Assessment of Nutritional Status of Pregnant Women Attending Antenatal Care at Public Hospitals in Gambella Region, Ethiopia: Institution-Based Cross-Sectional Study
Abstract:
Nutrition is a fundamental pillar of health,
particularly for pregnant women whose increased nutritional needs make them
vulnerable to deficiencies. This study aims to assess the nutritional status,
dietary diversity score (DDS), and associated risk factors among pregnant women
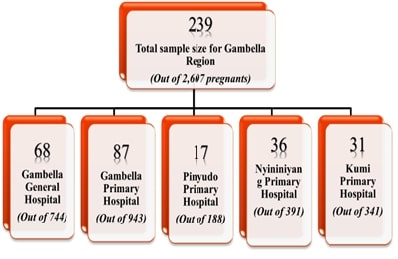
attending antenatal care in Gambella Region, South West Ethiopia. An
institution-based cross-sectional study was conducted from March to April 2023,
involving 237 pregnant women selected through consecutive sampling. Data were
collected using structured questionnaires, 24-hour dietary recall, mid-upper arm circumference (MUAC) measurements, and
haemoglobin testing. Bivariate and multivariate logistic regression analyses
were employed to identify factors associated with undernutrition, dietary
diversity, and anaemia. The prevalence of undernutrition was 37.1%, while 48.9%
of the participants had inadequate dietary diversity. Anaemia prevalence was
found to be 22.8%. Significant determinants of undernutrition included marital
status [adjusted odds ratio = 0.10, 95% CI: 0.01-0.81], STIs during pregnancy
(AOR = 1.97, 95% CI: 1.01-3.85), and family planning use (AOR = 0.49, 95% CI:
0.25-0.94). Inadequate dietary diversity was significantly associated with age
(AOR = 4.24, 95% CI: 1.01-17.84), household income (AOR = 3.00, 95% CI:
1.14-7.88), and family planning use (AOR = 3.62, 95% CI: 1.86-6.94). Housewives
were more likely to be anaemic compared to private employees (AOR = 0.14, 95%
CI: 0.03-0.78). The study highlights a high prevalence of undernutrition and
anemia among pregnant women in the Gambella Region, with significant
associations with socioeconomic and health factors. Integrating nutrition
education with reproductive health services and promoting economic empowerment
are crucial for improving maternal nutrition.
References:
[1].
Madhavi, L. H., Singh, H.
K. G., 2011, Nutritional status of rural pregnant women. People’s Journal of
Scientific Research, 4(2).
[2].
WHO, 2003, Joint WHO/FAO
expert report on diet, nutrition and the prevention of chronic diseases:
Executive summary. Food and Nutrition Bulletin, 24(3), 285-6.
[3].
Alemayehu, M. S., 2014,
Dietary practice and associated factors among pregnant women in Gondar town
north west, Ethiopia, 2014, International Journal of Nutrition and Food
Sciences.;4(6), 707-12.
[4].
Blössner, M., de Onis M.,
2005, Malnutrition: quantifying the health impact at national and local levels.
Geneva: World Health Organization.
[5].
Kiboi, W., Kimiywe, J.,
Chege, P., 2016, Dietary Diversity, Nutrient Intake and Nutritional Status
among Pregnant Women in Laikipia County, Kenya. International Journal of Health
Sciences & Research, 6(4).
[6].
EDHS, 2011, Ethiopian
demographic and health survey 2011.
[7].
Kedir, H., Berhane, Y.,
Worku, Y., 2014, Magnitude and determinants of malnutrition among pregnant
women in eastern Ethiopia: evidence from rural, community-based setting.
Maternal & Child Nutrition, 12(1), 51-63.
[8].
Desalegn, K., Pragya, S.,
Debebe, M., Tefera, B., 2015, Nutritional Status and Associated Factors among
Pregnant Women in Wondo Genet District, Southern Ethiopia. Journal of Food
Science and Engineering, 5(2).
[9].
Rao, K. M., Balakrishna,
N., Arlappa, N., Laxmaiah, A., Brahmam, G., 2010, Diet and Nutritional Status
of Women in India. Journal of Human Ecology, 29(3), 165-70.
[10].
Deghboudj, S., 2011,
Assessment of Nutritional Status of Pregnant Women Attending the City Tebessa
PMI (Algeria). National Journal of Physiology, Pharmacy & Pharmacology,
1(2), 97-105.
[11].
Lelissa, D., 2015,
Prevalence of Anemia Among Women Receiving Antenatal Care at Boditii Health
Center, Southern Ethiopia. Clinical Medicine Research, 4(3), 77-86.
[12].
WHO/UNICEF, 2001, Iron
Deficiency Anaemia Assessment, Prevention, and Control: A guide for programme
managers.
[13].
Nisar, Y. B., Dibley, M.
J., 2016, Iron/folic acid supplementation during pregnancy prevents neonatal
and under-five mortality in Pakistan: propensity score matched sample from two
Pakistan Demographic and Health Surveys, 9(1), 29621.
