Comprehensive Evaluation of Therapeutic Interventions for Oral Submucous Fibrosis: A Systematic Review of Clinical Trials
Abstract:
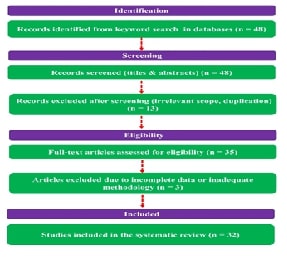
Oral submucous fibrosis (OSMF) is a chronic condition characterized by progressive fibrosis and thickening of the oral submucosa, leading to functional limitations such as restricted mouth opening (trismus), difficulty in chewing and swallowing, and a burning sensation in the oral cavity. This systematic review, conducted per PRISMA guidelines, synthesizes current evidence on OSMF management, evaluating therapeutic interventions and identifying areas for further research. A comprehensive search of databases including PubMed, Embase, Scopus, Web of Science, and CENTRAL, up to 2024, identified 48 studies. After screening for relevance and quality, 32 clinical trials were included. Eligible studies focused on pharmacological, surgical, and alternative treatments for OSMF, assessing outcomes such as mouth opening, pain reduction, and histopathological changes. Studies on animal models, in vitro research, reviews, and case reports were excluded. Due to significant heterogeneity in study designs and outcomes, a meta-analysis was not feasible. Instead, a qualitative synthesis revealed the effectiveness of various treatments. Local injections, particularly corticosteroids combined with agents like Salvia miltiorrhiza or lycopene, improved mouth opening and pain. Non-invasive approaches, including physiotherapy and herbal remedies, provided symptom relief, while surgical interventions were reserved for severe cases. Emerging therapies, such as transdermal fentanyl and laser fibrotomy, showed promise for personalized treatment. The review emphasizes early diagnosis, tailored interventions, and the need for further research into innovative therapies to enhance treatment outcomes for OSMF.References:
[1]. Shih, Y.-H., Wang, T.-H., Shieh, T.-M.,
& Tseng, Y.-H., 2019, Oral submucous fibrosis: A review on
etiopathogenesis, diagnosis, and therapy, International
Journal of Molecular Sciences, 20(11), 2940.
[2]. Muthukrishnan, A., & Warnakulasuriya,
S., 2018, Oral health consequences of smokeless tobacco use, Indian Journal of Medical
Research, 148(1), 35–40.
[3]. Pandiar, D., Krishnan, R. P., Ramani, P.,
Anand, R., & Sarode, S., 2023, Oral submucous fibrosis and the malignancy
arising from it, could best exemplify the concepts of cuproplasia and
cuproptosis, Journal of
Stomatology, Oral and Maxillofacial Surgery, 124(5), 101368.
[4]. Yuwanati, M., Ramadoss, R., Kudo, Y.,
Ramani, P., & Senthil Murugan, M., 2023, Prevalence of oral submucous
fibrosis among areca nut chewers: A systematic review and meta-analysis, Oral Diseases, 29(7),
1920–1926.
[5]. Peng, Q., Li, H., Chen, J., Wang, Y., &
Tang, Z., 2020, Oral submucous fibrosis in Asian countries, Journal of Oral Pathology &
Medicine, 49(4), 294–304.
[6]. Hande, A. H., Chaudhary, M. S., Gawande, M.
N., Gadbail, A. R., Zade, P. R., Bajaj, S., et al., 2019, Oral submucous
fibrosis: An enigmatic morpho-insight, Journal
of Cancer Research and Therapeutics, 15(3), 463–469.
[7]. Gupta, S., & Jawanda, M. K., 2021, Oral
submucous fibrosis: An overview of a challenging entity, Indian Journal of Dermatology,
Venereology, and Leprology, 87(6), 768–777.
[8]. Sarode, S. C., Gondivkar, S., Sarode, G.
S., Gadbail, A., & Yuwanati, M., 2021, Hybrid oral potentially malignant
disorder: A neglected fact in oral submucous fibrosis, Oral Oncology, 121, 105390.
[9]. Pandiar, D., G, P., Poothakulath Krishnan,
R., & T. N., U. M., 2023, Correlation between clinical and
histopathological stagings of oral submucous fibrosis: A clinicopathological
cognizance of 238 cases from south India, Cureus,
15, e49107.
