Sex Differences in Response to Antiretroviral Therapy Among People Living With HIV/Aids Attending Art Clinic in Federal Medical Centre, Abuja
Abstract:
To assess gender differences in response to antiretroviral therapy among
people living with HIV/AIDS attending ART Clinic in Federal Medical Center
(FMC), Abuja. A retrospective cross-sectional study was conducted among 595
HIV-positive adult patients attending HIV clinic in FMC Abuja between January
2021 and December 2022. Data was retrieved from the database of ART Clinic, FMC
Abuja, for patients who have been on TDF/3TC/DTG regimen for at least six
months before viral load testing. A total of 1,150 registered People Living
with HIV Aids (PLWHA) received care between January 2021 and December 2022 in
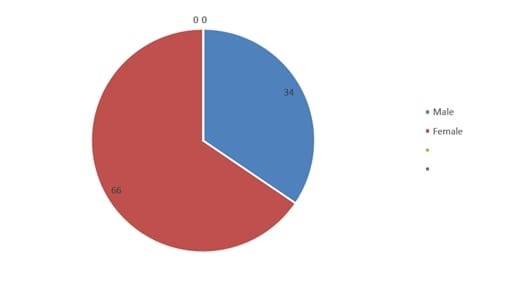
FMC Abuja. Only 595 had viral load test within the study period, comprising of
205 (34%) males and 390 (66%) females in a ratio of 1:1.9. The viral load of
the study participants ranged from 0 to 3,970,000.00 copies/ml with a standard
deviation of 310,099.63 copies/ml. 571 (96%) of the total study participants
had viral load less than 1,000 copies/ml, and 200 (35%) of them were males
whereas 371 (65%) were females. The remaining 24 (4%) of the study participants
who had viral load greater than 1,000 copies/ml were 8 (34%) males and 16 (66%)
females. The differences in the means of viral load between males and females
were not statistically significant, with a p-value of 0.054. This study found a
very high viral suppression and females were equally virally suppressed as the
males.
References:
[1] Kanki P. J, Hopper J. R, Essex M., The
origins of HIV-1 and HTLV-4/HIV-2. Annals of the New York Academy of Sciences.
1987; 511:370-375.
[2] UNAIDS Global Statistics. 2021 [cited May
2022]. Available from: https://www.unaids.org/en/resources/fact-sheet
[3] UNAIDS Press Release Abuja/Geneva 14th March
2019. https:// www.unaids. org/ en/ resou rces/ press centre/ press releaseand
state ntarc hive/2019/ march/ 20190 314_ nigeria. Accessed 22 Jan 2020.
[4] National Agency for the Control of AIDS
(NACA). Nigeria HIV Prevalence Rate. https:// naca. gov. ng/ Nigeria
[5] Gibbs A., 2010, Understandings of gender and
HIV in the South African media. AIDS Care 22
Suppl 2:1620–1628.
[6] Sordo del Castillo L, Ruiz-Pérez I, Olry de
Labry Lima A, Biological, psychosocial, therapeutic and quality of life
inequalities between HIV positive men and women – a review from a gender
perspective. AIDS Rev 2010; 12:113–120.
[7] Mboi, N., 1996, Women and AIDS in south and
South-East Asia: the challenge and the response. World Health Stat Q 49:94–105.
[8] World Health Organization, 2013, Consolidated
Guidelines on the Use of Antiretroviral Drugs for Treating and Preventing HIV
Infection: Recommendations for a Public Health Approach. World Health
Organization, Geneva.
[9] Federal Ministry of Health, 2016, National
Implementation Plan for Scale-Up of Viral Load Testing in Nigeria. Federal
Ministry of Health, Nigeria.
[10] Garcia de la Hera M, Ferreros I, del Amo J,
Garcia de Olalla P, Perez Hoyos S, Muga R, et al., 2004, Gender differences in
progression to AIDS and death from HIV seroconversion in a cohort of injecting
drug users from 1986 to 2001. Journal of Epidemiology and Community Health.
, 58(11):944-950
[11] Kovats S., 2015, Estrogen receptors regulate
innate immune cells and signaling pathways. Cellular Immunology, 294(2):63-69.
