Evaluation of Systemic Inflammation in Lichen Planus Using Neutrophil CD64
Abstract:
Lichen Planus
(LP) is a chronic inflammatory condition caused by T-cell-mediated immune
responses, primarily affecting the skin and oral mucosa. The inflammatory
marker CD64, which is expressed on neutrophils in response to inflammation, has
demonstrated promise as a biomarker in several inflammatory disorders; however,
its function in LP and its applicability for diagnosis and prognosis remain
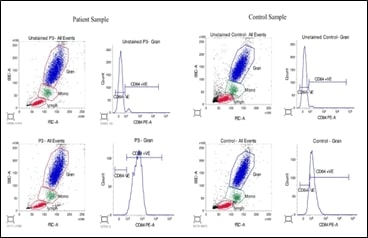
unknown. This study aims to evaluate systemic inflammation of LP patients using
neutrophil CD64 as a potential biomarker. A total of five patients with LP
diagnoses and five healthy controls were included in this study. nCD64
expression was measured by flow cytometric analysis from the peripheral blood
samples of patients and healthy controls. The mean fluorescence intensity of
nCD64 was noted and the data of patients and healthy controls were compared. A
robust systemic inflammatory response was seen in LP patients, as evidenced by
a substantially higher average nCD64 mean fluorescence intensity of 208.4 in
comparison to 45.6 in healthy controls (p=0.05). Patients with LP exhibited a
range of clinical features, including gingival desquamation, erosive lesions,
and white striae. The clinical severity of LP lesions was correlated with the
nCD64 mean fluorescence intensity whereas the severity of the disease was not
correlated with the existing marker, erythrocyte sedimentation rate values.
Thus nCD64 may be a useful biomarker for identifying systemic inflammation in patients
with Lichen Planus and this may lead to better diagnosis and treatment in such
patients. A large cohort study is warranted to confirm these preliminary
findings.
References:
[1]. Behera,
A., Krishnan, R.P. and Pandiar, D., 2023. Prevalence of Civatte Bodies in Oral
Lichen Planus and its Association in Cutaneous Lesions. Annals of
Dental Specialty, 11(4-2023), pp.16-19.
[2]. Soundarajan,
S. and Rajasekar, A., 2023. Antibacterial and anti-inflammatory effects of a
novel herb-mediated nanocomposite mouthwash in plaque-induced gingivitis: a
randomized controlled trial. Dental and Medical Problems, 60(3),
pp.445-451.
[3]. Ramamurthy,
J., 2023. Prevalence of Oral Mucosal Lesions in Patients with Type II Diabetes
Mellitus: A Retrospective Analysis. World Journal of Dentistry, 14(8),
pp.683-687.
[4]. Pandiar,
D., Krishnan, R.P., Behera, A. and Ramani, P., 2023. Intravascular Papillary
Endothelial Hyperplasia of Buccal Mucosa Masquerading as Mucocele-A Case
Report. Indian Journal of Dental Research, 34(4),
pp.445-447.
[5]. Sugerman, P.B., Savage, N.W., Walsh, L.J.,
Zhao, Z.Z., Zhou, X.J., Khan, A., Seymour, G.J., Bigby, M., 2002, The
pathogenesis of oral lichen planus. Crit Rev Oral Biol Med, 13(4), 350-65.
[6]. Vičić, M., Hlača, N., Kaštelan, M., Brajac, I.,
Sotošek, V., Prpić Massari, L., 2023, Comprehensive Insight into Lichen Planus
Immunopathogenesis. Int J Mol
Sci, 24(3),3038.
[7]. Bhattacharya, P., Budnick, I., Singh, M.,
Thiruppathi, M., Alharshawi, K., Elshabrawy, H., Holterman, M.J., Prabhakar,
B.S., 2015, Dual Role of GM-CSF as a Pro-Inflammatory and a Regulatory
Cytokine: Implications for Immune Therapy. J Interferon Cytokine Res, 35(8), 585-99.
[8]. Sanju, S., Jain, P., Vishnu Priya, V., Varma,
p.k., Mony, U., 2023, Quantitation of
mHLA-DR and nCD64 by Flow Cytometry to Study Dysregulated Host Response: The
Use of QuantiBRITE™ PE Beads and Its Stability, Appl Biochem Biotechnol, 195(9):5747-5752.
