Human Saliva and the COVID-19 Infection
Abstract:
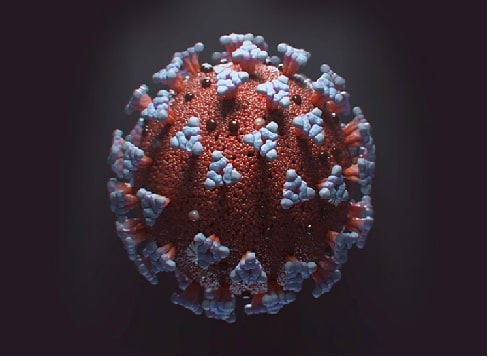
Human saliva is a complex mixture of various organic and
inorganic compounds and host-derived molecules. Performs numerous functions.
This comprehensive review will discuss the roles played by saliva in defence
against the SARS-CoV-2 virus and the use of saliva as a diagnostic fluid in COVID-19
screening will be discussed along with a brief note on SARS-CoV-2 transmission
through saliva. Saliva and SARS Cov 2: The antimicrobial and antiviral
properties of saliva are conferred by the salivary peptides such as defensins, cathelicidins,
and LL 37. Antiviral activity against the herpes virus, hepatitis C virus,
ebola virus and to an extent HIV has been documented. Since the COVID-19
pandemic has now occurred as a new global threat, it is being investigated if
saliva has certain properties that could defend against this infection. Studies
have found the regular presence of the SARS-CoV-2 virus, the aetiological agent
of the COVID-19 disease in saliva, hence saliva could be used as a diagnostic
tool. Some interesting findings have highlighted the presence of the virus in
salivary samples but documented its absence in throat swabs which is intriguing.
Despite having multifaceted roles, the drawback of saliva also lies in its
contribution to the transmission of the SARS-CoV-2 virus. Studies have shown
that viable viruses can be transmitted through saliva from person to person
through coughing and sneezing. Hence saliva could be regarded as a double-edged
sword in the COVID-19 pandemic.
References:
[1]. Anderson, P., Hector, M. P., & Rampersad, M. A., 2001, Critical pH in
Resting and Stimulated Whole Saliva in Groups of Children and Adults. International
Journal of Paediatric Dentistry, 11(4), 266–273, https://doi.org/10.1046/j.1365-263x.2001.00293.x
[2]. Alamoudi, N., Farsi, N., Faris, J., Masoud, I., Merdad, K., and Meisha,
D., 2004, Salivary Characteristics of Children and its Relation to Oral
Microorganism and Lip Mucosa Dryness. The Journal of Clinical Paediatric Dentistry,
28(3), 239–248. https://doi.org/10.17796/jcpd.28.3.h24774507006l550
[3].
Baskar, S. N., 1997,
Orban’s Oral Histology and Embryology. (11th ed. St. Louis: Harcourt Asia PIE
Ltd., Mosby).
[4]. Edgar, W. M.,1992, Saliva: Its Secretion, Composition and Functions. British
Dental Journal, 172(8), 305–312, https://doi.org/10.1038/sj.bdj.4807861
[5].
Roth, G., Calmes, R.,
1981, Salivary Glands and Saliva. Oral Biology, (CV Mosby, St Louis).
