Assessment of Risk Factors Associated with Common Fungal Pathogens Causing Otomycosis at a Tertiary Care Hospital in South India
Abstract:
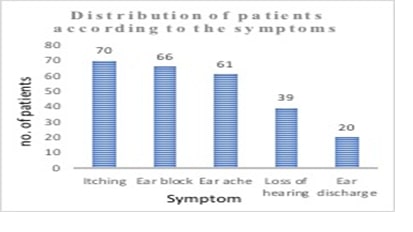
Otomycosis is one of the most prevalent fungal diseases of the external auditory canal in the tropical and sub-tropical regions of the world. Numerous environmental and host factors can put a person at risk for otomycosis. This cross-sectional study was undertaken over a one-year period at a tertiary care hospital, in South India after approval from Institutional Human Ethics Committee (IHEC), as there is limited data available on the clinical-mycological profile and its association with various risk factors in our region in the recent past. 90 ear swabs from clinically diagnosed otomycosis patients were sent to the laboratory for mycological examination from the Ear, Nose, and Throat (ENT) out-patient Department. Their clinical data was evaluated using a self-administered questionnaire. Mycological examination yielded 63 fungal isolates with Aspergillus niger as the predominant organism followed by other fungi; common risk factors identified were diabetes mellitus (92%), CSOM patients on steroid drops (91.6%), swimming (80%), CSOM patients on antibiotic drops (75%) with a significant association of p<0.05 between the above-mentioned risk factors and otomycosis. The current study highlights that proper identification of the causative agents is mandatory to prevent complications and recurrences, even when the patients' otoscopic findings and clinical presentations strongly suggest a fungal infection. Comparable with other superficial fungal infections, otomycosis does not represent a threat to life. However, prompt microbiological identification are essential for timely and effective therapy to avert major issues from otomycosis.References:
[1]. Ibekwe, T. S., & Nwaorgu, O. G.,
2011, Classification and Management Challenges of Otitis Media in a
Resource-Poor Country. Nigerian journal of clinical practice, 14(3),
262-262. https://doi.org/10.4103/1119-3077.86764
[2]. Agarwal,
P., & Devi, L. S., 2017, Otomycosis in a Rural Community Attending a
Tertiary Care Hospital: Assessment of Risk Factors and Identification of Fungal
and Bacterial Agents. Journal of Clinical and Diagnostic Research: JCDR,
11(6): DC14-DC18. https://doi.org/10.7860/JCDR/2017/25865.10068
[3]. Mofatteh, M. R.,
Naseripour Yazdi, Z., Yousefi, M., Namaei, M.H., 2018, Comparison of the Recovery
Rate of Otomycosis Using Betadine and Clotrimazole Topical Treatment. Brazilian Journal of Otorhinolaryngology, 84(4):404–409. https://doi.org/10.1016/j.bjorl.2017.04.004
[4]. Ho,
T., Vrabec, J. T., Yoo, D., & Coker, N. J., 2006, Otomycosis: clinical
features and treatment implications. Otolaryngology-Head and Neck Surgery: Official
Journal of American Academy of Otolaryngology-Head and Neck Surgery, 135(5),
787–791. https://doi.org/10.1016/j.otohns.2006.07.008
[5]. Malcolm, T. R., & Chin‐Hong,
P. V., 2013, Endemic Mycoses in Immunocompromised Hosts. Current Infectious
Diseases Reports, 15(6), 536-543. https://doi.org/10.1007/s11908-013-0387-4
[6]. Tasić-Otašević,
S., Golubović, M., Đenić, S., Ignjatović, A., Stalević, M., Momčilović, S.,
Bojanović, M., Arsić-Arsenijević, V., 2020, Species Distribution Patterns and
Epidemiological Characteristics of Otomycosis in Southeastern Serbia. Journal
de Mycologie Médicale, 30(3), 101011. https://doi.org/10.1016/j.mycmed.2020.101011
[7]. Pfaller, M. A., & Diekema, D. J., 2004, Rare and
Emerging Opportunistic Fungal Pathogens: Concern for Resistance Beyond Candida Albicans
and Aspergillus Fumigatus. Journal of Clinical Microbiology, 42(10),
4419-4431. https://doi.org/10.1128/jcm.42.10.4419-4431.2004
[8]. Ostrowski, V. B., & Wiet, R J., 1996, Pathologic Conditions
of the External Ear and Auditory Canal. Postgraduate Medicine, 100(3),
223-237. https://doi.org/10.3810/pgm.1996.09.79
[9]. Fisher,
M. C., Gurr, S. J., Cuomo, C. A., Blehert, D. S., Jin, H., Stukenbrock, E. H.,
Stajich, J. E., Kahmann, R., Boone, C., Denning, D. W., Gow, N. A. R., Klein,
B. S., Kronstad, J. W., Sheppard, D. C., Taylor, J. W., Wright, G. D., Heitman,
J., Casadevall, A., & Cowen, L. E., 2020, Threats Posed by the Fungal
Kingdom to Humans, Wildlife, and Agriculture. Microbiology, 11(3), e00449-20. https://doi.org/10.1128/mBio.00449-20
[10]. Galimberti, R., Torre, A C., Baztán, M C., &
Rodriguez-Chiappetta, F., 2012, Emerging Systemic Fungal Infections. Clinics
in Dermatology, 30(6), 633-650. https://doi.org/10.1016/j.clindermatol.2012.01.011
[11].
