Harnessing Phytomedicines: Anticancer Strategies Against Osteosarcoma- A Review
Abstract:
Osteosarcoma (OS), the most common primary
bone malignancy, predominantly affects children and adolescents, with poor prognosis
in advanced or metastatic cases. Originating from osteoblasts, OS is
characterized by rapid proliferation, local invasion, and a high propensity for
lung metastasis. It is classified as primary (central or surface) or secondary
when arising from preexisting conditions. Despite advances in chemotherapy and
surgery, the long-term survival rate for patients with metastatic or recurrent
OS remains poor, emphasizing the need for novel therapeutic approaches.
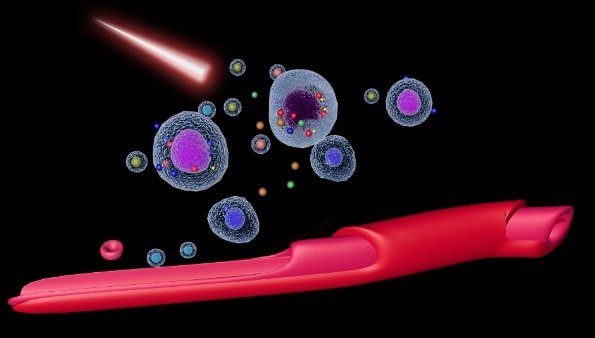
Phytomedicine, derived from plant-based compounds, has garnered attention for
its potential in targeting OS molecular pathways. Phytochemicals such as
curcumin, resveratrol, and epigallocatechin gallate (EGCG) exhibit therapeutic
effects by modulating key pathways, including Wnt/β-catenin, PI3K/AKT/mTOR, and
MAPK/ERK, which are crucial for OS cell migration, proliferation, and survival.
These compounds inhibit angiogenesis, promote apoptosis, and reduce metastasis
by regulating the epithelial-to-mesenchymal transition (EMT). Additionally,
they induce reactive oxygen species (ROS), trigger autophagy, and disrupt
cellular signaling, effectively killing OS cells. Emerging studies highlight
the potential of phytomedicines to enhance current treatments and improve
patient outcomes by offering less harmful and more effective options. This
review explores the molecular mechanisms underlying OS and evaluates
phytomedicine's role in developing innovative therapies. By integrating
genetic, molecular, and clinical profiles, these findings provide valuable insights
for advancing OS diagnosis and management, offering hope for more sustainable
and effective treatment strategies.
References:
[1]. Malawer, M., Sugarbaker,
P. H., Shmookler, B., Bickels, J., Jelinek, J., Sugarbaker, P., & Malawer,
M., 2001, Bone and soft-tissue sarcomas: epidemiology, radiology, pathology and
fundamentals of surgical treatment. Musculoskeletal Cancer Surgery:
Treatment of Sarcomas and Allied Diseases, 3-35.
[2]. DeVita, V., Lawrence,
T., Rosenberg, S., Weinberg, R. A., & DePinho, R. A. 2008, Cancer:
Principles and Practice of Oncology Vols 1 and 2. Philadelphia, PA, USA: Lippincott
Williams & Wilkins.
[3]. Kantarjian, H., Wolff,
R. A., & Koller, C. A. 2011, The MD Anderson manual of medical oncology.
[4]. Alessio, B.,
Massimiliano, D. P., & Nikolin, A., 2014, Osteosarcoma symptoms, diagnosis
and treatment options. Edwin Choy. Library of congress
cataloging-in-publication data.
[5]. Jayaraman, S.,
Natarajan, S. R., Veeraraghavan, V. P., & Jasmine, S., 2023, Unveiling the
anti-cancer mechanisms of calotropin: Insights into cell growth inhibition,
cell cycle arrest, and metabolic regulation in human oral squamous carcinoma
cells (HSC-3). Journal Of Oral Biology And Craniofacial Research, 13(6),
704–713. https://doi.org/10.1016/j.jobcr.2023.09.00.
