Assessment of Infection Prevention and Control (IPC) in Healthcare Facilities in Complex Humanitarian Emergencies - Cox’s Bazar Rohingya Refugee Camps - 2020
Abstract:
Infection
prevention and control (IPC) is crucial for the prevention of healthcare-associated
infections (HAIs) in healthcare facilities (HFs). The World Health Organization
(WHO) published eight core components (CCs) of IPC to guide IPC program
implementation in HFs. WHO also developed the IPC Assessment Framework (IPCAF)
tool to assess the level of IPC program implementation and identify areas for
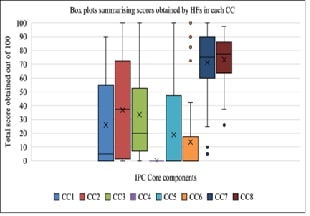
improvement in HFs. We conducted a cross-sectional study in Nov 2024 using the IPCAF
tool by extracting data from February 2020 IPCAF reports from 45 HFs in
Rohingya refugee camps. Conducted descriptive analysis using SPSS 29 for each IPC
CC, total IPC scores per HF and level of IPC promotion and practices obtained. 46.7%
of HFs scored as inadequate, 37.8% scored as basic, 11.1% as intermediate level
and 4.4% scored as an advanced level of IPC. 71% of the HFs did not have an IPC
program, 84% lacked standard precaution guidelines, 60% had not provided any
IPC training and none conducted HAI surveillance. 69% of the HFs did not follow
the multimodal strategy for IPC while 82% did not monitor IPC activities. 71%
of HFs had appropriate staffing, workload and bed occupancy and 51.1% of HFs
had functional hand hygiene stations at all points of care. There were no HFs
in the Rohingya refugee camps with fully implemented IPC programs in 2020. An
IPC program that aims at implementing all core components of the IPC program
should be considered for HFs in Cox’s Bazar refugee camps and similar settings.
References:
[1].
World
health Organization. 2024, August 3, Infection Prevention and Control. Infection
Prevention and Control Overview. https://www.who.int/health-topics/infection-prevention-and-control#tab=tab_1
[2].
World
Health Organisation. (n.d.). Infection prevention and control. Who.Int.
Retrieved March 15, 2020, from https://www.who.int/infection-prevention/en/
[3].
World
Health organization., 2023, Global strategy on infection prevention and
control.
[4].
World
Health Organization, 2020, Operational planning guidance to support country
preparedness and response. COVID 19 strategic preparedness and response. 22 May
2020. COVID-19: Critical preparedness, readiness and response.
[5].
World
Health Organization., 2021, Infection prevention and control during health care
when coronavirus disease (COVID-19) is suspected or confirmed. interim
guidance. 12 July 2021.
[6].
United
Nations, 2015, Transforming our world: the 2030 agenda for sustainable
development. 2015. https://sdgs.un.org/2030agenda
[7].
World
health Organization., 2015, Global Action Plan on Antimicrobial Resistance
2015.
[8].
World
Health Organization, 2005, International Health Regulations (2005) - Third
Edition. (World Health Organization, Ed.; Third, Vol. 3). World Health
organization. https://iris.who.int/bitstream/handle/10665/246107/9789241580496-eng.pdf
[9]. World Health
Organization, 2016, Health care without avoidable infections: the critical role
of infection prevention and control. World Health Organization.
[10].
Shackelford,
B. B., Cronk, R., Behnke, N., Cooper, B., Tu, R., D’Souza, M., Bartram, J.,
Schweitzer, R., & Jaff, D., 2020, Environmental health in forced
displacement: A systematic scoping review of the emergency phase. Science of
the Total Environment, 714. https://doi.org/10.1016/j.scitotenv.2020.136553
[11].
Breiman,
R. F., Shultz, A., Omollo, J. O., Burke, H., Qassim, M., Ochieng, J. B.,
Weinberg, M., & Feikin, D. R., 2009, Cholera outbreak in kenyan refugee
camp: Risk factors for illness and importance of sanitation. American
Journal of Tropical Medicine and Hygiene, 80(4). https://doi.org/10.4269/ajtmh.2009.80.640
[12].
