Charting the Monthly Waves: An Observational Study on the Dynamics of Premenstrual Syndrome
Abstract:
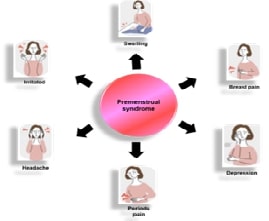
Premenstrual syndrome (PMS) is an assortment of
painful symptoms that occur around the period of menstruation and they are
related to hormonal changes that have been known by physicians for millennia,
potentially leading to difficulties in daily functioning and a poor quality of living.
The Moos Menstrual Distress Questionnaire (MDQ) was used to gather data in this
cross-sectional research with 200 participants in Chennai. ANOVA and T-tests
were used to examine the data using SPSS software. Participants were provided
with PMS reporting diaries to document symptoms for two consecutive menstrual
cycles. The 168 total sample sizes were calculated using the equation of power
analysis. There were no irregular menstrual periods among the girls. The
average age of the participants was 20.3 years and their average menarche age
was 13.5 years. Notably, 124 (73.8%) of individuals reported having considerable
blood flow during their menstrual cycle, with 142 (84.5%) of the individuals
reported having menstrual cramps. There was no discernible correlation found
between the prevalence of PMS and the use concerning junk food, physical
activity, sugar, salt, or citrus fruits. Although menstruation is a natural
physiological process, many individuals experience menstrual abnormalities and
PMS, which require treatment. It is recognized that a significant portion
of people have irregular periods and PMS highlights the need for efficient
treatment approaches, even though menstruation is a normal physiological function.
References:
[1].
Barker-Smith, H., 2020, Navigating the menstrual landscapes: From
the darkness to the light. Psychotherapy and Politics International,
18(2), e1533. https://doi.org/10.1002/ppi.1533.
[2].
Hamidovic, A., Karapetyan, K., Serdarevic, F., Choi, S.H.,
Eisenlohr-Moul, T., & Pinna, G., 2020, Higher circulating cortisol in the
follicular vs. luteal phase of the menstrual cycle: A meta-analysis. Frontiers
in Endocrinology, 11, 311. https://doi.org/10.3389/fendo.2020.00311.
[3].
Tiranini, L., & Nappi, R.E., 2022, Recent advances in
understanding/management of premenstrual dysphoric disorder/premenstrual
syndrome. Faculty Reviews, 11. https://doi.org/10.12703/r/11-9.
[4].
Abbas, K., Usman, G., Ahmed, M., Qazi, R., Asghar, A., Shah, A.M.,
Rizvi, A., Abid, K., Haq, K.U., Tahir, A., & Usama, S.M., 2020, Physical
and psychological symptoms associated with premenstrual syndrome and their
impact on the daily routine of women in a low socioeconomic status locality. Cureus,
12(10).
https://doi.org/10.7759/cureus.1111.
[5].
Akın, Ö., & Erbil, N., 2023, Investigation of coping behaviors
and premenstrual syndrome among university students. Current Psychology,
1-11.
https://doi.org/10.1007/s12144-023-03892-5
[6].
Chan, K., Rubtsova, A.A., & Clark, C.J., 2023, Exploring
diagnosis and treatment of premenstrual dysphoric disorder in the US healthcare
system: A qualitative investigation. BMC Women's Health, 23(1), 1-9. https://doi.org/10.1186/s12905-023-02222-0.
[7].
Batool, S., & Haleem, M., 2022, Unveiling the social studies
panorama: Unveiling the interconnectedness of human phenomena. Social
Sciences Spectrum, 1(1), 21-29.
[8].
Collatuzzo, G., & Boffetta, P., 2022, Application of P4
(predictive, preventive, personalized, participatory) approach to occupational
medicine. La Medicina del Lavoro, 113(1). https://doi.org/10.23749/mdl.v113i1.11939.
[9].
Kamel, D.M., Tantawy, S.A., Alsayed, N., Bekhet, A.H., Elbkery,
N., & Khairy, A., 2021, The relationship between premenstrual syndrome and
the quality of sleep among Egyptian women: An observational study. Archives
of the Balkan Medical Union, 56(2), 172-178.
[10].
