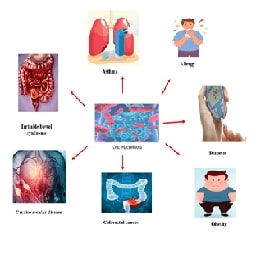
Therapeutic Potential of Gut Microbiota: Insights into Immune Modulation, Metabolite Signaling and Clinical Applications in Inflammatory and Metabolic Diseases
Abstract:
The gut
microbiota is a complex network of microorganisms inhabiting the
gastrointestinal tract and it has a great influence on intestinal health.
Disbalances within metabolic patterns and microbial diversity may cause
inflammatory bowel disease and other diseases. Microorganisms in intestinal
mucosa produce metabolites that act as signalling molecules and influence the
regulation of inflammation and the immune response. SCFAs and secondary bile
acids are metabolites that bind to specific receptors and trigger inflammatory
signals that affect intestinal immunity and host health. Moreover, metabolites
of tryptophan promote the integrity of the epithelial barrier and also interact
with intestinal mucosal aromatic hydrocarbon receptors (AHR) to regulate immune
homeostasis. By acting as precursors to AHR ligands together with SCFAs and
secondary bile acids, dietary-derived indoles relax the intestinal epithelium
inflammation and stress. The mechanistic and therapeutic advances in
non-alcoholic fatty liver disease (NAFLD) aim to alter host metabolism, reduce
inflammation, and reconstitute the integrity of the gut barrier through changes
in the composition of gut microbiota. Since dysbiosis in liver cirrhosis leads
to complications such as bacteremia and hepatic encephalopathy, probiotics and
synbiotics are being investigated to treat associated metabolic disorders.
References:
[1].
Bengmark,
S., 1998, Ecological control of the gastrointestinal tract. The role of
probiotic flora. Gut, 42(1), 2-7.
[2].
Gill,
S. R., Pop, M., DeBoy, R. T., Eckburg, P. B., Turnbaugh, P. J., Samuel, B. S.,
& Nelson, K. E., 2006, Metagenomic analysis of the human distal gut
microbiome. science, 312(5778), 1355-1359.
[3].
Takahashi,
K., Nishida, A., Fujimoto, T., Fujii, M., Shioya, M., Imaeda, H., &
Sugimoto, M., 2016, Reduced abundance of butyrate-producing bacteria species in
the fecal microbial community in Crohn's disease. Digestion, 93(1), 59-65.
[4].
Yarandi,
S. S., Peterson, D. A., Treisman, G. J., Moran, T. H., & Pasricha, P. J., 2016,
Modulatory effects of gut microbiota on the central nervous system: how gut
could play a role in neuropsychiatric health and diseases. Journal of
neurogastroenterology and motility, 22(2), 201.
[5].
Fu,
Y., Lyu, J., & Wang, S., 2023, The role of intestinal microbes on
intestinal barrier function and host immunity from a metabolite perspective.
Frontiers in immunology, 14, 1277102.
[6].
Den
Besten, G., Van Eunen, K., Groen, A. K., Venema, K., Reijngoud, D. J., &
Bakker, B. M., 2013, The role of short-chain fatty acids in the interplay
between diet, gut microbiota, and host energy metabolism. Journal of lipid Research,
54(9), 2325-2340.
[7].
Natividad,
J. M., & Verdu, E. F., 2013, Modulation of intestinal barrier by intestinal
microbiota: pathological and therapeutic implications. Pharmacological
research, 69(1), 42-51.
[8].
Chang,
C., & Lin, H., 2016, Dysbiosis in gastrointestinal disorders. Best practice
& research Clinical gastroenterology, 30(1), 3-15.
[9].
Musso,
G., Gambino, R., & Cassader, M., 2010, Obesity, diabetes, and gut
microbiota: the hygiene hypothesis expanded? Diabetes care, 33(10), 2277-2284.
[10].
Louis,
P., Hold, G. L., & Flint, H. J., 2014, The gut microbiota, bacterial
metabolites and colorectal cancer. Nature reviews microbiology, 12(10),
661-672.
