye OladiranDOI: 10.21522/TIJPH.2013.10.01.Art003Perception and Knowledge of Cancer and Cancer Screening among Staff of Military Hospital Lagos
Abstract:
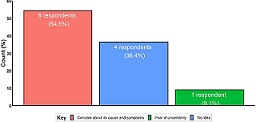
Perception and knowledge of cancer remain poor in developing countries. Problems associated with cancer incidence include late reporting due to fear, ignorance and financial constrains relating to cancer screening. This study sought to determine the perception and knowledge of cancer among health workers in Lagos. Method: A mixed-method study design comprising a qualitative study (Focus Group Discussions and In-depth Interview) and a quantitative study was employed to collect information from the staff of Military Hospital Lagos, southwest Nigeria. 30 Participants for the qualitative study were purposely recruited, while 200 participants for the quantitative study were selected using the proportional probability sampling technique after approval was received from the management of the hospital. Qualitative data was recorded using a recorder, transcribed verbatim, and analyzed thematically. Quantitative data was analyzed using SPSS 25.0 software at 95% CI, alpha set at 5%. Findings: The majority were women, 16(64.0%), with only 8(27%) of them under health insurance, with a minimum qualification of secondary school certificate, and mostly health attendants in the group discussion, while those in the interview group were all health professionals. The quantitative study revealed more males 106(53.0%), 73(36.5%) between 20-30 years, with 114(57.0%) married, over half, 122(61.0%) possessed a college degree, average income being >50-100 thousand naira monthly, 132(66.0%) respondents had health insurance. All cited fear and death sentence on hearing “cancer”, most had limited knowledge about cancer screening, only 5(2.5%) had any screening in the last 6 months.
Perception and Knowledge of Cancer and Cancer Screening among Staff of Military Hospital Lagos
References:
[1] Globocan 2012: Estimated Cancer Incidence, Mortality and Prevalence Worldwide in 2012 v1.0. IARC CancerBase No. 11. ISBN-13, 978-92-832-2447-1.
[2] Harcourt N, Ghebre RG, Whembolua GL, Zhang Y, Osman SW, & Okuyemi KS. (2014). Factors associated with breast and cervical cancer screening behavior among African immigrant women in Minnesota. Journal of immigrant and minority health, 16(3), 450-456.
[3] Tapera O, Nyakabau A, Simango N, Guzha B, Jombo-Nyakuwa S, Takawira E, Mapanga A, Makosa D, & Madzima B. (2021). Gaps and opportunities for cervical cancer prevention, diagnosis, treatment, and care: evidence from midterm review of the Zimbabwe cervical Cancer prevention and control strategy (2016–2020). BMC Public Health. 21. 10.1186/s12889-021-11532-y.
[4] Silvera, S. A. N., Bandera, E. V., Jones, B. A., Kaplan, A. M., & Demisse, K. (2020). Knowledge of, and beliefs about, access to screening facilities and cervical cancer screening behaviors among low-income women in New Jersey. Cancer Causes & Control, 31(1), 43-49.
[5] Logan L. & Mcilfatrick S. (2011). Exploring women's knowledge, experiences, and perceptions of cervical cancer screening in an area of social deprivation. European Journal of Cancer Care20, 720–727. doi.org/10.1111/j.1365-2354.2011.01254. x.
[6] Sheeran P, Harris PR, Epton T. (2014). Does a heightening risk appraisal change people’s intentions and behavior? A meta-analysis of experimental studies. Psychological bulletin, 140(2), 511–543. https://doi.org/10.1037/a0033065.
[7] Adetona AE, Osungbade KO, Akinyemi OO, Obembe TA (2021). Uptake of Breast Screening Among Female Staff at A Tertiary Health Institution in South-West Nigeria. Journal of Preventive Medicine and Care - 3(2):17-30. Doi 10.14302/issn.2474-3585.jpmc-20-3557.
[8] Keah MM, Kombe Y, & Ngure K. (2020). Factors Influencing the Uptake of Cervical Cancer Screening among Female Doctors and Nurses in Kenyatta National Hospital. Journal of Cancer and Tumor International, 10(3), 31-38. https://doi.org/10.9734/jcti/2020/v10i330131.
[9] Odenusi AO, Oladoyin VO, Asuzu MC (2020). Uptake of cervical cancer screening services and its determinants between health and non-health workers in Ibadan, south-Western Nigeria. Afr. J. Med. Med. Sci. (4) 49, 573-5.
[10] Bukowska-Durawa A, & Luszczynska A. (2014). Cervical cancer screening and psychosocial barriers perceived by patients. A systematic review. Contemporary oncology (Poznan, Poland), 18(3), 153–159. https://doi.org/10.5114/wo.2014.43158.
[11] Bradley DT, Treanor C, McMullan C, et al. Reasons for non-participation in the Northern Ireland Bowel Cancer Screening Programme: a qualitative study. BMJ Open 2015;5: e008266. doi:10.1136/ bmjopen-2015-008266.
[12] Marlow LAV, Waller J, & Wardle J. (2015). Barriers to cervical cancer screening among ethnic minority women: a qualitative study. The journal of family planning and reproductive health care, 41(4), 248–254. https://doi.org/10.1136/jfprhc-2014-101082.
[13] Marlow LAV, Wardle J & Waller J. (2015). Understanding cervical screening non-attendance among ethnic minority women in England. Br J Cancer 2015;113(5):833–839. Doi:10.1038/bjc.2015.248.
[14] Chorley AJ, Marlow LAV, Forster AS, Haddrell JB & Waller J. (2016). Experiences of cervical screening and barriers to participation in the context of an organized program: a systematic review and thematic synthesis. Psycho-Oncology 26: 161–172. Doi: 10.1002/pon.4126.
[15] Wright KO, Faseru B, Kuyinu YA, Faduyile FA. (2011). Awareness and uptake of the Pap smear among market women in Lagos, Nigeria. J Public Health Afr; 2(e14): 58-62. https://doi.org/10.4081/jphia.2011.e14.
[16] Vrinten C, McGregor LM, Heinrich M, von Wagner C, Waller J, Wardle J, Black GB. (2017). What do people fear about cancer? A systematic review and meta-synthesis of cancer fears in the general population. Psycho-oncology 26(8):1070-1079. doi: 10.1002/pon.4287.
[17] Vrinten C, Waller J, von Wagner C, Wardle J. (2015). Cancer fear: facilitator and deterrent to participation in colorectal cancer screening. Cancer Epidemiol Biomarkers Prev; 24(2):400-5. doi: 10.1158/1055-9965.EPI-14-0967.
[18] Licqurish S, Phillipson L, Chiang P, Walker J, Walter F & Emery J. (2017). Cancer beliefs in ethnic minority populations: a review and meta-synthesis of qualitative studies. European journal of cancer care, 26(1), 10.1111/ecc.12556. https://doi.org/10.1111/ecc.12556.
[19] Dim CC, Ekwe E, Madubuko T, Dim NR, Ezegwui HU. (2009). Improved awareness of Pap smear may not affect its use in Nigeria: a case study of female medical practitioners in Enugu, southeastern Nigeria. Trans R Soc Trop Med Hyg. 103(8): 852-854.
[20] Dim C C. (2012). Towards improving cervical cancer screening in Nigeria: A review of the basics of cervical neoplasm and cytology. Niger J Clin Pract 15:247-52.
https://www.njcponline.com/text.asp?2012/15/3/247/100615.
[21] Dim CC, Nwagha UI, Ezegwui HU & Dim NR. (2009). The need to incorporate routine cervical cancer counseling and screening in the management of women at the outpatient clinics in Nigeria, Journal of Obstetrics and Gynaecology; 29:8, 754-756, Doi: 10.3109/01443610903225323.
[22] Jensen LA, Allen MN. (1996). Meta-synthesis of qualitative findings. Qual Health Res;6 (4):553–560. Doi:10.1177/10497323960060 040.
[23] Dharni N, Armstrong D, Chung-Faye G, & Wright AJ (2017). Factors influencing participation in colorectal cancer screening - a qualitative study in an ethnic and socio-economically diverse inner-city population. Health expectations: an international journal of public participation in health care and health policy, 20(4), 608–617. https://doi.org/10.1111/hex.12489.
[24] Hewitson P, Ward AM, Heneghan C, Halloran SP & Mant D. (2011). Primary care endorsement letter and a patient leaflet to improve participation in colorectal cancer screening: results of a factorial randomized trial. British journal of cancer, 105(4), 475–480. https://doi.org/10.1038/bjc.2011.255.
Viewed PDF 1046 39 -
 Quality of Tuberculosis Services in Lusaka, Zambia; Patients’ PerspectiveAuthor: Theresa Chansa Chilufya SikateyoDOI: 10.21522/TIJPH.2013.10.01.Art004
Quality of Tuberculosis Services in Lusaka, Zambia; Patients’ PerspectiveAuthor: Theresa Chansa Chilufya SikateyoDOI: 10.21522/TIJPH.2013.10.01.Art004Quality of Tuberculosis Services in Lusaka, Zambia; Patients’ Perspective
Abstract:
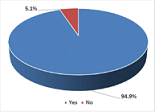
Zambia is among the 30 countries with high Tuberculosis (TB) burden, with an estimated 455 new cases per 100,000 people annually. Zambia and its partners are committed to accelerating the response to end TB through the provision of good quality of TB services, among other things. Despite the coordinated effort in addressing TB, little is documented about patients’ perceptions regarding the quality of TB services in Zambia. This study was conducted to assess the quality of TB services from the patient’s perspective. A facility-based cross-sectional study that utilized both quantitative and qualitative data collection. The study sample was 352 randomly selected patients on TB treatment and 58 purposefully selected TB treatment support persons. The patient’s perceived quality of care was measured by their perceived satisfaction of TB services in relation to accessibility of the TB clinic, timeliness of service provision, availability of qualified service providers, access to health education, the perceived attitude of service providers, and availability of drugs. Results revealed a high level of perceived good quality of TB services. The TB patients were more satisfied with the attitude of service providers, followed by the timeliness of service provision. Overall, 94.9% of the TB patients reported being satisfied with TB services. There is a high perception of good quality of TB services among the patients. Despite the high level of good quality, the study revealed limitations with regard to drug dispensation and the availability of qualified staff.
Quality of Tuberculosis Services in Lusaka, Zambia; Patients’ Perspective
References:
[1] Khatri, U. Davis, N., 2020. Quality of Tuberculosis Services Assessment in Ethiopia, Report. Measure Evaluation.
[2] Global tuberculosis report 2020. Geneva: World Health Organization; 2020. Licence: CC BY-NC-SA 3.0 IGO. Moh (2015), The National Health Strategic Plan (NHSP) 2017-2021, Lusaka. Zambia.
[3] De Schacht, C., Mutaquiha, C., Faria, F., Castro, G., Manaca, N., Manhiça, I., and Cowan, J., 2019. Barriers to access and adherence to tuberculosis services, as perceived by patients: A qualitative study in Mozambique. PloS one, 14(7), p.e0219470.
[4] Colvin, C., De Silva, G., Garfin, C., Alva, S., Cloutier, S., Gaviola, D., Oyediran, K., Rodrigo, T. and Chauffour, J., 2019. Quality of TB services assessment: The unique contribution of patient and provider perspectives in identifying and addressing gaps in the quality of TB services. Journal of clinical tuberculosis and other mycobacterial diseases, 17, p.100117.
[5] NAC. 2019. Global Fund 2020-2022 Allocation Letter. Access online at: http://www.nac.org.zm/ccmzambia/wp-content/uploads/2020/04/Zambia-2020-2022-allocation-letter-signed.pdf on15th December 2020.
[6] Bulage, L., Sekandi, J., Kigenyi, O. and Mupere, E., 2014. The quality of tuberculosis services in health care centres in a rural district in Uganda: the providers’ and clients’ perspective. Tuberculosis research and treatment, 2014.
[7] MoH (2015), Health Management Information System (HMIS), Lusaka. Zambia.
[8] MoH, (2018) The National Tuberculosis and leprosy Programme: TUBERCULOSIS Mannual, Lusaka Zambia. retrieved from https://www.who.int/hiv/pub/guidelines/zambia_Tuberculosis.pdf on 21st May 2019.
[9] Bhatnagar, H. (2019). User-experience and patient satisfaction with quality of Tuberculosis care in India: A mixed methods literature review. Journal of Clinical https://doi.org/10/1016/j.jctube2019.100127 accessed online at https://www.sciencedirect.com/science/article/pii/S2405579419300713 on 15th September 2020.
[10] Moore, Lynne PhD; Lavoie, André PhD; Bourgeois, Gilles MD; Lapointe, Jean MD Donabedian’s structure-process-outcome quality of care model, Journal of Trauma and Acute Care Surgery: June 2015 - Volume 78 - Issue 6 - p 1168-1175 doi: 10.1097/TA.0000000000000663.
[11] WHO (2016) Health workforce requirements for universal health coverage and the sustainable development goals Human Resources for Health Observer Series No 17 accessed on https://apps.who.int/iris/bitstream/handle/10665/250330/9789241511407-eng.pdf;sequence=1 on 20th October 2020.
[12] Dansereau, E., Masiye, F., Gakidou, E., Masters, S.H., Burstein, R. and Kumar, S., 2015. Patient satisfaction and perceived quality of care: evidence from a cross-sectional national exit survey of HIV and non-HIV service users in Zambia. BMJ Open, 5(12).
[13] Adhikary G, Shawon MSR, Ali MW, Shamsuzzaman M, Ahmed S, Shackelford KA, et al. (2018) Factors influencing patients’ satisfaction at different levels of health facilities in Bangladesh: Results from patient exit interviews. PLoS ONE 13(5): e0196643. Accessed online at https://doi.org/10.1371/journal.pone.0196643 on 15th September 2020.
[14] Charlotte, C. et al, (2019) Quality of TB services assessment: The Unique contribution of patient and provider perspectives in identifying and addressing gaps in the quality of TB services. Journal of Clinical Tuberculosis and other mycobacterial diseases, Vol 17, December 2019, 100117 https://doi.org/10.1016/j.jctube.2019.100117.
[15] Costa-Sánchez, C. and Míguez-González, M.I., 2018. use of social media for health education and corporate communication of hospitals. El profesional de la información, 27(5).
[16] Arsenault, C. Roder-DeWan, S. and Kruk M.E Measuring and improving the quality of Tuberculosis care a framework and implications from the Lancet Global Health commission Journal of Clinical
Tuberculosis and other Mycobacterial diseases vol. 16, August 2019 100112 https://doi.org/10.1016/j/jctube.2019.100112 https://www.sciencedirect.com/science/article/pii/S2405579419300531#bib0001.[17] WHO, (2015): The End Tuberculosis strategy, Geneva, Switzerland. Retrieved from https://www.who.int/Tuberculosis/strategy/end-Tuberculosis/en/ on 21st May 2019.
[18] Mergya Eticha, Belay & Atomsa, Alemayehu &, Birtukantsehaineh & Berheto, Tezera. (2014). Patients’ perspectives of the quality of tuberculosis treatment services in South Ethiopia. 3. 48-55. 10.11648/j.ajns.20140304.12.
[19] Aspler A, Menzies D, Oxlade O, Banda J, Mwenge L, Godfrey-Faussett P, Ayles H. Cost of tuberculosis diagnosis and treatment from the patient perspective in Lusaka, Zambia. Int J Tuberc Lung Dis. 2008 Aug; 12(8):928-35. PMID: 18647453.
[20] Vaida Bankauskaite, Osmo Saarelma, why are people dissatisfied with medical care services in Lithuania? A qualitative study using responses to open-ended questions, International Journal for Quality in Health Care, Volume 15, Issue 1, February 2003, Pages 23–029,
https://doi.org/10.1093/intqhc/15.1.23 accessed online at
https://academic.oup.com/intqhc/article/15/1/23/1797067 on 15th September 2020.
Viewed PDF 1094 41 -
 Promoting Healthy Aging through Lifestyle Changes: The Plausibility and Evidence-based RecommendationsAuthor: Abiodun Bamidele AdelowoDOI: 10.21522/TIJPH.2013.10.01.Art005
Promoting Healthy Aging through Lifestyle Changes: The Plausibility and Evidence-based RecommendationsAuthor: Abiodun Bamidele AdelowoDOI: 10.21522/TIJPH.2013.10.01.Art005Promoting Healthy Aging through Lifestyle Changes: The Plausibility and Evidence-based Recommendations
Abstract:
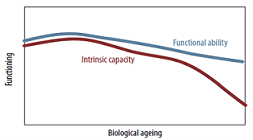
Through the advances in public health, most humans on earth are now assured to live to at least 60 years, regardless of their geographical location and socio-economic status. Between 2015 and 2050, the proportion of the world’s population 60 years and above will be expected to increase from 900 million to 2.1 billion, while the average global life expectancy will be expected to increase by additional 10 years. Experts have ascribed this development as the most significant social transformation of the 21st century. However, although the world may have successfully learned how to live longer, it has not necessarily learned how to live healthier. In most situations, old age is associated with significant loss of physical and mental functionalities, increased risk of developing multiple diseases (including COVID-19), and reduced quality of life. This association has been described as the most important global public health challenge of the 21st century. The objective of this article is to investigate the scientific plausibility of slowing down the aging process and to identify evidence-based measures of achieving healthy aging. A review of related online free-full articles written in the English language published from 2000 to 2021 was done. It was noticed that the pace and quality of aging can be significantly influenced by controlling the lifestyle determinants of aging. Although the science of healthy aging is still evolving, there is enough evidence for healthcare professionals to recommend evidence-based strategies of achieving healthy aging to the public and to policymakers.
Promoting Healthy Aging through Lifestyle Changes: The Plausibility and Evidence-based Recommendations
References:
[1] Lange J., and Grossman S., 2021, Chapter Three: Theories of Aging. Jones &Bartlett Learning, 2021. Date of access: 15/2/2021. https://samples.jbpub.com/9781284104479/Chapter_3.pdf.
[2] Cabrera A.J.R., 2015, Theories of Human Aging of Molecules to Society. MOJ Immunol, 2(2), 00041. https://DOI:10.15406/moji.2015.02.00041.
[3] Garrido A, Cruces J, Ceprián N, Vara E, and de la Fuente M, 2019, Oxidative-Inflammatory Stress in Immune Cells from Adult Mice with Premature Aging. Int. J. Mol. Sci., 20, 769. https://doi:10.3390/ijms20030769.
[4] Pathath A.W., 2017, Theories of Aging. International Journal of Indian Psychology, 4 (3), 15 – 22. https://DOI:10.25215/0403.142.
[5] Vin˜ J., Borra´ C., and Miquel J., 2007, Theories of Ageing. IUBMB Life, 59, 249–254.
[6] Miller J., 2011, The Fountain of Youth: The Quest for Biological Immortality, Date of access: 7/2/2021. http://www.slideshare.net/Justin2226/human-longevity-by-justin-miller.
[7] Belskya D.W, Caspic A., Houtsc R., Cohena H.J., Corcorane D.L, Danesef A., et al., 2015, Quantification of biological aging in young adults. PNAS, 4104 – 4110. www.pnas.org/cgi/doi/10.1073/pnas.1506264112.
[8] Jia L., Zhang W., and Chen X., 2017. Common methods of biological age estimation. Clinical Interventions in Aging, 12, 759–772.
[9] European Commission (2020). European Study to Establish Biomarkers of Human Ageing: Calculating one’s biological age. Date of access: 6/5/2021. https://cordis.europa.eu/article/id/90427-calculating-ones-biological-age.
[10] Jiang S., and Guo Y., 2020, Epigenetic Clock: DNA Methylation in Aging. Stem Cells International, 2020, 1 – 9. https://doi.org/10.1155/2020/1047896.
[11] World Health Organization, 2011, Global Health and Aging, Date of access: 2/4/2021. https://www.who.int/ageing/publications/global_health.pdf.
[12] Barratt J., 2017. We are living longer than ever. But are we living better? Date of access: 4/6/2021. https://www.statnews.com/2017/02/14/living-longer-living-better-aging/.
[13] United Nations, 2017, World Population Ageing, Date of access: 7/7/2021. https://www.un.org/en/development/desa/population/publications/pdf/ageing/WPA2017_Highlights.pdf.
[14] World Health Organization, 2018, Ageing and health, Date of access: 17/2/2021. https://www.who.int/news-room/fact-sheets/detail/ageing-and-health.
[15] Tabish S.A., 2012, Population aging is a global phenomenon, Date of access: 17/2/21. www.researchgate.net/publication/262915215_Population_aging_is_a_global_phenomenon.
[16] Khunti K., Singh A.K., Pareek M., and Hanif W., 2020, Is ethnicity linked to incidence or outcomes of covid-19? Preliminary signals must be explored urgently, BMJ, 369: 1 – 2. DOI: 10.1136/bmj.m1548.
[17] Beard J.R., Biggs S., Bloom D.E., Fried L.P., Hogan P., Kalache A., et al., 2012, Global Population Ageing: Peril or Promise, Geneva: World Economic Forum. Date of access: 15/5/2021. https://demographic-challenge.com/files/downloads/6c59e8722eec82f7ffa0f1158d0f4e59/ageingbook_010612.pdf.
[18] World Health Organization, 2017, Global strategy and action plan on ageing and health, Date of access: 2/4/2021. https://www.who.int/ageing/WHO-GSAP-2017.pdf.
[19] World Health Organization, 2017, WHO Clinical Consortium on Healthy Ageing. Topic focus: frailty and intrinsic capacity. Report of consortium meeting, Date of access: 3/6/2021. https://apps.who.int/iris/bitstream/handle/10665/272437/WHO-FWC-ALC-17.2-eng.pdf.
[20] World Health Organization, 2015, World report on ageing and health, Date of access: 1/3/2021.http://apps.who.int/iris/bitstream/handle/10665/186463/9789240694811_eng.pdf;jsessionid=FD0D4724D6073BBFC1CA52618828A755?sequence=1.
[21] Franklin B.A, and Cushman M., 2011, Recent Advances in Preventive Cardiology and Lifestyle Medicine. Circulation, 123, 2274 – 2283.
[22] Poulain M., Herm A., and Pes G., 2013, The Blue Zones: areas of exceptional longevity around the world. Vienna Yearbook of Population Research, 11, 87–108.
[23] Buettner D., and Skemp S., 2016, Blue Zones: Lessons from the World’s Longest Lived. American Journal of Lifestyle Medicine, 318 – 321. https://DOI:10.1177/1559827616637066.
[24] Kadey M., 2020, Health Lessons from the World’s Blue Zones, Date of access: 20/10/2021. https://www.ideafit.com/personal-training/health-lessons-from-the-worlds-blue-zones/.
[25] Kim S., and Jazwinski S.M., 2015, Quantitative measures of healthy aging and biological age. Healthy Aging Res., 4, 1 – 25. http://doi:10.12715/har.2015.4.26.
[26] Batchelor F., Haralambous B., Lin X., Joosten M., Williams S., Malta S., et al., & 2016, Healthy ageing literature review: Final report to the Department of Health and Human Services. State of Victoria, Department of Health and Human Services, Date of access; 24/7/2021. https://www2.health.vic.gov.au/ageing-and-aged-care.
[27] Rudnickaa E., Napierałab P., Podfigurnab A., Męczekalskib B., Smolarczyka R., and Grymowicza M., 2020, The World Health Organization (WHO) approach to healthy ageing. Maturitas 139 (2020), 6–11.
[28] Whitbourne S.K., 2012, What’s Your True Age? You may be a lot younger than you think, CommonLit, 2014-2021, Date pf access: 13/7/2021. https://www.commonlit.org/texts/what-s-your-true-age.
[29] Jarreau P., 2019, How Old Are You, really? Meet Your Biological Age. Life Omic Health, 2020, Date of access: 18/5/2021. https://lifeapps.io/brain/how-old-are-you-really-meet-your-biological-age/.
[30] Elysium, 2020, What Is Your Biological Age? And Why Does It Matter? Date of access: 8/7/2021. https://www.elysiumhealth.com/en-us/science-101/biological-age.
[31] Glanz K., Rimer B.K., & Viswanath K., 2008, Health Behavior and Health Education: Theory, Research, and Practice, 4th Edition, Date of access: 1/12/2021. https://iums.ac.ir/files/hshe-soh/files/beeduhe_0787996149(1).pdf.
[32] Terranova J., 2019, What’s Your Actual Age? Chronological vs. Biological Age, Thorne, 2019, Date of access: 4/9/2021. https://www.thorne.com/take-5-daily/article/what-s-your-actual-age-chronological-vs-biological-age.
[33] Lobachevsky University, 2020, Scientists have identified the role of chronic inflammation as the cause of accelerated aging, American Association for the Advancement of Science (AAAS), 2021, Date of access: 8/8/2021. https://eurekalert.org/pub_releases/2020-01/lu-shi012920.php.
[34] Watson K., 2019, Everything You Need to Know About Premature Aging, Date of access: 24/11/2020. https://www.healthline.com/health/beauty-skin-care/premature-aging#tips-for-prevention.
[35] Basaraba S., 2020, How Lifestyle and Habits Affect Biological Aging, Date of access: 21/8/2021. https://www.verywellhealth.com/what-is-biological-age-2223375.
[36] Shields A., 2020, How to Calculate Your Biological Age, Date of access: 15/9/2021. https://dralexisshields.com/biological-age.
[37] Raman R., 2016. How to Safely Get Vitamin D From Sunlight. Date of access: 14/1/2022. https://www.healthline.com/nutrition/vitamin-d-from-sun.
Viewed PDF 1335 35 -
 Conceptual Framework for Epidemics and Vaccination DilemmaAuthor: Odis Adaora IsabellaDOI: 10.21522/TIJPH.2013.10.01.Art006
Conceptual Framework for Epidemics and Vaccination DilemmaAuthor: Odis Adaora IsabellaDOI: 10.21522/TIJPH.2013.10.01.Art006Conceptual Framework for Epidemics and Vaccination Dilemma
Abstract:
Outbreaks of diseases have positive and negative effects on humans. An example of the positive epidemic dilemma was seen in the 2020 lockdown across the world where families spent quality time together and couples seeking for the fruit of the womb conceived after many years, working from home was introduced, Lagosians working from home reduced stress from traffic, remote jobs were increased, online zoom, Webex webinars, online surveys, seminars, conference, Viva Voca, graduation and growth for online business and banking. Apps were available for the masses to access health online, known as Telemedicine. While the negative epidemics dilemma includes loss of jobs, slow down in economy across the world, poverty, drug abuse, self–medication, Anti-microbial resistance, child abuse, rape, divorce, shadow pandemic, death, and no access to education for those that do not have internet facilities to learn/study/school online. Vaccine’s hesitancy is an established dilemma that contributes to significant health challenges which cause a high rate of infant sickness and death. There are certain factors like cultural, social, demographic, and psychosocial factors that contribute to the vaccine dilemma. This conceptual framework illustrates the factors that drive epidemics and vaccine dilemma, which can be vaccination acceptance and hesitancy. For an intervention to be implemented successfully, we need to understand the triggers of epidemics and vaccination dilemma. The socio-demographic characteristics like age, sex, marital status, level of education, choice of hospital, employment status, level of income, health insurance status and the number of children is significantly associated with vaccine uptake among parents.
Conceptual Framework for Epidemics and Vaccination Dilemma
References:
[1] Osibogun (2014) “Emerging and Remerging diseases – Stopping the spread”: Lecture delivered at the Health Week ceremony of the University of Lagos.
[2] Vaccinate your family, 2019, “Vaccines are cost savings”, https://www.vaccinateyourfamily.org/why-vaccinate/vaccine-benefits/costs-of-disease-outbreaks/.
[3] De Figueiredo A et al. (2016) “Forecasted trends in vaccination coverage and correlations with socioeconomic factors: A global time-series analysis over 30 years”. Lancet Glob. Health, Vol 4, no. 10, pp., 726–735. pmid:27569362 View Article PubMed/NCBI Google Scholar.
[4] Wessel L., (2017,) “Vaccine myths”. Science 2017; 356(6336):368–372. pmid:28450594 View Article PubMed/NCBI Google Scholar.
[5] Larson HJ, Jarrett C, Eckersberger E, Smith DM, Paterson P., (2014), “Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: A systematic review of published literature”, 2007-2012. Vaccine 2014; 32(19):2150–2159. PMID: 24598724 View Article PubMed/NCBI Google Scholar.
[6] Black S, Rappuoli R., (2010), “A crisis of public confidence in vaccines”. Sci. Transl. Med. 2010; Vol. 2, no. 61, pp., 61. PMID: 21148125 View Article PubMed/NCBI Google Scholar.
[7] Larson HJ., (2016) “Vaccine trust and the limits of information”. Science Vol. 353, no. 6305, pp., 1207–1208. PMID: 27634512 View Article PubMed/NCBI Google Scholar.
[8] Holme P, Saramäki J. (2012) “Temporal networks”. Phys Rep; no. 519, pp., 97–125.
[9] Jansen VAA et al., (2003), “Measles outbreaks in a population with declining vaccine uptake”. Science Vol. 301, no. 5634, pp., 804. PMID: 12907792 View Article PubMed/NCBI Google Scholar.
[10] Feh E, Fischbacher U., (2003), “The nature of human altruism”. Nature Vol., 2003; no. 425, pp., 785–791. View Article Google Scholar.
[11] Davis L., (1977), “Prisoners, paradox, and rationality”. Am PhilosQ,Vol. 14, no. 4, pp., 319–327.View Article Google Scholar.
[12] Sharma A, Menon SN, Sasidevan V, Sinha S (2019) “Epidemic prevalence information on social networks can mediate emergent collective outcomes in voluntary vaccine schemes”. PLoSComputBiolVol. 15, no. 5, e1006977. https://doi.org/10.1371/journal.pcbi.1006977.
[13] Verelst F, Willem L, Beutels P., (2016), “Behavioural change models for infectious diseasetransmission: a systematic review (2010-2015)”. J. R. Soc. Interface 2016; 13(125):20160820. pmid: 28003528 View Article PubMed/NCBI Google Scholar.
[14] Marien González Lorenzo A, Alessandra Piatti C, Liliana Coppola C, Maria Gramegna C, Vittorio Demicheli D, Alessia Melegaro E, Marcello Tirani A, Elena Parmelli F.G, Francesco Auxilia A Lorenzo Moja A.B, the Vaccine Decision Group, 2015, Conceptual frameworks and key dimensions to support coverage decisions for vaccines, Volume 33, Issue 9, 25 February 2015, Pages 1206-1217, https://doi.org/10.1016/j.vaccine.2014.12.020.
[15] Saint-Victor DS, Omer SB., (2013), “Vaccine refusal and the endgame: Walking the last mile first”. Phil. Trans. R. Soc. B 2013; 368(1623):20120148. PMID: 23798696 View Article PubMed/NCBI Google Scholar.
[16] Bauch CT, Galvani AP, Earn DJD., (2003) “Group interest versus self-interest in smallpox vaccination policy”. Proc. Natl. Acad. Sci. USA Vol. 100, no.18, pp., 564–567. View Article Google Scholar.
[17] Bauch CT, Earn DJD., (2004) “Vaccination and the theory of games”. Proc. Natl. Acad. Sci. USA, Vol 101, no. 36, pp., 391–394. View Article Google Scholar.
[18] Zhang H-F, Wu Z-X, Tang M, La Y-C., (2014), “Effects of behavioral response and vaccination policy on epidemic spreading—an approach based on evolutionary-game dynamics”. Sci. Rep. 2014; 4:5666. pmid: 25011424 View Article PubMed/NCBI Google Scholar.
[19] Verelst F, Willem L, Kessels R, Beutels P., (2018), “Individual decisions to vaccinate one’s child or oneself: A discrete choice experiment rejecting free-riding motives”. Soc. Sci. Med. Vol. 2018; no. 207, pp., 106–116. pmid: 29738898.
[20] Jolley D, Douglas KM., (2014), “The effects of anti-vaccine conspiracy theories on vaccination intentions”. PLoS ONE, Vol. 9, no. 2, pp., 89 - 177. pmid:24586574 View Article PubMed/NCBI Google Scholar.
[21] Larson HJ, Ghinai I., (2011), “Lessons from polio eradication”. Nature; no. 473, pp., 446–447. pmid:21614056 View Article PubMed/NCBI Google Scholar.
[22] Eubank S, et al., (2004), “Modelling disease outbreaks in realistic urban social networks”. Nature, Vol. 429, no. 6988, pp., 180–184. pmid:15141212 View Article PubMed/NCBI Google Scholar.
[23] Moinet A, Pastor-Satorras R, Barrat Alain., (2018), “Effect of risk perception on epidemic spreading in temporal networks”. Phy. Rev. E 2018; 97(1):012313. View Article Google Scholar.
[24] Rizzo A, Frasca M, Porfiri M., (2014), “Effect of individual behavior on epidemic spreading in activity-driven networks”. Phy. Rev. E Vol. 90, no. 4, 042801. View Article Google Scholar.
