Exploring Galium Aparine as a Promising Natural Therapy for Oral Squamous Cell Carcinoma
Abstract:
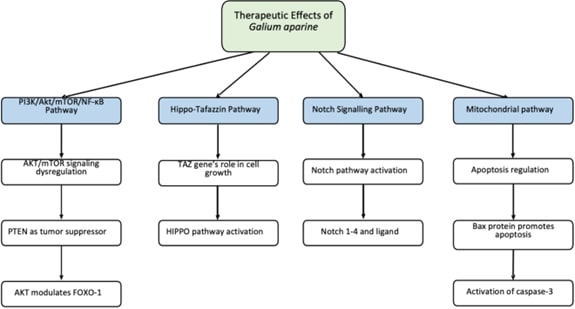
Oral Squamous Cell Carcinoma (OSCC) is a head and neck cancer that has a detrimental impact on patients' quality of life. Surgery, radiation, and chemotherapy are standard treatment procedures that often have adverse effects and are limited in effectiveness, necessitating the quest for other therapeutic techniques.Galium aparine, a phytochemical, is currently acknowledged as a potentially effective treatment for OSCC. According to the literature, Galium aparine has a wide range of chemical elements, including flavonoids like quercetin and rutin, iridoids like asperuloside and aucubin, and phenolic acids like chlorogenic and caffeic acids. These chemicals have antioxidant, anticancer, and immunomodulatory properties, which make Galium aparine a potential natural treatment for OSCC.Preliminary investigations demonstrate its ability to inhibit cancer cell development in vitro and in vivo by inducing apoptosis and/or regulating immune responses. Furthermore, G.aparine extracts have been employed as hepatoprotective agents in a variety of malignancies, including breast carcinoma and melanoma.As a result of Galium aparineextracts’s proven antioxidant and anti-cancer properties in cancerous tissues elsewhere in the body, we have finally concluded that it might possess similar properties in OSCC. To fully understand its modes of action and possible impact on improving outcomes for patients with oral squamous cell carcinoma, more investigation and clinical trials are needed.This paper provides an overview of Galium aparine's biological activities, composition, and role as a powerful anti-cancer agent, as well as potential future research directions.References:
[1]. Meier, J. K., Schuderer, J. G., Zeman, F.,
Klingelhöffer, C., Hullmann, M., Spanier, G., & Ettl, T., 2019,
Health-related quality of life: a retrospective study on local vs.
microvascular reconstruction in patients with oral cancer. BMC oral health, 19, 1-8.
[2].
Bagan, J.,
Sarrion, G. and Jimenez, Y., 2010, Oral cancer: clinical features. Oral oncology, 46(6), pp.414-417.
[3].
Warnakulasuriya,
S., 2020, Oral potentially malignant disorders: A comprehensive review on
clinical aspects and management. Oral
Oncology, 102,
p.104550.
[4].
Tarakji,
B., 2022, Dentists’ perception of oral potentially malignant disorders. International Dental Journal, 72(3), pp.414-419.
[5]. Kerr, A.R. and Lodi, G., 2021, Management of
oral potentially malignant disorders. Oral Diseases, 27(8),
pp.2008-2025.
[6]. Selvaraj FM, Pillai VR, Joseph AP, Ramani P, Pazhani J, Mony V.
Assessment of Tumor Budding in Different Grades of Oral Squamous Cell
Carcinoma. Journal of Orofacial Sciences. 2023 Jul 1;15(2):160-6.
[7].
Tuorkey,
M.J., 2015, Cancer therapy with phytochemicals: present and future
perspectives. Biomedical and
Environmental Sciences, 28(11),
pp.808-819.
[8].
Orhan, N.,
Orhan, D.D., Aslan, M., Şüküroğlu, M. and Orhan, I.E., 2012, UPLC–TOF-MS
analysis of Galium spurium towards its neuroprotective and anticonvulsant
activities. Journal of
ethnopharmacology, 141(1),
pp.220-227.
[9].
Bokhari,
J., Khan, M.R., Shabbir, M., Rashid, U., Jan, S. and Zai, J.A., 2013,
Evaluation of diverse antioxidant activities of Galium aparine. Spectrochimica Acta Part A: Molecular and
Biomolecular Spectroscopy, 102,
pp.24-29.
[10]. Deliorman, D.İ.D.E.M., Calis, I. and Ergun, F.,
2001, Iridoids from Galium aparine. Pharmaceutical
Biology, 39(3),
pp.234-235.
[11]. Simon, D., 2018, Recent advances in clinical
allergy and immunology. International
archives of allergy and immunology, 177(4), pp.324-333.
[12]. Vorob'ev, A.A., 2002, Principles of
classification and the strategy of immunomodulators used in medicine. Zhurnal Mikrobiologii, Epidemiologii i
Immunobiologii, (4), pp.93-98.
[13]. Vidalain, J.P., Onimus, M. and Michel, C.R.,
1975, Long-term results of sub-astragal and mediotarsal arthrodesis. Revue de chirurgie orthopedique et
reparatrice de l'appareil moteur, 61, pp.301-306.
