Effect of Access to Immunization Information on Vaccine Acceptance amongst Parents/Caregivers Visiting Health Facilities in Wushishi Local Government Area, Niger State
Abstract:
Globally, vaccines
are the most cost-effective medical intervention to prevent death and disease. The
objectives of this study were to assess the effect of access to immunization information
on vaccine acceptance amongst parents/caregivers visiting the major health facilities
within Wushishi Local Government Area, Niger State. A semi-structured interviewer-administered
questionnaire was used for this study. The result of the study showed a mean age
of respondents was 26.88 years. 96.5% of the respondents were females, 45.5% had
no formal education, 30.7% were unemployed, and 35.5% were of Hausa ethnicity. 65.1%
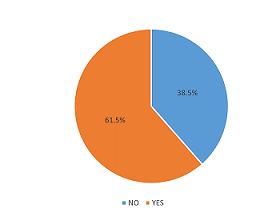
of respondents obtain information on routine immunization within 12 months before
the study. 54.5% had satisfactory knowledge of immunization, while 71.5% exhibited
a favorable attitude toward immunization. The major source of information was health
workers. Those who had access to information were more likely to have good knowledge
of immunization (X62=127.246, DF=1, p=0.001)
and a more favorable attitude towards immunization (X62=14.155,
DF=1, p=0.001). This study has demonstrated that
access to information on immunization greatly affects the knowledge and, consequently,
the attitude of parents toward making a positive decision to accept vaccination.
Efforts should be made to understand the content and effect of information sources
on knowledge and attitudes toward vaccination by relevant stakeholders involved
in the implementation of immunization programs.
References:
[1]
Njidda, U. M. (2017). Assessment
of Parents Knowledge towards the Benefits of Child Immunization in Maiduguri, Borno
State, Nigeria. Nursing & Care Open Access Journal, 3(2). https://doi.org/10.15406/ncoaj.2017.03.00067.
[2]
Feemster, K. A. (2020). Building
vaccine acceptance through communication and advocacy. Human Vaccines and Immunotherapeutics,
16(5), 1004–1006. https://doi.org/10.1080/21645515 .2020.1746603.
[3]
Handy, L. K., Maroudi, S.,
Powell, M., Nfila, B., Moser, C., Japa, I., Monyatsi, N., Tzortzi, E., Kouzeli,
I., Luberti, A., Theodoridou, M., Offit, P., Steenhoff, A., Shea, J. A., & Feemster,
K. A. (2017). The impact of access to immunization information on vaccine acceptance
in three countries. PLoS ONE, 12(8), 1–16. https://doi.org/10.1371/journal.pone.0180759.
[4]
Adebisi, Y. A., Alaran, A.
J., Bolarinwa, O. A., Akande-Sholabi, W., & Lucero-Prisno, D. E. (2021). When
it is available, will we take it? Social media users’ perception of hypothetical
covid-19 vaccine in nigeria. Pan African Medical Journal, 38. https://doi.org/10.11604/pamj.
2021.38.230.27325.
[5]
Zhao, Q., Sun, X., Xie,
F., Chen, B., Wang, L., Hu, L., & Dai, Q. (2021). Impact of COVID-19 on
psychological wellbeing. International Journal of Clinical and Health
Psychology, 21(3), 4–9. https://doi.org/10.1016/j.ijchp.2021.100252.
[6]
Torre, G. La, Scalingi, S.,
Garruto, V., Siclari, M., Chiarini, M., & Mannocci, A. (2017). Knowledge
, Attitude, and Behaviours towards Recommended Vaccinations among Healthcare Workers.
6–8. https://doi.org/10.3390/healthcare5010013.
[7]
Adeyanju, G. C., Sprengholz,
P., Betsch, C., & Essoh, T. A. (2021). Caregivers’ willingness to vaccinate
their children against childhood diseases and human papillomavirus: A cross-sectional
study on vaccine hesitancy in Malawi. Vaccines, 9(11). https://doi.org/10.3390/vaccines9111231.
