Study on Awareness, Knowledge, Attitude, and Practice Related to HPV Vaccination among Healthcare Workers
Abstract:
In India, cervical
cancer is the second most diagnosed cancer in women. The World Health
Organization (WHO) has set ambitious goals known as the 90-70-90 targets to
eliminate cervical cancer: achieving 90% HPV vaccination coverage, ensuring 70%
of eligible women undergo screening twice their lifetime, and providing
treatment for 90% of women diagnosed with invasive and pre-invasive cancer. This
study aims to assess awareness levels, evaluate knowledge, and explore current
practices regarding HPV vaccination. This cross-sectional study employed an
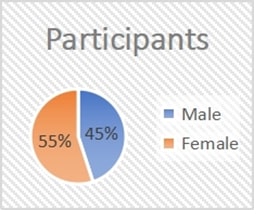
exploratory questionnaire-based survey among 200 healthcare workers at Sree
Balaji Medical College and Hospital. There is a
significant association (p = 0.002) between the type of healthcare worker
[clinical (90%) vs. non-clinical (70%)] and their awareness of HPV vaccination.
Clinical workers (85%) exhibit a significantly higher positive
attitude(p<0.01) compared to non-clinical workers (60%). The chi-square
analysis indicates a significant difference (p<0.001) in the practice of
regularly recommending or administering HPV vaccination between clinical (70%)
and non-clinical (30%) healthcare workers. There is a significant association
(p < 0.001) between Clinical workers who are likely to possess high
knowledge (70%) about HPV and its vaccination compared to non-clinical workers,
who predominantly fall into the moderate (52%) or low knowledge (48%)
categories. The findings underscore significant knowledge gaps, emphasizing the
need for improved counselling on HPV vaccination targets.
References:
[1].
KaarthigeyanK., 2012, Cervical cancer in India and HPV vaccination. Indian
J Med Paediatr Oncol. 2012, 33(1), 12, doi:https://doi.org/10.4103/0971-5851.96961
[2].
Plummer M, de Martel C, Vignat J, Ferlay J, Bray F, Franceschi S. Global
.., 2012,burden of cancers attributable to infections in 2012: a synthetic
analysis. Lancet Glob Health. 2016;4(9):e609-16, DOI: 10.1016/S2214-109X(16)30143-7
[3].
Guida, F., et al., 2022, Global and
regional estimates of maternal cancer-related orphans in 2020. Nat Med
28, 2563–2572. Nat Med. 2022
Dec;28(12):2563-2572. doi:
10.1038/s41591-022-02109-2. Epub 2022 Nov 20.
[4]. Gamble HL, Klosky JL, Parra
GR, Randolph ME., 2010, Factors influencing familial decision-making regarding
human papillomavirus vaccination. J Pediatr Psychol 2010;35:704- 15, doi: 10.1093/jpepsy/jsp108
[5].
Husain Y, Alalwan A, Al-Musawi Z, Abdulla G, Hasan K, JassimG, 2019
Knowledge towards human papilloma virus (HPV) infection and attitude towards
its vaccine in the Kingdom of Bahrain: cross- sectional study. BMJ Open.
2019; 9(9):e031017
DOI: 10.1136/bmjopen-2019-031017
[6].
Bhatla N, Joseph E., 2009, Cervical cancer prevention & the role of human
papillomavirus vaccines in India. Indian J Med Res. 2009; 130(3):334-40. PMID: 19901443
[7].
Markowitz
LE, Dunne EF, Saraiya M, et al., 2014, Human papillomavirus vaccination:
recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR
Recomm Rep 2014;63:1-30, PMID: 25167164
[8].
Brisson M, É B, Drolet M, Bogaards JA, Baussano I, Vänskä S, Jit M,Boily
M-C, Smith MA, Berkhof J, et al., 2016, Population-level impact, herdimmunity,
and elimination after human papillomavirus vaccination: A systematic review and
meta-analysis of predictions fromtransmission-dynamic models. Lancet Publ
Health. 2016;1(1):e8–e17.doi:10.1016/S2468-2667(16)30001-9
[9].
Wong
MC, Chan TT, Chan PK., 2015, A home-schooldoctor model to break the barriers
for uptake of human papillomavirus vaccine. BMC Public Health
2015;15:935. DOI 10.1186/s12889-015-2269-1
[10]. Al-Dubai,
S.A., et al., 2010,Knowledge, attitudes, and barriers for HPV vaccines among
Malaysian women. Asian Pac J Cancer Prev APJCP. 2010 Jan 1;11(4):887–892
[11]. McSherry, L.A., et al., 2012, Understanding primary care practitioners’
behaviors related to HPV using the Theoretical Domains Framework. Implement
Sci. 2012;7:73.
DOI: 10.1186/1748-5908-7-73
[12]. Durosoy R, Yamazhan M,
Taskbakan MI, Ergin I, Aysin M, Pullukcu H, et al. ,2012, HPV vaccine awareness
and willingness of first-year students entering university in western Turkey. Asian
Pac J Cancer Prev. 2010; 11(6): 1695-701
[13]. Basu, P.,
et al., 2006, Women’s perceptions and social barriers affecting compliance to
cervical screening: findings from a population-based study in India. Can
Detect Prev. 2016; 30(4): 369-74. PMID: 16963194, DOI: 10.1016/j.cdp.2006.07.004
[14]. Dabash R, Vajpayee J, Jacob M, Dzuba I, Lal N, Bradley J, et al., 2005 A
strategic assessment of cervical cancer prevention and treatment services in 3
districts of Uttar Pradesh, India. Reprod Health. 2005;2:11-6, Reproductive Health 2005, 2:11
doi:10.1186/1742-475-2-11
[15]. Pandey D, Vanya
V, Bhagat S, Vs B, Shetty J., 2012,Awareness and attitude towards human
papillomavirus (HPV) vaccine among medical students in a premier medical school
in India. PLoS One. 2012; 7(7); e40619. doi, DOI: 10.1371/journal.pone.0040619
[16]. Songthap A,
Pitisuttithum P, Kaewkungwal J, Fungladda W, Bussaratid V, Koonsaeng S., 2009. Knowledge,
attitudes, and acceptability of a human papillomavirus vaccine among healthcare
providers. Southeast Asian J Trop Med Public Health. 2009; 40:1048–56-pubmed. PMID: 19842388
[17]. Daley EM,
Vamos CA, Thompson EL, Zimet GD, Rosberger Z, Merrell L, Kline NS., 2017, The feminization
of HPV: how science,politics, economics and gender norms shaped U.S. HPV
vaccine implementation. Papillomavirus Res. 2017 Jun:3:142-148. doi: 10.1016/j.pvr.2017.04.004.
[18]. Aldrich
T, Becker D, Garcia SG, Lara D.,2005,Mexican physicians’ knowledge and
attitudes aboutthe
human papillomavirus and cervical cancer: a national survey. Sex Transm
Infect 2005; 81: 135-141, doi: 10.1136/sti.2003.008557,
PMID: 15800091
[19]. Suk R, Montealegre JR, Nemutlu
GS, et al., 2019 Public knowledge of human papillomavirus and receipt of
vaccination recommendations. JAMA Pediatr. 2019;173(11):1099-1102. doi:10.1001/jamapediatrics.2019.3105
[20].
Teresa, J., et al., 2011, Awareness of cervical cancer risk factors
among educated youth in India, Nepal, and Sri Lanka: a cross-sectional survey. Asian
Pacific J Cancer Prev. 2011;12:1707–1712

