Comparative Assessment of Health Status and Health-Seeking Behaviour of Household Heads in Rural and Urban Areas of Abia State, Nigeria
Abstract:
Health status of a nation is closely linked
to the health seeking behavior and its economic growth. Therefore, this study aims
to examine the health status and health-seeking behaviour of household heads in
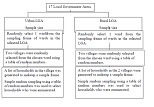
urban and rural areas of Abia State, Nigeria using a mixed model approach. An analytical
cross-sectional study design was employed where the quantitative data was collected
using a structured questionnaire to compare the health status and health-seeking
behaviour of urban (n=450) and rural household heads (n=447). For the qualitative
arm of the study, data was collected through focus group discussions using an interview
guide. The results show that a significantly higher percentage of rural household
heads (10.3%) perceive their health status as ‘very good’ compared to their urban
counterparts (4.2%), p-value <0.05. Additionally, urban household heads reported
a higher incidence of illness (85.2% vs. 36.2%), where malaria (70.9% vs. 9.9%)
and typhoid (34.3% vs. 4.3%)ranked highest. Regarding their health seeking behavior,
urban household heads were first sought care from to private hospitals (n=102, 26.6%)
followed by chemist shops (n=212, 55.2%), while their rural counterpart first sought
treatment from primary health centres. To conclude, these findings suggest that
although urban household heads have seemingly better health-seeking behaviour than
the rural, the effect of urbanization has negatively affected their health status.
Therefore, more concerted efforts should be geared at designing health promotion
campaigns to improve the health status of the population whilst addressing barriers
to seeking health care such as financial constraint and cost of transportation.
References:
[1] Sujatha,
V., 2017, What Is the Sociology behind Health Status and Health-seeking Behaviour?
Sociological Bulletin, 66(3), 286–301. Available at: https://doi.org/10.1177/0038022917727076.
[2] CDC, Health Status - Health, United States, Date of
access: 06/01/2024. Available at: https://www.cdc.gov/nchs/hus/topics/health-status.htm.
[3] Latunji,
O.O. and Akinyemi, O.O., 2018, Factors influencing health-seeking behaviour among
civil servants in Ibadan, Nigeria. Annals of Ibadan Postgraduate Medicine,
16(1), 52–60. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6143883/.
[4] Adam, V.Y.
and Aigbokhaode, A.Q., 2018, Sociodemographic factors associated with the healthcare-seeking
behavior of heads of households in a rural community in Southern Nigeria. Sahel Medical Journal, 21(1), 31–36. Available
at: https://www.smjonline.org/article.asp?issn=1118-8561;year=2018;volume=21;issue=1;spage=31;epage=36;aulast=Adam
[5] Bamgboye,
Elijah A., Odutsote, T., Olusanmi, I. et al., 2020, A comparison of male
and female-headed households of orphans and vulnerable children in Nigeria. Journal
of Public Health and Epidemiology, 12(3), 193–201. Available at: https://doi.org/10.5897/JPHE2019.1177.
[6] Oberoi,
S., Chaudhary, N., Patnaik, S. et al., 2016, Understanding health-seeking
behaviour, Journal of Family Medicine and Primary Care, 5(2), 463–464. Available
at: https://doi.org/10.4103/2249-4863.192376.
[7] Van Der
Hoeven, M., Kruger, A. and Greeff, M., 2012, Differences in health care seeking
behaviour between rural and urban communities in South Africa. International
Journal for Equity in Health, 11(1), 31. Available at: https://doi.org/10.1186/1475-9276-11-31.
[8] Onyeonoro,
U.U., Ogah, O. S., Ukegbu A. U. et al., 2016, Urban–Rural Differences in
Health-Care-Seeking Pattern of Residents of Abia State, Nigeria, and the Implication
in the Control of NCDs. Health Services Insights, 9, 29–36. Available at:
https://doi.org/10.4137/HSI.S31865.
[9] Adam, V.Y.
and Aigbokhaode, A.Q., 2015, Healthcare seeking behaviour of heads of households
in an urban community in south-south Nigeria. Annals of Biomedical Sciences,
14(1), 121–130. Available at: https://www.ajol.info/index.php/abs/article/view/113747.
