Therapeutic Applications of Fluorides in Dental and Medical Diseases-A Systematic Review
Abstract:
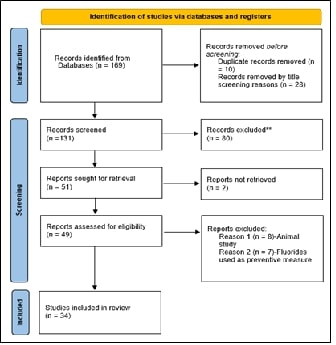
A
systematic review was conducted to evaluate the therapeutic applications of
fluoride, focusing on dental and medical uses. Searches were performed across
five major databases: PubMed, Embase, Cochrane Library, Scopus, and Web of
Science. A combination of MeSH terms and keywords was used to cover four
domains: Fluorides, Dental Therapeutics, Medical Therapeutics, and Outcomes.
Inclusion criteria focused on human studies published in English between 2000
and 2024, while exclusion criteria eliminated non-human studies, irrelevant
topics, and grey literature. This systematic review analyzed 34 studies on
fluoride's therapeutic uses. Fluoride was consistently effective in preventing
and managing dental caries, with combinations like 38% silver diamine fluoride
(SDF) and 5% sodium fluoride (NaF) varnish showing higher efficacy.
High-fluoride mouth rinses and toothpaste reduced demineralized lesions in
orthodontic patients, while Arg-NaF varnishes are effective against enamel
erosion. Sodium hyaluronate with fluoride improved gingival health. Some studies noted potential
negative effects on dental materials, such as reducing sealant bond strength,
highlighting the need for further research on fluoride's broader applications
and material interactions. In medical contexts, fluoride demonstrated
stabilizing effects in conditions like otosclerosis and osteoporosis, though
findings were inconsistent across studies. Fluoride is observed to have a positive
role in preventing and treating dental and bone diseases. Studies showed
fluoride in specific doses could enhance tooth caries resistance and enamel
erosion. Fluorides act in controlling osteosclerosis and osteoporosis by stabilizing
disease progression and improving bone density. However, more research is
needed to fully understand its long-term effects and optimize its use in both
fields.
References:
[1]. Institute of Medicine (US) Standing Committee on the
Scientific Evaluation of Dietary Reference Intakes,1997, Dietary Reference
Intakes for Calcium, Phosphorus, Magnesium, Vitamin D, and Fluoride. Washington
(DC): National Academies Press (US); Available from:https://www.ncbi.nlm.nih.gov/books/NBK109825/doi:10.17226/5776.PMID: 23115811.
[2]. Aoun, A., Darwiche, F., Al Hayek, S., & Doumit, J., 2018,
The Fluoride Debate: The Pros and Cons of Fluoridation. Preventive
nutrition and food science, 23(3), 171–180. https://doi.org/10.3746/pnf.2018.23.3.171
[3]. Everett, E. T., 2011, Fluoride's effects on the formation of
teeth and bones, and the influence of
genetics. Journal of dental research, 90(5),
552–560. https://doi.org/10.1177/0022034510384626
[4]. U.S. Department of Health and Human Services Federal Panel on
Community Water Fluoridation 2015, U.S. Public Health Service Recommendation
for Fluoride Concentration in Drinking Water for the Prevention of Dental
Caries. Public health reports (Washington, D.C.: 1974), 130(4),
318–331. https://doi.org/10.1177/003335491513000408.
[5]. Iheozor-Ejiofor, Z., Worthington, H. V., Walsh, T., O'Malley,
L., Clarkson, J. E., Macey, R., Alam, R., Tugwell, P., Welch, V., & Glenny,
A. M., 2015, Water fluoridation for the prevention of dental caries. The
Cochrane database of systematic reviews, 2015(6), CD010856. https://doi.org/10.1002/14651858.CD010856.pub2.
[6]. U.S. Environmental Protection Agency. Review of the
Fluoride Drinking Water Regulation. 2019.
[7]. Petersen, P. E., & Lennon, M. A., 2004, Effective use of
fluorides for the prevention of dental caries in the 21st century: the WHO
approach. Community dentistry and oral epidemiology,32(5),319–321. https://doi.org/10.1111/j.1600-0528.2004.00175.x.PMID:15341615
[8]. Mankar, N., Kumbhare, S., Nikhade, P., Mahapatra, J.,
Agrawal, P., 2023, Role of Fluoride in Dentistry: A Narrative Review. Cureus.
2023 Dec 21;15(12):e50884. doi: 10.7759/cureus.50884. PMID: 38249196;
PMCID: PMC10799546.
