Health Systems Strengthening: A Panacea to Improving Consumption of Public Healthcare Services in Northern Namibia: A Cross Sectional Study
Abstract:
The aim of the study was to assess the impact of health systems strengthening
on the consumption of public healthcare services in Northern Namibia. The study
assessed how the following components of health systems strengthening influence
the consumption of public health care services; (1) timeliness
and readiness of services rendered, (2) health workforce competence, (3) health
information systems, (4) availability of essential medicines, (5) healthcare financing
and lastly (6) leadership and governance. We used a quantitative descriptive
cross-sectional study design. 672 respondents were identified using the purposive
sampling technique and a well-structured Likert-scaled questionnaire was used for
the interviews. Collected information was entered into data sets and analysis was
done using Excel and Statistical Package for Social Sciences (SPSS) version 23.0
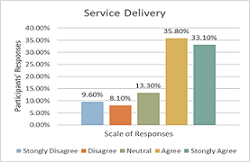
software. The results were that over 95% of
the respondents strongly agreed with each of the factors assessed. Health systems strengthening remains an important
factor in the delivery of health services. This was taken note of when 48% of the
participants agreed that a good competent health workforce determines their choice
of healthcare facility when they are not feeling well. This was further augmented
when 49% of the participants agreed that healthcare financing influences people’s
choice to go and seek healthcare services from government facilities. It was concluded that health systems strengthening
is the cornerstone for improved consumption of public health care services in Northern
Namibia. We recommend that governments should develop strong health systems
at all levels of health service delivery.
References:
[1] Adeoti, A.I and Awoniyi B, (2012). “Determinants of child and maternal health status and demand for health care services in Nigeria”. Editorial express.com/cgibin/conference/download.cgi?db_name=CSAE2012&paper_id=679.
[2] Everybody’s business — Strengthening health systems to improve health outcomes. WHO’s framework for action. Geneva, World Health Organization, 2007 (http://www.who.int/healthsystems/strategy/everybodys_business.pdf, accessed 26 April 2010).
[3] Monitoring and evaluation of health systems
strengthening. An operational framework. Paper prepared by WHO, World Bank, Global
Alliance on Vaccines Initiative (GAVI) and Global Fund to Fight AIDS, Tuberculosis
and Malaria (GFATM) (http://www.who.int/healthinfo/HSS_MandE_framework_Nov_2009.pdf,
accessed 15 June 2010).
[4] World health report 2000. Health systems performance
assessment. Geneva, World Health Organization, 2000(http://www.who.int/whr/2000/en/ndex.html,
accessed 26 April 2010).
[5] Roberts MJ, Hsiao W, Berman P, Reich MR. Getting
health reform right: a guide to improving performance and equity. New York, Oxford
University Press, 2008.
[6] Ghuman, B.S., Mehta Akshat 2005 Health Care
for the Poor in India with Special Reference to Punjab State, Network of Asia-Pacific
Schools and Institutes of Public Administration and Governance (NAPSIPAG) Annual
Conference 2005, Beijing, PRC, 5-7.
[7] International Monetary Fund (2005):
International Monetary Fund Annual Report 2005: Making the Global Economy Work
for All, retrieved from: https://www.imf.org/en/Publications/AREB/Issues/2016/12/31/International-Monetary-Fund-Annual-Report-2005-Making-the-Global-Economy-Work-for-All-18002.
[8] Republic of Kenya (2005). Kibera Social and
Economic Mapping. Household survey Report.
[9] Mwabu G.M., Ainsworth, M., Nyamete, A., (1993).
“Quality of Medical Care and Choice of Medical Treatment in Kenya. An Empirical
Analysis”. Journal of Human Resources 28(4), 283-291.
[10] Kothari, C.R. (2009) Research Methodology: Methods
and Techniques. New Age International, 401 p.
[11] Newing, H. (2011). Conducting Research in Conservation:
Social science methods and practice. Routledge, New York, United States of America.
[12] Castillo, J. J. (2009). Snowball sampling. Retrieved
from Experiment Resources: http://www.experimentresources.com/snowball-sampling.html.
[13] Naing, Lin & Winn, Than & Nordin, Rusli.
(2006). Practical Issues in Calculating the Sample Size for Prevalence Studies.
Archives of Orofacial Sciences. 1.
[14] Lavrakas, Paul. (2008). Encyclopedia of Survey
Research Methods. 10.4135/9781412963947.
[15] Miller, G. J. and Yang, K. (2008). Handbook
of Research Methods in Public Administration. New York: Auerbach Publications,
Taylor & Francis Group Modell, S. (2004) Performance.
[16] Scott, A.J. and Wild, C.J. (1986) Fitting Logistic
Models under Case-Control or Choice Based Sampling. Journal of the Royal Statistical
Society. Series B (Methodological), 48, 170-182. https://doi.org/10.1111/j.2517-6161.1986.tb01400.x.
[17] Advising on Research Methods: A Consultant’s
Companion, by Herman J. Ad`er, Gideon J. Mellenberg hand David J. Hand, Huizen,
Johannesvan Kessel Publishing, 2008, 574pp, ISBN978-9079418-01-5.
[18] Trochim, William M. K. (October 20, 2006).
“Likert Scaling”. Research Methods Knowledge Base, 2nd Edition; Galili, Tal (2010-04-07).
[19] Montgomery, D.C., Peck, E.A. and Vining, G.G.
(2001) Introduction to Linear Regression Analysis. 3rd Edition, Wiley, New York.
[20] Burns, N., and Grove, K. (2003). Understanding
nursing research (3rd ed.). Philadelphia: W.B. Saunders Company.
[21] Yang, K. (2008). Handbook of Research Methods
in Public Administration. Taylor & Francis Group, New York.
[22] Creswell, J. W. (2003). Research design: Qualitative,
quantitative, and mixed methods approach (2nd ed.). Thousand Oaks, CA: Sage.
[23] Book Review Research Methods in Education (6th
Edition) by Louis Cohen, Lawrence Manion and Keith Morrison 656 pp, Routledge, London,
UK, 2007; ISBN 0-415-36878-2.
[24] Health Metrics Network framework and standards
for country health information systems. Second edition. Geneva, World Health Organization,
2008 (http://www.who.int/healthmetrics/documents/hmn_framework200803.pdf, accessed
26 April 2010).
[25] Alderman, H. & Gertler, P. (1989). Substitutability
of public and private health care for the treatment of children in Pakistan. Living
Standards Measurement Study Working Paper 57, Washington: The World Bank.
[26] John, G., and Johnson, P. (2002). Research Methods
for Managers, 3rd ed., Sage Publications, London, United Kingdom.
[27] Sapsford, R. and Jupp, V. (2006). Data collection
and analysis. SAGE. pp. 28–. ISBN 978-0-7619-4363-1. Retrieved 2 November 2011.
[28] Schwartz J.B., Akin, J.S., Popkin, P.M. (1980).
“Price and Income Elasticities of Demand for Modern Health Care: the case of Infant
Delivery in the Philippines”. Word Economic Review.2(1):49-76.
[29] Rous, J. J. & Hotchkiss, D. R. (2003). Estimation
of the determinants of household health care expenditures in Nepal with controls
for endogenous illness and provider choice. Health Economics, 12: 431–451.
[30] Marczyk, G., DeMatteo, D., & Festinger,
D. (2005). Essentials of research design and methodology. Hoboken, NJ: John Wiley
& Sons.
[31] Namibia (2020): The Institute for Health
Metrics and Evaluation. Retrieved from: https://www.healthdata.org/namibia: institute
for health metrics and evaluation-Namibia, 2020.

