An Update on the Role of Omega-3 Fatty Acids in Metabolic Health and Insulin Resistance: A narrative review
Abstract:
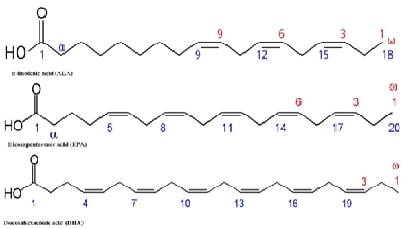
Insulin resistance and metabolic
health are largely regulated by important pathways that omega-3 fatty acids
influence. The molecular pathways by which Omega-3 fatty acids, specifically
Docosahexaenoic Acid (DHA) and Eicosapentaenoic Acid (EPA), work is the main
topic of concern in this narrative overview. Through modifying inflammatory
responses, enhancing lipid metabolism, and impacting insulin signaling
pathways, these fatty acids mainly increase insulin sensitivity. Studies have
demonstrated that EPA and DHA can increase insulin sensitivity by
downregulating the nuclear factor kappa B (NF-κB) pathway, reducing
pro-inflammatory cytokines, and increasing the activation of peroxisome
proliferator-activated receptors (PPARs). Furthermore, Omega-3s mitigate
lipotoxicity and encourage the effective utilization of fatty acids as an
energy source, all of which are critical for preserving insulin sensitivity.
They also lessen ectopic fat accumulation. Additionally, the interaction
between Omega-3s and membrane phospholipids enhances insulin receptor signaling
and activity. Notwithstanding these advantages, further research is necessary
to fully understand the unique impacts of certain Omega-3s, such as
Alpha-Linolenic Acid (ALA), on these pathways as well as how they might
interact with other dietary components and gut flora. We can more effectively
utilize the therapeutic potential of omega-3 fatty acids to enhance metabolic
health and combat insulin resistance by clarifying these pathways.
References:
[1].
Chatterjee,
S., Khunti, K., & Davies, M. J., 2017, Type 2 diabetes. Lancet,
389(10085), 2239–2251, https://doi.org/10.1016/S0140-6736(17)30058-2
[2].
Rajendran,
S., Mishra, S., Madhavanpillai, M., & G, V., 2022, Association of
hemoglobin glycation index with cardiovascular risk factors in non-diabetic
adults: A cross-sectional study. Diabetes & Metabolic Syndrome,
16(9), 102592, https://doi.org/10.1016/j.dsx.2022.102592
[3].
Sinha,
S., Haque, M., Lugova, H., & Kumar, S., 2023, The effect of Omega-3 fatty
acids on insulin resistance. Life, 13(6), 1322, https://doi.org/10.3390/life13061322
[4].
Natto,
Z. S., Yaghmoor, W., Alshaeri, H. K., & Van Dyke, T. E., 2019, Omega-3
fatty acids effects on inflammatory biomarkers and lipid profiles among
diabetic and cardiovascular disease patients: A systematic review and
meta-analysis. Scientific Reports, 9(1), 18867, https://doi.org/10.1038/s41598-019-54535-x
[5].
Yaribeygi,
H., Maleki, M., Jamialahmadi, T., Shakhpazyan, N. K., Kesharwani, P., &
Sahebkar, A., 2023, Nanoparticles with SGLT2 inhibitory activity: Possible
benefits and future. Diabetes & Metabolic Syndrome, 17(10), 102869, https://doi.org/10.1016/j.dsx.2023.102869
[6].
Samuel,
V. T., Petersen, K. F., & Shulman, G. I., 2010, Lipid-induced insulin
resistance: Unravelling the mechanism. Lancet, 375(9733), 2267–2277, https://doi.org/10.1016/S0140-6736(10)60408-4
[7].
Winn,
N. C., Pettit-Mee, R., Walsh, L. K., Restaino, R. M., Ready, S. T., Padilla,
J., & Kanaley, J. A., 2019, Metabolic implications of diet and energy
intake during physical inactivity. Medicine and Science in Sports and Exercise,
51(5), 995–1005, https://doi.org/10.1249/MSS.0000000000001892
[8].
Rahman,
M. S., Hossain, K. S., Das, S., Kundu, S., Adegoke, E. O., Rahman, M. A.,
Hannan, M. A., Uddin, M. J., & Pang, M. G., 2021, Role of insulin in health
and disease: An update. International Journal of Molecular Sciences,
22(12), 6403, https://doi.org/10.3390/ijms22126403
[9].
