Men’s Awareness, Support and Uptake of Modern Family Planning: A Case Study of Oyo State Nigeria
Abstract:
Amidst the availability of Modern Family
Planning (MFP), the prevalence of FP is still low in Africa. Involving men is a
critical factor for FP, owing to its benefits, decision making, use and
non-use. This study considers the view of men on FP and focused on their
perception, support and factors responsible for the use/non-use in Ibadan, Oyo
State, Nigeria. A cross-sectional study design among married men in in Oyo
State, Nigeria. A total of 452 were interviewed. Questionnaire developed using
Open Data Kit. Stata statistical was used for data analysis at p=0.05. The
majority were Muslims (61.7%), with highest level of education being secondary
education (58.4%); 40.3% between the ages of 41- 50. Awareness was high
(98.7%), with radio (77. %) being major sources. Almost all (98.2%, 97.4%,
92.0%) were aware of male condom, injectables and implants; 86.1% expressed
supports and accepted its use (82.1%). Reasons for stopping/not supporting
included personal choice (50%), side effects (18.9%) and infidelity (5.3%);
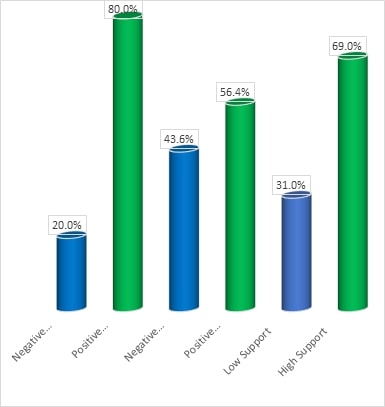
19.7% had negative perception, 43.6% negative perceived roles, 31.0% showed low
support. Level of education (x2=8.144, p-0.017) and perception; religion and
perceived roles (x2=12.089, p-0.002); level of education (x2=7.623, p-0.022)
and supports; use and level of supports (x2=62.281, p-0.000) were associated. There
was low level awareness, approval for, support and use of MFP. There is a need
to develop family and community level strategic SBCC messages to increase
awareness, approval, support and acceptance.
References:
[1]. Hoga, L.A., Rodolpho, J.R.,
Sato, P.M., Nunes, M.C. and Borges, A.L., 2014. Adult men's beliefs, values,
attitudes and experiences regarding contraceptives: a systematic review of
qualitative studies. Journal of clinical nursing, 23(7-8),
pp.927-939.
[2].
Kabagenyi, A., Jennings, L.,
Reid, A., Nalwadda, G., Ntozi, J. and Atuyambe, L., 2014, Barriers to male
involvement in contraceptive uptake and reproductive health services: a qualitative
study of men and women’s perceptions in two rural districts in Uganda. Reproductive
health, 11, pp.1-9.
[3]. Mulatu, T., Sintayehu, Y.,
Dessie, Y. and Dheresa, M., 2022, Male involvement in family planning use and
associated factors among currently married men in rural Eastern Ethiopia. SAGE
Open Medicine, 10, p.20503121221094178.
[4]. W.H.O. 2021, Sexual Reproductive Health:
Maternal health in Nigeria: Generating information for action. Geneva:
World Health Organization. Accessed 6 7, 2021. https://who.int/reproductivehealth.
[5]. Starbird, E., Norton, M.,
and Marcus, R., 2016, Investing in family planning: key to achieving the
sustainable development goals. Global health: science and practice, 4(2),
pp.191-210.
[6]. Ajayi, I. A., and Akpan, W., 2018, Use of
traditional and modern contraceptives among childbearing women: Findings from a
mixed methods study in two south-western Nigerian states." BMC Public
Health, 604-626.
[7]. NBS. 2015, Tanzania demographic and health
survey and malaria indicator survey. Tanzania: National Bureau of
Statistics.
[8]. Blackstone, S. R., Nwaozuru, U., and
Iwelunmor, J., 2017, Factors influencing contraceptive use in sub-saharan
Africa: A systematic review." International Quarterly of Community
Health Education, 241-260.
[9]. Msoka, A.C., Pallangyo,
E.S., Brownie, S., and Holroyd, E., 2019, My husband will love me more if I
give birth to more children: Rural women’s perceptions and beliefs on family
planning services utilization in a low resource setting. International
Journal of Africa Nursing Sciences, 10, pp.152-158.
[10]. Adongo, P.B., Tapsoba, P.,
Phillips, J.F., Tabong, P.T.N., Stone, A., Kuffour, E., Esantsi, S.F. and
Akweongo, P., 2014, “If you do vasectomy and come back here weak, I will
divorce you”: a qualitative study of community perceptions about vasectomy in
Southern Ghana. BMC International Health and Human Rights, 14,
pp.1-8.
