Self-Prescribed Pharmacological Drugs Used for Covid-19 Prevention and Treatment in the Current Pandemic
Abstract:
The practice of using pharmacological drugs not prescribed by qualified medical
practitioners is a worrying trend especially in the ongoing Covid-19 pandemic. It
is a global issue that has attracted the attention of physicians and various stakeholders
in the health care systems in developing and developed countries. Such practice
is associated with overdosage, allergic reaction, infection resistant to antibiotic,
wrong diagnosis, delay in seeking treatment at health facilities and drug addiction.
This study assessed the prevalence of self-prescribed
antibiotics, analgesics, vitamins, and minerals by a cross section of burgesses
in the Prices Town Regional Corporation (PTRC) in South Trinidad to treat and prevent
Covid-19 infection. A descriptive cross-sectional survey in online and paper
and pencil questionnaire formats was conducted from February 2022 to April 2022
on 286 self-selected participants from a population of 1000 residents. Data entry and analysis conducted after merging them using Google Charts. Prevalence of Ivermectin
was 9.44%, Zithromax 3.15, Steroids 3.5% Panadol 33.6%, Vitamins C 63.3%, Zinc 60.8%,
D3 55.2 %, and B Complex 11.9%. Multivariate
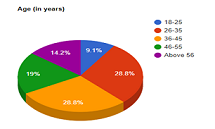
analysis performed on dependent and independent variables showed that the use of
self-prescribed medication was significantly associated with age group 26-35 years
(COR 0.15, p0.00129, 95% CI 0.04, 0.51 at significance level
of p≤0.05) and marital status of being separated from spouses (COR 2.48, p0.0229, 95% CI 1.02, 6.06, significance level of p≤0.05).
More females practiced self-medication compared to males.
The researcher recommends health education to curb the practice.
References:
[1]
Nasir, M., Talha, K. A., Chowdhury, A.S. M.,
Zahan, T., Rawshan, Perveen, R. A. (2020). Prevalence, Pattern and Impact of Self
Medication of Anti-infective Agents During Covid-19 Outbreak in Dhaka City. 10.21203/rs.3.rs-57011/v1.
file:///C:/Users/Fagbola/Downloads/Prevalence_Pattern_and_Impact_of_Self_Medication_o.pdf].
[2]
Sankaranarayanan, R. (2017). Can we classify
cross- sectional studies into analytical studies? Retrieved from: https://www.researchgate.net/post/Dear-all-Can-we-classify-cross-sectional-studies-into-analytical-studies/589dea50eeae39590619ad32/citation/download.
[5]
Wegbom, A. I, Edet, C. K., Raimi, O., Fagbamigbe,
A. F., and Kiri. VA., (2021) Self-Medication Practices and Associated Factors in
the Prevention and/or Treatment of Covid-19 Virus: A Population-Based Survey in
Nigeria. Front. Public Health. https://doi.org/10.3389/fpubh.2021.606801.
[7]
Adebisi, Y.A., Jimoh, N.D., and Ogunkola, I. O. (2021).
The use of antibiotics in Covid-19 management: a rapid review of national treatment
guidelines in 10 African countries. Trop Med Health 49, 51 (2021). https://doi.org/10.1186/s41182-021-00344-w.
[8] Locquet, Médéa; Diep, Anh Nguyet; Beaudart, Charlotte;
Dardenne, Nadia; Brabant, Christian; Bruyère, Olivier; Donneau, A. Françoise. (2021).
A systematic review of prediction models to diagnose Covid-19 in adults admitted
to healthcare centers. Arch Public Health; 79(1): 105, 2021 Jun 18. DOI:
10.1186/s13690-021-00630-3.
[9] Popp,
M., Stegemann, M., Riemer, M., Metzendorf, M-I., Romero, C. S., Mikolajewska, A.,
Kranke, P., Meybohm, P., Skoetz, N., and Weibel, S. (2021). Antibiotics for the
treatment of Covid-19. Cochrane Database of Systematic Reviews 2021, Issue 10. Art.
No.: CD015025. DOI: 10.1002/14651858.CD015025.
[10] Tekeba, A., Ayele, Y., Negash,
B., & Gashaw, T. (2021). Extent of and Factors Associated with Self-Medication
among Clients Visiting Community Pharmacies in the Era of Covid-19: Does It Relieve
the Possible Impact of the Pandemic on the Health-Care System? Risk management
and healthcare policy, 14, 4939–4951. https://doi.org/10.2147/RMHP.S338590.