[10]. Sharma, M., Shetty, S. S., &
Radhakrishnan, R., 2018, Oral submucous fibrosis as an overhealing wound:
Implications in malignant transformation, Recent
Patents on Anti-Cancer Drug Discovery, 13(3), 272–291.
[11]. Gayathri, K., Malathi, N., Gayathri, V.,
Adtani, P. N., & Ranganathan, K., 2023, Molecular pathways of oral
submucous fibrosis and its progression to malignancy, Archives of Oral Biology, 148,
105644.
[12]. Xu, H., Lyu, F.-Y., Song, J.-Y., Xu, Y.-M.,
Jiang, E.-H., Shang, Z.-J., et al., 2021, Research achievements of oral
submucous fibrosis: Progress and prospect, Biomedical
Research International, 2021, 6631856.
[13]. Chen, X., Xie, H., & Guo, J., 2023,
Drug treatment for oral submucous fibrosis: An update, BMC Oral Health, 23, 748.
[14]. Shen, Y.-W., Shih, Y.-H., Fuh, L.-J., &
Shieh, T.-M., 2020, Oral submucous fibrosis: A review on biomarkers, pathogenic
mechanisms, and treatments, International
Journal of Molecular Sciences, 21(21), 7231.
[15]. Chen, J., Wu, Y., Peng, J., & Ma, L.,
2021, Oral opening training increases oral opening in patients with oral
submucous fibrosis, Journal
of Central South University Medical Sciences, 46(6), 731–735.
[16]. Baptist, J., Shakya, S., & Ongole, R.,
2016, Rebamipide to manage stomatopyrosis in oral submucous fibrosis, Journal of Contemporary Dental
Practice, 17(11), 1009–1012.
[17]. Bhadage, C. J., Umarji, H. R., Shah, K.,
& Välimaa, H., 2013, Vasodilator isoxsuprine alleviates symptoms of oral
submucous fibrosis, Clinical
Oral Investigations, 17(6), 1375–1382.
[18]. Memon, A. B., Rahman, A. A. U., Channar, K.
A., Zafar, M. S., & Kumar, N., 2022, Evaluating the oral-health-related
quality of life of oral submucous fibrosis patients before and after treatment
using the OHIP-14 tool, International
Journal of Environmental Research and Public Health, 19(3), 1821.
[19]. Raizada, M. K., Sable, D. M., Chowdhery,
A., Chavan, M. S., & Rajpurohit, L. S., 2017, Oral submucous fibrosis:
Current perspectives, Journal
of Oral Pathology & Medicine, 46(6), 439–442.
[20]. Veedu, A., Balan, R., & Sankar, A.,
2015, A randomized double-blind, multiple-arm trial comparing the efficacy of
submucosal injections of hyaluronidase, dexamethasone, and combination of
dexamethasone and hyaluronidase in the management of oral submucous fibrosis, Oral Surgery, Oral Medicine, Oral
Pathology and Oral Radiology, 120(5), 588–593.
[21]. Singh, M., Niranjan, H. S., Mehrotra, R.,
Sharma, D., & Gupta, S. C., 2010, Efficacy of hydrocortisone
acetate/hyaluronidase vs. triamcinolone acetonide/hyaluronidase in the
treatment of oral submucous fibrosis, Indian
Journal of Medical Research, 131, 665–669.
[22]. Lyu, F.-Y., Wang, H.-F., Xu, C.-J., Xu, Z.,
Li, D.-M., & Chi, Y.-T., 2016, Expression of secreted frizzled-related
protein-1 in patients with oral submucous fibrosis, Zhonghua Kou Qiang Yi Xue Za Zhi,
51(10), 616–622.
[23]. Shandilya, S., Mohanty, S., Sharma, P.,
Chaudhary, Z., Kohli, S., & Kumar, R. D., 2021, Effect of botulinum toxin-A
on pain and mouth opening following surgical intervention in oral submucous
fibrosis: A controlled clinical trial, Journal
of Craniomaxillofacial Surgery, 49(8), 675–681.