[8]
Hmr, A., Glenton, C., &
Lewin, S. (2017). qualitative evidence ( Review ). https://doi.org/10.1002/14651858.CD011787.pub2.www.cochranelibrary.com.
[9]
Sondagar, C., Xu, R., MacDonald,
N. E., & Dubé, E. (2020). Vaccine acceptance: How to build and maintain trust
in immunization. Canada Communicable Disease Report, 46(5), 155–159.
https://doi.org/10.14745/ccdr.v46i05a09.
[10]
Obasohan, P. E., Mustapha,
M. A., Makada, A., & Obasohan, D. N. (2018). Evaluating the reasons for partial
and non-immunization of children in Wushishi local government area, Niger state,
Nigeria: Methodological comparison. African Journal of Reproductive Health,
22(4), 113–122. https://doi.org/10.29063/ajrh2018/v22i4.12.
[11]
Hogue, M. D., & Meador,
A. E. (2016). Vaccines and Immunization Practice. Nursing Clinics of North America,
51(1), 121–136. https://doi.org/10.1016/j.cnur.2015.10.005.
[12]
Durán-Méndez, A., Jardínez-Vera,
A. C., Jiménez-Muñoz, E., & Peón, A. N. (2021). A brief history of vaccines
and an overview of their benefits. Revista de La Sociedad Española de Beneficencia,
2(1), 1–6. https://doi.org/10.46295/2:1.vachi
[13]
Filia, A., Bella, A., Ancona,
F. D., Fabiani, M., Giambi, C., Rizzo, C., Ferrara, L., Pascucci, M. G., & Rota,
M. C. (2019). Childhood vaccinations : knowledge , attitudes and practices of paediatricians
and factors associated with their confidence in addressing parental concerns , Italy
, 2016. Eurosurveillance, 24(6). https://doi.org/10.2807/1560-7917.ES.2019.24.6.1800275.
[14]
Taiwo, L., Idris, S., Abubakar,
A., Nguku, P., Nsubuga, P., Gidado, S., Okeke, L., Emiasegen, S., & Waziri,
E. (2017). Factors affecting access to information on routine immunization among
mothers of under 5 children in Kaduna state Nigeria, 2015. Pan African Medical
Journal, 27, 1–8. https://doi.org/10.11604/pamj.2017.27.186.11191.
[15]
Lewandowska, A., Lewandowski,
T., Rudzki, G., & Rudzki, S. (n.d.). Opinions and Knowledge of Parents Regarding
Preventive Vaccinations of Children and Causes of Reluctance toward Preventive Vaccinations.
[16]
Larson Williams, A., Mitrovich,
R., Mwananyanda, L., & Gill, C. (2019). Maternal vaccine knowledge in low- and
middle-income countries—and why it matters. Human Vaccines and Immunotherapeutics,
15(2), 283–286. https://doi.org/10.1080/21645515.2018.1526589.
[17]
Jones, A. M., Omer, S. B.,
Bednarczyk, R. A., Halsey, N. A., Moulton, L. H., & Salmon, D. A. (2012). Parents’
Source of Vaccine Information and Impact on Vaccine Attitudes, Beliefs, and Nonmedical
Exemptions. Advances in Preventive Medicine, 2012 (February 2004),
1–8. https://doi.org/10.1155/2012/932741.
[18]
Adedokun, S. T., Uthman, O.
A., Adekanmbi, V. T., & Wiysonge, C. S. (2017). Incomplete childhood immunization
in Nigeria: A multilevel analysis of individual and contextual factors. BMC Public
Health, 17(1), 1–10. https://doi.org/10.1186/s12889-017-4137-7.
[19]
GebreEyesus, F., Amlak, T.,
Tarekegn, T., Shiferaw, B., Mewahegn, M., Emeria, O., Agerie, A., & Chanie,
D. (2021). Knowledge , Attitude , and Practices of Parents About Immunization of
Infants and Its Associated. Dovepress, 12(223), 223–238. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8121275/pdf/phmt-12-223.pdf
[20]
Sallam, M. (2021). Worldwide
Vaccine Hesitancy. Vaccines, 1–14. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7920465/.