[25] Massaro E, Bagnoli F., (2014), “Epidemic spreading and risk perception in multiplex networks: A self-organized percolation method”. Phy. Rev. E 2014; Vol. 90, no. 5, 052817. View Article Google Scholar.
[26] Oku, A., Oyo-Ita, A., Glenton, C. et al. Factors affecting the implementation of childhood vaccination communication strategies in Nigeria: a qualitative study. BMC Public Health 17, 200 (2017). https://doi.org/10.1186/s12889-017-4020-6.
[27] Harapan H, Wagner AL, Yufika A, Winardi W, Anwar S, Gan AK, et al. (2020) Acceptance of a COVID-19 vaccine in Southeast Asia: a cross-sectional study in Indonesia. Front Public Health. 8:381. DOI: 10.3389/fpubh.2020.00381PubMed Abstract, CrossRef Full Text, Google Scholar.
[28] Wang J, Jing R, Lai X, Zhang H, Lyu Y, Knoll MD, et al. (2020) Acceptance of COVID-19 vaccination during the COVID-19 pandemic in China. Vaccines. 8:482. DOI: 10.3390/vaccines8030482 PubMed Abstract, CrossRef Full Text, Google Scholar.
[29] Bell S, Clarke R, Mounier-Jack S, Walker JL, Paterson P. (2020) Parents’ and guardians’ views on the acceptability of a future COVID-19 vaccine: a multi-methods study in England. Vaccine. 38:7789–98. doi: 10.1016/j.vaccine.2020.10.027 PubMed Abstract, CrossRef Full Text, Google Scholar.
[30] Reiter PL, Pennell ML, Katz ML. (2020) Acceptability of a COVID-19 vaccine among adults in the United States: How many people would get vaccinated? Vaccine. 38:6500–7. DOI: 10.1016/j.vaccine.2020.08.043PubMed Abstract, CrossRef Full Text | Google Scholar.
[31] Guidry JPD, Laestadius LI, Vraga EK, Miller CA, Perrin PB, Burton CW, et al. (2021) Willingness to get the Covid-19 vaccine with and without emergency use authorization. Am J Infect Control. 49:137–42. DOI: 10.1016/j.ajic.2020.11.018 PubMed Abstract, CrossRef Full Text, Google Scholar.
[32] Dror AA, Eisenbach N, Taiber S, Morozov NG, Mizrachi M, Zigron A, et al. (2020) Vaccine hesitancy: the next challenge in the fight against COVID-19. Eur J Epidemiol. 35:775–9. DOI: 10.1007/s10654-020-00671-y PubMed Abstract, CrossRef Full Text, Google Scholar.
[33] Goldman RD, Yan TD, Seiler M, Cotanda CP, Brown JC, Klein EJ, et al. (2020) Caregiver willingness to vaccinate their children against COVID-19: Cross-sectional survey. Vaccine. 38:7668–73. DOI: 10.1016/j.vaccine.2020.09.084 PubMed Abstract, CrossRef Full Text, Google Scholar.
[34] Lazarus JV, Ratzan SC, Palayew A, Gostin LO, Larson HJ, Rabin K, et al. (2021). A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 27:225–8. DOI: 10.1038/s41591-020-1124-9 PubMed Abstract, CrossRef Full Text, Google Scholar.
[35] Salali GD, Uysal MS. (2020) COVID-19 vaccine hesitancy is associated with beliefs on the origin of the novel coronavirus in the UK and Turkey. Psychol Med. 1−3. DOI: 10.1017/S0033291720004067 PubMed Abstract, CrossRef Full Text, Google Scholar.
[36] Su Z, Wen J, Abbas J, McDonnell D, Cheshmehzangi A, Li X, et al. (2020) A race for a better understanding of COVID-19 vaccine non-adopters. Brain Behav Immun Health. 9:100159. doi: 10.1016/j.bbih.2020.100159 PubMed Abstract, CrossRef Full Text, Google Scholar.
[37] Joshi, A., Kaur, M., Kaur, R., Grover, A., Nash, D., & El-Mohandes, A. (2021). Predictors of COVID-
19 Vaccine Acceptance, Intention, and Hesitancy: A Scoping Review. Frontiers in public health, 9, 698111. https://doi.org/10.3389/fpubh.2021.698111.Viewed PDF 2233 53 -
 Assessment of Health Worker’s Pattern of Managing Severe Malaria in Children Under the Age of Five (0-5years) in Northwestern Nigeria - A Cross-Sectional Study of Hospitals in Kebbi StateAuthor: Manir Hassan JegaDOI: 10.21522/TIJPH.2013.10.01.Art007
Assessment of Health Worker’s Pattern of Managing Severe Malaria in Children Under the Age of Five (0-5years) in Northwestern Nigeria - A Cross-Sectional Study of Hospitals in Kebbi StateAuthor: Manir Hassan JegaDOI: 10.21522/TIJPH.2013.10.01.Art007Assessment of Health Worker’s Pattern of Managing Severe Malaria in Children Under the Age of Five (0-5years) in Northwestern Nigeria - A Cross-Sectional Study of Hospitals in Kebbi State
Abstract:
While severe malaria (SM) contributes to high mortality in children in Nigeria, appropriate treatment is cardinal in reducing SM death. However, there exist limited studies on how health workers (HWs) manage SM in children in Nigeria. The study aimed to assess the health worker’s treatment practices for severe malaria in children. A cross-sectional survey of severe malaria (SM) management in children (0- 5 years) was conducted in 377 participants across randomly selected 5 hospitals in Kebbi State. Data abstraction form was used to obtain parameters for SM from the patient’s record. A structured questionnaire was utilized to get information from HWs regarding the management of SM. Statistical analysis was done using SPSS version 23.0. A total of 377 cases of SM were identified. Documented symptoms for SM symptoms included fever (43.2 %), convulsion –seizure (26.3%), pallor (10.3%), and loss of consciousness (3.2%). All the cases (100%) were tested for malaria, with RDT being the commonest (60.2%) technique used, while 71 (18.83%) cases received intra-artesunate, 24 (6.36%) received intravenous quinine. 125 (33.16%) children fully recovered, with 87 (23.08%) discharge cases, and 41 (19.80%) received a follow-up dose of ACT. However, a mortality rate of 26.79% was observed. The pattern of managing severe malaria in this study resulted in improved quality of life in above half of the studied population. However, a higher rate is possible should health workers be given more on-the-job supervision. Besides, further study would be required to ascertain the source of knowledge of severe malaria management in the region.
Assessment of Health Worker’s Pattern of Managing Severe Malaria in Children Under the Age of Five (0-5years) in Northwestern Nigeria - A Cross-Sectional Study of Hospitals in Kebbi State
References:
[1] Bamiselu, O.F., Ajayi, I., Fawole, O. et al. Adherence to malaria diagnosis and treatment guidelines among healthcare workers in Ogun State, Nigeria. BMC Public Health 16, 828 (2016). https://doi.org/10.1186/s12889-016-3495-x.
[2] World Health Organization. 2020. Malaria key facts. https://www.who.int/news-room/fact-sheets/detail/malaria. Accessed on 1st January 2022.
[3] World Health Organization. (2015). World malaria report 2015. World Health Organization. https://apps.who.int/iris/handle/10665/200018. Accessed 4th December 2021.
[4] WHO. The World malaria report at a glance. 2019. https://www.who.int/news-room/feature-stories/detail/world-malaria-report-2019. Accessed on 7th November 2021.
[5] Severe Malaria observatory. 2020. Severe Malaria Criteria, Features & Definition. https://www.severemalaria.org/severe-malaria/severe-malaria-criteria-features-definition. Accessed on 15th December 2021.
[6] White NJ. 2004. Review series Antimalarial drug resistance,. 2004;113(8).
https://doi.org/10.1172/JCI21682.
[7] Global Partnership to Roll Back Malaria. 2000. The African Summit on Roll Back Malaria, Abuja, Nigeria, April 25, 2000. World Health Organization. https://apps.who.int/iris/handle/10665/67815.
[8] Kain KC, Harrington MA, Tennyson S, Keystone JS. Imported malaria: prospective analysis of problems in diagnosis and management. Clin Infect Dis. 1998 Jul;27(1): 142-9. doi: 10.1086/514616. PMID: 9675468.
[9] Mutsigiri-Murewanhema, Faith & Mafaune, Patron & Shambira, Gerald & Juru, Tsitsi & Bangure, Donewell & Mungati, More & Gombe, Notion & Tshimanga, Mufuta. 2017. Factors associated with severe malaria among children below ten years in Mutasa and Nyanga districts, Zimbabwe, 2014-2015. Pan African Medical Journal. 27. 23. 10.11604/pamj.2017.27.23.10957.
[10] Langhorne J, Ndungu FM, Sponaas A-M, Marsh K. Immunity to malaria: more questions than answers. Nat Immunol. 2008; 9:725 -32.DOI: https://doi.org/10.4269/ajtmh.2012.11-0504.
[11] Kyei-Baafour E, Tornyigah B, Buade B, Bimi L, Oduro AR, Koram KA, Gyan BA, Kusi KA. 2020. Impact of an Irrigation Dam on the Transmission and Diversity of Plasmodium falciparum in a Seasonal Malaria Transmission Area of Northern Ghana Trop Med. 2020 Mar 19;2020:1386587. DOI: 10.1155/2020/1386587. eCollection 2020.PMID: 32308690.
[12] Dzeing-Ella A, Obiang PCN, Tchoua R, Planche T, Mboza B, Mbounja M.2005. Severe falciparum malaria in Gabonese children: clinical and laboratory features. Malar J. 2005(4). DOI: 10.1186/1475-2875-4-1.
[13] Edelu BO, Ndu IK, Igbokwe OO, Iloh ON. 2018. Severe falciparum malaria in children in Enugu, Southeast Nigeria. Niger J Clin Pract. 2018 Oct;21(10):1349-1355. DOI: 10.4103/njcp.njcp_140_18. PMID: 30297570.
[14] Okunola PO, Ibadin MO, Ofovwe GE, Ukoh G.2012. Co-existence of urinary tract infection and malaria among children under five years old: a report from Benin City, Nigeria. Saudi J Kidney Dis Transpl. 2012 May;23(3):629-34. PMID: 22569460.
[15] Ukwaja KN, Aina OB, Talabi AA .2011. Clinical overlap between malaria and pneumonia: can malaria rapid diagnostic test play a role? J Infect Dev Ctries 5:199-203. doi: 10.3855/jidc.945.
[16] Shah, M.P., Briggs-Hagen, M., Chinkhumba, J. et al. Adherence to national guidelines for the diagnosis and management of severe malaria: a nationwide, cross-sectional survey in Malawi, 2012. Malar J 15, 369 (2016). https://doi.org/10.1186/s12936-016-1423-2.
[17] Achan J, Tibenderana J, Kyabayinze D, Mawejje H, Mugizi R, Mpeka B, et al. 2011. Case management of severe malaria–a forgotten practice: experiences from health facilities in Uganda. Plos one. 2011.DOI: 10.1371/journal.pone. 0017053.s006.
[18] Nwaneli EI, Eguonu I, Ebenebe JC, Osuorah CDI, Ofiaeli OC, Nri-Ezedi CA.2020. Malaria prevalence and its sociodemographic determinants in febrile children - a hospital-based study in a developing community in South-East Nigeria. Journal of preventive medicine and hygiene. 2020;61(2): E173-e80. doi: https://dx.doi.org/10.15167%2F2421-4248%2Fjpmh2020.61.2.1350.
[19] Breman JG. The ears of the hippopotamus: manifestations, determinants, and estimates of the malaria burden. Am J Trop Med Hyg. 2001 Jan-Feb;64(1-2 Suppl):1-11. DOI: 10.4269/ajtmh.2001.64.1. PMID: 11425172.
[20] Kwenti, T.E., Kwenti, T.D.B., Latz, A. et al. Epidemiological and clinical profile of paediatric malaria: a cross-sectional study performed on febrile children in five epidemiological strata of malaria in Cameroon. BMC Infect Dis 17, 499 (2017). https://doi.org/10.1186/s12879-017-2587-2.
[21] WHO Guidelines for malaria, 16th February 2021. Geneva: World Health Organization; 2021 (WHO/UCN/GMP/2021.01). Licence: CC BY-NC-SA 3.0 IGO. https://cdn.who.int/media/docs/default-source/malaria/who-ucn-gmp-2021.01-eng.pdf.
[22] Wikipedia. Kebbi State from Wikipedia, the free encyclopedia.https://en.m.wikipedia.org/wiki/Kebbi_State. Accessed on 2nd October 2021.
[23] Bamgboye EA. 2013. Sample size determination in: Lecture notes on research methodology in the health and medical sciences. Ibadan. Folbam publishers. 2013:168-96.https://www.npmj.org/article.asp?issn=1117-1936;year=2020;volume=27;issue=2;spage=67;epage=75;aulast=Bolarinwa. Accessed on 17th September 2021.
[24] Batwala, V., Magnussen, P. & Nuwaha, F. 2010. Are rapid diagnostic tests more accurate in the diagnosis of plasmodium falciparum malaria compared to microscopy at rural health centres?. Malar J 9, 349 (2010). https://doi.org/10.1186/1475-2875-9-349.
[25] Orish, V.N., De-Gaulle, V.F. & Sanyaolu, A.O.2018. Interpreting rapid diagnostic test (RDT) for Plasmodium falciparum. BMC Res Notes 11, 850 (2018). https://doi.org/10.1186/s13104-018-3967-4.
[26] Batwala, V., Magnussen, P. & Nuwaha, F. 2011. Comparative feasibility of implementing rapid diagnostic test and microscopy for parasitological diagnosis of malaria in Uganda. Malar J 10, 373 (2011). https://doi.org/10.1186/1475-2875-10-373.
[27] Neumann CG, Bwibo NO, Siekmann JH, McLean ED, Browdy B, Drorbaugh N. 2008. Comparison of blood smear microscopy to a rapid diagnostic test for in-vitro testing for P. falciparum malaria in Kenyan school children. East Afr Med J. 2008 Nov;85(11):544-9. doi: 10.4314/eamj. v85i11.9670.
[28] Endeshaw, T., Gebre, T., Ngondi, J. et al. 2008. Evaluation of light microscopy and rapid diagnostic test for the detection of malaria under operational field conditions: a household survey in Ethiopia. Malar J 7, 118 (2008). https://doi.org/10.1186/1475-2875-7-118.
[29] Wongsrichanalai C, Barcus MJ, Muth S, Sutamihardja A, Wernsdorfer WH. 2007. A review of malaria diagnostic tools: microscopy and rapid diagnostic test (RDT). Am J Trop Med Hyg. 2007 Dec;77(6 Suppl):119-27. PMID: 18165483.
[30] Manyando, C., Njunju, E.M., Chileshe, J. et al. 2014. Rapid diagnostic tests for malaria and health workers’ adherence to test results at health facilities in Zambia. Malar J 13, 166 (2014). https://doi.org/10.1186/1475-2875-13-166.
[31] Ayieko, P., Irimu, G., Ogero, M. et al.2019. Effect of enhancing audit and feedback on uptake of childhood pneumonia treatment policy in hospitals that are part of a clinical network: a cluster randomized trial. Implementation Sci 14, 20 (2019). https://doi.org/10.1186/s13012-019-0868-4.
[32] Irimu G, Ogero M, Mbevi G, Agweyu A, Akech S, Julius T, et al. 2018. Approaching quality improvement at scale: a learning health system approach in Kenya. BMJ. 2018; 103:1013–9. DOI: 10.1093/cid/ciz844.
[33] Ampadu HH, Asante KP, Bosomprah S, Akakpo S, Hugo P, Gardarsdottir H, Leufkens HGM, Kajungu D, Dodoo ANO. 2019. Prescribing patterns and compliance with World Health Organization recommendations for the management of severe malaria: a modified cohort event monitoring study in public health facilities in Ghana and Uganda. Malar J. 2019 Feb 8;18(1):36. DOI: 10.1186/s12936-019-2670-9. PMID: 30736864; PMCID: PMC6368732.
[34] Dondorp A, Nosten F, Stepniewska K, Day N, White N;.2005. Southeast Asian Quinine Artesunate Malaria Trial (SEAQUAMAT) group. Artesunate versus quinine for treatment of severe falciparum malaria: a randomized trial. Lancet. 2;366(9487):717-25. DOI: 10.1016/S0140-6736(05)67176-0. PMID: 16125588.
Viewed PDF 1196 33 -
 Drug Utilization Pattern of Antihypertensives in a Private Healthcare Setting in Enugu, NigeriaAuthor: Ngozi Dorathy UdemDOI: 10.21522/TIJPH.2013.10.01.Art008
Drug Utilization Pattern of Antihypertensives in a Private Healthcare Setting in Enugu, NigeriaAuthor: Ngozi Dorathy UdemDOI: 10.21522/TIJPH.2013.10.01.Art008Drug Utilization Pattern of Antihypertensives in a Private Healthcare Setting in Enugu, Nigeria
Abstract:
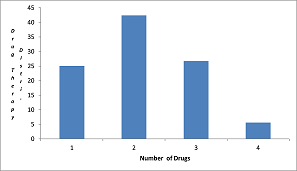
Hypertension is a public health challenge worldwide. Drug utilization study is a component of medical audit that monitors and evaluates prescribing practices and recommends necessary modifications. This study focused on the drug utilization pattern of antihypertensive drugs. The study was a retrospective study of facility records on drug use among hypertensive patients. It was conducted in a private health care setting facility in Enugu. A total of 1,005 prescriptions were evaluated for drug prescribing patterns. The blood pressure control was evaluated. A combination of two drugs was frequently prescribed (42.3%). Drug prescribing pattern showed that Angiotensin receptor blocker (Losartan) was mostly frequently prescribed (38.94%). Drug utilization of antihypertensive drugs was in agreement with JNC 7&8 recommendations. In the study combination of two or more anti-hypertensive drugs was frequently prescribed. The blood pressure control among the population was greater than 90%.
Drug Utilization Pattern of Antihypertensives in a Private Healthcare Setting in Enugu, Nigeria
References:
[1] World Health Organization (WHO). https://www.who.int. Accessed on 25/6/2021.
[2] World Health Organization 2013. Global health observatory (GHO) data.; https://www.who.int gho
Accessed on 20/9/2019.
[3] Oke O., Adedapo A. 2015, Antihypertensive drug utilization and blood pressure control in a Nigerian hypertensive population. Gen. Med.; 3 (2); DOI 10.4172/2327-5146.1000169.
[4] Centers for Disease Control and Prevention 2020. Facts about hypertension. https://www.cdc.gov blood pressure Accessed on 2/5/2021.
[5] Bosu W.K., Reilly S.T., Aheto J.M.K., Zuccelli E. 2016, Hypertension in older adults in Africa: Asystematic review and meta-analysis PLos ONE; 4(4): e0214934. DOI: 101371/journal.pone.0214934.
[6] Arodiwe E.B., Nwokediuko S.C., Ike S.O. 2014, Medical causes of death in a teaching hospital in South-Eastern Nigeria: A 16-year review. Niger J Clin Pract.; 17(6):711-6. DOI: 10.4103/1119-3077.144383.
[7] James A.P., Oparil S., Carter B. L.et al 2014, A 2014 evidence-based guideline for the management of high blood pressure in adults: Report from the Panel Members Appointed to the Eighth Joint National Committee (JNC 8). JAMA .311(17):507- 520. DOI:10.100/jama2013.284427.
[8] Jarari N., Rao N., Peela R., Ellafi K.A., Shakila S., Said R.A., et al.2016, A review on prescribing patterns of antihypertensive drugs. Clin. Hypertension, 22:7, www.doi.org/10.1186/s40885-016-0042-0.
[9] Nachiya J.R.A.M., Parimalakrihnan S., Ramakrishna R.M. 2015, Study on drug utilization pattern of antihypertensive medications on out-patients and in-patients in a tertiary care teaching hospital: A cross sectional study. Afri, J of Pharm and Pharmacol.,9(11), 383-396. doi.10.5897/AJPP.2014.4263.
[10] Shah J., Balraj A. 2017, Drug utilization pattern of antihypertensive agents in patients of hypertensive nephropathy in a tertiary care teaching hospital; a cross-sectional study. Int. J. Basic Clin. Pharmacol., 6:2131-3. doi.10.18203/2319-2003.IJbcp20173636.
[11] AlavudeenSS, Alakhali KL, Ansari AS, Khan N. Prescribing pattern of anti-hypertensive drugs in diabetic patients of Southern Province Kingdom of Saudi Arabia. Ars. Pharmaceutical., 56(2): 109-11.
[12] Mohan M. 2016, Drug utilization evaluation of antihypertensives in a super speciality hospital. Int. J of Pharma. Research & Review., 5(9):1-8.
[13] Amit S., Tanpreet K.B., Vishal G., Mahendra S.R., Manik C., Gaur A. 2018, Drug utilization study on hypertensive patients and assessment of medication adherence to JNC-8 Guidelines in North Indian tertiary care hospital: A cross-sectional study. Adv. Res. Gastroentero. Hepatol., 9 [1]: 555751. Doi. 10.19080/ARGH.2018.09.555751.
[14] Yadav K., Singh A., Sigdel M., Malla B., Guragain S., Aryal B., et al. 2015, Antihypertensive drugs utilization pattern in the clinic of a remote village of Nepal. Int. J. of Health Sciences and Research, 5(12):185-189.
[15] Jaiprakash H., Vinotini K., Vindiya., Vsalni., Vikneshwara, Vigneswaram et al.2013, Drug utilization study of antihypertensive drugs in a clinic in Malaysia. Int. J. of Basic and Clin Pharmacol., 2(4): 407-410.
[16] Sani M., Mijinyawa M., Adamu B., Abdu A., Borodo M. 2008, Blood Pressure control among treated hypertensives in a tertiary health institution. Nigeria J. Med., 17(3):270-274 Doi: 10.4314/njm.v.17i3.37394.PMID:18788251.
[17] Salako B.L., Ayodele O.E., Kadiri S., Arije A. 2002, Assessment of blood pressure control in a Black African population. Trop. Cardiol. 2002; 28(109):3-6.
[18] Mutnick A.H. 2004, Hypertension In: Leon S., Alam M., Sourney and Swanson L. ed, Comprehensive Pharmacy Review for NCLE. 5th edn., Philadelphia: Lippincott Williams and Wilkins, 762-767.
[19] Oparah C.2010, Pharmaceutical care in hypertension. In Opara C. ed Essentials of pharmaceutical care, 2nd edition Lagos: Cybex, 403.
[20] Adedapo D.A., Adedeji W.A., Adeosun A.M., Olaremi J., Okunlola C.K.2016, Antihypertensive drug use and blood pressure control among in-patients with hypertension in Nigeria tertiary health centre. Int. J. of Basic and Clin.Pharmacol., 5(3): 696-701. doi.org/10.18203/2319-2003IJPC20161503.
Viewed PDF 1043 26 -
 Assessing the Relationship between Individual Level Dietary Intake and the Occurrence of Preeclampsia/Eclampsia and Haemorrhage among Pregnant Women in Eastern Region of Ghana: A Prospective Cohort StudyAuthor: James Atampiiga AvokaDOI: 10.21522/TIJPH.2013.10.01.Art009
Assessing the Relationship between Individual Level Dietary Intake and the Occurrence of Preeclampsia/Eclampsia and Haemorrhage among Pregnant Women in Eastern Region of Ghana: A Prospective Cohort StudyAuthor: James Atampiiga AvokaDOI: 10.21522/TIJPH.2013.10.01.Art009Assessing the Relationship between Individual Level Dietary Intake and the Occurrence of Preeclampsia/Eclampsia and Haemorrhage among Pregnant Women in Eastern Region of Ghana: A Prospective Cohort Study
Abstract:
Pre-eclampsia/eclampsia (PE-E) and haemorrhage are dangerous diseases that occur in pregnancy. This study seeks to assess the relationship between individual-level dietary intake and the occurrence of pre-eclampsia/eclampsia and haemorrhage among pregnant women in the Eastern Region of Ghana. The prospective cohort study involved all pregnant women in their third trimester of pregnancy (>28 weeks gestational age) reporting for antenatal care (ANC) in seven Hospitals in the Eastern Region of Ghana. The study used a 24-hour repeated dietary recall to elicit dietary intake information from pregnant women until delivery. The majority of pregnant women in this study had adequate consumption of phosphorus far above the RDI, coupled with an inadequate intake of calcium, excess intake of sodium, and manganese. The average dietary intake for carbohydrates in this study was rather higher than the RDA. There was a statistically significant association between PE-E and the intake of vitamin C. A statistically significant association exists between the intake of calcium and vitamin A and haemorrhage. The findings show that pregnant women who consumed adequate and excess amounts of vitamin C reduced their odds of developing PE-E by 41.7% and 39.8%, respectively. The results show that pregnant women who had an excess intake of calcium were 6.128 times the odds of developing haemorrhage compared to those who had inadequate intake. Again, pregnant women who had adequate intake of vitamin A were 4.351 times the odds of developing haemorrhage compared to those who had inadequate intake. It is recommended that more nutrition specialists to be trained and posted to counsel pregnant women on nutrition in pregnancy to avert the consequences of PE-E and haemorrhage.
Assessing the Relationship between Individual Level Dietary Intake and the Occurrence of Preeclampsia/Eclampsia and Haemorrhage among Pregnant Women in Eastern Region of Ghana: A Prospective Cohort Study
References:
[1] World Health Organization. (2018). WHO recommendations: policy of interventionist versus expectant management of severe pre-eclampsia before term.
[2] Say, L., Chou, D., Gemmill, A., Tunçalp, Ö., Moller, A. B., Daniels, J., Gülmezoglu, A. M., Temmerman, M., & Alkema, L. (2014). Global causes of maternal death: A WHO systematic analysis. The Lancet Global Health, 2(6). https://doi.org/10.1016/S2214-109X(14)70227-X.
[3] Peraçoli et al. (2020). Pre-eclampsia / Eclampsia. 318–332.
[4] Brown et al. (2018). Hypertensive Disorders of Pregnancy. 24–43. https://doi.org/10.1161/hypertensionaha.117.10803.
[5] Sánchez-aranguren, L. C., Prada, C. E., Riaño-medina, C. E., & Lopez, M. (2014). Endothelial dysfunction and preeclampsia : role of oxidative stress. 5(October), 1–11. https://doi.org/10.3389/fphys.2014.00372.
[6] Mannaerts, D., Faes, E., Gielis, J., Craenenbroeck, E. Van, Cos, P., Spaanderman, M., Gyselaers, W., Cornette, J., & Jacquemyn, Y. (2018). Oxidative stress and endothelial function in normal pregnancy versus pre-eclampsia , a combined longitudinal and case-control study. 1–9.
[7] Say, L., Chou, D., Gemmill, A., Tunçalp, Ö., Moller, A., Daniels, J., Gülmezoglu, A. M., Temmerman, M., & Alkema, L. (2006). Global causes of maternal death : a WHO systematic analysis. 323–333. https://doi.org/10.1016/S2214-109X(14)70227-X.
[8] Asamoah, B. O., Moussa, K. M., Stafström, M., & Musinguzi, G. (2011). Distribution of causes of maternal mortality among different socio-demographic groups in Ghana ; a descriptive study.
[9] Moyer, C., Gyasi, R. K., Akosa, A. B., Tettey, Y., Akakpo, P. K., & Anim, J. T. (2013). Pregnancy related causes of deaths in ghana : a 5-year retrospective study. 47(4), 158–163.
[10] Ghana Health Service (GHS) Annual Report, Eastern Region-2020.
[11] GDHS, (2021). Population and Housing Census, 2021 Preliminary Report.
[12] Cochran, W. G. 1963. Sampling Techniques, 2nd Ed., New York: John Wiley and Sons, Inc.
[13] Veena, S. R., Gale, C. R., Krishnaveni, G. V, Kehoe, S. H., Srinivasan, K., & Fall, C. H. D. (2016). Association between maternal nutritional status in pregnancy and offspring cognitive function during childhood and adolescence ; a systematic review. BMC Pregnancy and Childbirth. https://doi.org/10.1186/s12884-016-1011-z.
[14] Grum, T., Hintsa, S., & Hagos, G. (2018). Dietary factors associated with preeclampsia or eclampsia among women in delivery care services in Addis Ababa, Ethiopia : a case-control study. BMC Research Notes, 1–5. https://doi.org/10.1186/s13104-018-3793-8.
[15] Endeshaw, M., Ambaw, F., Aragaw, A., & Ayalew, A. (2014). Effect of Maternal Nutrition and Dietary Habits on Preeclampsia : A Case-Control Study. January. https://doi.org/10.4236/ijcm.2014.521179.
[16] Ram, D., Id, S., Sangroula, R. K., Shakya, N. S., Yadav, R., Chaudhary, N. K., Man, P., & Pradhan, S. (2019). Effect of nutrition education on hemoglobin level in pregnant women : A quasi- experimental study. 1–12.
[17] Stadlmayr, & et al.,. (2012). Table de composition des aliments d´Afrique de l´Ouest West African Food Composition Table.
[18] Saaka, M., & Oladele, J. (2020). Adequacy of nutrient intakes among pregnant women in northern Ghana. 11(1), 145–164.
[19] Ayensu et al. (2020). Prevalence of anaemia and low intake of dietary nutrients in pregnant women living in rural and urban areas in the Ashanti region of Ghana. 1–15. https://doi.org/10.1371/journal.pone.0226026.
[20] Zhao, W., Yu, K., Tan, S., Zheng, Y., Zhao, A., Wang, P., & Zhang, Y. (2017). Dietary diversity scores: An indicator of micronutrient inadequacy instead of obesity for Chinese children. BMC Public Health, 17(1), 1–11. https://doi.org/10.1186/s12889-017-4381-x.
[21] Adikari, A. M. N. T., Sivakanesan, R., Wijesinghe, D. G. N. G., & Liyanage, C. (2016). Assessment of Nutritional Status of Pregnant Women in a Rural Area in Sri Lanka. 27(2), 203–211.
[22] Institute of Medicine (IOM), 2006.
[23] Kominiarek, M. A., & Rajan, P. (2017). HHS Public Access. 100(6), 1199–1215. https://doi.org/10.1016/j.mcna.2016.06.004.Nutrition.
[24] Saaka, M. (2020). Adequacy of nutrient intakes among pregnant women in Northern Ghana. August. https://doi.org/10.26596/wn.2020111145-164.
[25] Lee, S. E., Talegawkar, S. A., Merialdi, M., & Caulfield, L. E. (2013). Dietary intakes of women during pregnancy in low- and middle-income countries. Public Health Nutrition, 16(8), 1340–1353. https://doi.org/10.1017/S1368980012004417.
[26] Nguyen, P. H., Huybregts, L., Sanghvi, T. G., Tran, L. M., Frongillo, E. A., Menon, P., & Ruel, M. T. (2018). Dietary Diversity Predicts the Adequacy of Micronutrient Intake in Pregnant Adolescent Girls and Women in Bangladesh, but Use of the 5-Group Cutoff Poorly Identifies Individuals with Inadequate Intake. https://doi.org/10.1093/jn/nxy045.
[27] Marvin-Dowle, K., Burley, V. J., & Soltani, H. (2016). Nutrient intakes and nutritional biomarkers in pregnant adolescents: A systematic review of studies in developed countries. BMC Pregnancy and Childbirth, 16(1), 1–24. https://doi.org/10.1186/s12884-016-1059-9.
[28] Nove, A., Matthews, Z., Neal, S., & Camacho, A. V. (2014). Maternal mortality in adolescents compared with women of other ages: Evidence from 144 countries. The Lancet Global Health, 2(3), e155–e164. https://doi.org/10.1016/S2214-109X(13)70179-7.
[29] Apungu, F. K. (2019). Nutritional and health status of people living with HIV / AIDS in the eastern region of Ghana. November. https://doi.org/10.1108/NFS-05-2019-0145.
[30] Bobić et al. (2015). Perinatal Epidemiological Risk Factors For Preeclampsia. 54(1), 9–13.
[31] Imdad, A., Jabeen, A., & Bhutta, Z. A. (2011). Role of calcium supplementation during pregnancy in reducing the risk of developing gestational hypertensive disorders : a meta-analysis of studies from developing countries. 11(Suppl 3).
[32] Jabeen, M., Yakoob, M. Y., Imdad, A., & Bhutta, Z. A. (2011). Impact of interventions to prevent and manage preeclampsia and eclampsia on stillbirths. BMC Public Health, 11(SUPPL. 3), S6. https://doi.org/10.1186/1471-2458-11-S3-S6.
[33] Abu-saad, K., & Fraser, D. (2010). Maternal Nutrition and Birth Outcomes. March. https://doi.org/10.1093/epirev/mxq001.
[34] Duley, L., Meher, S., & Abalos, E. (2006). Clinical review Management of pre-eclampsia. box 5.
