Association of COVID-19, Diabetes in Mucormycosis Patient- A Hospital-Based Study
Abstract:
Mucormycosis (previously called zygomycosis) is a serious but rare
fungal infection caused by a group of moulds called mucormycetes. These moulds
live throughout the environment. Mucormycosis mainly affects people who have
health problems or take medicines that lower the body's ability to fight germs
and sickness. This research aimed to study the association of COVID, diabetes
and mucormycosis in a population reporting to Saveetha Dental College and
Hospitals, Chennai in a period from June 2019 to June 2023. The data of
patients reporting to Saveetha Dental College and Hospitals was reviewed and
patients with mucormycosis were selected for the study. It included parameters
like age, gender, Coronavirus Disease-19(COVID-19) history and systemic
disease. Frequency test was used to detect the significance between age,
gender, COVID-19 history and systemic condition. Chi-square tests were carried
out using age, and gender as independent variables and COVID-19 history, and systemic
condition as dependent variables. Statistical analysis was done by Pearson's chi-square
test. P value < 0.05 was considered statistically significant. In this
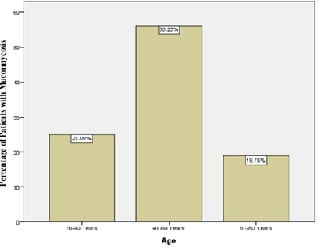
study, we observed that the most common age group diagnosed with mucormycosis
was found to be 41-60 years of age (56%) and males were more commonly affected
(88%). More than 50% of patients gave a history of COVID-19 and 50% were diabetic.
The most common intraoral presentation was found to be palatal swelling (19%),
and most of the patients had unilateral swelling. When associating swelling
with different age groups, unilateral swelling was found to be more in young
adults (56%) while bilateral swelling was profound in older people. The chi-square
value was found to be significant (0.035). In this study, we observed that the
most common age group diagnosed with mucormycosis was found to be 41-60 years
of age and males were more commonly affected. The majority of them had a
history of COVID-19 and were diabetic. The most common intraoral presentation
was found to be palatal swelling, and most of the patients had unilateral
swelling. Collectively, these findings suggest a familiar connection between
mucormycosis, COVID-19 and diabetes.
References:
[1].
Semwal, N., Rautela, A., Joshi, D., and Singh, B.,
2021, Black Fungus (Mucormycosis) A Rare Fungal Infection caused by COVID-19. Int.
J. Pharm. Bio Med. Sci, 1(4):31-37.
[2].
Thornton, C. R., 2020, Detection of the ‘big five’mold
killers of humans: Aspergillus, Fusarium, Lomentospora, Scedosporium and
Mucormycetes. Advances in applied microbiology, 110:1-61. https://doi.org/10.1016/bs.aambs.2019.10.003
[3].
Chander, J., 2017, Textbook of medical mycology. JP
Medical Ltd.
[4].
Wani, A. A., 2021, Mucormycosis (black fungus) an
emerging threat during 2nd wave of COVID-19 pandemic in India: a review. Haya
Saudi J Life Sci, 6(7):143-146. DOI:
10.36348/sjls.2021.v06i07.003
[5].
Cornely,
O. A., Alastruey-Izquierdo, A., Arenz, D., Chen, S. C., Dannaoui, E.,
Hochhegger, B., Hoenigl, M., Jensen, H. E., Lagrou, K., Lewis, R. E. and
Mellinghoff, S. C., 2019, Global guideline for the diagnosis and management of
mucormycosis: an initiative of the European Confederation of Medical Mycology
in cooperation with the Mycoses Study Group Education and Research Consortium. The
Lancet infectious diseases, 19(12): e405-e421.
[6].
Prakash,
H. and Chakrabarti, A., 2019, Global epidemiology of mucormycosis. Journal
of Fungi, 5(1):26. http://dx.doi.org/10.3390/jof5010026
[7]. Martínez-Herrera, E., Frías-De-León, M. G.,
Julián-Castrejón, A., Cruz-Benítez, L., Xicohtencatl-Cortes, J., and
Hernández-Castro, R., 2020, Rhino-orbital mucormycosis due to Apophysomyces
ossiformis in a patient with diabetes mellitus: a case report. BMC
infectious diseases, 20(1): 1-4.
https://doi.org/10.1186/s12879-020-05337-4
[8]. Walsh, T. J., Gamaletsou, M. N., McGinnis, M. R., Hayden, R.
T., and Kontoyiannis, D. P., 2012, Early clinical and laboratory diagnosis of
invasive pulmonary, extrapulmonary, and disseminated mucormycosis
(zygomycosis). Clinical Infectious Diseases, 54(suppl_1): S55-S60.
https://doi.org/10.1093/cid/cir868
[9]. Garg, D., Muthu, V., Sehgal, I. S., Ramachandran, R., Kaur, H.,
Bhalla, A., Puri, G. D., Chakrabarti, A., and Agarwal, R., 2021, Coronavirus
disease (Covid-19) associated mucormycosis (CAM): case report and systematic
review of literature. Mycopathologia, 18(2)6:289-298. https://doi.org/10.1007/s11046-021-00528-2
[10]. Ramani, P., Krishnan, R. P., Pandiar, D., Benitha, J. G.,
Ramalingam, K., and Gheena, S., 2022, Chronic invasive aspergillosis with
fulminant mucormycosis sparing palate in a post-COVID-19 patient-a case report.