[6]. Edgar, W. M., 1990, Saliva and Dental Health. Clinical Implications of
Saliva: Report of a Consensus Meeting. British Dental Journal, 169(3-4),
96–98, https://doi.org/10.1038/sj.bdj.4807284
[7]. K, H. S., R, G., Ramani, P., & Veeraraghavan, V. P., 2024, Longitudinal
Study on Salivary IL-6 Trajectories in Postoperative OSCC Patients After
Chemotherapy and Radiotherapy. Journal of Stomatology, Oral and
Maxillofacial Surgery, 101909. Advance Online Publication. https://doi.org/10.1016/j.jormas.2024.101909
[8]. Alam, M. K., Zaman, M. U., Alqhtani, N. R., Alqahtani, A. S., Alqahtani,
F., Cicciù, M., & Minervini, G., 2024, Salivary Biomarkers and
Temporomandibular Disorders: A Systematic Review Conducted According to PRISMA Guidelines
and the Cochrane Handbook for Systematic Reviews of Interventions. Journal
of Oral Rehabilitation, 51(2), 416–426. https://doi.org/10.1111/joor.13589
[9]. Thomas, J. T., Joseph, B., Varghese, S., Thomas, N. G., Kamalasanan
Vijayakumary, B., Sorsa, T., Anil, S., & Waltimo, T., 2024, Association Between
Metabolic Syndrome and Salivary MMP-8, Myeloperoxidase in Periodontitis. Oral Diseases,
Advance Online Publication. https://doi.org/10.1111/odi.15014
[10]. Fathima, R., Ramamoorthi, R.,
Gopalakrishnan, S., Jayaseelan, V. P., & Muniapillai, S., 2024, Expression of
Salivary Levels of S100A7 in Oral Submucous Fibrosis and Oral Leukoplakia. Journal
of Oral and Maxillofacial Pathology: JOMFP, 28(1), 84–89. https://doi.org/10.4103/jomfp.jomfp_113_23
[11]. Dawes, C., 1998, Recent Research on Calculus. The New Zealand Dental Journal,
94(416), 60–62.
[12]. Malamud, D., Abrams, W. R., Barber, C. A., Weissman, D., Rehtanz, M.,
& Golub, E., 2011, Antiviral Activities in Human Saliva. Advances in Dental
Research, 23(1), 34–37. https://doi.org/10.1177/0022034511399282
[13]. Wu, Z., Van, Ryk, D., Davis, C., Abrams, W. R., Chaiken, I., Magnani, J.,
& Malamud, D., 2003, Salivary Agglutinin Inhibits HIV Type 1 Infectivity
Through Interaction with Viral Glycoprotein 120. AIDS Research and Human
Retroviruses, 19(3), 201–209, https://doi.org/10.1089/088922203763315704
[14]. White, M. R., Crouch, E., Vesona, J., Tacken, P. J., Batenburg, J. J.,
Leth-Larsen, R., Holmskov, U., and Hartshorn, K. L., 2005, Respiratory Innate
Immune Proteins Differentially Modulate the Neutrophil Respiratory Burst
Response to Influenza a Virus. Lung Cellular and Molecular Physiology. American
Journal of Physiology, 289(4), L606–L616, https://doi.org/10.1152/ajplung.00130.2005
[15]. Nagashunmugam, T., Malamud, D., Davis, C., Abrams, W. R., & Friedman,
H. M.,1998, Human Submandibular Saliva Inhibits Human Immunodeficiency Virus
Type 1 Infection by Displacing Envelope Glycoprotein gp120 from the Virus. The
Journal of Infectious Diseases, 178(6), 1635–1641, https://doi.org/10.1086/314511
[16]. Banerjee, A., Kulcsar, K., Misra, V., Frieman, M., & Mossman, K.,
2019, Bats and Coronaviruses. Viruses, 11(1), 41, https://doi.org/10.3390/v11010041
[17]. Yang, D., & Leibowitz, J. L., 2015, The Structure and Functions of
Coronavirus Genomic 3' and 5' Ends. Virus Research, 206, 120–133, https://doi.org/10.1016/j.virusres.2015.02.025
[18].
Ramaiah. A.,
Arumugaswami, V., 2020, Insights into Cross-Species Evolution of Novel Human
Coronavirus 2019-nCoV and Defining Immune Determinants for Vaccine Development.
bioRxiv https://doi:10.1101/2020.01.29.925867
[19].
Chan, J. F., Kok, K. H.,
Zhu, Z., Chu, H., To, K. K., Yuan, S., and Yuen, K. Y., 2020, Genomic
Characterization of the 2019 Novel Human-Pathogenic Coronavirus Isolated from a
Patient with Atypical Pneumonia After Visiting Wuhan. Emerging Microbes &
Infections, 9(1), 221–236, https://doi.org/10.1080/22221751.2020.1719902
[20].
Wu, A., Peng, Y., Huang,
B., Ding, X., Wang, X., Niu, P., Meng, J., Zhu, Z., Zhang, Z., Wang, J., Sheng,
J., Quan, L., Xia, Z., Tan, W., Cheng, G., & Jiang, T., 2020, Genome
Composition and Divergence of the Novel Coronavirus (2019-nCoV) Originating in
China. Cell Host & Microbe, 27(3), 325–328, https://doi.org/10.1016/j.chom.2020.02.001
[21].