Connolly,
M. A., Gayer, M., Ryan, M. J., Salama, P., Spiegel, P., & Heymann, D. L.,
2004, Communicable diseases in complex emergencies: Impact and challenges. In
Lancet (Vol. 364, Issue 9449). https://doi.org/10.1016/S0140-6736(04)17481-3
[13].
Behnke,
N. L., Cronk, R., Shackelford, B. B., Cooper, B., Tu, R., Heller, L., &
Bartram, J., 2020, Environmental health conditions in protracted displacement:
A systematic scoping review. Science of the Total Environment, 726. https://doi.org/10.1016/j.scitotenv.2020.138234
[14].
Cooper,
B., Behnke, N. L., Cronk, R., Anthonj, C., Shackelford, B. B., Tu, R., &
Bartram, J., 2021, Environmental health conditions in the transitional stage of
forcible displacement: A systematic scoping review. In Science of the Total
Environment (Vol. 762). https://doi.org/10.1016/j.scitotenv.2020.143136
[15].
UNHCR,
& Government of Bangladesh., 2024, Joint Government of Bangladesh - UNHCR
Population Factsheet - 30 June 2024. https://data.unhcr.org/en/country/bgd
[16].
Cox’s
Bazar Health Sector., 2024, Cox’s Bazar Health Sector bulletin - May 2024. https://rohingyaresponse.org/wp-content/uploads/2024/06/CXB-Health-Sector-Bulletin-May-2024.pdf
[17]. World Health
Organization., 2016, Guidelines on core components of infection prevention and
control programmes at the national and acute health care facility level. In
World Health Organization.
[18].
World
Health Organization., 2018, Infection prevention and control assessment
framework at the facility level. World Health Organization.
[19].
Kamara,
R. Z., Kamara, I. F., Moses, F., Kanu, J. S., Kallon, C., Kabba, M., Moffett,
D. B., Fofanah, B. D., Margao, S., Kamara, M. N., Moiwo, M. M., Kpagoi, S. S.
T. K., Tweya, H. M., Kumar, A. M. V., & Terry, R. F., 2023, Improvement in
Infection Prevention and Control Compliance at the Three Tertiary Hospitals of
Sierra Leone following an Operational Research Study. Tropical Medicine and
Infectious Disease, 8(7). https://doi.org/10.3390/tropicalmed8070378
[20].
World
Health Organization., 2018, Infection prevention and control assessment
framework at the facility level. World Health Organization.
[21].
Ahmado,
M. A., Alghajar, M., Meagher, K., Patel, P., & Ekzayez, A., 2024, Infection
Prevention and Control (IPC) in conflict-affected areas in Northeast Syria: A
cross-sectional study. IJID Regions, 100412. https://doi.org/10.1016/J.IJREGI.2024.100412
[22].
Tomczyk,
S., Twyman, A., de Kraker, M. E. A., Coutinho Rehse, A. P., Tartari, E.,
Toledo, J. P., Cassini, A., Pittet, D., & Allegranzi, B., 2022, The first
WHO global survey on infection prevention and control in health-care
facilities. The Lancet Infectious Diseases, 22(6). https://doi.org/10.1016/S1473-3099(21)00809-4
[23].
Oppong,
T. B., Amponsem-Boateng, C., Kyere, E. K. D., Wang, Y., Gheisari, Z., Oppong,
E. E., Opolot, G., Duan, G., & Yang, H., 2020, Infection prevention and
control preparedness level and associated determinants in 56 acute healthcare
facilities in Ghana. Infection and Drug Resistance, 13. https://doi.org/10.2147/IDR.S273851
[24].
Asgedom,
A. A., 2024, Status of infection prevention and control (IPC) as per the WHO
standardised Infection Prevention and Control Assessment Framework (IPCAF)
tool: existing evidence and its implication. In Infection Prevention in
Practice (Vol. 6, Issue 2). https://doi.org/10.1016/j.infpip.2024.100351
[25].
