Assessment of Infection Prevention and Control Programs in Some Health Facilities in Cameroon using the World Health Organization Assessment Framework
Abstract:
Healthcare associated
infections (HCAI) remain a global` problem, affecting millions of people
worldwide and accounting for prolonged hospitalization and increased financial
burden. Establishing infection prevention and control (IPC) programs is
effective in reducing the incidence of HCAI, but the status of IPC programs is
not well documented in Cameroon. We assessed the core components of IPC
programs with a focus on HCAI surveillance in some health facilities using the
WHO assessment framework (IPCAF). We carried out a cross-sectional study from
October 2019 to January 2021. Health facilities were chosen purposefully.
Trained data collectors traveled to health facilities and administered the
IPCAF questionnaire to authorities of health facilities. All eight components
of an IPC program were assessed. Data collected was analyzed using Statistic
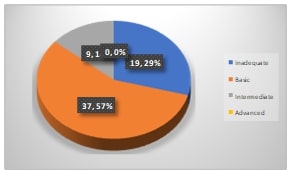
Package for Social Sciences (SPSS 27.0) software. Altogether 65 health
facilities were assessed, 81.5% of which were public facilities. The median
IPCAF score from the health facilities was 275 (Range: 112.5- 595) on a scale
of 800, with most (86%) of them having either an inadequate (29%) or a basic
(57%) IPC status. None of the health facilities attained the advanced IPC
status. HCAI surveillance was the weakest of the eight IPC core components.
Most (89.2%) of the health facilities did not include HCAI surveillance in
their IPC programs. There is therefore need to strengthen IPC programs in
health facilities in Cameroon, with a focus on the surveillance of HCAIs, which
was the weakest core component.
References:
[1] Raoofi, S., Pashazadeh Kan, F., Rafiei, S.,
Hosseinipalangi, Z., Noorani Mejareh, Z., Khani, S., Abdollahi, B., Seyghalani
Talab, F., Sanaei, M., Zarabi, F. and Dolati, Y., 2023. Global prevalence of
nosocomial infection: A systematic review and meta-analysis. PLoS One, 18(1),
p.e0274248.
[2] Allegranzi, B., Nejad, S.B. and Pittet, D.,
2017. The Burden of Healthcare‐Associated Infection. Hand hygiene: a handbook
for medical professionals, pp.1-7.
[3] Allegranzi, B., Nejad, S.B., Combescure,
C., Graafmans, W., Attar, H., Donaldson, L. and Pittet, D., 2011. Burden of
endemic health-care-associated infection in developing countries: systematic
review and meta-analysis. The Lancet, 377(9761), pp.228-241.
[4] Nejad, S.B., Allegranzi, B., Syed, S.B.,
Ellis, B. and Pittet, D., 2011. Health-care-associated infection in Africa: a
systematic review. Bulletin of the World Health Organization, 89(10),
pp.757-765.
[5] Nouetchognou, J.S., Ateudjieu, J., Jemea,
B., Mesumbe, E.N. and Mbanya, D., 2016. Surveillance of nosocomial infections
in the yaounde university teaching hospital, Cameroon. BMC Research Notes, 9,
pp.1-8.
[6] Storr, J., Twyman, A., Zingg, W., Damani,
N., Kilpatrick, C., Reilly, J., Price, L., Egger, M., Grayson, M.L., Kelley, E.
and Allegranzi, B., 2017. Core components for effective infection prevention
and control programmes: new WHO evidence-based recommendations. Antimicrobial
Resistance & Infection Control, 6, pp.1-18.
[7] Lukas, S., Hogan, U., Muhirwa, V., Davis,
C., Nyiligira, J., Ogbuagu, O. and Wong, R., 2016. Establishment of a
hospital-acquired infection surveillance system in a teaching hospital in
Rwanda. International Journal of Infection Control, 12(3).
[8] Stone, P.W., Pogorzelska-Maziarz, M.,
Herzig, C.T., Weiner, L.M., Furuya, E.Y., Dick, A. and Larson, E., 2014. State
of infection prevention in US hospitals enrolled in the National Health and
Safety Network. American Journal of Infection Control, 42(2), pp.94-99.
[9] Alrebish, S.A., Yusufoglu, H.S., Alotibi,
R.F., Abdulkhalik, N.S., Ahmed, N.J. and Khan, A.H., 2022, December.
Epidemiology of Healthcare-Associated Infections and Adherence to the HAI
Prevention Strategies. In Healthcare (Vol. 11, No. 1, p. 63). MDPI.
[10] Allegranzi, B. and Pittet, D., 2009. Role
of hand hygiene in healthcare-associated infection prevention. Journal of
hospital infection, 73(4), pp.305-315.
[11] Ilesanmi, O.S., Afolabi, A.A., Akande, A.,
Raji, T. and Mohammed, A., 2021. Infection prevention and control during
COVID-19 pandemic: realities from health care workers in a north central state
in Nigeria. Epidemiology & Infection, 149, p.e15.