Yuan, Y., Cao, D., Zhang,
Y., Ma, J., Qi, J., Wang. Q., et al., 2017, Cryo-EM Structures of MERS-CoV and
SARS-CoV Spike Glycoproteins Reveal the Dynamic Receptor Binding Domains. Nat
Commun, 8:15092, https://doi:10.1038/ncomms15092
[22].
Walls, A. C., Xiong, X.,
Park, Y. J., Tortorici, M. A., Snijder, J., Quispe, J., Cameroni, E., Gopal,
R., Dai, M., Lanzavecchia, A., Zambon, M., Rey, F. A., Corti, D., &
Veesler, D., 2019, Unexpected Receptor Functional Mimicry Elucidates Activation
of Coronavirus Fusion. Cell, 176(5), 1026–1039.e15. https://doi.org/10.1016/j.cell.2018.12.028
[23].
Paules, C. I., Marston,
H, D., & Fauci, A. S., 2020, Coronavirus Infections-More than Just the
Common Cold. JAMA, 323(8), 707–708, https://doi.org/10.1001/jama.2020.0757
[24].
Xu, H., Zhong, L., Deng,
J., Peng, J., Dan, H., Zeng, X., Li, T., & Chen, Q., 2020, High Expression
of ACE2 Receptor of 2019-nCoV on the Epithelial Cells of Oral Mucosa. International
Journal of Oral Science, 12(1), 8, https://doi.org/10.1038/s41368-020-0074-x
[25].
Iwabuchi, H.,
Fujibayashi, T., Yamane, G. Y., Imai, H., & Nakao, H., 2012, Relationship Between
Hyposalivation and Acute Respiratory Infection in Dental Outpatients.
Gerontology, 58(3), 205–211. https://doi.org/10.1159/000333147
[26].
Magister, S., & Kos,
J., 2013, Cystatins in Immune System. Journal of Cancer, 4(1), 45–56. https://doi.org/10.7150/jca.5044
[27].
Collins, A. R., &
Grubb, A., Cystatin, D., 1998, A Natural Salivary Cysteine Protease Inhibitor,
Inhibits Coronavirus Replication at its Physiologic Concentration. Oral
Microbiology and Immunology, 13(1), 59–61, https://doi.org/10.1111/j.1399-302x.1998.tb00753.x
[28].
Dawes, C., Pedersen, A.
M., Villa, A., Ekström, J., Proctor, G. B., Vissink, A., Aframian, D., McGowan,
R., Aliko, A., Narayana, N., Sia, Y. W., Joshi, R. K., Jensen, S. B., Kerr, A.
R., & Wolff, A., 2015, The Functions of Human Saliva: A Review Sponsored by
the World Workshop on Oral Medicine VI. Archives of Oral Biology, 60(6),
863–874, https://doi.org/10.1016/j.archoralbio.2015.03.004
[29].
Irmak, M. K., Erdem, U.,
& Kubar, A., 2012, Antiviral Activity of Salivary microRNAs for Ophthalmic
Herpes Zoster. Theoretical Biology and Medical Modelling, 9(1), 21, https://doi.org/10.1186/1742‐4682‐9‐21
[30].
Baghizadeh Fini, M.,
2020, Oral Saliva and COVID-19. Oral Oncology, 108, 104821. https://doi.org/10.1016/j.oraloncology.2020.104821
[31].
Centers for Disease
Control and Prevention Transmission of Coronavirus Disease 2019 (COVID-19). Accessed
18th Mar 2020, Available at: https://www.cdc.gov/coronavirus/2019-ncov/about/transmission.html
[32].
To, K. K., Tsang, O. T.,
Yip, C. C., Chan, K. H., Wu, T. C., Chan, J. M., Leung, W. S., Chik, T. S.,
Choi, C. Y., Kandamby, D. H., Lung, D. C., Tam, A. R., Poon, R. W., Fung, A.
Y., Hung, I. F., Cheng, V. C., Chan, J. F., & Yuen, K. Y., 2020, Consistent
Detection of 2019 Novel Coronavirus in Saliva. Clinical Infectious Diseases: An
Official Publication of the Infectious Diseases Society of America, 71(15),
841–843. https://doi.org/10.1093/cid/ciaa149
[33].