[14].
McLean, E., Cogswell, M.,
Egli, I., Wojdyla, D., De Benoist, B., 2008, Worldwide prevalence of anaemia,
WHO vitamin and mineral nutrition information system, 1993–2005. Public Health
Nutrition, 12(4), 444.
[15].
EDHS, 2016, Ethiopian
demographic and health survey 2016.
[16].
Getachew, M., Yewhalaw,
D., Tafess, K., Getachew, Y., Zeynudin, A., 2012, Anaemia and associated risk
factors among pregnant women in Gilgel Gibe dam area, Southwest Ethiopia.
Parasites & Vectors, 5(1).
[17].
Abriha, A., Yesuf, M. E.,
Wassie, M. M., 2014, Prevalence and associated factors of anemia among pregnant
women of Mekelle town: a cross sectional study. BMC Research Notes, 7(888).
[18].
Gedefaw, L., Ayele, A.,
Asres, Y., Mossie, A., 2015, Anaemia and associated factors among pregnant
women attending antenatal care clinic in Walayita Sodo town, Southern Ethiopia.
Ethiopian Journal of Health Sciences, 25(2).
[19].
Haileslassie, K.,
Mulugeta, A., Girma, M., 2013, Feeding practices, nutritional status and
associated factors of lactating women in Samre Woreda, South Eastern Zone of
Tigray, Ethiopia. Nutrition Journal, 12(1).
[20].
IYCN, 2011, Guidance for
Formative Research on Maternal Nutrition. Washington DC.
[21].
Opara, J. A., Adebola,
H., Nkasiobi, O. S., 2011, Malnutrition During Pregnancy among Child Bearing
Mothers in Mbaitolu of South-Eastern Nigeria. Advances in Biological Research,
5(2).
[22].
Lee, S. E., Merialdi, M.,
Caulfield, L. E., 2012, Dietary intakes of women during pregnancy in low- and
middle-income countries. Public Health Nutrition, 16(8), 1340-53.
[23].
Khoushabi F., Saraswathi
G., 2010, Association between maternal nutrition status and birth weight of
neonates in selected hospitals in Mysore city, India. Pakistan Journal of
Nutrition, 9(12), 1124-30.
[24].
Worldbank, 2006,
Repositioning Nutrition as Central to Development. Washington, DC.
[25].
Cheng, Y., Dibley, M. J.,
Zhang, X. L., Zeng L., Yan, H., 2009, Assessment of dietary intake among
pregnant women in a rural area of western China. BMC Public Health, 9(22).
[26].
Khandat, M., 2014,
Nutritional Status of Rural Pregnant Women in Beed District of Maharashtrastate
of India. International Proceedings of Chemical, Biological and Environmental
Engineering, 67:92-6.
[27].
EDHS, 2014, Ethiopian
demographic and health survey 2014.
[28].
Charles, A. M.,
Campbell-Stennett, D., Yatich, N., Jolly, P. R., 2010, Predictors of anemia
among pregnant women in Westmoreland, Jamaica. Health Care for Women
International, 31(7), 585-98.
[29].
McDonald, C. M., McLean,
J., Kroeun, H., Talukder, A., Lynd, L. D., Green, T. J., 2015, Household food
insecurity and dietary diversity as correlates of maternal and child
undernutrition in rural Cambodia. European Journal of Clinical Nutrition,
69(2), 242-6.
[30].
Mihiretie, H., Mitiku,
A., Bacha, C., Getahun, D., 2015, Magnitude of Anemia and Associated Factors
among Pregnant Women Attending Antenatal Care in Nekemte Health Center. Journal
of Medical Microbiology & Diagnosis, 4(3).
[31].
dos Santos Quaresma, M.
V. L., Ulmer, F. B., Amorin, B. P., Azevedo, G. F., Seixas, T. A., Nakamoto, F.
P., 2022, Effect of oral contraceptive use on weight loss and body composition
following low-calorie diet intervention. Clinical Nutrition ESPEN, 48, 247-52.
[32].
Shamim, A. A., Mashreky,
S. R., Ferdous, T., Tegenfeldt, K., Roy, S., Rahman, A., K., Shaheen, N., 2016,
Pregnant Women Diet Quality and Its Sociodemographic Determinants in
Southwestern Bangladesh. Food Nutr Bull., 37(1), 14-26.
[33].
Data4Diets, 2023,
Data4Diets: Building Blocks for Diet-related Food Security Analysis, Version
2.0. Data4Diets, https://inddex.nutrition.tufts.edu/data4diets
[34].
Yimer B., Baraki N.,
Mesfin F., 2016, Under Nutrition and Associated Factors among Adolescent
Pregnant Women in Shashemenne District, West Arsi Zone, Ethiopia: A
Communitybased Study. Journal of Nutrition & Food Sciences, 06(01).
[35].
