DOI: 10.21522/TIJPH.2013.12.02.Art035
Authors : Aravind Kumar Subramanian, Niharika Bhatia
Abstract:
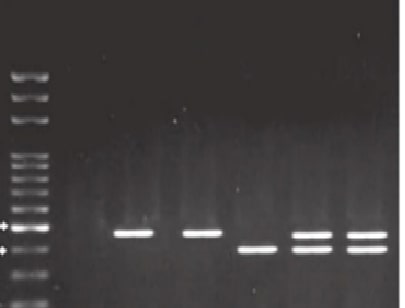
Cleft lip/palate (CL/P) is among the most common congenital anomalies worldwide. This study investigates the association between matrix metalloproteinase 9 (MMP9) gene polymorphism (rs3918242) and nonsyndromic CL/P in an Indian population. The study involved 120 individuals with nonsyndromic CL/P and 140 healthy controls. DNA was extracted from blood samples, and genotyping for MMP9 polymorphisms was performed using polymerase chain reaction (PCR) and restriction fragment length polymorphism (RFLP) techniques with SphI enzymes. Statistical analysis included univariate and multivariate logistic regression models to calculate odds ratios and 95% confidence intervals, with significance set at P<0.05. Results indicated a significant association between MMP9 polymorphism and nonsyndromic CL/P, showing a higher prevalence of the T allele and TT genotype in cases compared to controls. This study suggests a potential link between MMP9 polymorphism and nonsyndromic CL/P in the Indian population, emphasizing the need for further research with larger and more diverse samples to provide more robust evidence. Expanded studies across different ethnic groups are crucial for a deeper understanding of the genetic factors contributing to CL/P.
References:
[1] Soghani, B., Ebadifar, A., Khorram Khorshid, H. R.,
Kamali, K., Hamedi, R., Aghakhani Moghadam, F., 2017, The Study of Association between
Reduced Folate Carrier 1 Polymorphism and Non-Syndromic Cleft Lip/Palate in
Iranian Population. Bioimpacts, Nov 28;7(4):263–8.
[2]
Maragathavalli, G., 2021. Prevalence of Commonest Form
of Cleft Lip in Patients Reported to a University Hospital Setting-A
Retrospective Analysis. International Journal of Pharmaceutical Research
(09752366). Jan 1;13(1). https://openurl.ebsco.com/EPDB%3Agcd%3A9%3A19902537/detailv2?sid=ebsco%3Aplink%3Ascholar&id=ebsco%3Agcd%3A155803083&crl=c
[3] Babu,
H., 2020. Assessment of Association Between Age, Gender, Consanguinity and
Cleft Deformity-A Retrospective Analysis. Int J Dent Oral Sci. Sep
30;48–51. https://www.lcebyhkzz.cn/article/view/2023/5519.pdf
[4] Peng, H. H, Chang, N. C., Chen, K. T., Lu, J. J.,
Chang, P. Y., Chang, S. C., et al., 2016, Nonsynonymous Variants in Myh9 and
Abca4 are the Most Frequent Risk Loci Associated with Nonsyndromic Orofacial
Cleft in Taiwanese Population, BMC Med Genet. Aug 15;17(1):59.
[5] Pendem, S., Chandra, R. B., Selvarasu, K., Krishnan, M., Muthusekhar, M.
R., Preethi, J., 2024. Analysis of Different Facets of the Rule of 10 for Cleft
Lip Repair for Their Application in the Current Era. Cureus. Feb;16(2). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10924625/
[6] Iamaroon, A., Wallon, U. M.,
Overall, C. M., Diewert, V. M., 1996, Expression
of 72-Kda Gelatinase (Matrix Metalloproteinase-2) in the Developing Mouse
Craniofacial Complex, Arch Oral Biol. Dec;41(12):1109–19.
[7] Morris-Wiman, J., Du Y, Brinkley, L., 1999, Occurrence and Temporal Variation in
Matrix Metalloproteinases and their Inhibitors During Murine Secondary Palatal
Morphogenesis, J Craniofac Genet Dev Biol. Oct-Dec;19(4):201–12.
[8] Blavier, L., Lazaryev, A., Groffen, J., Heisterkamp,
N., DeClerck, Y. A., Kaartinen, V., 2001, Tgf-Beta3-Induced Palatogenesis
Requires Matrix Metalloproteinases, Mol Biol Cell. May;12(5):1457–66.
[9] Zhang, B., Henney, A., Eriksson, P., Hamsten, A.,
Watkins, H., Ye, S., 1999, Genetic Variation at the Matrix Metalloproteinase-9
Locus on Chromosome 20q12.2-13.1, Hum Genet, Nov;105(5):418–23.
[10] Menezes-Silva, R., Khaliq, S., Deeley, K., Letra, A.,
Vieira, A. R., 2012, Genetic Susceptibility to Periapical Disease: Conditional
Contribution of Mmp2 and Mmp3 Genes to the Development of Periapical Lesions
and Healing Response, J Endod. May;38(5):604–7.