[6]. Jame, A., James, L.,
Gulley., Carmen, J., 2014, Allegra. Bethesda handbook of clinical oncology -
Fourth edition © 2014
by Lippincott Williams & Wilkins, a Wolters Kluwer business. Section 7:
Musculoskeletal; 21. Sarcomas and Malignancies of the Bone, Patrick J. Mansky
and Lee J. Helman. ISBN 978-1-4511-8758-8. Library of Congress
Cataloging-in-Publication Data.
[7]. Kazantseva, L., Becerra,
J., & Santos-Ruiz, L., 2022, Traditional Medicinal Plants as a Source of
Inspiration for Osteosarcoma Therapy. Molecules (Basel,
Switzerland), 27(15),5008. https://doi.org/10.3390/molecules27155008
[8]. Durfee, R. A., Mohammed,
M., & Luu, H. H. 2016, Review of Osteosarcoma and Current
Management. Rheumatology and therapy, 3(2), 221–243. https://doi.org/10.1007/s40744-016-0046-y
[9]. Hansen, M. F., Seton,
M., & Merchant, A., 2006, Osteosarcoma in Paget's disease of bone. Journal
of bone and mineral research: The official journal of the American Society for
Bone and Mineral Research, 21 Suppl 2, P58–P63. https://doi.org/10.1359/jbmr.06s211.
[10].
Deyrup,
A. T., Montag, A. G., Inwards, C. Y., Xu, Z., Swee, R. G., & Krishnan Unni,
K., 2007, Sarcomas arising in Paget disease of bone: a clinicopathologic
analysis of 70 cases. Archives of pathology & laboratory medicine, 131(6),
942–946. https://doi.org/10.5858/2007-131-942-SAIPDO.
[11].
Rickel,
K., Fang, F., & Tao, J., 2017, Molecular genetics of osteosarcoma. Bone, 102,
69–79. https://doi.org/10.1016/j.bone.2016.10.017.
[12].
Fiedorowicz,
M., Bartnik, E., Sobczuk, P., Teterycz, P., & Czarnecka, A. M., 2018,
Molecular biology of sarcoma. Oncology in Clinical Practice, 14(6),
307-330.
[13].
Czarnecka,
A. M., Synoradzki, K., Firlej, W., Bartnik, E., Sobczuk, P., Fiedorowicz, M., .
& Rutkowski, P., 2020, Molecular biology of osteosarcoma. Cancers, 12(8),
2130.
[14].
Fathima,
J. S., Jayaraman, S., Sekar, R., & Syed, N. H., 2024, The role of MicroRNAs
in the diagnosis and treatment of oral premalignant disorders. Odontology,
1-10.
[15].
Savage,
S. A., & Mirabello, L., 2011, Using epidemiology and genomics to understand
osteosarcoma etiology. Sarcoma, 2011(1), 548151.
[16].
Huvos,
A. G., 1986, Osteogenic sarcoma of bones and soft tissues in older persons. A
clinicopathologic analysis of 117 patients older than 60 years. Cancer, 57(7),
1442-1449.
[17].
Rani,
A. S., & Kumar, S., 1992, Transformation of non-tumorigenic osteoblast-like
human osteosarcoma cells by hexavalent chromates: alteration of morphology,
induction of anchorage-independence and proteolytic function. Carcinogenesis, 13(11),
2021-2027.
[18].
Dutra,
F. R., & Largent, E. J., 1950, Osteosarcoma induced by beryllium
oxide. The American journal of pathology, 26(2), 197.
[19].
Mazabraud,
A., 1975, Experimental production of bone sarcomas in the rabbit by a single
local injection of beryllium. Bulletin Du Cancer, 62(1),
49-58.
[20].
Casali,
P. G., Bielack, S., Abecassis, N., Aro, H. T., Bauer, S., Biagini, R., &
Blay, J. Y., 2018, Bone sarcomas: ESMO–PaedCan–EURACAN Clinical Practice
Guidelines for diagnosis, treatment and follow-up. Annals of Oncology, 29,
iv79-iv95.
[21].
Sruthi,
M. A., Mani, G., Ramakrishnan, M., & Selvaraj, J., 2023, Dental caries as a
source of Helicobacter pylori infection in children: An RT‐PCR study. International
Journal of Paediatric Dentistry, 33(1), 82-88.
