Drivers, Reasons, and Experiences of Default and Missed Measles Vaccination in Ethiopia: A Qualitative Study
Abstract:
Despite the
availability of a safe and free vaccine, measles first and second-dose
vaccination coverage is still low in Ethiopia. Studies that examine caregivers'
reasons for not receiving the measles vaccination in Ethiopia are scarce.
Hence, this qualitative study aimed to uncover drivers, reasons, and
experiences of default and missed measles vaccination from a caregiver
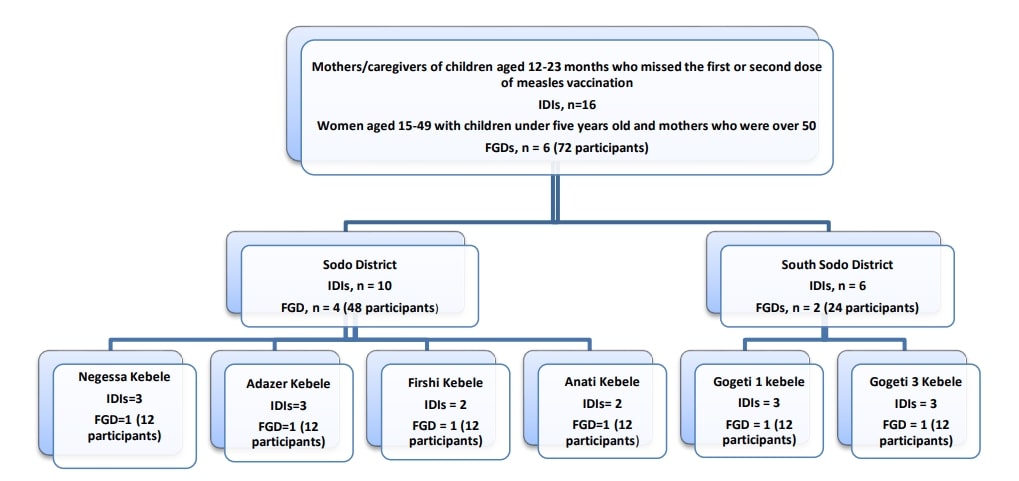
perspective. A case study was conducted from
December 2023 to May 2024 in the east Gurage zone of central Ethiopia. Data
were collected through sixteen in-depth interviews with mothers who had measles
vaccine-missed children and six focus group discussions with women aged 15-49
with children under five years old and mothers who were over 50. Caregivers were asked
to answer open-ended questions regarding reasons for missing the measles
vaccination. Data were coded, categorized, and
analyzed manually by using an inductive thematic analysis approach. The four
fundamental trustworthiness metrics for qualitative research were considered. Finally,
we presented the themes and sub-themes supporting them with representative
quotations. Geographic barriers, transportation costs, inconvenience of
vaccination dates, lack of information when to return, mistrust, rumours, poor
attendance in pregnant women's conferences, lack of autonomy to travel,
workload, economic dependency, poor male involvement, mother-in-laws’
influence, rounds of vaccination and administration routes, and adverse events
following immunization were identified as reasons for missing measles
vaccination. These reasons were found at each stage in the immunization
journey. Hence, applying a human-centred design with tailored intervention
might be important to address barriers at each stage.
References:
[1]. Centers for Disease Control and Prevention, 2024, “About Measles,” Measles (Rubeola). [Online]. Available: https://www.cdc.gov/measles/about/index.html [Accessed: 23-Jun-2024].
[2].
World
Health Organization, 2024, “Measles.” [Online]. Available: https://www.who.int/news-room/fact-sheets/detail/measles
[Accessed: 23-Jun-2024].
[3].
World
Health Organization Regional Office for Africa (WHO-AFRO), 2024,
“Vaccine-Preventable Disease Outbreaks on the Rise in Africa,” WHO | Regional
Office for Africa. [Online]. Available: https://www.afro.who.int/news/vaccine-preventable-disease-outbreaks-rise-africa
[Accessed: 31-Aug-2024].
[4].
World
Health Organization, 2024, “Immunization Coverage.” [Online]. Available: https://www.who.int/news-room/fact-sheets/detail/immunization-coverage
[Accessed: 31-Aug-2024].