[35] Torjusen, H., Brantsæter, A. L., Haugen, M., Alexander, J., Bakketeig, L. S., Lieblein, G., Stigum, H., Næs, T., Swartz, J., Holmboe-ottesen, G., Roos, G., & Meltzer, H. M. (2014). Reduced risk of pre-eclampsia with organic vegetable consumption : results from the prospective Norwegian Mother and Child Cohort Study. 1–11. https://doi.org/10.1136/bmjopen-2014-006143.
[36] Agrawal, S., Fledderjohann, J., Vellakkal, S., & Stuckler, D. (2015). Adequately Diversified Dietary Intake and Iron and Folic Acid Supplementation during Pregnancy Is Associated with Reduced Occurrence of Symptoms Suggestive of Pre- Eclampsia or Eclampsia in Indian Women. 1–23. https://doi.org/10.1371/journal.pone.0119120.
[37] Hofmeyr GJ, Lawrie TA, Atallah AN, Duley L, Torloni MR (2014) Calcium supplementation during pregnancy for preventing hypertensive disorders and related problems.Cochrane Database Syst Rev 6: CD001059. doi:10.1002/14651858.CD001059.pub4 PMID: 24960615.
[38] Jain S, Sharma P, Kulshreshtha S, Mohan G, Singh S (2010) The role of calcium, magnesium, and zinc in pre-eclampsia. Biological trace element research 133(2): 162–170. doi:10.1007/s12011-009-8423-9 PMID: 19547932.
[39] World Health Organization. (2020). Calcium supplementation before pregnancy for the prevention of pre-eclampsia and its complications. https://apps.who.int/iris/bitstream/handle/10665/331787/9789240003118-eng.pdf?ua=1.
Viewed PDF 913 32 -
 Mental and Technical Readiness of Freshmen Nursing Students in an Online Learning ModalityAuthor: Gerald T. MalabarbasDOI: 10.21522/TIJPH.2013.10.01.Art010
Mental and Technical Readiness of Freshmen Nursing Students in an Online Learning ModalityAuthor: Gerald T. MalabarbasDOI: 10.21522/TIJPH.2013.10.01.Art010Mental and Technical Readiness of Freshmen Nursing Students in an Online Learning Modality
Abstract:
The Covid-19 pandemic opens more windows to online learning globally. With this, all countries have shifted their educational setup to online learning modalities due to this pandemic. This study assessed the level of mental and technical readiness in the online learning modality of freshmen nursing students in one of the catholic private institutions in the Philippines. The researchers made use of descriptive research. An adapted questionnaire was used as a data-gathering tool but subjected to a reliability test. Results revealed that most of the respondents were female, graduated from the STEM strand, and belong to poor families. It further disclosed that for the mental dimension, the students were ready, and for the technical dimension, they were only somewhat ready. Additionally, inferential statistics showed that among the student’s profiles, the family’s monthly income showed a significant difference specifically between the poor and the lower-middle-income group both in mental and technical dimensions. The proposed psycho-social programs were focused on the topmost indicators that obtained the lowest mean scores among indicators observed, such as the presence of distractions, spending 20-30 hours each week on an online course, and availability of reliable person around, lack of a printer, stable internet connection, and the student’s device compatibility needed for online learning. Thus, the researchers highly recommend that the institution should intensify its orientation program on the use of the learning management system of an online learning modality and improve its program on mental health issues for both students, parents, and teachers.
Mental and Technical Readiness of Freshmen Nursing Students in an Online Learning Modality
References:
[2] El-Seoud, M. S. A., Islam A.T.F., Eddin, T., Seddiek, N., El-Khouly, M. M., & Nosseir, A. (2014). E-learning and students’ motivation: A research study on the effect of E-learning on higher education. International Journal of Emerging Technologies in Learning, 9(4), 20-26. https://www.researchgate.net/publication/264417866_ELearning_and_Students’_Motivation_A_Research_Study_on_the_Effect_of_E-Learning_on_Higher_Education.
[3] Blaschke, L.M., & Bedenlier, S. (2020, April). Online learning.
https://www.researchgate.net/publication/342344404_Online_Learning.
[4] Coman, C., Tiru, L. G., An-Schmitz, L. M., Stanciu, C., & Bularca, M. C. (2020). Online teaching and learning in higher education during the Coronavirus pandemic: Students’ perspective. Sustainability 12, 1-24. https://www.mdpi.com/2071-1050/12/24/10367/pdf.
[5] Armstrong-Mensah, E., Ramsey-White, K., Yankey, B., & Self-Brown, S. (2020). COVID-19 and distance learning: Effects on Georgia State University School of public health students. Frontiers in Public Health,8. 1-10. https://www.frontiersin.org/articles/10.3389/fpubh.2020.576227/full.
[6] Asian Development Bank. (2021). COVID-19 and education in Asia and the Pacific guidance note. https://www.adb.org/documents/covid-19-education-asia-pacific-guidance-note.
[7] Agaton, C. B., & Cueto, L. J. (2021). Learning at home: Parents’ lived experiences on distance learning during COVID-19 pandemic in the Philippines. International Journal of Evaluation and Research in Education,10(3), 901-911. http://ijere.iaescore.com/index.php/IJERE/article/view/21136.
[9] David, F. (2002). Understanding and doing research: A handbook for beginners. Panorama Printing Inc. (Trial Edition., pp. 104-106).
[10] Vicki Williams, V. (n.d.). Online readiness assessment. Retrieved October 15, 2021. https://pennstate.qualtrics.com/jfe/form/SV_7QCNUPsyH9f012B?s=246aa3a5c4b64bb386543eab834f8e75.
[11] Taber, K. (2017). The use of Cronbach’s alpha when developing and reporting research instruments in science education. Res Sci Educ.file:///E:/research/The_Use_of_Cronbachs_Alpha_When_Developing_and_Re.pdf.
[12] Gras, R. M. L., Sánchez-López, M. P., Román, A. I. S., Corbalán, J. (2013). Health and gender in female-dominated occupations: The case of male nurses. The Journal of Men’s Studies, 21(2),135-148 https://www.researchgate.net/publication/273690724_Health_and_Gender_in_Female-Dominated_Occupations_The_Case_of_Male_Nurses.
[13] Albert, J. R. G., Abrigo, M. R. M., Quimba, F. M. A., & Jana Flor V. Vizmanos, J. F. V. (2020). Poverty, the middle class, and income distribution amid COVID-19. Discussion Paper Series No. 2020-22. 1-56. https://pidswebs.pids.gov.ph/CDN/PUBLICATIONS/pidsdps2022.pdf.
[14] Ocampo, D. S. (2014). The K to 12 Curriculum. 1-18. Retrieved from: https://industry.gov.ph/wp-content/uploads/2015/05/6th-TID-Usec.-Ocampos-Presentation-on-K-to-12.pdf.
[15] Kurt, A. A., Doğan, E., Erdoğmuş, Y. K., & Emiroğl, B. G. (2018). Examining computer gaming addiction in terms of different variables. World Journal on Educational Technology, 10(10), 30-40. https://www.researchgate.net/publication/324170945_Examining_computer_gaming_addiction_in_terms_of_different_variables.
[16] Raiyn, J. (2016). The role of visual learning in improving students’ high order thinking skills. Journal of Education and Practice, 7(24), 115-121. http://www.sciepub.com/reference/185998.
[17] Shapiro, S. S., & Wilk, M. B., (1965) An analysis for variance test for normality. Biometrika 52(3&4), 591. https://www.jstor.org/stable/2333709.
[18] Hermantoa, Rai, N. G. M., & Fahmi, A. (2021). Students’ opinions about studying from home during the Covid-19 pandemic in Indonesia. Cypriot Journal of Educational Sciences, 16(2), 499-510. https://orcid.org/0000-0001-6566-9299.
[19] Oducado, R. M. F., & Homelo V. Estoque, H. (2021). Online learning in nursing education during the Covid-19 pandemic: Stress, satisfaction, and academic performance. Journal of Nursing Practice, 4(2), 143-153. https://doi.org/10.30994/jnp.v4i2.128.
[20] Khan, F. M., Begum, M, & Imad, M. (2019). Relationship between students’ home environment and their academic achievement at secondary school level. Pakistan Journal of Distance & Online
Learning, 5(2), 223-234. http://journal.aiou.edu.pk/journal1/index.php/PJDOL/article/view/564.[21] Binlingan, A. N. L., Ognayon, P. J., Batchi, J., & Gotia, K. C. L. (2021). Online readiness and self-efficacy of students as reflected on online learning. https://www.researchgate.net/publication/355903386_Online_Readiness_and_Self-Efficacy_of_Students_as_reflected_on_Online_Learning.
[22] Rotas, E. E., & Cahapay, M. B., (2020). Difficulties in remote learning: Voices of Philippine university students in the wake of COVID-19 crisis. Asian Journal of Distance Education, 15(2), 147- 158. http://www.asianjde.com/ojs/index.php/AsianJDE/article/view/504.
Viewed PDF 1639 67 -
 Behavioral Skills and Hypertension Prevention Practices among Teachers in Selected Secondary Schools in Sagamu Local Government Area, Ogun State, NigeriaAuthor: Raymond S DankoliDOI: 10.21522/TIJPH.2013.10.01.Art011
Behavioral Skills and Hypertension Prevention Practices among Teachers in Selected Secondary Schools in Sagamu Local Government Area, Ogun State, NigeriaAuthor: Raymond S DankoliDOI: 10.21522/TIJPH.2013.10.01.Art011Behavioral Skills and Hypertension Prevention Practices among Teachers in Selected Secondary Schools in Sagamu Local Government Area, Ogun State, Nigeria
Abstract:
The development of chronic illness such as hypertension among individuals in occupations such as teaching has been associated with a high level of stress and sedentary behaviours. This study, therefore, evaluated the behavioural skills and hypertension prevention practices among secondary school teachers in Sagamu Local Government Area of Ogun State, Nigeria. This study adopted a cross-sectional design. A Multi-stage sampling technique was used to select 418 respondents for the study. A validated semi-structured questionnaire was used for data collection. Data collected were analysed using descriptive and inferential statistics at ≤0.05 level of significance. The mean age of the respondents was 42.61±7.79 years. More than half, 250 (59.8%) of the respondents were females, with the majority 375 (89.7%) being married. A greater proportion 313 (74.9%) of the respondents had Bachelor’s degree (B.Sc). While about quarter 105 (25.1%) of them had worked for a period of 6-10 years. Most 299 (71.5%) of the respondents had high behavioral skills towards hypertension prevention. Less than half 192 (45.9%) of the respondents had high prevention practice. Behavioral skills significantly contributed to the prevention practices (Odds ratio= 1.12; CL= 1.05- 1.20; p = 0.001). The study revealed that the teachers had high behavioural skills and low hypertension prevention. It is recommended that the state ministry of education through the state ministry of health should conduct a health education program to improve the hypertension prevention practices of teachers.
Behavioral Skills and Hypertension Prevention Practices among Teachers in Selected Secondary Schools in Sagamu Local Government Area, Ogun State, Nigeria
References:
[1] NCD Risk Factor Collaboration (NCD-RisC). 2017. Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19·1 million participants. Lancet; 389:37–55. https://doi:10.1016/S0140-6736(16)31919-5.
[2] Mills, K., Bundy, J., Kelly, T., Reed, J., Kearney, P., Reynolds, K., Chen, J., and He, J. 2016. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation.; 134:441–450. https://doi:10.1161/circulationaha.115.018912.
[3] Eman, A. 2020. Diversity and Equality in Health. Retrieved from
https://diversityhealthcare.imedpub.com/hypertension-2020-market-analysis.php?aid=26209.
[4] World Health Organization 2015. WHO global health observatory data repository. Retrieved from: https://www.who.int/data/gho/data/indicators/indicator-details/GHO/raised-blood-pressure-(sbp-=140-or-dbp-=90)-(age-standardized-estimate).
[5] Akinlua, T., Meakin, R., Umar, A.M., and Freemantle, N. 2015. Current Prevalence Pattern of Hypertension in Nigeria: A Systematic Review. PLoS ONE 10(10): e0140021. https://doi:10.1371/journal. pone.0140021.
[6] Damasceno, A., Azevedo, A., Silva-Matos, C., Prista, A., Diogo, D., and Lunet, N.2009. Hypertension prevalence, awareness, treatment, and control in mozambique: urban/rural gap during the epidemiological transition. Hypertension;54(1):77-83. https://doi:10.1161/hypertensionaha.109.132423.
[7] Adeloye, D., Basquill, C., Aderemi, A., Thompson, J., and Obi, F. 2015. An estimate of the prevalence of hypertension in Nigeria: a systematic review and meta-analysis. Journal of Hypertension 33(2):230-242.
[8] Olamoyegun, M.A., Oluyombo, R., Iwuala, SO., Asaolu, SO. 2016. Epidemiology and patterns of hypertension in semi-urban communities, south-western Nigeria. Cardiovascular Journal African. 23;27(6):356-360. https://doi:10.5830/CVJA-2016-037.
[9] Okubadejo, N., Ozoh,O., Ojo, O., Akinkugbe, A., Odeniyi, I., Adegoke, O., Bello, B., and Agabi, O. 2019, Prevalence of hypertension and blood pressure profile amongst urban-dwelling adults in Nigeria: a comparative analysis based on recent guideline recommendations. Clinical Hypertension, 25,7.
[10] Miazgowski T, Kopec J, Widecka K, Miazgowski B, Kaczmarkiewicz A. 2016. Epidemiology of hypertensive heart disease in Poland: findings from the Global Burden of Disease Study. Archives of Medical Science https://doi:10.5114/aoms.2019.85222.
[11] Fasoro O. 2017. Awareness of Hypertension among public Secondary Schools Teachers in Local Governments Area of Ekiti State, Nigeria. International Journal of Medicinal Research and Application. Vol.1 (21) pp 05-09.
[12] Fisher, W. A., Fisher, J. D., & Harman, J. 2003. The information-motivation behavioural skill model: a general social psychological approach to understanding promoting health behaviour. In J. Suls, & K. A. Wallston (Eds.), Social psychological foundation of health and illness (pp. 82e106). Malden, MA:Blackwell.
[13] Ajewole, I., Fasoro, A., and Agbana, R. 2017, Awareness of hypertension among Public Secondary School Teachers in a Local Government Area of Ekiti State, Nigeria International Journal of Medical Research and Applications, 1(2); 05-09.
[14] Famuyiwa S.A. 2019. Knowledge, Attitude and Hypertension at Risk Behaviour of Secondary School Teachers in Oluyole Local Government of Oyo State, Nigeria. Ibadan Journal of Educational Studies. Vol 16, Nos 1& 2. ISSN: 1596-5953.
[15] Oladoyinbo, C., Ekerette, N., & Ogunbi, T. 2015. Obesity and hypertension amongst Traders in Ijebu-Ode, Nigeria. African Journal of Biomedical Research, 18,23-27.
[16] Odelola, O., Akinpelu, A.,Idowu A., Adesegun, O., et al. (2021). Hypertension: predictors of knowledge among market women in the sub-urban Town of Sagamu, South-west Nigeria. African Journal of Health Science, 34(4); 526-536.
[17] Sarah, J.M, John, S., and Madhanagopal, R. 2017. Lifestyle determinants of hypertension among Female School Teachers. International Journal. of Life Sciences, 5 (4): 696-702.
[18] Amanyire, J, Tumwebaze, M., Mugisha, M. & Bright, L. 2019. Prevalence and risk factors for hypertension, diabetes, and obesity among Lecturers and Support Staff of Bishop Stuart University in Mbarara, Uganda. Open Journal of Applied Sciences, 9, 126-137. doi: 10.4236/ojapps.2019.93012.
[19] Fikadu, G., & Lemma, S. 2016. Socioeconomic status and hypertension among Teachers and Bankers in Addis Ababa, Ethiopia. International journal of hypertension, 4143962.
https://doi.org/10.1155/2016/4143962.
[20] Mirzaei, M., Mirzaei, M., Bagheri, B. 2020. Awareness, treatment, and control of hypertension and related factors in adult Iranian population. BMC Public Health 20, 667 https://doi.org/10.1186/s12889-020-08831-1.
[21] Rajkumar, E., and Romate, J. 2020. Behavioural risk factors, hypertension knowledge, and hypertension in Rural India. International Journal of Hypertension, 2020;7. Doi. Or/10.1155/2020/8108202
[22] Oladapo O.O, Salako L, Sadiq L, Soyinka K and Falase A.O. 2013. Knowledge of Hypertension and other Risk Factors for Heart Disease among Yoruba Rural Southwestern Nigerian Population. British Journal of Medicine & Medical Research;3: 993‐1003.
Viewed PDF 1254 25 -
 Uptake of Cancer Screening among Staff of Military Hospital LagosAuthor: Abiola Ajoke Odeleye OladiranDOI: 10.21522/TIJPH.2013.10.01.Art012
Uptake of Cancer Screening among Staff of Military Hospital LagosAuthor: Abiola Ajoke Odeleye OladiranDOI: 10.21522/TIJPH.2013.10.01.Art012Uptake of Cancer Screening among Staff of Military Hospital Lagos
Abstract:
The uptake of cancer screening services remains poor in developing countries due to altered perception and awareness of cancer. Difficulties associated with cancer screening include late reporting due to fear, ignorance, cost, and cultural issues. This study sought to establish the utilization of cancer screening services among health workers in Military Hospital Lagos (MHL) and the reasons for poor utilization of such services. Method: This quantitative study utilized 200 participants in MHL, Southwest, Nigeria to collect information. Proportionate probability sampling was used to determine those needed from each department and then conveniently selected after approval was received from the management of the hospital. Data was analyzed using SPSS 25.0 software at 95% CI with an alpha set at 5%. Findings: Participants were mostly males 106 (53.0%), between the age range of 20-30 years 73(36.5%), mostly married 114 (57.0%), with 122(61.0%) possessing a college degree, 90(45.0%) having average income >50-100 thousand naira and 132(66.0%) possessing health insurance. Major factors identified for influencing screening utilization were fear of a positive result, ignorance, belief in not being at risk, having many contending issues, nonchalant attitude to health, financial constraint. Conclusion: A low level of cancer screening and uptake was noticed among these health workers. This raises the need for urgent enlightenment about cancer screening even among health workers, and cancer screening made more available and affordable with easy accessibility to reduce the incidence and mortality of invasive cancer.
Uptake of Cancer Screening among Staff of Military Hospital Lagos
References:
[1] Jedy-Agba E, Curado MP, Ogunbiyi O, Oga E, Fabowale T et al. (2012) Cancer incidence in Nigeria: A report from population-based cancer registries. Cancer Epidemiol. 36(5), 271-8. www.pubmed.ncbi.nlm.nih.gov/22621842/
DOI: 10.1016/j.canep.2012.04.007.
[2] Akram M, Iqbal M, Daniyal M, Khan A U. (2017). Awareness and current knowledge of breast cancer. Biological Research. DOI:10.1186/s40659-017-0140-9.
[3] Odenusi AO, Oladoyin VO, Asuzu MC (2020). Uptake of cervical cancer screening services and its determinants between health and non-health workers in Ibadan, south-Western Nigeria. Afr. J. Med. Med. Sci. 49(4), 573-584.
[4] Arbyn M, Weiderpass E, Bruni L, et al. (2019). Estimates of incidence and mortality of cervical cancer in 2018: a worldwide analysis. Lancet Glob Health. 2022 Jan; 10(1): e41]. Lancet Glob Health. 2020;8 (2): e191-e203. doi:10.1016/S2214-109X (19)30482-6.
[5] Smith RA, Andrews KS, Brooks D, et al (2019). Cancer screening in the United States: a review of current American Cancer Society guidelines and current issues in cancer screening. CA Cancer J Clin. 69:184-210. doi: 10.3322/caac.21557.
[6] Ferlay J, Soerjomataram I, Dikshit R, et al. (2015) Cancer incidence and mortality worldwide: sources, methods, and major patterns in GLOBOCAN 2012. Int J Cancer. 136(5): E359-E386. doi:10.1002/ijc.29210.
[7] Mukhtar R, Mehmood R, Parveen S, Hussain M & Arif M (2015). Prevalence of cervical cancer in a developing country: Pakistan. Global Journal of Medical Research. Vol. 15(3-F). Retrieved from https://medicalresearchjournal.org/index.php/GJMR/article/view/953.
[8] Mema SC, Yang H, Vaska M, Elnitsky S, & Jiang Z. (2016). Integrated Cancer Screening Performance Indicators: A Systematic Review. PloS one, 11(8), e0161187. https://doi.org/10.1371/journal.pone.0161187.
[9] Adeloye D, David RA, Aderemi AV, Iseolorunkanmi A, Oyedokun A, Iweala EE, Omoregbe N, & Ayo CK. (2016). An estimate of the incidence of prostate cancer in Africa: a systematic review and meta-analysis. PLoS One. 11(4): e0153496. https://doi.org/10.1371/journal.pone.0153496S.
[10] Adewole IF, Benedet JL, Crain B, & Follen M. (2006). Evolving a strategic approach to cervical cancer in Africa. Gynecologic oncology. 99. S209-12. 10.1016/j.ygyno.2005.07.086.
[11] Dim CC, Ekwe E, Madubuko T, Dim NR and Ezegwui HU (2009). Improved awareness of Pap smear may not affect its use in Nigeria: a case study of female medical practitioners in Enugu, southeastern Nigeria. Trans R Soc Trop Med Hyg. 103(8):852-854.
[12] Ehiemere I, Frank MD, and Robinson-Bassey G (2015). Attitude and practice of cervical cancer screening among female health workers in University of Port-Harcourt teaching hospital Rivers State. Journal of Research in Nursing and Midwifery. 4(5):72-82.
[13] Oche M, Kaoje A, Gana G, & Ango J (2013). Cancer of the cervix and cervical screening: Current knowledge, attitude, and practices of female health workers in Sokoto, Nigeria. International Journal of Medicine and Medical Sciences. 5(3):106-109.
[14] Goldie SJ, Gaffikin L, Goldhaber-Fiebert JD, et al. (2005). Cost-effectiveness of cervical-cancer screening in five developing countries. N Eng J Med. 353(20):2158-2168.
[15] Duraisamy K, Jaganathan K and Bose JC (2011). Methods of detecting cervical cancer. Advances in Biological Research. 2011;5(4):226-232.
[16] Kuhn L, Denny L, Pollack A, Lorincz A, Richart RM and Wright TC (2000). Human papillomavirus DNA testing for cervical cancer screening in low-resource settings. J Natl Cancer Inst. 92(10):818-825.
[17] Tapera O, Nyakabau A, Simango N, Guzha B, Jombo-Nyakuwa S, Takawira E, Mapanga A, Makosa D, & Madzima B. (2021). Gaps and opportunities for cervical cancer prevention, diagnosis, treatment, and care: evidence from a midterm review of the Zimbabwe cervical Cancer prevention and control strategy (2016–2020). BMC Public Health. 21. 10.1186/s12889-021-11532-y.
[18] Silvera, S. A. N., Bandera, E. V., Jones, B. A., Kaplan, A. M., & Demisse, K. (2020). Knowledge of, and beliefs about, access to screening facilities and cervical cancer screening behaviors among low-income women in New Jersey. Cancer Causes & Control, 31(1), 43-49.
[19] Ilevbare, O. E., Adegoke, A. A., & Adelowo, C. M. (2020). Drivers of cervical cancer screening uptake in Ibadan, Nigeria. Heliyon, 6(3), e03505.
[20] Ugwu E, Obi S, Ezechukwu P, Okafor I & Ugwu A (2013). Acceptability of human papilloma virus vaccine and cervical cancer screening among female health-care workers in Enugu, Southeast Nigeria. Niger J Clin Pract. 16(2):249-252.
[21] Owoeye I & Ibrahim I. (2013). Knowledge and attitude towards cervical cancer screening among female students and staff in a tertiary institution in the Niger Delta. International Journal of Medicine and Biomedical Research. 2(1):48-56.
[22] Hyacinth HI, Adekeye OA, Ibeh JN and Osoba T. (2012). Cervical cancer and pap smear awareness and utilization of pap smear test among Federal civil servants in North Central Nigeria. PLoS One. 7(10): e46583.
[23] Glanz K, Bishop DB. (2012). The role of behavioral science theory in the development and implementation of public health interventions. Annual Review of Public Health. 21:299–418. doi: 10.1146/annurev.publhealth.012809.103604.
[24] Jones CL, Jensen JD, Scherr CL, Brown NR, Christy K., & Weaver J. (2015). The Health Belief Model as an explanatory framework in communication research: exploring parallel, serial, and moderated mediation. Health communication, 30(6), 566–576.
https://doi.org/10.1080/10410236.2013.873363.
[25] Wayne W. LaMorte (2019). https://sphweb.bumc.bu.edu/otlt/mph-modules/sb/behavioralchangetheories/index.html.
[26] Alsulaiman SA & Rentner TL. (2018). The health belief model and preventive measures: A Study of the ministry of a health campaign on coronavirus in Saudi Arabia. Journal of International Crisis and Risk Communication Research, 1(1), 27-56. https://doi.org/10.30658/jicrcr.1.1.3.
[27] Carpenter CJ (2010). A meta-analysis of the effectiveness of the health belief model variables in predicting behavior. Health Communication. 25:661–669. doi: 10.1080/10410236.2010.521906.
[28] Hewitson P, Ward A, Heneghan C. et al. (2011). Primary care endorsement letter and a patient leaflet to improve participation in colorectal cancer screening: results of a factorial randomized trial. Br J Cancer 105, 475–480 (2011). https://doi.org/10.1038/bjc.2011.255.
[29] Vrinten C, Waller J, von Wagner C, & Wardle J. (2015). Cancer fear: facilitator and deterrent to participation in colorectal cancer screening. Cancer epidemiology, biomarkers & prevention: a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology, 24(2), 400–405. https://doi.org/10.1158/1055-9965.EPI-14-0967.
[30] Peters GJY, Ruiter RAC & Kok G. (2013). Threatening communication: a critical re-analysis and a revised meta-analytic test of fear appeal
theory, Health Psychology Review, 7:sup1, S8-S31, DOI: 10.1080/17437199.2012.703527.[31] Keah M, Kombe Y & Ngure K. (2020). Factors Influencing the Uptake of Cervical Cancer Screening among Female Doctors and Nurses in Kenyatta National Hospital. Journal of Cancer and Tumor International. 31-38. 10.9734/jcti/2020/v10i330131.
[32] Adetona AE, Osungbade KO, Akinyemi OO, Obembe TA. (2021) Uptake of Breast Screening Among Female Staff at A Tertiary Health Institution in South-West Nigeria. Journal of Preventive Medicine and Care - 3(2):17-30. https://openaccesspub.org/jcc/article/1115.
[33] Mhamdi SE, Bouanene I, Bouslah A, Sriha A, Salem KB et al. (2011) Breast and cervical cancer screening: Knowledge, attitudes, and practice of health personnel in the region of Monastir (Tunisia). http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L70589843.Trop Med Int Heal. 16, 318.
[34] Arulogun OS & Maxwell OO. (2012) Perception and utilization of cervical cancer screening services among female nurses in University College Hospital, Ibadan., Nigeria. PanAfrMed J 11, 69.
[35] Ndikom CM & Ofi BA. (2012) Awareness, perception and factors affecting utilization of cervical cancer screening services among women in Ibadan, Nigeria: a qualitative study. Reprod Health. 9, 11.
[36] Kumbrija S, Milakoviæ SB, Jeliniæ JD, et al. (2007). Health care professionals—attitudes towards their own health. Acta Med Croatica. 2007;61(1):105-110.
Viewed PDF 1304 25 -
 Occupational Wellness and its Determinants among Cocoa Farmers in South-West NigeriaAuthor: Joseph KuyeDOI: 10.21522/TIJPH.2013.10.01.Art013
Occupational Wellness and its Determinants among Cocoa Farmers in South-West NigeriaAuthor: Joseph KuyeDOI: 10.21522/TIJPH.2013.10.01.Art013Occupational Wellness and its Determinants among Cocoa Farmers in South-West Nigeria
Abstract:
Occupational wellness is essential for cocoa farmers’ health and productivity since a significant proportion of their time is spent at work. It is a measure of individual wellbeing, focusing on the psychosocial status as it relates to individuals’ profession. This study assessed occupational wellness and its determinants among cocoa farmers in the South-West region of Nigeria. A descriptive cross-sectional study design was used to study 244 cocoa farmers in Ekiti and Osun States. Also, the local government areas were purposively selected as being well known for cocoa production. A semi-structured interviewer-administered questionnaire was used to obtain data on sociodemographic characteristics and occupational wellness. Occupational wellness was scored based on their response to eight sets of questions with a 4-point Likert scale response. Association between the farmers’ characteristics and occupational wellness was assessed using Mann Whitney U and Kruskal Wallis tests. Determinants of occupational wellness were assessed using quantile regression. The median occupational wellness score was 25.0 (IQR = 24.0 – 29.0). People of low educational status had higher occupational wellness scores, p < 0.001. Significant associations were also observed between other characteristics like sex, religion, marital status, geographical location, farm ownership, and occupational wellness. Farm ownership was also a significant determinant of occupational wellness. The occupational wellness status is due to a complex mix of occupational factors, sociodemographic factors, and geographic factors. Health promotion will be key in maintaining a balance of the mix to enhance the general wellbeing and productivity of the farmers.
Occupational Wellness and its Determinants among Cocoa Farmers in South-West Nigeria
References:
[1] Occupational Wellness. Retrieved from https://aaep.org/wellness/occupational-wellness.
[2] Occupational Wellness. Retrieved from https://spokane.wsu.edu/wellness/occupational-wellness.
[3] Occupational Wellness. Retrieved from https://www.aquinas.edu/health-wellness/occupational-wellness.
[4] Occupational Wellness Assessment: Profile, Analysis Report and Improvement Plan. Retrieved from https://interpersonalwellness.com/wp-content/uploads/2014/04/Occupational-Wellness-Assessment-2014-04-14.pdf.
[5] Marshall C. (2020). Analysis of a comprehensive wellness program’s impact on job satisfaction in the workplace. International Hospitality Review, 34(2):221-241.
[6] Kabango J (2013). The perceived effects of workplace health promotion programs on job satisfaction at Oserian Development Company. University of Nairobi; 2013.
[7] Richemond D., & Needham C. (2020). The Impact of Wellness Programs on Employee Job Satisfaction in Colleges and Universities. Open Journal of Business and Management, 08:569-599.
[8] Janet J (2014). Psychosocial stress burnout among professional managers in health service institutions. J Indian Journal of Health and Wellbeing, 5(5):539.
[9] Lucia‐Casademunt A.M., Ariza‐Montes J.A., Morales‐Gutiérrez† A.C. (2013). Determinants of occupational well‐being among executive women. Academia Revista Latinoamericana de Administración, 26(2):229-257.
[10] Qi M., Moyle W., Jones C., Weeks B (2019). Physical Activity and Psychological Well-Being in Older University Office Workers: Survey Findings. Workplace Health and Safety, 67(3):123-130.
[11] Afolabi F. (2020). Workplace Health and Safety in the Informal Sector: A Case Study of Nigeria Informal Entrepreneurs. International Conference on Applied Research in Business, Management and Economics.
[12] Aminu F., Ayinde I., Sanusi R. (2020). Multivariate Probit Analysis Of Factors Predisposing Cocoa Farmers To Pesticide Toxicity In Nigeria. Nigerian Journal of Agricultural Economics, 10(2066-2021-965):51-63.
[13] Oludoye O.O., Robson M.G., Siriwong W. (2021). Using the Socio-Ecological Model to Frame the Influence of Stakeholders on Cocoa Farmers’ Pesticide Safety in Nigeria: Findings from a Qualitative Study. Risk Management and Healthcare Policy, 14:2357.
[14] Aminu F. (2020): Pesticide Use And Health Hazards Among Cocoa Farmers: Evidence From Ondo And Kwara States Of Nigeria. Nigeria Agricultural Journal 2020, 51(2):263-273.
[15] Ogunjimi S (2012). Farmers’ knowledge level of precautionary measures in agro-chemicals usage on cocoa production in Osun and Edo States, Nigeria. International Journal of Agriculture and Forestry, 2(4) 186-194.
[16] Abasimi E. (2015) The Relationships among Psychosocial Work Environment, Job Stress Recovery Experiences, Psychological Capital and Occupational Wellbeing: A Study among Nurses and Teachers in the Tamale Metropolis. Ghana: University of Ghana.
[17] Oduwaiye M., Akangbe J., Komolafe S., Ajibola B. (2015). An assessment of knowledge of farming-related hazards and precautionary practices of farmers in Kwara State, Nigeria. Journal of research in forestry, wildlife, and environment, 7(2):27-35.
[18] Akinleye M., Tijani M., Abdulwahab R. (2015). Helmet use as a safety tool among motorcycle riders in ibadan, oyo state, Nigeria. LAUTECH Journal of Engineering and Technology, 9(1):131-138.
[19] Amfo B., Mensah J.O., Aidoo R. (2020). Migrants’ satisfaction with working conditions on cocoa farms in Ghana. J International Journal of Social Economics.
