Dental Pulp Stem Cell-Based Therapy for Human Diseases
Abstract:
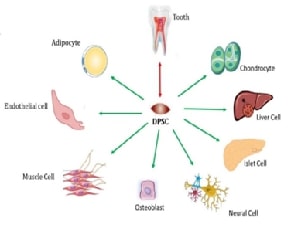
Stem cells, which can self-renew
and develop into specialized cell types, are used in stem cell therapy, an
emerging multidisciplinary approach, to repair and regenerate tissue. This
medication may be beneficial for a variety of conditions, such as cardiovascular
disease, neurological disorders, autoimmune diseases, and certain types of
cancer. However, problems like safety, scalability, and ethical quandaries
persist. Dental pulp stem cells (DPSCs), derived from the soft tissue of teeth,
offer a clear advantage over other stem cell sources due to their accessibility
and regeneration potential. DPSCs are valuable for immunological regulation,
neurological therapy, and bone regeneration since they may be obtained
non-invasively from extracted teeth and differentiate into a variety of cell
types, including osteoblasts, adipocytes, and neurons. DPSCs can promote tissue
healing and reduce inflammation due to their immunomodulatory qualities. They
also release growth factors and cytokines, which help heal damaged tissues. In
clinical settings, DPSCs still have limitations despite their potential, such
as the need for homogeneity and scalability. However, because of their broad
differentiation potential, ease of procurement, and immune-regulatory
qualities, they are positioned as a promising resource in regenerative
medicine. This review highlights the characteristics, mechanisms of action, and
therapeutic potential of DPSCs in the treatment of diseases, with a special
focus on their role in bone regeneration, tissue repair, and neuroprotection.
Further research and clinical testing are needed to get past barriers and
optimize the use of DPSCs in regenerative therapies.
References:
[1]. Trapana,
J., Weinerman, J., Lee, D., Sedani, A., Constantinescu, D., Best, T., M. Hare,
J. M., 2024, Cell-based therapy in the treatment of musculoskeletal
diseases. Stem cells translational medicine, 13(10), 959-978.
[2]. Rahman,
M. M., Islam, M. R., Islam, M. T., Harun-Or-Rashid, M., Islam, M., Abdullah, S.,
and Mostafa-Hedeab, G., 2022, Stem cell transplantation therapy and
neurological disorders: current status and future perspectives. Biology,
11(1), 147.
[3]. Senthil,
R., Anitha, R., and Lakshmi, T., 2024, Mineralized collagen fiber-based dental
Implant: novel perspectives. Journal of Advanced Oral Research, 15(1),
62-69.
[4]. Roato,
I., Chinigò, G., Genova, T., Munaron, L., and Mussano, F., 2021, Oral cavity as
a source of mesenchymal stem cells useful for regenerative medicine in
dentistry. Biomedicines, 9(9), 1085.
[5]. Mehta,
V., Negi, S., Mathur, A., Tripathy, S., Oberoi, S., Shamim, M. A., and
Karobari, I., 2024, Oral health status among the transgender population of
India: A systematic review and meta‐analysis. Special Care in Dentistry.
[6]. Baraniak,
P. R., and McDevitt, T. C., 2010, Stem cell paracrine actions and tissue
regeneration. Regenerative medicine, 5(1), 121-143.
[7]. Tsutsui,
T. W., 2020, Dental pulp stem cells: advances to applications. Stem cells and cloning:
advances and applications, 33-42.
[8]. Ogata,
K., Moriyama, M., Matsumura-Kawashima, M., Kawado, T., Yano, A., and Nakamura,
S., 2022, The therapeutic potential of secreted factors from dental pulp stem
cells for various diseases. Biomedicines, 10(5), 1049.
[9]. Al
Madhoun, A., Sindhu, S., Haddad, D., Atari, M., Ahmad, R. and Al-Mulla, F.,
2021, Dental pulp stem cells derived from adult human third molar tooth: a
brief review. Frontiers in Cell and Developmental Biology, 9, 717624.