[11]. Wondim, G., Degu, G., Teka, Y., and Diress, G., 2020, Male involvement
in family planning utilization and associated factors in Womberma District,
Northern Ethiopia: community-based cross-sectional study. Open Access
Journal of Contraception, pp.197-207.
[12]. Asare, O., Otupiri, E.,
Apenkwa, J. and Odotei-Adjei, R., 2017, Perspectives of urban Ghanaian women on
vasectomy. Reproductive Health, 14, pp.1-6.
[13]. Hutchinson, P.L., Anaba, U.,
Abegunde, D., Okoh, M., Hewett, P.C. and Johansson, E.W., 2021, Understanding
family planning outcomes in northwestern Nigeria: analysis and modeling of
social and behavior change factors. BMC Public Health, 21(1),
p.1168.
[14]. Izugbara, C.O., and Ezeh,
A.C., 2010, Women and high fertility
in Islamic northern Nigeria. Studies
in family planning, 41(3),
pp.193-204.
[15]. Obasohan, P.E., 2015, Religion, ethnicity and
contraceptive use among reproductive age women in Nigeria. International Journal of MCH and AIDS, 3(1), p.63.
[16]. Ijadunola, M.Y., Abiona,
T.C., Ijadunola, K.T., Afolabi, O.T., Esimai, O.A. and OlaOlorun, F.M., 2010, Male involvement in family
planning decision making in Ile-Ife, Osun State, Nigeria. African journal of reproductive health, 14(4).
[17]. Oyo State., 2024, About Oyo State. Accessed: 11th
January, 2024. (https://old.oyostate.gov.ng/about-oyo-state/).
[18]. Okwor, E.U., and Olaseha,
I.O., 2010, Married men's perception about spousal use of modern
contraceptives: a qualitative study in Ibadan northwest local government area,
southwest Nigeria. International quarterly of community health
education, 30(3), pp.223-238.
[19]. Sekoni, O.O., and Oladoyin,
V.O., 2016, Determinants of family planning uptake among men in Ibadan,
Nigeria. Journal of Community Medicine and Primary Health Care, 28(1),
pp.38-44.
[20]. Sabale, U., Suryarao, P.,
and Kodla, C., 2022, Study of Awareness of Family Planning Methods among
Married Men. Journal
of South Asian Federation of Obstetrics and Gynaecology, 14(5), pp.531-533.
[21]. Omolase, C.O., Faturoti,
S.O., and Omolase, B.O., 2009, Awareness of family planning amongst antenatal
patients in a Nigerian community: an exploratory study. Annals of Ibadan postgraduate medicine, 7(1), pp.36-39.
[22]. Withers, M., Dworkin, S.L.,
Zakaras, J.M., Onono, M., Oyier, B., Cohen, C.R., Bukusi, E.A., Grossman, D.
and Newmann, S.J., 2015. ‘Women now wear trousers’: men's perceptions of family
planning in the context of changing gender relations in western Kenya. Culture,
health & sexuality, 17(9), pp.1132-1146.
[23]. Withers, M., Dworkin, S.L., Onono, M., Oyier, B., Cohen, C.R., Bukusi,
E.A. and Newmann, S.J., 2015. Men's perspectives on their role in family
planning in Nyanza Province, Kenya. Studies in Family Planning, 46(2),
pp.201-215.
[24]. Thummalachetty, N., Mathur,
S., Mullinax, M., DeCosta, K., Nakyanjo, N., Lutalo, T., Brahmbhatt, H. and
Santelli, J.S., 2017, Contraceptive knowledge, perceptions, and concerns among
men in Uganda. BMC public health, 17, pp.1-9.
[25]. Harrington, E.K., McCoy,
E.E., Drake, A.L., Matemo, D., John-Stewart, G., Kinuthia, J. and Unger, J.A.,
2019, Engaging men in an mHealth approach to support postpartum family planning
among couples in Kenya: a qualitative study. Reproductive health, 16,
pp.1-11.
[26]. Obare, F., Odwe, G. and Cleland, J., 2021, Men’s needs and women’s
fears: gender-related power dynamics in contraceptive use and coping with
consequences in a rural setting in Kenya. Culture, health &
sexuality, 23(12), pp.1748-1762.
[27]. Koffi, T.B., Weidert, K.,
Bitasse, E.O., Mensah, M.A.E., Emina, J., Mensah, S., Bongiovanni, A. and
Prata, N., 2018, Engaging men in family planning: Perspectives from married men
in Lomé, Togo. Global Health: Science and Practice, 6(2),
pp.317-329.