[11]
Del-Toro-Rubio, M., Bohórquez-Moreno, C., Díaz-Pérez,
A., and Barrios-Puerta, Z. (2020). Factors associated with self-medication in adolescents
in the rural area of Cartagena, Colombia. Arch Med (Manizales) 2020; 20(2):356-363.
https://doi.org/10.30554/archmed.20.2.3697.2020.
[12]
Abdelwahed RNK, Jassem M, Alyousbashi A. Self-Medication Practices,
Prevalence, and Associated Factors among Syrian Adult Patients: A Cross-Sectional
Study. J Environ Public Health. 2022 Jun 28; 2022:9274610. doi: 10.1155/2022/9274610.
PMID: 35800339; PMCID: PMC9256391.
[13] Hughes, C. M., McElnay, J.
C., & Fleming, G. F. (2001). Benefits and risks of self-medication. Drug
safety, 24(14), 1027–1037. https://doi.org/10.2165/00002018-200124140-00002.
[14]
WHO (2000). World Health Organization Guidelines
for the Regu latory Assessment of Medicinal Products for use in Self-Medication.
https://apps.who.int/iris/bitstream/handle/10665/66154/WHO_EDM_QSM_00.1_eng.pdf.
[15] Topinková, E., Baeyens, J.P., Michel,
JP. et al. (2012). Evidence-Based Strategies for the Optimization of Pharmacotherapy
in Older People. Drugs Aging 29, 477–494 (2012). https://doi.org/10.2165/11632400-000000000-00000.
[16] Montastruc, J. L., Bagheri, H., Geraud,
T., & Lapeyre-Mestre, M. (1997). Pharmacovigilance de l’automédication [Pharmacovigilance
of self-medication]. Therapie, 52(2), 105–110. https://pubmed.ncbi.nlm.nih.gov/9231503/.
[17]
Fair, R. J., & Tor, Y. (2014). Antibiotics and bacterial resistance
in the 21st century. Perspectives in medicinal chemistry, 6, 25–64.
https://doi.org/10.4137/PMC.S14459.
[18]Banić Tomišić, Z. (2011).
The Story of Azithromycin. Kemija u industriji/Journal of Chemists and Chemical
Engineers. 60. 603-617. https://www.researchgate.net/publication/286136408_The_Story_of_Azithromycin/citation/download.
[19] Hauk L. (2014). AAP releases guideline
on diagnosis and management of acute bacterial sinusitis in children one to 18 years
of age. American family physician, 89(8), 676–681.https://pubmed.ncbi.nlm.nih.gov/24784128/.
[20] Oldenburg CE, Pinsky BA, Brogdon J,
et al. Effect of Oral Azithromycin vs Placebo on Covid-19 Symptoms in Outpatients
With SARS-CoV-2 Infection: A Randomized Clinical Trial. JAMA. 2021;326(6):490–498.
doi:10.1001/jama.2021.11517. https://jamanetwork.com/journals/jama/fullarticle/2782166.
[21]
Dorobisz, K., Dorobisz, T., Janczak, D., & Zatoński, T. (2021).
Doxycycline in the Coronavirus Disease 2019 Therapy. Therapeutics and clinical
risk management, 17, 1023–1026. https://doi.org/10.2147/TCRM.S314923.
[22] Chivese, T., Omran A.H., Musa, G. H.,
Al-Wattary, N., Badran, S., Soliman, N., Ahmed T.M., Matizanadzo, J., Mohamed M.
M., Thalib, E. L., and Suhail A.R. (2021). Efficacy of chloroquine and hydroxychloroquine
in treating Covid-19 infection: A meta-review of systematic reviews and an updated
meta-analysis, Travel Medicine and Infectious Disease, Volume 43, 2021, 02135, ISSN
1477-8939, https://doi.org/10.1016/j.tmaid.2021.102135.
[26] Caly. L.,
Druce J.D., Catton, M.G., Jans, D.A., Wagstaff, K.M. The FDA-approved drug ivermectin inhibits the replication of SARS-CoV-2 in vitro. Antiviral Research, Volume 178, 2020,104787, ISSN 0166 3542, https://doi.org/10.1016/j.antiviral.2020.104787. (https://www.sciencedirect.com/science/article/pii/S0166354220302011).
[28] Babalola,
O. E., Bode, C. O., Ajayi, A. A., Alakaloko, F. M., Akase, I. E., Otrofanowei, E.,
Adeyemo, A. O., and Omilabu, S. (2021) change to 2022. Ivermectin shows clinical
benefits in mild to moderate covid-19: a randomized controlled double blind dose
response study in Lagos. medRxiv 2021.01.05.21249131; doi: https://doi.org/10.1101/2021.01.21249131.