Cissé,
D. M., Laure, E. E. M., Blaise, K. A., Jean Paul, N. N., Gbonon, M. V., Mayaka,
C. R. A., Eugénie, G. D., Simplice, D. N., Philippe, K. L., & Mamadou, S.,
2023, Evaluation of the implementation of hospital hygiene components in 30
health-care facilities in the autonomous district of Abidjan (Cote d’Ivoire)
with the WHO Infection Prevention and Control Assessment Framework (IPCAF). BMC
Health Services Research, 23(1). https://doi.org/10.1186/s12913-023-09853-2
[26].
Harun,
M. G. D., Anwar, M. M. U., Sumon, S. A., Hassan, M. Z., Haque, T.,
Mah-E-Muneer, S., Rahman, A., Abdullah, S. A. H. M., Islam, M. S., Styczynski,
A. R., & Kaydos-Daniels, S. C., 2022, Infection prevention and control in
tertiary care hospitals of Bangladesh: results from WHO infection prevention
and control assessment framework (IPCAF). Antimicrobial Resistance and
Infection Control, 11(1). https://doi.org/10.1186/s13756-022-01161-4
[27].
Kamara,
I. F., Tengbe, S. M., Fofanah, B. D., Bunn, J. E., Njuguna, C. K., Kallon, C.,
& Kumar, A. M. V., 2022, Infection Prevention and Control in Three Tertiary
Healthcare Facilities in Freetown, Sierra Leone during the COVID-19 Pandemic:
More Needs to Be Done! International Journal of Environmental Research and
Public Health, 19(9). https://doi.org/10.3390/ijerph19095275
[28]. World Health
Organization, 2018, 2018 Global reference list of 100 core health indicators
(plus health-related SDGs). World Health Organization.
[29].
Government
of Bangladesh., 2018, Hospital Infection Prevention and Control manual.
[30].
Martin,
E. K., Salsgiver, E. L., Bernstein, D. A., Simon, M. S., Greendyke, W. G.,
Gramstad, J. M., Weeks, R., Woodward, T., Jia, H., Saiman, L., Furuya, E. Y.,
& Calfee, D. P., 2019, Sustained improvement in hospital cleaning
associated with a novel education and culture change program for environmental
services workers. Infection Control and Hospital Epidemiology, 40(9). https://doi.org/10.1017/ice.2019.183
[31].
Allegranzi,
B., Conway, L., Larson, E., & Pittet, D., 2014, Status of the
implementation of the World Health Organization multimodal hand hygiene
strategy in United States of America health care facilities. American
Journal of Infection Control. https://doi.org/10.1016/j.ajic.2013.11.015
[32].
Krein,
S. L., Hofer, T. P., Kowalski, C. P., Olmsted, R. N., Kauffman, C. A., Forman,
J. H., Banaszak-Holl, J., & Saint, S., 2007, Use of central venous
catheter-related bloodstream infection prevention practices by US hospitals. Mayo
Clinic Proceedings, 82(6), 672–678.
[33].
HEKS/EPER,
& WHO., 2019, LESSONS LEARNT FROM WASH FIT INTERVENTIONS IN THE FDMN
SETTLEMENTS, COX’S BAZAAR.
[34].
Haley,
R. W., Culver, D. H., White, J. W., Morgan, W. M., Emori, T. G., Munn, V. P.,
& Hooton, T. M., 1985, The efficacy of infection surveillance and control
programs in preventing nosocomial infections in US hospitals. American
Journal of Epidemiology, 121(2), 182–205. https://doi.org/10.1093/oxfordjournals.aje.a113990
[35].
Weinshel,
K., Dramowski, A., Hajdu, Á., Jacob, S., Khanal, B., Zoltán, M., Mougkou, K.,
Phukan, C., Staneloni, M. I., & Singh, N., 2015, Gap analysis of infection
control practices in low- and middle-income countries. Infection Control and
Hospital Epidemiology, 36(10). https://doi.org/10.1017/ice.2015.160
[36].
Stempliuk,
V., 2018, Surveillance of Healthcare-Associated Infections in Low- and
Middle-Income Countries: From the Need to a Reality. Current Treatment
Options in Infectious Diseases, 10(1). https://doi.org/10.1007/s40506-018-0148-x
[37].