[20] Higuchi A., Coq Huelva D., Arias Gutiérrez R., Alfalla Luque R. (2020). Farmer satisfaction and cocoa cooperative performance: evidence from Tocache, Peru. International Food and Agribusiness Management Review: 23 (2) pg: 217 – 234.
[21] Adewole D., Akanbi S., Osungbade K., Bello S. (2017). Expanding health insurance scheme in the informal sector in Nigeria: awareness as a potential demand-side tool. Pan African Medical Journal 2017, 27.
[22] Zacher H., Schmitt A. (2016). Work Characteristics and Occupational Well-Being: The Role of Age, 7(1411).
Viewed PDF 999 34 -
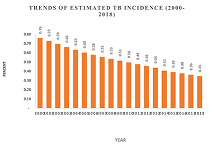 Determinants of Quality of Tuberculosis Services in Lusaka, ZambiaAuthor: Theresa Chansa Chilufya SikateyoDOI: 10.21522/TIJPH.2013.10.01.Art014
Determinants of Quality of Tuberculosis Services in Lusaka, ZambiaAuthor: Theresa Chansa Chilufya SikateyoDOI: 10.21522/TIJPH.2013.10.01.Art014Determinants of Quality of Tuberculosis Services in Lusaka, Zambia
Abstract:
The Zambian government, through the Vision 2030 policy, has prioritized health and is committed to the attainment of ‘equity of access to cost-effective quality health services, as close to the family as possible by providing a continuum of care with particular emphasis on promotional, preventive, curative, and rehabilitation services. This, however, is challenged by the high disease burden of communicable and Non-Communicable Diseases (NCDs) tuberculosis inclusive. This study was conducted to identify and assess determinants of the quality of TB services. The study utilized a cross-sectional design involving a mixed-methods approach consisting of a desk review facility-based survey of patients on TB treatment using quantitative and qualitative data collection techniques. The study covered 352 randomly selected TB patients, 58 conveniently selected TB treatment support persons, 9 purposively selected TB community volunteers, and 6 purposively selected facility-based service providers. The determinants of good quality of TB care include technical performance, access to services, the effectiveness of care, interpersonal relations, the efficiency of service delivery, continuity of service, safety, physical infrastructure, comforts, and choice of service. Results confirm that good health is a function of the quality of healthcare and utilization of healthcare services and service utilization is affected by social demographics of patients such as age, sex, marital status, type of TB treatment support person, inter alia. Patient’s demographic factors determined how the patient view the quality of TB serviced they received.
Determinants of Quality of Tuberculosis Services in Lusaka, Zambia
References:
[1] Global tuberculosis report 2020. Geneva: World Health Organization; 2020. Licence: CC BY-NC-SA 3.0 IGO.MoH (2015), The National Health Strategic Plan (NHSP) 2017-2021, Lusaka. Zambia.
[2] Silva, D.R., Muñoz-Torrico, M., Duarte, R., Galvão, T., Bonini, E.H., Arbex, F.F., Arbex, M.A., Augusto, V.M., Rabahi, M.F. and Mello, F.C.D.Q., 2018. Risk factors for tuberculosis: diabetes, smoking, alcohol use, and the use of other drugs. Jornal Brasileiro de Pneumologia, 44(2), pp.145-152.
[3] NAC. 2019. Global Fund 2020-2022 Allocation Letter. Access online at: http://www.nac.org.zm/ccmzambia/wp-content/uploads/2020/04/Zambia-2020-2022-allocation-letter-signed.pdf on15th December 2020.
[4] Kapata, N., Chanda-Kapata, P., Ngosa, W., Metitiri, M., Klinkenberg, E., Kalisvaart, N., Sunkutu, V., Shibemba, A., Chabala, C., Chongwe, G. and Tembo, M., 2016. The prevalence of tuberculosis in Zambia: results from the first national TB prevalence survey, 2013–2014. PLoS One, 11(1), p.e0146392.
[5] MoH, (2012) NATIONAL HEALTH POLICY “A Nation of Healthy and productive People” Lusaka, Zambia accessed at https://www.moh.gov.zm/docs/healthpolicy.pdf on 26th February 2021.
[6] Swati Sadaphal, Neeraj Kak, Silvia Holschneider, Alisha Smith-Arthur, and Refiloe Matji TB Care II. 2013. Quality Improvement Handbook for TB and MDT-TB. University Research Co., LLC.
[7] WHO consolidated guideline on self-care interventions for health: sexual and reproductive health and rights. Geneva: World Health Organization; 2019. Licence: CC BY-NC-SA 3.0 IGO.
[8] TB CARE I. International Standards for Tuberculosis Care, Edition 3. TB CARE I, The Hague, 2014.
[9] Fecso, A.B., Szasz, P., Kerezov, G. and Grantcharov, T.P., 2017. The effect of technical performance on patient outcomes in surgery. Annals of Surgery, 265(3), pp.492-501.
[10] Masiye, Felix & Kaonga, Oliver. (2016). Determinants of Healthcare Utilisation and Out-of-Pocket Payments in the Context of Free Public Primary Healthcare in Zambia. International Journal of Health Policy and Management. 5. 693-703. 10.15171/ijhpm.2016.65. accessed on https://www.researchgate.net/publication/310050022_Determinants_of_Healthcare_Utilisation_and_Out-of-Pocket_Payments_in_the_Context_of_Free_Public_Primary_Healthcare_in_Zambia/citation/download on 20th January 2021.
[11] Kruk ME, Larson E, Twum-Danso NA. Time for a quality revolution in global health. Lancet Glob Health 2016;4(9): e594–6.
[12] Zyaambo, C., Siziya, S., & Fylkesnes, K. 2012. Health status and socio-economic factors associated with health facility utilization in rural and urban areas in Zambia. BMC health services research, 12, 389. https://doi.org/10.1186/1472-6963-12- Accessed at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3536624/ on 20th January 2021.
[13] Al-Yateem N. (2020) Determinants of Quality of Healthcare for Adolescents and Young Adults. In: Betz C., Coyne I. (eds) Transition from Pediatric to Adult Healthcare Services for Adolescents and Young Adults with Long-term Conditions. Springer, Cham. https://doi.org/10.1007/978-3-030-23384-6_3 https://link.springer.com/chapter/10.1007/978-3-030-23384-6_3 accessed on 3rd December 2020.
[14] Mpaata, Kaziba & Lubogoyi, Bumaali & Okiria, John. (2017). Determinants of Quality of Patients Care in Public Hospitals in Uganda: Requirements for Organizational Effectiveness Clients’ Perspective. International Journal of Science and Research (IJSR). 6. 469-472. 10.21275/ART20172157. Accessed at https://www.researchgate.net/publication/329245439_on 3rd December 2020.
[15] Johnson I, McDonnell C, O’Connell AM, Glynn L. Patient perspectives on health, health needs, and health care services in a rural Irish community: a qualitative study. Rural and Remote Health 2011; 11: 1659. Available: www.rrh.org.au/journal/article/1659 accessed 6th January 2021.
[16] Azuh, D., Ogundipe, A. and Ogundipe, O. 2019, Determinants of Women Access to Healthcare Services in Sub-Saharan Africa; Department of Economics, Development Studies Covenant University, Ota, Ogum, Nigeria; DOI: 10.2174/1874944501912010504 accessed at https://openpublichealthjournal.com/contents/volumes/V12/TOPHJ-12-504/TOPHJ-12-504.pdf on 20th January 2020.
Viewed PDF 1321 32 -
 National Health Insurance Scheme and Health Care Needs of Federal Medical Centre Workers, in Makurdi, Benue State NigeriaAuthor: Comfort Ene OkpeDOI: 10.21522/TIJPH.2013.10.01.Art015
National Health Insurance Scheme and Health Care Needs of Federal Medical Centre Workers, in Makurdi, Benue State NigeriaAuthor: Comfort Ene OkpeDOI: 10.21522/TIJPH.2013.10.01.Art015National Health Insurance Scheme and Health Care Needs of Federal Medical Centre Workers, in Makurdi, Benue State Nigeria
Abstract:
This study assesses the impact of National Health Insurance Scheme on the health care needs of workers in Federal Medical Centre Makurdi, Benue State Nigeria. The data for the study were collected through questionnaires and in-depth interviews. Questionnaires were administered on a sample of 341 respondents. Data analysis was quantitative and qualitative in nature. The specific objectives of the study were to examine the level of awareness about NHIS among the staff of FMC; assess the National Health Insurance healthcare services available in FMC Makurdi; examine the health care needs of the staff of FMC Makurdi; examine the impact of NHIS on health needs of workers in FMC Makurdi; assess the challenges of implementing NHIS in FMC Makurdi and suggest ways of minimising the implementation challenges of NHIS in FMC Makurdi. The analysed results show that, though all the staff of FMC, Makurdi were registered members of the National Health Insurance Scheme, many of them lacked adequate awareness on key issues about the Scheme, Federal Medical Centre Makurdi offers several healthcare services under the NHIS, even though the NHIS was overwhelmingly accepted by staff of FMC Makurdi as having a positive impact on staff of the FMC such as reducing the financial hardship of their medical bills, affordable services and greater access to medical care, the scheme is not perfect. The study therefore, recommends among other that there is need for aggressive awareness programme of the scheme in order to reveal its benefits to all Nigeria citizens.
National Health Insurance Scheme and Health Care Needs of Federal Medical Centre Workers, in Makurdi, Benue State Nigeria
References:
[1] WHO, 1978, Declaration of Alma-Ata, International Conference on Primary Healthcare, Alma-Ata, USSR, http://www.who.int 6-l2.
[2] Apeloko D. O., 2017, “Health Insurance Scheme (NHIS) In Nigeria: An Empirical Survey” International Journal of Politics and Good Governance, 8 (8.4): 1-25.
[3] Gana D., 2010, “Roles of the Healthcare Provider in Health insurance,” Nigeria Medical Association – Annual Conference Paper.
[4] Murray, J. (2007). Origins of American Health Insurance: A History of Industrial Sickness Funds. New Haven, CT, Yale University Press.
[5] Adesina, D. (2009). The National Health Insurance Scheme. Obtained electronically from http://www.thenigeriandoctor.org/news.php?extend.850. Retrieved 15th April 2014.
[6] Femi, T. (2014) “Executive Secretary’s Welcome Notes’, National Health Insurance Scheme [electronic], Available at NHIS website, http://www.nhis.gov.ngindex.php.
[7] Escobar, J. et al (2010). “Isotope Measurement of Ostracod and Gastropod Shells for Climate Reconstruction: Evaluation of Within-Sample Variability and Determination of Optimum Sample size.” J. Paleolimnol. 43 (4).
[8] Ibiwoye, A. &Adeleke, A. (2007). “The Impact of Health Insurance on Healthcare Provision in Developing Countries.” Ghana Journal of Development Studies, 4(21), 49-58.
[9] King, G. et’al (2009). “Public Policy for the Poor? A Randomised Assessment of the Mexican Universal Health Insurance Programme.” Lancet. 373(9673): 1447-54.
[10] Gustafsson-wright, et al., (2013). “A Short-Term Impact Evaluation of Health Insurance Fund Program in Central KwaraState.”Available at http://www.aiid.org/php?id=73&37.
[11] Smith, K.V. and Sulzbach, S. (2008). “Community-Based Health Insurance and Access to Maternal Health Services: Evidence from Three West African Countries.” Social Science & Medicine 66(12), 2460-73.
[12] Agba, M (2010). “Perceived impact of National Health Insurance Schemes (NHIS) Among Registered Staff in Federal Polytechnic ldah, IKogi State, Nigeria.” Studies of Sociology of Science, 1 (1), 44-49.
[13] Dalal, K. and Dawad, S. (2009). “Non-utilization of Public Health care facilities: Examining the Reasons Through a National Study of Women in India.” Rural Remote Health. 9(3):1178.
[14] De Costa, A and Diwan, V. (2007). “Where is the Public Health Sector?’ Public and Private Sector Healthcare Provision in Madhya Pradesh, India.” Health Policy.84(2-3),269-76.
[15] Osuorji E. C. (2005) National Health Insurance Scheme. Obtained electronically from http://www.medikkajournal.com/NHIS.htmRetrieved 15th June 2016 [6] Onyedibe, K., Goyit, M., &Nnadi, N. (2012). “An Evaluation of the National Health Insurance Scheme (NHIS) in Jos, a North Central Nigeria City.” Global Advanced Research Journal of Microbiology, 1(1), 005-012.
[16] Giedion, U. Diaz, B. Y. and Alfonso, E. A. (2007). “The Impact of Subsidized Health Insurance on Access, Utilization and Health Status: The Case of Colombia.” World Bank, Washington, DC.
[17] Obansa, S.A. and Orimisan A. (2013). “Health care financing in Nigeria: Prospects and Challenges. Mediterranean Journal of Social Sciences [Internet]. 2013; 4(1): 221-236. Available at: http://www.mcser.org/images/stories/mjss.january.2013/s.a.j.obansa-helth-care financing.pdf.
[18] WHO, (2000). “World Health Report 2000 – Health Systems Improving Performance.” Health Systems Financing. World Health Organization (WHO), Geneva. Electronically sourced from http://www.who.int.healthsystems/topics/financing/en/On 15/4/2014.
[19] WHO, (2000). Round Table Discussion on Inefficiency and Wastage in the Health Sector. WHO, Geneva.
[20] WHO (2002). “Definition of Health, Preamble to the Constitution of the World Health Organization as Adopted by the International Health Conference, New York, 19–22 June 1946; In Grad, Frank P. (2002). “The Preamble of the Constitution of the World Health Organization”.
Viewed PDF 1332 35 -
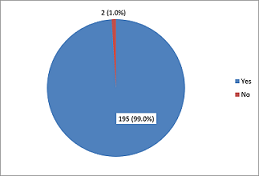 Knowledge, Determinants of Attitude and Willingness for Cosmetic Surgery among Online Media Users in NigeriaAuthor: Tope Michael IpinnimoDOI: 10.21522/TIJPH.2013.10.01.Art016
Knowledge, Determinants of Attitude and Willingness for Cosmetic Surgery among Online Media Users in NigeriaAuthor: Tope Michael IpinnimoDOI: 10.21522/TIJPH.2013.10.01.Art016Knowledge, Determinants of Attitude and Willingness for Cosmetic Surgery among Online Media Users in Nigeria
Abstract:
Cosmetic surgery has become popular in both developed and developing countries. The aim of this study is to identify the level of knowledge, determinants of attitude, and willingness for cosmetic surgery among online media users in Nigeria. A semi-structured online questionnaire was designed on Google forms and was forwarded to respondents via the investigator’s social media networks (Email, WhatsApp, Facebook). Data on socio-demographic characteristics, level of knowledge, attitude, and willingness for cosmetic surgery was collected from one hundred and ninety-seven online users and analyzed using SPSS version 20.0. P-value less than or equal to 0.05 was taken as significant. The mean age of the respondent was 28.0 ± 7.1 years with a male to female ratio of 1:1.4. The majority (91.9%) of the respondents had good knowledge of cosmetic surgery, but 53.0% of the respondents have a positive attitude to cosmetic surgery. More than three-quarters (77.7%) were unwilling to have cosmetic surgery, and satisfaction with body image was the most frequent reason stated. The younger age group, respondents that are Christians, and personal income of above ₦1,000,000 ($2,595.63) per annum were predictors of a positive attitude to cosmetic surgery. The respondents had good knowledge of cosmetic surgery. However, the attitude towards cosmetic surgery was relatively poor. Factors such as age, religion, ethnic affiliation, and income were important determinants of the attitude towards cosmetic surgery.
Knowledge, Determinants of Attitude and Willingness for Cosmetic Surgery among Online Media Users in Nigeria
References:
[1] Harris DL. Cosmetic surgery-where does it begin?. British Journal of Plastic Surgery. 1982; 35:281-86.
[2] Atiyeh BS, Rubiez MT, Hayek SN. Aesthetic/ cosmetic surgery and ethical challenges. Aesthetic Plast Surg. 2008; 32:829-39. doi:10.1007/s00266-008-9246-3.
[3] Crockett RJ ,Pruzansky T PJ. The influence of plastic surgery “Reality Tv” shows on cosmetic surgery patient’s expectations and decision making. Plast Reconstr Surg. 2007;120:316–24.
[4] American Society for Aesthetic Plastic Surgery. 2016 Cosmetic Surgery National Data Bank Statistics. 2016. Available at http://www.surgery.org/ sites/default/files/ASAPS-Stats2016.pdf (Last accessed 18 August 2020).
[5] BBC News. Big rise in cosmetic surgery ops. 2006. Available at http://news.bbc.co.uk/2/hi/health/4609166.stm (Last accessed 18 August 2020).
[6] Arab K, Barasain O, Altaweel A, Alkhayyal J, Alshiha L, Barasain R et al. Influence of Social Media on the Decision to Undergo a Cosmetic Procedure. Plast Reconstr Surg Glob Open. 2019 Aug; 7(8): e2333.
[7] Hopkins ZH, Moreno C, Secrest AM,.Influence of Social Media on Cosmetic Procedure Interest. J Clin Aesthet Dermatol. 2020 Jan; 13(1): 28–31.
[8] Patil SB, Kale SM, Khare N, Jaiswal S, Ingole S. Aesthetic surgery: Expanding horizons: Concepts, desires, and fears of rural women in central India. Aesthetic Plast Surg. 2011;35:717–23. doi:10.1007/s00266-011-9675-2.
[9] Xing, India: Chamber for Foreign Trade, per capita income.
http://www.xing.com/app/forum/seoparser/icfft/news-244442/ India-per-capita-income-up-at-rs-33-283-17882502/ (Last accessed 30 August 2020).
[10] Bidkhori M, Yaseri M, Sari AA, Majdzadeh R. Relationship between Socioeconomic Factors and Incidence of Cosmetic Surgery in Tehran, Iran. Iran J Public Health. 2021 Feb; 50(2): 360–368.doi: 10.18502/ijph. v50i2.5351.
[11] Yoon S, Kim YA. Cosmetic Surgery and Self-esteem in South Korea: A Systematic Review and Meta-analysis. Aesthetic Plast Surg. 2020;44:229–38. doi:10.1007/s00266-019-01515-1.
[12] Abubakar AI, Jamda MA, Ibrahim A, Ajani A, Iyun K, Opara KO. University students and cosmetic surgery in Nigeria: A survey of perception, attitudes, and experiences. Niger J Plast Surg. 2016;12:12-16.
[13] Holcomb JD, Gentile RD. Aesthetic facial plastic surgery of male patients: demographics and market trends. Facial Plast Surg. 2005; 21:223-31.
[14] Henderson-king D, Brooks KD. Materialism, Sociocultural Appearance Messages, And Paternal Attitudes Predict College Women’s Attitudes About Cosmetic Surgery. Psychology of Women Quarterly. 2009;33:133–42.
[15] Sinno S, Lam G, Brownstone ND, Steinbrech DS. An Assessment of Gender Differences in Plastic Surgery Patient Education and Information in the United States: Are We Neglecting Our Male Patients? Aesthetic Surgery Journal, Volume 36, Issue 1, January 2016, Pages 107–110, https://doi.org/10.1093/asj/sjv100.
[16] Adedeji OA, Oseni GO, Olaitan PB. Awareness and Attitude of Healthcare Workers to Cosmetic Surgery in Osogbo, Nigeria. Surgery Research and Practice 2014; 2014:1-8 doi:10.1155/2014/869567.
[17] Adeyemo WL, Mofikoya BO, Bamgbose BO. Knowledge and perceptions of facial plastic surgery among a selected group of professionals in Lagos, Nigeria. J Plast Reconstr Aesthetic Surg. 2010;63:578–82. doi:10.1016/j.bjps.2009.01.046.
[18] Al Doheyan T, Al-Saad A, Al Haidar A, Al Fwzan H, Al Askar J, Al Malki F et al. Attitude and Practices Concerning Cosmetic Surgery among Female Medical Students at the University Hospital, King Saud University, Riyadh, Saudi Arabia. British Journal of Medicine & Medical Research. 2016 14(4): 1-10.
[19] Bank TW. Poverty head counts ratio. 2020. Available from:
https://data.worldbank.org/indicator/SI.POV.NAH?locations=BG&most_recent_year_desc=false (Last accessed 15 September 2020).
[20] Muslu Ü, Demir E. The Effect of Religious Beliefs on the Attitude of Aesthetic Surgery Operation in Islam. J Relig Health. 2019;59:804–15. doi:10.1007/s10943-019-00767-0.
[21] Atiyeh BS, Kadry M, Hayek SN et al. Aesthetic Surgery and Religion: Islamic Law Perspective. Aesth Plast Surg 32, 1–10 (2008). https://doi.org/10.1007/s00266-007-9040-7.
Viewed PDF 1196 40 -
 Pain Experience and Coping Strategies Employed by Women in Labor in a Secondary Health Facility in Ilorin, Kwara State, NigeriaAuthor: Onasoga, Olayinka ADOI: 10.21522/TIJPH.2013.10.01.Art017
Pain Experience and Coping Strategies Employed by Women in Labor in a Secondary Health Facility in Ilorin, Kwara State, NigeriaAuthor: Onasoga, Olayinka ADOI: 10.21522/TIJPH.2013.10.01.Art017Pain Experience and Coping Strategies Employed by Women in Labor in a Secondary Health Facility in Ilorin, Kwara State, Nigeria
Abstract:
Labour pain experience is distinctive and complex, and women use various coping strategies to cope with it. Hence, this study attempted to explore pain experience and coping strategies employed by women in labor in a secondary health facility in Ilorin, Kwara State, Nigeria. A qualitative exploratory research design was used, and a purposive sampling technique was used to select a total of ten (10) mothers who delivered within 48hours in the healthcare facility. A total of three FGD sessions were conducted, each had between 3 and 4 participants. The semi-structured interview guide was used for data collection, and the data were analyzed using content analysis. The women who participated in this study were between 20 and 42years of age, and they perceived labour pain differently. Some of the women described labour pain as very painful; others said the pain is normal, while some said the pain cannot be compared with anything. The study revealed that younger women who are primiparous perceived labor pain as more severe than the multiparous women. All the participants said that birth information and instructions received from the midwives, as well as the presence of caring midwives, help to relieve labour pains and consequently influence their pain experience(s) positively. The coping strategies used varied among participants, and deep breathing techniques, relaxation, and vertical positions were the major coping strategies used. Therefore, the provision of adequate labour information on coping strategies and the presence of caring midwives influenced the labour experience(s) positively.
Pain Experience and Coping Strategies Employed by Women in Labor in a Secondary Health Facility in Ilorin, Kwara State, Nigeria
References:
[1] Akadri, A. A., & Odelola, O. I. (2018). Labour pain perception: experiences of Nigerian mothers. Pan African Medical Journal, 30(1). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6320448/.
[2] Makvandi, S., Mirzaiinajmabadi, K., Mirteimoori, M., & Esmaily, H. (2018). Effect of normal physiologic childbirth program in mother-friendly hospitals on the duration of labor. Electronic Journal of General Medicine, 15(3). https://www.ajol.info/index.php/jfas/article/view/169254.
[3] Shnol, H., Paul, N., & Belfer, I. (2014). Labor pain mechanisms. International anesthesiology clinics, 52(3), 1-17 https://journals.lww.com/anesthesiaclinics/Citation/2014/05230/Labor_Pain_Mechanisms.2.aspx.
[4] Obuna, J. A., & Umeora, O. U. J. (2014). Perception of labor pain and utilization of obstetric analgesia by Igbo women of Southeast Nigeria. Journal of Obstetric Anaesthesia and Critical Care, 4(1), 18-32
https://www.joacc.com/article.asp?issn=2249-4472;year=2014;volume=4;issue=1;spage=18;epage=22;aulast=Obuna.
[5] Asl, B. M. H., Vatanchi, A., Golmakani, N., & Najafi, A. (2018). Relationship between behavioral indices of pain during labor pain with pain intensity and duration of delivery. Electronic physician, 10(1), 6240.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5854000/.
[6] Whitburn, L. Y., Jones, L. E., Davey, M. A., & Small, R. (2017). The meaning of labour pain: how the social environment and other contextual factors shape women’s experiences. BMC Pregnancy and Childbirth, 17(1), 1-10. https://doi.org/10.1186/s12884-017-1343-3.
[7] Aziato, L., Acheampong, A. K., & Umoar, K. L. (2017). Labour pain experiences and perceptions: a qualitative study among post-partum women in Ghana. BMC Pregnancy and Childbirth, 17(1), 1-9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5322618/.
[8] Polit, D.F., & Beck, C.T. (2018). Essentials of nursing research. Appraising evidence for nursing practice (9th ed.). Philadelphia: Wolters Kluwer Health.
[9] Kongsuwan, W., & Chatchawet, W. (2021). Level of Labor Pain, Level of Labor Pain Behaviors, and Cultural Pain Behaviors among First-Time Indonesian Muslim Mothers. Open Journal of Obstetrics and Gynecology, 11(01), 27. https://www.scirp.org/journal/paperinformation.aspx?paperid=106687.
[10] Labor, S., & Maguire, S. (2008). The pain of labour. Reviews in Pain, 2(2), 15-19. https://journals.sagepub.com/doi/10.1177/204946370800200205.
[11] Onasoga, O.A., Aluko J. O., Afolayan, J. A., & Bakare G. Y (2019) Compliance with Labour and Birth Information among Postnatal Women Attending General Hospital Ilorin. African Journal of Behavioural and Scale Development Research. 1(1): 37-44.
[12] Duncan, L. G., Cohn, M. A., Chao, M. T., Cook, J. G., Riccobono, J., & Bardacke, N. (2017). Benefits of preparing for childbirth with mindfulness training: a randomized controlled trial with active comparison. BMC pregnancy and childbirth, 17(1), 1-11. https://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/s12884-017-1319-3.
[13] Tahereh, F.N., Robab, L. R., & Hossein, E. (2017). The best encouraging persons in labor: A content analysis of Iranian mothers’ experiences of labor support. Plos one, 12(7), e0179702. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5499987/.
[14] Karlsdottir, S. I., Halldorsdottir, S., & Lundgren, I. (2014). The third paradigm in labour pain preparation and management: the childbearing woman’s paradigm. Scandinavian journal of caring sciences, 28(2), 315-327. https://pubmed.ncbi.nlm.nih.gov/23815344/.
[15] Hodnett, E. D., Gates, S., Hofmeyr, G. J., & Sakala, C. (2013). Continuous support for women during childbirth. Cochrane database of systematic reviews, (7). https://pubmed.ncbi.nlm.nih.gov/23857334/.
[16] Lebni, J. Y., Farahani, F. K., Solhi, M., & Azar, F. E. F. (2021). Causes and Grounds of Childbirth Fear and Coping Strategies Used by Kurdish Adolescent Pregnant Women in Iran: A Qualitative Study. Journal of Reproduction & Infertility, 22(1), 47. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7903670/.
[17] Mamba, N., & Tagutanazvo, O. B. (2021). First-time mothers’ experiences of the first stage of labour in hospitals in the HhoHho region, Eswatini. African Journal of Midwifery and Women’s Health, 15(1), 1-8. https://www.magonlinelibrary.com/doi/abs/10.12968/ajmw.2020.0013.
[18] Campbell, V., & Nolan, M. (2019). ‘It definitely made a difference: a grounded theory study of yoga for pregnancy and women’s self-efficacy for labour. Midwifery, 68, 74-83. https://eprints.worc.ac.uk/7307/1/Campbell%20V%252c%20Nolan%20M%252c%20It%20definitely%20made%20a%20difference.pdf.
[19] Wharton, K. R., Ecker, J. L., & Wax, J. R. (2017). Approaches to limit intervention during labor and birth. Committee Opinion No. 687. American College of Obstetricians and Gynecologists. Obstet Gynecol, 129, e20-e28. https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2019/02/approaches-to-limit-intervention-during-labor-and-birth.
[20] Newnham, E., Karlsdottir, S. I., & Sanders, R. (2019). Humanising of Childbirth: re-envisaging labour pain: a humanistic approach. The Practising Midwife, 22(10), 14-17. https://ueaeprints.uea.ac.uk/id/eprint/80275/1/Accepted_Manuscript.pdf.
[21] Thomson, G., Feeley, C., Moran, V. H., Downe, S., & Oladapo, O. T. (2019). Women’s experiences of pharmacological and non-pharmacological pain relief methods for labour and childbirth: a qualitative systematic review. Reproductive health, 16(1), 1-20. https://pubmed.ncbi.nlm.nih.gov/31146759/. Viewed PDF 1485 62 -
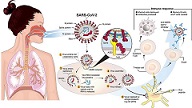 Covid-19 in Nigeria: Lockdown Measures and a Chronological Epidemiological Review During the First WaveAuthor: Idowu OluwafemiDOI: 10.21522/TIJPH.2013.10.01.Art018
Covid-19 in Nigeria: Lockdown Measures and a Chronological Epidemiological Review During the First WaveAuthor: Idowu OluwafemiDOI: 10.21522/TIJPH.2013.10.01.Art018Covid-19 in Nigeria: Lockdown Measures and a Chronological Epidemiological Review During the First Wave
Abstract:
This study provides a general epidemiological review of Corona-virus disease in Nigeria during the first wave of the pandemic from February to December 2020 and the efforts of the Federal Government of Nigeria (FGN) to curtail the disease. Coronavirus disease is a highly transmissible and pathogenic viral disease caused by severe acute respiratory syndrome-coronavirus 2(SARS-CoV2), which emerged in Wuhan, China, in December 2019 and later spread worldwide. The first confirmed case of the disease in Nigeria was in February 2020, and the subject was an Italian who works in Nigeria but returned from Milan, Italy to Lagos, after which the virus spread to other parts of the country. In order to curtail the spread of the menace, lockdown measures were introduced by the FGN during the first wave since there is no precise treatment for the disease, thus making prevention critical. Despite these measures, the spread of Covid-19 in Nigeria continues to record a significant surge beyond the first wave.
Covid-19 in Nigeria: Lockdown Measures and a Chronological Epidemiological Review During the First Wave
References:
[1] Hu, B., Guo. H., Zhou, P. and Shi., Z., 2021, Characteristics of SARS-CoV-2 and Covid-19. Nature Reviews Microbiology, 19(3),141-154. doi: 10.1038/s41579-020-00459-7.
[2] Latinne, A. et al., 2020, Origin and cross-species transmission of bat coronaviruses in China Nature Communications, 11(1),4235. doi: 10.1038/s41467-020-17687-3.
[3] Zhu, H., Wei, L. and Niu, P., 2020, The novel coronavirus outbreak in Wuhan, China. Global Health Research and Policy, 5(1),1–3. doi.org/10.1186/s41256-020-00135-6.
[4] World Health Organization, 2021, WHO-convened global study of oigins of SARS-CoV-2’, Infectious Disease Immunology, Publish Ah(February). doi: 10.1097/id9.0000000000000017.
[5] Wiersinga, W. J, et al., 2020, Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (Covid-19): A Review’, JAMA – Journal of the American Medical Association, 324(8),782-793. doi: 10.1001/jama.2020.12839.
[6] World Health Organization, 2021, Statement for healthcare professionals: How Covid-19 vaccines are regulated for safety and effectiveness. https://www.who.int/news/item/11-06-2021-statement-for-healthcare-professionals-how-covid-19-vaccines-are-regulated-for-safety-and-effectiveness (accessed January 10, 2022).
[7] World Health Organization, 2020, Rational use of personal protective equipment for coronavirus disease 2019 (Covid-19). World Health Organization, 2019(February), pp. 1–7. Available at: https://apps.who.int/iris/bitstream/handle/10665/331695/WHO-2019-nCov-IPC_PPE_use-2020.3-eng.pdf.
[8] Corman, V.M., Muth, D., Niemeyer, D. and Drosten, C., 2018, Hosts and sources of endemic human coronaviruses Advance in Virus Research, 100,163-188. doi: 10.1016/bs.aivir.2018.01.001.
[9] Cui, J., Li, F., Shi, Z.L., 2019, Origin and evolution of pathogenic coronaviruses. Nature Reviews Microbiology, 17(3),181-192. doi: 10.1038/s41579-018-0118-9.
[10] Yang, Y., 2020, The deadly cronaviruses: The 2003 SARS pandemic and the 2020 novel coronavirus epidemic in china, The company’s public news and information Journal of Autoimmunity 109, p. 102487.Available at: https://www.sciencedirect.com/science/article/pii/S0896841120300470?via%3Dihub.
[11] Abdool, K., Salim, S. and de Oliveira, T., 2021, New SARS-CoV-2 variants-clinical, public health, and vaccine implications New England Journal of Medicine Massachusetts, 384(19),1866-1868.
[12] Centers for Disease Control and Prevention., 2021, New Covid-19 Variants. [First published 11 February 2020].
[13] Lauring, A. S. and Hodcroft, E. B., 2021, Genetic variants of SARS-CoV-2-What do they mean? . Journal of the American Medical Association, 325(6),529–531.
