Antimicrobial Activity of Novel Triterpenoid Derivatives Isolated from Ethyl Acetate Extract of Cassia fistula Stem Bark: In-vitro and In-silico Analysis
Abstract:
Standard
treatments for bacterial infections are becoming increasingly ineffective as
antibiotic resistance grows worldwide. Due to the overuse of antibiotics,
multidrug-resistant bacteria have emerged as a serious hazard and a major
worldwide healthcare issue in the twenty-first century. Traditional approaches
to creating novel antibacterial medications are insufficient to fulfil the
existing pipeline, hence new tactics in the field of antibacterial discovery
are being developed. Cassia fistula (C.fistula), a member of the Leguminosae
family, naturally contains antibacterial properties. The plant is used to cure
skin diseases, liver problems, tuberculose glands, and hematemesis, pruritus,
leucoderma, and diabetes. As a result, effective antimicrobial treatment beyond
antibiotics is critical. The Plants contain a wide range of secondary
metabolites, including tannins, terpenoids, alkaloids, flavonoids, and
glycosides, which have antibacterial characteristics. Terpenenes and terpenoids
are effective against bacteria, fungus, viruses, and protozoa. Terpenes' mode
of action involves lipophilic chemicals disrupting membranes. Adding a methyl
group to increase the hydrophilicity of kaurene diterpenoids decreased their
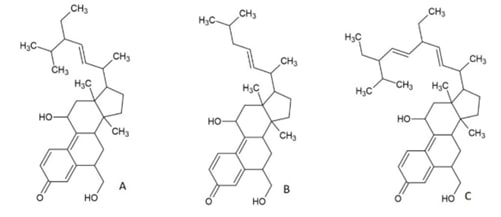
antibacterial efficacy significantly. In the study, antibacterial screening
assay against S.aureus and K.pneumonia, a new chemical isolated from
C.fistula's ethyl acetate extract demonstrated wider inhibitory zones than the
positive control. The treated culture's genomic DNA profile remains unchanged after
treatment with the new chemical. The new chemical suppressed protein synthesis,
resulting in reduced protein content in treated cultures of both strains,
confirming its bactericidal effect. Further immune-blot analysis is required to
confirm the particular protein. Investigating a novel triterpenoid that reduces
pharmaceutical drug load and resistance risk, as well as treatment costs, could
offer promising therapeutic options for treating secondary urinary tract
infections associated with diabetes.
References:
[1].
Deshmukh, R. K., &
Gaikwad, K. K., 2022, Natural antimicrobial and antioxidant compounds for
active food packaging applications. Biomass Conversion and Biorefinery,
1-22. doi:10.1007/s13399-022-02623.
[2]. Towers, G. H., Lopez, A., Hudson, J. B, 2001,
Antiviral and antimicrobial activities of medicinal plants Journal
of Ethnopharmacology, 77, 189-96.https://doi.org/
10.1016/s0378-8741(01)00292-6.
[3].
Dahanukar, S. A.,
Kulkarni, R. A, & Rege, N. N.,2000, Pharmacology of medicinal plants and
natural products. Indian Journal of Pharmacology, 32(4): S81-S118.
[4].
Rajalakshmi, M., Eliza, J.,
Cecilia Edel Priya, L. V., et al., 2009, Biochemical and histopathological
study of Cassia fistula bark extracts in STZ induced diabetic rats. International
Journal of Biotechnology, 2: 134-139.
[5].
Sabapathy, I., Christopher,
I., Periyasamy, V., & Manikkam, R., 2022, Molecular docking analysis of
tetracyclic triterpenoids from Cassia fistula L. with targets for diabetes
mellitus. Bioinformation, 2022, 18(3), 200-205.
doi:10.6026/97320630018200.
[6].
Jayaraman, S., Natarajan, S.
R., Ponnusamy, B., Veeraraghavan, V. P., & Jasmine, S., 2023, Unlocking the
potential of beta sitosterol: Augmenting the suppression of oral cancer cells
through extrinsic and intrinsic signalling mechanisms. The Saudi Dental
Journal, 35(8), 1007-1013.
[7].
Dinga E., Mthiyane, D. M.
N., Marume, U, et al., 2022, Biosynthesis of ZnO nanoparticles using Melia
azedarach seed extract: evaluation of the cytotoxic and antimicrobial
potency. OpenNano, 8,100068.
[8].
Ecevit, K., Barros, A. A.,
Silva, J. M., & Reis, R. L, 2022, Preventing microbial infections with
natural phenolic compounds. Future Pharmacology, 2(4),
460-498.