[12] Huskins, W.C., Soule, B.M., O'Boyle, C.,
Gulácsi, L., O'Rourke, E.J. and Goldmann, D.A., 1998. Hospital infection
prevention and control: a model for improving the quality of hospital care in
low-and middle-income countries. Infection Control & Hospital Epidemiology,
19(2), pp.125-135.
[13] Barlam, T.F., Cosgrove, S.E., Abbo, L.M.,
MacDougall, C., Schuetz, A.N., Septimus, E.J., Srinivasan, A., Dellit, T.H.,
Falck-Ytter, Y.T., Fishman, N.O. and Hamilton, C.W., 2016. Executive summary:
implementing an antibiotic stewardship program: guidelines by the Infectious
Diseases Society of America and the Society for Healthcare Epidemiology of
America. Clinical Infectious Diseases, 62(10), pp.1197-1202.
[14] Haynes, A.B., Weiser, T.G., Berry, W.R.,
Lipsitz, S.R., Breizat, A.H.S., Dellinger, E.P., Herbosa, T., Joseph, S.,
Kibatala, P.L., Lapitan, M.C.M. and Merry, A.F., 2009. A surgical safety
checklist to reduce morbidity and mortality in a global population. New England
journal of medicine, 360(5), pp.491-499.
[15] Dramowski, A., Whitelaw, A. and Cotton,
M.F., 2016. Assessment of terminal cleaning in pediatric isolation rooms:
Options for low-resource settings. American Journal of Infection Control,
44(12), pp.1558-1564.
[16] Weinshel, K., Dramowski, A., Hajdu, Á.,
Jacob, S., Khanal, B., Zoltán, M., Mougkou, K., Phukan, C., Staneloni, M.I. and
Singh, N., 2015. Gap analysis of infection control practices in low-and
middle-income countries. infection control & hospital epidemiology, 36(10),
pp.1208-1214.
[17] Vilar-Compte, D.,
Camacho-Ortiz, A. and Ponce-de-León, S., 2017. Infection control in limited resources countries:
challenges and priorities. Current infectious disease reports, 19, pp.1-7.
[18] Tomczyk, S., Aghdassi, S., Storr, J.,
Hansen, S., Stewardson, A.J., Bischoff, P., Gastmeier, P. and Allegranzi, B.,
2020. Testing of the WHO Infection Prevention and Control Assessment Framework
at acute healthcare facility level. Journal of Hospital Infection, 105(1),
pp.83-90.
[19] Abraao, L.M., Nogueira-Junior, C., Orlandi,
G.M., Zimmerman, P.A. and Padoveze, M.C., 2022. Infection prevention and
control program assessment tools: A comparative study. American Journal of
Infection Control, 50(10), pp.1162-1170.
[20] Jeong, Y., Joo, H., Bahk, H., Koo, H., Lee,
H. and Kim, K., 2022. A nationwide survey on the implementation of infection
prevention and control components in 1442 hospitals in the Republic of Korea:
comparison to the WHO Infection Prevention and Control Assessment Framework
(IPCAF). Antimicrobial Resistance & Infection Control, 11(1), p.71.
[21] Harun, M.G.D., Anwar, M.M.U., Sumon, S.A.,
Hassan, M.Z., Haque, T., Mah-E-Muneer, S., Rahman, A., Abdullah, S.A.H.M.,
Islam, M.S., Styczynski, A.R. and Kaydos-Daniels, S.C., 2022. Infection
prevention and control in tertiary care hospitals of Bangladesh: results from
WHO infection prevention and control assessment framework (IPCAF).
Antimicrobial Resistance & Infection Control, 11(1), p.125.
[22] Tomczyk, S., Twyman, A., de Kraker, M.E.,
Rehse, A.P.C., Tartari, E., Toledo, J.P., Cassini, A., Pittet, D. and
Allegranzi, B., 2022. The first WHO global survey on infection prevention and
control in health-care facilities. The Lancet Infectious Diseases, 22(6),
pp.845-856.
[23] Abalkhail, A. and Alslamah, T., 2022.
Institutional factors associated with infection prevention and control
practices globally during the infectious pandemics in resource-limited
settings. Vaccines, 10(11), p.1811.
[24] Manchanda, V., Suman, U. and Singh, N.,
2018. Implementing infection prevention and control programs when resources are
limited. Current Treatment Options in Infectious Diseases, 10, pp.28-39.
[25] Sengupta, S., Barman, P. and Lo, J., 2019.
Opportunities to overcome implementation challenges of infection prevention and
control in low-middle income countries. Current Treatment Options in Infectious
Diseases, 11, pp.267-280.
[26] Stempliuk, V., 2018. Surveillance of
Healthcare-Associated Infections in Low-and Middle-Income Countries: From the
Need to a Reality. Current Treatment Options in Infectious Diseases, 10(1),
pp.1-6.