[14] Swelum, A.A. et al., 2020, ‘Covid-19 in Human, animal, and environment: A review’, Frontiers in Veterinary Science, 7:1-13. doi: 10.3389/fvets.2020.00578.
[15] Lauer, S.A., et al., 2020, The incubation period of coronavirus disease 2019 (Covid-19) from publicly reported confirmed cases: Estimation and application. Annals of Internal fMedicine, 172(9),577–582. doi: 10.7326/M20-0504.
[16] Paul, S. and Lorin, E., 2021, Distribution of incubation periods of Covid-19 in the Canadian context Science Reports, 11(1):1–9. doi: 10.1038/s41598-021-91834-8.
[17] Funk, C.D., Laferrière, C. and Ardakani, A, 2020, Transmission and life cycle of SARS-CoV-2 causing Covid-19. https://en.wikipedia.org/wiki/COVID-19#/media/File:Fphar-11-00937-g001.jpg.
[18] Islam, M.A., 2021, “Prevalence and characteristics of fever in adult and paediatric patients with coronavirus disease 2019 (COVID-19): A systematic review and meta-analysis of 17515 patients PLOS ONE. 16 (4): e0249788.
[19] Agyeman, A.A, et al., 2020, Smell and taste dysfunction in patients with COVID-19: A systematic review and meta-analysis Mayo Clinic Proceedings, 95(8),1621–1631.
[20] Saniasiaya, J., Islam, M. A., and Abdullah., B., 2020. Prevalence and characteristics of taste disorders in cases of COVID-19: A meta-analysis of 29,349 Patients. Otolaryngology–Head and Neck Surgery 165 (1):33-42.
[21] Centers for Disease Control and Prevention U.S, 2020a, “Interim clinical guidance for management of patients with confirmed coronavirus disease (Covid-19)”.
[22] Centers for Disease Control and Prevention U.S. (2020b). https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html (accessed January 10, 2022).
[23] Reuters, 2020, Italian with coronavirus in Nigeria was not isolated for almost 24 hours. www.reuters.com/article/us-china-health-nigeria-idUSKCN20M07D.
[24] Okoroiwu, H.U, Ogar, C.O., Nja, G.M.E., Abunimye, D.A. and Ejemot-Nwadiaro, R.I, 2021, Covid-19 in nigeria: Account of epidemiological events, response, management, preventions and lessons learned. Germs 11:391–402. https://doi.org/10.18683/germs.2021.1276.
[25] World Health Organization, 2021, Covid-19 weekly epidemiological update, edition 56, 7 September 2021.
[26] International Monitoring Fund, 2021, Policy Responses to Covid-19. Imf 2020:1–189. https://www.imf.org/en/Topics/imf-and-covid19/Policy-Responses-to-Covid-19 (accessed February 10, 2022)
[27] Milibari, A.A, 2020, iMedPub Journals Current Situation of Coronavirus Disease : Albaraa A Milibari 10–3. https://doi.org/10.36648/1791-809X.S1.005.
[28] Organisation for Economic Cooperation and Development (OECD), 2020, The territorial impact of Covid-19 : Managing The Crisis Across Levels of Government. Organ Fo Econ Coop Dev 2020:2–44.
Viewed PDF 1127 30 -
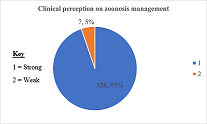 Leptospirosis Diagnostic Capacity in Public Health Facilities within Nairobi County, KenyaAuthor: Niala Isaiah OrodiDOI: 10.21522/TIJPH.2013.10.01.Art019
Leptospirosis Diagnostic Capacity in Public Health Facilities within Nairobi County, KenyaAuthor: Niala Isaiah OrodiDOI: 10.21522/TIJPH.2013.10.01.Art019Leptospirosis Diagnostic Capacity in Public Health Facilities within Nairobi County, Kenya
Abstract:
The presence of biotic and abiotic reservoirs is a possible indicator of leptospirosis occurrence in Nairobi County, which has a large proportion of informal settlements. Despite these epidemiological risk factors, little or no attention is accorded to leptospirosis. The study assessed the degree of leptospirosis diagnostic capacity in public health facilities within Nairobi County, Kenya. A descriptive cross-sectional study involving 133 clinicians and 15 laboratory personnel across 15 public health facilities was conducted between August and December 2019. The perception of zoonotic management was high as 95% (126) had a strong score while 5% (7) had a weak score. Healthcare facility level (χ2 (3) = 14.09, p < 0.05), professional designation (χ2 (1) = 4.26, p < 0.05) had a significant association with suspecting zoonosis. The length of service as a clinician was a significant predictor of suspecting zoonosis, Wald = 11.11, p < 0.05. Inter-agency collaboration was low as 89% (119) reported a lack of sharing zoonosis information, and only 8% (10) indicated that there was information sharing. The clinical suspicion index was low, 3.8% of the participants suspected the disease in practice, and 2.3% would consider leptospirosis in the differential diagnosis of FUO. All 15 public health facilities lacked leptospirosis laboratory diagnostic capacity. The probable diagnosis of leptospirosis is low due to a low clinical suspicion index and lack of awareness. There is a lack of laboratory diagnostic capacity. Sensitisation of clinicians and laboratory personnel is critical in increasing the diagnostic capacity of leptospirosis.
Leptospirosis Diagnostic Capacity in Public Health Facilities within Nairobi County, Kenya
References:
[1] Haake, D. A., & Levett, P. N. (2014). Leptospirosis in humans. Current Topics in Microbiology and Immunology, 65-97. https://doi.org/10.1007/978-3-662-45059-8_5.
[2] Costa, F., Hagan, J. E., Calcagno, J., Kane, M., Torgerson, P., Martinez-Silveira, M. S., Stein, C., Abela-Ridder, B., & Ko, A. I. (2015). Global morbidity and mortality of leptospirosis: A systematic review. PLOS Neglected Tropical Diseases, 9(9), e0003898. https://doi.org/10.1371/journal.pntd.0003898.
[3] Wuthiekanun, V., Sirisukkarn, N., Daengsupa, P., Sakaraserane, P., Sangkakam, A., Chierakul, W., Smythe, L. D., Symonds, M. L., Dohnt, M. F., Slack, A. T., Day, N. P., & Peacock, S. J. (2007). Clinical diagnosis and geographic distribution of leptospirosis, Thailand. Emerging Infectious Diseases, 13(1), 124-126. https://doi.org/10.3201/eid1301.060718.
[4] Mgode, G. F., Machang’u, R. S., Mhamphi, G. G., Katakweba, A., Mulungu, L. S., Durnez, L., Leirs, H., Hartskeerl, R. A., & Belmain, S. R. (2015). Leptospira Serovars for diagnosis of leptospirosis in humans and animals in Africa: Common leptospira isolates and reservoir hosts. PLOS Neglected Tropical Diseases, 9(12), e0004251. https://doi.org/10.1371/journal.pntd.0004251.
[5] Halliday, J. E., Allan, K. J., Ekwem, D., Cleaveland, S., Kazwala, R. R., & Crump, J. A. (2015). Endemic zoonoses in the tropics: A public health problem hiding in plain sight. Veterinary Record, 176(9), 220-225. https://doi.org/10.1136/vr.h798.
[6] Gebreyes, W. A., Dupouy-Camet, J., Newport, M. J., Oliveira, C. J., Schlesinger, L. S., Saif, Y. M., Kariuki, S., Saif, L. J., Saville, W., Wittum, T., Hoet, A., Quessy, S., Kazwala, R., Tekola, B., Shryock, T., Bisesi, M., Patchanee, P., Boonmar, S., & King, L. J. (2014). The global one health paradigm: Challenges and opportunities for tackling infectious diseases at the human, animal, and environment interface in low-resource settings. Plos Neglected Tropical Diseases, 8(11), e3257. https://doi.org/10.1371/journal.pntd.0003257.
[7] Halliday, J., Daborn, C., Auty, H., Mtema, Z., Lembo, T., Bronsvoort, B. M., Handel, I., Knobel, D., Hampson, K., & Cleaveland, S. (2012). Bringing together emerging and endemic zoonoses surveillance: Shared challenges and a common solution. Philosophical Transactions of the Royal Society B: Biological Sciences, 367(1604), 2872-2880. https://doi.org/10.1098/rstb.2011.0362.
[8] Adler, B., & de la Peña Moctezuma, A. (2010). Leptospira and leptospirosis. Veterinary Microbiology, 140(3-4), 287-296. https://doi.org/10.1016/j.vetmic.2009.03.012.
[9] De Brito, T., Silva, A. M., & Abreu, P. A. (2018). Pathology and pathogenesis of human leptospirosis: A commented review. Revista do Instituto de Medicina Tropical de São Paulo, 60(0). https://doi.org/10.1590/s1678-9946201860023.
[10] Faisal, S. M., McDonough, S. P., & Chang, Y. (2012). Leptospira: Invasion, pathogenesis and persistence. The Pathogenic Spirochetes: strategies for evasion of host immunity and persistence, 143-172. https://doi.org/10.1007/978-1-4614-5404-5_88.
[11] Crump, J. A., Morrissey, A. B., Nicholson, W. L., Massung, R. F., Stoddard, R. A., Galloway, R. L., Ooi, E. E., Maro, V. P., Saganda, W., Kinabo, G. D., Muiruri, C., & Bartlett, J. A. (2013). Etiology of severe non-malaria febrile illness in northern Tanzania: A prospective cohort study. PLoS Neglected Tropical Diseases, 7(7), e2324. https://doi.org/10.1371/journal.pntd.0002324.
[12] Biggs, H. M., Hertz, J. T., Munishi, O. M., Galloway, R. L., Marks, F., Saganda, W., Maro, V. P., & Crump, J. A. (2013). Estimating leptospirosis incidence using hospital-based surveillance and a population-based health care utilization survey in Tanzania. PLoS Neglected Tropical Diseases, 7(12), e2589. https://doi.org/10.1371/journal.pntd.0002589.
[13] Fischer, R. S., & Flores Somarriba, B. (2017). Challenges to diagnosing leptospirosis in endemic regions require urgent attention. Current Tropical Medicine Reports, 4(2), 57-61. https://doi.org/10.1007/s40475-017-0110-x.
[14] Destoumieux-Garzón, D., Mavingui, P., Boetsch, G., Boissier, J., Darriet, F., Duboz, P., Fritsch, C., Giraudoux, P., Le Roux, F., Morand, S., Paillard, C., Pontier, D., Sueur, C., & Voituron, Y. (2018). The one health concept: 10 Years old and a long road ahead. Frontiers in Veterinary Science, 5. https://doi.org/10.3389/fvets.2018.00014.
[15] llan, K. J., Biggs, H. M., Halliday, J. E., Kazwala, R. R., Maro, V. P., Cleaveland, S., & Crump, J. A. (2015). Epidemiology of leptospirosis in Africa: A systematic review of a neglected zoonosis and a paradigm for ‘One health’ in Africa. PLOS Neglected Tropical Diseases, 9(9), e0003899. https://doi.org/10.1371/journal.pntd.0003899.
[16] Lau, C. L., Smythe, L. D., Craig, S. B., & Weinstein, P. (2010). Climate change, flooding, urbanisation and leptospirosis: Fuelling the fire? Transactions of the Royal Society of Tropical Medicine and Hygiene, 104(10), 631-638. https://doi.org/10.1016/j.trstmh.2010.07.002.
[17] Torgerson, P. R., Hagan, J. E., Costa, F., Calcagno, J., Kane, M., Martinez-Silveira, M. S., Goris, M. G., Stein, C., Ko, A. I., & Abela-Ridder, B. (2015). Global burden of leptospirosis: Estimated in terms of disability adjusted life years. PLOS Neglected Tropical Diseases, 9(10), e0004122. https://doi.org/10.1371/journal.pntd.0004122.
[18] Musso, D., & La Scola, B. (2013). Laboratory diagnosis of leptospirosis: A challenge. Journal of Microbiology, Immunology and Infection, 46(4), 245-252. https://doi.org/10.1016/j.jmii.2013.03.001.
[19] Durski, K., Jancloes, M., Chowdhary, T., & Bertherat, E. (2014). A global, multi-disciplinary, multi-sectorial initiative to combat leptospirosis: Global leptospirosis environmental action network (GLEAN). International Journal of Environmental Research and Public Health, 11(6), 6000-6008. https://doi.org/10.3390/ijerph110606000.
[20] De Vries, S. G., Visser, B. J., Nagel, I. M., Goris, M. G., Hartskeerl, R. A., & Grobusch, M. P. (2014). Leptospirosis in sub-Saharan Africa: A systematic review. International Journal of Infectious Diseases, 28, 47-64. https://doi.org/10.1016/j.ijid.2014.06.013.
[21] Baer, R., Turnberg, W., Yu, D., & Wohrle, R. (2009). Leptospirosis in a small animal veterinarian: Reminder to follow standardized infection control procedures. Zoonoses and Public Health, 57(4), 281-284. https://doi.org/10.1111/j.1863-2378.2009.01240.x.
[22] Bett, B., Said, M. Y., Sang, R., Bukachi, S., Wanyoike, S., Kifugo, S. C., Otieno, F., Ontiri, E., Njeru, I., Lindahl, J., & Grace, D. (2017). Effects of flood irrigation on the risk of selected zoonotic pathogens in an arid and semi-arid area in the eastern Kenya. Plos One, 12(5), e0172626. https://doi.org/10.1371/journal.pone.0172626.
[23] Cook, E. A., De Glanville, W. A., Thomas, L. F., Kariuki, S., Bronsvoort, B. M., & Fèvre, E. M. (2016). Risk factors for leptospirosis seropositivity in slaughterhouse workers in western Kenya. Occupational and Environmental Medicine, 74(5), 357-365. https://doi.org/10.1136/oemed-2016-103895.
[24] Munyua, P., Bitek, A., Osoro, E., Pieracci, E. G., Muema, J., Mwatondo, A., Kungu, M., Nanyingi, M., Gharpure, R., Njenga, K., & Thumbi, S. M. (2016). Prioritization of zoonotic diseases in Kenya, 2015. Plos One, 11(8), e0161576. https://doi.org/10.1371/journal.pone.0161576.
[25] De Geus, A., Wolff, J. W., & Timmer, V. E. A. (1977). Clinical leptospirosis in Kenya, II. A field study in Nyanza Province. East African medical journal, 54(3), 125-132. https://www.cabdirect.org/cabdirect/abstract/19792903083.
[26] Wachira, B. W., & Smith, W. (2013). Major incidents in Kenya: The case for emergency services development and training. Prehospital and Disaster Medicine, 28(2), 170-173. https://doi.org/10.1017/s1049023x13000010
[27] Halliday, J. E., Knobel, D. L., Allan, K. J., De C. Bronsvoort, B. M., Handel, I., Agwanda, B., Cutler, S. J., Olack, B., Ahmed, A., Hartskeerl, R. A., Njenga, M. K., Cleaveland, S., & Breiman, R. F. (2013). Urban leptospirosis in Africa: A cross-sectional survey of leptospira infection in rodents in the Kibera urban settlement, Nairobi, Kenya. The American Journal of Tropical Medicine and Hygiene, 89(6), 1095-1102. https://doi.org/10.4269/ajtmh.13-0415.
[28] Harris, P. A., Taylor, R., Thielke, R., Payne, J., Gonzalez, N., & Conde, J. G. (2009). Research electronic data capture (Redcap)—A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 42(2), 377-381. https://doi.org/10.1016/j.jbi.2008.08.010.
[29] Slotved, H., Yatich, K. K., Sam, S. O., & Ndhine, E. O. (2017). The capacity of diagnostic laboratories in Kenya for detecting infectious diseases. Tropical Medicine and Health, 45(1). https://doi.org/10.1186/s41182-017-0049-6.
[30] Bandara, K. K., Gunasekara, C. P., Weerasekera, M. M., Ranasinghe, N., Hapugoda, M., Marasinghe, C., & Fernando, N. (2016). Comparison of three rapid diagnostic assays for diagnosis of leptospirosis in a resource-poor setting. https://doi.org/10.20959/wjpr20167-6634.
[31] Kumar, S. S. (2013). Indian guidelines for the diagnosis and management of human leptospirosis. Medicine Update, 2013.
[32] Ahmad, S. N., Shah, S., & Ahmad, F. H. (2005). Laboratory diagnosis of leptospirosis. Journal of postgraduate medicine, 51(3), 195. https://www.jpgmonline.com/article.asp?issn=0022-3859;year=2005;volume=51;issue=3;spage=195;epage=200;aulast=Ahmad.
[33] Gunasekara, C. P., Sumaiha, M. H. F., Damayanthi, M. K. S., Weerasekara, M. M., & Fernando, S. S. N. (2017). Utility of a modified silver staining technique for detection of Leptospira. https://sljid.sljol.info/articles/abstract/10.4038/sljid.v7i2.8142/.
[34] Mohamad Safiee, A. W., Mohd Ali, M. R., Fauzi, M. H., Muhd Besari, A., Yean Yean, C., Neela, V. K., & Ismail, N. (2020). Leptospiral Culture without 5’-Fluorouracil Revealed Improved Leptospira Isolation from Febrile Patients in North-Eastern Malaysia. International journal of environmental research and public health, 17(4), 1307. https://doi.org/10.3390/ijerph17041307
[35] Rao, M., Amran, F., & Aqilla, N. (2019). Evaluation of a rapid kit for detection of IgM against Leptospira in human. Canadian Journal of Infectious Diseases and Medical Microbiology, 2019. https://doi.org/10.1155/2019/5763595.
[36] Odhiambo, F., Galgalo, T., Wences, A., Muchemi, O. M., Kanyina, E. W., Tonui, J. C., ... & Boru, W. (2014). Antimicrobial resistance: capacity and practices among clinical laboratories in Kenya, 2013. The Pan African Medical Journal, 19. https://doi.org/10.11604/pamj.2014.19.332.5159.
[37] Kariuki, S., & Dougan, G. (2014). Antibacterial resistance in sub-Saharan Africa: an underestimated emergency. Annals of the New York Academy of Sciences, 1323(1), 43. https://doi.org/10.1111/nyas.12380.
[38] Onsare, R. S., Micoli, F., Lanzilao, L., Alfini, R., Okoro, C. K., Muigai, A. W., ... & Rondini, S. (2015). Relationship between antibody susceptibility and lipopolysaccharide O-antigen characteristics of invasive and gastrointestinal nontyphoidal Salmonellae isolates from Kenya. Plos neglected tropical diseases, 9(3), e0003573. https://doi.org/10.1371/journal.pntd.0003573.
Viewed PDF 1341 31 -
 An Assessment of the Factors that Contribute to Non-Adherence to Ant-Retroviral Therapy (Art) Treatment among HIV Patients at Nchanga North General Hospital-Chingola, ZambiaAuthor: Judith MusondaDOI: 10.21522/TIJPH.2013.10.01.Art020
An Assessment of the Factors that Contribute to Non-Adherence to Ant-Retroviral Therapy (Art) Treatment among HIV Patients at Nchanga North General Hospital-Chingola, ZambiaAuthor: Judith MusondaDOI: 10.21522/TIJPH.2013.10.01.Art020An Assessment of the Factors that Contribute to Non-Adherence to Ant-Retroviral Therapy (Art) Treatment among HIV Patients at Nchanga North General Hospital-Chingola, Zambia
Abstract:
The research study was aimed at assessing the factors that contribute to non-adherence to Ant-Retroviral Therapy (ART) treatment among HIV patients at Nchanga North General Hospital-Chingola. With regards to the objectives, they were to establish the individual factors, social-cultural factors, social-economic factors, environmental factors, and health care provider factors contributing to non-adherence to Ant-Retroviral Therapy (ART) treatment among HIV patients. A descriptive cross-sectional design that was quantitative in nature was used for the study. The study targeted 162 non-adherent patients. In collecting data, structured questionnaires were used. A purposive sampling technique was used to select 115 respondents. The collected data was entered into data sets and analysed using Statistical Package for Social Sciences (
SPSS) version 23.0 software to dissolve the portents and to evaluate the extent of ART non-adherence amongst male patients. The study concluded that non- adherence at Nchanga North Hospital is brought about by factors such as individual factors, social-cultural factors, social-economic factors, environmental factors, and health care provider factors. The research recommends that patient’s preventive interventions such as community adherence supporter programs ought to be developed and implemented for the purposes of improving and ensuring ART adherence. An Assessment of the Factors that Contribute to Non-Adherence to Ant-Retroviral Therapy (Art) Treatment among HIV Patients at Nchanga North General Hospital-Chingola, Zambia
References:
[1] UNAIDS., 2012, UNAIDS Report on the global AIDS epidemic. Accessed 11 Jan 2022 from https://www.unaids.org/en/resources/documents/2019/2019-UNAIDS-data.
[2] Zambian Demographic Health Survey (2018). Zambia Statistics Agency, Ministry of health. Accessed 3 Jan 2022 from http://www.zamstats.gov.zm/phocadownload/Demography/ZDHS%20Key%20Indicator%20Report%202018.pdf.
[4] Lane, N. S., 2021, How Close Are We to a Cure for HIV? Accessed 2 Jan 2022 from https://www.verywellhealth.com/cure-for-hiv-5088720.
[5] Sasaki, Y., Kakimoto, K., Dube, C. et al. 2012, Adherence to antiretroviral therapy (ART) during the early months of treatment in rural Zambia: influence of demographic characteristics and social surroundings of patients. Annals of Clinical Microbiology and Antimicrobials 11(34), 202-228. https://doi.org/10.1186/1476-0711-11-34.
[6] Boateng D., Kwapong, G. D., Agyei-Baffour, P., 2013, Knowledge, perception about antiretroviral therapy (ART) and prevention of mother-to-child-transmission (PMTCT) and adherence to ART among HIV positive women in the Ashanti Region, Ghana: a cross-sectional study. BMC Women’s Health, 13: 2-8. Doi: http://dx.doi.org/10.4314/thrb.v20i4.x.
[7] Skovdal, M., Campbell, C., Nhongo, K., Nyamakupa, C., & Gregson, S., 2011, Contextual and psychosocial influences on antiretroviral therapy adherence in rural Zimbabwe: towards a systematic framework or progamme planners. International Journal of Health Planning and Management, 1(26), 296-318. https://doi.org/10.1177/1359105318788692.
[8] Monjok, E., Smesny, A., Okokon, I. B., Mgbere, O., & Essien, E. J., 2010, Adherence to antiretroviral therapy in Nigeria: an overview of research studies and implications for policy and practice. HIV/AIDS - Research and Palliative Care, 2, 69 - 76. doi: 10.2147/hiv. s9280
[9] Mbuagbaw, L., Thabane, L., Ongolo-Zogo, P. et al., 2012, Trends and determining factors associated with adherence to antiretroviral therapy (ART) in Cameroon: a systematic review and analysis of the CAMPS trial. AIDS Res Ther 9(37), 9-37, https://doi.org/10.1186/1742-6405-9-37.
[11] Mwanza, D., 2020, HIV/AIDS Patients’ Adherence to Antiretroviral Therapy at Chawama Hospital. Lusaka, UNZA Press.
[13] Hanass-Hancock J, Bond V, Solomon P, Cameron C, Maimbolwa M, Menon A, and Nixon S., 2020, Perspectives on ART adherence among Zambian adults living with HIV: insights raised using HIV-related disability frameworks. AIDS Care, 32(5), 623-629. doi: 10.1080/09540121.2019.1653441.
[14] National AIDS Council., 2013, Hiv and Aids situation. Retrieved January 11, 2022, from National Aids Council Website: https://www.nac.org.zw.
[15] Jones, D., Cook, R., Spence, A., Weiss, S. M. and Chitalu, N., 2014, Antiretroviral Therapy in Zambia: Do Partners on ART Enhance Adherence? Journal of the International Association of Providers of AIDS Care, 13(6), 497-500. https://doi.org/10.1177/2325957414553843.
[16] Yamanie, T. (1964). Statistics: An Introductory Analysis. Portland: Hamper and Row Publishers.
[19] Koe, W.-L. (2016). The Relationship between Individual Entrepreneurial Orientation (IEO) and Entrepreneurial Intention. Journal of Global Entrepreneurship Research, 6(13), 121-132. https://doi.org/10.1186/s40497-016-0057-8.
[21] Fisher, J. D., Fisher, W. A., Amico, K. R., & Harman, J. J. (2016). An information-motivation-behavioral skills model of adherence to antiretroviral therapy. Health Psychology, 25(4), 462-473. doi:10.1037/0278-6133.25.4.462.
[22] Nozaki, I., Dube, C., Kakimoto, K., Yamada, N. and Simpungwe, J. B., 2011, Social factors affecting ART adherence in rural settings in Zambia, AIDS Care, 23:7, 831-838, DOI: 10.1080/09540121.2010.542121.
[23] Langebeek, N, Gisolf, E.H, Reiss, P, et al., 2014, Predictors and correlates of adherence to combination antiretroviral therapy (ART) for chronic HIV infection: a meta-analysis. BMC Med, 12(1), 142-156. doi:10.1186/preaccept-1453408941291432.
[24] Birbeck, G. L., Kvalsund, M. P., Byers, P. A., Bradbury, R., Mang’ombe, C., Organek, N., Kaile T., Sinyama, A. M., Sinyangwe, S. S., Malama, K., Malama, C., 2011, Neuropsychiatric and socioeconomic status impact antiretroviral adherence and mortality in rural Zambia. AmJTrop Med Hyg, 85 (4), 782-789. 10.4269/ajtmh.2011.11-0187.
[25] Basti, B. D., Mahesh, V., Bant, D. D., & Bathija, G. V., 2017, Factors affecting antiretroviral treatment adherence among people living with human immunodeficiency virus/acquired immunodeficiency syndrome: A prospective study. Journal of family medicine and primary care, 6(3), 482–486. https://doi.org/10.4103/2249-4863.222014.
[26] Altice, F. L., Mostashari, F., & Friedland, G. H. (2001). Trust and the Acceptance of and Adherence to Antiretroviral Therapy. JAIDS Journal of Acquired Immune Deficiency Syndromes, 28(1), 47-58. DOI:10.1097/00042560-200109010-00008.
Viewed PDF 1173 28 -
 Perception and Hypertension Prevention Practices of Teachers in selected Secondary Schools in Sagamu Local Government Area Ogun State, NigeriaAuthor: Raymond S DankoliDOI: 10.21522/TIJPH.2013.10.01.Art021
Perception and Hypertension Prevention Practices of Teachers in selected Secondary Schools in Sagamu Local Government Area Ogun State, NigeriaAuthor: Raymond S DankoliDOI: 10.21522/TIJPH.2013.10.01.Art021Perception and Hypertension Prevention Practices of Teachers in selected Secondary Schools in Sagamu Local Government Area Ogun State, Nigeria
Abstract:
Prevention of Hypertension is important for reducing the high prevalence and incidence of Hypertension and can help reduce resultant morbidities and consequences of cardiovascular disorders. This study assessed the perception of teachers on hypertension prevention in selected secondary schools in Sagamu Local Government Area, Ogun State, Nigeria. The study employed a descriptive cross-sectional design. A Multi-stage sampling technique was used to select 418 respondents for the study. A validated semi-structured questionnaire was used for data collection. Descriptive and inferential statistics was used to analyze the data collected at ≤0.05 level of significance. The respondents had a mean age of 42.61±7.79 years, with 313 (74.9%) of them having a bachelor’s degree. The respondents’ perception of hypertension prevention measured on a 72-point rating scale showed that the respondents had a mean score of 47.10±8.48. Most 225(53.8%) of the respondents had a moderate perception of hypertension prevention. The respondents’ hypertension prevention practices measured on a 24-point rating scale showed that the respondents had a mean score of 15.34±4.95. Less than half 184(44.0%) of the respondents had moderate hypertension prevention practices. Furthermore, there is a significant relationship between respondents’ perception and their hypertension prevention practice. The study revealed that the majority of the respondents had moderate perception of Hypertension and moderate prevention practices of Hypertension. It is recommended that the state ministry of education through the state ministry of health should conduct health education and promotion programs among teachers to change their perception of hypertension prevention which will, in turn, influence their prevention practices.
Perception and Hypertension Prevention Practices of Teachers in selected Secondary Schools in Sagamu Local Government Area Ogun State, Nigeria
References:
[1] Chruściel, P., Stemplewska, P., Stemplewski, A., Wattad, M., Bielecka-Dąbrowa, A., Maciejewski, M., Penson, P., Bartlomiejczyk, M., and Banach, M. 2019, Associations between the lipid profile and the development of hypertension in young individuals – the preliminary study. Archives of Medical Science. 16. 10.5114/aoms.2019.86197.
[2] World Health Organization, 2019. Hypertension. Accessed 20/6/2021 https://www.who.int/news-room/fact-sheets/detail/hypertension.
[3] Okubadejo, N., Ozoh, O., Ojo, O., Akinkugbe, A., Odeniyi, I., Adegoke, O., Bello, B., and Agabi, O. 2019, Prevalence of hypertension and blood pressure profile amongst urban-dwelling adults in Nigeria: a comparative analysis based on recent guideline recommendations. Clinical Hypertension, 25,7.
[4] Ogah, O., and Rayner, B. 2013, Recent advances in Hypertension in sub-Saharan Africa. Heart, 99(19),1390–1397. Doi. 10.1136/heartjnl-2012-303227.
[5] Hendriks, M., Wit, F., Roos, M., Brewster, L., Akande, T., de Beer, H., et al.,2012, Hypertension in Sub-Saharan Africa: cross-sectional surveys in four rural and urban communities,” PLoS ONE, 7(3), e32638.
[6] Vijayakumar, S, Laxmi, A., Pasula, S, Adepuk, K & Mahamood, A 2013, Prevalence awareness and control of Hypertension in school teachers in Warangal, Andhra Pradesh India. International Journal of Biological and Medical Research, 4(2); 3247-3249.
[7] Wjayathunge, L., and Hettiaratchi, U. 2017, Assessment of Knowledge and risk factors of Hypertension among school teachers in the selected district in North Central Province of Sri-Lanka. International Journal of Scientific and Research Publication, 7(11); 404-408.
[8] Bariua, R., Alam, M., Parvin, N., and Chowdhary, R .2018, Prevalence of Hypertension and its risk factors among school teachers in Dhaka Bangladesh. International Journal of Research in Medical science, 6(9); 2902-2910.
[9] Rosenstock, I. M., Strecher, V. J., and Becker, M. H. 1988, Social Learning Theory and the Health Belief Model. Health Education Quarterly, 15(2), 175–183. https://doi.org/10.1177/109019818801500203.
[10] Ajewole, I., Fasoro, A., and Agbana, R. 2017, Awareness of Hypertension among Public Secondary School Teachers in a Local Government Area of Ekiti State, Nigeria International Journal of Medical Research and Applications, 1(2); 05-09.
[11] Famuyiwa, S.A., 2019, Knowledge, Attitude and Hypertension at Risk Behaviour of Secondary School Teachers in Oluyole Local Government of Oyo State, Nigeria. Ibadan Journal of Educational Studies. 16 (2).
[12] Amanyire, J., Tumwebaze, M., Mugisha, M., and Bright, L. 2019, Prevalence and risk factors for Hypertension, diabetes, and obesity among Lecturers and Support Staff of Bishop Stuart University in Mbarara, Uganda. Open Journal of Applied Sciences, 9, 126-137. doi: 10.4236/ojapps.2019.93012.
[13] Mini, G. K., Sarma, P. S., Priya, C., and Thankappan, K. R, 2020, Control of Hypertension among teachers in schools in Kerala (CHATS-K), India. Indian heart journal, 72(5), 416–420. https://doi.org/10.1016/j.ihj.2020.06.005.
[14] Mirzaei, M., Mirzaei, M., and Bagheri, B. 2020, Awareness, treatment, and control of Hypertension and related factors in adult Iranian population. BMC Public Health 20, 667 https://doi.org/10.1186/s12889-020-08831-1.
[15] Abiy, T. A., and Teketel, E. 2019, Lifestyle modification practice and associated factors among diagnosed hypertensive patients in Mizan Tepi University Teaching Hospital Southwest Ethiopia, cross-sectional study. Pan African Medical Journal-Clinical Medicine, 2,156, 1-7. Doi; 1011604/pamj-cm.2020.2156.22010.
[16] Fikadu, G., and Lemma, S. 2016, Socioeconomic status and Hypertension among Teachers and Bankers in Addis Ababa, Ethiopia. International Journal of Hypertension, 4143962. https://doi.org/10.1155/2016/4143962.
[17] Abdullahi, A.A., and Amzat, J. 2011, Knowledge of Hypertension among the staff of University of Ibadan, Nigeria. Journal of Public Health and Epidemiology, 3, 204-209.
[19] Hussain, O.J., and Ajuwon, A. J., 2020, Prevalence, Knowledge and preventive practices against Hypertension among police officers in Ibadan. Annals of Ibadan postgraduate medicine, 18(2), 114–121.