[9]. Hoque, M. E., Showva, N. N., Ahmed, M., Rashid, A. B.,
Sadique, S. E., El-Bialy, T., & Xu, H., 2022, Titanium and titanium alloys
in dentistry: current trends, recent developments, and future prospects. Heliyon,
8(11), e11300. https://doi.org/10.1016/j.heliyon.2022.e11300 (Retraction
published Heliyon. 2024 May 27;10(11):e31978. doi:
10.1016/j.heliyon.2024.e31978).PMID: 36387463; PMCID: PMC9640965.
[10]. Medjedovic, E., Medjedovic, S., Deljo, D., & Sukalo, A.,
2015, Impact Of Fluoride On
Dental Health Quality. Materia Socio-Medica, 27(6),
395–398. Https://Doi.Org/10.5455/Msm. 2015. 27.395-398. Pmid: 26889098; Pmcid: Pmc4733546.
[11]. Kleerekoper, M., 1998, The role of fluoride in the prevention
of osteoporosis. Endocrinology and metabolism clinics of North America, 27(2),
441–452. https://doi.org/10.1016/s0889-8529(05)70015-3. PMID: 9669148.
[12]. Ginaldi, L., Mengoli, L. P., & De Martinis, M., 2009, Osteoporosis, inflammation and
ageing. In Handbook on Immunosenescence: Basic Understanding and Clinical
Applications (Vol. 9781402090639, pp. 1329–1352). Springer Netherlands.
https://doi.org/10.1007/978-1-4020-9063-9_64.
[13]. Haguenauer, D., Welch, V., Shea, B., Tugwell, P., &
Wells, G., 2000, Fluoride for treating postmenopausal osteoporosis. The
Cochrane database of systematic reviews, 2000(4), CD002825. https://doi.org/10.1002/14651858.CD002825.
[14]. Pak, C. Y., Adams-Huet, B., Sakhaee, K., Bell, N. H., Licata,
A., Johnston, C. et.al, 1996,
Comparison of nonrandomized trials with slow-release sodium fluoride with a
randomized placebo-controlled trial in postmenopausal osteoporosis. Journal
of bone and mineral research: the official journal of the American Society for
Bone and Mineral Research, 11(2), 160–168. https://doi.org/10.1002/jbmr.5650110204.
[15]. Abdellatif, E. B., El Kashlan, M. K., & El Tantawi, M.,
2023, Silver diamine fluoride with sodium fluoride varnish versus silver
diamine fluoride in arresting early childhood caries: a 6-months follow up of a
randomized field trial. BMC oral health, 23(1), 875. https://doi.org/10.1186/s12903-023-03597-5.
[16]. Pørksen, C. J., Ekstrand, K. R., Markvart, M., Larsen, T.,
Garrido, L. E., & Bakhshandeh, A., 2023, The efficacy of combined arginine
and probiotics as an add-on to 1450 ppm fluoride toothpaste to prevent and
control dental caries in children - A randomized controlled trial. Journal
of dentistry, 137, 104670. https://doi.org/10.1016/j.jdent.2023.104670.
[17]. Quritum, M., Abdella, A., Amer, H., & El Tantawi, M.,
2024, Effect of silver diamine fluoride and nano silver fluoride on oral
health-related quality of life of children with early childhood caries: A
randomized clinical trial. Journal of dentistry, 142, 104878. https://doi.org/10.1016/j.jdent.2024.104878.
[18]. Enerbäck, H., Lövgren, M. L., Strömberg, N., &
Westerlund, A., 2023, Effect of high-fluoride toothpaste and mouth rinse on the
prevention of demineralized lesions during orthodontic treatment: a randomized
controlled trial. European journal of orthodontics, 45(5),
477–484. https://doi.org/10.1093/ejo/cjad044.
[19]. Yip, K., Lam, P. P. Y., & Yiu, C. K. Y., 2022, Prevalence
and Associated Factors of Erosive Tooth Wear among Preschool Children-A
Systematic Review and Meta-Analysis. Healthcare (Basel,
Switzerland), 10(3), 491. https://doi.org/10.3390/healthcare10030491.
[20]. Axe, A., Burnett, G. R., Milleman, K. R., Patil, A., &
Milleman, J. L., 2019, Randomized Controlled Clinical Study to Determine the
Oral and Dermal Tolerability of an Experimental Denture Wipe. Journal
of prosthodontics : official journal of the American College of
Prosthodontists, 28(2), 138–145. https://doi.org/10.1111/jopr.12992.
[21]. Yassin, R., Amer, H., & Tantawi, M. E., 2023,
Effectiveness of silver diamine fluoride versus sodium fluoride varnish
combined with mother's motivational interviewing for arresting early childhood
caries: a randomized clinical trial. BMC oral health, 23(1),
710. https://doi.org/10.1186/s12903-023-03456-3.
