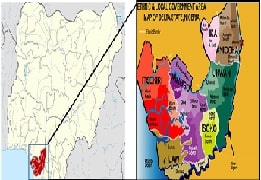
Utilization of Public Healthcare Facilities in Delta State, Nigeria
Abstract:
Nigeria's healthcare system is a complex blend of public
and private providers, each offering varying levels of service and
accessibility. In Delta State, healthcare utilisation patterns are influenced
by factors such as affordability, accessibility, and perceived quality of care.
The study examines the utilisation of public healthcare facilities in Delta
State, Nigeria, exploring residents' preferences and comparing public and
private healthcare services. A cross-sectional quantitative survey was
conducted among 1,191 residents across six Local Government Areas in Delta
State, using face-to-face and virtual questionnaires administered from March 1,
2024, to June 6, 2024. Descriptive statistics were used to analyse the data. The
survey revealed that 92.53% have used public healthcare facilities at least
within the space of five years, while 67.17% were more frequent users. A total of
39.00% of respondents prefer to use public hospitals; 24.90% prefer private
facilities; and 36.10% equally prefer both. In terms of specific features, the public
facilities were rated better for their affordability (89.99%) and accessibility
(59.53%). However, private facilities were perceived to provide more effective care
(58.5%) and operate with better equipment and infrastructure (50.5%), while public
facilities performed better in terms of staff quality (53.65%) and value for
money (53.15%). The study highlights the strong demand for public health
services in Delta State but also identifies areas for improvement in care
quality, equipment, and infrastructure in public facilities, which can be
achieved through targeted investments and quality improvement initiatives to
enhance public confidence and achieve universal health coverage.
References:
[1].
National
Academies of Sciences, E., Division, H. and M., Services, B. on H. C., and Disabilities,
C. on H. C. U. and A. with, 2018, “Factors That Affect Health-Care
Utilization,” Health-Care Utilization as a Proxy in Disability Determination,
National Academies Press (US). [Online]. Available: https://www.ncbi.nlm.nih.gov/books/NBK500097/. [Accessed: 19-Jan-2025].
[2].
Leonard, K. L., and Masatu, M. C., 2007,
“Variations In The Quality Of Care Accessible To Rural Communities In Tanzania:
Some Quality Disparities Might Be Amenable to Policies That Do Not Necessarily
Relate to Funding Levels.,” Health Affairs, 26(Suppl2), pp. w380–w392. https://doi.org/10.1377/hlthaff.26.3.w380.
[3].
Verma,
H., Aggarwal, A., Rattan, V., and Mohanty, U., 2012, “Access to Public Dental
Care Facilities in Chandigarh,” Indian J Dent Res, 23(1), p. 121. https://doi.org/10.4103/0970-9290.99057.
[4].
Mannan,
M. A., 2013, “Access to Public Health Facilities in Bangladesh: A Study on
Facility Utilisation and Burden of Treatment,” The Bangladesh development
studies : The Journal of the Bangladesh Institute of Development Studies,
36(4).
[5].
Gemignani,
R., Tsimpo, C., and Wodon, Q., 2014, “Making Quality Care Affordable for the
Poor: Faith-Inspired Health Facilities in Burkina Faso,” The Review of Faith
& International Affairs, 12(1), pp. 30–44. https://doi.org/10.1080/15570274.2013.876732.
[6].
Ged,
O., 2016, “The Quality of Healthcare Service Delivery in Nigeria: An Assessment
of the Availability of Some Basic Medical Devices/Equipment in the Primary
Health Care Centres in Delta State,” Online Journal of Health and Allied
Sciences, 15(1). [Online]. Available: https://www.ojhas.org/issue57/2016-1-6.html. [Accessed: 24-Nov-2023].
[7].
Fullman,
N., Yearwood, J., Abay, S. M., Abbafati, C., Abd-Allah, F., et al., 2018,
“Measuring Performance on the Healthcare Access and Quality Index for 195
Countries and Territories and Selected Subnational Locations: A Systematic
Analysis from the Global Burden of Disease Study 2016,” The Lancet,
391(10136), pp. 2236–2271. https://doi.org/10.1016/S0140-6736(18)30994-2.