[22].
Rothzerg,
E., Xu, J., & Wood, D, 2023, Different Subtypes of Osteosarcoma:
Histopathological Patterns and Clinical Behaviour. Journal of Molecular
Pathology, 4(2), 99-108.
[23].
Kundu,
Z. S., 2014, Classification, imaging, biopsy and staging of osteosarcoma. Indian
Journal Of Orthopaedics, 48(3), 238-246.
[24].
Abate,
M. E., Longhi, A., Galletti, S., Ferrari, S., & Bacci, G., 2010,
Non‐metastatic osteosarcoma of the extremities in children aged 5 years or
younger. Pediatric Blood & Cancer, 55(4), 652-654.
[25].
Kager,
L., Zoubek, A., Pötschger, U., Kastner, U., Flege, S., Kempf-Bielack, B.,
& Bielack, S. S., 2003, Primary metastatic osteosarcoma: presentation and
outcome of patients treated on neoadjuvant Cooperative Osteosarcoma Study Group
protocols. Journal of Clinical Oncology, 21(10), 2011-2018.
[26].
Pakos,
E. E., Nearchou, A. D., Grimer, R. J., Koumoullis, H. D., Abudu, A., Bramer, J.
A., & Ioannidis, J. P., 2009, Prognostic factors and outcomes for
osteosarcoma: an international collaboration. European Journal Of
Cancer, 45(13), 2367-2375.
[27].
Cho,
W. H., Song, W. S., Jeon, D. G., Kong, C. B., Kim, M. S., Lee, J. A., &
Lee, S. Y., 2010, Differential presentations, clinical courses, and survivals
of osteosarcomas of the proximal humerus over other extremity locations. Annals
Of Surgical Oncology, 17, 702-708.
[28].
Kaste,
S. C., Liu, T., Billups, C. A., Daw, N. C., Pratt, C. B., & Meyer, W. H.,
2004, Tumor size as a predictor of outcome in pediatric non‐metastatic
osteosarcoma of the extremity. Pediatric Blood & Cancer, 43(7),
723-728.
[29].
Kager,
L., Zoubek, A., Dominkus, M., Lang, S., Bodmer, N., Jundt, G., & COSS Study
Group., 2010, Osteosarcoma in very young children: experience of the
Cooperative Osteosarcoma Study Group. Cancer, 116(22),
5316-5324.
[30].
Hayden,
J. B., & Hoang, B. H., 2006, Osteosarcoma: basic science and clinical
implications. Orthopedic Clinics, 37(1), 1-7.
[31].
Misaghi,
A., Goldin, A., Awad, M., & Kulidjian, A. A., 2018, Osteosarcoma: A
comprehensive review. Sicot-j, 4.
[32].
Ries,
L. A. G., Melbert, D., Krapcho, M., Stinchcomb, D. G., Howlader, N., Horner, M.
J., & Edwards, B., 2008, SEER cancer statistics review, 1975–2005. Bethesda,
MD: National Cancer Institute, 2999.
[33].
Ajani,
U. A., 2007, United States cancer statistics: 2004 incidence and mortality.
[34].
U.S.
Cancer Statistics Working Group. United States Cancer Statistics: 2001
Incidence and Mortality. Atlanta, GA: Centers for Disease Control and
Prevention and National Cancer Institute; 2004.
[35].
Mirabello,
L., Troisi, R. J., & Savage, S. A., 2009, International osteosarcoma
incidence patterns in children and adolescents, middle ages and elderly
persons. International Journal Of Cancer, 125(1), 229-234.
[36].
Colina,
M., La Corte, R., De Leonardis, F., & Trotta, F., 2008, Paget’s disease of
bone: a review. Rheumatology International, 28(11), 1069-1075.
[37].
Cooper,
C., Harvey, N. C., Dennison, E. M., & van Staa, T. P., 2006, Update on the
epidemiology of Paget's disease of bone. Journal of Bone and Mineral
Research, 21(S2), P3-P8.
