Clinical Manifestations of Cryptococcal Meningitis in HIV Negative Patients-A Case Study
Abstract:
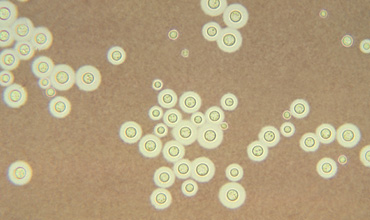
Cryptococcal Meningitis (CM) is a central nervous
system infection caused by a fungus. A large majority of cases are caused by
Cryptococcus neoformans var. neoformans. The fungus C. neoformans is found in
soil that contains bird droppings, particularly pigeon excreta, all over the
world. Cryptococcusneoformans var. gatti, on the other hand, is found primarily
in tropical and subtropical regions trees, most commonly eucalyptus trees. It
grows in the debris around the trees’ bases. Cryptococcal meningitis usually
occurs in people who have a compromised immune system and is a rare occurrence
in someone who has a normal immune system. Of the two fungi, Cryptococcalgattii
is the one more likely to infect someone with a normal immune system.The
incidence of infections caused by C.neoformans has risen markedly over the past
20 years as a result of the HIV/AIDS epidemic and increasing use of
immunosuppressive therapies. Cryptococcal meningitis is a common opportunistic
infection and an AIDS-defining illness in patients with late-stage HIV
infection, particularly in Southeast Asia and Southern and East Africa. It is
widely considered as the most common life-threatening AIDS related fungal
infection. Cryptococcal meningitis has been estimated at about 70 to 90%
worldwide in AIDS patients with mortalities of between 50% to 70% in
Sub-Saharan Africa. [2,3,4] Mortality from HIV-associated cryptococcal
meningitis remains high (13–33%), even in developed countries, because of the
inadequacy of current antifungal drugs and combinations, and the complication
of raised intracranial pressure.[2,7,8]In the cases presented, the findings
were so non-specific that the diagnosis was highly dependent on the CSF findings.
Based on the characteristics of the presenting signs and symptoms, Cryptococcal
meningitis should always be included in the differential diagnosis of chronic
or subacute meningoencephalitis, since clinical features are not specific.
References:
[1.] 2013-14
Zambia Demographic Health Survey
[2.] Abadi et
al. 1999
[3.] Casadevall
A (1998): Cryptococcus neoformans. Washington, DC: ASM Press, Perfect JR
[4.] Centers for
Disease Control and Prevention: C. gattii Infection Statistics (http://www.cdc.gov/fungal/diseases/cryptococcosis-gattii/statistics.html),
last updated May 2015.
[5.] Dr. Stephen
Berger (2015).Cryptococcosis: Global Status, By GIDEON Informatics, Inc.,
[6.] Dr. Peter
Mwaba (BSc.Hb.MBChB): The clinical and laboratory setting of cyptococcal
meningitis as seen at university teaching hospital, Lusaka and to evaluate
efficacy of fluconazole in its therapy, 1997.
[7.] French N,
Gray K, Watrea C et al. (2002) Cryptococcal infection in a cohort of
HIV-1-infected Ugandan adults. AIDS, 16, 1031–1038.
[8.] Geneva,
World Health Organization: Rapid advice: diagnosis, prevention and management
of cryptococcal disease in HIV infected adults, adolescents and children, 2013.
[9.] Holmes CB,
Losina E, Walensky RP, Yazdanpanah Y, Freedberg K :Review of human
immunodeficiency virus type 1-related opportunistic infections in Sub-Saharan
Africa, Clin Infect Dis, 36, 652–662. (2003)
[10.] John W
King, MD( 2014).Cryptococcosis
[11.] Kaplan JE,
Masur H, Holmes KK, USPHS, Infectious Diseases Society of America (2002)
Guidelines for Preventing Opportunistic Infections Among HIV-Infected Persons
2002. Recommendations of the U.S. Public Health Service and the Infectious
Diseases Society of America. MMWR Recomm Rep, 51: 1–46.
[12.] Lalloo D,
Fisher D, Naraqi S, Laurenson I, Temu P, Sinha A, et al. Cryptococcal
meningitis (C. neoformans var. gattii) leading to blindness in previously
healthy Melanesian adults in Papua New Guinea. The Quarterly journal of
medicine. 1994 Jun;87(6):343-9.
[13.] Mwaba P.
Mwansa J, Chintu C et al. (2001) Clinical presentation, natural history, and
cumulative death rates of 230 adults with primary cryptococcal meningitis in
Zambian AIDS patients treated under local conditions. Postgrad Med J, 77,
769–773.
[14.] McCarthy
et al. 2006
[15.] Meiring et
al. 2012.
[16.] Meiring
ST, Quan VC, Cohen C, Dawood H, Karstaedt AS, McCarthy KM, Whitelaw AC,
Govender NP, Group for Enteric, Respiratory and Meningeal disease Surveillance
in South Africa (GERMS-SA) AIDS. 2012 Nov 28; 26(18):2307-14. [PubMed] A
comparison of cases of paediatric-onset and adult-onset cryptococcosis detected
through population-based surveillance, 2005-2007.
[17.] Robinson
PA, Bauer M, Leal ME et al. (1999) Early mycological treatment failure in
AIDS-associated cryptococcal meningitis. Clin Infect Dis, 28, 82–92.
[18.] Seaton RA,
Naraqi S, Wembri JP, Warrell DA (1996) Predictors of outcome in Cryptococcus
neoformans var. gattii meningitis. Q J Med, 89, 423–8.
[19.] Sarah S.
Long, Larry K. Pickering, Charles G. Prober: Principles and Practice of
Pediatric Infectious Diseases, 2012 (https://books.google.co.zm/books?isbn=1455739855)
[20.] Sloan D1,
Dlamini S, Paul N, Dedicoat M. Treatment of acute cryptococcal meningitis in
HIV infected adults, with an emphasis on resource-limited settings. [Cochrane
Database Syst Rev. 2008 Oct 8;(4):CD005647. doi:
10.1002/14651858.CD005647.pub2.
[21.] Tihana
Bicanic and Thomas S. Harrison: Cryptococcal meningitis. British Medical
Bulletin, (February, 2005).
[22.] The
Nigerian Journal of Medicine, Vol.19, No. 4 October - December 2010.
[23.] Thomas KE,
Hasbun R, Jekel J, Quagliarello VJ (2002). "The diagnostic accuracy of
Kernig's sign, Brudzinski's sign, and nuchal rigidity in adults with suspected
meningitis". Clin. Infect. Dis. 35 (1): 46–52. doi:10.1086/340979. PMID
12060874.
[24.] Yuanjie
Z1, Jianghan C, Nan X, Xiaojun W, Hai W, Wanqing L, Julin G. Cryptococcal
meningitis in immunocompetent children. Mycoses. 2012 Mar;55(2):168-71. doi:
10.1111/j.1439-0507.2011.02063.x. Epub 2011 Jul 18.

