Perceived Quality of Health Care Provided to Mothers during Immediate Postpartum Period at Health Facilities in Kakamega County, Kenya
Abstract:
Health care workers are essential
in averting the high infant and mortality rates in Kenya. The immediate postpartum
period is a delicate period when the mother and infant's health is in danger with
evidence indicating the majority of deaths occurring during this period. The aim
of the study was to assess mothers' perception
of quality of care during the immediate postpartum period in selected facilities
in Kakamega County in Kenya. Socio-demographic factors, knowledge and health services
provided during the immediate postpartum period were evaluated. A cross-sectional
descriptive study design to collect quantitative data was adopted. Self-administered
questionnaires were utilized to collect data. The study participants were 257 postnatal
mothers who were systematically sampled from facilities within Kakamega County.
Quantitative data was analyzed using SPSS version 21.0. Descriptive statistics were
used to present quantitative data in frequency tables, charts, and graphs. Inferential
statics were done using Chi-Square tests at a 95% confidence interval (p<0.05).
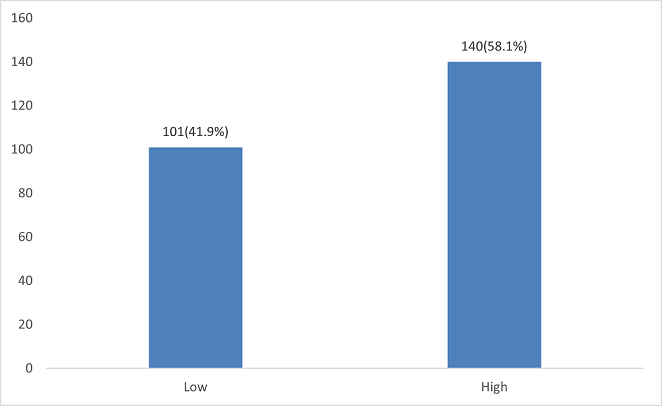
The results revealed majority of the women perceived the quality of postpartum care
as slightly above average at 3.18(63.6%). 58.1% of participants had high knowledge
on immediate postpartum care. Knowledge level (p = 0.018) had a significant association
with the perceived postpartum care quality. Socio-demographic factors such as age
(p=0.014), education (p=0.001), and parity (p=0.029) were associated with the perceived
quality of postpartum care. Availability of family planning (p=0.050),
immunization (p=0.001), and nutritional counseling services (p=0.012) was associated
with the perceived quality of postpartum care. In conclusion the perceived quality
of postpartum care was slightly above average with availability of health services
positively influencing perception.
References:
[1] WHO 2022 Recommendations on Maternal
and Newborn Care for a Positive Postnatal Experience. Accessed on 2nd October 2022
from: https://www.who.int/publications/i/item/9789240045989.
[2] Immigration and Checkpoints Authority
(ICA) (Singapore). Singapore Report on Registration of Births and Deaths 2020. Singapore:
Immigration and Checkpoints Authority (ICA) (Singapore). https://www.ica.gov.sg/docs/default-source/ica/stats/annual-bd-statistics/stats_2021_annual_rbd_report.pdf.
[3] KNBS and ICF. 2023. Kenya Demographic
and Health Survey 2022. Key Indicators Report. Nairobi, Kenya and Rockville, Maryland,
USA: KNBS and ICF. https://dhsprogram.com/pubs/pdf/PR143/PR143.pdf.
[4] WHO Technical Consultation Postpartum
and postnatal care. Managing newborn Problems: a guide for doctors’ nurses and midwives.
Accessed on 28th Jan 2021 on https://www.who.int/publications/i/item/WHO-MPS-10.03.
[5] Richard Scholnik 2022, Maternal and Infant
Mortality Data Factsheet; Ranking of Countries. https://data.worldbank.org/indicator/SP.DYN.IMRT.IN.
[6] UNFPA & Kenyan Ministry of Health
2018, The UNFPA Advocacy Campaign Report to End Preventable Maternal and Newborn
Mortality in Kenya. Accessed on https://kenya.unfpa.org/sites/default/files/pub-pdf/UNFPA%20RMNCAH%20Advocacy%20Campaign%20Assessment%20Summary%5BTo%20Print%5D.pdf.
[7] Ihudiebube-Splendor, C. N., & Chikeme,
P. C, 2020, A descriptive cross-sectional study: Practical and Feasible Design in
investigating Health Care–Seeking Behaviors of Undergraduates. In SAGE Research
Methods Cases: Medicine and Health. SAGE Publications, Ltd., https://dx.doi.org/10.4135/9781529742862.