Kamali Sarvestani,
H., Seifi, A., Falahatinejad, M., & Mahmoudi, S., 2022, Black Aspergilli as
Causes of Otomycosis in the Era of Molecular Diagnostics, a Mini-Review. Journal De Mycologie Medicale, 32(2), 101240. https://doi.org/10.1016/j.mycmed.2021.101240
[12].
Aneja, K.R., Sharma,
C., Joshi, R., 2010, Fungal Infection of the Ear: A Common Problem in the North
Eastern Part of Haryana. International Journal
of Pediatric Otorhinolaryngology, 74:604–607. https://doi.org/10.1016/j.ijporl.2010.03.001
[13].
Buonafina-Paz, M. D.,
Santos, F. A., Leite-Andrade, M. C., Alves, A. I., Bezerra, J. D., Leal, M. C.,
Robert, E., Pape, P. L., Lima-Neto, R. G., & Neves, R. P., 2022, Otomycosis
Caused by the Cryptic and Emerging Species Aspergillus Sydowii: Two Case
Reports. Future Microbiology,17:1437–1443. https://doi.org/10.2217/fmb-2022-0137
[14]. Bojanović,
M., Stalević, M., Arsić-Arsenijević, V., Ignjatović, A., Ranđelović, M.,
Golubović, M., Živković-Marinkov, E., Koraćević, G., Stamenković, B., Otašević,
S., 2023, Etiology, Predisposing Factors, Clinical Features and Diagnostic
Procedure of Otomycosis: A Literature Review. Journal of Fungi, 9(6):662.
http://doi.org/10.3390/jof9060662
[15]. Bluestone, C D., & Klein, J O., 1999, Consultation with
the Specialist: Chronic Suppurative Otitis Media. Pediatrics in Review,
20(8), 277-279. https://doi.org/10.1542/pir.20-8-277
[16]. Patricia, M. T., 2014,
Bailey & Scott’s Diagnostic Microbiology. (Elsevier, St. Louis, MO).
10.1309/LM5JC0PH0OGGBSZZ
[17]. Odds, F. C., &
Bernaerts, R., 1994, CHROMagar Candida, A New Differential Isolation Medium for
Presumptive Identification of Clinically Important Candida Species. Journal
of Clinical Microbiology, 32(8):1923–1929. https://doi.org/10.1128/jcm.32.8.1923-1929.1994
[18]. Yegane
Mogadam, A., Asadi, M. A., Dehghani, R., Hooshyar, H., 2009, The Prevalence of
Otomycosis in Kasham Iran During 2001-2003. Jundishapur J Microbiol, 2(1):18–21.
[19]. Asoegwu,
C. N., Oladele, R. O., Kanu, O. O., Peters, R. F., & Nwawolo, C. C., 2023.
Clinical and Microbiological Profile of Otomycosis in Lagos, Nigeria. The Nigerian
Postgraduate Medical Journal,30(2), 132–136. https://doi.org/10.4103/npmj.npmj_9_23
[20]. Prasad,
S. C., Kotigadde, S., Shekhar, M., Thada, N. D., Prabhu, P., D' Souza, T.,
& Prasad, K. C., 2014, Primary Otomycosis in the Indian Subcontinent: Predisposing
Factors, Microbiology, and classification. International Journal of
Microbiology, 2014, 636493. https://doi.org/10.1155/2014/636493
[21]. Hagiwara,
S., Tamura, T., Satoh, K., Kamewada, H., Nakano, M., Shinden, S., Yamaguchi,
H., & Makimura, K., 2019, The Molecular Identification and Antifungal
Susceptibilities of Aspergillus Species Causing Otomycosis in Tochigi, Japan. Mycopathologia,
184(1), 13–21. https://doi.org/10.1007/s11046-018-0299-9
[22]. Onotai,
L., & Osuji, A. E., 2017, Otomycosis: Management Challenges and Outcomes in
a Resource Poor Country. The Nigerian Health Journal, 16(4), 219.