[14]. Sun, H. X., Xie, Y. and Ye, Y. P., 2009,
Advances in saponin-based adjuvants. Vaccine, 27(12),
pp.1787-1796.
[15]. Mocan, A., Crișan, G., Vlase, L., Crișan, O.,
Vodnar, D.C., Raita, O., Gheldiu, A.M., Toiu, A., Oprean, R. and Tilea, I.,
2014, Comparative studies on polyphenolic composition, antioxidant and
antimicrobial activities of Schisandra chinensis leaves and fruits. Molecules, 19(9), pp.15162-15179.
[16]. Taylor, K., 1999, Galium aparine L. Journal of Ecology, 87(4), pp.713-730.
[17]. Mitova, M.I., Anchev, M.E., Handjieva, N.V. and
Popov, S.S., 2002, Iridoid patterns in Galium L. and some phylogenetic
considerations. Zeitschrift für
Naturforschung C, 57(3-4),
pp.226-234.
[18]. Ilina, T., Kashpur, N., Granica, S., Bazylko,
A., Shinkovenko, I., Kovalyova, A., Goryacha, O. and Koshovyi, O., 2019,
Phytochemical profiles and in vitro immunomodulatory activity of ethanolic
extracts from Galium aparine L. Plants, 8(12), p.541.
[19]. Al-Snafi, A.E., 2022, Constituents, nutritional
and pharmacological importance of Prunus persica-A review. World Journal of Advanced Pharmaceutical and
Medical Research, 3(1),
pp.019-029.
[20]. Kanso, M.A., Hijazi, M.A., El-Lakany, A. and
Aboul-Ela, M., 2024, Review on phytochemical constituents and pharmacological
activities of genus Galium. Journal
of Applied Pharmaceutical Science.
[21]. Kuhtinskaja, M., Bragina, O., Kulp, M. and
Vaher, M., 2020, Anticancer effect of the iridoid glycoside fraction from
Dipsacus fullonum L. leaves. Natural
Product Communications, 15(9),
p.1934578X20951417.
[22]. Saar-Reismaa, P., Koel, M., Tarto, R. and
Vaher, M., 2022, Extraction of bioactive compounds from Dipsacus fullonumleave
using deep eutectic solvents. Journal
of Chromatography A, 1677,
p.463330.
[23]. Vorob'ev, A.A., 2002, Principles of
classification and the strategy of immunomodulators used in medicine. Zhurnal Mikrobiologii, Epidemiologii i
Immunobiologii, (4), pp.93-98.
[24]. Dai, J. and Mumper, R.J., 2010, Plant
phenolics: extraction, analysis and their antioxidant and anticancer
properties. Molecules, 15(10), pp.7313-7352.
[25]. Ilina, T., Skowrońska, W., Kashpur, N.,
Granica, S., Bazylko, A., Kovalyova, A., Goryacha, O. and Koshovyi, O., 2020,
Immunomodulatory activity and phytochemical profile of infusions from Cleavers
herb. Molecules, 25(16), p.3721.
[26]. Bradic, J., Petkovic, A. and Tomovic, M., 2021,
Phytochemical and Pharmacological properties of some species of the
genus. Experimental and Applied
Biomedical Research (EABR), 22(3),
pp.187-193.
[27]. Arts, I.C. and Hollman, P.C., 2005, Polyphenols
and disease risk in epidemiologic studies. The American journal of clinical nutrition, 81(1), pp.317S-325S.
[28]. Manach, C., Scalbert, A., Morand, C., Rémésy,
C. and Jiménez, L., 2004, Polyphenols: food sources and bioavailability. The American journal of clinical nutrition, 79(5), pp.727-747.
[29]. Wang, C., Gong, X., Bo, A., Zhang, L., Zhang,
M., Zang, E., Zhang, C. and Li, M., 2020, Iridoids: research advances in their
phytochemistry, biological activities, and pharmacokinetics. Molecules, 25(2), p.287.
[30]. Liu, S., Khan, A.R., Yang, X., Dong, B., Ji, J.
and Zhai, G., 2021, The reversal of chemotherapy-induced multidrug resistance
by nanomedicine for cancer therapy. Journal
of Controlled Release, 335,
pp.1-20.
[31]. Naeem, A., Hu, P., Yang, M., Zhang, J., Liu,
Y., Zhu, W. and Zheng, Q., 2022, Natural products as anticancer agents: current
status and future perspectives. Molecules, 27(23), p.8367.
[32]. Harsha, C., Banik, K., Ang, H.L., Girisa, S.,
Vikkurthi, R., Parama, D., Rana, V., Shabnam, B., Khatoon, E., Kumar, A.P. and
Kunnumakkara, A.B., 2020, Targeting AKT/mTOR in oral cancer: mechanisms and
advances in clinical trials. International
journal of molecular sciences, 21(9), p.3285.
[33]. Christianto, S., Li, K.Y., Huang, T.H. and Su,
Y.X., 2022, The Prognostic Value of Human Papilloma Virus Infection in Oral
Cavity Squamous Cell Carcinoma: A Meta‐Analysis. The Laryngoscope, 132(9),
pp.1760-1770.