[8] WHO Programming Strategies for Postpartum
Family Planning 2013: Family planning services, Counseling, Postpartum Period &
Contraception. https://apps.who.int/iris/bitstream/handle/10665/93680/9789241506496_eng.pdf.
[9] Ministry of Health Kenya: National Orientation
Package for Targetted Post Natal Care 2011. http://guidelines.health.go.ke:8000/media/Orientation_Package_for_Targeted_Post_Natal_Care_1.pdf.
[10] Ministry of Health Kenya- National Guidelines
for Quality Obstetric and Perinatal Care http://guidelines.health.go.ke:8000/media/National_Guidelines_for_Quality_Obstetrics_and_Perinatal_Care.pdf.
[11] Ministry of Health Kenya- Emergency Obstetric
and Neonatal Care- A Harmonized Competency Based Training Curriculum for Kenya https://pdf.usaid.gov/pdf_docs/pa00jvxx.pdf.
[12] National Bureau of Statistics-Kenya and
ICF International. 2015. 2014 KDHS Key Findings. Rockville, Maryland, USA: KNBS
and ICF International. https://dhsprogram.com/pubs/pdf/fr308/fr308.pdf, https://www.dhsprogram.com/pubs/pdf/sr227/sr227.pdf.
[13] Wickramasinghe, S.A., Gunathunga, M.W.
& Hemachandra, D.K.N.N 2019. Client perceived quality of the postnatal care
provided by public sector specialized care institutions following a normal vaginal
delivery in Sri Lanka: a cross sectional study. BMC Pregnancy Childbirth 19, 485.
https://doi.org/10.1186/s12884-019-2645-4.
[14] Larson E, Hermosilla S, Kimweri A, Mbaruku
GM, Kruk ME., 2014, Determinants of perceived quality of obstetric care in rural
Tanzania: a cross-sectional study. BMC Health Serv Res. 2014 Oct 18; 14:483. doi:
10.1186/1472-6963-14-483. PMID: 25326007; PMCID: PMC4283093.
[15] Sagawa, J., Kabagenyi, A., Turyasingura,
G. et al., 2021, Determinants of postnatal care service utilization among mothers
of Mangochi district, Malawi: a community-based cross-sectional study. BMC Pregnancy
Childbirth 21, 591. https://doi.org/10.1186/s12884-021-04061-4.
[16] Gabee, Niebyl, Simpson, Landon, Galn,
Jauniaux, Driscoll, Berghella & Grobman, 2017: Obstetrics Normal and Problem
Pregnancies, Seventh Edition, Postpartum care. Elsevier publishers- New York. Pg
467-517.
[17] WHO 2019: Maternal Mortality Fact Sheets.
https://www.who.int/news-room/fact-sheets/detail/maternal-mortality.
[18] World Health Organization. Maternal and
Newborn Health/Safe Motherhood Unit. (1998). Postpartum care of the mother and
newborn: a practical guide: report of a technical working group. World Health Organization.
https://apps.who.int/iris/handle/10665/66439.
[19] Mugyenyi GR, Ngonzi J, Wylie BJ, Haberer
JE, Boatin AA.,2021, Quality of vital sign monitoring during obstetric hospitalizations
at a regional referral and teaching hospital in Uganda: an opportunity for improvement.
Pan Afr Med J. 2021 Mar 11; 38:252. doi: 10.11604/pamj.2021.38.252.21749. PMID:
34104300; PMCID: PMC8164430.
[20] Kairithia Fredrick, Karanja, G. Joseph,
Eunice Cheserem, Kinuthia John, Chege Mwangi, Wamalwa Dalton 2015, Adequacy of vital
signs monitoring post-delivery mothers at the Naivasha District Hospital of Nakuru
County, Kenya. International Journal of Medical and Clinical Sciences, Vol. 2(1):
pp 030-035, January 2015.Copyright © 2014 Spring Journals. FullLength Research Paper
Accessed on 15th July 2021on https://www.springjournals.net/full-articles/springjournals.netijmcsarticleskairithiaetal.,.pdf?view=inline.
[21] Ngare DK, Mutunga JN, 1999, Prevalence
of malnutrition in Kenya. East Africa Medical Journal. 1999 July; 76(7):376-80.
PMID: 10520364.
[22] De Vita, M., Scolfaro, C., Santini, B.
et al, 2019, Malnutrition, morbidity, and infection in the informal settlements
of Nairobi, Kenya: an epidemiological study. Ital J Pediatr 45, 12 (2019). https://doi.org/10.1186/s13052-019-0607-0.