[9]. Rajasekaran, K., Renu, K., Sankaran, K.,
Veeraraghavan, V.P., Rengasamy, G., Ronsivalle, V., Cicciù, M. and Minervini,
G., Determination of red blood cell parameters for signs of iron deficiency
anemia in patients with oral diseases. Minerva dental and oral science. DOI: 10.23736/S2724-6329.24.04907-6.
[10].
Sundaravadivelu,
I., Renu, K., Kavitha, S., Priya, V.V., Gayathri, R., Ronsivalle, V., Cicciù,
M. and Minervini, G., 2024. Elucidating hematological profile and electrolyte
balance in oral cancer patients. Minerva Dental and Oral Science.
doi: 10.23736/S2724-6329.24.04902-7.
[11].
Wang, X.,
Li, Z.Y., Zeng, L., Zhang, A.Q., Pan, W., Gu, W., Jiang, J.X., 2015, Neutrophil
CD64 expression as a diagnostic marker for sepsis in adult patients: A meta-analysis.
Crit Care, 19(1), 245.
[12].
Deng, X.,
Wang, Y., Jiang, L., Li, J., Chen, Q., 2023, Updates on immunological
mechanistic insights and targeting of the oral lichen planus microenvironment. Front Immunol, 13, 1023213.
[13].
Renu, K., Gopalakrishnan, A.V. and
Madhyastha, H., 2024. Is periodontitis triggering an inflammatory response in
the liver, and does this reaction entail oxidative stress?. Odontology,
pp.1-14. doi: 10.1007/s10266-024-01032-x.
[14].
Rajendran,
P., Renu, K., Abdallah, B.M., Ali, E.M., Veeraraghavan, V.P., Sivalingam, K.,
Rustagi, Y., Abdelsalam, S.A., Ibrahim, R.I.H. and Al-Ramadan, S.Y., 2024.
Nimbolide: promising agent for prevention and treatment of chronic diseases (recent update). Food & Nutrition Research, 68. DOI:10.29219/fnr.v68.9650.
[15].
Rajendran,
P., Renu, K., Ali, E.M., Genena, M.A.M., Veeraraghavan, V., Sekar, R., Sekar,
A.K., Tejavat, S., Barik, P. and Abdallah, B.M., 2024. Promising and
challenging phytochemicals targeting LC3 mediated autophagy signaling in cancer
therapy. Immunity, Inflammation and Disease, 12(10),
p.e70041. doi: 10.1002/iid3.70041.
[16].
Chandrasekar,
M., Divya, B., Gunasekaran, N., Vasanthi, V., Kumar, H.N., Rajkumar, K., 2023,
CD44 Expression in Oral Lichen Planus and Related Lesions-An
Immunohistochemical Study. Indian
Dermatol Online J,
14(5),624-629.
[17].
Pham, H.M.,
Nguyen, D.L.M., Duong, M.C., Tran, L.T., Pham, T.T.N., 2023, Diagnostic Value
of Neutrophil CD64 in Sepsis Patients in the Intensive Care Unit: A
Cross-Sectional Study. Diagnostics
(Basel), 13(8),1427.
[18].
Hassan, U.,
Ghonge, T., Reddy, Jr. B., Patel, M., Rappleye, M., Taneja, I., Tanna, A.,
Healey, R., Manusry, N., Price, Z., Jensen, T., 2017, A point-of-care
microfluidic biochip for quantification of CD64 expression from whole blood for
sepsis stratification. Nature Communications, 8(1),15949.
[19]. Ataş, H., Cemil, B.Ç., Kurmuş, G.I., Gönül, M.,
2016, Assessment of systemic inflammation with neutrophil-lymphocyte ratio in
lichen planus. Postepy Dermatol
Alergol, 33(3):188-92.
[20]. Lu, L., Jin, X., Zhang, Q., 2019, CD35 and CD64
of Neutrophils Can Differentiate Between Bacterial and Viral Infections in
Children by Simultaneous Quantitative Analysis. Med Sci Monit,
25, 7728-7734.