[38].
Mirabello,
L., Troisi, R. J., & Savage, S. A., 2009, Osteosarcoma incidence and
survival rates from 1973 to 2004: data from the Surveillance, Epidemiology, and
End Results Program. Cancer: Interdisciplinary International
Journal of the American Cancer Society, 115(7), 1531-1543.
[39].
Ries,
L. A. G., Smith, M. A., Gurney, J., Linet, M., Tamra, T., Young, J., 1999,
Cancer incidence and survival among children and adolescents: United States
SEER Program 1975-1995. Cancer incidence and survival among children and
adolescents: United States SEER Program 1975-1995.
[40].
Polednak,
A. P., 1985, Primary bone cancer incidence in black and white residents of New
York State. Cancer, 55(12), 2883-2888.
[41].
Parkin,
D. M., Stiller, C. A., Draper, G. J., & Bieber, C. A., 1988, The
international incidence of childhood cancer. International Journal of
Cancer, 42(4), 511-520.
[42].
Linabery,
A. M., & Ross, J. A., 2008, Trends in childhood cancer incidence in the US
(1992–2004). Cancer: Interdisciplinary International Journal of the
American Cancer Society, 112(2), 416-432.
[43].
Oyemade,
G. A. A., & Abioye, A. A., 1982, Primary malignant tumors of bone:
incidence in Ibadan, Nigeria. Journal of the National Medical
Association, 74(1), 65.
[44].
Oboirien,
M., & Khalid, A., 2013, Knowledge and belief about traditional bone
setters’ practices in Sokoto, North-West Nigeria. Internet J Orthop
Surg, 21(2).
[45].
Fraumeni
JR, J. F., 1967, Stature and malignant tumors of bone in childhood and
adolescence. Cancer, 20(6), 967-973.
[46].
Ruza,
E., Sotillo, E., Sierrasesúmaga, L., Azcona, C., & Patiño-García, A., 2003,
Analysis of polymorphisms of the vitamin D receptor, estrogen receptor, and
collagen Iα1 genes and their relationship with height in children with bone
cancer. Journal of pediatric hematology/oncology, 25(10),
780-786.
[47].
Spjut,
H. J., 1971, Tumors of bone and cartilage. US Department of Defense, Armed
Forces Institute of Pathology.
[48].
Longhi,
A., Pasini, A., Cicognani, A., Baronio, F., Pellacani, A., Baldini, N., &
Bacci, G., 2005, Height as a risk factor for osteosarcoma. Journal of
pediatric hematology/oncology, 27(6), 314-318.
[49].
Goodman,
M. A., McMaster, J. H., Drash, A. L., Diamond, P. E., Kappakas, G. S., &
Scranton Jr, P. E., 1978, Metabolic and endocrine alterations in osteosarcoma
patients. Cancer, 42(2), 603-610.
[50].
Mirabello,
L., Pfeiffer, R., Murphy, G., Daw, N. C., Patiño-Garcia, A., Troisi, R. J., .
& Savage, S. A., 2011, Height at diagnosis and birth-weight as risk factors
for osteosarcoma. Cancer Causes & Control, 22, 899-908.
[51].
Matsunaga,
E., 1980, Hereditary retinoblastoma: host resistance and second primary
tumors. Journal of the National Cancer Institute, 65(1),
47-51.
[52].
Draper,
G. J., Sanders, B. M., & Kingston, J. E., 1986, Second primary neoplasms in
patients with retinoblastoma. British journal of cancer, 53(5),
661-671.
[53].
Matsunaga,
E., 1980, Hereditary retinoblastoma: host resistance and second primary
tumors. Journal of the National Cancer Institute, 65(1),
47-51.
[54].
Draper,
G., Sanders, B., Kingston, J., 1986, Second primary neoplasms in patients with
retinoblastoma. British Journal of Cancer, 53(5), 661.
[55].