[8].
Al-Jabri,
F. Y. M., Turunen, H., and Kvist, T., 2021, “Patients’ Perceptions of
Healthcare Quality at Hospitals Measured by the Revised Humane Caring Scale,” Journal
of Patient Experience, 8, p. 23743735211065265. https://doi.org/10.1177/23743735211065265.
[9].
Balogun,
J. A., 2021, “A Qualitative Investigation of the Barriers to the Delivery of
High-Quality Healthcare Services in Nigeria,” The Nigerian Healthcare System:
Pathway to Universal and High-Quality Health Care, J.A. Balogun, ed., Springer
International Publishing, Cham, pp. 345–359. https://doi.org/10.1007/978-3-030-88863-3_11.
[10]. Bellio, E., and Buccoliero, L., 2021, “Main
Factors Affecting Perceived Quality in Healthcare: A Patient Perspective
Approach,” The TQM Journal, 33(7), pp. 176–192. https://doi.org/10.1108/TQM-11-2020-0274.
[11]. Ali, J., Jusoh, A., Idris, N., and Nor, K.
M., 2023, “Healthcare Service Quality and Patient Satisfaction:
A Conceptual Framework,” International Journal of Quality &
Reliability Management, 41(2), pp. 608–627. https://doi.org/10.1108/IJQRM-04-2022-0136.
[12]. Agency for Healthcare Research and Quality
(AHRQ), 2015, “Types of Health Care Quality Measures.” [Online]. Available: https://www.ahrq.gov/talkingquality/measures/types.html. [Accessed: 24-Nov-2023].
[13]. Ejughemre, U. J., 2015, “Out of Pocket
Spending for Healthcare Services: A Study Assessing the Relationship between
Payment Methods and Perceived Satisfaction with the Quality of Care in a
Tertiary Health Facility in Delta State, Nigeria,” Journal of Community
Medicine and Primary Health Care, 27(1), pp. 27–36.
[14]. Onwujekwe, O., Ezumah, N., Mbachu, C., Obi,
F., Ichoku, H., Uzochukwu, B., and Wang, H., 2019, “Exploring Effectiveness of
Different Health Financing Mechanisms in Nigeria; What Needs to Change and How
Can It Happen?” BMC Health Services Research, 19(1), p. 661. https://doi.org/10.1186/s12913-019-4512-4.
[15]. Smith, E., 2021, “Foreign Investors Are
Gearing up to Plug Nigeria’s $82 Billion Health-Care Gap,” CNBC. [Online].
Available: https://www.cnbc.com/2021/01/04/nigerias-82-billion-health-care-gap-investors-stand-by.html. [Accessed: 26-Apr-2023].
[16]. WHO, 2023, “Health Financing,” World Health
Organization. [Online]. Available: https://www.who.int/health-topics/health-financing. [Accessed: 15-Sep-2023].
[17]. McIntyre, D., Obse, A. G., Barasa, E. W., and
Ataguba, J. E., 2018, “Challenges in Financing Universal Health Coverage in
Sub-Saharan Africa,” Oxford Research Encyclopedia of Economics and Finance, Oxford
University Press. https://doi.org/10.1093/acrefore/9780190625979.013.28.
[18]. Costa-Font, J., Batinti, A., and Turati, G.,
eds., 2023, Handbook on the Political Economy of Health Systems, Edward
Elgar Publishing. https://doi.org/10.4337/9781800885066.
[19]. Kodali, P. B., 2023, “Achieving Universal
Health Coverage in Low- and Middle-Income Countries: Challenges for Policy
Post-Pandemic and Beyond,” RMHP, Volume 16, pp. 607–621. https://doi.org/10.2147/RMHP.S366759.
[20]. Omuta, G. E. D., 2016, “Infrastructure and
Health Care Services in the Niger Delta Region of Nigeria: A Case Study of
Physical Amenities in the Primary Health Care System in Delta State,” Online
Journal of Health and Allied Sciences, 14(4). [Online]. Available: https://www.ojhas.org/issue56/2015-4-2.html. [Accessed: 14-Apr-2023].