[12] Overbaugh J, Bangham C, R., 2001 Selection
forces and constraints on retroviral sequence variation. Science, 292(5519):1106-1109
[13] Carael M, Marais H, Polsky J, Mendoza A., Is
there a gender gap in the HIV response? Evaluating national HIV responses from
the United Nations General Assembly Special Session on HIV/AIDS country
reports. J Acquir Immune Defic Syndr, 2009; 52 Suppl 2:S111–S118.
[14] Tashima, K. T, Hogan, J. W, Gardner, L. I,
Korkontzelou, C, Schoenbaum, E. E, Schuman, P., et al., 2001, A longitudinal
analysis of hospitalization and emergency department use among human
immunodeficiency virus-infected women reporting protease inhibitor use. Clin
Infect Dis, 33:2055–2060.
[15] Carpenter, C. C, Mayer, K. H, Stein, M. D,
Leibman BD, Fisher, A, Fiore, T. C., 1991, Human immunodeficiency virus
infection in North American women: experience with 200 cases and a review of
the literature. Medicine (Baltimore), 60:307–325.
[16] Nicastri E, Angeletti C, Palmisano L, Sarmati
L, Chiesi A, Geraci A, et al., 2005, Gender differences in clinical progression
of HIV-1-infected individuals during long-term highly active antiretroviral
therapy. AIDS. 19(6):577-583.
[17] Minkoff, H. L, Willoughby, A, Mendez, H,
Moroso G, Holman S, Goedert J. J, et al., 1990, l. Seriou’s infections during
pregnancy among women with advanced human immunodeficiency virus infection. Am
J Obstet Gynecol, 162:30-34.
[18] Suba Z., 2020, Prevention and therapy of
COVID-19 via exogenous estrogen treatment for both male and female patients. Journal
of Pharmacy & Pharmaceutical Sciences, 23(1):75-85.
[19] Gandhi M, Bacchetti P, Miotti P, Quinn T. C,
Veronese F, Greenblatt R. M., 2002, Does patient sex affect human
immunodeficiency virus levels? Clinical Infectious Diseases, 35(3):313-322.
[20] Mosha, F., 2021, Gender
Differences in Human Immunodeficiency Virus (HIV) Disease Progression and
Treatment Outcomes. IntechOpen. doi: 10.5772/intechopen.92898.
[21] Hawkins C, Chalamilla G, Okuma J, Spiegelman
D, Hertzmark E, Aris E, et al., 2011, Sex differences in antiretroviral
treatment outcomes among HIV infected adults in an urban Tanzanian setting.
AIDS, 25(9):1189-1197.
[22] Druyts E, Dybul M, Kanters S, Nachega J,
Birungi J, Ford N, et al., 2013, Male sex and the risk of mortality among
individuals enrolled in antiretroviral therapy programs in Africa: A systematic
review and meta-analysis. AIDS, 27(3):417-425.
[23] Onayemi O, Oripelaye M, Afolabi O, and
Olanrewaju O., 2018, The effects of gender on clinical and immunological
response to antiretroviral therapy among people living with HIV in Ile-Ife,
Nigeria. HIV & AIDS Review. International Journal of HIV-Related
Problems, 17(4), 278-282. https://doi.org/10.5114/hivar.2018.80260.
[24] Isaac, E. W., Ajani, A., Difa, A. J., Aremu,
J. T., Oluwaseun, O. C. and Hassan, M.D., 2021, Viral Suppression in Adult
Nigerians in a Regional Antiretroviral Therapy Programme: A Cross Sectional
Descriptive Study. World Journal of AIDS, 11, 1-14. https://doi.org/10.4236/wja.2021.111001.
[25] World Health Organization, 2016, Global
Report on Early Warning Indicators of HIV Drug Resistance. http://www.who.int/hiv/pub/drugresistance/ewi-hivdr-2016/en/
[26] 90-90-90, An Ambitious Treatment Target to Help End the AIDS Epidemic,
UNAIDS, Geneva, Switzerland, 2017, https://www.unaids.org/sites/default/files/media_asset/90-90-90_en.pdf.