[20] Annadurai, K., 2018, Awareness and preventive practices related to Hypertension among government school teachers in rural Tamil Nadu. Journal of Comprehensive Health, 6(1), 09 - 13. https://doi.org/10.53553/JCH.v06i01.003.
[21] Oladapo, O.O., Salako, L., Sadiq, L., Soyinka, K., and Falase, A.O., 2013, Knowledge of Hypertension and other Risk Factors for Heart Disease among Yoruba Rural Southwestern Nigerian Population. British Journal of Medicine & Medical Research; 3: 993‐1003.
[22] Demaio, A., Otogntuga, D., Courten, M., Bygbjerg, I, Enkhtuya, P., Meyrowitsch, D., and Oyunbileg, J., 2013, Hypertension and hypertension-related disease in Monogolia; findings of a national knowledge, attitude & practices study. BMC Public Health, 13, 194. http://doi.org//10.118611471-2458-13-194.
Viewed PDF 1222 24 -
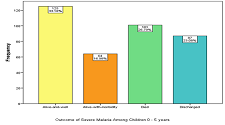 Assessing Health Workers’ Adherence to the National Guidelines for Diagnosis and Treatment of Severe Malaria in Children (0-5 Years) - A Cross-Sectional Study of Hospitals in Kebbi State, NigeriaAuthor: Manir Hassan JegaDOI: 10.21522/TIJPH.2013.10.01.Art022
Assessing Health Workers’ Adherence to the National Guidelines for Diagnosis and Treatment of Severe Malaria in Children (0-5 Years) - A Cross-Sectional Study of Hospitals in Kebbi State, NigeriaAuthor: Manir Hassan JegaDOI: 10.21522/TIJPH.2013.10.01.Art022Assessing Health Workers’ Adherence to the National Guidelines for Diagnosis and Treatment of Severe Malaria in Children (0-5 Years) - A Cross-Sectional Study of Hospitals in Kebbi State, Nigeria
Abstract:
Adherence to treatment guidelines for severe malaria (SM) is a vital component of malaria control strategies. Non-compliance with treatment guidelines has implications on effective SM case management, particularly in children. The study aimed to assess Health workers’ adherence to the National Treatment Guideline for Diagnosis and Treatment of SM in children. A retrospective audit of patients’ records treated for SM from 1st January 2018 to 30th December 2019 was carried out through data abstraction in 5 General hospitals in Kebbi state. Also, questionnaires were distributed to health workers to assess their knowledge of the treatment guideline. Data from the hospitals were analyzed using SPSS version 23.0 and evaluated for HW’s adherence to treatment guidelines in the management of SM cases. A total of 377 cases of severe malaria (SM) were identified. All the cases (100%) were tested for malaria, with RDT being the commonest (60.2%) technique used, while 71 (18.83%) cases received intra-artesunate, 24 (6.36%) received intravenous quinine, and 41 (19.80%) received a follow-up dose of ACT. From the 50 health workers sampled, 38 (76%) of the responders established laboratory confirmation for SM, and all (100%) the responders had received one or more pieces of training on malaria treatment, with 28 (56%) respondents confirming the availability of National Treatment Guidelines for Diagnosis and Treatment of malaria. Findings suggest good compliance with the National Guidelines for Diagnosis and Treatment of severe malaria. However, there is a need to ensure the availability of a copy of the Guidelines in hospitals to sustain the present adherence observed.
Assessing Health Workers’ Adherence to the National Guidelines for Diagnosis and Treatment of Severe Malaria in Children (0-5 Years) - A Cross-Sectional Study of Hospitals in Kebbi State, Nigeria
References:
[1] Mousa A, Al-Taiar A, Anstey NM, Badaut C, Barber BE, Bassat Q, et al.2020. The impact of delayed treatment of uncomplicated P. falciparum malaria on progression to severe malaria: A systematic review and a pooled multicentre individual-patient meta-analysis. PLOS Medicine. 2020;17 (10): e1003359. https://doi.org/10.1371/journal.pmed.1003359.
[2] WHO. Severe malaria. 2014.Trop Med Int Health. 2014 Sep;19 Suppl 1:7-131. DOI: 10.1111/tmi.12313_2. PMID: 25214480.
[3] Gething, P.W., Battle, K.E., Bhatt, S. et al. 2014. Declining malaria in Africa: improving the measurement of progress. Malar J 13, 39 (2014). https://doi.org/10.1186/1475-2875-13-39.
[4] Nkumama IN, O’Meara WP, Osier FHA. Changes in Malaria Epidemiology in Africa and New Challenges for Elimination. Trends Parasitol. 2017;33(2):128-140. doi:10.1016/j.pt.2016.11.006.
[5] Adela Budimu, Basiliana Emidi, Sixbert Mkumbaye, Debora C. Kajeguka, “Adherence, Awareness, Access, and Use of Standard Diagnosis and Treatment Guideline for Malaria Case Management among Healthcare Workers in Meatu, Tanzania”, Journal of Tropical Medicine, vol. 2020, ArticleID 1918583, 6 pages, 2020. https://doi.org/10.1155/2020/1918583.
[6] World Health Organization. 2020. Malaria key facts. https://www.who.int/news-room/fact-sheets/detail/malaria. Accessed on 1st January 2022.
[7] Severe Malaria observatory. 2020. Severe Malaria Criteria, Features & Definition. https://www.severemalaria.org/severe-malaria/severe-malaria-criteria-features-definition. Accessed on 15th December 2021.
[8] World Health Organization. (2015). Guidelines for the treatment of malaria, 3rd ed. World Health Organization. https://apps.who.int/iris/handle/10665/16244.
[9] Guidelines for the Treatment of Malaria. 2010. 2nd ed. Geneva: World Health Organization; 2010. PMID: 25473692.
[10] Zurovac D, Githinji S, Memusi D, et al. 2014. Major improvements in the quality of malaria case-management under the “test and treat” policy in Kenya. PLoS One. 2014;9(3): e92782. Published 2014 Mar 24. DOI: 10.1371/journal.pone.0092782.
[11] Zurovac D, Ndhlovu M, Rowe AK, Hamer DH, Thea DM, Snow RW. 2005. Treatment of paediatric malaria during a period of drug transition to artemether-lumefantrine in Zambia: cross-sectional study. BMJ. 2005 Oct 1;331(7519):734. DOI: 10.1136/bmj.331.7519.734. PMID: 16195289; PMCID: PMC1239975.
[12] Hensen B, Paintain LS, Shretta R, Bruce J, Jones C, Webster J. Taking stock; provider prescribing practices in the presence and absence of ACT stock. Malar J. 2011; 10:218. DOI: 10.1186/1475-2875-10-218.
[13] Mangham LJ, Cundill B, Ezeoke O, Nwala E, Uzochukwu C, Wiseman V, Onwujekwe O. Treatment of uncomplicated malaria at public health facilities and medicine retailers in southeastern Nigeria. Malar J. 2011; 10:155. DOI: 10.1186/1475-2875-10-155.
[14] Meremikwu M, Okomo U, Nwachukwu C, Oyo-Ita A, Eke-Njoku J, Okebe J, Oyo-Ita E, Garner P. Antimalarial drug prescribing practice in private and public health facilities in south-east Nigeria: a descriptive study. Malar J. 2007; 6:55. DOI: 10.1186/1475-2875-6-55.
[15] Ezenduka CC, Okonta MJ, Esimone CO. Adherence to treatment guidelines for uncomplicated malaria at two public health facilities in Nigeria; Implications for the ‘test and treat’ policy of malaria case management. J Pharm Policy Pract. 2014;7(1):15. Published 2014 Nov 14. doi:10.1186/2052-3211-7-15.
[16] Mubi, M., Kakoko, D., Ngasala, B. et al. Malaria diagnosis and treatment practices following the introduction of rapid diagnostic tests in Kibaha District, Coast Region, Tanzania. Malar J 12, 293 (2013). https://doi.org/10.1186/1475-2875-12-293.
[17] K. Bruxvoort, C. Festo, M. Cairns et al., 2015. “Measuring patient adherence to malaria treatment: a comparison of results from self-report and a customised electronic monitoring device,” PLoS One, vol. 10, https://go.gale.com/ps/i.do?id=GALE%7CA423309685&sid=googleScholar&v=2.1&it=r&linkaccess=abs&issn=19326203&p=AONE&sw=w&userGroupName=anon%7E4408d840. Accessed on 12th December 2021.
[18] Bamiselu, O.F., Ajayi, I., Fawole, O. et al. 2016. Adherence to malaria diagnosis and treatment guidelines among healthcare workers in Ogun State, Nigeria. BMC Public Health 16, 828 (2016). https://doi.org/10.1186/s12889-016-3495-x.
[19] M. Nanyingi, “Adherence to laboratory findings in the management of malaria in the high and low transmission areas of Nakasongola and Kabalore Districts of Uganda,” Health policy development, vol. 6, pp. 164–172, 2008. http://www.bioline.org.br/request?hp08019. Accessed on 10th November 2021.
[20] Bawate, C., Callender-Carter, S.T., Nsajju, B. et al. 2016. Factors affecting adherence to national malaria treatment guidelines in the management of malaria among public healthcare workers in Kamuli District, Uganda. Malar J 15, 112 (2016). https://doi.org/10.1186/s12936-016-1153-5.
[21] Philllips-Howard PA, Wannemuehler KA, Ter Kuile FO, Hawley WA, Kolczak MS, Odhacha A, Vulule JM, Nahlen B: Diagnostic and prescribing practices in peripheral health facilities in rural Western Kenya. Am J Trop Med Hyg. 2003, 68 (Suppl 4): 44-49. http://dx.doi.org/10.4269/ajtmh.2003.68.44.
[22] Achan J, Tibenderana J, Kyabayinze D, Mawejje H, Mugizi R, Mpeka B, et al. 2011. Case management of severe malaria–a forgotten practice: experiences from health facilities in Uganda. Plos one. 2011.DOI: 10.1371/journal.pone. 0017053.s006.
[23] Federal Republic of Nigeria. 2005. National Antimalarial Treatment Policy. Abuja, Nigeria: FMOH, National Malaria, and Vector Control Division; 2005. https://extranet.who.int/countryplanningcycles/sites/default/files/country_docs/Nigeria/nigeria_draft_malaria_strategic_plan_2009-2013.pdf. Accessed on 5th November 2021.
[24] Mangham LJ, Cundill B, Ezeoke O, Nwala E, Uzochukwu C, Wiseman V, Onwujekwe O. 2011. Treatment of uncomplicated malaria at public health facilities and medicine retailers in southeastern Nigeria. Malar J. 2011; 10:155. DOI: 10.1186/1475-2875-10-155.
[25] Onwujekwe O, Uzochukwu B, Dike N, Uguru N, Nwobi E, Shu E. 2009. Malaria treatment perceptions, practices, and influences on provider behaviour: comparing hospitals and non-hospitals in south-east Nigeria. Malar J. 2009; 8:246. DOI: 10.1186/1475-2875-8-246.
[26] Nwaneli EI, Eguonu I, Ebenebe JC, Osuorah CDI, Ofiaeli OC, Nri-Ezedi CA.2020. Malaria prevalence and its sociodemographic determinants in febrile children - a hospital-based study in a developing community in South-East Nigeria. Journal of preventive medicine and hygiene. 2020;61(2): E173-e80. DOI: https://dx.doi.org/10.15167%2F2421-4248%2Fjpmh2020.61.2.1350.
[27] Breman JG. 2001. The ears of the hippopotamus: manifestations, determinants, and estimates of the malaria burden. Am J Trop Med Hyg. 2001 Jan-Feb;64(1-2 Suppl):1-11. DOI: 10.4269/ajtmh.2001.64.1. PMID: 11425172.
[28] Kwenti, T.E., Kwenti, T.D.B., Latz, A. et al. 2017. Epidemiological and clinical profile of paediatric malaria: a cross-sectional study performed on febrile children in five epidemiological strata of malaria in Cameroon. BMC Infect Dis 17, 499 (2017). https://doi.org/10.1186/s12879-017-2587-2.
[29] Ezenduka, C. C., Okonta, M. J., & Esimone, C. O. 2014. Adherence to treatment guidelines for uncomplicated malaria at two public health facilities in Nigeria; Implications for the ‘test and treat’ policy of malaria case management. Journal of pharmaceutical policy and practice, 7(1), 15. https://doi.org/10.1186/2052-3211-7-15.
[30] Chuma J, Abuya T, Memusi D, Juma E, Akhwale W, Ntwiga J, Nyandigisi A, Tetteh G, Shretta R, Amin A. 2009.Reviewing the literature on access to prompt and effective malaria treatment in Kenya: implications for meeting the Abuja targets. Malar J. 2009; 8:243. DOI: 10.1186/1475-2875-8-243.
[31] Wikipedia. Kebbi State from Wikipedia, the free encyclopedia. https://en.m.wikipedia.org/wiki/Kebbi_State. Accessed on 2nd October 2021.
[32] Bamgboye EA. 2013. Sample size determination in: Lecture notes on research methodology in the health and medical sciences. Ibadan. Folbam publishers. 2013:168-96. https://www.npmj.org/article.asp?issn=1117-1936;year=2020;volume=27;issue=2;spage=67;epage=75;aulast=Bolarinwa. Accessed on 17th September 2021.
[33] Ayieko, P., Irimu, G., Ogero, M. et al.2019. Effect of enhancing audit and feedback on uptake of childhood pneumonia treatment policy in hospitals that are part of a clinical network: a cluster randomized trial. Implementation Sci 14, 20 (2019). https://doi.org/10.1186/s13012-019-0868-4.
[34] Irimu G, Ogero M, Mbevi G, Agweyu A, Akech S, Julius T, et al. 2018. Approaching quality improvement at scale: a learning health system approach in Kenya. BMJ. 2018; 103:1013–9. DOI: 10.1093/cid/ciz844.
[35] Mangham LJ, Cundill B, Ezeoke O, Nwala E, Uzochukwu C, Wiseman V, Onwujekwe O: 2011. Treatment of uncomplicated malaria at public health facilities and medicine retailers in southeastern Nigeria. Malar J. 2011, 10: 155-10.1186/1475-2875-10-155. doi:10.1186/1475-2875-10-155.
[36] Meremikwu, M., Okomo, U., Nwachukwu, C. et al. 2007. Antimalarial drug prescribing practice in private and public health facilities in South-east Nigeria: a descriptive study. Malar J 6, 55 (2007). https://doi.org/10.1186/1475-2875-6-55.
[37] Ezenduka CC, Ogbonna BO, Ekwunife OI, Okonta MJ, Esimone CO: Drugs use pattern for uncomplicated malaria in retail medicine outlets in Enugu urban, southeast Nigeria: implications for malaria treatment policy. Malar J. 2014, 13: 243-10.1186/1475-2875-13-243. doi:10.1186/1475-2875-13-243.
[38] National Population Commission of Nigeria. 2006. National Bureau of Statistics (web). https://www.citypopulation.de/php/nigeria-admin.php?adm1id=NGA022. Accessed on 2nd January 2022.
[39] Neumann CG, Bwibo NO, Siekmann JH, McLean ED, Browdy B, Drorbaugh N. 2008. Comparison of blood smear microscopy to a rapid diagnostic test for in-vitro testing for P. falciparum malaria in Kenyan school children. East Afr Med J. 2008 Nov;85(11):544-9. DOI: 10.4314/eamj. v85i11.9670.
[40] Endeshaw, T., Gebre, T., Ngondi, J. et al. 2008. Evaluation of light microscopy and rapid diagnostic test for the detection of malaria under operational field conditions: a household survey in Ethiopia. Malar J 7, 118 (2008). https://doi.org/10.1186/1475-2875-7-118.
[41] Wongsrichanalai C, Barcus MJ, Muth S, Sutamihardja A, Wernsdorfer WH. 2007. A review of malaria diagnostic tools: microscopy and rapid diagnostic test (RDT). Am J Trop Med Hyg. 2007 Dec;77(6 Suppl):119-27. PMID: 18165483.
[42] Manyando, C., Njunju, E.M., Chileshe, J. et al. 2014. Rapid diagnostic tests for malaria and health workers’ adherence to test results at health facilities in Zambia. Malar J 13, 166 (2014). https://doi.org/10.1186/1475-2875-13-166.
[43] Batwala, V., Magnussen, P. & Nuwaha, F. 2011. Comparative feasibility of implementing rapid diagnostic test and microscopy for parasitological diagnosis of malaria in Uganda. Malar J 10, 373 (2011). https://doi.org/10.1186/1475-2875-10-373.
[44] Bamiselu, O.F., Ajayi, I., Fawole, O. et al. 2016. Adherence to malaria diagnosis and treatment guidelines among healthcare workers in Ogun State, Nigeria. BMC Public Health 16, 828 (2016). https://doi.org/10.1186/s12889-016-3495-x.
[45] Uzochukwu BS, Chiegboka LO, Enwereuzo C, Nwosu U, Okoroafor D, Onwujekwe OE, Uguru NP, Sibeudu FP, Ezeoke OP: Examining appropriate diagnosis and treatment of malaria: availability and use of rapid diagnostic tests and artemisinin-based combination therapy in public and private health facilities in southeast Nigeria. BMC Public Health. 2010, 10: 486-10.1186/1471-2458-10-486.
[46] Ampadu HH, Asante KP, Bosomprah S, Akakpo S, Hugo P, Gardarsdottir H, Leufkens HGM, Kajungu D, Dodoo ANO. 2019. Prescribing patterns and compliance with World Health Organization recommendations for the management of severe malaria: a modified cohort event monitoring study in public health facilities in Ghana and Uganda. Malar J. 2019 Feb 8;18(1):36. DOI: 10.1186/s12936-019-2670-9. PMID: 30736864; PMCID: PMC6368732.
[47] Tetteh, M., Dwomoh, D., Asamoah, A. 2019. et al. Impact of malaria diagnostic refresher training programme on competencies and skills in malaria diagnosis among medical laboratory professionals: evidence from Ghana 2015–2019. Malar J 20, 255 (2021). https://doi.org/10.1186/s12936-021-03796-x.
[48] Moura, S., Fançony, C., Mirante, C. et al. 2014. Impact of a training course on the quality of malaria diagnosis by microscopy in Angola. Malar J 13, 437 (2014). https://doi.org/10.1186/1475-2875-13-437.
[49] Addo KK, Yeboah-Manu D, Dan-Dzide M, Owusu-Darko K, Caulley P, Mensah GI, Minamikawa M, Lienhardt C, Bonsu FA, Ofori-Adjei D. 2010. Diagnosis of tuberculosis in ghana: the role of laboratory training. Ghana Med J. 2010 Mar;44(1):31-6. DOI: 10.4314/gmj. v44i1.68854. PMID: 21326989; PMCID: PMC2956310.
[50] Reji, P., Aga, G. & Abebe, G. 2013. The role of AFB microscopy training in improving the performance of laboratory professionals: analysis of pre and post-training evaluation scores. BMC Health
Serv Res 13, 392 (2013). https://doi.org/10.1186/1472-6963-13-392.[51] Ugwu I. Omale. 2021. Knowledge, attitude, and practice of the National Guidelines for Diagnosis and Treatment of Malaria among medical doctors in Ebonyi state, Nigeria: A cross-sectional survey. https://doi.org/10.1371/journal.pone.0257600.
Viewed PDF 1060 26 -
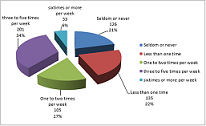 The Combined Effect of Socio Demographical Factors and Physical Exercise Training on Cardiovascular Health of Fresh Students of Babcock University Ilishan-Remo, Ogun State, NigeriaAuthor: Oyerinde Oyewole OlusesanDOI: 10.21522/TIJPH.2013.10.01.Art023
The Combined Effect of Socio Demographical Factors and Physical Exercise Training on Cardiovascular Health of Fresh Students of Babcock University Ilishan-Remo, Ogun State, NigeriaAuthor: Oyerinde Oyewole OlusesanDOI: 10.21522/TIJPH.2013.10.01.Art023The Combined Effect of Socio Demographical Factors and Physical Exercise Training on Cardiovascular Health of Fresh Students of Babcock University Ilishan-Remo, Ogun State, Nigeria
Abstract:
Lack of physical activities is one of the strongest risk factors for many chronic cardiovascular diseases, including hypertension, diabetes, obesity, osteoporosis, colon cancer, and depression. This was an experimental study that employed both qualitative and quantitative data collection methods that involved pre-exercise medical evaluation and survey. It investigated the effects of two independent variables, which are the correlate of Socio-demographic factors and PE training on cardiovascular diseases among 600 volunteered fresh students at Babcock University. The data were subjected to statistical analysis, and result were presented in tables and figures. The result of the Mean Arterial Pressure (MAP) showed that there was no significant relationship P>0.05 between gender, level of education, vital signs, and anthropometric measurement. Well above average (74.3%) had a normal MAP, and many (21.5%) were between pre-diabetics. The combined result of the Body Mass Index showed many (60.9%) were obese and overweight. Irregular participation in Physical Activities showed a significant relationship (P<0.05) even do some 160(26.7%) had excellent overall physical health, and 173 (28.8%) had good overall physical health. There were significant interactional effects between groups and time for perceived benefits, interpersonal norms, social support, counter heart conditioning, stimulus control, overall time spent on being physically active per week (P<0.05). In conclusion, it is recommended that collegiate should engage in regular physical activity at a level appropriate to their capacities, needs, and interests to maintain optimal cardiovascular health status.
The Combined Effect of Socio Demographical Factors and Physical Exercise Training on Cardiovascular Health of Fresh Students of Babcock University Ilishan-Remo, Ogun State, Nigeria
References:
[1] Stock S, Miranda C, Evans S, Plessis S, Ridley J, Yeh S, Chanoine JP (2007): Healthy Buddies: a novel, peer-led health promotion program for the prevention of obesity and eating disorders in children in elementary school. US National Library of Medicine National Institute of Health Pediatrics. 2007 Oct; 12 0(4): e1059-68.
[2] World Health Organization (WHO), (2006). The World Health Report 2000: Health Systems: Improving Performance WHO Library Cataloguing in Publication Data. ISBN 92 4 156198 X (NLM Classification: WA 540.1) ISSN 1020-3311.
[3] Obiyemi O.O., Oyerinde O.O, Oniyangi S.O., Abu, D.A., Adeoye O. A. (2013); Predictors of female lecturers’ participation in physically involving wellness activities in FCT, College of education, zuba, Abuja, Nigeria. International Journal of West Africa University Games (IJWAUG) 86.
[4] Task Force on Community Preventive Services (TFCPS), (2013). Evaluation of a teacher-led physical activity curriculum to increase preschooler physical activity Open Journal of Preventive Medicine Vol.3, No.1, 141-147 (2013) DOI:10.4236/ojpm.2013.31018.
[5] Centers for Disease Control (CDC), (2012): Youth Risk Behaviour Surveillance System, Youth Risk Behaviour Surveillance. United States, 2003 MMWR 53(SS-2):1–29, 2004. http://www.cdc.gov/healthyyouth/yrbs/. Dietary Guidelines for Americ Ans, 2005.
[6] WHO, (2020). Impact of COVID-19 on people’s livelihoods, their health, and our food systems Joint statement by ILO, FAO, IFAD, and WHO 13 October 2020.
[7] Jonathan Lerner, Con Burns, and Áine de Róiste, (2011) Correlates of Physical Activity Among College Students Recreational Sports Journal, 2011, 35, 95-106 © 2011 Nirsa Foundation.
[8] Lori Lynn DeLong, (2006); College Students’ Motivation for Physical Activity (B.A., Louisiana College, 1995 M.Ed., University of Louisiana at Monroe, December 2006).
[9] Wijndaele K, Philippaerts R, Matton L, De Bourdeaudhuij I, Taks M, Lefevre J., (2006); Reliability and validity of a computer-assisted physical activity questionnaire for 12- to 18-year-old boys and girls. Proceedings of the 8th Annual Congress European College of Sport Science: July 9, 13, 2003; Salzburg. 2003.
[10] Al-kuraishy, Ali I. Al-Gareeb, Susana G. Guerreiro, Natália Cruz-Martins, Gaber El-Saber Batiha, (2021); COVID-19 in Relation to Hyperglycemia and Diabetes Mellitus. Cardiovascular. Med., 20 May 2021 | https://doi.org/10.3389/fcvm.2021.644095.
[11] Schwarzer, R. (2020). Modeling health behavior change: How to predict and modify. The adoption and maintenance of health behaviors. Applied Psychology: An International Review, 57(1), 1-29.
[12] O’Brien, C.O., Peters, J., Murphy, P., et al. (2000); Irish Heart Foundation Position Statement on Physical Activity. Retrieved from Website: https://irishheart.ie/ on:5/10/07.
[13] Kurokawa Y, Kani R, Takatori E, (2020); Assessment of health-related quality of life in cancer outpatients treated with chemotherapy. Gan To Kagaku Ryoho. 2020 Mar;39(3):409-14. Medical University Hospital. Department of Clinical Oncology, Tokyo.
[14] WHO, Department of Health and Human Service (DHHS), (2008): Physical activity Guideline for America. Improving performance. Be Active, Healthy, and Happy! www.health.gov/paguidelines.
[15] WHO, Department of Health and Human Service (DHHS), (2007): Physical activity Guideline for America 2nd Edition. Physical Activity Guidelines for Americans 2nd edition https://health.gov/sites/default/files/2019-09/Physical_Activity_Guidelines_2nd_edition.pdf.
[16] Fahey, T., Delaney, L., & Gannon, B. (2005); School Children and Sport in Ireland. Published by the ESRI in conjunction with The Irish Sports Council: Dublin and obtained from https://www.esri.ie/ on 10/7/07.
[17] Lalor, K., de Róiste, A., & Devlin, M. (2007). Young people in contemporary Ireland. Pp 1–57, 82–85, 103–105, 113, 295. Dublin: Gill & Macmillan Ltd.
[18] Amusa L.O., (1986): The place of recreation in preventive medicine proceeding of 16th annual conference of Napher (pp. 61-64).
[19] Oyerinde,Oyewole Olusesan, Aja Godwin ND, Atulomah Ndumele SO, Oyerinde Oyesegun Olufemi, Olaoye Paul Olufemi, and Adeoye Ayodele, (2014): Impact of Teacher-Led Physical Exercise on Self-Efficacy and Physical Activity Performances of First Year Undergraduate Students in a Private University, Ogun State, Nigeria. Kuwait Chapter of Arabian Journal of Business and Management Review Vol. 4 No.1.
[20] Centers for Disease Control (CDC), (2005): Healthy Weight, Nutrition, and Physical Activity https://www.cdc.gov/ Press Release CDC Breaks Ground on New Lifestyle Center, Dedicates new streetscape January 31, 2005.
[21] WHO, Department of Health and Human Service (DHHS) (2008). Physical activity Guideline for America accessed online at www.who.int/whr2009/2001/archives/2000/en/contents.htm, on June 3, 2009. WHO, (2008).
[22] Wijsman, C.A, Westendorp G.J., Verhagen, A.L.M, Catt, M, Slagboom, P.E., de Craen J.M., Broekhuizen, k., van Mechelen, W., van Heemst D, van der Ouderaa F, Mooijaart, SP, (2013).: Effects of a Web-Based Intervention on Physical Activity and Metabolism in Older Adults: Randomized Controlled Trial. i-JMIR Vol 15, No 11 (2013)> Wijsman.
[23] Emily B. K, Leigh T. R, Ross C. B, Gregory W. H, Elizabeth H. H, Kenneth E. P, Elaine J. S, Mummy W. R, Phaedra C, (2013) & the Task Force on Community Preventive Services, (2013): Evaluation of a teacher-led physical activity curriculum to increase pre-schooler physical activity Open Journal of Preventive Medicine Vol.3, No.1, 141-147 (2013) doi:10.4236/ojpm.2013.31018.
[24] Emily B. K, Leigh T. R, Ross C. B, Gregory W. H, Elizabeth H. H, (2012): Effects of Teacher-Encouraged Physical Activity on Preschool Playgrounds. The online version of this article can be found at: DOI: 10.1177/1053815109331858 Journal of Early Intervention 2009 31: 126 University of South Carolina, Columbia http://jei.sagepub.com/content/31/2/126.
[25] WHO, (2009). Delivering quality health, services A global imperative for universal health coverage. Assessed online at www.who.int/whr2009/.
[26] Harris KC, Kuramoto LK, Schulzer M, Retallack JE. (2009) Effect of school-based physical activity interventions on body mass index in children: a meta-analysis. CMAJ. 2009 Mar 31;180(7):719-26. Department of Paediatrics, British Columbia Children’s Hospital, Vancouver, BC. kharris2@cw.bc.ca.
[27] Centers for Disease Control, (2007); MyPyramid and Physical Activity Tracker. Websites
for physical activity information Centers for Disease Control and Prevention Centers for Disease Control and Prevention, Obesity Trends Getting Physically Active Good Nutrition and Physical Activity Plans (mypyramid.gov) http://www.cdc.gov/nccdphp/dnpa/obesity/trend/maps/.[28] American Diabetes Association (1990. 2000): Diabetes trends in the U.S.: 1990-1998. Diabetes Care 2021 Jul; 44 (7): 1462- 1471. https://doi.org/10.2337/dc20-2257 Diabetes Care 2000 Sep; 23(9): 1278-1283. https://doi.org/10.2337/diacare.23.9.1278.
[29] Obiyemi O.O., Oyerinde O.O, Oniyangi S.O., Abu, D.A., Adeoye O. A. (2013): Effects of Teacher-Encouraged Physical Activity on Preschool Playgrounds. The online version of this article can be found at: DOI: 10.1177/1053815109331858 Journal of Early Intervention 2009 31: 126 University of South Carolina, Columbia http://jei.sagepub.com/content/31/2/126.
[30] Barr-Anderson, Daheia J., Melissa N. Laska, Sara Veblen-Mortenson, Kian Farbakhsh Bonnie Dudovitz (2012): A School-Based, Peer Leadership Physical Activity Intervention for 6th Graders: Feasibility and Results of a Pilot Study Published in Journal of Physical Activity and Health, Volume 9, Issue 4, 2012, pages 492-499. 5-1-2012.
[31] Dobbins M, Husson H, DeCorby K, & LaRocca R.L, (2013): School-based physical activity programs for promoting physical activity and fitness in children and adolescents aged 6 to 18. Cochrane Database System Rev. 2013 Feb 28;2:CD007651. DOI: 10.1002/14651858.CD007651.pub2.
Viewed PDF 1186 45 -
 The Impact of Covid-19 Pandemic and Gender-Based Violence on Uptake of HIV Services in Touboro District Hospital, CameroonAuthor: Sandrine MewoabiDOI: 10.21522/TIJPH.2013.10.01.Art024
The Impact of Covid-19 Pandemic and Gender-Based Violence on Uptake of HIV Services in Touboro District Hospital, CameroonAuthor: Sandrine MewoabiDOI: 10.21522/TIJPH.2013.10.01.Art024The Impact of Covid-19 Pandemic and Gender-Based Violence on Uptake of HIV Services in Touboro District Hospital, Cameroon
Abstract:
As we move towards HIV epidemic control in Cameroon, we strive to limit the number of new infections by maintaining on-treatment PWHIV. The emergence of the Covid-19 pandemic may cause interruptions in HIV treatment and slow progression. COVID-19 control measures have caused; the lockdown of businesses, some health services, and imposed work from home, with intimate partners and more people spending longer hours together at home. As a consequence, there is an increased risk of gender-based violence (GBV). GBV can affect adherence to treatment in PWHIV and prevent them from accessing health services. The main objective of the study was to determine the effect of Covid-19 and GBV on the uptake of HIV services by assessing interruptions in treatment. Using a structured questionnaire, demographic data, Information on COVID-19 and intimate partner violence were obtained from 339 participants between 15 and 60 years old, taking HIV treatment at the Touboro district hospital. We used the Antiretroviral treatment register of the health facility to extract data on the frequency and duration of interruption in treatment. The Prevalence of intimate partner violence was high in our study participants, although interruption in treatment was only significant in respondents who reported verbal abuse. A strong association was observed between Covid 19 and interruption in treatment. There was equally an association between Covid-19 and an increase in intimate IPV. Other Socio-demographic variables found to affect interruption in treatment were level of Education of the partner, Age difference with intimate partner greater than 10years, and early years on antiretroviral therapy. According to the study, Both Gender-based violence (IPV) and Covid-19 affect interruption in antiretroviral treatment.
The Impact of Covid-19 Pandemic and Gender-Based Violence on Uptake of HIV Services in Touboro District Hospital, Cameroon
References:
[1] WHO, HIV/AIDS (key facts), Date of access: 29/05/2021. https://www.who.int/news-room/fact-sheets/detail/hiv-aids.
[2] UNAIDS, Global HIV & AIDS statistics- fact sheet, Date of access: 21/03/2021. https://www.unaids.org/en/resources/fact-sheet.
