Perspective for Low COVID-19 Vaccination Uptake and its Effect in Ndola District, Zambia: A Qualitative Analysis
Abstract:
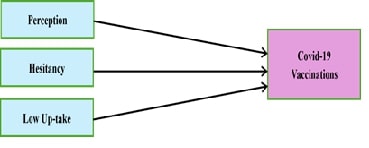
Despite strides in vaccination, hurdles remain, especially regarding the uncertain acceptance of COVID-19 Vaccinations among healthcare workers and the public. This study assessed the Perspective of Low COVID-19 Vaccination Uptake and its Effect; contributing factors, perception and consequences of Low COVID-19 Vaccination Uptake evaluated. The study site was St. Dominic's Hospital (St. DH) and neighbouring area, Ndola, Zambia, utilising a qualitative research design. Purposive sampling was employed selected 50 participants were for Focus Group Discussions, and data was analysed thematically. The participants’ age group was 21-50 years. The findings revealed both positive perceptions and underscored the importance of vaccination in reducing the severity of disease and preventing deaths, recognizing the benefits of immunization. 53.7% of married have negative perceptions statistically significant (P-value <0.001) others expressing concerns about adverse effects, doubt, anxiety about safety, efficacy and mistrust in fast vaccine production. Anxiety about safety was prevalent at 86.4%, particularly in males P<0.001) and 41-50 years P<0.001). Regarding contributing Factors of hesitancy: 65.5% expressed reluctance with significant associations among 31-40 years (AOR=5.81 [2.14-15.80]; P=0.001), also were social and political factors, traditional beliefs, fear and misinformation. Moreover, (96.2%) expressed the negative effects of low COVID-19 vaccination, emphasizing the consequences of economic disruption, increased health risks and mental impacts. Participants highlighted strategies to address the Low COVID-19 Vaccination Uptake: community sensitization through various communication channels, outreach campaigns, and involvement of partnerships, health authorities and international organizations in a coordinated manner to address concerns. Prioritizing accurate information to build trust and improve the Uptake.
References:
[1]. Adane, M., Ademas, A., & Kloos, H., 2022,
Knowledge, attitudes, and perceptions of COVID-19 vaccine and refusal to
receive COVID-19 vaccine among healthcare workers in northeastern Ethiopia. BMC Public Health, 22.
[2]. Afriyie, D. K., Asare, G. A., Amponsah, S. K., &
Godman, B., 2020, COVID-19 pandemic in resource-poor countries: challenges,
experiences and opportunities in Ghana. Journal
of Infection in Developing Countries, 14, 838–843, https://doi.org/10.3855/jidc.12909.
[3]. Fares, S., Elmnyer, M. M., Mohamed, S. S., &
Elsayed, R., 2021, COVID-19 Vaccination Perception and Attitude among
Healthcare Workers in Egypt. Journal of
Primary Care & Community Health, 12, https://doi.org/10.1177/21501327211013303.
[4]. Gerts, D., Shelley, C. D., Parikh, N., Pitts, T.,
Ross, C. W., Fairchild, G., et al., 2021, “Thought I’d share first” and other
conspiracy theory tweets from the COVID-19 infodemic: Exploratory study. JMIR Public Health and Surveillance, 7, https://doi.org/10.2196/26527.
[5]. Haque, A., & Pant, A. B., 2020, Efforts at
COVID-19 vaccine development: Challenges and successes. Vaccines, 8, 1–16, https://doi.org/10.3390/vaccines8040739.
[6]. Islam, M. S., Kamal, A. H. M., Kabir, A., Southern, D.
L., Khan, S. H., Murshid Hasan, S. M., et al., 2021, COVID-19 vaccine rumours
and conspiracy theories: The need for cognitive inoculation against
misinformation to improve vaccine adherence. PLoS One, 16, https://doi.org/10.1371/journal.pone.0251605.