[22]. Francese, M. M., Gonçalves, I. V. B., Vertuan, M., de Souza,
B. M., & Magalhães, A. C., 2022, The protective effect of the experimental
TiF4 and chitosan toothpaste on erosive tooth wear in
vitro. Scientific reports, 12(1), 7088. https://doi.org/10.1038/s41598-022-11261-1.
[23]. Bansal, K., Shamoo, A., Mani, K., K, P. D., Verma, A.,
Mathur, V. P., & Tewari, N., 2023, Silver diamine fluoride modified
atraumatic restorative treatment compared to conventional restorative technique
on carious primary molars-A randomized controlled trial. Journal of
dentistry, 138, 104698. https://doi.org/10.1016/j.jdent.2023.104698
[24]. Dhanapriyanka, M., Kosgallana, S., Kanthi, R. D. F. C.,
Jayasekara, P., Dao, T. M. A., Ha, D. H., & Do, L., 2024, Professionally
applied fluorides for preventing and arresting dental caries in low- and
middle-income countries: Systematic review. Journal of public health
dentistry, 84(2), 213–227. https://doi.org/10.1111/jphd.12617.
[25]. Peter, Joby & Chandra, H., & Sakhare, Dhanashree, 2023, Systemic Fluorides and Dental Health.
10.2174/9789815080803123030018.
[26]. Lubojanski, A., Piesiak-Panczyszyn, D., Zakrzewski, W.,
Dobrzynski, W., Szymonowicz, M., Rybak, Z.,
et.al; 2023, The Safety of Fluoride Compounds and Their Effect on
the Human Body-A Narrative Review. Materials (Basel,
Switzerland), 16(3), 1242. https://doi.org/10.3390/ma16031242.
[27]. Cumerlato, C. B. D. F., Santos, C. S. D., Rotta, R. N.,
Cademartori, M. G., & Corrêa, M. B., 2022, Is professionally applied
topical fluoride effective in treating incipient caries? A systematic
review. Brazilian oral research, 36, e083. https://doi.org/10.1590/1807-3107bor-2022.vol36.0083
[28]. Teimoory, N., Katebi, K., Ghahramanzadeh, A., & Vafaei,
A., 2023, Effects of
topical fluoride treatment on the bond strength of pit and fissure sealants: A
systematic review. Journal of dental research, dental clinics, dental
prospects, 17(2), 81–86. https://doi.org/10.34172/joddd.2023.39160
[29]. Sardana, D., Manchanda, S., Ekambaram, M., Yang, Y., McGrath,
C. P., & Yiu, C. K. Y., 2019, Effectiveness of self-applied topical
fluorides against enamel white spot lesions from multi-bracketed fixed
orthodontic treatment: a systematic review. European journal of
orthodontics, 41(6), 661–668. https://doi.org/10.1093/ejo/cjz015
[30]. Zhang, C., Yan, K., Fu, C., Peng, H., Hawker, C. J., &
Whittaker, A. K., 2022, Biological Utility of Fluorinated Compounds: from
Materials Design to Molecular Imaging, Therapeutics and Environmental
Remediation. Chemical reviews, 122(1), 167–208. https://doi.org/10.1021/acs.chemrev.1c00632.
[31]. Cruise, A. S., Singh, A., & Quiney, R. E., 2010, Sodium
fluoride in otosclerosis treatment: review. The Journal of laryngology
and otology, 124(6), 583–586. https://doi.org/10.1017/S0022215110000241.
[32]. Derks, W., De Groot, J. A., Raymakers, J. A., & Veldman,
J. E., 2001, Fluoride therapy for cochlear otosclerosis? an audiometric and
computerized tomography evaluation. Acta oto-laryngologica, 121(2),
174–177. https://doi.org/10.1080/000164801300043361.
[33]. Dequeker, J., & Declerck, K., 1993, Fluor in the
treatment of osteoporosis. An overview of thirty years clinical research. Schweizerische
medizinische Wochenschrift, 123(47), 2228–2234.
[34]. Shambaugh G. E., Fluoride Therapy for Otosclerosis. Arch Otolaryngol Head Neck Surg. 1990;116(10):1217.
doi:10.1001/archotol.1990.01870100111026.
[35]. Kerr, G. S., & Hoffman, G. S., 1989, Fluoride therapy for
otosclerosis. Ear, nose, & throat journal, 68(6), 426–429.