[9].
Terefe, E. M., 2022, In vitro and in silico pharmacologic evaluation of
the antiretroviral activity of croton species. Diss. University of Nairobi.
[10]. Alam, M., Bano, N., Ahmad, T., et
al., 2022, Synergistic Role of Plant Extracts and Essential Oils against
Multidrug Resistance and Gram-Negative Bacterial Strains Producing
Extended-Spectrum β-Lactamases. Antibiotics. 11(7), 855.https://doi.org/10.3390/antibiotics11070855.
[11]. Sruthi, M. A., Mani, G.,
Ramakrishnan, M., & Selvaraj, J., 2023, Dental caries as a source of
Helicobacter pylori infection in children: An RT‐PCR study. International
Journal of Paediatric Dentistry, 33(1), 82-88.
[12].
Hochma, E., Yarmolinsky,
L., Khalfin, B., et al. 2021, Antimicrobial effect of phytochemicals from
edible plants. Processes, 9(11),
2089.
[13]. Pauli, A.,
Amicbase., 2006, Essential Oils Supplementary Information. Review Science,
13.
[14].
Singh, R., & Sankar,
C., 2012, Screening of the Cassia fistula flowers extract for the Anti-acne
activity. Res. J. Recent Sci. 2012, 1(11): 53-55.
[15].
Jayaraman, S.,
Natarajan, S. R., Veeraraghavan, V. P., & Jasmine, S., 2023, Unveiling the
anti-cancer mechanisms of calotropin: Insights into cell growth inhibition,
cell cycle arrest, and metabolic regulation in human oral squamous carcinoma
cells (HSC-3). Journal of Oral Biology and Craniofacial Research, 13(6),
704-713.
[16]. Awal, M. A.,
Ahsan, S. M., Haque, E., et al., 2010, In vitro antibacterial activity of leaf
and root extract of Cassia Fistula. Dinajpur Medical College Journal,
3(1),10-13.
[17]. Sharma, A.,
Chandraker, S., Patel, V. K., & Ramteke, P., Antibacterial activity of
medicinal plants against pathogens causing complicated Urinary Tract
Infections. Indian J Pharm Sci. 2009, 71(2): 136-139.https://doi.org/10.4103/0250-474x.54279.
[18].
Webber, D. M., Wallace,
M. A., Burnham, C. D., 2022, Stop Waiting for Tomorrow: Disk Diffusion
Performed on Early Growth Is an Accurate Method for Antimicrobial
Susceptibility Testing with Reduced Turnaround Time. Journal of Clinical
Microbiology, 2022, 60(5): e0300720. doi: 10.1128/JCM.03007-20.
[19]. Peterson, L. R., & Shanholtzer,
C. J., 1992, Tests for bactericidal effects of antimicrobial agents: technical
performance and clinical relevance. Clinical Microbiology Reviews, 5(4), 420-432.https://doi.org/10.1128/cmr.5.4.420
[20].
Spring, K. R., &
Davidson, M. W., Introduction to fluorescence microscopy. Nikon MicroscopyU,
09- 28.
[21]. Michele, D. E., Barresi, R.,
Kanagawa, M., et al., 2002, Post-translational disruption of
dystroglycan–ligand interactions in congenital muscular dystrophies. Nature,
418(6896), 417-421.https://doi.org/10.1038/nature00837.
[22].
Ahmad, F., Jabeen, K.,
Iqbal, S., Umar, A., Ameen, F., Gancarz, M., & Eldin Darwish, D.B.,
Influence of silicon nanoparticles on Avena sativa L. to alleviate the biotic
stress of Rhizoctonia solani. Scientific Reports, 3(1), 15191. doi:
10.1038/s41598-023-41699-w.
[23].
Ahmed, O. M., Saleh, A. S.,
Ahmed, E. A., Ghoneim, M. M., Ebrahim, H. A., Abdelgawad, M. A., Abdel-Gabbar,
M., Efficiency of Bone Marrow-Derived Mesenchymal Stem Cells and Hesperetin in
the Treatment of Streptozotocin-Induced Type 1 Diabetes in Wistar Rats. 16(6), 859. doi: 10.3390/ph16060859.
[24].
Krishnan, R. P.,
Pandiar, D., Ramani, P., & Jayaraman, S., 2025, Molecular profiling of oral
epithelial dysplasia and oral squamous cell carcinoma using next generation
sequencing. Journal of Stomatology, Oral and Maxillofacial Surgery, 126(4),
102120.