[7]. Kabamba Nzaji, M., Kabamba Ngombe, L., Ngoie Mwamba,
G., Banza Ndala, D. B., Mbidi Miema, J., Luhata Lungoyo, C., et al., 2020,
Acceptability of vaccination against COVID-19 among healthcare workers in the
Democratic Republic of Congo. Pragmatic
and Observational Research, 11, 103–109, https://doi.org/10.2147/por.s271096.
[8]. Kanyike, A. M., Olum, R., Kajjimu, J., Ojilong, D.,
Akech, G. M., Nassozi, D. R., et al., 2021, Acceptance of the coronavirus
disease-2019 vaccine among medical students in Uganda.Tropical Medicine and Health, 49, https://doi.org/10.1186/s41182-021-00331-1.
[9]. Sallam, M., Dababseh, D., Eid, H., Hasan, H., Taim,
D., Al-Mahzoum, K., et al., 2021, Low COVID19 vaccine acceptance is correlated
with conspiracy beliefs among university students in Jordan. International Journal of Environmental
Research and Public Health, 18, 1–14, https://doi.org/10.3390/ijerph18052407.
[10]. Puri, N., Coomes, E. A., Haghbayan, H., &
Gunaratne, K., 2020, social media and vaccine hesitancy: New updates for the
era of COVID-19 and globalized infectious diseases. Human Vaccines & Immunotherapeutics, 16(12), 2586–2593, https://doi.org/10.1080/21645515.2020.1780846.
[11]. Karaivanov, A., Kim, D., Lu, S. E., & Shigeoka,
H., 2022, COVID-19 vaccination mandates and vaccine uptake. Nature Human Behaviour, 6, 1615–1624, https://doi.org/10.1038/s41562-02201363-1.
[12]. Li, Y., & Niu, Y., 2021, A commentary on “The
socio-economic implications of the coronavirus pandemic (COVID-19): A review.” International Journal of Surgery, 95, https://doi.org/10.1016/j.ijsu.2021.106048.
[13]. Martin, K., Moonga, K., Christabel, N. H., Moses, M.,
Steward, M., & Ozawa, S., 2023, Attitudes towards vaccines and intentions
to vaccinate against COVID-19 among undergraduate students at the University of
Zambia. African Journal of Pharmacy and
Pharmacology, 17, 155–164, https://doi.org/10.5897/ajpp2023.5357.
[14]. Ndejjo, R., Chen, N., Kabwama, S. N., Namale, A.,
Wafula, S. T., Wanyana, I., et al., 2023, Uptake of COVID-19 vaccines and
associated factors among adults in Uganda: A cross-sectional survey. BMJ Open, 13, 1–9, https://doi.org/10.1136/bmjopen-2022-067377.
[15]. Morens, D. M., Breman, J. G., Calisher, C. H.,
Doherty, P. C., Hahn, B. H., Keusch, G. T., et al., 2020, The origin of
COVID-19 and why it matters. American
Journal of Tropical Medicine and Hygiene, 103, 955–959, https://doi.org/10.4269/ajtmh.20-0849.
[16]. Mudenda, S., Mukosha, M., Hikaambo, C. N., Meyer, J.
C., Fadare, J., Kampamba, M., et al., 2022, Awareness and acceptance of
COVID-19 vaccines and associated factors among pharmacy students in Zambia. Malawi Medical Journal, 34, 273–280, https://doi.org/10.4314/mmj.v34i4.8.
[17]. Mudenda, S., 2021, COVID-19 vaccine acceptability and
hesitancy in Africa: Implications for addressing vaccine hesitancy. Journal of Biomedical Research &
Environmental Sciences, 2, 999–1004, https://doi.org/10.37871/jbres1342.
[18]. Haque, M., Abubakar, A., Ogunleye, O., Sani, I.,
Sefah, I., Kurdi, A., et al., 2021, Changes in availability, utilization, and
prices of medicines and protection equipment for COVID-19 in an urban
population of Northern Nigeria. Journal
of Research in Pharmacy Practice, 10, 17, https://doi.org/10.4103/jrpp.jrpp_20_92.