Takayama, E., Tanaka, H., Kamimoto, Y.,
Sugiyama, T., Okano, T., Kondo, E., & Ikeda, T., 2020, Relationship between a
high Edinburgh Postnatal Depression Scale score and premenstrual syndrome: A
prospective, observational study. Taiwanese Journal of Obstetrics and
Gynecology, 59(3), 356-360. https://doi.org/10.1016/j.tjog.2020.03.001.
[11].
Hashim, M.S., Obaideen, A.A., Jahrami, H.A., Radwan, H., Hamad,
H.J., Owais, A.A., Alardah, L.G., Qiblawi, S., Al-Yateem, N., & Faris,
M.E.A.I.E., 2019, Premenstrual syndrome is associated with dietary and
lifestyle behaviors among university students: A cross-sectional study from
Sharjah, UAE. Nutrients, 11(8), 1939. https://doi.org/10.3390/nu11081939.
[12].
Helmy, N.A., Kamel, D.M., Gabr, A.A., & Shehata, M.A. Does
dietary habits/food consumption affect the premenstrual syndrome incidence
among a cohort of Egyptian females: An observational study.
[13]. Rezende, A.P.R.,
Alvarenga, F.R., Ramos, M., Franken, D.L., Costa, J.S.D.D., Pattussi, M.P.,
& Paniz, V.M.V., 2022, Prevalence of premenstrual syndrome and associated
factors among academics of a university in midwest Brazil. Revista Brasileira de
Ginecologia e Obstetrícia, 44, 133-141. https://doi.org/10.1055/s-0041-1739560.
[14].
Heydari, N., Abootalebi, M., Tayebi, N.,
Hassanzadeh, F., Kasraeian, M., Emamghoreishi, M., & Akbarzadeh, M., 2019, The effect of
aromatherapy on mental, physical symptoms, and social functions of females with
premenstrual syndrome: A randomized clinical trial. Journal of Family
Medicine and Primary Care, 8(9), 2990. https://doi.org/10.4103/jfmpc.jfmpc_472_19.
[15].
Azhary, J.M.K., Leng, L.K., Razali, N., Sulaiman, S., Wahab,
A.V.A., Adlan, A.S.A., & Hassan, J., 2022, The prevalence of menstrual
disorders and premenstrual syndrome among adolescent girls living in North
Borneo, Malaysia: A questionnaire-based study. BMC Women's Health,
22(1), 1-9.
https://doi.org/10.1186/s12905-022-01714-7.
[16].
Kim, Y.J., & Park, Y.J., 2020, Menstrual cycle characteristics
and premenstrual syndrome prevalence based on the daily record of severity of
problems in Korean young adult women. Journal of Korean Academy of Nursing,
50(1), 147-157. https://doi.org/10.4040/jkan.2020.50.1.147.
[17].
Shrestha, D.B., Shrestha, S., Dangol, D., Aryal, B.B., Shrestha,
S., Sapkota, B., & Rai, S., 2019, Premenstrual syndrome in students of a
teaching hospital. Journal of Nepal Health Research Council, 17(2),
253-257.
https://doi.org/10.33314/jnhrc.v17i2.1996.
[18].
Abbas, K., Usman, G., Ahmed, M., Qazi, R., Asghar, A., Shah, A.M.,
Rizvi, A., Abid, K., Haq, K.U., Tahir, A., & Usama, S.M., 2020, Physical
and psychological symptoms associated with premenstrual syndrome and their
impact on the daily routine of women in a low socioeconomic status locality. Cureus,
12(10).
https://doi.org/10.7759/cureus.11110.
[19].
Thakur, H., Pareek, P., Sayyad, M.G., & Otiv, S., 2022,
Association of premenstrual syndrome with adiposity and nutrient intake among
young Indian women. International Journal of Women's Health, 665-675. https://doi.org/10.2147/IJWH.S344383.
[20].
Huwaida, D.Z., & Dewi, Y.L.R., 2022, Unhealthy diet and stress
are correlated with premenstrual syndrome in adolescent girls in Tangerang. Media
Gizi Indonesia, 17(2). https://doi.org/10.20473/mgi.v17i2.61-67.