[29] Baracaldo-Santamaría, D.,
Pabón-Londoño, S., & Rojas-Rodriguez, L. C. (2022). Drug safety of frequently
used drugs and substances for self-medication in Covid-19. Therapeutic advances
in drug safety, 13, 20420986221094141. https://doi.org/10.1177/20420986221094141.
[35]
Manjani, L., Desai, N., Kohli, A., Arya, R., Woods, C., and Desale,
S. (2021). Effects of acetaminophen on outcomes in patients hospitalized with Covid-10.
Presented at: CHEST 2021; October 17-20, 2021; Orlando, FL/Virtual. Abstract A1072.
https://journal.chestnet.org/article/S0012-3692(21)02443-0/fulltext#relatedArticles.
[36]
Sestili P, Fimognari, C. (2020). Paracetamol‐Induced
Glutathione Consumption: Is There a Link with Severe Covid‐19 Illness? Front
Pharmacol. 2020;11: 579944. 10.3389/fphar.2020.579944 https://www.frontiersin.org/articles/10.3389/fphar.2020.579944/full.
[37]
Pandolfi, S., Simonetti, V., Ricevuti, G., & Chirumbolo, S.
(2021). Paracetamol in the home treatment of early Covid-19 symptoms: A possible
foe rather than a friend for elderly patients? Journal of medical virology,
93(10), 5704–5706. https://doi.org/10.1002/jmv.27158.
[38]
Kelleni M. T. (2022). NSAIDs and Kelleni’s protocol as potential
early Covid-19 treatment game changer: could it be the final countdown? Inflammopharmacology,
30(1), 343–348. https://doi.org/10.1007/s10787-021-00896-7.
[39]
Wijaya, I., Andhika, R., Huang, I., Purwiga, A., & Budiman,
K. Y. (2021). The effects of aspirin on the outcome of Covid-19: A systematic review
and meta-analysis. Clinical epidemiology and global health, 12, 100883.
https://doi.org/10.1016/j.cegh.2021.100883.
[40] Voruganti, D., Bassareo, P. P. and Calcaterra, G.
(2022). Does aspirin save lives in patients with Covid-19? Heart 2022;
108:88-89. https://heart.bmj.com/content/108/2/88.citation-tools.
[41]
Mosleh, G., Badr, P., Zaeri, M., & Mohagheghzadeh, A. (2021).
Potentials of Antitussive Traditional Persian Functional Foods for Covid-19 Therapy†.
Frontiers in pharmacology, 12, 624006. https://doi.org/10.3389/fphar.2021.624006.
[42]
Zhang, D. H., Zhang, X., Peng, B., Deng, S. Q., Wang, Y. F., Yang,
L., Zhang, K. Z., Ling, C. Q., & Wu, K. L. (2020). Network pharmacology suggests
biochemical rationale for treating Covid-19 symptoms with a Traditional Chinese
Medicine. Communications biology, 3(1), 466. https://doi.org/10.1038/s42003-020-01190-y.
[43]
Esam Z. (2020). Protective potential of expectorants against Covid-19.
Medical hypotheses, 142, 109844. https://doi.org/10.1016/j.mehy.2020.109844.
[48]
Jurowski, K., Szewczyk, B., Nowak, G., & Piekoszewski, W.
(2014). Biological consequences of zinc deficiency in the pathomechanisms of selected
diseases. Journal of biological inorganic
chemistry: JBIC: a publication of the Society of Biological Inorganic Chemistry,
19(7), 1069–1079. https://doi.org/10.1007/s00775-014-1139-0.
[50] Tan, B., Chew, N., Lee, G., Jing, M.,
Goh, Y., Yeo, L., Zhang, K., Chin, H. K., Ahmad, A., Khan, F. A., Shanmugam, G.
N., Chan, B., Sunny, S., Chandra, B., Ong, J., Paliwal, P. R., Wong, L., Sagayanathan,
R., Chen, J. T., Ng, A., Sharma, V. K. (2020). Psychological Impact of the Covid-19
Pandemic on Health Care Workers in Singapore. Annals of internal medicine,
173(4), 317–320. https://doi.org/10.7326/M20-1083.
[51]
Ragan, I., Hartson,
L., Pidcoke, H., Bowen, R., & Raymond P. (2020). Pathogen reduction of SARS-CoV-2 virus in plasma and whole blood using riboflavin
and UV light. doi: https://doi.org/10.1101/2020.05.03.074971.
[52] Mikkelsen, K., Stojanovska, L., Prakash,
M., & Apostolopoulos, V. (2017). The effects of vitamin B on the immune/cytokine
network and their involvement in depression. Maturitas, 96, 58–71.
https://doi.org/10.1016/j.maturitas.2016.11.012.
