Development and Characterization of a Magnesium Membrane Loaded with Hyaluronic Acid, Tricalcium Phosphate, and Quercetin for Bone Healing Applications
Abstract:
This study aims to develop and
characterize a hyaluronic acid/Tricalcium Phosphate (TCP)/quercetin-doped
magnesium membrane for Guided Bone Regeneration (GBR), targeting applications
in periodontal and other biomedical fields. The goal is to create a biocompatible,
hydrophilic membrane with enhanced properties suitable for promoting bone
regeneration. A polymeric solution containing TCP, PVA, hyaluronic acid, and
quercetin-doped magnesium nanoparticles was electrospun to create nanofibrous
membranes. These membranes were analyzed using FTIR for chemical interactions,
XRD for nanoparticle distribution, SEM for morphology, and water contact angle
measurements for hydrophilicity. Cell viability was assessed with an MTT assay
using Dental Pulp Stem Cells, and bone formation potential was evaluated using
MG63 and osteoclast cells with Alizarin Red staining. The fabricated membranes
demonstrated significant hydrophilicity, which is critical for GBR
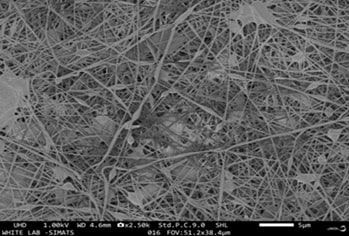
applications. SEM analysis revealed a nanofibrous structure with appropriate
pore size, facilitating cell attachment and growth. The FTIR confirmed the
expected chemical bonding, while XRD verified the incorporation of
magnesium-doped nanoparticles. MTT assays showed high cell viability,
indicating good biocompatibility. Furthermore, the bone formation assay
confirmed the membrane’s potential to support osteogenesis. These
findings suggest that the hyaluronic acid/TCP/quercetin-doped magnesium
membranes developed in this study exhibit favorable properties for use in
guided bone regeneration, offering promising potential for addressing the
limitations of current periodontal treatments and improving patient outcomes.
References:
[1].
Nazir
MA., 2017, Prevalence of periodontal disease, its association with systemic
diseases and prevention. Int J Health Sci (Qassim). Apr-Jun;11(2):72-80.
PMID: 28539867; PMCID: PMC5426403.
[2].
Gasner
NS, Schure RS. Periodontal disease. InStatPearls [Internet] 2023 Apr 10. StatPearls
Publishing.
[3].
Amato
M, Santonocito S, Polizzi A, Tartaglia GM, Ronsivalle V, Viglianisi G,
Grippaudo C, 2023, Isola G. Local Delivery and Controlled Release Drugs
Systems: A New Approach for the Clinical Treatment of Periodontitis Therapy. Pharmaceutics.
Apr 21;15(4):1312. Doi: 10.3390/pharmaceutics15041312. PMID: 37111796; PMCID:
PMC10143241.
[4].
Ren
Y, Fan L, Alkildani S, Liu L, Emmert S, Najman S, Rimashevskiy D, Schnettler R,
Jung O, Xiong X, Barbeck M., 2022, Barrier Membranes for Guided Bone
Regeneration (GBR): A Focus on Recent Advances in Collagen Membranes. Int J
Mol Sci. Nov 29;23(23):14987. Doi: 10.3390/ijms232314987. PMID: 36499315;
PMCID: PMC9735671.
[5]. Dave PH, Vishnupriya V, Gayathri R., 2016, Herbal remedies for anxiety
and depression-A review. J Adv Pharm Technol Res 9:1253
[6]. Balaji V, Priya VV, Gayathri R., 2017, Awareness of risk factors for
obesity among College students in Tamil Nadu: A Questionnaire based study. J
Adv Pharm Technol Res 10:1367
[7].
Witika
BA, Makoni PA, Matafwali SK, Chabalenge B, Mwila C, Kalungia AC, Nkanga CI,
Bapolisi AM, Walker RB., 2020, Biocompatibility of Biomaterials for
Nanoencapsulation: Current Approaches. Nanomaterials (Basel). Aug
22;10(9):1649. Doi: 10.3390/nano10091649. PMID: 32842562; PMCID: PMC7557593.
[8].
Prakoso
AT, Basri H, Adanta D, Yani I, Ammarullah MI, Akbar I, Ghazali FA, Syahrom A,
Kamarul T., 2023, The Effect of Tortuosity on Permeability of Porous Scaffold. Biomedicines.
Feb 1;11(2):427. Doi: 10.3390/biomedicines11020427. PMID: 36830961; PMCID:
PMC9953537.
[9]. Gayathri R, Anuradha V Phytochemical screening and total phenolic
content of aqueous and acetone extracts of seed, butter, mace of nutmeg
(Myristica fragrans Houtt). Int. J. Pharm. Sci. Rev. Res.