[21]. Liu, Q., Gao, Y., Yang, T., Zhou, Z., Lin, K.,
Zhang, W., Li, T., Lu, Y., Shao, L., Zhang, W., 2022, nCD64 index as a novel
inflammatory indicator for the early prediction of prognosis in infectious and
non-infectious inflammatory diseases: An observational study of febrile
patients. Front Immunol, 13, 905060.
[22]. Dimoula, A., Pradier, O., Kassengera, Z.,
Dalcomune, D., Turkan, H., Vincent, J.L., 2014, Serial determinations of
neutrophil CD64 expression for the diagnosis and monitoring of sepsis in
critically ill patients. Clinical
infectious diseases, 58(6),
820-9.
[23]. Ghosh, P.S., Singh, H., Azim, A., Agarwal, V.,
Chaturvedi, S., Saran, S., Mishra, P., Gurjar, M., Baronia, A.K., Poddar, B.,
Singh, R.K., Mishra, R., 2018, Correlation of Neutrophil CD64 with Clinical
Profile and Outcome of Sepsis Patients during Intensive Care Unit Stay. Indian J Crit Care Med, 22(8), 569-574.
[24]. Meier-Schiesser, B., Zecha, C., Zierold, S.,
Kolm, I., Röckel, M., Fröhlich, W., Mittag, N., Schmitt, C., Kumbrink, J.,
Hassel, J.C., Berking, C., Nashan, D., French, L.E., Vera-González, J., Dummer,
R., Kerl-French, K., Heinzerling, L., 2024, Checkpoint inhibitor-induced lichen
planus differs from spontaneous lichen planus on the clinical, histological,
and gene expression level. JAAD Int, 15:157-164.
[25]. Rassol, H.J., Zaidan, T.F., 2023,
Immunohistochemical expression of T-cell subsets (CD4 and CD8) in oral lichen
planus. Pan African Medical Journal, 45(1), 147.
[26]. Agnes, S.S., Sanju, Jain, P., Varma, P.K.,
Mony, U., 2021, Non-classical monocytes and its potential in diagnosing sepsis
post cardiac surgery. International Immunopharmacology, 99,108037
[27]. Mony, U., Sanju, S.,
Jain, P., Sugavanan, K., Sebastian, A., Theertha, M., Sidharthan, N., Varma, P.K.,
2019. Detection of dysregulated host response by flow cytometry may pre-empt
early diagnosis of sepsis after cardiac surgery. Blood, 134, 4863.
[28]. Ng, P.C., Li, G., Chui, K.M., Chu, W.C., Li, K., Wong, R.P.,
Chik, K.W., Wong, E., Fok, T.F., 2004, Neutrophil CD64 is a sensitive
diagnostic marker for early-onset neonatal infection. Pediatr Res,
56(5), 796-803.
[29]. Allen, E., Bakke, A.C., Purtzer, M.Z., Deodhar, A., 2002,
Neutrophil CD64 expression: Distinguishing acute inflammatory autoimmune
disease from systemic infections. Annals of the rheumatic diseases,
61(6), 522-5.
[30]. Kaarthikeyan, G., Jayakumar, N.D. and Sivakumar, D., 2019.
Comparative Evaluation of Bone Formation between PRF and Blood Clot Alone as
the Sole Sinus-Filling Material in Maxillary Sinus Augmentation with the
Implant as a Tent Pole: A Randomized Split-Mouth Study. Journal of long-term
effects of medical implants, 29(2).
[31]. Kavarthapu, A. and Malaiappan, S., 2019.
Comparative evaluation of demineralized bone matrix and type II collagen
membrane versus eggshell powder as a graft material and membrane in rat
model. Indian Journal of Dental Research, 30(6),
pp.877-880.
[32]. Manchery, N., John, J., Nagappan, N.,
Subbiah, G.K. and Premnath, P., 2019. Remineralization potential of dentifrice
containing nanohydroxyapatite on artificial carious lesions of enamel: A
comparative: in vitro: study. Dental research journal, 16(5),
pp.310-317.
[33]. Renu, K., 2024. A molecular viewpoint of the intricate relationships among HNSCC, HPV infections, and the oral microbiota dysbiosis. Journal of Stomatology, Oral and Maxillofacial Surgery, p.102134.