Natesan,
V., & Kim, S. J., 2021, Lipid metabolism, disorders and therapeutic drugs -
Review. Biomolecules & Therapeutics, 29(6), 596–604, https://doi.org/10.4062/biomolther.2021.122
[10].
Hardy,
O. T., Czech, M. P., & Corvera, S., 2012, What causes the insulin
resistance underlying obesity? Current Opinion in Endocrinology, Diabetes, and
Obesity, 19(2), 81–87, https://doi.org/10.1097/MED.0b013e3283514e13
[11].
Rekha,
K., Venkidasamy, B., Samynathan, R., Nagella, P., Rebezov, M., Khayrullin, M.,
Ponomarev, E., Bouyahya, A., Sarkar, T., Shariati, M. A., Thiruvengadam, M.,
& Simal-Gandara, J., 2024, Short-chain fatty acid: An updated review on
signaling, metabolism, and therapeutic effects. Critical Reviews in Food
Science and Nutrition, 64(9), 2461–2489, https://doi.org/10.1080/10408398.2022.2124231
[12].
Cholewski,
M., Tomczykowa, M., & Tomczyk, M., 2018, A comprehensive review of
chemistry, sources and bioavailability of omega-3 fatty acids. Nutrients,
10(11), 1662, https://doi.org/10.3390/nu10111662
[13].
Rodriguez-Leyva,
D., Dupasquier, C. M., McCullough, R., & Pierce, G. N., 2010, The
cardiovascular effects of flaxseed and its omega-3 fatty acid, alpha-linolenic
acid. The Canadian Journal of Cardiology, 26(9), 489–496, https://doi.org/10.1016/s0828-282x(10)70455-4
[14].
Weitz,
D., Weintraub, H., Fisher, E., & Schwartzbard, A. Z., 2010, Fish oil for
the treatment of cardiovascular disease. Cardiology in Review, 18(5), 258–263, https://doi.org/10.1097/CRD.0b013e3181ea0de0
[15].
Bradbury,
J., 2011, Docosahexaenoic acid (DHA): An ancient nutrient for the modern human
brain. Nutrients, 3(5), 529–554, https://doi.org/10.3390/nu3050529
[16].
Calder,
P. C., 2010, Omega-3 fatty acids and inflammatory processes. Nutrients,
2(3), 355–374, https://doi.org/10.3390/nu2030355
[17].
Samanta,
S., Sarkar, T., Chakraborty, R., Rebezov, M., Shariati, M. A., Thiruvengadam,
M., & Rengasamy, K. R. R., 2022, Dark chocolate: An overview of its
biological activity, processing, and fortification approaches. Current
Research in Food Science, 5, 1916–1943, https://doi.org/10.1016/j.crfs.2022.10.017
[18].
Gharraee,
N., Wang, Z., Pflum, A., Medina-Hernandez, D., Herrington, D., Zhu, X., &
Meléndez, G. C., 2022, Eicosapentaenoic acid ameliorates cardiac fibrosis and
tissue inflammation in spontaneously hypertensive rats. Journal of Lipid
Research, 63(11), 100292, https://doi.org/10.1016/j.jlr.2022.100292
[19].
Chen,
C., Yang, Y., Yu, X., Hu, S., & Shao, S., 2017, Association between omega-3
fatty acids consumption and the risk of type 2 diabetes: A meta-analysis of
cohort studies. Journal of Diabetes Investigation, 8(4), 480–488, https://doi.org/10.1111/jdi.12614
[20].
Li,
M., Chi, X., Wang, Y., Setrerrahmane, S., Xie, W., & Xu, H., 2022, Trends
in insulin resistance: Insights into mechanisms and therapeutic strategy. Signal
Transduction and Targeted Therapy, 7(1), 216, https://doi.org/10.1038/s41392-022-01073-0
[21].
Qiu,
Y. Y., Zhang, J., Zeng, F. Y., & Zhu, Y. Z., 2023, Roles of the peroxisome
proliferator-activated receptors (PPARs) in the pathogenesis of nonalcoholic
fatty liver disease (NAFLD). Pharmacological Research, 192, 106786, https://doi.org/10.1016/j.phrs.2023.106786
[22].
Boopathi,
S., Haridevamuthu, B., Mendonca, E., Gandhi, A., Priya, P. S., Alkahtani, S.,
Al-Johani, N. S., Arokiyaraj, S., Guru, A., Arockiaraj, J., & Malafaia, G.,
2023, Combined effects of a high-fat diet and polyethylene microplastic
exposure induce impaired lipid metabolism and locomotor behavior in larvae and
adult zebrafish. The Science of the Total Environment, 902, 165988, https://doi.org/10.1016/j.scitotenv.2023.165988
[23].