[3] UNAIDS, Global HIV & AIDS statistics- fact sheet, Date of access: 29/05/2021. https://www.unaids.org/en/resources/fact-sheet.
[4] Leddy, A. M., Weiss, E., Yam E., et Pulerwitz, J., 2019, Gender-based violence and engagement in biomedical HIV prevention, care and treatment: a scoping review. BMC Public Health, 19(1), 897 https://doi.org/10.1186/s12889-019-7192-4.
[5] WHO, 2004, Violence Against Women and HIV/AIDS: Critical Intersections - Intimate Partner Violence and HIV/AIDS. Inf. Bull. Ser, 1, 1–9. https://www.who.int/hac/techguidance/pht/InfoBulletinIntimatePartnerViolenceFinal.pdf.
[6] Peltz, A., Reitenauer, E., 2021, Gender Equality and Gender-based Violence Prevention & Response Services in USAID’s PEPFAR Programs. Intra Health. https://www.intrahealth.org/sites/ihweb/files/asap-attachment-files/asapwebinargegbvpreventionandresponseservicesinusaidspepfarprograms-updated22321.pdf.
[7] WHO, 2013, 16 Ideas for addressing violence against women in the context of the HIV epidemic: a programming tool. World Health Organization, ISBN 978 92 4 150653 3.
[8] UN WOMEN, Covid-19: Emerging gender data and why it matters, Date of access: 09/05/2021. https://data.unwomen.org/resources/Covid-19-emerging-gender-data-and-why-it-matters.
[9] PEPFAR, 2020, PEPFAR Technical Guidance in Context of Covid-19 Pandemic, state.gov, 1–8. https://www.state.gov/wp-content/uploads/2020/10/10.07.2020-PEPFAR-Technical-Guidance-During-Covid.pdf.
[10] Chenneville, T., Gabbidon, K., Hanson, P., et Holyfield, C., 2020, The Impact of Covid-19 on HIV Treatment and Research: A Call to Action. Int. J. Environ. Res. Public Health, 17(12), 4548, 1-14. https://doi.org/10.3390/ijerph17124548.
[11] WHO, Weekly epidemiological update on Covid-19 - 27 April 2021,
[12] Date of access: 09/05/2021. https://www.who.int/publications/m/item/weekly-epidemiological-update-on-Covid-19---27-april-2021.
[13] WHO, Cameroon: WHO Coronavirus Disease (Covid-19) Dashboard, Date of access: 31/01/201. https://Covid19.who.int/region/afro/country/cm.
[14] Judson, S. D., Njabo, K. Y., et Torimiro, J. N., 2020, Regional vulnerability for Covid-19 in Cameroon. The Pan African medical journal, 37(Suppl 1), 16. https://doi.org/10.11604/pamj.supp.2020.37.16.26167.
[15] Marzo, R. R., Singh, A., et Mukti, R. F., 2021, A survey of psychological distress among Bangladeshi people during the Covid-19 pandemic.Clinical Epidemiology and Global Health. Elsevier, 10, p. 100693. DOI: 10.1016/J.CEGH.2020.100693.
[17] Kamberi, F. et al., 2021, Impact of Covid-19 pandemic on mental health, risk perception and coping strategies among health care workers in Albania - evidence that needs attention, Clinical Epidemiology and Global Health. Elsevier, 12, 100824. DOI: 10.1016/J.CEGH.2021.100824.
[18] El-Abasiri, R. A. et al., 2020, Evaluating the psychological distress of the coronavirus disease 2019 pandemic in Egypt, European Journal of Molecular and Clinical Medicine, 7(5), 1–12. Available at: https://www.embase.com/search/results?subaction=viewrecord&id=L2010164833&from=export.
[19] Htay, M. N., et al., 2021 , How healthcare workers are coping with mental health challenges during Covid-19 pandemic? - A cross-sectional multi-countries study, Clinical Epidemiology, and Global Health. Elsevier B.V., 11(February), 100759. DOI: 10.1016/j.cegh.2021.100759.
[20] UNAIDS, Covid-19, and HIV: 1 moment, 2 epidemics, 3 opportunities—how to seize the moment to learn, leverage, and build a new way forward for everyone’s health and rights, Date of access: 09/05/2021. https://www.unaids.org/en/resources/documents/2020/20200909_lessons_hiv_Covid.
[21] Fiorentino, M., Sagaon-Teyssier, L., Ndiaye, K., Suzan-Monti, M., Mengue, M. T., Vidal, L., Kuaban, C., March, L., Laurent, C., Spire, B., Boyer, S., et EVOLCam Study Group, 2019, Intimate partner violence against HIV-positive Cameroonian women: Prevalence, associated factors, and relationship with antiretroviral therapy discontinuity-results from the ANRS-12288 EVOLCam survey. Women’s health (London, England), 15, 1745506519848546. https://doi.org/10.1177/1745506519848546.
[22] Kapiga, S., Harvey, S., Muhammad, A. K., Stöckl, H., Mshana, G., Hashim, R., Hansen, C., Lees, S., et Watts, C., 2017, Prevalence of intimate partner violence and abuse and associated factors among women enrolled into a cluster randomised trial in northwestern Tanzania. BMC public health, 17(1), 190. https://doi.org/10.1186/s12889-017-4119-9.
[23] Karakurt, G., Silver, K. E., 2013, Emotional abuse in intimate relationships: the role of gender and age. Violence and Victims, 28(5), 804–821. https://doi.org/10.1891/0886-6708.vv-d-12-00041.
[24] Fiorentino, M., Sagaon-Teyssier, L., Ndiaye, K., Suzan-Monti, M., Mengue, M. T., Vidal, L., Kuaban, C., March, L., Laurent, C., Spire, B., Boyer, S., et EVOLCam Study Group, 2019, Intimate partner violence against HIV-positive Cameroonian women: Prevalence, associated factors, and relationship with antiretroviral therapy discontinuity-results from the ANRS-12288 EVOLCam survey. Women’s health (London, England), 15, 1745506519848546. https://doi.org/10.1177/1745506519848546.
[25] Humanitarian Response, Cameroon: South West Region GBV Rapid assessment – Key findings, January 2019, Date of access: 30/09/2021 https://www.humanitarianresponse.info/en/operations/cameroon/document/cameroon-south-west-region-gbv-rapid-assessment-–-key-findings-January.
[26] Dlamini, P. S., Kohi, T. W., Uys, L. R., Phetlhu, R. D., Chirwa, M. L., Naidoo, J. R., Holzemer, W. L., Greeff, M., et Makoae, L. N., 2007, Verbal and physical abuse and neglect as manifestations of HIV/AIDS stigma in five African countries. Public health nursing (Boston, Mass.), 24(5), 389–399. https://doi.org/10.1111/j.1525-1446.2007.00649.x.
[27] Global Campus of Human Rights, Mitigating the Impact of Covid-19 on HIV Responses in Africa - Global Campus of Human Rights, Date of access: 30/09/2021. https://gchumanrights.org/preparedness/article-on/mitigating-the-impact-of-Covid-19-on-hiv-responses-in-africa.html.
[28] WHO, WHO warns that HIV infection increases the risk of severe and critical Covid-19, Date of
access: 30/09/2021. https://www.who.int/news/item/15-07-2021-who-warns-that-hiv-infection-increases-risk-of-severe-and-critical-Covid-19.[29] Waite, K. R., Paasche-Orlow, M., Rintamaki, L. S., Davis, T. C., et Wolf, M. S., 2008, Literacy, social stigma, and HIV medication adherence. Journal of general internal medicine, 23(9), 1367–1372. https://doi.org/10.1007/s11606-008-0662-5.
[30] UN WOMEN, Covid-19 and ending Violence Against Women and Girls, Date of access: 30/09/2021. https://www.unwomen.org/en/digital-library/publications/2020/04/issue-brief-Covid-19-and-ending-violence-against-women-and-girls.
[31] Aye, S. S., et Rillera, M. R., 2020, Readiness for inter-professional education at health sciences: A study of educational technology prespective, World Journal on Educational Technology: Current Issues, 12(3), 207–216. doi: 10.18844/wjet.v%vi%i.4992.
[32] Soe, S., 2020, Cypriot Journal of Educational Readiness for interprofessional education amongst students at public and private Medical Universities in Malaysia, 15(6), 1454–1463.
Viewed PDF 1285 43 -
 Effects of Pregnancy-Induced Psychological and Emotional Factors on the Occurrence of Preeclampsia/Eclampsia (PE-E) and HaemorrhageAuthor: James Atampiiga AvokaDOI: 10.21522/TIJPH.2013.10.01.Art025
Effects of Pregnancy-Induced Psychological and Emotional Factors on the Occurrence of Preeclampsia/Eclampsia (PE-E) and HaemorrhageAuthor: James Atampiiga AvokaDOI: 10.21522/TIJPH.2013.10.01.Art025Effects of Pregnancy-Induced Psychological and Emotional Factors on the Occurrence of Preeclampsia/Eclampsia (PE-E) and Haemorrhage
Abstract:
Preeclampsia/eclampsia (PE-E) and haemorrhage are the topmost causes of maternal and perinatal deaths in the world. This study was designed to assess the effects of pregnancy-induced psychological and emotional factors on the occurrence of PE-E and haemorrhage. The study was a prospective cohort involving all pregnant women >28 weeks of gestation reporting for antenatal care (ANC) in seven Hospitals in the Eastern Region of Ghana. The study redesigned the Revised Cognitive Therapy Scale (CTS-R) to suit this study using a five-point score scale. The results show that the predictor variables; fear, anger, sadness, disgust, love, hate, tension, anxiety, depression, and dejection, were all statistically significant and associated with PE-E and haemorrhage except joy, acceptance, and happiness. Pregnant women who experienced high (2) and highest (4) levels of fear had reduced odds of PE-E by 34% and 15.8%, respectively. Those who recorded low levels of love were 9.8 times the odds of PE-E, those with low (1), high (2), higher (3), and highest (4) levels of anxiety had reduced odds of PE-E by 22.2%, 37.3%, 21.3%, and 10% respectively. Pregnant women with low levels of psychological and emotional issues were about 3 times the odds of PE-E compared to those who were normal. In conclusion, the study shows a significant association between preeclamptic/eclamptic pregnant women and different levels of fear, anger, sadness, Love, hate, depression, dejection, anxiety, and tension. It is recommended that Ghana Health Service should institute psychological and emotional counselling as part of ANC services in order to manage pregnant women who may need them to avert the effects on pregnancy and birth outcome.
Effects of Pregnancy-Induced Psychological and Emotional Factors on the Occurrence of Preeclampsia/Eclampsia (PE-E) and Haemorrhage
References:
[1] WHO, (2017), Maternal mortality Evidence brief. 1, 1–4.
[2] World Health Organization. (2018). WHO recommendations: policy of interventionist versus.
[3] WHO (2019), -RHR-19.20-eng.pdf, https://apps.who.int/iris/bitstream/handle/10665/329886/WHO-RHR-19.20-eng.pdf downloaded on 26/12/2021?
[4] Sánchez-aranguren, L. C., Prada, C. E., Riaño-medina, C. E., & Lopez, M. (2014), Endothelial dysfunction and preeclampsia: role of oxidative stress. 5(October), 1–11. https://doi.org/10.3389/fphys.2014.00372.
[5] Liu, L., Johnson, H. L., Cousens, S., Perin, J., Scott, S., Lawn, J. E., Rudan, I., Campbell, H., Cibulskis, R., & Li, M. (2010), Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. The Lancet, 379(9832), 2151–2161. https://doi.org/10.1016/S0140-6736(12)60560-1.
[6] Khan, K. S., Wojdyla, D., Say, L., Gülmezoglu, A. M., & Look, P. F. A. Van. (2006), WHO analysis of causes of maternal death: a systematic review. 367. https://doi.org/10.1016/S0140-6736(06)68397-9.
[7] Galaa, S. Z. (2010), Trends and Causes of Maternal Mortality at the Wa Regional Hospital, Ghana: 2005-2010. 13(1), 2005–2010.
[8] Say, L., Chou, D., Gemmill, A., Tunçalp, Ö., Moller, A., Daniels, J., Gülmezoglu, A. M., Temmerman, M., & Alkema, L. (2006), Global causes of maternal death: a WHO systematic analysis. 323–333. https://doi.org/10.1016/S2214-109X(14)70227-X.
[9] Aborigo, R. A., Moyer, C. A., Gupta, M., Adongo, P. B., Williams, J., Hodgson, A., Allote, P., & Engmann, C. M. (2014), Obstetric Danger Signs and Factors Affecting Health Seeking Behaviour among the Kassena-Nankani of Northern Ghana: A Qualitative Study. 18(September), 78–86.
[10] Storm, F., Agampodi, S., Eddleston, M., Sørensen, J. B., Konradsen, F., & Rheinländer, T. (2014), Edinburgh Research Explorer Indirect causes of maternal death Indirect causes of. The Lancet Global Health, 2(10), e566. https://doi.org/10.1016/S2214-109X(14)70297-9.
[11] Sumankuuro, J., Crockett, J., & Wang, S. (2017), Maternal health care initiatives: Causes of morbidities and mortalities in two rural districts of Upper West Region, Ghana. 1–18.
[12] Moyer, C., Gyasi, R. K., Akosa, A. B., Tettey, Y., Akakpo, P. K., & Anim, J. T. (2013), Pregnancy-Related Causes of Deaths in Ghana: A 5-Year Retrospective Study. 47(4), 158–163.
[13] Awoonor-williams, J. K. (2018), Maternal Death in Rural Ghana: A Case study in the Upper east Region of Ghana. 6(April), 1–6. https://doi.org/10.3389/fpubh.2018.00101.
[14] Asamoah, B. O., Moussa, K. M., Stafström, M., & Musinguzi, G. (2011), Distribution of causes of maternal mortality among different socio-demographic groups in Ghana; a descriptive study.
[15] GDHS, 2021. Population and Housing Census, 2021 Preliminary Report.
[16] Blackburn, I. M., James, I. A., Milne, D. L., Baker, C., Standart, S., Garland, A., & Reichelt, F. K. (2001), The revised cognitive therapy scale (CTS-R): Psychometric properties. Behavioural and Cognitive Psychotherapy, 29(4), 431–446. https://doi.org/10.1017/s1352465801004040.
[17] Harmon-jones, C., Bastian, B., & Harmon-jones, E. (2016), The Discrete Emotions Questionnaire: A New Tool for Measuring State Self-Reported Emotions. 1–25. https://doi.org/10.1371/journal.pone.0159915.
[18] Cochran, W.G. (1963) Sampling Techniques, Wiley, New York.
[19] Veena, S. R., Gale, C. R., Krishnaveni, G. V, Kehoe, S. H., Srinivasan, K., & Fall, C. H. D. (2016), Association between maternal nutritional status in pregnancy and offspring cognitive function during childhood and adolescence; a systematic review. BMC Pregnancy and Childbirth. https://doi.org/10.1186/s12884-016-1011-z.
[20] Grum, T., Hintsa, S., & Hagos, G. (2018), Dietary factors associated with preeclampsia or eclampsia among women in delivery care services in Addis Ababa, Ethiopia: a case-control study. BMC Research Notes, 1–5. https://doi.org/10.1186/s13104-018-3793-8.
[21] Endeshaw, M., Ambaw, F., Aragaw, A., & Ayalew, A. (2014), Effect of Maternal Nutrition and Dietary Habits on Preeclampsia: A Case-Control Study. January. https://doi.org/10.4236/ijcm.2014.521179.
[22] Ram, D., Id, S., Sangroula, R. K., Shakya, N. S., Yadav, R., Chaudhary, N. K., Man, P., & Pradhan, S. (2019), Effect of nutrition education on hemoglobin level in pregnant women: A quasi-experimental study. 1–12.
[23] Krishnamurti (2019b), Pregnancy Hypertension. 18 (September), 55–57. https://doi.org/10.1016/j.preghy.2019.09.003.
[24] Boene, H., Vidler, M., Sacoor, C., Nhama, A., Nhacolo, A., Bique, C., Alonso, P., Sawchuck, D., Qureshi, R., Macete, E., Menéndez, C., & Dadelszen, P. Von. (2016), Community perceptions of pre-eclampsia and eclampsia in southern Mozambique. Reproductive Health, 13(Suppl 1). https://doi.org/10.1186/s12978-016-0135-y.
[25] Pevzner. (2017), Cardiac extraction from suckling rat HHS Public Access. Physiology & Behavior, 176(3), 139–148. https://doi.org/10.1016/j.copsyc.2017.06.016.Emotion.
[26] Smyth et al (2016), Redalyc. Physical activity and anger or emotional upset are triggers of acute myocardial infarction. The Inter-Heart study.
[27] Lassi, Z. S., Kumar, R., Mansoor, T., Salam, R. A., Das, J. K., & Bhutta, Z. A. (2014), Essential interventions: implementation strategies and proposed packages of care. 11(Suppl 1), 1–17.
[28] Amoroso, C. R., Hanna, E. K., LaBar, K. S., Schaich Borg, J., Sinnott-Armstrong, W., & Zucker, N. L. (2020), Disgust Theory Through the Lens of Psychiatric Medicine. Clinical Psychological Science, 8(1), 3–24. https://doi.org/10.1177/2167702619863769.
[29] Postma, I. R., Bouma, A., Ankersmit, I. F., & Zeeman, G. G. (2014), and eclampsia: a long-term follow-up study. The American Journal of Obstetrics & Gynecology, 211(1), 37.e1-37. e9. https://doi.org/10.1016/j.ajog.2014.01.042.
[30] Carter, C. S., Caldwell, H. K., Bosch, O. J., & Carter, C. S. (2017), The Oxytocin – vasopressin Pathway in the Context of Love and Fear. 8(December), 1–12. https://doi.org/10.3389/fendo.2017.00356.
[31] Zwart, P. L. De, Jeronimus, B. F., & Jonge, P. De. (2019), Empirical evidence for definitions of episode, remission, recovery, relapse, and recurrence in depression: a systematic review. 544–562. https://doi.org/10.1017/S2045796018000227.
[32] Mostofsky, E., Penner, E. A., & Mittleman, M. A. (2014), Outbursts of anger as a trigger of acute cardiovascular events: A systematic review and meta-analysis. European Heart Journal, 35(21), 1404–1410. https://doi.org/10.1093/eurheartj/ehu033.
[33] Navarro, J. I., Marchena, E., & Menacho, I. (2013). The Psychology of Hatred. 10–17.
[34] Qiu, C., Williams, M. A., Calderon-margalit, R., Cripe, S. M., & Sorensen, T. K. (2009), Preeclampsia Risk in Relation to Maternal Mood and Anxiety Disorders Diagnosed Before or During Early Pregnancy. 22(4). https://doi.org/10.1038/ajh.2008.366.
[35] Hosseini, A., & Jalali, M. (2018), The Possible Biological Effects of Long-term Stress on Depression. Medbiotech Journal, 2(4), 149–152. https://doi.org/10.22034/mbt.2018.80819.
[36] Yu, Y., Zhang, S., Mallow, E. B., Wang, G., Hong, X., Walker, S. O., Pearson, C., Heffner, L., Zuckerman, B., & Wang, X. (2014), NIH Public Access. 209(5), 1–16. https://doi.org/10.1016/j.ajog.2013.07.003.
[37] Ensari, I., Burg, M. M., Diaz, K. M., Fu, J., Duran, A. T., Suls, J. M., Sumner, J. A., Monane, R., Julian, J. E., Zhao, S., Chaplin, W. F., & Shimbo, D. (2018), Putative mechanisms Underlying Myocardial infarction onset and Emotions (PUME): A randomised controlled study protocol. BMJ Open, 8(5). https://doi.org/10.1136/bmjopen-2017-020525.
[38] Schetter, C. D., Tanner, L., & Angeles, L. (2015), HHS Public Access. 25(2), 141–148. https://doi.org/10.1097/YCO.0b013e3283503680.Anxiety.
[39] Fernández-Carrasco. (n.d.). Significance of A ff ection Changes during Pregnancy: Intimacy , Passion , and Commitment.
[40] Curtis, V. (2011), Why disgust matters. 3478–3490. https://doi.org/10.1098/rstb.2011.0165.
[41] Sternberg, 2005, p.69
[42] Lane, A. M., Terry, P. C., Devonport, T. J., Friesen, A. P., Totterdell, P. A., & Lane, A. M. (2017), A Test and Extension of Lane and Terry ’ s (2000) Conceptual Model of Mood-Performance Relationships Using a Large Internet Sample. 8(April), 1–11. https://doi.org/10.3389/fpsyg.2017.00470.
[43] Nabulo, H., Ruzaaza, G., Mugabi, F., & Bajunirwe, F. (2021), Perceptions on preeclampsia and eclampsia among senior, older women, in rural Southwestern Uganda. Journal of Global Health Reports, 1–19. https://doi.org/10.29392/001c.19464.
[44] Mommersteeg, P. M. C., Drost, J. T., Ottervanger, J. P., Angela, H. E., Maas, M., Mommersteeg, P. M. C., Drost, J. T., Ottervanger, J. P., Angela, H., & Mommersteeg, P. M. C. (2016). Long-term follow-up of psychosocial distress after early onset preeclampsia: the Preeclampsia Risk EValuation in FEMales cohort study Long-term follow-up of psychosocial distress after early onset preeclampsia : 8942. https://doi.org/10.3109/0167482X.2016.1168396.
Viewed PDF 1094 34 -
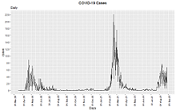 Trends in Testing and Positivity in Banadir, Somalia During the First Seventeen Months of the Covid-19 Pandemic, 2020Author: Sulaiman BanguraDOI: 10.21522/TIJPH.2013.10.01.Art026
Trends in Testing and Positivity in Banadir, Somalia During the First Seventeen Months of the Covid-19 Pandemic, 2020Author: Sulaiman BanguraDOI: 10.21522/TIJPH.2013.10.01.Art026Trends in Testing and Positivity in Banadir, Somalia During the First Seventeen Months of the Covid-19 Pandemic, 2020
Abstract:
Coronavirus Disease (Covid-19) is an infectious respiratory disease caused by a new strain of CoronaVirus. Many countries, including Somalia, have experienced two or more waves of the disease. The spread of Covid-19 in Banadir was a sporadic event distributed in many locations. The study aims to assess the time trends of Covid 19 testing positivity rate in the Banadir region of Somalia during the first seventeen months of the Covid-19 pandemic. A cross-sectional analytical study involving the review, analysis, and interpretation of existing dataset collected in the course of Covid-19 response between March 2020 and August 2021 to characterize the time trends of Covid 19 testing, compare the testing rates, attack rate, and positivity rates, and determine factors associated with positive Covid-19 tests in Banadir region. The categorical data were compared using a chi-square test. A total of 164 836 entries were analysed in this study. The majority (67.9%) of the participants were male, while close to a third (29.7%) were aged between 25-35 years, and 27.1% were aged 36-50 years. A total of 6,404(3.9%) participants tested positive for the Covid 19 virus. The chi-square test revealed bivariate association of age (P<0.001) and gender (P<0.001) were significantly associated with positive test results. Females and persons above 70 years had higher positivity of 4.4% and 13.7 %, respectively, compared to males and younger age groups. Banadir has recorded three waves of Covid 19 transmission from March 2020 to September 2021. Covid-19 vaccination uptake is needed to minimize spread.
Trends in Testing and Positivity in Banadir, Somalia During the First Seventeen Months of the Covid-19 Pandemic, 2020
References:
[1] John Hopkins University. (2021, November 25). John Hopkins University Corona Virus Resource Centre. Retrieved from Covid-19 Dashboard: https://coronavirus.jhu.edu/map.html.
[2] Deepak Pradhan, P. B. (2020, April 24). A Review of Current Interventions for Covid-19 Prevention. Elsevier, 363-374. Retrieved from https://doi.org/10.1016/j.arcmed.2020.04.020.
[3] AARP. (2021, February 3). Three Most Dangerous Underlying Conditions for Covid-19. AARP. Retrieved from http://www.aarp.org/.
[4] African Centres for Disease Control. (2021, November 25). African CDC Covid-19 Dashboard. Retrieved from African CDC Covid-19 Dashboard: https://africacdc.org/covid-19/.
[5] Vemu Lakshmi, T. S. (2011, June). Application of Polymerase Chain Reaction to Detect HIV-1 DNA in Pools of Dried Blood Spots. PMC Us National Library of Medicine, v. 51(2), 117-123. DOI:10.1007/s12088-011-0163-9.
[6] CDC. (2021, August 10). Diagnostic Methods. GLOBAL IMMUNISATION - Central for Disease Control and Prevention. Retrieved from https://www.cdc.gov/globalhealth/immunization/default.htm.
[7] United Nations. (2021). United Nations Covid 19 response. Retrieved from Covid-19 in Fragile Settings: Ensuring a Conflict-Sensitive Response: https://www.un.org/en/un-coronavirus-communications-team/covid-19-fragile-settings-ensuring-conflict-sensitive-response.
[8] United Nations Office for Coordination of Humanitarian Affairs. (2020). Humanitarian Needs Overview, Somalia. Mogadishu: Unocha.
[9] Lisa Maragakis. (2021, October 21). Coronavirus Second Wave, Third Wave and Beyond: What Causes a Covid Surge. (John Hopkins School of Medicine) Retrieved November 25, 2021, from John Hopkins School of Medicine-Health: https://www.hopkinsmedicine.org/health/conditions-and-diseases/coronavirus/first-and-second-waves-of-coronavirus.
[10] Tomáš Gavenčiak, J. T. (2021, June 13). Seasonal variation in SARS-CoV-2 transmission in temperate climates. medRxiv. DOI: https://doi.org/10.1101/2021.06.10.21258647.
[11] Sandra B. Nelson, C. M. (2021, September 26). Prevalence and risk factors for in-school transmission of SARS-CoV-2 in Massachusetts K-12 public schools, 2020-2021. JOHNS HOPKINS (BLOOMBERG School of Public Health). DOI: https://doi.org/10.1101/2021.09.22.21263900.
[12] Haitao Song, G. F. (2021, December 14). The Second Wave of Covid-19 in South and Southeast Asia and the Effects of Vaccination. Frontiers in Medicine. Retrieved from https://doi.org/10.3389/fmed.2021.773110.
[13] Gabriel Chamie, S. N. (2021, April 01). HIV testing approaches to reach the first UNAIDS 95% target in sub-Saharan Africa. The Lancet HIV, 8(4), E225-E236, DOI: https://doi.org/10.1016/S2352-3018(21)00023-0.
[14] Maheu-Giroux, M., Marsh, K., Doyle, C. M., Godin, A., Lanièce Delaunay, C., Johnson, L. F., . . . Hankins, C. A. (2019, December 15). National HIV testing and diagnosis coverage in sub-Saharan Africa. AIDS, 33(p), P s255-s269. DOI:10.1097/QAD.0000000000002386.
[15] Tim c. olde Hartman, J. G. (2020, December 12). Sex and Gender-Related Differences in Covid-19 Diagnoses and SARS-CoV-2 Testing Practices During the First Wave of the Pandemic: The Dutch Lifelines Covid-19 Cohort Study. Mary Ann Liebert, Inc., publishers Coronavirus Resource Center, 30(12). Retrieved from https://doi.org/10.1089/jwh.2021.0226.
[16] Eileen P Scully, G. S.-R. (2021, August 31). Sex and Gender Differences in Testing, Hospital Admission, Clinical Presentation, and Drivers of Severe Outcomes from Covid-19. NIH_The National Center for Biotechnology Information advances science and health, 8(9), 448. DOI: 10.1093/ofid/ofab448. eCollection 2021 Sep.
[17] Mauvais-Jarvis, F. M. (2020). Sex and gender: modifiers of health, disease, and medicine. The Lancet, 396(10250), 565-582.
[18] Bischof, E. W. (2020). Clinical trials for Covid-19 should include sex as a variable. The Journal of clinical investigation, 130(7), 3350-3352. doi:10.1172/JCI139306.
[19] Wu, Z. &. (2020, February 24). Characteristics of and important lessons from the coronavirus disease 2019 (Covid-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. Jama Network, 323(13), 1239-1242. DOI:10.1001/jama.2020.2648.
[20] Klein, S. L.-J. (n.d.). Biological sex impacts Covid-19 outcomes. PLoS pathogens. DOI: https://doi.org/10.1371/journal.ppat.1008570.g001.
[21] Peckham, H. d. (2020, December 9). Male sex was identified by global Covid-19 meta-analysis as a risk factor for death and ITU admission. Nature Communications. Retrieved from https://www.nature.com/articles/s41467-020-19741-6.
[22] Jakhmola, S., Baral, B., & Jha, H. C. (2021, March 31). A comparative analysis of Covid-19 outbreak on age groups and both the sexes of the population from India and other countries. NIH, 15(3), 333-341. DOI:10.3855/jidc.13698.
[23] Centers for Disease Control and Prevention. (2021, January 1). Covid-19 Starts Covid-19 Incidence, by Age Group, United State March 1 -November 14. Mortality and Morbidity Weekly Report (MMWR), 69(5152), 1664. Retrieved from http://dx.doi.org/10.15585/mmwr.mm695152a8.
[24] Ameen Younus, R. A.-A.-F. (2022, January 28). Perceived Covid-19 vaccine effectiveness, acceptance, and drivers of vaccination decision-making among the general adult population: A global survey of 20 countries. PLOS. Retrieved from https://doi.org/10.1371/journal.pntd.0010103.
[25] Roy Rillera Marzo, W. S. (2022, January 05). Hesitancy in Covid-19 vaccine uptake and its associated factors among the general adult population: a cross-sectional study in six Southeast Asian countries. BMC Tropical medicine and Health.
Viewed PDF 968 21 -
 Health Care Delivery System and the Reduction of Maternal and Child Mortality in Hospitals of Makurdi Benue State NigeriaAuthor: Comfort Ene OkpeDOI: 10.21522/TIJPH.2013.10.01.Art027
Health Care Delivery System and the Reduction of Maternal and Child Mortality in Hospitals of Makurdi Benue State NigeriaAuthor: Comfort Ene OkpeDOI: 10.21522/TIJPH.2013.10.01.Art027Health Care Delivery System and the Reduction of Maternal and Child Mortality in Hospitals of Makurdi Benue State Nigeria
Abstract:
The objectives of this publication are to find the historical background of maternal and child health care delivery, the incidence of maternal and child mortality, causes of maternal and child mortality, challenges in accessing maternal health care services of Nigeria. Data for the study were sourced from both primary and secondary means. Primary data was drawn through questionnaire and hospital records. Questionnaire was distributed to a sample of 369 respondents out of 4,740 population of staff of four purposely selected largest hospitals in Makurdi, Benue State. The sample size was determined through Taro Yamane’s formula, while the Bourley’s proportional allocation formula was used to determine the sample size per each hospital. Data were analyzed using descriptive statistics like tables, percentages, mean and standard deviation, while the test of hypotheses were done through Chi-square. The analyzed result shows that; the availability of maternal and child health care services in the hospitals were poor; accessibility of maternal and child health care services was also poor; Furthermore, Maternal and infant mortality is essentially high and increasing in hospitals of Makurdi, Benue State Nigeria. Several challenges are militating against effective healthcare delivery, therefore, the study recommended, among others, that government and other stakeholders should make conscious efforts to ensure that adequate facilities, tools, and equipment are provided for the hospitals to enhance the quality of maternal and child healthcare services in the Benue State of Nigeria.
Health Care Delivery System and the Reduction of Maternal and Child Mortality in Hospitals of Makurdi Benue State Nigeria
References:
[1] Omo-Aghoja, L. O., Aisien, O. A., Akuse, J. T., Bergstrom, S. and Okonofua, F. E., 2010. Maternal Mortality and emergency obstetric care in Benin City, South-south. Nigeria Journal of Clinical Medicine and Research, 2(4): 55-60.
[2] Harrison, K. A. 2009., The struggle to Reduce High Maternal Mortality in Nigeria African Journal of Reproductive Health, 13(3):9-20.
[3] Kana, M. A., Doctor, H. V., Peleteiro, B., Lunet, N. and Barros, H., 2015., Maternal and child health interventions in Nigeria: a systematic review of published studies from 1990 to 2014. BMC Public Health. 15:334.
[4] Uneke, C. P. J., Sombie, I., Keita, N., Lokossou, V., Johnson, E. and Ongolo-Zogo, P. 2017., An Assessment of National Maternal and Child Health Policy-Makers’ Knowledge and Capacity for Evidence-Informed Policy-Making in Nigeria. International Journal of Health Policy Management, 6(6): 309–316.
[5] Mojekwu, J. N. (2005). Maternal Mortality: Natural Risk to Women, Ghana Journal of Development Studies, 2(1): 129-141.
[6] Mojekwu, J. N. and Ibekwe, U. 2012., Maternal Mortality in Nigeria: Examination of Intervention Methods International Journal of Humanities and Social Science, 2(20):135-149.
[7] Campbell, J. (2011). Nigeria: Dancing on the Brink. Rowman and Littlefield Publishers, 88pp.