[10]. Baghaei,
K., Hashemi, S. M., Tokhanbigli, S., Rad, A. A., Assadzadeh-Aghdaei, H.,
Sharifian, A., and Zali, M. R., 2017, Isolation, differentiation, and
characterization of mesenchymal stem cells from human bone marrow. Gastroenterology
and hepatology from bed to bench, 10(3), 208.
[11]. Ram, R.
M., and Prasad, M., 2025, An unusual surgical complication: Slipped molar
lodged in vocal cords and its anesthetic management. Journal of Oral Biology
and Craniofacial Research, 15(1), 22-24.
[12]. Mattei,
V., and Delle Monache, S., 2023, Dental pulp stem cells (DPSCs) and tissue
regeneration: mechanisms mediated by direct, paracrine, or autocrine effects. Biomedicines,
11(2), 386.
[13]. Goswami,
T. K., Singh, M., Dhawan, M., Mitra, S., Emran, T. B., Rabaan, A. A., and
Dhama, K., 2022, Regulatory T cells (Tregs) and their therapeutic potential
against autoimmune disorders–Advances and challenges. Human vaccines and
immunotherapeutics, 18(1), 2035117.
[14]. Yamada,
Y., Nakamura-Yamada, S., Kusano, K., and Baba, S., 2019, Clinical potential and
current progress of dental pulp stem cells for various systemic diseases in
regenerative medicine: a concise review. International journal of molecular
sciences, 20(5), 1132.
[15]. La
Noce, M., Paino, F., Spina, A., Naddeo, P., Montella, R., Desiderio, V., and
Laino, L., 2014, Dental pulp stem cells: state of the art and suggestions for a
true translation of research into therapy. Journal of dentistry, 42(7),
761-768.
[16]. Luo,
L., He, Y., Wang, X., Key, B., Lee, B. H., Li, H., Ye, Q., 2018, Potential
roles of dental pulp stem cells in neural regeneration and repair. Stem
cells international, (1), 1731289.
[17]. Li, F.,
Wang, X., Shi, J., Wu, S., Xing, W. and He, Y., 2023, Anti-inflammatory effect
of dental pulp stem cells. Frontiers in Immunology, 14, 1284868.
[18]. Mattei,
V., and Delle Monache, S., 2023, Dental pulp stem cells (DPSCs) and tissue
regeneration: mechanisms mediated by direct, paracrine, or autocrine effects. Biomedicines,
Jan 28; 11(2):386.
[19]. Anderson,
S., Prateeksha, P., and Das, H., 2022, Dental pulp-derived stem cells reduce
inflammation, accelerate wound healing and mediate M2 polarization of myeloid
cells. Biomedicines, 10(8), 1999.
[20]. Li, F.,
Wang, X., Shi, J., Wu, S., Xing, W., and He, Y., 2023, Anti-inflammatory effect
of dental pulp stem cells. Frontiers in Immunology, 14, 1284868.
[21]. Xue,
N., Ding, X., Huang, R., Jiang, R., Huang, H., Pan, X., and Wang, Y., 2022,
Bone tissue engineering in the treatment of bone defects. Pharmaceuticals,
15(7), 879.
[22]. Kwack,
K. H., and Lee, H. W., 2022, Clinical potential of dental pulp stem cells in
pulp regeneration: current endodontic progress and future perspectives. Frontiers
in Cell and Developmental Biology, 10, 857066.
[23]. Longoni,
A., Utomo, L., van Hooijdonk, I. E., Bittermann, G. K. P., Vetter, V. C.,
Kruijt Spanjer, E. C., and Gawlitta, D., 2020, The chondrogenic differentiation
potential of dental pulp stem cells. European Cells and Materials, 39,
121-135.
[24]. Mattei,
V., Martellucci, S., Pulcini, F., Santilli, F., Sorice, M., and Delle Monache,
S., 2021, Regenerative potential of DPSCs and revascularization: direct,
paracrine or autocrine effect? Stem cell reviews and reports, 1-12.
