Prevalence and Factors Associated with Covid-19 Infection and Mortality Among Frontline Healthcare Workers in Kaduna State
Abstract:
This
study in Kaduna State, Nigeria, examined the prevalence, and factors as associated
with COVID-19 infection and mortality among frontline healthcare workers (HCWs)
in a descriptive, cross- sectional study, where data of HCWs from secondary
source, Surveillance Outbreak Response Management and Analysis System (SORMAS),
was exported to Microsoft excel and evaluated using SPSS version 26 to provide
a snapshot of the vaccine uptake among HCWs in Kaduna state. The study
population were all healthcare workers in Kaduna State, Nigeria that were
tested for COVID-19 from the onset of the pandemic in Kaduna to 29th August
2022. The consents of all persons were obtained prior to testing data upload to
the electronic platform of SORMAS. Prevalence of COVID-19 infection was notably
higher pre-vaccination (12%) but dropped to 5.9% post-vaccination, showcasing
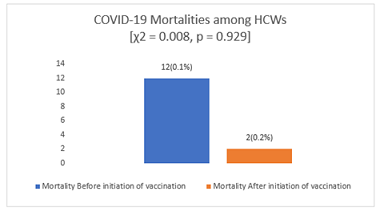
the vaccine’s effectiveness in reducing HCW infections. However,
COVID-19-related mortality rates remained relatively consistent, irrespective
of vaccination status. Demographics played a role in infection risk. Female
HCWs, urban dwellers, and those with higher education levels faced elevated
infection risks. Additionally, close contacts with probable COVID-19 cases
increased infection likelihood. Concerning mortality, males experienced more
COVID-19-related deaths, but no significant links were found with age,
residential area, or contact history. Symptoms significantly associated with
COVID-19 infection included fever, abdominal pain, cough, sore throat, loss of
taste, and loss of smell. The prevalence of COVID-19 infection among the HCWs
was higher before the COVID-19 vaccination was introduced (12%) compared to
after the vaccine was introduced in Kaduna State. These findings offer valuable
insights into the pandemic’s impact on frontline workers in Nigeria’s Kaduna
State.
References:
[1] Poudel K, Subedi P. Impact of COVID-19 pandemic on
socioeconomic and mental health aspects in Nepal. Int J Soc Psychiatry. 2020;66(8):748–55.
[2] Tong X, Ning M, Huang R, Jia B, Yan X, Xiong Y, et
al. Surveillance of SARS-CoV-2 infection among frontline health care workers in
Wuhan during COVID-19 outbreak. Immunity, Inflamm Dis. 2020;8(4):840–3.
[3] Abdel Wahed WY, Hefzy EM, Ahmed MI, Hamed NS.
Assessment of Knowledge, Attitudes, and Perception of Health Care Workers
Regarding COVID-19, A Cross-Sectional Study from Egypt. J Community Health
[Internet]. 2020;45(6):1242–51. Available from: https://doi.org/10.1007/s10900-020-00882-0.
[4] Htay MNN, Marzo RR, Bahari R, AlRifai A, Kamberi F,
El-Abasiri RA, et al. How healthcare workers are coping with mental health
challenges during COVID-19 pandemic? -A cross-sectional multi-countries study. Clin
Epidemiol Glob Heal. 2021;11:100759.
[5] World Health Organization. The impact of COVID-19 on
health and care workers: a closer look at deaths. Health Workforce Department -
Working Paper 1. Geneva; 2021.
[6] Organization WH. Joint WHO/ILO policy guidelines on
improving health worker access to prevention, treatment and care services for
HIV and TB. 2010.
[7] Wu Z, McGoogan JM. Characteristics of and Important
Lessons from the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary
of a Report of 72314 Cases from the Chinese Center for Disease Control and
Prevention. JAMA - J Am Med Assoc. 2020;323(13):1239–42.
[8] Peckham H, de Gruijter NM, Raine C, Radziszewska A,
Ciurtin C, Wedderburn LR, et al. Male sex identified by global COVID-19
meta-analysis as a risk factor for death and ITU admission. Nat Commun.
2020;11(1):1–10.
[9] Mariam Saleh. • Africa: COVID-19 vaccination rate by
country [Internet]. 2022 [cited 2022 Jul 2]. p. 1–2. Available from: https://www.statista.com/statistics/1221298/covid-19-vaccination-rate-in-african-countries/.
[10] Organization WH. WHO Regional Committee for
South-East Asia: Report of the Seventy-third session, Thailand (Virtual), 9-10
September 2020. World Health Organization. Regional Office for South-East Asia;
2021.
[11] Commission NP. Priority table, volume four:
Population distribution by age and sex. Natl Popul Comm Abuja. 2010.
[12] Stephen RI, Olumoh J, Tyndall J, Adegboye O. Risk
Factors for COVID-19 Infection among Healthcare Workers in North-East Nigeria.
Healthc. 2022;10(10).
[13] Alasia DD, Maduka O. Prevalence and Pattern of
COVID-19 among Healthcare Workers in Rivers State Nigeria. Occup Dis Environ
Med. 2021;09(01):20–32.
[14] Alajmi J, Jeremijenko AM, Abraham JC, Alishaq M,
Concepcion EG, Butt AA, et al. COVID-19 infection among healthcare workers in a
national healthcare system: The Qatar experience. Int J Infect Dis. 2020;100:386–9.