Wang,
L. L., Gannavarapu, A., Kozinetz, C. A., Levy, M. L., Lewis, R. A.,
Chintagumpala, M. M., Ruiz-Maldanado, R., Contreras-Ruiz, J., Cunniff, C., Erickson,
R. P., Lev, D., Rogers, M., Zackai, E. H., & Plon, S. E., 2003, Association
between osteosarcoma and deleterious mutations in the RECQL4 gene in
Rothmund-Thomson syndrome. Journal of the National Cancer Institute, 95(9),
669–674. https://doi.org/10.1093/jnci/95.9.669.
[56].
Hicks,
M. J., Roth, J. R., Kozinetz, C. A., & Wang, L. L., 2007, Clinicopathologic
features of osteosarcoma in patients with Rothmund-Thomson syndrome. Journal
of clinical oncology : Official journal of the American Society of Clinical
Oncology, 25(4), 370–375. https://doi.org/10.1200/JCO.2006.08.4558.
[57].
Porter,
D. E., Holden, S. T., Steel, C. M., Cohen, B. B., Wallace, M. R., & Reid,
R., 1992, A significant proportion of patients with osteosarcoma may belong to
Li-Fraumeni cancer families. The Journal of bone and joint surgery.
British volume, 74(6), 883–886. https://doi.org/10.1302/0301-620X.74B6.1447251.
[58].
Araki,
N., Uchida, A., Kimura, T., Yoshikawa, H., Aoki, Y., Ueda, T., Takai, S., Miki,
T., & Ono, K., 1991, Involvement of the retinoblastoma gene in primary
osteosarcomas and other bone and soft-tissue tumors. Clinical
orthopaedics and related research, (270), 271–277.
[59].
Thomas,
L., Mautner, V. F., Cooper, D. N., & Upadhyaya, M., 2012, Molecular
heterogeneity in malignant peripheral nerve sheath tumors associated with
neurofibromatosis type 1. Human genomics, 6(1), 18. https://doi.org/10.1186/1479-7364-6-18.
[60].
Deshpande,
A., & Hinds, P. W., 2006, The retinoblastoma protein in osteoblast
differentiation and osteosarcoma. Current molecular medicine, 6(7),
809–817. https://doi.org/10.2174/156652401060607080.
[61].
Feugeas,
O., Guriec, N., Babin-Boilletot, A., Marcellin, L., Simon, P., Babin, S.,
Thyss, A., Hofman, P., Terrier, P., Kalifa, C., Brunat-Mentigny, M., Patricot,
L. M., & Oberling, F., 1996, Loss of heterozygosity of the RB gene is a
poor prognostic factor in patients with osteosarcoma. Journal of
clinical oncology : official journal of the American Society of Clinical
Oncology, 14(2), 467–472. https://doi.org/10.1200/JCO.1996.14.2.467.
[62].
Miller,
C. W., Aslo, A., Tsay, C., Slamon, D., Ishizaki, K., Toguchida, J., Yamamuro,
T., Lampkin, B., & Koeffler, H. P., 1990, Frequency and structure of p53
rearrangements in human osteosarcoma. Cancer research, 50(24),
7950–7954.
[63].
Miller,
C. W., Aslo, A., Won, A., Tan, M., Lampkin, B., & Koeffler, H. P., 1996,
Alterations of the p53, Rb and MDM2 genes in osteosarcoma. Journal of
cancer research and clinical oncology, 122(9), 559–565. https://doi.org/10.1007/BF01213553.
[64].
Gokgoz,
N., Wunder, J. S., Mousses, S., Eskandarian, S., Bell, R. S., & Andrulis,
I. L., 2001, Comparison of p53 mutations in patients with localized
osteosarcoma and metastatic osteosarcoma. Cancer, 92(8),
2181–2189. https://doi.org/10.1002/1097-0142(20011015)92:8<2181::aid-cncr1561>3.0.co;2-3.
[65].
Berman,
S. D., Calo, E., Landman, A. S., Danielian, P. S., Miller, E. S., West, J. C.,
Fonhoue, B. D., Caron, A., Bronson, R., Bouxsein, M. L., Mukherjee, S., &
Lees, J. A., 2008, Metastatic osteosarcoma induced by inactivation of Rb and
p53 in the osteoblast lineage. Proceedings of the National Academy of
Sciences of the United States of America, 105(33), 11851–11856. https://doi.org/10.1073/pnas.0805462105.