[25]. Mattei,
V., and Delle Monache, S., 2023, Dental pulp stem cells (DPSCs) and tissue
regeneration: mechanisms mediated by direct, paracrine, or autocrine effects. Biomedicines,
11(2), 386.
[26]. Johnson,
K. E., and Wilgus, T. A., 2014, Vascular endothelial growth factor and
angiogenesis in the regulation of cutaneous wound repair. Advances in wound
care, 3(10), 647-661.
[27]. Ueda,
T., Inden, M., Ito, T., Kurita, H., Hozumi, I., 2020, Characteristics and
therapeutic potential of dental pulp stem cells on neurodegenerative diseases. Frontiers
in Neuroscience, 14, 407.
[28]. Saremi,
J., Mahmoodi, N., Rasouli, M., Ranjbar, F. E., Mazaheri, E. L., Akbari, M., and
Azami, M., 2022, Advanced approaches to regenerate spinal cord injury: the
development of cell and tissue engineering therapy and combinational
treatments. Biomedicine and Pharmacotherapy, 146, 112529.
[29]. Blais,
M., Lévesque, P., Bellenfant, S., and Berthod, F., 2013, Nerve growth factor,
brain-derived neurotrophic factor, neurotrophin-3 and glial-derived
neurotrophic factor enhance angiogenesis in a tissue-engineered in vitro model.
Tissue Engineering Part A, 19(15-16), 1655-1664.
[30]. Xiong,
W., Liu, Y., Zhou, H., Jing, S., He, Y., and Ye, Q., 2022, Alzheimer’s disease:
pathophysiology and dental pulp stem cells therapeutic prospects. Frontiers
in Cell and Developmental Biology, 10, 999024.
[31]. Kulkarni,
O. P., Lichtnekert, J., Anders, H. J., and Mulay, S. R., 2016, The immune
system in tissue environments regaining homeostasis after injury: is
“inflammation” always inflammation? Mediators of inflammation, 2016(1),
2856213.
[32]. Shi,
X., Mao, J., and Liu, Y., 2020, Pulp stem cells derived from human permanent
and deciduous teeth: Biological characteristics and therapeutic applications. Stem
cells translational medicine, 9(4), 445-464.
[33]. Pezhouman,
A., Nguyen, N. B., Kay, M., Kanjilal, B., Noshadi, I., and Ardehali, R., 2023,
Cardiac regeneration–Past advancements, current challenges, and future
directions. Journal of Molecular and Cellular Cardiology.
[34]. Li, X.
L., Fan, W., Fan, B., and Zhang, Y., 2024, Dental pulp regeneration strategies:
A review of status quo and recent advances. Bioactive Materials, 38,
258-275.
[35]. Min,
Q., Yang, L., Tian, H., Tang, L., Xiao, Z., Shen, J., and Zhou, Y., 2023,
Immunomodulatory mechanism and potential application of dental pulp-derived
stem cells in immune-mediated diseases. International Journal of Molecular
Sciences, 24(9), 8068.
[36]. Isomäki,
P., and Punnonen, J., 1997, Pro-and anti-inflammatory cytokines in rheumatoid
arthritis. Annals of medicine, 29(6), 499-507.
[37]. Cavallo,
S., 2020, Immune-mediated genesis of multiple sclerosis. Journal of
Translational Autoimmunity, 3, 100039.
[38]. Potdar,
P. D., and Jethmalani, Y. D., 2015, Human dental pulp stem cells: Applications
in future regenerative medicine. World journal of stem cells, 7(5), 839.
[39]. Yang,
D., Solidum, J. G. N., and Park, D., 2023, Dental pulp stem cells and current
in vivo approaches to study dental pulp stem cells in pulp injury and
regeneration. Journal of Bone Metabolism, 30(3), 231.