[23] Gudu, E., Obonyo, M., Omballa, V. et
al, 2020, Factors associated with malnutrition in children < 5 years in western
Kenya: a hospital-based unmatched case control study. BMC Nutr 6, 33. https://doi.org/10.1186/s40795-020-00357-4.
[24] Mkoka, D.A., Goicolea, I., Kiwara, A.
et al, 2014, Availability of drugs and medical supplies for emergency obstetric
care: experience of health facility managers in a rural District of Tanzania. BMC
Pregnancy Childbirth 14, 108. https://doi.org/10.1186/1471-2393-14-108.
[25] Pattinson RC, Makin JD, Pillay Y, Van
den Broek N, Moodley J, 2015, Basic and comprehensive emergency obstetric and neonatal
care in 12 South African health districts. S Afr Med J. 2015 Apr; 105(4):256-60.
doi: 10.7196/samj.9181. PMID: 26294861.
[26] Berhane, B., Gebrehiwot H., and Weldemariam,
S. et al. 2019: Quality of basic Emergency obstetric and newborn care (BEmONC) services
from patients’ perspective in Adigrat town, Eastern zone of Tigray, Ethiopia. 2017:
A cross sectional study. BMC Pregnancy Childbirth 19, 190 (2019). https://doi.org/10.1186/s12884-019-2307-6.
[27] Tamirat G, Merga D, Addis E, Bikila B
and Tesfaye A.Y, Ahmadinezhad M, Vizeshfar F, Pakniat A 2022. Mothers' Perceptions
of the Quality of Postnatal Care Provided in Health Centers and the Associated Factors:
A Cross-Sectional Study. International Journal of Community Based Nursing and Midwifery.
2022 Apr; 10(2):110-119. doi:10.30476/IJCBNM.2021.90057.1663. PMID: 35372630; PMCID:
PMC8957657.
[28] Kamau, Immaculate & Mwanza, (2022).
Factors Influencing Delivery of Postnatal Care Education to Mothers Pre-discharge
in health facilities in Nairobi County, Kenya. 10.24105/gjbahs.7.1.1803.
[29] Immaculate Wambui Kamau, K. Njoroge,
Albert Bundi 2016: Adequacy of Postnatal Care Education Given to Mothers Pre-Discharge
in Health Facilities in Nairobi County. European International Journal of Science
and Technology Vol. 15. No: 4. https://www.academia.edu/40590069/.
[30] Charlotte et al. 2018: Opportunities
for African Newborn; Postnatal Care, Chapter 4. New York Publisher – New York. Page
80 – 120.
[31] Jemberia, M.M., Berhe, E.T., Mirkena,
H.B. et al., 2018, Low level of knowledge about neonatal danger signs and its associated
factors among postnatal mothers attending at Woldia general hospital, Ethiopia.
matern health, neonatol and perinatol 4, 5 (2018). https://doi.org/10.1186/s40748-018-0073-5.
[32] Leta M, 2022, Level of knowledge toward
essential newborn care practices among postnatal mothers in governmental hospitals
of Harar Town, Eastern Ethiopia. SAGE Open Med. 2022 Feb 8;
10:20503121221076364. doi: 10.1177/20503121221076364. PMID: 35154740; PMCID: PMC8832633.
[33] Dhingra U, Gittelsohn J, Suleiman AM,
Suleiman SM, Dutta A, Ali SM, Gupta S, Black RE, Sazawal S, 2014, Delivery, immediate
newborn, and cord care practices in Pemba Tanzania: a qualitative study of community,
hospital staff and community level care providers for knowledge, attitudes, belief
systems and practices. BMC Pregnancy Childbirth. 2014 May 22; 14:173. doi: 10.1186/1471-2393-14-173.
PMID: 24885689; PMCID: PMC4049503.
[34] Parashar M, Singh S, Kishore J, Patavegar
BN, 2015, Breastfeeding Attachment and Positioning Technique, Practices, and Knowledge
of Related Issues Among Mothers in a Resettlement Colony of Delhi. ICAN: Infant,
Child, & Adolescent Nutrition. 2015;7(6):317-322. doi:10.1177/1941406415602528.
[35] Megersa, Nega & Gutema, Befikadu
& Bancha, Takalign & Amana, Gizachew & Hajo, Abdo & Kusse, Yisehak
& Zerihun, Eshetu & Aschalew, Zeleke, 2019, Breast Feeding Practice: Positioning
and Attachment during Breast Feeding among Lactating Mothers Visiting Health Facility
in Areka Town, Southern Ethiopia. International Journal of Pediatrics. 2019. 1-6.
10.1155/2019/8969432.