Hong, K. H., Lee, S. W.,
Kim, T. S., Huh, H. J., Lee, J., Kim, S. Y., Park, J. S., Kim, G. J., Sung, H.,
Roh, K. H., Kim, J. S., Kim, H. S., Lee, S. T., Seong, M. W., Ryoo, N., Lee,
H., Kwon, K. C., & Yoo, C. K., 2020, Guidelines for Laboratory Diagnosis of
Coronavirus Disease 2019 (COVID-19) in Korea. Annals of Laboratory Medicine,
40(5), 351–360. https://doi.org/10.3343/alm.2020.40.5.351
[34].
Ng, K., Poon, B. H.,
Kiat Puar, T. H., Shan Quah, J. L., Loh, W. J., Wong, Y. J., Tan, T. Y., &
Raghuram, J., 2020, COVID-19 and the Risk to Health Care Workers: A Case
Report. Annals of Internal Medicine, 172(11), 766–767. https://doi.org/10.7326/L20-0175
[35].
Chojnowska, S., Baran,
T., Wilińska, I., Sienicka, P., Cabaj-Wiater, I., & Knaś, M., 2018, Human Saliva
as a Diagnostic Material. Advances in Medical Sciences, 63(1), 185–191, https://doi.org/10.1016/j.advms.2017.11.002
[36].
To, K. K., Tsang, O. T.,
Yip, C. C., Chan, K. H., Wu, T. C., Chan, J. M., Leung, W. S., Chik, T. S.,
Choi, C. Y., Kandamby, D. H., Lung, D. C., Tam, A. R., Poon, R. W., Fung, A.
Y., Hung, I. F., Cheng, V. C., Chan, J. F., & Yuen, K. Y., 2020, Consistent
Detection of 2019 Novel Coronavirus in Saliva. Clinical Infectious Diseases: An
Official Publication of the Infectious Diseases Society of America, 71(15),
841–843. https://doi.org/10.1093/cid/ciaa149
[37].
To, K. K., Tsang, O. T.,
Leung, W. S., Tam, A. R., Wu, T. C., Lung, D. C., Yip, C. C., Cai, J. P., Chan,
J. M., Chik, T. S., Lau, D. P., Choi, C. Y., Chen, L. L., Chan, W. M., Chan, K.
H., Ip, J. D., Ng, A. C., Poon, R. W., Luo, C. T., Cheng, V. C., Yuen, K. Y.,
2020, Temporal Profiles of Viral Load in Posterior Oropharyngeal Saliva Samples
and Serum Antibody Responses During Infection by SARS-CoV-2: An Observational
Cohort Study. The Lancet. Infectious diseases, 20(5), 565–574, https://doi.org/10.1016/S1473-3099(20)30196-1
[38].
Azzi, L., Carcano, G.,
Gianfagna, F., Grossi, P., Gasperina, D. D., Genoni, A., Fasano, M., Sessa, F.,
Tettamanti, L., Carinci, F., Maurino, V., Rossi, A., Tagliabue, A., & Baj,
A., 2020, Saliva is a Reliable Tool to Detect SARS-CoV-2. The Journal of
Infection, 81(1), e45–e50, https://doi.org/10.1016/j.jinf.2020.04.005
[39].
Han, M. S., Seong, M.
W., Heo, E. Y., Park, J. H., Kim, N., Shin, S., Cho, S. I., Park, S. S., &
Choi, E. H., 2020, Sequential Analysis of Viral Load in a Neonate and Her
Mother Infected With Severe Acute Respiratory Syndrome Coronavirus 2. Clinical infectious
diseases : an official publication of the Infectious Diseases Society of
America, 71(16), 2236–2239, https://doi.org/10.1093/cid/ciaa447
[40].
Wan, S., Xiang, Y.,
Fang, W., Zheng, Y., Li, B., Hu, Y., Lang, C., Huang, D., Sun, Q., Xiong, Y.,
Huang, X., Lv, J., Luo, Y., Shen, L., Yang, H., Huang, G., & Yang, R.,
2020, Clinical Features and Treatment of COVID-19 Patients in Northeast
Chongqing. Journal of Medical Virology, 92(7), 797–806, https://doi.org/10.1002/jmv.25783
[41].