[27] Kiweewa, F, Esber, A, Musingye, E, Reed D,
Crowell T. A, Cham F, et al., 2019, HIV virologic failure and its predictors
among HIV-infected adults on antiretroviral therapy in the African Cohort
Study. PLoS One,14:1–16. https:// doi. org/ 10. 1371/ journ al. pone.
02113 44.
[28] Tchouwa, G.T., Eymard-Duvernay, S., Cournil,
A., Lamare, N., Serrano, L., Butel, C., et al., 2018, Nationwide Estimates of
Viral Load Suppression and Acquired HIV Drug Resistance in Cameroon. Clinical
Medicine, 1, 21-27. https://doi.org/10.1016/j.eclinm.2018.06.005.
[29] Ofori-Attah P, Ameke L. S, Obirikorang, C,
Orish, V. N, Kpene, G. E, Agboli, E, et al, 2020, Viral suppression and its
associated factors in HIV patients on highly active antiretroviral therapy
(HAART): a retrospective study in the Ho Municipality, Ghana. AIDS Res Treat,
1–7.
[30] Desta, A. A, Tewolde, W. W, Futwi, N,
Gebrecherkos, T. G, Goyitom, G. G, Asfawosen, A. B, et al., 2020, HIV
virological non-suppression and factors associated with non-suppression among
adolescents and adults on antiretroviral therapy in northern Ethiopia: a
retrospective study. BMC Infect Dis., 20:1–10.
[31] Ssemwanga D, Asio J, Watera C, Nannyonjo M,
Nassolo F, Lunkuse S, et al., 2020, Prevalence of viral load suppression,
predictors of virological failure and patterns of HIV drug resistance after 12
and 48 months on first-line antiretroviral therapy: a national cross-sectional
survey in Uganda. J Antimicrob Chemother, 75(5):1280–9. https://
doi.org/ 10. 1093/ jac/dkz561
[32] Cornell, M., Schomaker, M., Garone, D. B.,
Giddy, J., Hoffmann, C. J., Lessells, R., et al., 2012, Gender Differences in
Survival among Adult Patients Starting Antiretroviral Therapy in South Africa:
A Multicentre Cohort Study. PLoS Medicine, 9, e1001304. https://doi.org/10.1371/journal.pmed.1001304.
[33] De Beaudrap, P., Thiam, M., Diouf, A.,
Toure-Kane, C., Ngom-Gueye, N.F., Vidal, N., et al., 2013, Risk of Virological
Failure and Drug Resistance during First and Second-Line Antiretroviral Therapy
in a 10-Year Cohort in Senegal: Results from the ANRS 1215 Cohort. Journal
of Acquired Immune Deficiency Syndromes, 62, 381-387. https://doi.org/10.1097/QAI.0b013e31827a2a7a
[34] Datay, M. I., Boulle, A., Mant, D. and
Yudkin, P., 2010, Associations with Virologic Treatment Failure in Adults on
Antiretroviral Therapy in South Africa. Journal of Acquired Immune
Deficiency Syndromes, 54, 489-495. https://doi.org/10.1097/QAI.0b013e3181d91788.
[35] Abioye, A. I., Soipe, A. I., Salako, A. A.,
Odesanya, M. O., Okuneye, T. A., Abioye, A. I., et al., 2015, Are There
Differences in Disease Progression and Mortality among Male and Female HIV
Patients on Antiretroviral Therapy? A Meta-Analysis of Observational Cohorts. AIDS
Care, 27, 1468-1486. https://doi.org/10.1080/09540121.2015.1114994
[36] Beckham, S. W., Beyrer, C., Luckow, P.,
Doherty, M., Negussie, E. K. and Baral, S. D., 2016, Marked Sex Differences in
All-Cause Mortality on Antiretroviral Therapy in Low- and Middle-Income
Countries: A Systematic Review and Meta-Analysis. Journal of the
International AIDS Society, 19, Article ID: 21106. https://doi.org/10.7448/IAS.19.1.21106
[37] Sunkanmi F, Paul Y, Peter D, Nsikan A, Joseph J, Opada E, et al. Factors influencing viral load non-suppression among people living with HIV (PLHIV) in Borno State, Nigeria: a case of Umaru Shehu Ultra-Modern Hospital. J Adv Med Res. 2020; 32:98–105.