Swanson,
D., Block, R., & Mousa, S. A., 2012. Omega-3 fatty acids EPA and DHA:
Health benefits throughout life. Advances in Nutrition (Bethesda, Md.),
3(1), 1–7, https://doi.org/10.3945/an.111.000893
[24].
Calder,
P. C., 2013, Omega-3 polyunsaturated fatty acids and inflammatory processes:
Nutrition or pharmacology? British Journal of Clinical Pharmacology,
75(3), 645–662, https://doi.org/10.1111/j.1365-2125.2012.04374.x
[25].
Fazelian,
S., Moradi, F., Agah, S., Hoseini, A., Heydari, H., Morvaridzadeh, M., Omidi,
A., Pizarro, A. B., Ghafouri, A., & Heshmati, J., 2021, Effect of omega-3
fatty acids supplementation on cardio-metabolic and oxidative stress parameters
in patients with chronic kidney disease: A systematic review and meta-analysis.
BMC Nephrology, 22(1), 160, https://doi.org/10.1186/s12882-021-02351-9
[26].
Calder,
P. C., 2015, Marine omega-3 fatty acids and inflammatory processes: Effects,
mechanisms and clinical relevance. Biochimica et Biophysica Acta,
1851(4), 469–484, https://doi.org/10.1016/j.bbalip.2014.08.010
[27].
Wen,
J., Satyanarayanan, S. K., Li, A., Yan, L., Zhao, Z., Yuan, Q., Su, K. P.,
& Su, H., 2024, Unraveling the impact of omega-3 polyunsaturated fatty
acids on blood-brain barrier (BBB) integrity and glymphatic function. Brain,
Behavior, and Immunity, 115, 335–355, https://doi.org/10.1016/j.bbi.2023.10.018
[28].
Elisia,
I., Yeung, M., Kowalski, S., Wong, J., Rafiei, H., Dyer, R. A., Atkar-Khattra,
S., Lam, S., & Krystal, G., 2022, Omega 3 supplementation reduces
C-reactive protein, prostaglandin E2 and the granulocyte/lymphocyte ratio in
heavy smokers: An open-label randomized crossover trial. Frontiers in
Nutrition, 9, 1051418, https://doi.org/10.3389/fnut.2022.1051418
[29].
Allam-Ndoul,
B., Guénard, F., Barbier, O., & Vohl, M. C., 2017, Effect of different
concentrations of omega-3 fatty acids on stimulated THP-1 macrophages. Genes
& Nutrition, 12, 7, https://doi.org/10.1186/s12263-017-0554-6
[30].
Flock,
M. R., Skulas-Ray, A. C., Harris, W. S., Gaugler, T. L., Fleming, J. A., &
Kris-Etherton, P. M, 2014, Effects of supplemental long-chain omega-3 fatty
acids and erythrocyte membrane fatty acid content on circulating inflammatory
markers in a randomized controlled trial of healthy adults. Prostaglandins,
Leukotrienes, and Essential Fatty Acids, 91(4), 161–168, https://doi.org/10.1016/j.plefa.2014.07.006
[31].
Indian
Council of Medical Research & National Institute of Nutrition, 2024, Dietary
Guidelines for Indians, ICMR-NIN. Available at https://main.icmr.nic.in/sites/default/files/upload_documents/DGI_07th_May_2024_fin.pdf
[32].
Office
of Dietary Supplements. (n.d.). Omega-3 fatty acids - Health professional. National
Institutes of Health, https://ods.od.nih.gov/factsheets/Omega3FattyAcids-HealthProfessional/
[33].
Mason,
R. P., & Sherratt, S. C. R., 2017, Omega-3 fatty acid fish oil dietary
supplements contain saturated fats and oxidized lipids that may interfere with
their intended biological benefits. Biochemical and Biophysical Research
Communications, 483(1), 425–429, https://doi.org/10.1016/j.bbrc.2016.12.127
[34].
Asghari,
K. M., Saleh, P., Salekzamani, Y., Dolatkhah, N., Aghamohammadzadeh, N., &
Hashemian, M., 2024, The effect of curcumin and high-content eicosapentaenoic
acid supplementations in type 2 diabetes mellitus patients: A double-blinded
randomized clinical trial. Nutrition & Diabetes, 14(1), 14, https://doi.org/10.1038/s41387-024-00274-6