[21]. Kigozi, E., 2020, “Application of Mixed
Methods Approach in Studies on Quality Assurance in Educational Institutions: A
Systematic Review of Literature from 2005-2019,” IJIBS, 6(1), pp.
396–410. https://doi.org/10.20533/ijibs.2046.3626.2020.0051.
[22]. City Population, 2022, “Delta (State,
Nigeria) - Population Statistics, Charts, Map and Location.” [Online].
Available: https://citypopulation.de/en/nigeria/admin/NGA010__delta/. [Accessed: 24-Apr-2023].
[23]. 247ureports.com, 2017,
“Nigeria_Delta_State_map,” 247ureports.com. [Online]. Available: https://247ureports.com/2017/05/delta-state-police-kill-5-kidnappers-armed-robbery-suspects/nigeria_delta_state_map-2/. [Accessed: 21-Apr-2023].
[24]. Gbemre, Z., 2019, “When Will Delta State Be
from from Political Captivity?” Bigpen Nigeria. [Online]. Available: https://bigpenngr.com/2019/03/30/when-will-delta-state-be-free-from-political-captivity/. [Accessed: 21-Apr-2023].
[25]. dbpedia.org, “About: Delta State.” [Online].
Available: https://dbpedia.org/page/Delta_State. [Accessed: 17-Dec-2023].
[26]. United Nations, 2014, Delta State Development
Performance, United Nations, Asaba. [Online]. Available: https://www.undp.org/sites/g/files/zskgke326/files/migration/ng/UNDP_NG_DeltaState_Health_2015.pdf.
[27]. SpinWheelApp, 2023, “Editor | Spin the Wheel
- Random Picker,” Wheel Maker. [Online]. Available: https://spinthewheel.app/0bhxMPPkoe. [Accessed: 17-Dec-2023].
[28]. Glen, S., 2018, “Sample Size in Statistics
(How to Find It): Excel, Cochran’s Formula, General Tips,” Statistics How To.
[Online]. Available: https://www.statisticshowto.com/probability-and-statistics/find-sample-size/. [Accessed: 17-Dec-2023].
[29]. Zoho, 2019, “Sample Size Calculator -
Understanding Sample Size | Zoho Survey,” Zoho. [Online]. Available: https://www.zoho.com/survey/sample-size.html. [Accessed: 17-Dec-2023].
[30]. Levesque, J.-F., Harris, M. F., and Russell,
G., 2013, “Patient-Centred Access to Health Care: Conceptualising Access at the
Interface of Health Systems and Populations,” International Journal for
Equity in Health, 12(1), p. 18. https://doi.org/10.1186/1475-9276-12-18.
[31]. Donabedian, A., 1988, “The Quality of Care.
How Can It Be Assessed?” JAMA, 260(12), pp. 1743–1748. https://doi.org/10.1001/jama.260.12.1743.
[32]. Parasuraman, A. P., Zeithaml, V., and Berry,
L., 1988, “SERVQUAL: A Multiple- Item Scale for Measuring Consumer Perceptions
of Service Quality,” Journal of Retailing.
[33]. Mosadeghrad, A. M., 2012, “A Conceptual
Framework for Quality of Care,” Mater Sociomed, 24(4), pp. 251–261. https://doi.org/10.5455/msm.2012.24.251-261.
[34]. RAND, 2023, “Patient Satisfaction
Questionnaires (PSQ-III and PSQ-18).” [Online]. Available: https://www.rand.org/health-care/surveys_tools/psq.html. [Accessed: 24-Apr-2023].
[35]. Nwokoro, U. U., Ugwa, O. M., Ekenna, A. C.,
Obi, I. F., Onwuliri, C. D., and Agunwa, C., 2022, “Determinants of Primary
Healthcare Services Utilisation in an Under-Resourced Rural Community in Enugu
State, Nigeria: A Cross-Sectional Study,” Pan Afr Med J, 42, p. 209. https://doi.org/10.11604/pamj.2022.42.209.33317.