[24]. Jiang, X., Zhang, Y., Li, F., Zhu, Y.,
Chen, Y., & Yang, S., 2015, Allicin as a possible adjunctive therapeutic
drug for stage II oral submucous fibrosis: A preliminary clinical trial in a
Chinese cohort, International
Journal of Oral and Maxillofacial Surgery, 44(12), 1540–1546.
[25]. Cox, S., & Zoellner, H., 2009, Oral
submucous fibrosis: Insights into pathogenesis, Journal of Oral Pathology &
Medicine, 38(3), 220–226.
[26]. Nerkar Rajbhoj, A., Kulkarni, T. M., Shete,
A., Shete, M., Gore, R., & Sapkal, R., 2021, A comparative study to
evaluate efficacy of curcumin and Aloe Vera gel along with oral physiotherapy
in the management of oral submucous fibrosis: A randomized clinical trial, Asian Pacific Journal of Cancer
Prevention, 22(1), 107–112.
[27]. Adhikari, S., Rimal, J., Maharjan, I. K.,
& Shrestha, A., 2022, Efficacy of curcumin in combination with
intralesional dexamethasone with hyaluronidase in the treatment of oral
submucous fibrosis: A randomized controlled trial, Asian Pacific Journal of Cancer
Prevention, 23(10), 3125–3132.
[28]. Singh, N., Hebbale, M., Mhapuskar, A., Ul
Nisa, S., Thopte, S., & Singh, S., 2016, Effectiveness of Aloe Vera and
antioxidant along with physiotherapy in the management of oral submucous
fibrosis, Journal of
Contemporary Dental Practice, 17(1), 78–84.
[29]. Ardra, A., Bharati, P., & Venkataswamy
Reddy, A., 2017, Oral submucous fibrosis: An updated clinical perspective, Journal of Oral Pathology &
Medicine, 46(1), 50–55.
[30]. Chandrashekar, A., Annigeri, R. G., Va, U.,
& Thimmasetty, J., 2021, A clinicobiochemical evaluation of curcumin as gel
and as buccal mucoadhesive patches in the management of oral submucous
fibrosis, Oral Surgery, Oral
Medicine, Oral Pathology, and Oral Radiology, 131(4), 428–434.
[31]. Bohra, A., Maheswari, T. N. U., Harsh, A.,
& Garg, A., 2021, Black turmeric and Aloe Vera in the management of oral
submucous fibrosis: A prospective clinical study, Asian Pacific Journal of Cancer
Prevention, 22(12), 3941–3947.
[32]. Pipalia, P. R., Annigeri, R. G., &
Mehta, R., 2016, Clinicobiochemical evaluation of turmeric with black pepper
and nigella sativa in the management of oral submucous fibrosis: A
double-blind, randomized preliminary study, Oral
Surgery, Oral Medicine, Oral Pathology, Oral Radiology, 122(6), 705–712.
[33]. Srivastava, R., Kundu, A., Pradhan, D.,
Jyoti, B., Chokotiya, H., & Parashar, P., 2021, A comparative study to
evaluate the efficacy of curcumin lozenges (TurmNova®) and intralesional
corticosteroids with hyaluronidase in the management of oral submucous
fibrosis, Journal of
Contemporary Dental Practice, 22(6), 751–755.
[34]. Tp, B., T, A. G., Varghese, M., Raghavan,
R., Vm, M. N., & Pius, A., 2019, Evaluation of therapeutic efficacy of
different treatment modalities in oral submucous fibrosis: A comparative study, Journal of Contemporary Dental
Practice, 20(3), 390–394.
[35]. Ambereen, A., Bhutia, O., Roychoudhury, A.,
Yadav, R., Khakhla, D. H., & Vishwakarma, K., 2021, Is coronoidectomy
superior to coronoidotomy for improving maximum incisal opening in patients
with oral submucous fibrosis? Journal
of Oral and Maxillofacial Surgery, 79(6), 863.e1–863.e7.
[36]. Dani, V. B., & Patel, S. H., 2018, The
effectiveness of therapeutic ultrasound in patients with oral submucosal
fibrosis, Indian Journal of
Cancer, 55(3), 248–250.
