The Great Imposter: A Rare Case of a Pseudomyxoma Peritonei Mirroring Severe Appendicitis
Abstract:
PMP (Pseudomyxoma Peritonei) is an uncommon
disease occurring most commonly via pierced Appendiceal epithelial
tumour followed by ovaries. The best therapy contains a mix
of CRS (Cytoreductive surgery) along with intense HIPEC (Intraperitoneal
chemotherapy). There is an argument related to the diagnostic category on its
predictive significance. Tomography computer imaging is the best pre-operative method. High tumour
indicator is associated with poorer diagnosis and bigger reappearance rates. A
33-year-old female was admitted to the emergency department
of Sree Balaji Medical College and Hospital with severe pain over the right iliac fossa with four episodes
of vomiting
and one episode of fever. On Examination, he had Tenderness and Rebound
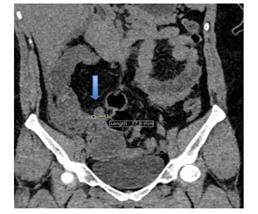
Tenderness over the Right Iliac Fossa. CECT showed features suggestive of Acute
Appendicitis and the patient was taken up for Surgery where a biopsy showed Pseudomyxoma Peritonei. The
patient further underwent
HIPEC and was followed up for 1 year with no recurrence of the disease.
References:
[1]. Bevan, K.
E., Mohamed, F., & Moran, B. J., 2010. Pseudomyxoma peritonei. World
Journal of Gastrointestinal Oncology, 2, 44–50. https://doi.org/10.4251/wjgo.v2.i1.444omini
https://pubmed.ncbi.nlm.nih.gov/21160816/
[2].
Smeenk, R. M.,
Verwaal, V. J., & Zoetmulder, F. A. N., 2007. Pseudomyxoma
peritonei. Cancer Treatment Reviews, 33, 579–586. Elsevier. https://europmp.eu/wp-content/uploads/2020/05/PSOGI_Guidelines-1.pdf
[3].
Moran, B. J., 2006. Establishment of a
peritoneal malignancy treatment centre in the United Kingdom. European
Journal of Surgical Oncology, 32, 614–618. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4204597/
[4]. Werth, R., 1884. Klinische and anastomische
Untersuchungen zur Lehre von der Bauchgeswulsten und der Laparotomy. Archiv
für Gynäkologie, 84, 100–118. http://www.worldwidejournals.org/index.php/ijsr/article/view/952
[5]. Garg, P., Garg, N., Peer, S., Chholak, D., & Kaur, M., 2024.
Pseudomyxoma peritonei leading to ‘jelly belly’ abdomen: A case report and
review of the literature. Journal of Medical Case Reports, 18, Article
296. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC11212264/
[6]. E. J. Arbuthnot, J. Parker, T. Cecil, F. Mohamed, R., Williams, M.
Page, and B. Moran, “Peritoneal malignancy in the global COVID-19 pandemic:
experience of recovery and restoration in a high-volume centre through NHS and
independent sector collaboration,” Ann. R. Coll. Surg. Engl. 106,
385–388, 2024. DOI: 10.1308/rcsann.2022.0074. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10981979/
[7]. Bouquot, M., Dohan, A., Gayat, E., Barat, M., Glehen, O., Pocard,
M., Rousset, P., & Eveno, C., 2018. Prediction of resectability in
pseudomyxoma peritonei with a new CT score. Annals of Surgical Oncology, 25,
694–701. https://pubmed.ncbi.nlm.nih.gov/29192372/
[8]. Sugarbaker, P. H., “Pseudomyxoma peritonei,” CANCER Treat. Res.
81, 105–119 1996. DOI: 10.1007/978-1-4613-1245-1_10. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4013295/
[9]. Moran, B. J., & Cecil, T.
D., 2003. The etiology, clinical presentation, and management of pseudomyxoma
peritonei. Surgical Oncology Clinics of North America, 12, 585–603. https://pubmed.ncbi.nlm.nih.gov/14567019/
[10].Mittal, R., Chandramohan, A., & Moran, B., 2017. Pseudomyxoma peritonei: Natural history and treatment. International Journal of Hyperthermia, 33, 511–519. https://www.tandfonline.com/doi/full/10.1080/02656736.2017.1310938