[36]. Muhammed, K. A., Umeh, K. N., Nasir, S. M.,
and Suleiman, I. H., 2013, “Understanding the Barriers to the Utilization of
Primary Health Care in a Low-Income Setting: Implications for Health Policy and
Planning,” J Public Health Afr, 4(2), p. e13. https://doi.org/10.4081/jphia.2013.e13.
[37]. Nwankwo, I. U., Udeobasi, O., Osakwe, C. S.,
and Okafor, G., 2017, “Public Perception and Assessment of Primary Healthcare
Service in Mbaukwu Community of Awka South Local Government Area, Anambra
State, Southeast Nigeria.” [Online]. Available: https://www.semanticscholar.org/paper/Public-Perception-and-Assessment-of-Primary-Service-Nwankwo-Udeobasi/40b9a08828bb0e6a58c13570c0060a44cf11bd6f#citing-papers. [Accessed: 19-Jan-2025].
[38]. Adam, V. Y., and Awunor, N. S., 2014,
“Perceptions and Factors Affecting Utilization of Health Services in a Rural
Community in Southern Nigeria,” Journal of Medicine and Biomedical Research,
13(2), pp. 117–124. [Online]. Available: https://www.ajol.info/index.php/jmbr/article/view/118413. [Accessed: 19-Jan-2025].
[39]. Otovwe, A., and Elizabeth, S., 2017,
“Utilization of Primary Health Care Services in Jaba Local Government Area of
Kaduna State Nigeria,” Ethiop J Health Sci, 27(4), pp. 339–350.
[Online]. Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5615023/. [Accessed: 19-Jan-2025].
[40]. Darrudi, A., Ketabchi Khoonsari, M. H., and
Tajvar, M., 2022, “Challenges to Achieving Universal Health Coverage Throughout
the World: A Systematic Review,” J Prev Med Public Health, 55(2), pp.
125–133. https://doi.org/10.3961/jpmph.21.542.
[41]. Hanson, K., Brikci, N., Erlangga, D.,
Alebachew, A., De Allegri, M., et al., 2022, “The Lancet Global Health
Commission on Financing Primary Health Care: Putting People at the Centre,” The
Lancet Global Health, 10(5), pp. e715–e772. https://doi.org/10.1016/S2214-109X(22)00005-5.
[42]. Vanguard, 2020, “Delta Is 2nd Least Poor
State in Nigeria - NBS - Vanguard News,” News. [Online]. Available: https://www.vanguardngr.com/2020/05/delta-is-2nd-least-poor-state-in-nigeria-nbs/. [Accessed: 06-Jan-2025].
[43]. Erubami, J., Tebekaemi, P., and Egbon, K.,
2023, “Perception of Online Medical Crowdfunding Posts among Social Media Users
in Nigeria,” Journal of Management and Social Sciences, 8.
[44]. Mahmoud, A. B., Ekwere, T., Fuxman, L., and
Meero, A. A., 2019, “Assessing Patients’ Perception of Health Care Service
Quality Offered by COHSASA-Accredited Hospitals in Nigeria,” SAGE Open,
9(2), p. 2158244019852480. https://doi.org/10.1177/2158244019852480.
[45]. Peabody, J. W., Rahman, O., Fox, K., and
Gertler, P., 1994, “Quality of Care in Public and Private Primary Health Care
Facilities: Structural Comparisons in Jamaica,” Bull Pan Am Health Organ,
28(2), pp. 122–141.
[46]. Agha, S., and Do, M., 2009, “The Quality of
Family Planning Services and Client Satisfaction in the Public and Private
Sectors in Kenya,” International Journal for Quality in Health Care,
21(2), pp. 87–96. https://doi.org/10.1093/intqhc/mzp002.
[47]. Hutchinson, P. L., Do, M., and Agha, S.,
2011, “Measuring Client Satisfaction and the Quality of Family Planning
Services: A Comparative Analysis of Public and Private Health Facilities in
Tanzania, Kenya and Ghana,” BMC Health Serv Res, 11(1), p. 203. https://doi.org/10.1186/1472-6963-11-203.
[48]. Karkee, R., Lee, A. H., and Pokharel, P. K.,
2014, “Women’s Perception of Quality of Maternity Services: A Longitudinal
Survey in Nepal,” BMC Pregnancy Childbirth, 14(1), p. 45. https://doi.org/10.1186/1471-2393-14-45.