[10]. Jerusha SP, Gayathri R, Vishnupriya V., 2016, Preliminary
phytochemical analysis and cytotoxicity potential of Bacopa monnieri on oral
cancer cell lines. Int J Pharm Sci Rev Res 39:4–8
[11]. Tirupathi S, Afnan L., 2024, Dental Pulp Derived Stem Cells for Facial
Nerve Regeneration and Functional Repair: A Systematic Review of Animal
Studies. Current Oral Health Reports 11:198–214.
[12].
Humaira,
Raza Bukhari SA, Shakir HA, Khan M, Saeed S, Ahmad I, Muzammil K, Franco M,
Irfan M, Li K. Hyaluronic acid-based nanofibers: Electrospun synthesis and
their medical applications; recent developments and future perspective. Front
Chem. 2022 Dec 23;10:1092123. Doi: 10.3389/fchem.2022.1092123. PMID:
36618861; PMCID: PMC9816904.
[13].
Sanz-Horta
R, Matesanz A, Gallardo A, Reinecke H, Jorcano JL, Acedo P, Velasco D, Elvira
C., 2023, Technological advances in fibrin for tissue engineering. J Tissue
Eng., Aug 14;14:20417314231190288. Doi: 10.1177/20417314231190288. PMID:
37588339; PMCID: PMC10426312.
[14].
Liu
S, Yu JM, Gan YC, Qiu XZ, Gao ZC, Wang H, Chen SX, Xiong Y, Liu GH, Lin SE,
McCarthy A, John JV, Wei DX, Hou HH., 2023, Biomimetic natural biomaterials for
tissue engineering and regenerative medicine: new biosynthesis methods, recent
advances, and emerging applications. Mil Med Res. Mar 28;10(1):16. Doi:
10.1186/s40779-023-00448-w. PMID: 36978167; PMCID: PMC10047482.
[15].
Zhang
Y, Zhang C, Li Y, Zhou L, Dan N, Min J, Chen Y, Wang Y., 2023, Evolution of
biomimetic ECM scaffolds from decellularized tissue matrix for tissue
engineering: A comprehensive review. Int J Biol Macromol. Aug 15;246:125672. Doi:
10.1016/j.ijbiomac.2023.125672. Epub 2023 Jul 3. PMID: 37406920.
[16].
Zhang
X, Reagan MR, Kaplan DL., 2009, Electrospun silk biomaterial scaffolds for
regenerative medicine. Adv Drug Deliv Rev. Oct 5;61(12):988-1006. Doi:
10.1016/j.addr.2009.07.005. Epub 2009 Jul 28. PMID: 19643154; PMCID:
PMC2774469.
[17]. Kumar JK, Surendranath P, Eswaramoorthy R., 2023, Regeneration of
immature incisor using platelet rich fibrin: report of a novel clinical
application. BMC Oral Health 23:69
[18]. Kishen A, Cecil A, Chitra S., 2023, Fabrication of hydroxyapatite
reinforced polymeric hydrogel membrane for regeneration. Saudi Dent J
35:678–683
[19]. Ramamurthy J, Bajpai D., 2024, Role of alginate-based scaffolds for
periodontal regeneration of intrabony defects: A systematic review. World J
Dent 15:181–187
[20]. Renu, K., 2024. A molecular viewpoint of the
intricate relationships among HNSCC, HPV infections, and the oral microbiota
dysbiosis. Journal of Stomatology, Oral and Maxillofacial Surgery,
p.102134.
[21].
Wang
Z, Wang Y, Yan J, Zhang K, Lin F, Xiang L, Deng L, Guan Z, Cui W, Zhang H.,
2021, Pharmaceutical electrospinning and 3D printing scaffold design for bone regeneration.
Adv Drug Deliv Rev. Jul; 174:504-534. Doi: 10.1016/j.addr.2021.05.007. Epub
2021 May 13. PMID: 33991588.
[22].
Şeker
Ş, Elçin AE, Elçin YM., 2023, Advances in Regenerative Medicine and
Biomaterials. Methods Mol Biol.; 2575:127-152. Doi:
10.1007/978-1-0716-2716-7_7. PMID: 36301474.
[23].
Kaarthikeyan,
G., Jayakumar, N.D. and Sivakumar, D., 2019. Comparative Evaluation of Bone
Formation between PRF and Blood Clot Alone as the Sole Sinus-Filling Material
in Maxillary Sinus Augmentation with the Implant as a Tent Pole: A Randomized
Split-Mouth Study. Journal of long-term effects of medical implants, 29(2).
[24].
Kavarthapu,
A. and Malaiappan, S., 2019. Comparative evaluation of demineralized bone
matrix and type II collagen membrane versus eggshell powder as a graft material
and membrane in rat model. Indian Journal of Dental Research, 30(6),
pp.877-880.
[25]. Manchery, N., John, J., Nagappan, N., Subbiah, G.K. and Premnath, P., 2019. Remineralization potential of dentifrice containing nanohydroxyapatite on artificial carious lesions of enamel: A comparative: in vitro: study. Dental research journal, 16(5), pp.310-317.