[11].
Macfarlane,
S., & Macfarlane, G. T., 2003, Regulation of short-chain fatty acid
production. Proceedings of the Nutrition Society, 62(1), 67-72.
[12].
Derrien,
M., Vaughan, E. E., Plugge, C. M., & de Vos, W. M., 2004, Akkermansia
muciniphila gen. nov., sp. nov., a human intestinal mucin-degrading bacterium. International
Journal of Systematic and Evolutionary Microbiology, 54(5), 1469-1476.
[13].
Morrison,
D. J., & Preston, T., 2016, Formation of short chain fatty acids by the gut
microbiota and their impact on human metabolism. Gut Microbes, 7(3),
189-200.
[14].
Donohoe,
D. R., Collins, L. B., Wali, A., Bigler, R., Sun, W., & Bultman, S. J., 2012,
The Warburg effect dictates the mechanism of butyrate-mediated histone
acetylation and cell proliferation. Molecular cell, 48(4), 612-626.
[15].
Lin,
L., & Zhang, J., 2017, Role of intestinal microbiota and metabolites on gut
homeostasis and human diseases. BMC immunology, 18, 1-25.
[16].
Martens,
J. H., Barg, H., Warren, M. A., & Jahn, D., 2002, Microbial production of
vitamin B 12. Applied microbiology and biotechnology, 58, 275-285.
[17].
Staley,
C., Weingarden, A. R., Khoruts, A., & Sadowsky, M. J., 2017, Interaction of
gut microbiota with bile acid metabolism and its influence on disease states.
Applied microbiology and biotechnology, 101, 47-64.
[18].
Palau-Rodriguez,
M., Tulipani, S., Isabel Queipo-Ortuño, M., Urpi-Sarda, M., Tinahones, F. J.,
& Andres-Lacueva, C., 2015, Metabolomic insights into the intricate gut
microbial–host interaction in the development of obesity and type 2 diabetes.
Frontiers in Microbiology, 6, 1151.
[19].
Swanson,
P. A., Kumar, A., Samarin, S., Vijay-Kumar, M., Kundu, K., Murthy, N., &
Neish, A. S., 2011, Enteric commensal bacteria potentiate epithelial
restitution via reactive oxygen species-mediated inactivation of focal adhesion
kinase phosphatases. Proceedings of the National Academy of Sciences, 108(21),
8803-8808.
[20].
Reunanen,
J., Kainulainen, V., Huuskonen, L., Ottman, N., Belzer, C., Huhtinen, H., &
Satokari, R., 2015, Akkermansia muciniphila adheres to enterocytes and
strengthens the integrity of the epithelial cell layer. Applied and
environmental microbiology, 81(11), 3655-3662.
[21].
Graziani,
F., Pujol, A., Nicoletti, C., Dou, S., Maresca, M., Giardina, T., &
Perrier, J., 2016, Ruminococcus gnavus E1 modulates mucin expression and
intestinal glycosylation. Journal Of Applied Microbiology, 120(5), 1403-1417.
[22].
Rogier,
E. W., Frantz, A. L., Bruno, M. E., & Kaetzel, C. S., 2014, Secretory IgA
is concentrated in the outer layer of colonic mucus along with gut bacteria.
Pathogens, 3(2), 390-403.
[23].
Hevia,
A., Delgado, S., Sánchez, B., & Margolles, A., 2015, Molecular players
involved in the interaction between beneficial bacteria and the immune system.
Frontiers in microbiology, 6, 1285.
[24].
Ng,
K. M., Ferreyra, J. A., Higginbottom, S. K., Lynch, J. B., Kashyap, P. C.,
Gopinath, S., & Sonnenburg, J. L., 2013, Microbiota-liberated host sugars
facilitate post-antibiotic expansion of enteric pathogens. Nature, 502(7469),
96-99.
[25].
Everard,
A., Belzer, C., Geurts, L., Ouwerkerk, J. P., Druart, C., Bindels, L. B., &
Cani, P. D., 2013, Cross-talk between Akkermansia muciniphila and intestinal
epithelium controls diet-induced obesity. Proceedings of the national academy
of sciences, 110(22), 9066-9071.