[11] Price, S. J., Greaves, D. R., Watkins, H., 2001, Identification
of Novel, Functional Genetic Variants in the Human Matrix Metalloproteinase-2
Gene: Role of Sp1 in Allele-Specific Transcriptional Regulation. J Biol
Chem., Mar 9;276(10):7549–58.
[12] Yang, J., Fan, X. H., Guan, Y. Q., Li, Y., Sun, W.,
Yang, X. Z., et al., 2010, MMP-2 Gene Polymorphisms in Type 2 Diabetes Mellitus
Diabetic Retinopathy, Int J Ophthalmol. Jun 18;3(2):137–40.
[13] Pérez-Hernández, N.,
Vargas,-Alarcón G., Martínez-Rodríguez, N.,
Martínez-Ríos, M. A., Peña-Duque, M.
A., Peña-Díaz
A de la., et al., 2012, The Matrix Metalloproteinase 2-1575 Gene Polymorphism
is Associated with the Risk of Developing Myocardial Infarction in Mexican
Patients, J Atheroscler Thromb, Jun 27;19(8):718–27.
[14] Ganapathy, D., Pranati, A. H., 2021. Prevalence of
Cleft Lip: A Retrospective Hospital Based Study. Int J Dentistry Oral Sci.
Jan 29;8(01):1551-4.
https://d1wqtxts1xzle7.cloudfront.net/72459845/IJDOS_2377_8075_08_1051-libre.pdf?1634191418=&response-content-disposition=inline%3B+filename%3DPrevalence_Of_Cleft_Lip_A_Retrospective.pdf&Expires=1719488733&Signature=Kk6nCzWspNS0HQOq87G1sc40tBG0RtzyoemyuvH-zqeMwy6X1bp6UBYppWHmV4U1PuqxngjvMdUZzEQiVSMcnsU2VHC4YgZ6rO99p6Ki5JU6gi4nfB4I5yUp5nmEbtf19uSnu4SVB70u9QqhGCa4ddDnn94Qa5MvowBvhELJM3bPQFCPn26dLJbdxNVgsHCq6-0iR5nek5zUcd9qF5UujwME-dgsrojH1y6w7w5LJdlkbpRpDYT1QYVYunUAv5wjXjjFI-F4F2bcbN2JvUYFzBfRespkK0zio6IGTcCLc0DCiwJy-YZnuLX~VvoFYt-N9yYHMTAsb-GwsjvFS7RLGQ__&Key-Pair-Id=APKAJLOHF5GGSLRBV4ZA.
[15] Jamalvandi, M., Motovali-Bashi, M., Amirmahani, F.,
Darvishi, P., Jamshidi Goharrizi, K., 2018, Association of T/A polymorphism in
miR-1302 binding site in CGA Gene with Male Infertility in Isfahan population. Mol
Biol Rep. Aug;45(4):413–7.
[16] Fatehi, Z., Amirmahani, F.,
Tavassoli, M., 2019, Association Study of TAAAA
Polymorphism in the First Intron of p53 Gene With Risk of Colorectal Cancer in
Iranian Population. Egypt J Med Hum Genet [Internet]. Dec;20(1).
Available from: https://jmhg.springeropen.com/articles/10.1186/s43042-019-0024-3
[17] Smane-Filipova, L., Pilmane, M., Akota, I., 2016,
MMPS and TIMPS Expression in Facial Tissue of Children with Cleft Lip and
Palate, Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub,
Dec;160(4):538–42.
[18] Stetler-Stevenson, W. G., 2008, The Tumor
Microenvironment: Regulation by MMP-Independent Effects of Tissue Inhibitor of
Metalloproteinases-2. Cancer Metastasis Rev. Mar., 27(1):57–66.
[19] Letra, A., Silva, R. A., Menezes, R., Astolfi, C. M.,
Shinohara, A., de Souza, A. P., et al., 2007, MMP Gene Polymorphisms As
Contributors for Cleft Lip/Palate: Association with MMP3 but not MMP1, Arch
Oral Biol. Oct;52(10):954–60.
[20] Letra, A., da Silva, R. A., Menezes, R., de Souza, A.
P., de Almeida, A. L. P. F., Sogayar, M. C., et al., 2007, Studies with MMP9
Gene Promoter Polymorphism and Nonsyndromic Cleft Lip and Palate, Am J Med
Genet A., Jan 1;143A(1):89–91.
[21] Kumari, P., Singh, S. K., Raman, R., 2019, TGFβ3,
MSX1, and MMP3 as Candidates For Nscl±P in an Indian Population., Cleft
Palate Craniofac J., Mar;56(3):363–72.
[22]
Arvind, T. P., Jain, R. K., Nagi, R., Tiwari, A,
Evaluation of Alveolar Bone Microstructure around Impacted Maxillary Canines
using Fractal Analysis in Dravidian Population: A Retrospective CBCT Study.
The Journal of Contemporary Dental Practice. 2022 Sep 23;23(6):593-600