[66].
Walkley,
C. R., Qudsi, R., Sankaran, V. G., Perry, J. A., Gostissa, M., Roth, S. I.,
Rodda, S. J., Snay, E., Dunning, P., Fahey, F. H., Alt, F. W., McMahon, A. P.,
& Orkin, S. H., 2008, Conditional mouse osteosarcoma, dependent on p53 loss
and potentiated by loss of Rb, mimics the human disease. Genes &
development, 22(12), 1662–1676. https://doi.org/10.1101/gad.1656808.
[67].
Desai,
A. G., Qazi, G. N., Ganju, R. K., El-Tamer, M., Singh, J., Saxena, A. K., Bedi,
Y. S., Taneja, S. C., & Bhat, H. K., 2008, Medicinal plants and cancer
chemoprevention. Current drug metabolism, 9(7), 581–591. https://doi.org/10.2174/138920008785821657.
[68].
Yin,
S. Y., Wei, W. C., Jian, F. Y., & Yang, N. S., 2013, Therapeutic
applications of herbal medicines for cancer patients. Evidence-based
complementary and alternative medicine : eCAM, 302426. https://doi.org/10.1155/2013/302426.
[69]. Cragg, G. M., &
Newman, D. J., 2005, Plants as a source of anti-cancer agents. Journal
of ethnopharmacology, 100(1-2), 72–79. https://doi.org/10.1016/j.jep.2005.05.011.
[70]. Krishnan, R. P.,
Pandiar, D., Ramani, P., & Jayaraman, S., 2024, Molecular profiling of oral
epithelial dysplasia and oral squamous cell carcinoma using next generation
sequencing. Journal of stomatology, oral and maxillofacial
surgery, 126(4), 102120. Advance online publication. https://doi.org/10.1016/j.jormas.2024.102120.
[71].
Prasanth,
N. V., Dilip, C., Sanal Dev, K. T., Augustine, L., & Saraswathi, R., 2010,
Evaluation of in vitro cytotoxic and antioxidant activities of Ipomoea
batatas. Int J Pharm Pharm Sci, 2(3), 91-2.
[72]. Umadevi, M., Kumar, K.
S., Bhowmik, D., & Duraivel, S., 2013, Traditionally used anticancer herbs
in India. Journal of Medicinal Plants Studies, 1(3), 56-74.
[73]. Rahmani, A. H.,
Alzohairy, M. A., Khan, M. A., & Aly, S. M., 2014, Therapeutic implications
of black seed and its constituent thymoquinone in the prevention of cancer
through inactivation and activation of molecular pathways. Evidence‐Based
Complementary and Alternative Medicine, 2014(1), 724658.
[74]. Huang, W. Y., Cai, Y.
Z., & Zhang, Y., 2009, Natural phenolic compounds from medicinal herbs and
dietary plants: potential use for cancer prevention. Nutrition and
cancer, 62(1), 1-20.
[75]. Sagar, S., Ramani, P.,
Moses, S., Gheena, S., & Selvaraj, J., 2024, Correlation of salivary
cytokine IL-17A and 1, 25 dihydroxycholecalciferol in patients undergoing
orthodontic treatment. Odontology, 1-10.
[76]. Chen, S., Jin, Z., Dai,
L., Wu, H., 2018, Aloperine induces apoptosis and inhibits invasion in MG-63
and U2OS human osteosarcoma cells. Biomed Pharmacother, 97, 45-52.
[77].
Chen,
C. Z., 2016, Berberine induced apoptosis of human osteosarcoma cells by
inhibiting phosphoinositide 3 kinase/protein kinase B (PI3K/Akt) signal pathway
activation.
[78].
Chen,
G., Xia, H., Zhang, Z. G., & Yu, H. L., 2017, Resveratrol in management of
bone and spinal cancers. Natural product research, 33(4),
516-526.
[79].