Jayatilleke,
K., 2020, Challenges in Implementing Surveillance Tools of High-Income
Countries (HICs) in Low Middle Income Countries (LMICs). Current Treatment
Options in Infectious Diseases, 12(3). https://doi.org/10.1007/s40506-020-00229-2
[38].
World
Health Organization, 2016, Guidelines on core components of infection
prevention and control programmes at the national and acute health care
facility level. In World Health Organization.
[39].
Zamudio-Lugo,
I., Meza-Chávez, A., Martínez-Sánchez, Y., Miranda-Novales, M. G.,
Espinosa-Vital, J. G., & Rodríguez-Sing, R., 2012, Multimodal study of hand
hygiene in a third level pediatric hospital. Boletín Médico Del Hospital
Infantil de México, 69(5).
[40].
Dramowski,
A., Aucamp, M., Bekker, A., Pillay, S., Moloto, K., Whitelaw, A. C., Cotton, M.
F., & Coffin, S., 2021, NeoCLEAN: a multimodal strategy to enhance
environmental cleaning in a resource-limited neonatal unit. Antimicrobial
Resistance and Infection Control, 10(1). https://doi.org/10.1186/s13756-021-00905-y
[41].
Walker,
J. L., Sistrunk, W. W., Higginbotham, M. A., Burks, K., Halford, L., Goddard,
L., Thombs, L. A., Austin, C., & Finley, P. J., 2014, Hospital hand hygiene
compliance improves with increased monitoring and immediate feedback. American
Journal of Infection Control, 42(10). https://doi.org/10.1016/j.ajic.2014.06.018
[42].
Meng,
M., Sorber, M., Herzog, A., Igel, C., & Kugler, C., 2019, Technological
innovations in infection control: A rapid review of the acceptance of behavior
monitoring systems and their contribution to the improvement of hand hygiene.
In American Journal of Infection Control (Vol. 47, Issue 4). https://doi.org/10.1016/j.ajic.2018.10.012
[43].
Northey,
C., 2012, Improving Hand Hygiene Practice Through Utilization of Automated Hand
Hygiene Monitoring and Feedback Technology. American Journal of Infection
Control, 40(5). https://doi.org/10.1016/j.ajic.2012.04.273
[44].
World
Health Organization. 2010, Hand Hygiene Self-Assessment Framework 2010. Clean
Care Is Safe Care.
[45].
Lowe,
H., Woodd, S., Lange, I. L., Janjanin, S., Barnett, J., & Graham, W., 2021,
Challenges and opportunities for infection prevention and control in hospitals
in conflict-affected settings: a qualitative study. Conflict and Health,
15(1). https://doi.org/10.1186/s13031-021-00428-8
[46].
Tahir,
M. A., Khan, M. A., Ikram, A., Chaudhry, T. H., Jabeen, A., Quddous, A., &
Haq, I. U., 2023, Assessment of Infection Prevention and Control (IPC)
Implementation and Strategies Used for IPC Preparedness at Facility Level in
Underdeveloped Areas of Pakistan. Infection and Drug Resistance, 16. https://doi.org/10.2147/IDR.S399830
[47].
Anthony,
M., Bedford-Russell, A., Cooper, T., Fry, C., T Heath, P., Kennea, N.,
McCartney, M., Patel, B., Pollard, T., Sharland, M., & Wilson, P., 2013,
Managing and preventing outbreaks of Gram-negative infections in UK neonatal
units. Archives of Disease in Childhood: Fetal and Neonatal Edition, 98(6). https://doi.org/10.1136/archdischild-2012-303540
[48].
Zeb,
S., & Ali, T. S., 2021, Factors associated with the compliance of standard precaution,
Review article. Journal of the Pakistan Medical Association, 71(2 B). https://doi.org/10.47391/JPMA.416
[49]. World Health
Organization (WHO). (n.d.). Health workforce requirements for universal health
coverage and the Sustainable Development Goals. (Human Resources for Health
Observer, 17). World Health Organization.
[50]. World Health Organization., 2010, Workload Indicators of Staffing Need: User’s Manual.

