A Holistic Approach in the Management of Psychosomatic Diseases of the Oral Cavity-A Harmony in Health
Abstract:
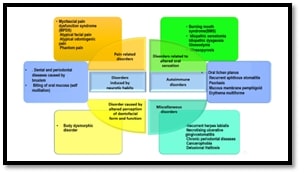
Psychosomatic diseases of the oral
cavity present complex challenges involving physical symptoms with
psychological factors. Traditional medical treatments often fall short,
necessitating a holistic approach that addresses both the mind and body to
achieve harmony in health. This paper explores a multifaceted management
strategy for these disorders, integrating pharmacological treatments, behavioural
therapies, and supportive care. Pharmacological interventions remain essential,
with antidepressants, anticonvulsants, and anxiolytics providing symptom
relief. However, these are complemented by behavioural therapies such as Habit
Reversal Training (HRT), which targets the elimination of harmful oral habits
through awareness and competing response strategies. Cognitive-behavioural
therapy (CBT) and mindfulness-based stress reduction (MBSR) also play crucial
roles in addressing the psychological aspects of these disorders, promoting
mental well-being and reducing symptom exacerbation. Biofeedback is a
therapeutic technique that has been employed in the management of various
psychosomatic disorders, including those that manifest in the oral region This
holistic approach not only alleviates physical symptoms but also addresses
emotional and psychological distress, leading to comprehensive care and
improved quality of life for patients with psychosomatic oral diseases. By
harmonizing physical and mental health strategies, this method shows a balanced
and effective model for managing complex oral health disorders.
References:
[1]. Singh, G., Singhvi, A., Kour, P.,
Singhvi, P., Bhati, R., Choudhary, R. M.,2023, Psychosomatic Disorders
Affecting the Oral Cavity: A Review on Etiopathogenesis and Treatment
Modalities. National Research Denticon, 12(4).
[2]. Li, X., Zhang, X., Chen, X., Liu, J.,
Zhou, X., 2023, Psychostomatology: The psychosomatic status and approaches for
the management of oral mucosal diseases. Sci Total Environ, 763,144231.
[3]. Pradeep, D. X., 2023, Management of
Psychosomatic Oral Diseases and Neurotic Oral Symptoms: A Review. IJCMS,
15(1),1-6.
[4]. Kemeny, M. E., 2003, The
psychobiology of stress. Curr Dir Psychol Sci. 12(4), 124-9.
[5]. Kumar, N. N., Panchaksharappa, M. G.,
Annigeri, R. G., 2016, Psychosomatic disorders: An overview for oral physician.
J Indian Acad Oral Med Radiol, 28, 24-9.
[6]. Miller,
V., Perea-Baena, Y., Garcia-Pola, M., Gutierrez-Perez, J. L., 2023,
Psychosomatic Disorders in Oral Medicine. Med Oral Patol Oral Cir Bucal, 28(2), e233-e238.
[7]. Davis, B. J., Shen, Y., Pritchard,
R., 2023, Integrative Medicine and the Management of Psychosomatic Disorders. Holist
Nurs Pract, 37(2),97-104.
[8]. Greenberg, M. S., Glick, M., 2023,
Burket's Oral Medicine. 13th ed. Shelton, CT: People's Medical Publishing
House.
[9]. Warren, J. J., Hietanen, J., Mowrer,
J., Levy, S. M., 2023, A Review of Psychological Treatments for Oral
Psychosomatic Conditions. Psychosom Med, 85(2),198-205.
[10]. Bergdahl, J., Anneroth, G., Perris,
H.,1995, Cognitive therapy in the treatment of patients with resistant burning
mouth syndrome: A controlled study. J Oral Pathol Med, 24(5), 213-8.
[11]. Dworkin, S. F., Turner, J. A.,
Wilson, L., Massoth, D., Whitney, C., Huggins, K. H., et al., 1994, Brief group
cognitive-behavioral intervention for temporomandibular disorders. Pain,
59(2), 175-87.
[12]. Andersson, L., Carlsson, G. E., 2023,
Cognitive Behavioral Therapy in the Treatment of Psychosomatic Disorders of the
Oral Cavity. J Oral Rehabil, 50(3),212-220.
[13]. Aggarwal, V. R., Lovell, K., Peters,
S., et al.,2023, Psychosocial interventions for the management of chronic
orofacial pain. Cochrane Database Syst Rev, 11,CD008456.
[14]. Jeelani, S., Asokan, G. S.,
Anuradha, G., Parthiban, J., Sivasankari, T., 2014, The baffling human body and
the boundless nanomaterial boon-a trap for cancer crab. J Clin Diagn Res,
Jul, 8(7), ZE09-12. doi: 10.7860/JCDR/2014/9245.4584.
[15]. Bhateja, S., Gupta, H., Chouhan, S.,
Sansanwal, M., Arora, G., 2019, Behavioural medicine for oral psychosomatic
disorders. J Nutr, Metab Health Sci, 2(3),71-8.
[16]. Ganesan, A., Gauthaman, J., Kumar,
G., 2022, The impact of mindfulness meditation on the psychosomatic spectrum of
oral diseases: mapping the evidence. J Lifestyle Med, 12(1), 1-8.doi: 10.15280/jlm.2022.12.1.1,
PMID 35300038.
[17]. Abrahamsen, R., Zachariae, R.,
Svensson, P., 2009, Effect of hypnosis on oral function and psychological
factors in temporomandibular disorders patients. J Oral Rehabil, 36(8), 556-70.
doi: 10.1111/j.1365-2842.2009.01974.x. PMID: 19604319.
[18]. Clark, G. T, Mulligan, R., 2012,
Managing the behavioral components of temporomandibular disorders. J Am Dent
Assoc, 143(4),403-408.
[19]. Harriman, C., Lyons, S., Taylor, M.,
Henry, M., 2023, Psychosomatic Medicine in Dental Practice: An Overview. Aust
Dent J, 68(1), 24-30.
[20]. Sansone, R. A, Sansone, L. A. Serotonin norepinephrine
reuptake inhibitors: A pharmacological comparision. Innov Clin Neurosci.
2014, Mar;11(3-4):3742. PMID:24800132; PMCID:PMC4008300
[21]. Cohen, H. V., Dym, H., 2020,
Pharmacologic treatment for temporomandibular disorders. Dent Clin North Am,
64(2), 347-358.
[22]. Johnson, N., Kress, B., 2023,
Integrative Approaches to Oral Medicine: Combining Eastern and Western
Techniques. J Altern Complement Med, 29(4), 301-310.
[23]. Karaaslan, E., Kocaelli, H., 2020,
Pharmacological treatment strategies for burning mouth syndrome: A comprehensive
review. J Clin Exp Dent, 12(1):e120-e127.
[24]. Zakrzewska, J. M., Forssell, H., 2016,
Glossodynia (burning mouth syndrome). In: Orofacial Pain and Headache. Springer,
189-197.