[37]. Patil, P., Hazarey, V., Chaudhari, R.,
& Nimbalkar-Patil, S., 2016, Clinical efficacy of a mouth-exercising device
adjunct to local ointment intra-lesional injections and surgical treatment for
oral submucous fibrosis: A randomized controlled trial, Asian Pacific Journal of Cancer
Prevention, 17(3), 1255–1259.
[38]. Dasukil, S., Jena, A. K., Boyina, K. K.,
Grover, S., Arora, G., & Ahmed, Z. U., 2022, Functional outcome of two
different grafting techniques in the surgical management of oral submucous
fibrosis: A comparative evaluation, Oral
and Maxillofacial Surgery, 26(5), 477–483.
[39]. Pandey, M., Thomas, G., Somanathan, T.,
Sankaranarayanan, R., Abraham, E. K., Jacob, B. J., et al., 2001, Evaluation of
surgical excision of non-homogeneous oral leukoplakia in a screening
intervention trial, Kerala, India, Oral
Oncology, 37(2), 103–109.
[40]. Su, W. W.-Y., Yen, A. M.-F., Chiu, S.
Y.-H., & Chen, T. H.-H., 2010, A community-based RCT for oral cancer
screening with toluidine blue, Journal
of Dental Research, 89(9), 933–937.
[41]. Sankaranarayanan, R., Mathew, B., Jacob, B.
J., Thomas, G., Somanathan, T., Pisani, P., et al., 2000, Early findings from a
community-based, cluster-randomized, controlled oral cancer screening trial in
Kerala, India, Cancer, 88(3),
664–673.
[42]. Jiang, X.-W., Zhang, Y., Yang, S.-K.,
Zhang, H., Lu, K., & Sun, G.-L., 2013, Efficacy of salvianolic acid B
combined with triamcinolone acetonide in the treatment of oral submucous
fibrosis, Oral Surgery, Oral
Medicine, Oral Pathology, Oral Radiology, 115(3), 339–344.
[43]. Wu, Y., Peng, J., Que, G., Xu, C., &
Yin, X., 2010, Therapeutic effect of the combination of traditional Chinese
medicine and western medicine on patients with oral submucous fibrosis, Journal of Central South
University Medical Sciences, 35(4), 358–364.
[44]. Thakur, G., Thomas, S., Bhargava, D., &
Pandey, A., 2015, Does topical application of placental extract gel on
postoperative fibrotomy wound improve mouth opening and wound healing in
patients with oral submucous fibrosis? Journal
of Oral and Maxillofacial Surgery, 73(7), 1439.e1–1439.e10.
[45]. Rajendran, R., Rani, V., & Shaikh, S.,
2006, Pentoxifylline therapy: A new adjunct in the treatment of oral submucous
fibrosis, Indian Journal of
Dental Research, 17(4), 190–198.
[46]. Nihadha, P. M., Chugh, A., Kaur, A., Kumar,
S., Naveen, K. H., Bhatia, P. K., et al., 2022, Transdermal fentanyl patch
versus standard analgesia in postoperative oral submucous fibrosis patients: A
triple-blinded, randomized control trial, British
Journal of Oral and Maxillofacial Surgery, 60(11), 1246–1253.
[47]. Rai, A., Kaur, M., Gombra, V., Hasan, S.,
& Kumar, N., 2019, Comparative evaluation of curcumin and antioxidants in
the management of oral submucous fibrosis, Journal
of Investigative and Clinical Dentistry, 10(1), e12464.
[48]. Tai, Y. S., Liu, B. Y., Wang, J. T., Sun,
A., Kwan, H. W., & Chiang, C. P., 2001, Oral administration of milk from
cows immunized with human intestinal bacteria leads to significant improvements
of symptoms and signs in patients with oral submucous fibrosis, Journal of Oral Pathology &
Medicine, 30(10), 618–625.
[49]. Gupta, S., Piyush, P., Mahajan, A.,
Mohanty, S., Ghosh, S., & Singh, K., 2018, Fibrotomy with diode laser (980
nm) and habit correlation in oral submucous fibrosis: A report of 30 cases, Lasers in Medical Science, 33(8),
1739–1745.