Wang,
Y., Xu, S., Wu, Y., & Zhang, J., 2016, Cucurbitacin E inhibits osteosarcoma
cells proliferation and invasion through attenuation of PI3K/AKT/mTOR
signalling pathway. Bioscience reports, 36(6), e00405.
[80].
Peng,
L., Liu, A., Shen, Y., Xu, H. Z., Yang, S. Z., Ying, X. Z., . & Shen, W.
D., 2013, Antitumor and anti-angiogenesis effects of thymoquinone on
osteosarcoma through the NF-κB pathway. Oncology reports, 29(2),
571-578.
[81]. Li, X., Zhao, Y., Wu, W.
K., Liu, S., Cui, M., & Lou, H., 2011, Solamargine induces apoptosis
associated with p53 transcription-dependent and transcription-independent
pathways in human osteosarcoma U2OS cells. Life sciences, 88(7-8),
314-321.
[82]. Jin, S., Xu, H. G.,
Shen, J. N., Chen, X. W., Wang, H., & Zhou, J. G., 2009, Apoptotic effects
of curcumin on human osteosarcoma U2OS cells. Orthopaedic surgery, 1(2),
144-152.
[83]. Lv, T. Z., & Wang,
G. S., 2015, Antiproliferation potential of withaferin A on human osteosarcoma
cells via the inhibition of G2/M checkpoint proteins. Experimental and
therapeutic medicine, 10(1), 323-329.
[84]. Pazhani, J., Chanthu,
K., Jayaraman, S., & Varun, B. R., 2023, Evaluation of salivary MMP-9 in
oral squamous cell carcinoma and oral leukoplakia using ELISA. Journal
of Oral and Maxillofacial Pathology, 27(4), 649-654.
[85].
Chen,
X. J., Duan, F. D., Zhang, H. H., Xiong, Y., & Wang, J., 2012, Sodium
selenite-in duced apoptosis mediated by ROS attack in human osteosarcoma U2OS
cells. Biological trace element research, 145, 1-9.
[86].
Yang,
Q., Li, S., Fu, Z., Lin, B., Zhou, Z., Wang, Z., . & Cai, Z., 2017,
Shikonin promotes adriamycin‑induced apoptosis by upregulating caspase‑3 and
caspase‑8 in osteosarcoma. Molecular medicine reports, 16(2),
1347-1352.
[87]. Pichaiyan, V.,
Mariyappan, S., Saravanan, R., & Ramalingam, S., 2018, Herbal remedy for
osteosarcoma-challenging evolution. Asian Journal of Pharmaceutical and
Clinical Research, 52-56.
[88]. Yang, J., Nie, J., Ma,
X., Wei, Y., Peng, Y., & Wei, X., 2019, Targeting PI3K in cancer:
mechanisms and advances in clinical trials. Molecular cancer, 18(1),
26.
[89]. Arafeh, R., &
Samuels, Y., 2019, PIK3CA in cancer: The past 30 years. In Seminars in
cancer biology (Vol. 59, pp. 36-49). Academic Press.
[90]. Whitman, M., Downes, C.
P., Keeler, M., Keller, T., & Cantley, L. (1988). Type I
phosphatidylinositol kinase makes a novel inositol phospholipid,
phosphatidylinositol-3-phosphate. Nature, 332(6165),
644-646.
[91]. Alzahrani, A. S., 2019,
PI3K/Akt/mTOR inhibitors in cancer: At the bench and bedside. In Seminars
in cancer biology (Vol. 59, pp. 125-132). Academic Press.
[92].
Jayaraman,
S., Natarajan, S. R., Ponnusamy, B., Veeraraghavan, V. P., & Jasmine, S.,
2023, Unlocking the potential of beta sitosterol: Augmenting the suppression of
oral cancer cells through extrinsic and intrinsic signalling mechanisms. The
Saudi Dental Journal, 35(8), 1007-1013.
[93].
Tapia,
O., Riquelme, I., Leal, P., Sandoval, A., Aedo, S., Weber, H., & Roa, J.
C., 2014, The PI3K/AKT/mTOR pathway is activated in gastric cancer with
potential prognostic and predictive significance. Virchows Archiv, 465,
25-33.