Peng, Y. D., Meng, K.,
Guan, H. Q., Leng, L., Zhu, R. R., Wang, B. Y., He, M. A., Cheng, L. X., Huang,
K., & Zeng, Q. T., 2020, Zhonghua Xin Xue Guan Bing Za Zhi, 48(6), 450–455,
https://doi.org/10.3760/cma.j.cn112148-20200220-00105
[42].
Cerón, J. J.,
Martinez-Subiela, S., Ohno, K., & Caldin, M., 2008, A Seven-Point Plan for
Acute Phase Protein Interpretation in Companion Animals. Veterinary Journal
(London, England: 1997), 177(1), 6–7, https://doi.org/10.1016/j.tvjl.2007.12.001
[43].
Wan, S., Yi, Q., Fan,
S., Lv, J., Zhang, X., Guo, L., Lang, C., Xiao, Q., Xiao, K., Yi, Z., Qiang,
M., Xiang, J., Zhang, B., Chen, Y., & Gao, C., 2020, Relationships Among
Lymphocyte Subsets, Cytokines, and the Pulmonary Inflammation Index in
Coronavirus (COVID-19) Infected Patients. British Journal of Haematology,
189(3), 428–437, https://doi.org/10.1111/bjh.16659
[44].
Tvarijonaviciute, A.,
Martinez-Lozano, N., Rios, R., Marcilla de Teruel, M. C., Garaulet, M., and
Cerón, J. J., 2020, Saliva as a Non-Invasive Tool for Assessment of Metabolic
and Inflammatory Biomarkers in Children. Clinical Nutrition (Edinburgh,
Scotland), 39(8), 2471–2478, https://doi.org/10.1016/j.clnu.2019.10.034
[45].
Parra, M. D., Tecles,
F., Martínez-Subiela, S., & Cerón, J. J., 2005, C-Reactive Protein
Measurement in Canine Saliva. Official Publication of the American Association
of Veterinary Laboratory Diagnosticians. Journal of Veterinary Diagnostic
Investigation Inc, 17(2), 139–144. https://doi.org/10.1177/104063870501700207
[46].
Chen, L., Zhao, J., Peng, J., Li, X., Deng, X.,
Geng, Z., Shen, Z., Guo, F., Zhang, Q., Jin, Y., Wang, L., & Wang, S.,
2020, Detection of SARS-CoV-2 in Saliva and Characterization of Oral Symptoms
in COVID-19 patients. Cell proliferation, 53(12), e12923. https://doi.org/10.1111/cpr.12923
[47]. Williams,
E., Bond, K., Zhang, B., Putland, M., & Williamson, D. A., 2020, Saliva as
a Noninvasive Specimen for Detection of SARS-CoV-2. Journal of Clinical
Microbiology, 58(8), e00776-20. https://doi.org/10.1128/JCM.00776-20
[48]. Sagar, S., Ramani, P., Moses, S.,
Gheena, S., & Selvaraj, J., 2024, Correlation of Salivary Cytokine IL-17A
and 1,25 Dihydroxycholecalciferol in Patients Undergoing Orthodontic Treatment.
Odontology, 112(3), 966–975. https://doi.org/10.1007/s10266-023-00890-1
[49]. Alam, M. K., Zaman, M. U., Alqhtani, N. R.,
Alqahtani, A. S., Alqahtani, F., Cicciù, M., & Minervini, G., 2024,
Salivary Biomarkers and Temporomandibular Disorders: A Systematic Review
conducted according to PRISMA guidelines and the Cochrane Handbook for
Systematic Reviews of Interventions. Journal of oral rehabilitation, 51(2),
416–426. https://doi.org/10.1111/joor.13589
[50]. Kritika, S., Mahalaxmi, S., Srinivasan,
N., & Krithikadatta, J., 2023, Deciphering the Role of Saliva in COVID 19:
A Global Cross-Sectional Study on the Knowledge, Awareness and Perception Among
Dentists. BMC Oral Health,23(1), 424.
https://doi.org/10.1186/s12903-023-03152-2