[53]
Shakoor, H., Feehan, J., Al Dhaheri, A., Ali,
H., Platat, C., Ismail, L., Apostolopoulos, V., Stojanovska, L. (2020). Immune-boosting
role of vitamins D, C, E, zinc, selenium, and omega-3 fatty acids: Could they help
against Covid-19? Maturitas. 143. 10.1016/j.maturitas.2020.08.003.
[56]
Schlueter, A. K., & Johnston, C. S. (2011). Vitamin C: Overview
and Update. Journal of Evidence-Based Complementary & Alternative Medicine,
49–57. https://doi.org/10.1177/1533210110392951.
[58] Pisoschi, A.M., et al. (2021) Oxidative Stress Mitigation by Antioxidants—An
Overview on Their Chemistry and Influences on Health Status. European Journal of
Medicinal Chemistry, 209, Article ID: 112891. https://doi.org/10.1016/j.ejmech.2020.112891.
[59]
Science, M., Maguire, J. L., Russell, M. L., Smieja, M., Walter,
S. D., & Loeb, M. (2013). Low serum 25-hydroxyvitamin D level and risk of upper
respiratory tract infection in children and adolescents. Clinical infectious
diseases: an official publication of the Infectious Diseases Society of America,
57(3), 392–397. https://doi.org/10.1093/cid/cit289.
[60]
Aglipay, M., Birken, C. S., Parkin, P. C., Loeb, M. B., Thorpe,
K., Chen, Y., Laupacis, A., Mamdani, M., Macarthur, C., Hoch, J. S., Mazzulli, T.,
Maguire, J. L., & TARGet Kids! Collaboration (2017). Effect of High-Dose vs
Standard-Dose Wintertime Vitamin D Supplementation on Viral Upper Respiratory Tract
Infections in Young Healthy Children. JAMA, 318(3), 245–254. https://doi.org/10.1001/jama.2017.8708.
[63]
Olayemi J, Olayinka B, Musa I. (2010). Evaluation
of Antibiotic Self-Medication Pattern Amongst Undergraduate Students of Ahmadu Bello
University (Main Campus), Zaria. Journal Applied Sciences and Engineering Technology,
2(1): 35-38. https://maxwellsci.com/print/rjaset/v2-35-38.pdf.
[65] Amaha. M. H., Alemu, B.M,
and Atomsa, G. E. (2019) Self-medication practice and associated factors among adult
community members of Jigjiga town, Eastern Ethiopia. PLoS ONE 14(6): e0218772. https://doi.org/10.1371/journal.pone.0218772.
[66] Alshammari F, Alobaida A,
Alshammari A, Alharbi A, Alrashidi A, Almansour A, Alremal A and Khan KU (2021)
University Students’ Self-Medication Practices and Pharmacists’ Role: A Cross-Sectional
Survey in Hail, Saudi Arabia. Front. Public Health 9:779107. doi: 10.3389/fpubh.2021.779107.
[67] Zeru N, Fetene D, Geberu
DM, Melesse AW, Atnafu A. Self-Medication (2020): Practice and Associated Factors
Among University of Gondar College of Medicine and Health Sciences Students: A Cross-Sectional
Study. Patient Prefer Adherence. 2020; 14:1779-1790
https://doi.org/10.2147/PPA.S274634.
[68] Makowska, M., Boguszewski,
R., Nowakowski, M., & Podkowińska, M. (2020). Self-Medication-Related Behaviors
and Poland’s Covid-19 Lockdown. International Journal of Environmental Research
and Public Health, 17(22), 8344. MDPI AG. Retrieved from http://dx.doi.org/10.3390/ijerph17228344.
[69] Shaamekhi, H. R., Asghari
Jafarabadi, M., & Alizadeh, M. (2019). Demographic determinants of self-medication
in the population covered by health centers in Tabriz. Health promotion perspectives,
9(3), 181–190. https://doi.org/10.15171/hpp.2019.26.
[70] Demissie, F., Ereso, K.,
& Paulos, G. (2022). Self-Medication Practice with Antibiotics and Its Associated
Factors Among Community of Bule-Hora Town, Southwest Ethiopia. Drug, healthcare,
and patient safety, 14, 9–18. https://doi.org/10.2147/DHPS.S325150.
[71] Bello, I,
B., Akinnawo, E, O., Akpunne, B, O., Mopa-Egbunu, A. (2022). Knowledge of Covid-19
and preventive measures on self-medication practices among Nigerian undergraduates,
Cogent Arts & Humanities, 9:1, 2049480, DOI: 10.1080/23311983.2022.2049480.
https://doi.org/10.1080/23311983.2022.2049480.