[40]. Nijhawan,
L. P., Janodia, M. D., Muddukrishna, B. S., Bhat, K. M., Bairy, K. L., Udupa,
N., and Musmade, P. B., 2013, Informed consent: Issues and challenges. Journal
of advanced pharmaceutical technology and research, 4(3), 134-140.
[41]. Ayanoğlu,
F. B., Elçin, A. E., and Elçin, Y. M., 2020, Bioethical issues in genome
editing by CRISPR-Cas9 technology. Turkish Journal of Biology, 44(2),
110-120.
[42]. Bradlow,
D. D., Palmieri, A., and Salman, S. M., 2002, Regulatory frameworks for dam
safety: A comparative study. World Bank Publications.
[43]. Yuan,
B. Z., 2015, Establishing a quality control system for stem cell-based
medicinal products in China. Tissue engineering Part A, 21(23-24),
2783-2790.
[44]. Fodor
Duric, L., Basic Jukic, N., and Vujicic, B., 2024, Comparison of Autologous and
Allogeneic Adipose-Derived Stem Cells in Kidney Transplantation: Immunological
Considerations and Therapeutic Efficacy. Journal of clinical medicine, 13(19),
5763.
[45]. Abolarinwa,
B. A., Shaw, M. K., and Lee, C. H., 2021, Perspectives on challenges to cell
therapy development in Taiwan: strengthening evidential standards and ways
forward. Frontiers in Bioengineering and Biotechnology, 9, 789043.
[46]. Amaya-Amaya,
J., Montoya-Sánchez, L., and Rojas-Villarraga, A., 2014, Cardiovascular
involvement in autoimmune diseases. BioMed research international,
2014(1), 367359.
[47]. Mehta,
P. K., Levit, R. D., Wood, M. J., Aggarwal, N., O'Donoghue, M. L., Lim, S. S.,
and Pepine, C. J., 2023, Chronic rheumatologic disorders and cardiovascular
disease risk in women. American Heart Journal Plus: Cardiology Research and
Practice, 27, 100267.
[48]. Do, A.
V., Khorsand, B., Geary, S. M., and Salem, A. K., 2015, 3D printing of
scaffolds for tissue regeneration applications. Advanced healthcare
materials, 4(12), 1742-1762.
[49]. Min,
Q., Yang, L., Tian, H., Tang, L., Xiao, Z., Shen, J., and Zhou, Y., 2023,
Immunomodulatory mechanism and potential application of dental pulp-derived
stem cells in immune-mediated diseases. International Journal of Molecular
Sciences, 24(9), 8068.
[50]. Yamada,
Y., Nakamura-Yamada, S., Konoki, R., and Baba, S., 2020, Promising advances in
clinical trials of dental tissue-derived cell-based regenerative medicine. Stem
cell research & therapy, 11, 1-10.
[51]. Ferro,
F., Spelat, R., and Baheney, C. S., 2014, Dental pulp stem cell (DPSC)
isolation, characterization, and differentiation. Stem Cells and Tissue
Repair: Methods and Protocols, 91-115.
[52]. Dresser,
R., 2010, Stem cell research as innovation: expanding the ethical and policy
conversation. Journal of Law, Medicine & Ethics, 38(2), 332-341.
[53]. Timothy, C. N., Samyuktha, P. S., and Brundha, M. P., 2019, Dental pulp stem cells in regenerative medicine–a literature review. Research Journal of Pharmacy and Technology, 12(8), 4052-4056.
[54]. Malakondaiah, S., Pavithravedhavalli, V., Kayal, L., Ryntathiang, I., and Jothinathan, M. K. D., 2024, Stem cell therapy: A new path in tackling oral cancer. Journal of Stomatology, Oral and Maxillofacial Surgery, 101967.
[55]. Shekar, N. D., Kayal, L., Babu, N. A., Jothinathan, M. K. D., and Ryntathiang, I., 2024, Pioneering the use of micro-biomarkers in oral cancer detection. Oral Oncology Reports, 100412.