[5].
World
Health Organization, 2023, “Measles - Ethiopia.” [Online]. Available: https://www.who.int/emergencies/disease-outbreak-news/item/2023-DON460
[Accessed: 23-Jun-2024].
[6].
United
Nations Children’s Fund, 2019, “The 2019 Ethiopia Mini Demographic and Health
Survey | UNICEF Ethiopia.” [Online]. Available: https://www.unicef.org/ethiopia/reports/2019-ethiopia-mini-demographic-and-health-survey
[Accessed: 14-Jul-2024].
[7].
Burton,
A., Kowalski, R., Gacic-Dobo, M., Karimov, R., and Brown, D., 2012, “A formal
representation of the WHO and UNICEF estimates of national immunization
coverage: A computational logic approach,” PLoS ONE, 7(10), p.
e47806. https://doi.org/10.1371/journal.pone.0047806
[8].
Novilla,
M. L. B., Goates, M. C., Redelfs, A. H., Quenzer, M., Novilla, L. K. B.,
Leffler, T., Holt, C. A., Doria, R. B., Dang, M. T., Hewitt, M., Lind, E.,
Prickett, E., and Aldridge, K., 2023, “Why parents say no to having their
children vaccinated against measles: A Systematic Review of the Social
Determinants of Parental Perceptions on MMR Vaccine Hesitancy,” Vaccines
(Basel), 11(5), p. 926. https://doi.org/10.3390/vaccines11050926
[9].
Adugna,
B., Tola, A., Fite, M. B., and Motuma, A., 2024, “Determinants of second-dose
measles vaccination dropout in Ethiopia: A community-based matched case-control
study,” Heliyon, 10(9), p. e30764. https://doi.org/10.1016/j.heliyon.2024.e30764
[10].
Sabahelzain,
M. M., Moukhyer, M., van den Borne, B., and Bosma, H., 2022, “Vaccine hesitancy
among parents and its association with the uptake of measles vaccine in Urban
Settings in Khartoum State, Sudan,” Vaccines, 10(2), p. 205. https://doi.org/10.3390/vaccines10020205
[11].
Majekodunmi,
O. B., Oladele, E. A., and Greenwood, B., “1 Title: Factors Affecting Poor
Measles Vaccination Coverage in Sub- 2 Saharan Africa with a Special Focus on
Nigeria: A Systematic 3 Review.”
[12].
Abegaz,
M. Y., Seid, A., Awol, S. M., and Hassen, S. L., 2023, “Determinants of incomplete
child vaccination among mothers of children aged 12–23 Months in Worebabo
District, Ethiopia: Unmatched Case-Control Study,” PLOS Global Public Health,
3(8), p. e0002088. https://doi.org/10.1371/journal.pgph.0002088
[13].
Tadesse,
T., Getachew, K., Assefa, T., Ababu, Y., Simireta, T., Birhanu, Z., and
Hailmichael, Y., 2017, “Factors and misperceptions of routine childhood
immunization service uptake in Ethiopia: findings from a nationwide qualitative
study,” Pan African Medical Journal, 28. https://doi.org/10.11604/pamj.2017.28.290.14133
[14].
Hailu,
C., Fisseha, G., and Gebreyesus, A., 2022, “Determinants of measles vaccination
dropout among 12 − 23 Months Aged Children in pastoralist community of Afar,
Ethiopia,” BMC Infectious Diseases, 22(1), p. 376. https://doi.org/10.1186/s12879-022-07350-1
[15].
Sako,
S., Gilano, G., and Hailegebreal, S., 2023, “Determinants of childhood
vaccination among Children Aged 12–23 months in Ethiopia: A community-based
cross-sectional study,” BMJ Open, 13(3), p. e069278. https://doi.org/10.1136/bmjopen-2022-069278
[16].