[36]. Caverzasio, J., Imai, T., Ammann, P., Burgener, D., & Bonjour,
J. P., 1996, Aluminum potentiates the effect of fluoride on tyrosine
phosphorylation and osteoblast replication in vitro and bone mass in
vivo. Journal of bone and mineral research: the official journal of the
American Society for Bone and Mineral Research, 11(1), 46–55. https://doi.org/10.1002/jbmr.5650110108.
[37]. Colletti, V., & Fiorino, F. G., 1991, Effect of sodium
fluoride on early stages of otosclerosis. The
American journal of otology, 12(3), 195–198.PMID: 1882968.
[38]. Linthicum, F. H., Jr, House, H. P., & Althaus, S. R.,
1973, The effect of sodium fluoride on otosclerotic activity as determined by
strontium. The Annals of otology, rhinology, and laryngology, 82(4),
609–615. https://doi.org/10.1177/000348947308200417.
[39]. Rich, C., Ensinck, J., & Ivanovich, P., 1964, The Effects
Of Sodium Floride On Calcium Metabolism Of Subjects With Metabolic Bone
Diseases. The Journal of clinical investigation, 43(4),
545–555. https://doi.org/10.1172/JCI104940.
[40]. Shambaugh, G. E., Jr, & Petrovic, A., 1968, Effects of
sodium fluoride on bone. Application to otosclerosis and other decalcifying
bone diseases. JAMA, 204(11), 969–973.
[41]. Rich, C., & Ivanovich, P., 1965, Response to sodium fluoride in severe primary
osteoporosis. Annals of internal medicine, 63(6), 1069–1074. https://doi.org/10.7326/0003-4819-63-6-1069.
[42]. Valeria, Gaudieri., Emilia, Zampella., Adriana, D'Antonio., Alberto,
Cuocolo. 18F-sodium fluoride and vascular calcification: Some like it
hot. Journal of Nuclear Cardiology, (2020).1-3. doi: 10.1007/S12350-020-02125-0
[43]. Haguenauer, D., Welch, V., Shea, B., Tugwell, P., Adachi, J.
D., & Wells, G., 2000, Fluoride for the treatment of postmenopausal
osteoporotic fractures: a meta-analysis. Osteoporosis International: a
Journal established as result of cooperation between the European Foundation
for Osteoporosis and the National Osteoporosis Foundation of the USA, 11(9),
727–738. https://doi.org/10.1007/s001980070051.
[44]. Aaseth, Jan & Shimshi, Mona & Gabrilove, J., &
Birketvedt, Grethe, 2004, Fluoride: A Toxic or Therapeutic Agent in the
Treatment of Osteoporosis. The Journal of Trace Elements in Experimental
Medicine. 17. 83 - 92. 10.1002/jtra.10051.
[45]. Karjalainen, S., Kärjä, J., Härmä, R., & Juola, E., 1982,
Effect of drinking water fluoridation on stapedial otosclerosis in a low
fluoride area. Acta oto-laryngologica, 94(1-2), 111–119. https://doi.org/10.3109/00016488209128895.
[46]. Gold, S. R., Miller, V., Kamerer, D. B., & Koconis, C.
A., 1998, Fluoride treatment for facial nerve stimulation caused by cochlear
implants in otosclerosis. Otolaryngology--head and neck surgery :
official journal of American Academy of Otolaryngology-Head and Neck Surgery, 119(5),
521–523. https://doi.org/10.1016/S0194-5998(98)70116-0.
[47]. Vartiainen, E., Karjalainen, S., Nuutinen, J., Suntioinen,
S., & Pellinen, P., 1994, Effect of drinking water fluoridation on hearing
of patients with otosclerosis in a low fluoride area: a follow-up study. The
American journal of otology, 15(4), 545–548.
[48]. Lewy A., 1944, Possible Value Of Nontoxic Concentrations Of Fluorine In The
Prevention of Deafness
From Otosclerosis And Fibrosis: Its Possible Value In Prevention Of Other
Diseases. Arch Otolaryngol. 39(2):152–154.
doi:10.1001/archotol.1944.00680010163005.
[49]. Ismail, A. I., & Hasson, H., 2008, Fluoride supplements,
dental caries and fluorosis: a systematic review. Journal of the
American Dental Association (1939), 139(11), 1457–1468. https://doi.org/10.14219/jada.archive.2008.0071.
[50]. Rošin-Grget, K., Peroš, K., Sutej, I., & Bašić, K., 2013,
The cariostatic mechanisms of fluoride. Acta medica academica, 42(2),
179–188. https://doi.org/10.5644/ama2006-124.85.
[51]. Featherstone, J. D., 1999, Prevention and reversal of dental
caries: role of low level fluoride. Community dentistry and oral
epidemiology, 27(1), 31–40. https://doi.org/10.1111/j.1600-0528.1999.tb01989.x