Annals of Maxillofacial Surgery, 12(1): 102-105.
10.4103/ams.ams_296_21
[11]. Bala, K., Chander, J., Handa, U., Punia, R. S. and Attri, A.
K., 2015, A prospective study of mucormycosis in north India: experience from a
tertiary care hospital. Medical mycology, 53(3):248-257. https://doi.org/10.1093/mmy/myu086
[12]. Madhavan, Y., Sai, K. V., Shanmugam, D. K., Manimaran, A.,
Guruviah, K., Mohanta, Y. K., Venugopal, D. C., Mohanta, T. K., Sharma, N., and
Muthupandian, S., 2022, Current treatment options for COVID-19 associated
mucormycosis: present status and future perspectives. Journal of Clinical
Medicine, 11(13):3620. https://doi.org/10.3390/jcm11133620
[13]. Madhumitha, M. and Pillai, D. S., 2023, Correlation of
Diabetic Status and Coronavirus Disease 2019 (COVID-19) in Patients with
Mucormycosis: A Retrospective Clinical Study. Cureus, 15(11): e48936. 10.7759/cureus.48936
[14]. Rajashri, R., Muthusekhar, M. R. and Kumar, S. P., 2020,
Mucormycosis following tooth extraction in a diabetic patient: a case report. Cureus,
12(8): e9757. 10.7759/cureus.9757
[15]. Prakash, H., Ghosh, A. K., Rudramurthy, S. M., Singh, P.,
Xess, I., Savio, J., Pamidimukkala, U., Jillwin, J., Varma, S., Das, A. and
Panda, N. K., 2019, A prospective multicenter study on mucormycosis in India:
Epidemiology, diagnosis, and treatment. Medical mycology, 57(4):395-402.
https://doi.org/10.1093/mmy/myy060
[16]. John, T. M., Jacob, C. N. and Kontoyiannis, D. P., 2021,
When uncontrolled diabetes mellitus and severe COVID-19 converge: the perfect
storm for mucormycosis. Journal of fungi, 7(4):298. https://doi.org/10.3390/jof7040298
[17]. Singh, A. K., Singh, R., Joshi, S. R., and Misra, A., 2021,
Mucormycosis in COVID-19: a systematic review of cases reported worldwide and
in India. Diabetes & Metabolic Syndrome: Clinical Research & Reviews,
15(4):102146. https://doi.org/10.1016/j.dsx.2021.05.019
[18]. Roden, M. M., Zaoutis, T. E., Buchanan, W. L., Knudsen, T. A.,
Sarkisova, T. A., Schaufele, R. L., Sein, M., Sein, T., Chiou, C. C., Chu, J. H.,
and Kontoyiannis, D. P., 2005, Epidemiology and outcome of zygomycosis: a
review of 929 reported cases. Clinical infectious diseases, 41(5):634-653.
https://doi.org/10.1086/432579
[19]. Priya, P., Ganesan, V., Rajendran, T., and Geni, V. G., 2020,
Mucormycosis in a tertiary care center in South India: a 4-year experience. Indian
Journal of Critical Care Medicine: Peer-reviewed, Official Publication of
Indian Society of Critical Care Medicine, 24(3):168. 10.5005/jp-journals-10071-23387
[20]. Baldin, C., and Ibrahim, A. S., 2017, Molecular mechanisms
of mucormycosis—The bitter and the sweet. PLoS pathogens, 13(8):e1006408.
https://doi.org/10.1371/journal.ppat.1006408
[21]. Gupta, G., Singh, Y., Thangavelu, L., Singh, S. K., Dureja,
H., Chellappan, D. K., and Dua, K., 2021, Emerging cases of mucormycosis under
COVID‐19
pandemic in India: Misuse of antibiotics. Drug Development Research, 82(7):880-882.
https://doi.org/10.1002/ddr.21862
[22]. Doni, B. R., Peerapur, B. V., Thotappa, L. H., and Hippargi,
S. B., 2011, Sequence of oral manifestations in rhino-maxillary mucormycosis. Indian
Journal of Dental Research, 22(2):331-335. 10.4103/0970-9290.84313
[23]. Nicolatou‐Galitis, O., Sachanas, S., Drogari‐Apiranthitou, M., Moschogiannis, M.,
Galiti, D., Yiakoumis, X., Rontogianni, D., Yiotakis, I., Petrikkos, G., and
Pangalis, G., 2015, Mucormycosis presenting with dental pain and palatal ulcer
in a patient with chronic myelomonocytic leukaemia: case report and literature
review. JMM Case Reports, 2(1), p.e000014. https://doi.org/10.1099/jmmcr.0.000014