[94].
Porta,
C., Paglino, C., & Mosca, A., 2014, Targeting PI3K/Akt/mTOR signaling in
cancer. Frontiers in oncology, 4, 64.
[95].
Uddin,
M. J., Shamsuzzaman, M., Horng, L., Labrique, A., Vasudevan, L., Zeller, K.,
Chowdhury, M., Larson, C. P., Bishai, D., & Alam, N., 2016, Use of mobile
phones for improving vaccination coverage among children living in rural
hard-to-reach areas and urban streets of Bangladesh. Vaccine, 34(2),
276–283. https://doi.org/10.1016/j.vaccine.2015.11.024.
[96].
O’Donnell,
J. S., Massi, D., Teng, M. W., & Mandala, M., 2018, PI3K-AKT-mTOR
inhibition in cancer immunotherapy, redux. In Seminars in cancer
biology (Vol. 48, pp. 91-103). Academic Press.
[97].
Ramakrishnan,
V., & Kumar, S., 2018, PI3K/AKT/mTOR pathway in multiple myeloma: from
basic biology to clinical promise. Leukemia & lymphoma, 59(11),
2524-2534.
[98].
Gobin,
B., Huin, M. B., Lamoureux, F., Ory, B., Charrier, C., Lanel, R., &
Heymann, D., 2015, BYL719, a new α‐specific PI3K inhibitor: Single
administration and in combination with conventional chemotherapy for the
treatment of osteosarcoma. International journal of cancer, 136(4),
784-796.
[99].
Meric-Bernstam,
F., Akcakanat, A., Chen, H., Do, K. A., Sangai, T., Adkins, F., & Yao, J.,
2012, PIK3CA/PTEN mutations and Akt activation as markers of sensitivity to
allosteric mTOR inhibitors. Clinical cancer research, 18(6),
1777-1789.
[100].
Yang,
Q., & Guan, K. L., 2007, Expanding mTOR signaling. Cell research, 17(8),
666-681.
[101].
Yu,
G., Wang, J., Chen, Y., Wang, X., Pan, J., Li, G., & Xie, K., 2009,
Overexpression of phosphorylated mammalian target of rapamycin predicts lymph
node metastasis and prognosis of chinese patients with gastric cancer. Clinical
Cancer Research, 15(5), 1821-1829.
[102].
Luo,
Y., Xu, W., Li, G., & Cui, W., 2018, Weighing in on mTOR complex 2
signaling: the expanding role in cell metabolism. Oxidative medicine
and cellular longevity, 2018(1), 7838647.
[103]. Smith, C. R., Leon, M.
B., Mack, M. J., Miller, D. C., Moses, J. W., Svensson, L. G., & Pocock, S.
J., 2011, Transcatheter versus surgical aortic-valve replacement in high-risk
patients. New England Journal of Medicine, 364(23), 2187-2198.
[104]. Steelman, L. S., Abrams,
S. L., Whelan, J., Bertrand, F. E., Ludwig, D. E., Bäsecke, J., & McCubrey,
J. A., 2008, Contributions of the Raf/MEK/ERK, PI3K/PTEN/Akt/mTOR and Jak/STAT
pathways to leukemia. Leukemia, 22(4), 686-707.
[105]. Yasothkumar, D., Ramani,
P., Jayaraman, S., Ramalingam, K., & Tilakaratne, W. M., 2024, Expression
Profile of Circulating Exosomal microRNAs in Leukoplakia, Oral Submucous
Fibrosis, and Combined Lesions of Leukoplakia and Oral Submucous Fibrosis. Head
and Neck Pathology, 18(1), 28.
[106]. Kang, X. H., Hu, W. H,
Pei, S. S., 2017, Effects of Sodium Cantharidate and vitamin B6
on apoptosis and survivin expression in human osteosarcoma
cells. China
Medical Herald.
14, 16-19.
[107]. Hua, F., Shang, S., Hu, Z. W., 2017, Seeking new anti-cancer agents from autophagy-regulating natural products. J Asian Nat Prod Res. 19(4), 305-313.