[25]. Mahesh, B., & Satish, S., 2008, Antimicrobial activity of
someimportant medicinal plant aga inst plant and humanpathogens. World
Journal of Agricultural Sciences, 4, 839-843.
[26]. Babu, P., Dinesh., & Subhasree, R. S., 2009, Antimicrobial activities
of Lawsonia inermis-a review. Academic Journal of Plant Sciences, 2(4),
231-232.
[27]. Sher, A., 2009, Antimicrobial activity of natural products from medicinal
plants. Gomal Journal of Medical Sciences.7(1), 72-78.
[28]. Pazhani, J., Chanthu, K., Jayaraman, S., & Varun, B. R., 2023,
Evaluation of salivary MMP-9 in oral squamous cell carcinoma and oral
leukoplakia using ELISA. Journal of Oral and Maxillofacial Pathology, 27(4),
649-654.
[29]. Khatoon, L., Baliraine, F. N., Bonizzoni, M, et al., 2009, Prevalence of
antimalarial drug resistance mutations in Plasmodium vivax and P. falciparum
from a malaria-endemic area of Pakistan. The American Journal of Tropical
Medicine and Hygiene, 81 (3),525.
[30]. El-Jakee, J. K., Nagwa, S., Atta, A., et al., 2011, Antimicrobial
resistance in clinical isolates of Staphylococcus aureus from bovine and human
sources in Egypt." Glob. Vet. 7, 581-586.
[31]. Patel, P. G., Raval, P. N., et al., 2012, Bacteriological profile and
antibiogram of gram-negative organisms isolated from medical and neurology
intensive care unit with special reference to multi-drug resistant organisms. National
journal of Medical Research, 2 (3), 335-338.
[32]. Fathima, J. S., Jayaraman, S., Sekar, R., & Syed, N. H., 2024, The
role of MicroRNAs in the diagnosis and treatment of oral premalignant
disorders. Odontology, 1-10. Patel, B.V.,
[33]. Akiyama, H., Fujii, K., Yamasaki, O., et al., 2001, Antibacterial action
of several tannins against Staphylococcus aureus. Journal of Antimicrobial
Chemotherapy, 48(4), 487-491.
[34]. Ceylan, E., & Daniel, Y. C.,2004, Fung Antimicrobial activity of
spices 1. Journal of Rapid Methods & Automation in Microbiology, 12
(1), 1-55. https://doi.org/10.1111/j.1745-4581.2004.tb00046.x.
[35]. Fernandez-Lopez, J., Zhi, N., Aleson-Carbonell, L., et al., 2005,
Antioxidant and antibacterial activities of natural extracts: application in
beef meatballs." Meat Science, 69, (3), 371-380. https://doi.org/10.1016/j.meatsci.2004.08.004.
[36]. Karsha, P. V., & Lakshmi, O. B., 2010, Antibacterial activity of black
pepper (Piper nigrum Linn.) with special reference to its mode of action on
bacteria. 2010.
[37]. Yasothkumar, D., Ramani, P., Jayaraman, S., Ramalingam, K., &
Tilakaratne, W. M., 2024, Expression Profile of Circulating Exosomal microRNAs
in Leukoplakia, Oral Submucous Fibrosis, and Combined Lesions of Leukoplakia
and Oral Submucous Fibrosis. Head and Neck Pathology, 18(1),
28.
[38]. Li, X. Z., Plésiat, P., & Nikaido, H., 2015, The challenge of
efflux-mediated antibiotic resistance in Gram-negative bacteria." Clinical
Microbiology Review, 28, (2), 337-418. https://doi.org/10.1128/CMR.00117-14.
[39]. Mehta, R., & Champney, W. S., 2003, Neomycin and paromomycin inhibit
30S ribosomalsubunit assembly in Staphylococcus aureus. Current Microbiology,
47, 237-243. DOI: 10.1007/s00284-002-3945-9.
[40]. Böddeker, N., Bahador, G., Gibbs, C., et al., 2002, Characterization of a
novel antibacterial agentthat inhibits bacterial translation. Cambridge
Journal, 8, 1120-1128. 10.1017/s1355838202024020.
[41]. Sagar, S., Ramani, P., Moses, S., Gheena, S., & Selvaraj, J., 2024, Correlation of salivary cytokine IL-17A and 1, 25 dihydroxycholecalciferol in patients undergoing orthodontic treatment. Odontology, 1-10.

