Etiology, Clinical Manifestations, Diagnosis and Management of Antepartum Hemorrhage in Two Referral Hospitals in Douala-Cameroon
Abstract:
Antepartum hemorrhage certainly has
an easy clinical diagnosis, but it is complex because of its complications and multidisciplinary
treatment. Despite initial care, some patients are still subject to perinatal and
maternal morbidity and mortality. To limit these consequences, our study aims to
identify the etiology, clinical manifestations, diagnosis and management of antepartum
hemorrhage at the Laquintinie Hospital and the General Hospital of Douala in Cameroon.
To achieve this objective, a quantitative descriptive study was conducted from May
1, 2020 to May 1, 2022 and included 166 pregnant women diagnosed with antepartum
hemorrhage in the maternity wards of these hospitals. Data was collected by reviewing
medical records and interviewing mothers using a questionnaire. We used the convenience
sampling technique and the data collected were processed with SPSS 2.3. At the end
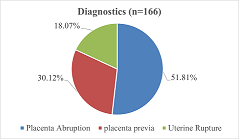
of this analysis, the study showed that the most recurrent cause of antepartum hemorrhage
was placenta abruption (51.81%). The clinical consequence was marked mainly by anemia
(50.60%). Caesarean section was the most common method of management (94.20%). The
results suggest that antepartum hemorrhage is a public health problem.
References:
[1] Amitava R.S.,
Saikat S.R., Biswa jit N., Gaurab M., Jayanta M., 2010, Management of obstetric
haemorrhage. M.E. J. Anaesth. 20(4), 499-508.
[2] Lamina M.A.,
and Oladapo O,T., 2011, Maternal and Fetal Outcome of Obstetric Emergencies in a
Tertiary Health Institution in South Western Nigeria, International Scholarly Research
Network ISRN Obstetrics and Gynecology. Vol.2011, 1-4. Article ID 160932, doi:10.5402/2011/160932
[3] Awat I. H.,
2018, The maternal and perinatal outcome in antepartum hemorrhage: A cross-sectional
study. Zanco J. Med. Sci., 22(2), 155-163, https://doi.org/10.15218/zjms.2018.021.
[4] Singhal S.,
Nymphaea, Nanda S., 2007, Maternal and perinatal outcome in antepartum hemorrhage:
A study at a tertiary care referral institute. The Internet Journal of Gynecology
and Obstetrics, 9(2). https://print.ispub.com/api/0/ispub-article/3465.
[5] Lakshmipriya
K., Vijayalakshmi V., Padmanaban S., 2019, A study of maternal and fetal outcome
in Antepartum haemorrhage. Int J Gynecol Obstet, 3(1), 96–99. doi: 10.33545/gynae.2019.v3.i1b.19.
[6] Green J. R.,
1989, Placental abnormalities: Placenta previa and abruption placenta, Maternal
& fetal medicine. In: Creasy RK, Resnik R editors Principles and Practice 3rd
edition. Philadelphia, WB Saunders,; 588-602.
[7] Sheikh F.,
Khokhar S., Sirichand
P., Shaikh R., 2010, A study of antepartum haemorrhage: Maternal and perinatal
outcomes. Medical
Channel 16. 268-271.
[8] Royal College
of Obstetricians and Gynaecologists, Antepartum Haemorrhage, Green‑top Guideline
No. 63. London: RCOG; 2011.
[9] World Health
Organization, 2019, Trends in maternal mortality: 2000 to 2017: estimates by WHO,
UNICEF, UNFPA, World Bank Group and the United Nations Population Division. Geneva:
Trends in maternal mortality: 2000 to 2017: estimates by WHO, UNICEF, UNFPA, World
Bank Group and the United Nations Population Division, Geneva:
[10] Institut National
de la Statistique (INS et ICF., 2019, Enquête Démographique et de Santé du Cameroun
2018. Indicateurs Clés. Yaoundé, Cameroun, et Rockville, Maryland, USA : INS et
ICF.
[11] Amelia B. and
Andrew N., 2005, Continuing Education in Anaesthesia. Critical Care & Pain 5(6)
183–186, https://doi.org/10.1093/bjaceaccp/mki049.
[12] Radhika M.
G., Annie R., and Ayshath S., 2020, Maternal outcome in antepartum Haemorrhage:
A study at a tertiary care Centre, International Journal of Clinical Obstetrics
and Gynaecology, 4(5): 05-08
[13] Lankoande M.,
Papougnezambo B., Sosthène O., 2017, Incidence and outcome of severe antepartum
hemorrhage at the Teaching Hospital Yalgado Ouédraogo in Burkina Faso, BMC Emergency
Medicine 17:17, 7 pages, doi: 10.1186/s12873-017-0128-3.
[14] Subrata D.,
Ajit R., Bhattacharyya, 2020, A study of risk factors and obstetric outcome of antepartum
haemorrhage in a tertiary care hospital of eastern India; Panacea Journal of Medical
Sciences, 10(3). //doi.org/10.18231/j.pjms.2020.055, , http//www.ipinnovative.com
[15] Majumder S.,
Shah P., Deliwala K.J., Patel R., Madiya A., 2016, Study of foetomaternal outcome
of antepartum haemorrhage in pregnancy. Int J Reprod Contracept Obstet Gynecol,
4(6):1936–1939. doi: 10.1016/j.jece.2016.08.032.
[16] Taylor V. M.,
Peacock S., Kramer M. D., Vaughan T. L., 1995, Increased risk of placenta previa
among women of Asian origin. Obstetrics and Gynecology, 86(5):805-808.
[17] Takai I, U.,
Sayyadi B. M,, Galadanci H. S., 2017, Antepartum hemorrhage: A retrospective analysis
from a northern Nigerian teaching hospital. International Journal of Applied and Basic Medical Research 7(2):112–116.
doi: 10.4103/2229-516x.205819.
[18] Sharmila G.,
and Prasanna., 2016, Maternal and perinatal outcome in antepartum hemorrhage. IAIM;
3(9), 148-160
[19] Ikechebelu
J. I., and Onwusulu D.N., 2007, Placenta praevia: Review of clinical presentation
and management in a Nigerian teaching hospital, Niger J. Med., 16, 61‑64.
[20] Yadav M. C.,
Mehta K., Choudhary V. A., 2019, A study of antepartum hemorrhage and its maternal
and perinatal outcome at tertiary care hospital in Western Rajasthan. JMSCR, 7(9),
80–85.
[21] Park, K. (2007).
Preventive medicine in obstetrics, paediatrics and geriatrics In: Park, textbook
of preventive and social medicine.
19thedition. Banaras Das Bhanot’jabalpur ,445-447.
[22] Youssouf, C.
(2021).Les Hémorragies du 3ème trimestre de la Grossesse au Centre de
Santé de Référence de Kalaban Coro.