[28]. Ezeanolue, E.E., Iwelunmor, J., Asaolu, I., Obiefune, M.C., Ezeanolue,
C.O., Osuji, A., Ogidi, A.G., Hunt, A.T., Patel, D., Yang, W. and Ehiri, J.E.,
2015, Impact of male partner’s awareness and support for contraceptives on
female intent to use contraceptives in southeast Nigeria. BMC public
health, 15, pp.1-6.
[29]. Ankomah, A., Anyanti, J. and
Oladosu, M., 2011, Myths, misinformation, and communication about family
planning and contraceptive use in Nigeria. Open Access Journal of
Contraception, pp.95-105.
[30]. Gueye, A., Speizer, I.S., Corroon, M. and Okigbo, C.C., 2015, Belief in
family planning myths at the individual and community levels and modern
contraceptive use in urban Africa. International perspectives on sexual
and reproductive health, 41(4), p.191.
[31]. Gebremariam, A., and
Addissie, A., 2014, Intention to use long acting and permanent contraceptive
methods and factors affecting it among married women in Adigrat town, Tigray,
Northern Ethiopia. Reproductive health, 11, pp.1-9.
[32]. Chola, L., McGee, S.,
Tugendhaft, A., Buchmann, E. and Hofman, K., 2015, Scaling up family planning
to reduce maternal and child mortality: the potential costs and benefits of modern
contraceptive use in South Africa. PloS one, 10(6),
p.e0130077.
[33]. Kebede, A., Abaya, S.G.,
Merdassa, E. and Bekuma, T.T., 2019, Factors affecting demand for modern
contraceptives among currently married reproductive age women in rural Kebeles
of Nunu Kumba district, Oromia, Ethiopia. Contraception and
reproductive medicine, 4, pp.1-15.
[34]. Kamal, M.M., Islam, M.S.,
Alam, M.S. and Hasssn, A.E., 2013, Determinants of male involvement in family
planning and reproductive health in Bangladesh. American Journal of
Human Ecology, 2(2), pp.83-93.
[35].
Amu, E.O., Akinwumi, A.F.
and Odu, O.O., 2021, Family Planning Awareness, Perception, Utilization and
Barriers among Women in Irepodun Local Government Area, Osun State,
South-Western Nigeria. Nigerian Journal of Family Practice, 12(1),
pp.31-39.
[36]. Asmamaw, D.B., Eshetu, H.B.
and Negash, W.D., 2022, Individual and community-level factors associated with
intention to use contraceptives among reproductive age women in sub-Saharan
Africa. International Journal of Public Health, 67, p.1604905.
[37]. Akamike, I.C., Okedo-Alex,
I.N., Eze, I.I., Ezeanosike, O.B. and Uneke, C.J., 2020, Why does uptake of
family planning services remain sub-optimal among Nigerian women? A systematic
review of challenges and implications for policy. Contraception and
reproductive medicine, 5, pp.1-11.
[38]. Semachew Kasa, A., Tarekegn,
M. and Embiale, N., 2018. Knowledge, attitude and practice towards family
planning among reproductive age women in a resource limited setting of
Northwest Ethiopia. BMC
research notes, 11,
pp.1-6.
[39]. Steinfeld, R.L., Newmann,
S.J., Onono, M., Cohen, C.R., Bukusi, E.A. and Grossman, D., 2013, Overcoming
Barriers to Family Planning through Integration: Perspectives of HIV‐Positive
Men in Nyanza Province, Kenya. AIDS Research and Treatment, 2013(1),
p.861983.
[40]. Nmadu, A.G., Joshua, I.A., Omole, V.N., Usman, N.O., Igboanusi, C.J.C.
and Gobir, A.A., 2019, Male involvement in family planning in Northern Nigeria:
A review of literature. Journal of Medicine in the Tropics, 21(1),
pp.6-9.
[41]. Adanikin, A.I., McGrath, N.
and Padmadas, S.S., 2017, Impact of men’s perception on family planning demand
and uptake in Nigeria. Sexual
& Reproductive Healthcare, 14,
pp.55-63.
[42]. Adedini, S.A., Babalola, S.,
Ibeawuchi, C., Omotoso, O., Akiode, A. and Odeku, M., 2018, Role of religious
leaders in promoting contraceptive use in Nigeria: evidence from the Nigerian
urban reproductive health initiative. Global Health: Science and
Practice, 6(3), pp.500-514.