[10] Onwujekwe, O., Onoka, C., Uguru, N., Nnenna, T., Uzochukwu, B.,
Eze, S., Kirigia, J., and Petu, A., 2010,
Preferences for benefit packages for community-based health insurance: an exploratory
study in Nigeria. BMC Health Services Research, 10, 162. Retrieved
from: https://doi.org/10.1186/1472-6963-10-162.
[11] Usman A.,2013, Preferred Mode of Payments for Community-Based
Health Care Financing Scheme among Households in Osun State, Southwestern Nigeria.
Journal of Natural Science Research.3(1).
[12] Akinyemi,
K.O., Oyefolu, A. O, Mutiu, W. B. et al., 2018, Typhoid Fever: Tracking the
Trend in Nigeria. The American Journal of Tropical Medicine and Hygiene,
99(3 Suppl), 41. Available at: https://doi.org/10.4269/ajtmh.18-0045.
[13] De Silva,
P.M. and Marshall, J.M., 2012, Factors Contributing to Urban Malaria Transmission
in Sub-Saharan Africa: A Systematic Review. Journal of Tropical Medicine,
2012, e819563. Available at: https://doi.org/10.1155/2012/819563.
[14] Brenyah,
R.C., Osakunor, D.N.M. and Ephraim, R.K.D., 2013, Factors influencing urban malaria:
a comparative study of two communities in the Accra Metropolis. African Health
Sciences, 13(4), 992. Available at: https://doi.org/10.4314/ahs.v13i4.19.
[15] Mainous,
A.G. and Kohrs, F.P., 1995, A comparison of health status between rural and urban
adults. Journal of Community Health, 20(5), 423–431. Available at: https://doi.org/10.1007/BF02260438.
[16] Onwujekwe,
O. Chukwuogo, O., Ezeoke, U. O. et al., 2011, Asking people directly about
preferred health-seeking behaviour yields invalid response: an experiment in south-east
Nigeria. Journal of Public Health, 33(1), 93–100. Available at: https://doi.org/10.1093/pubmed/fdq065.
[17] Sambo, M.,
Ejembi, C.I., Adamu, Y.M. et al., 2005, Out-of-pocket health expenditure
for under-five illnesses in a semi-urban community in Northern Nigeria. Journal
of Community Medicine and Primary Health Care, 16(1), 29–32. Available at: https://doi.org/10.4314/jcmphc.v16i1.32404.
[18] Brieger,
W.R. Osamor, P.E., Salami, K.K. et al., 2004, Interactions between patent
medicine vendors and customers in urban and rural Nigeria. Health Policy and
Planning, 19(3), 177–182. Available at: https://doi.org/10.1093/heapol/czh021.
[19] Uzochukwu,
B.S.C., Onwujekwe, E., Onoka, C. et al., 2008, Rural-Urban Differences in
Maternal Responses to Childhood Fever in South East Nigeria. PLOS ONE, 3(3),
e1788. Available at: https://doi.org/10.1371/journal.pone.0001788.
[20] Jordan,
H., Roderick, P., Onoka, C. et al., 2004, Distance, rurality and the need
for care: access to health services in South West England. International Journal
of Health Geographics, 3(1), 21. Available at: https://doi.org/10.1186/1476-072X-3-21.
[21] Oldenburg,
C.E., Sie, A., Ouattara, M. et al., 2021, Distance to primary care facilities
and healthcare utilization for preschool children in rural northwestern Burkina
Faso: results from a surveillance cohort. BMC Health Services Research, 21(1),
212. Available at: https://doi.org/10.1186/s12913-021-06226-5.
[22] Shao, Q.,
Tao, R. and Luca, M.M., 2022, The Effect of Urbanization on Health Care Expenditure:
Evidence From China. Frontiers in Public Health, 10, 850872. Available at:
https://doi.org/10.3389/fpubh.2022.850872.
Ibirongbe, D., Durowade, D.O., Ibirongbe, A. T. et al., 2022, Health Care Financing and Financial Hardship among Rural and Urban Households in Ekiti State, Nigeria. Journal of Community Medicine and Primary Health Care, 34(3), 126–139. Available at: https://doi.org/10.4314/jcmphc.v34i3.10