Tafasa S.M., Darega J.,
Dida N., Gemechu F.D., 2023, Dietary diversity, undernutrition and associated
factors among pregnant women in Gindeberet district, Oromia, Ethiopia: a
cross-sectional study. BMC Nutr, 9(1), 115.
[36].
Ali F., Thaver I., Khan
S.A., 2014, Assessment of dietary diversity and nutritional status of pregnant
women in Islamabad, Pakistan. J Ayub Med Coll Abbottabad, 26(4).
[37].
Geta T.G., Gebremedhin
S., Omigbodun A.O., 2022, Dietary Diversity Among Pregnant Women in Gurage
Zone, South Central Ethiopia: Assessment Based on Longitudinal Repeated
Measurement. Int J Womens Health,14, 599-615
[38].
Gebremichael M.A., Lema
T.B., 2023, Dietary Diversity, Nutritional Status, and Associated Factors Among
Pregnant Women in Their First Trimester of Pregnancy in Ambo District, Western
Ethiopia. Nutr Metab Insights, 16:11786388231190515.
[39].
Uwase A., Nsereko E.,
Pillay N., Levin J., 2024, Dietary diversity and associated factors among
pregnant women in the Southern Province of Rwanda: A facility-based
cross-sectional study. PLoS One, 19(2), e0297112.Ayele, E., Gebreayezgi, G.,
Mariye, T.,
[40].
Meseret, A., Aschalew,
G., Tigist, K., Mohammed, S., Yadessa, O., 2013, Prevalence of anemia and
associated risk factors among pregnant women attending antenatal care in Azezo
Health Center Gondar town, Northwest Ethiopia. J Interdiscipl Histopathol, 1(3),
137-44.
[41].
Zewde, A., Hailu, J.,
2014, Prevalence of anemia among pregnant women attending antenatal care at
Tikur Anbessa specialized hospital, Addis Ababa Ethiopia. Journal of Hematology
& Thromboembolic Diseases, 2(1).
[42].
Hinderaker, S. G., Olsen,
B. E., Bergsjø, P., Lie, R., T., Gasheka, P., Kvåle, G., 2001, Anemia in
pregnancy in the highlands of Tanzania. Acta Obstetricia et Gynecologica
Scandinavica, 80(1), 18-26.
[43].
Mahanta, L. B., Roy, T.
D., Dutta, R. G., & Devi, A. (2012). Nutritional status and the impact of
socioeconomic factors on pregnant women in Kamrup district of
Assam. Ecology of food and nutrition, 51(6), 463–480.
https://doi.org/10.1080/03670244.2012.705701
[44].
Girma, W. and Genebo, T.
(2002) Determinants of the Nutritional Status of Mothers and Children in
Ethiopia. Health and Nutrition Research Institute, Addis Ababa.
[45].
Ivers, L. C., Cullen, K. A., Freedberg, K. A.,
Block, S., Coates, J., & Webb, P. (2009). HIV/AIDS, undernutrition, and
food insecurity. Clinical infectious diseases : an official publication of
the Infectious Diseases Society of America, 49(7), 1096–1102.
https://doi.org/10.1086/605573
[46].
Naik, R., & Smith, R.
(2015). Family Planning Improves Nutrition. H. P. Project. https://www.healthpolicyproject.com/pubs/691_FPandNutritionBrief.pdf
[47].
Rana, M. J., & Goli,
S. (2017). Family Planning and Its Association with Nutritional Status of
Women: Investigation in Select South Asian Countries. Indian Journal of Human
Development, 11(1), 56-75. https://doi.org/10.1177/0973703017712392
[48].
Mandal S., Sinha N.K.,
Samanta P., Das S., Bose K., 2011, Anthropometric assessment of nutritional
status among college women of Midnapore, west Bengal, India. International
journal of life science and pharma research, 1(1).
[49].
Wondmeneh T. G. (2022).
Dietary diversity practice and its influencing factors among pregnant women in
Afar region of Ethiopia: mixed method study. BMC pregnancy and
childbirth, 22(1), 291. https://doi.org/10.1186/s12884-022-04641-y
[50].
Serbesa, M. L., Iffa, M.
T., & Geleto, M. (2019). Factors associated with malnutrition among
pregnant women and lactating mothers in Miesso Health Center,
Ethiopia. European journal of midwifery, 3, 13. https://doi.org/10.18332/ejm/110131
[51].
Getahun, G. K., Ahmed, S.
M., Degif, A. B., & Haile, M. G. (2023). The assessment of dietary
diversity score and associated factors among pregnant women of Batu district,
Southern Ethiopia, 2021: a community-based cross-sectional study. Annals of
medicine and surgery (2012), 85(3), 383–389. https://doi.org/10.1097/MS9.0000000000000239
[52]. Mohammed, F., Abdirizak, N., Jibril, A., & Oumer, A. (2023). Correlates of minimum dietary diversity among pregnant women on antenatal care follow up at public health facility in Puntland, Somalia. Scientific reports, 13(1), 21935. https://doi.org/10.1038/s41598-023-48983-9