Shearer,
J. C., Nava, O., Prosser, W., Nawaz, S., Mulongo, S., Mambu, T., Mafuta, E.,
Munguambe, K., Sigauque, B., Cherima, Y. J., Durosinmi-Etti, O., Okojie, O.,
Hadejia, I. S., Oyewole, F., Mekonnen, D. A., Kanagat, N., Hooks, C., Fields,
R., Richart, V., and Chee, G., 2023, “Uncovering the drivers of childhood
immunization inequality with caregivers, community members and health system
stakeholders: Results from a Human-Centered Design Study in DRC, Mozambique and
Nigeria,” Vaccines, 11(3), p. 689. https://doi.org/10.3390/vaccines11030689
[17].
Moser,
A., and Korstjens, I., “Series: Practical Guidance to Qualitative Research.
Part 1: Introduction,” Eur J Gen Pract, 23(1), pp. 271–273. https://doi.org/10.1080/13814788.2017.1375093
[18].
Ethiopian
Statistical Service, 2024, “Population Projection.” [Online]. Available: https://www.statsethiopia.gov.et/population-projection/
[Accessed: 13-Oct-2024].
[19].
United
Nations Children’s Fund, 2018, “Demand for Health Services | UNICEF Office of
Innovation.” [Online]. Available: https://www.unicef.org/innovation/reports/demand-health-services
[Accessed: 22-Jun-2024].
[20].
Technical
Network for Strengthening Immunization Services (TechNet-21), 2023, “BeSD
Childhood Vaccination In-Depth Interview Guides,” TechNet-21. [Online].
Available: https://www.technet-21.org/en/resources/tool/besd-childhood-vaccination-in-depth-interview-guides
[Accessed: 01-Sep-2024].
[21].
Ogunbanjo,
G., Mabuza, L., Govender, I., and B, M., 2014, “Qualitative Data Analysis and
Writing Results (Workshop).”
[22].
Guye,
A. H., Nigussie, T., Tesema, M., Shambi, D. B., Diriba, B. S., Tefera, E. M.,
and Girma, Y., 2023, “Exploring barriers of childhood full vaccination among
children Living in Siraro District, West Arsi Zone, Oromia Region, Ethiopia: A
Qualitative Study,” Front. Pediatr., 11. https://doi.org/10.3389/fped.2023.1083358
[23].
Sodeinde,
K., Amoran, O., Abiodun, O., Adekoya, A., Abolurin, O., and Imhonopi, B., 2020,
“A rural/urban comparison of paternal involvement in childhood immunisation in
Ogun Central Senatorial District, Nigeria,” The Nigerian postgraduate Medical
Journal, 27, pp. 336–342. https://doi.org/10.4103/npmj.npmj_101_20
[24].
Ullah,
K., Saleem, J., Zakar, R., Ishaq, M., Khattak, F. A., Majeed, F., Sadiqa, H.
A., and Fischer, F., 2024, “Exploring the reasons for defaulting from childhood
immunization: A Qualitative Study in Pakistan,” BMC Public Health, 24(1),
p. 408. https://doi.org/10.1186/s12889-024-17926-y
[25].
Thirunavukkarasu,
A., Alanazi, M. F. A., Al-Hazmi, A. H., ALruwaili, B. F., Alsaidan, A. A.,
Alruwaili, T. A. M., Algaed, M. A. M., Alsharari, A. K., Alenazi, R. H.,
Alshalan, A. M., and Alshalan, S. M., 2023, “Maternal perception, hesitancy,
and satisfaction toward Childhood Immunization in Primary Health Centers, Hafr
Al-Batin: A Multicenter Cross-Sectional Study from Eastern Saudi Arabia,” RMHP,
16, pp. 2357–2368. https://doi.org/10.2147/RMHP.S406933
[26].
Yitbarek,
K., Abraham, G., and Morankar, S., 2019, “Contribution of Women’s Development
Army to maternal and Child Health in Ethiopia: A Systematic Review of
Evidence,” BMJ Open, 9(5), p. e025937. https://doi.org/10.1136/bmjopen-2018-025937
[27].
Adesina,
M. A., Olufadewa, I. I., Oladele, R. I., Solagbade, A., and Olaoyo, C., 2023,
“Determinants of childhood immunization among Rural Mothers in Nigeria,” Popul.
Med., 5(September), pp. 1–7. https://doi.org/10.18332/popmed/171542
[28].
