Assessing the Impact of Competency-Based Medical Education (CBME): Insights from Medical Students
Abstract:
The National Medical
Commission (NMC) in India introduced the Competency-Based Medical Education
(CBME) curriculum to enhance medical education quality and align with global
standards. This curriculum emphasizes developing specific competencies, and ensuring
medical students possess essential skills, knowledge, and attitudes. A survey
among 500 final-year students and CRMIs at Sree Balaji Medical College and
Hospital assessed their views on the CBME curriculum using a Google Forms
questionnaire. Key findings include the majority finding the Foundation Course
necessary for their medical training, most students rating Basic Life Support
(BLS) training as very useful, and field visits generally seen as beneficial,
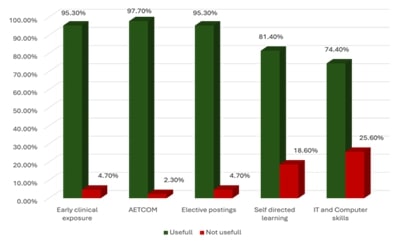
while opinions on IT skills sessions were mixed. Early clinical exposure
significantly enhanced the learning experience, with high preferences for small
group teaching, self-directed learning, reflective learning, and AETCOM
training in Phase I MBBS. Elective postings were considered beneficial by most
respondents. Students had a mixed understanding of the new assessment schemes
under CBME, and subject integration was found to be very beneficial, with
preferences for both horizontal and vertical integration. Many students found
Phase I MBBS to be academically stressful and strongly suggested more time for
sports and physical activities. Overall, the CBME curriculum was positively
received, particularly in early clinical exposure, skill development, and
subject integration. However, areas such as IT skills training, the duration of
the Foundation Course, and better synchronization of vertical integration
require improvement. Addressing these concerns can lead to better-prepared
medical graduates, capable of meeting the healthcare needs of the population with
a strong emphasis on practical skills, ethical practice, and continuous
learning.
References:
[1].
The tyranny
of the Medical Council of India’s new (2019) MBBS curriculum: Abolition of the
academic discipline of family physicians and general practitioners from the
medical education system of India. J Family Med Prim Care 2019; 8:323‑5.
[2].
Frank JR,
Mungroo R, Ahmad Y, Wang M, De Rossi S, Horsley T. Toward a definition of
competency‑based education in medicine: A systematic review of published
definitions. Med Teach 2010; 32:631‑7.
[3].
Medical
Council of India. Early Clinical Exposure for the Undergraduate Medical
Education Training Program;2019. p. 1‑43.
[4].
Medical
Council of India, Competency based Undergraduate curriculum for the Indian
Medical Graduate. Vol. 2. New Delhi, Medical Council of India; 2018.
[5].
Medical
Council of India, Competency based Undergraduate curriculum for the Indian
Medical Graduate. Vol. 3. New Delhi, Medical Council of India; 2018.
[6].
Medical
Council of India. Attitude, Ethics and Communication (AETCOM). Competencies for
the Indian Medical Graduate. New Delhi: Medical Council of India; 2018.
[7].
7.Medical
Council of India. Alignment and Integration Module for Undergraduate Medical
Education Program. New Delhi, Medical Council of India; 2019. p. 1‑34.
[8].
Sharma R,
Bakshi H, Kumar P. Competency‑based undergraduate curriculum: A critical view.
Indian J Community Med 2019; 44:77‑80.
[9].
Medical
Council of India, Competency based Undergraduate curriculum for the Indian
Medical Graduate. Vol. 1. New Delhi, Medical Council of India; 2018.
[10]. Chacko TV. Moving toward competency‑based education:
Challenges and the way forward. Arch Med Health Sci 2014; 2:247‑53.
[11]. Shah N, Desai C, Jorwekar G, Badyal D, Singh T.
Competency‑based medical education: An overview and application in
pharmacology. Indian J Pharmacol 2016;48: S5‑S9.
[12]. Basheer A. Competency‑based medical education in India:
Are we ready? J Curr Res Sci Med 2019; 5:1‑3.
[13]. Srimathi T. A study on students feedback on the
foundation course in first year MBBS curriculum. Int J Med Res Health Sci 2014;
3:575‑9.
[14]. Singh S, Ghosh S, Pandya H. Foundation programme for MBBS
students at entry level: Experience at an Indian medical school. Southeast
Asian J Med Edu 2007; 1:33‑7.
[15]. Sangappa SB, Tekian A. Communication skills course in an
Indian undergraduate dental curriculum: a randomized controlled trial. J Dent
Educ 2013; 77:1092‑8.
[16]. Choudhary A, Gupta V. Teaching communications skills to
medical students: Introducing the fine art of medical practice. Int J Appl
Basic Med Res 2015;5: S41‑4.
[17]. Komattil R, Hande SH, Mohammed CA, Subramaniam B.
Evaluation of a personal and professional development module in an
undergraduate medical curriculum in India. Korean J Med Educ 2016; 28:117‑21.
[18]. Ashin S, Shahid A, Gondal GM. Teaching communication
skills and medical ethics to undergraduate medical students. J Adv Med Prof
2013; 1:72‑76.
[19]. Modi JN, Anshu ‑, Chhatwal J, Gupta P, Singh T. Teaching
and Assessing Communication Skills in Medical Undergraduate Training. Indian
Pediatr 2016; 53:497‑504.
[20]. Naineni K, Rao GVR, Saie U. Addressing the challenges of
training in communication skills in medicine in India. J Res Med Educ Ethics
2016; 6:10‑14.
[21]. Dyrbye LN, Thomas MR, Shanafelt TD. Medical student
distress: causes, consequences, and proposed solutions. Mayo Clin Proc 2005;
80:1613‑22.
[22]. Dyrbye LN, Thomas MR, Shanafelt TD. Systematic review of
depression, anxiety, and other indicators of psychological distress among U.S.
and Canadian medical students. Acad Med 2006; 81:354‑73.
[23]. Given JL, Tjia J. Depressed medical students’ use of
mental health services and barrier to use. Acad Med 2002; 77:918‑21.
[24]. Guthrie E, Black D, Bagalkote H, Shaw C, Campbell M,
Creed F. Psychological stress and burnout in medical students: a five‑year
prospective longitudinal study. J R Soc Med 1998; 91:237‑43.
[25]. Sidik MS, Kaneson N. The prevalence of depression among
medical students. Malays J Psychiatry. 2003; 11:12‑17.
[26]. Yusoff MS, Rahman A. Stress management for medical
students: A systematic review. In: Social Sciences and Cultural Studies‑Issues
of Language, Public Opinion, Education and Welfare. Vol. 1. London, IntechOpen
Limited; 2012. p. 477‑97.