[8] The National Center for Biotechnology Information (NCBI) 2011.
[9] UNICEF, 2009; National Demographic Health Survey.
[10] WHO, UNICEF, UNFPA, World Bank, and UNPD (2014). Trends in Maternal Mortality: 1990 To 2013, Geneva: WHO Press.
[11] Ode, I. O. (2006) Demography: Principles and Application, Makurdi: Selfers Academic Press Ltd.
[12] Abdulraheem, I. S. I., Olapipo, A. R. and Amodu, M. O., 2012., Primary health care services in Nigeria: Critical issues and strategies for enhancing the use by the rural communities. Journal of Public Health and Epidemiology, 4(1): 5-13.
[13] Wunsch, J. S. and Olowu, D., 1996. Regime transformation from below: decentralization, local governance, and democratic reform in Nigeria in Journal of Comparative International Development, 31(4): 66-82.
[14] World Bank, 2018, Reproductive, Maternal, Newborn, Child, And Adolescent Health, Washington D. C.: The World Bank Group.
[15] UNICEF, 2009, State of the World’s Children (SOWC) New York: UNICEF.
[16] World Health Organization, 2005 Maternal Mortality in 2005 Estimates developed by WHO, UNICEF, UNFPA, and The World Bank http://www.who.int/-whosis/mme_2005.pdf.
[17] Shiffman, J. and Okonofua, F. E., 2007., The state of political priority for safe motherhood in Nigeria, British Journal of Obsterics and Gynaecology, 114:127-133.
[18] Okoosi-Simbine, A. T., 2011., Gender Politics and the 2011 Elections, Journal of African Elections, 11(1): 74-99.
[19] Obansa, S. A. and Orimisan, A. (2013). Health care financing in Nigeria: Prospects and Challenges, Mediterranean Journal of Social Sciences, 4(1): 221-236.
[20] UNICEF (2016). Evaluation of the maternal, newborn and child health week in Nigeria, Abuja: UNICEF.
[21] Ujah, I. A. O., Aisien, O. A., Mutihir, J. T., Vanderagt, D. J., Glew, R. H. and Uguru, V. E., 2005., Factors Contributing to Maternal Mortality in North-Central Nigeria., A Seventeen-year Review., African Journal Reproduction Health, 9(3): 27-40.
[22] Uneke, C. P. J., Sombie, I., Keita, N., Lokossou, V., Johnson, E. and Ongolo-Zogo, P., 2017. An Assessment of National Maternal and Child Health Policy-Makers’ Knowledge and Capacity for Evidence-Informed Policy-Making in Nigeria. International Journal of Health Policy Management, 6(6): 309–316.
Viewed PDF 1258 53 -
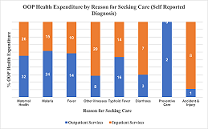 Assessment of Household Out-of-pocket (OOP) Contributions to Health Expenditure in Niger State North Central NigeriaAuthor: Inuwa JunaiduDOI: 10.21522/TIJPH.2013.10.01.Art028
Assessment of Household Out-of-pocket (OOP) Contributions to Health Expenditure in Niger State North Central NigeriaAuthor: Inuwa JunaiduDOI: 10.21522/TIJPH.2013.10.01.Art028Assessment of Household Out-of-pocket (OOP) Contributions to Health Expenditure in Niger State North Central Nigeria
Abstract:
In Nigeria, revenue for financing the health sector is collected from pooled and un‐pooled sources. The un‐pooled sources contribute over 70% of total health expenditure, and this can be Out-of-Pockets (OOPs) in the form of fees to healthcare providers at the time of service. The aim of the study was to estimate the out-of-pocket health expenditure of the households in Niger State. A cross-sectional quantitative study was carried out among 1,235 households made up of 6,482 individuals using a multi-stage stratified probability sampling technique. Data was collected using a well-structured survey instrument and analyzed using descriptive statistics and SPSS statistical software version 23. Findings shows that the annual per capita out-of-pocket expenditure on health services was approximately ₦19,463 ($46.9), and 64% of the total OOP expenditure is spent on public facilities. 32% of the OOP was incurred mainly from accessing maternal health services, with 56% likely to incur catastrophic expenditure. 75% of the sampled population expressed willingness to enroll into a form of health insurance, and an average household is willing to pay a monthly premium of ₦798 ($1.9) for health insurance. The study shows the urgency with which policy makers need to increase public healthcare funding and provide social health protection plans against informal OOP health payments. Furthermore, for Niger State to achieve the recommended benchmark of 30% OOP as a percentage of total health expenditure, it is critical that the newly signed into law contributory health insurance scheme is well designed, successfully implemented, and financially sustainable.
Assessment of Household Out-of-pocket (OOP) Contributions to Health Expenditure in Niger State North Central Nigeria
References:
[1] United Nations General Assembly. Seventy-fourth Session. Agenda item 126. Global health and foreign policy. Resolution adopted by the General Assembly on 10 October 2019, Contract No: A/74/L.4. Available online at https://undocs.org/en/A/RES/74/2. (Last accessed June 2021).
[2] Okungu V, Chuma J, McIntyre D. The Cost of Free Health Care for all Kenyans: Assessing the Financial Sustainability of Contributory and Non-contributory Financing Mechanisms. International journal for equity in health. 2017; 16(1): 39. DOI:.org/10.1186/s12939-017-0535-9.
[3] Uzochukwu B, Ughasoro MD, Etiaba E, Okwuosa C, Envuladu E, Onwujekwe OE. Health Care Financing in Nigeria: Implications for Achieving Universal Health Coverage. Nigerian Journal of Clinical Practice. 2015; 18(4): 437-444. Available online at http://www.njcponline.com. (Last accessed June 2021).
[4] Ifeagwu SC, Yang JC, Ratanshi RP, Carol Brayne C. Health Financing for Universal Health Coverage in Sub-Saharan Africa: A Systematic Review. Global Health Research and Policy. 2021; 6:8. DOI: org/10.1186/s41256-021-00190-7.
[5] Mathur M, Mathur N, Khan N, et al. Predictors of ‘Out-of-Pocket Expenditure’ on Routine Immunization of Under-Five Children: A Regression Analysis. Cureus. 2020; 12(12): e11859. DOI 10.7759/cureus.11859.
[6] Evans DB, Etienne C. Health Systems Financing and the Path to Universal Coverage. Bull World Health Organ. 2010;88(6):402.
[7] Sambo MN, Abdulrazaq GA, Shamang, AF, Ibrahim AA. Household cost of antenatal care and delivery services in a rural community of Kaduna State, Northwest Nigeria. Niger Med Journal. 2013; 54(2): 87-91.
[8] Van Doorslaer E, O’Donnell O, Rannan‐ Eliya RP, Somanathan A, Adhikari SR, Garg CC, et al. Catastrophic payments for healthcare in Asia. Health Economics. 2007 Nov 1; 16(11): 1159.
[9] Adesina AD, Ogaji DS. Out-of-Pocket Payment for Healthcare and Implications for Households: Situational Analysis in Yenagoa, Bayelsa State. Journal of Community Medicine and Primary Health Care. 2020; 32 (1) 1-16.
[10] World Health Organization; JICA; The Global Fund to Fight AIDS, Tuberculosis, and Malaria; and the African Development Bank. UHC in Africa: A Framework for Action. Washington, DC. 2016 World Bank.
[11] Akazili J, McIntyre D, Kanmiki EW, Gyapong J, Oduro A, Sankoh O, et al. Assessing the Catastrophic Effects of Out-of-Pocket Healthcare Payments Prior to the Uptake of a Nationwide Health Insurance Scheme in Ghana. Global Health Action. 2017;10(1):1289735.
[12] Onwujekwe OE, Uzochukwu BS, Obikeze EN, Okoronkwo I, Ochonma OG, Onoka CA. Investigating determinants of out‐of‐pocket spending and strategies for coping with payments for healthcare in southeast Nigeria. BMC Health Serv Res. 2010; 10:67.
[13] World Health Report. Health Systems Financing: The Path to Universal Coverage. Geneva: World Health Organization; 2010.
[14] Kalu-Umeh NN, Sambo MN, Idris SH, Kurfi AM. Costs and Patterns of Financing Maternal Health Care Services in Rural Communities in Northern Nigeria: Evidence for Designing National Fee Exemption Policy. International Journal of MCH and AIDS. 2013; 2(1): 163-172.
[15] PHC-MoU. Memorandum of Understanding (MoU) on the collaboration for Strengthening the Primary Health Care System between Niger State Government and Bill and Melinda Gates Foundation. October 10th, 2017.
[16] Transforming Primary Healthcare in Niger State: Highlights from the Niger State Primary Health Care Diagnostic Assessment. May 31st, 2016.
[17] National Population Commission (NPC) [Nigeria] and ICF. 2019. Nigeria Demographic and Health Survey 2018. Abuja, Nigeria, and Rockville, Maryland, USA: NPC and ICF.
[18] State Ministry of Health. Getting Ready for Universal Health Coverage in Niger State: A Stakeholder Assessment of Readiness and a Path Forward. Minna, Niger State. Nigeria. January 2018.
[19] Niger Health 1.0. Niger State Health Restoration Agenda. Niger State Ministry of Health. April 2016. Niger State Vision Document (Niger 1.0).
[20] NPHCDA. National Primary Health Care Under One Roof (PHCUOR) Scorecard Assessment. National Primary Health Care Development Agency. November 2019.
[21] Utan OE, Gooyabadi A. Patterns of African Healthcare Funding: Investment Implications for Public-Private Partnerships. Texila International Journal of Public Health DOI: 10.21522/TIJPH.2013.09.02. Art006.
[22] WHO. Public Financing for Health in Africa: From Abuja to the SDGs. Geneva: World Health Organization; 2016.
[23] Buigut S, Ettarh R, Amendah DD. Catastrophic health expenditure and its determinants in Kenya slum communities. International Journal for Equity in Health. 2015; May 14; 14(1): 46.
[24] Kusi A, Hansen KS, Asante FA, Enemark U. Does the National Health Insurance Scheme provide financial protection to households in Ghana? BMC Health Services Research. 2015 Aug 15; 15(1): 331.
[25] Aregbeshola BS. Out-of-pocket payments in Nigeria. Correspondence. Lancet. 2016 Jun 18; (387): 2506.
[26] Aregbeshola BS, Khan SM. Out-of-pocket payments, catastrophic health expenditure, and poverty among households in Nigeria 2010. Int J Health Policy Manag. 2018;7(9):798–806. doi:10.15171/ijhpm.2018.19.
[27] Adesina AD, Ogaji DS. Out-of-Pocket Payment for Healthcare and Implications for Households: Situational Analysis in Yenagoa, Bayelsa State. Journal of Community Medicine and Primary Health Care. 2020; 32 (1) 1-16.
[28] Onoka CA, Onwujekwe OE, Hanson K, Uzochukwu BS. Examining catastrophic health expenditures at variable thresholds using household consumption expenditure diaries. Tropical Medicine & International Health. 2011 Oct 1; 16(10): 1334-1341.
[29] Niger State Population Commission (NSPC). 2011.State Bureau of Statistics. Facts and Figures on Niger State Minna, Niger State. 2011 Edition. Available online from: https://nairametrics.com/wp-content/uploads/2013/05/Facts-and-Figures-about-Niger-State1.pdf.
[30] National Population Commission (NPC) (2006) Nigeria National Census: Population Distribution by Sex, State, LGAs and Senatorial District: 2006 Census Priority Tables (Vol. 3). http://www.population.gov.ng/index.php/publication/140-popn-distri-by-sex-state-jgas-and-senatorial-distr-2006.
[31] Swetha NB., Shobha, Sriram S. Assessment of out-of–pocket health expenditure and prevalence of protective mechanisms against it among the households in an urban area, Bangalore: a longitudinal study. Int. J. Community Med Public Health. 2019; 6, 263-7.
[32] Main causes of death in Nigeria 2019. Published by Statista Research Department, Mar 5, 2021. Available online from: https://www.statista.com/statistics/1122916/main-causes-of-death-and-disability-in-nigeria/.
Viewed PDF 1290 45 -
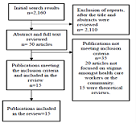 Discrimination and Stigma of Mentally Ill Patients among Health Care Workers and the Public in Developing Countries; its Effect on the Integration of Mental Health Services into the Primary Health Care System- A Systematic ReviewAuthor: Roxanne Stowe MaloneyDOI: 10.21522/TIJPH.2013.10.01.Art029
Discrimination and Stigma of Mentally Ill Patients among Health Care Workers and the Public in Developing Countries; its Effect on the Integration of Mental Health Services into the Primary Health Care System- A Systematic ReviewAuthor: Roxanne Stowe MaloneyDOI: 10.21522/TIJPH.2013.10.01.Art029Discrimination and Stigma of Mentally Ill Patients among Health Care Workers and the Public in Developing Countries; its Effect on the Integration of Mental Health Services into the Primary Health Care System- A Systematic Review
Abstract:
Discrimination and stigmatization against the mentally ill are issues of concern for years and have negatively affected the health outcomes of the mentally ill. The WHO has advised that integration of mental health services is necessary to close the treatment gap that currently exists. The aim of this paper is to synthesize evidence from various researchers regarding the presence of discrimination and stigma of mentally ill patients among health care workers and the public and to identify its effect on the integration of mental health services into the primary health care system. A systematic search was conducted in the PubMed, EBSCO HOST, Google scholar, MEDLINE databases. Fifteen (15) studies were evaluated to determine the level of stigma and discrimination towards the mentally ill patient by health professionals and the public. Studies conducted in developing countries identified that stigma and discrimination against the mentally ill among health care workers and members of the general public exists, and this negatively affects the integration process. Fear of seeking help from the health care service providers and administration of poor quality of health care to this category of patients are some of the effects. Stigma and discrimination are still major issues in developing countries; it is imperative that means of resolving these issues are developed. The gap in mental health treatment exists and is growing. Education: increased public awareness and good governance of the health system are just a few ways in which we can resolve these problems.
Discrimination and Stigma of Mentally Ill Patients among Health Care Workers and the Public in Developing Countries; its Effect on the Integration of Mental Health Services into the Primary Health Care System- A Systematic Review
References:
[1] World Health Organization, 2001, The World health report 2001: Mental Health: New understanding, new hope. World Health Organization, Switzerland.
[2] American Psychological Association, 2019, Discrimination: what it is, how to cope, https://www.apa.org/topics/racism-bias-discrimination/types-stress.
[3] Oxford reference, 2021, Stigma, https://www.oxfordreference.com/view/10.1093/oi/authority.20111007171501221.
[4] World Health Organization, 2019, Mental disorders, https://www.who.int/news-room/fact-sheets/detail/mental-disorders.
[5] Thorncroft, G., Rose, D. Kassam, A., 2007, Discrimination in health care against people with mental illness. International Review of Psychiatry, 19:2, 113-122, https://doi.org/10.1080/09540260701278937.
[6] Bjorkman, T., Angelman, T., Jonsson, M., 2008, Attitudes towards people with mental illness: a cross-sectional study among nursing staff in psychiatric and somatic care. Scandinavian journal of caring sciences, https://doi.org/10.1111/j.14716712.2007.00509.x.
[7] Alfredsson, M., Sebastian, M.S. & Jeghannathan B., 2017, Attitudes towards mental health and the integration of mental health services into primary health care: a cross-sectional survey among health-care workers in Lvea Em District, Cambodia. Global Health Action. 10:1,133157, https://doi.org/10.1080/16549716.2017.1331579.
[8] Loch, A.A., Guarniero, F.B., Lawson, F.L., Hengartner, M.P., Rossler, W., Gattaz, W. F. & Wang, Y.P., 2013, Stigma towards schizophrenia: do all psychiatrists behave the same? Latent profile analysis of a national sample of psychiatrists in Brazil. Biomed Central Psychiatry. 13:92, https://doi.org/10.1186/1471-244X-13-92.
[9] Egbe, C.O., Brooke-Sumner, C., Kathree, T., Selohilwe, O. & Thornicroft, G., 2014, Psychiatric stigma and discrimination in South Africa: perspectives from key stakeholders. BMC Psychiatry 14, 191, https://doi.org/10.1186/1471-244X-14-191.
[10] Hanafiah, A.N, & Van Bortel, T.A., 2015, A qualitative exploration of the perspectives of mental health professionals on stigma and discrimination of mental illness in Malaysia. International Journal of Mental Health Systems, 9, 10, https://doi.org/10.1186/s13033-015-0002-1.
[11] Kapungwe, A., Cooper, S., Mwanza, J., Mwape, L., Sikwese, A., Kakuma, R., Lund, C., Flisher, AJ. & The Mental Health and Poverty Project Research Programme Consortium, 2010, Mental illness-stigma and discrimination in Zambia. African Journal of Psychiatry, 13(3), 192-203, https://www.ajol.info/index.php/ajpsy/article/view/57913.
[12] Kapungwe, A., Cooper, S., Mayeya, J., Mwanza, J., Mwape, L., Sikwese, A., Lund, C., & Mental Health and Poverty Project Research Programme Consortium, 2011, Attitudes of primary health care providers towards people with mental illness: evidence from two districts in Zambia. African journal of psychiatry, 14(4), 290–297, https://doi.org/10.4314/ajpsy.v14i4.6.
[13] Luitel, N.P.; Jordans, M.J.D.; Subba, P.; & Komproe, I.H., 2020, Perception of service users and their caregivers on primary care-based mental health services: a qualitative study in Nepal. BMC Family Practice 21, 202, https://doi.org/10.1186/s12875-020-01266-y.
[14] James, B. O., Omoaregba, J. O., & Okogbenin, E. O., 2012, Stigmatising attitudes towards persons with mental illness: a survey of medical students and interns from southern Nigeria. Mental illness, 4(1), e8, https://doi.org/10.4081/mi.2012.e8.
[15] Youssef, F., 2018, Attitudes toward mental illness among Caribbean medical students. Education for Health. 31:3-9, http://doi.org/10.4103/1357-6283.239029.
[16] Hanlon, C., Eshetu, T., Alemayehu, D., Fekadu, A., Semrau, M., Thornicroft, G., Kigozi, F., Marais, D.L., Petersen, I. & Alem, A., 2017, Health system governance to support scale-up of mental health care in Ethiopia: A qualitative study. International Journal of Mental Health Systems 11, 38, https://doi.org/10.1186/s13033-017-0144-4.
[17] Mfoafo-M’Carthy, M. & Sossou, M.A., 2017, Stigma, Discrimination, and Social Exclusion of the Mentally Ill: The Case of Ghana. Journal of Human Rights and Social Work 2, 128–133, https://doi.org/10.1007/s41134-017-0043-2.
[18] Jenkins, R.; Othieno C.; Okeyo, S.; Aruwa, J.; Kingora, J. & Jenkins, B., 2013, Health system challenges to integration of mental health delivery in primary care in Kenya- perspectives of primary care health workers. BMC Health Services Research 13, 368, https://doi.org/10.1186/1472-6963-13-368.
[19] Liang, D.; Mays, V.; Hwang W., 2017, Integrated mental health services in China: challenges and planning for the future. Health Policy and Planning 33(1), 107-122, https://doi.org/10.1093/heapol/czx137.
[20] Hickling, F.W., Robertson-Hickling, H. & Paisley V., 2011, Deinstitutionalization and attitudes toward mental illness in Jamaica: a qualitative study. ev Panam Salud Publica. 29(3):169–76, https://www.scielosp.org/article/ssm/content/raw/?resource_ssm_path=/media/assets/rpsp/v29n3/04.pdf.
[21] Hussain, S. S., Khan, M. M., Gul, R. B., Asad, N., 2018, Integration of mental health into primary healthcare: Perceptions of stakeholders in Pakistan. Eastern Mediterranean Health Journal, 24(2), 146-153, https://ecommons.aku.edu/pakistan_fhs_mc_psychiatry/109.
[22] Adebowale, T., Umukoro, O.L., Gater, R., Akinhanmi, A., Ogunlesi A., Helme, C., Wood, G. & Ibikunle, I., 2014, Evaluation of a Mental Health Training Course for Primary Health Care Workers in Ogun State, Southwest, Nigeria. Journal of Psychiatry, 17:5, 14-25, http://dx.doi.org/10.4172/Psychiatry.1000141.
Viewed PDF 1280 47 -
 4 Dimensional X-Strain Speckle Tracking Echocardiography: Assessment of Normal Values of Left Ventricular Rotation and Twist, in Healthy Indian Adults during Covid-19 PandemicAuthor: Akhil MehrotraDOI: 10.21522/TIJPH.2013.10.01.Art030
4 Dimensional X-Strain Speckle Tracking Echocardiography: Assessment of Normal Values of Left Ventricular Rotation and Twist, in Healthy Indian Adults during Covid-19 PandemicAuthor: Akhil MehrotraDOI: 10.21522/TIJPH.2013.10.01.Art0304 Dimensional X-Strain Speckle Tracking Echocardiography: Assessment of Normal Values of Left Ventricular Rotation and Twist, in Healthy Indian Adults during Covid-19 Pandemic
Abstract:
Cardiac MRI and 2Dimensional speckle Tracking Echocardiography (2D STE) are the most sought-after methods to evaluate LV twist mechanics. LV rotational deformation resembles the wringing of a towel, and this deformation is referred as LV twist (LVT), and the subsequent recoil in diastole is known as LV untwist (LVUT). 2D/3D/4D twist mechanics assessment by STE is inherently associated with limitations. Recently introduced 4D XStrain STE has been used for evaluation of strain parameters because of better appraisal of contractile properties of LV, to analyse complex multi-dimensional LV rotational mechanics. This novel technology is a reliable, affordable, and simple tool for quantification of regional myocardial functions, particularly LV strain and rotation parameters. To evaluate and establish the normal values of LV rotation and twist by 4D XStrain STE in healthy Indian adults during the Covid-19 pandemic was the aim of the current study. 46 subjects were enrolled (34 males & 12 females). LA size, LV mass, CO, LVEDV and mitral E/A ratio were significantly greater in males (p<0.01) even though EF was higher in females (p<0.01). GLS, GCS, and GRS were increased in males (p<0.01). Peak basal rotation, peak twist, peak twist rate, and peak untwist rate were also greater in males (p<0.01), nonetheless, peak apical rotation and papillary muscle rotational velocity were greater in females (p<0.01). However, MV rotational velocity was increased in males (p<0.01). This is the first research publication of normal values of LV rotation and twists in healthy Indian adults by 4D XStrain STE.
4 Dimensional X-Strain Speckle Tracking Echocardiography: Assessment of Normal Values of Left Ventricular Rotation and Twist, in Healthy Indian Adults during Covid-19 Pandemic
References:
[1] Lower R. Tractatus de Corde, London, UK: Oxford University Press, 1669.
[2] Arts T, Hunter WC, Douglas AS, et al. Macroscopic three-dimensional motion patterns of the left ventricle. Adv Exp Med Biol 1993; 346:383-92.
[3] Hansen DE, Daughters GT 2nd, Alderman EL, Ingels NB Jr., Miller DC. Torsional deformation of the left ventricular midwall in human hearts with intramyocardial markers: regional heterogeneity and sensitivity to the inotropic effects of abrupt rate changes. Circ Res 1988:62:941-52.
[4] Bell SP, Nyland L, Tischler MD, et al. Alterations in the determinants of diastolic suction during pacing tachycardia. Circ Res 2000; 87:235-40.
[5] Gorman JH 3rd, Gupta KB, Streicher JT, et al. Dynamic three-dimensional imaging of the mitral valve and left ventricle by rapid sonomicrometry array localization. J Thorac Cardiovasc Surg 1996; 112:712-26.
[6] Gibbins Krocker CA, Ter Keurs HE, Knudtson ML, Tyberg JV, Beyar R. An optical device to measure the dynamics of apex rotation of the left ventricle AM j physiol 1993; 265:H1444-9.
[7] Marcelli E, Plicchi G, Cercenclli L, Bortolami F. First experimental evaluation of cardiac apex rotation with an epicardial coriolis force sensor ASAIO J 2005; 51:696-701.
[8] Buchalter MB, Weiss JL, Rogers WJ, et al. Non-invasive quantification of left ventricular rotational deformation in normal humans using magnetic resonance imaging myocardial tagging Circulation 1990;81:1236-44.
[9] Buchalter MB, Rademakers FE, Weiss JL, et al. Rotational deformation of the canine left ventricle measured by magnetic resonance tagging effects of catecholamines, ischaemia, and pacing, Cardiovasc Res 1994;28:629-35.
[10] Lorenz CH, Pastorek JS, Bundy JM. Delineation of normal human left ventricular twist throughout systole by tagged cine magnetic resonance imaging. J Cardiovasc Magn Reson 2000; 2:97-108.
[11] Kim HK, Sohn DW, Lee SE, et al. Assessment of left ventricular rotation and torsion with two-dimensional speckle tracking echocardiography. J Am Soc Echocardiogr 2007; 20:45-53.
[12] Notomi Y, Lysyansky P, Setser RM, et al. Measurement of ventricular torsion by two-dimensional ultrasound speckle tracking imaging. J Am Coll Cardiol 2005; 45:2034-41.
[13] Notomi Y, Setser RM, Shiota T, et al. Assessment of left ventricular torsional deformation by Doppler tissue imaging: validation study with tagged magnetic resonance imaging. Circulation 2005; 111:1141-7.
[14] Helle-Valle T, Crosby J, Edvardsen T, et al. New non-invasive method for assessment of left ventricular rotation: speckle tracking echocardiography. Circulation 2005; 112:3149-56.
[15] Kaku K, Takeuchi M, Tsang W, Takigiku K, Yasukochi S, Patel AR, Mor Avi V, Lang RM, Otsuji Y. Age-related normal range of left ventricular strain and torsion using three-dimensional speckle-tracking echocardiography. J Am Soc Echocardiogr. 2014; 27:55-64. DOI: 10.1016/j. echo.2013.10.002.
[16] Takahashi K, Al Naami G. Thompson R, Inage A, Mackie AS, Smallhorn JF. Normal rotational, torsion, and untwisting data in children, adolescents, and young adults. J Am Soc Echocardiogr. 2010; 23:286-293. DOI: 10.1016/j.echo.2009.11.018.
[17] Omar AMS, Vallabhajosyula S, Sengupta P: Left ventricular twist and torsion. Research observations and clinical applications. Circ Cardiovasc Imaging 2015; 8: e003029.
[18] Sengupta PP, Tajik AJ, Chandrasekaran K, Khandheria BK. Twist mechanics of the left ventricle: principles and application. JACC Cardiovasc Imaging. 2008; 1:366-376. DOI: 10.1016/j.jcmg.2008.02.006.
[19] Burns AT, La Gerche A. Prior DL, Macisaac Al. Left ventricular untwisting is an important determinant of early diastolic function. JACC Cardiovasc Imaging. 2009:2:709-716. DOI: 10.1016/j.jcmg.2009.01.015.
[20] Sengupta PP, Krishnamoorthy VK, Korinek J, Narula J, Vannan MA, Lester SJ, Tajik JA, Seward JB, Khandheria BK, Belohlavek M. Left ventricular form and function revisited: applied translational science to cardiovascular ultrasound imaging. J Am Soc Echocardiogr.2007; 20: 539-551.DOI: 10.1016/j.echo.2006.10.013.
[21] Notomi Y, Lysyansky P. Setser RM, Shiota T, Popovic ZB, Martin-Miklovic MG, Weaver JA, Oryszak SJ, Greenberg NL, White RD, Thomas JD. Measurement of ventricular torsion by two-dimensional ultrasound speckle tracking imaging. J Am Coll Cardiol. 2005; 45:2034-2041. DOI: 10.1016/j.jacc.2005.02.082.
[22] Young AA, Cowan BR. Evaluation of left ventricular torsion by cardiovascular magnetic resonance. J Cardiovasc Magn Reson. 2012; 14:49. DOI: 10.1186/1532-429X-14-49.
[23] Jung B, Zaitsev M, Hennig J, Markl M. Navigator gated high temporal resolution tissue phase mapping of myocardial motion, Magn Reson Med. 2006;55:937-942. DOI: 10.1002/mrm.20808.
[24] Goffinet C, Chenot F, Robert A, et al. Assessment of sub endocardial vs. subepicardial left ventricular rotation and twist using two-dimensional speckle tracking Echocardiography: Comparison with tagged cardiac magnetic resonance. Eur Heart J 2009; 30:608-617.
[25] Muraru, D.; Niero, A.; Zanella, H. R.; Cherata, D.; Badano, L.P. Three-dimensional speckle tracking echocardiography: Benefits and limitations of integrating myocardial mechanics with three-dimensional imaging. Cardiovasc. Diagn. Ther. 2018, 8, 101-117.
[26] Friedewald WT, Levy RI, Fredrickson Estimation of the concentration of density lipoprotein in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972; 18:499-502.
[27] Lang, R. M., Bierig, M., Devereux, R. B., et al. (2005) Recommendations for Chamber Quantification: A Report from the American Society of Echocardiography’s Guidelines and Chamber Quantification Writing Group. Developed in Conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. Journal of the American Society of Echocardiography, 18, 1440-1463.
[28] Devereux, R. B., Alonso, D.R., Lutas, E. M., Gottlieb, G.J., Campo, E., Sachs, I., et al.: (1986) Echocardiographic Assessment of Left Ventricular Hypertrophy. Comparison to Necropsy Findings. American Journal of Cardiology, 57,450-458.
[29] Sengupta, P.P., Tajik, A. J., Chandrasekaran, K. and Khandheria, B. K. (2008) Twist Mechanics of the Left Ventricle: Principles and Application. JACC. Cardiovascular Imaging. 1, 366-376.
[30] Nakatani S. Left ventricular rotation and twist: why should we learn? J Cardiovasc Ultrasound. (2011) 19:1-6.
[31] Nemes A, Kalapos A, Domsik P, Forster T. [Left ventricular rotation and twist of the heart. Clarification of some concepts]. Orv Hetil. (2012) 153:1547-51.
[32] Kormanyos A, Kalapos A, Domsik P, Lengyel C, Forster T, Nemes A. Normal values of left ventricular rotational parameters in healthy adults-Insights from the three-dimensional speckle-tracking echocardiographic MAGYAR-Healthy study. Echocardiography. (2019) 36:714-21.
[33] Gonenc Kocabay, Denisa Muraru, Diletta Peluso, Umberto Cucchini Sorina Mihaila, Seena Padayattil-Jose, Denas Gentian, Sabino Iliceto, Dragos Vinereanu, Luigi P. Badano. Normal Left ventricular mechanics by two-dimensional speckle tracking echocardiography. Reference values in healthy adults. Rev Esp Cardiol. 2014; 67:651-8.
[34] Nirvarthi Maharaj, Ferande Peters, Bijoy K. Khandheria, Elena Libhaber, Mohammed R. Essop, Left ventricular twist in a normal African adult population, European Heart Journal-Cardiovascular Imaging, Volume 14, Issue 6, June 2013, Pages 526-533.
[35] Kormanyos A, Kalapos A, Domsik P, Lengyel C, Forster T, Nemes A, Normal values of left ventricular rotational parameters in healthy adults-Insights form the three-dimensional speckle tracking echocardiographic MAGYAR-Healthy Study. Echocardiogarphy. 2019 Apr;36 (4):714-721.
[36] Zhang, Li & Zhang, Jing & Han, Wei & Gao, Jun & He, Lin & Yang, Yali & Yin, Ping & Xie, Mingxing & Ge, Shuping. (2016). Three-Dimensional Rotation, Twist and Torsion Analyses Using Real-Time 3D Speckle Tracking Imaging: Feasibility, Reproducibility, and Normal Ranges in Pediatric Population. Plos One.
[37] Yilmaz, Sabiye & Kilic, Harun & Demirtas, Saadet & Vatan, Mehmet & Edem, Efe & Agac, Mustafa & Pabuccu, Mustafa & Caker, Mehmet & Vural, Mustafa G & Aksoy, Murat & Tatli, Ersan & Gunduz, Huseyin & Akdemir, Ramazan. (2017). Age-ralated Changes in the Left Ventricular Twist. Kosuyolu Heart Journal. 20. 1225-129.
[38] Mor-Avi, Lang RM, Badano LP, Zamorano JL, et al. Current and evolving echocardiographic techniques for the quantitative evaluation of cardiac mechanics: ASE/EAE consensus statement on methodology and indications endorsed by the Japanese Society of Echocardiography. J Am Soc Echocardiogr. 2011; 24:277-313.
[39] Pedrizzetti G, Sengupta S, Caracciolo G, et al. Three-dimensional principal strain analysis for characterizing subclinical changes in left ventricular function. J Am Soc Echocardiogr. 2014; 27:1041.
[40] Bhan A, sirker A, Zhang J et al. High frequency speckle tracking echocardiography in the assessment of left ventricular function and remodeling after murine myocardial infarction. Am J Physiol Heart Circ Physiol. 2014; 306:H1371-H1383.
Viewed PDF 1283 33