[15] The Centers for Disease Control and Prevention.
Characteristics of Health Care Personnel with COVID-19 —. MMWR Morb Mortal
Wkly Rep. 2020;69(15):477–81.
[16] Dzinamarira T, Nkambule SJ, Hlongwa M, Mhango M,
Iradukunda PG, Chitungo I, et al. Risk Factors for COVID-19 Infection Among
Healthcare Workers. A First Report from a Living Systematic Review and
meta-Analysis. Saf Health Work. 2022;13(3):263–8.
[17] Soegiarto G, Purnomosari D, Wulandari L, Mahdi BA,
Fahmita KD, Hadmoko ST, et al. Incidence of SARS-CoV-2 infection in hospital
workers before and after vaccination programme in East Java, Indonesia–A
retrospective cohort study. Lancet Reg Heal - Southeast Asia. 2023;10(December
2022):100130.
[18] Elsayed MEG, El-Abasiri RA, Marzo RR, Dardeer KT,
Kamal MA, Abdelaziz H, et al. Mental health, risk perception, and coping
strategies among healthcare workers in Egypt during the COVID-19 pandemic. PLoS
One. 2023;18(2):e0282264.
[19] Marzo RR, ElSherif M, Abdullah MSAM Bin, Thew HZ,
Chong C, Soh SY, et al. Demographic and work-related factors associated with
burnout, resilience, and quality of life among healthcare workers during the
COVID-19 pandemic: A cross sectional study from Malaysia. Front Public Heal.
2022;10:1021495.
[20] Marzo RR, Khaled Y, ElSherif M, Abdullah MSAM Bin,
Zhu Thew H, Chong C, et al. Burnout, resilience and the quality of life among
Malaysian healthcare workers during the COVID-19 pandemic. Front Public
Heal. 2022;10:1021497.
[21] Hwaij RA, Ghrayeb F, Marzo RR, AlRifai A.
Palestinian healthcare workers mental health challenges during COVID-19
pandemic: a cross-sectional study. Med Res Arch. 2022;10(10).
[22] RilleraMarzo R, Villanueva Iii EQ, Chandra U, Htay
MNN, Shrestha R, Shrestha S. Risk perception, mental health impacts and coping
strategies during COVID-19 pandemic among Filipino healthcare workers. J
Public health Res. 2021;10(2_suppl):jphr-2021.
[23] Kamberi F, Sinaj E, Jaho J, Subashi B, Sinanaj G,
Jaupaj K, et al. Impact of COVID-19 pandemic on mental health, risk perception
and coping strategies among health care workers in Albania-evidence that needs
attention. Clin Epidemiol Glob Heal. 2021;12:100824.
[24] Htay MNN, Marzo RR, AlRifai A, Kamberi F, El-Abasiri
RA, Nyamache JM, et al. Immediate impact of COVID-19 on mental health and its
associated factors among healthcare workers: A global perspective across 31
countries. J Glob Health. 2020;10(2).
[25] Chandan S, Khan SR, Deliwala S, Mohan BP, Ramai D,
Chandan OC, et al. Postvaccination SARS‐CoV‐2 infection among healthcare
workers – A Systematic Review and meta‐analysis. J Med Virol. 2021;1–14.
[26] Bruxvoort KJ, Sy LS, Qian L, Ackerson BK, Luo Y, Lee
GS, et al. Effectiveness of mRNA-1273 against delta, mu, and other emerging
variants of SARS-CoV-2: Test negative case-control study. BMJ.
2021;375:1–10.
[27] Chemaitelly H, Yassine HM, Benslimane FM, Al Khatib
HA, Tang P, Hasan MR, et al. mRNA-1273 COVID-19 vaccine effectiveness against
the B.1.1.7 and B.1.351 variants and severe COVID-19 disease in Qatar. Nat
Med. 2021;27(9):1614–21.
[28] Elimian K, Musah A, King C, Igumbor E, Myles P,
Aderinola O, et al. COVID-19 mortality rate and its associated factors during
the first and second waves in Nigeria. PLOS Glob Public Heal.
2022;2(6):e0000169.
[29] Elimian KO, Ochu CL, Ebhodaghe B, Myles P, Crawford
EE, Igumbor E, et al. Patient characteristics associated with COVID-19
positivity and fatality in Nigeria: Retrospective cohort study. BMJ Open.
2020;10(12):1–16.
[30] Matheson J, Nathan M, Pickard H, Vanino E. Why has
coronavirus affected cities more than rural areas? Economics Observatory. 2020.
[31] Raghupathi V, Raghupathi W. The influence of
education on health: an empirical assessment of OECD countries for the period
1995 – 2015. Arch Public Heal. 2020;78:20.
[32] Abdullah M, Chai P, Chong M, Tohit E, Ramasamy R, Pei C, et al. Gender effect on in vitro lymphocyte subset levels of healthy individuals. Cell Immunol. 2012;272(2):214–9.
[33] Ekawati LL, Arif A, Hidayana I, Nurhasim A, Munziri
MZ, Lestari KD, et al. Mortality among healthcare workers in Indonesia during
18 months of COVID-19. PLOS Glob Public Heal.
2022;2(12):e0000893.