[26].
Zhao,
S., Liu, W., Wang, J., Shi, J., Sun, Y., Wang, W., & Hong, J., 2017, Akkermansia
muciniphila improves metabolic profiles by reducing inflammation in chow
diet-fed mice. J Mol Endocrinol, 58(1), 1-14.
[27].
Jandhyala,
S. M., Talukdar, R., Subramanyam, C., Vuyyuru, H., Sasikala, M., & Reddy,
D. N., 2015, Role of the normal gut microbiota. World journal of
gastroenterology: WJG, 21(29), 8787.
[28].
Han,
R., Ma, J., & Li, H.,2018, Mechanistic and therapeutic advances in
non-alcoholic fatty liver disease by targeting the gut microbiota. Frontiers of
Medicine, 12, 645-657.
[29].
Suk,
K. T., & Kim, D. J.,2019, Gut microbiota: novel therapeutic target for
nonalcoholic fatty liver disease. Expert Review of Gastroenterology &
Hepatology, 13(3), 193-204.
[30].
Lv,
H., Tao, F., Peng, L., Chen, S., Ren, Z., Chen, J., & Wan, C., 2023, In
vitro probiotic properties of Bifidobacterium animalis subsp. lactis SF and its
alleviating effect on non-alcoholic fatty liver disease. Nutrients, 15(6),
1355.
[31].
Usami,
M., Miyoshi, M., & Yamashita, H., 2015, Gut microbiota and host metabolism
in liver cirrhosis. World journal of gastroenterology, 21(41), 11597.
[32].
Pushpanathan,
P., Mathew, G. S., Selvarajan, S., Seshadri, K. G., & Srikanth, P., 2019,
Gut microbiota and its mysteries. Indian Journal of Medical Microbiology,
37(2), 268-277.
[33].
Migliore,
L., Nicoli, V., & Stoccoro, A., 2021, Gender specific differences in
disease susceptibility: the role of epigenetics. Biomedicines, 9(6), 652.
[34].
Rizzetto,
L., Fava, F., Tuohy, K. M., & Selmi, C., 2018, Connecting the immune
system, systemic chronic inflammation and the gut microbiome: the role of sex. Journal
of autoimmunity, 92, 12-34.
[35].
Chang,
C. S., & Kao, C. Y., 2019, Current understanding of the gut microbiota
shaping mechanisms. Journal of biomedical science, 26(1), 59.
[36].
Langan,
D., Rose, N. R., & Moudgil, K. D., 2020, Common innate pathways to
autoimmune disease. Clinical Immunology, 212, 108361.
[37].
Neish,
A. S., 2009, Microbes in gastrointestinal health and disease. Gastroenterology,
136(1), 65-80.
[38].
Van
den Elsen, L. W., Garssen, J., Burcelin, R., & Verhasselt, V., 2019, Shaping
the gut microbiota by breastfeeding: the gateway to allergy prevention?
Frontiers in pediatrics, 7, 47.
[39].
Berg,
G., Rybakova, D., Fischer, D., Cernava, T., Vergès, M. C. C., Charles, T.,
& Schloter, M., 2020, Microbiome definition re-visited: old concepts and
new challenges. Microbiome, 8, 1-22.
[40].
Laterza,
L., Rizzatti, G., Gaetani, E., Chiusolo, P., & Gasbarrini, A., 2016, The
gut microbiota and immune system relationship in human graft-versus-host
disease. Mediterranean Journal of Hematology and Infectious Diseases,
8(1).
[41].
Deo,
P. N., & Deshmukh, R., 2019, Oral microbiome: Unveiling the fundamentals. Journal
Of Oral and Maxillofacial Pathology, 23(1), 122-128.
[42].
Dickson,
R. P., & Huffnagle, G. B., 2015, The lung microbiome: new principles for
respiratory bacteriology in health and disease. PLoS pathogens, 11(7),
e1004923.