[49]. WHO, 2017, “Health Is a Fundamental Human
Right.” [Online]. Available: https://www.who.int/news-room/commentaries/detail/health-is-a-fundamental-human-right. [Accessed: 02-Jan-2023].
[50]. Aregbeshola, B., 2019, “Health Care in
Nigeria: Challenges and Recommendations,” Social Protection. [Online].
Available: https://socialprotection.org/discover/blog/health-care-nigeria-challenges-and-recommendations. [Accessed: 14-Apr-2023].
[51]. Jahan, S., and Oda, T., 2000, “Distributuin
of Public Facilities in Dhaka, Bangladesh: A Spatial Analysis,” [Kobe
University Faculty of Human Development Research Bulletin], 7(2), pp. 201–210. https://doi.org/10.24546/81000376.
[52]. Hu, P., Liu, Z., and Lan, J., 2019, “Equity
and Efficiency in Spatial Distribution of Basic Public Health Facilities: A
Case Study from Nanjing Metropolitan Area,” Urban Policy and Research,
37(2), pp. 243–266. https://doi.org/10.1080/08111146.2018.1523055.
[53]. Kumar, A., Sharma, D. K., Bhojpuri Adhyayan
Kendra, B.H.U. Varanasi, Prakash, S., Department of Geography, Institute of
Science, Banaras Hindu University, Varanasi, Yadava, R. S., and Department of
Geography, Institute of Science, Banaras Hindu University, Varanasi, 2020, “Spatial
Distribution of Public Health Care Facilities in Rural Areas of Nalanda
District, Bihar,” ngji, 66(4), pp. 387–399. https://doi.org/10.48008/ngji.1756.
[54]. Mwesigwa, C. L., Okumu, B. A., Kirabo-Nagemi,
C., Ejuu, E., Kruger, E., and Tennant, M., 2020, “Mapping the Geographic
Availability of Public Dental Services in Uganda Relative to Ruralization and
Poverty of the Population,” JGOH, 2, pp. 86–92. https://doi.org/10.25259/JGOH_66_2019.
[55]. Eze, B., and Jones, M., 2022, “Does the
Perceived Healthcare Quality Provided by Full-Time Government Employee Doctors
in the Public System Differ from the Perceived Care Quality in Their Own
Privately Managed Facilities in Nigeria?” Journal of Hospital
Administration, 10(6). https://doi.org/10.5430/jha.v10n6p1.
[56]. Leslie, H. H., Sun, Z., and Kruk, M. E.,
2017, “Association between Infrastructure and Observed Quality of Care in 4
Healthcare Services: A Cross-Sectional Study of 4,300 Facilities in 8
Countries,” PLoS Med, 14(12), p. e1002464. https://doi.org/10.1371/journal.pmed.1002464.
[57]. Vora, D. K. S., and Mavalankar, D. V., 2014,
“Quality of Reproductive and Child Health Care in the Private Sector in India:
Issues and Options,” International Journal of Science and Research,
3(8), pp. 181–186.
[58]. Bitrán, R., 1995, “Efficiency and Quality in
the Public and Private Sectors in Senegal,” Health Policy Plan, 10(3),
pp. 271–283. https://doi.org/10.1093/heapol/10.3.271.
[59]. FreshAngle, 2021, “Delta State 2022 Budget
Address, Read Before Dtha by His Excellency, Senator, Dr. Ifeanyi Okowa,” Fresh
Angle Nigeria. [Online]. Available: https://freshangleng.com/14976/delta-state-2022-budget-address--read-before-dtha-by-his-excellency--senator--dr--ifeanyi-okowa. [Accessed: 06-Oct-2023].
[60]. DSCHC, 2023, “PharmAccess, DSCHC, Host Access
to Finance Impact Evaluation Report Dissemination,” Delta State Contributory
Health Commission. [Online]. Available: https://dschc.org.ng/PharmAccess,%20DSCHC,%20host%20Access%20to%20Finance%20Impact%20Evaluation%20Report%20Dissemination.html. [Accessed: 06-Oct-2023].