https://doi.org/10.60787/tnhj.v16i4.260
[23]. Aggarwal, S. K.,
Jaiswal, K., 2019, Fungal Profile and its Characteristics in Patients of
Otomycosis‑A Prospective Study. National Journal of Laboratory Medicine,
8(4):MO04-MO07.
[24]. Gupta, S.,
Mahajan, B., 2015, Prevalence and Demographical Profile of Patients Presenting with
Otomycosis. JK Science, 17:138‑42.
[25]. Ameye, S. A.,
Adeyemo, A., Eziyi, J. A., Amusa, Y. B., 2018, Clinical Profile of Otomycosis
in a Sub‑Saharan African Tertiary Health Center. An International Journal of
Otorhinolaryngology Clinics, 10:52‑5. http://doi.org/10.5005/jp-journals-10003-1290
[26]. Howlader,
A., Nagarajan, P., Ragunathan, L., 2022, Mycological Profile in Otomycosis
Patients and their Drug Sensitivity: A Cross-sectional Study at Union
Territory of Puducherry, India, Journal of Clinical And Diagnostic
Research, 16(10), DC11-DC15. https://www.doi.org/10.7860/JCDR/2022/57715/17073
[27]. Ashopa,V.,
Verma,U., Nareda, P., Gupta, E., prakash, P., 2020, Assessment of Risk
Factors and Microbial Profile of Otomycosis in Patients Attending Tertiary
Level Hospital of Western Rajasthan, India, Journal of clinical and
diagnostic research.14(2),DC01-DC04. https://www.doi.org/10.7860/JCDR/2020/43153/13477
[28]. Taneja, M. K., 1998, Acute
Otitis Media. Indian Journal of Otology, 4(4):161-164.
[29]. Mawson, S. R., and
Ludman, H., 1979, In:Diseases of the Ear: A Textbook of Otology. (Chicago
Yearbook Medical Publishing, pp 328-30).
[30]. Kunelskaya, V. Y.
A., 1969, Significance of Fungal Flora in Chronic Suppurative Otitis Media. Vestn
Otorinolaringol (Rus), 31(2):28–32.
[31]. Viswanatha, B., &
Naseeruddin, K., 2011, Fungal Infections of the Ear in Immunocompromised Host: A
Review. Mediterranean Journal of Hematology and Infectious Diseases,
3(1): e2011003. http://doi.org/10.4084/MJHID.2011.003
[32]. Anwar, K., &
Gohar, M. S., 2014, Otomycosis; Clinical Features, Predisposing Factors and
Treatment Implications. Pakistan Journal of Medical Sciences, 30(3):564–567.
https://doi.org/10.12669/pjms.303.4106
[33]. Pontes,
Z. B., Silva, A. D., Lima, E.deO., Guerra, M.deH., Oliveira, N. M., Carvalho,
M.deF., & Guerra, F. S., 2009, Otomycosis: A Retrospective Study. Brazilian
Journal of Otorhinolaryngology,75(3), 367–370. https://doi.org/10.1016/S1808-8694(15)30653-4
[34]. Padma,
R., Mrunal, P., Ketki, P., Nidhi, A., 2023, Otitis Media and its Associated
Risk Factors: An Investigation into Patients’ Knowledge, Attitudes, Practices,
and Information Sources at a Hospital Setting. MGM Journal of Medical
Sciences, 10(3): p 540-547.https://doi.org/10.4103/mgmj.mgmj_127_23
[35]. Suresh,
S., Suresh, S., & Sivasamy, S., 2021, Prevalence of Otomycosis in Patients
with Cerumen Impaction due to Earphone Usage During COVID-19.
Indonesian Journal of Medical Sciences and Public Health. 2(1), 28 – 39.
https://doi.org/10.11594/ijmp.02.01.04