[34]. Cavalcante, G.C., Schaan, A.P., Cabral, G.F.,
Santana-da-Silva, M.N., Pinto, P., Vidal, A.F. and Ribeiro-dos-Santos, Â.,
2019, A cell’s fate: an overview of the molecular biology and genetics of
apoptosis. International journal
of molecular sciences, 20(17),
p.4133.
[35]. Schmidt, M., Polednik, C., Roller, J. and
Hagen, R., 2014, Galium verum aqueous extract strongly inhibits the motility of
head and neck cancer cell lines and protects mucosal keratinocytes against
toxic DNA damage. Oncology
Reports, 32(3),
pp.1296-1302.
[36]. Zhang, J., Zheng, G., Zhou, L., Li, P., Yun,
M., Shi, Q., Wang, T. and Wu, X., 2018, Notch signalling induces
epithelial-mesenchymal transition to promote metastasis in oral squamous cell
carcinoma. International journal
of molecular medicine, 42(4),
pp.2276-2284.
[37]. Zong, W.X., Rabinowitz, J.D. and White, E.,
2016, Mitochondria and cancer. Molecular
cell, 61(5),
pp.667-676.
[38]. Carr, C., Ng, J. and Wigmore, T., 2008, The
side effects of chemotherapeutic agents. Current Anaesthesia & Critical Care, 19(2), pp.70-79.
[39]. Kelland, L., 2007, The resurgence of
platinum-based cancer chemotherapy. Nature
Reviews Cancer, 7(8),
pp.573-584.
[40]. Kayl, A.E. and Meyers, C.A., 2006, Side-effects
of chemotherapy and quality of life in ovarian and breast cancer
patients. Current opinion in
obstetrics and gynaecology, 18(1),
pp.24-28.
[41]. Laanet, P.R., Saar-Reismaa, P., Jõul, P.,
Bragina, O. and Vaher, M., 2023, Phytochemical screening and antioxidant
activity of selected Estonian Galium species. Molecules, 28(6),
p.2867.
[42]. Hamdi, O.H., Saadedin, S.M. and Al_Zaidi, I.H.,
2021, Green biosynthesis of silver nanoparticles using gallium aparine green
part extract and anti-skin cancer activity. Medico-legal Update, 21(2),
pp.908-913.
[43]. Atmaca, H., Bozkurt, E., Cittan, M. and Tepe,
H.D., 2016, Effects of Galium aparine extract on the cell viability, cell cycle
and cell death in breast cancer cell lines. Journal of ethnopharmacology, 186, pp.305-310.
[44]. Sahin, B., Karabulut, S., Filiz, A.K.,
Özkaraca, M., Gezer, A., Akpulat, H.A. and Ataseven, H., 2022, Galium aparine
L. protects against acetaminophen-induced hepatotoxicity in rats. Chemico-Biological Interactions, 366, p.110119.
[45]. Mazzio, E.A. and Soliman, K.F., 2010, In vitro
screening of tumoricidal properties of international medicinal herbs: part
II. Phytotherapy Research, 24(12), pp.1813-1824.
[46]. Corrigan, D., Timoney, R.F. and Donnelly, D.M.,
1978, Iridoids and alkanes in twelve species of Galium and Asperula. Phytochemistry, 17(7), pp.1131-1133.
[47]. Ramasubramanian
A, Arumugam P, Ramani P, Kannan BC, Murugan MS. Identification of Novel
Cytochrome C1 (CYC1) Gene Expression in Oral Squamous Cell Carcinoma- An
Evaluative Study. Ann Maxillofac Surg. 2022 Jul-Dec;12(2):144-150. doi:
10.4103/ams.ams_26_22. Epub 2022 Aug 24. PMID: 36874769; PMCID: PMC9976869.
[48]. Renu, K., 2024. A molecular viewpoint of the
intricate relationships among HNSCC, HPV infections, and the oral microbiota
dysbiosis. Journal of Stomatology, Oral and Maxillofacial Surgery, p.102134.
[49]. Subramanian, A.K. and Balakrishnan, N.,
Evaluation of Biological Response Elicited by Two Novel Tooth Cream
Formulations of Cocos nucifera-Cell Line Studies and MTT Assay on Human
Gingival Fibroblast.
[50]. Kaarthikeyan, G., Jayakumar, N.D. and
Sivakumar, D., 2019. Comparative Evaluation of Bone Formation between PRF and
Blood Clot Alone as the Sole Sinus-Filling Material in Maxillary Sinus
Augmentation with the Implant as a Tent Pole: A Randomized Split-Mouth
Study. Journal of long-term effects of medical implants, 29(2).
[51]. Kavarthapu, A. and Malaiappan, S., 2019.
Comparative evaluation of demineralized bone matrix and type II collagen
membrane versus eggshell powder as a graft material and membrane in rat
model. Indian Journal of Dental Research, 30(6),
pp.877-880.
[52]. Manchery, N., John, J., Nagappan, N.,
Subbiah, G.K. and Premnath, P., 2019. Remineralization potential of dentifrice
containing nanohydroxyapatite on artificial carious lesions of enamel: A
comparative: in vitro: study. Dental research journal, 16(5),
pp.310-317.