Kolawole,
O. T., Akinyemi, A., and Solanke, B. L., 2023, “Household Vulnerability and
Childhood Immunization Status in Nigeria,” SAGE Open. https://doi.org/10.1177/21582440231179943
[29].
Amoah,
A., Issaka, J., Ayebeng, C., and Okyere, J., 2023, “Influence of women
empowerment on childhood (12–23 Months) Immunization Coverage: Recent
Evidence from 17 Sub-Saharan African Countries,” Tropical Medicine and
Health, 51(1), p. 63. https://doi.org/10.1186/s41182-023-00556-2
[30].
Simegn,
W., Diress, M., Gela, Y. Y., Belay, D. G., Ayelign Kibret, A., Chilot, D.,
Sinamaw, D., Abdu Seid, M., Andualem, A. A., Anmut Bitew, D., Eshetu, H. B.,
and Mohammed Seid, A., 2023, “Childhood Vaccination Practices and Associated
Factors among Mothers/Caregivers in Debre Tabor Town, Northwest Ethiopia: A
Cross-Sectional Study,” Front Pediatr, 11, p. 1070722. https://doi.org/10.3389/fped.2023.1070722
[31].
Powelson,
J., Kalepa, J., Kachule, H., Nkhonjera, K., Matemba, C., Chisema, M.,
Chumachapera, T., and Lawrence, E., 2024, “Using Community-Based, Participatory
Qualitative Research to Identify Determinants of Routine Vaccination Drop-out
for Children under 2 in Lilongwe and Mzimba North Districts, Malawi,” BMJ
Open, 14(2), p. e080797. https://doi.org/10.1136/bmjopen-2023-080797
[32].
Gelagay,
A. A., Geremew, A. B., Teklu, A., Mekonnen, Z. A., Gera, R., Ba-Nguz, A., and
Tilahun, B., 2021, “Full Immunization Coverage and Its Determinants among
Children Aged 12-23 Months in Wogera District, Northwest Ethiopia,” Ethiopian
Journal of Health Development, 35(3). [Online]. Available: https://www.ajol.info/index.php/ejhd/article/view/217886
[Accessed: 07-Jul-2024].
[33].
Okafor,
I. P., Chukwudi, C. L., Igwilo, U. U., and Ogunnowo, B. E., 2022, “‘Men Are the
Head of the Family, the Dominant Head’: A Mixed Method Study of Male
Involvement in Maternal and Child Health in a Patriarchal Setting, Western
Nigeria,” PLOS ONE, 17(10), p. e0276059. https://doi.org/10.1371/journal.pone.0276059
[34].
Mogoi,
D., Muchiri, E. M., and Mutuma, A. M., 2020, “Vaccine Coverage of Newly
Introduced Vaccines and Factors Influencing among Children Less Than 23 Months
in Laikipia North Subcounty,” Open Journal of Preventive Medicine, 10(2),
pp. 9–43. https://doi.org/10.4236/ojpm.2020.102002
[35].
Malande,
O. O., Munube, D., Afaayo, R. N., Annet, K., Bodo, B., Bakainaga, A., Ayebare,
E., Njunwamukama, S., Mworozi, E. A., and Musyoki, A. M., 2019, “Barriers to
Effective Uptake and Provision of Immunization in a Rural District in Uganda,” PLoS
One, 14(2), p. e0212270. https://doi.org/10.1371/journal.pone.0212270
[36].
Bangura,
J. B., Xiao, S., Qiu, D., Ouyang, F., and Chen, L., 2020, “Barriers to
Childhood Immunization in Sub-Saharan Africa: A Systematic Review,” BMC
Public Health, 20(1), p. 1108. https://doi.org/10.1186/s12889-020-09169-4
[37].
Pugliese-Garcia,
M., Heyerdahl, L. W., Mwamba, C., Nkwemu, S., Chilengi, R., Demolis, R.,
Guillermet, E., and Sharma, A., 2018, “Factors Influencing Vaccine Acceptance
and Hesitancy in Three Informal Settlements in Lusaka, Zambia,” Vaccine, 36(37),
pp. 5617–5624. https://doi.org/10.1016/j.vaccine.2018.07.042