[19]. MacDonald, N. E., 2021, How government policies and
political ideologies impact vaccine acceptance: COVID-19 and beyond. CANVax, 1–5, https://canvax.ca/brief/how-governmentpolicies-and-political-ideologies-impact-vaccine-acceptance-covid-19-and
(accessed February 16, 2024).
[20]. Sallam, M., 2021, COVID-19 vaccine hesitancy
worldwide: A concise systematic review of vaccine acceptance rates. Vaccines, 9, 1–15, https://doi.org/10.3390/vaccines9020160.
[21]. Pugliese-Garcia, M., Heyerdahl, L. W., Mwamba, C.,
Nkwemu, S., Chilengi, R., Demolis, R., et al., 2018, Factors influencing
vaccine acceptance and hesitancy in three informal settlements in Lusaka,
Zambia. Vaccine, 36, 5617–5624, https://doi.org/10.1016/j.vaccine.2018.07.042.
[22]. Palamenghi, L., Barello, S., Boccia, S., &
Graffigna, G., 2020, Mistrust in biomedical research and vaccine hesitancy: The
forefront challenge in the battle against COVID-19 in Italy. European Journal of Epidemiology, 35,
785–788, https://doi.org/10.1007/s10654-020-00675-8.
[23]. Creswell, J. W., & Creswell, J. D., 2022, Research Design: Qualitative, Quantitative,
and Mixed Methods Approaches (6th ed.). SAGE Publications.
[24]. MFL, 2022, Facility name: Kavu 1st Level Hospital (St
Dominics Hospital). MFL. http://154.120.217.168:8081/mfl/frontend/web/facility/view?id=2253.
[25]. Wong, C. L., Leung, A. W. Y., Chung, O. M. H., &
Chien, W. T., 2022, Factors influencing COVID-19 vaccination uptake among
community members in Hong Kong: A cross-sectional online survey. BMJ Open, 12, https://doi.org/10.1136/bmjopen-2021-058416.
[26]. Sallam, M., Dababseh, D., Eid, H., Al-Mahzoum, K.,
Al-Haidar, A., Taim, D., et al., 2021, High rates of COVID-19 vaccine hesitancy
and its association with conspiracy beliefs: A study in Jordan and Kuwait among
other Arab countries. Vaccines, 9,
1–16, https://doi.org/10.3390/vaccines9010042.
[27]. Qasim, R., Shah, H., Sultan, A., Yaqoob, M., Haroon,
R., Mistry, S. K., et al., 2022, Exploring the beliefs and experiences regarding
COVID-19 vaccine hesitancy and acceptance in a slum of Karachi, Pakistan. Health Promotion International, 37,
1–12, https://doi.org/10.1093/heapro/daac140.
[28]. Schmelz, K., & Bowles, S., 2022, Opposition to
voluntary and mandated COVID-19 vaccination as a dynamic process: Evidence and
policy implications of changing beliefs. Proceedings
of the National Academy of Sciences of the United States of America, 119, https://doi.org/10.1073/pnas.2118721119.
[29]. MacDonald, N. E., Eskola, J., Liang, X., Chaudhuri,
M., Dube, E., Gellin, B., et al., & SAGE Working Group on Vaccine
Hesitancy, 2015, Vaccine hesitancy: Definition, scope, and determinants. Vaccine, 33, 4161–4164.
[30]. Stecula, D. A., Kuru, O., & Jamieson, K. H., 2020, How trust in experts and media use affect acceptance of common anti-vaccination claims. Harvard Kennedy School Misinformation Review, 1, 1–11, https://doi.org/10.37016/mr-2020-007.
[31]. Mudenda, S., Mukosha, M., Fadare, J. O., & Godman,
B., 2021, Awareness and acceptance of COVID-19 vaccines among pharmacy students
in Zambia: The implications for addressing vaccine hesitancy. Research Square, 1–22.
[32]. Duroseau, B., Kipshidze, N., & Limaye, R. J., 2023, The impact of delayed access to COVID-19 vaccines in low- and lower-middle-income countries. Frontiers in Public Health, 10, https://doi.org/10.3389/fpubh.2022.1087138.

