Systemic Effects on Access to and Utilization of Quality Contraceptive Services by Women of Reproductive age During Covid-19 Pandemics in Oyo State, Nigeria
Abstract:
The indirect health impacts include
diversion or depletion of resources to provide routine care and decreased access
to routine care resulting from an inability to travel due to restriction, fear,
or other factors. This paper presents the findings of a cross-sectional quantitative
study exploring systemic effects on access to and utilization of quality contraceptive
services by women of reproductive age during the Covid-19 pandemic in Oyo State,
Nigeria. A purposive sampling technique was used to select 471 users of users of
MNCH services (postnatal clinic and family planning services and immunization uptakes)
that responded to 43 structured questionnaires that included socio-demographical
characteristics, knowledge of contraceptive products and service availability, contraceptive
supplies, access and utilization, health system opportunities and challenges amidst
Covid-19 pandemics. Of the 471 respondents, the mean age of respondents was 29.63±
3.29years, with (34.2%) within 26-30 years age group. Majorly self-employed/business
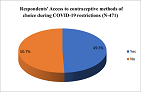
(74.9%), (91.1%) Yorubas ethnicity. Only 49.2% accessed contraceptive services during
restrictions; due to overwhelming fear of Covid-19 by (31.7%), and disruption of
services (31.1%). Others mentioned cost, restriction in movement, and difficulty
in seeing caregivers. With 65.4% of the total respondents currently obtained a method
with easy in restrictions. The Chi-square test, on the relationship between respondents’
access to and utilization of contraceptive services with systemic factors shows
a significant relationship with p =0.004 during the pandemic. It becomes highly
imperative that the family planning program be redesigned to improve the health
system as part of the preparedness measures to address gaps due to the Covid-19
restrictions.
References:
[1] Zulu JM, et al, 2015. Innovation in health service
delivery: integrating community health assistants into the health system at the
district level in Zambia. BMC Health Serv Res. 2015;15(1):1.
[2] Schneider H, Lehmann U, 2016. From Community
Health Workers to Community Health Systems: Time to Widen the Horizon? Health Syst
Reform;2(2):112–8.
[3] Vinit Sharma et al.,
2020Why the Promotion of
Family Planning Makes More Sense Now Than Ever Before? First Published August 5, 2020, https://doi.org/10.1177/0972063420935545.
[4] Purdy C, 2020. Opinion: How will Covid-19 affect
global access to contraceptives—and what can we do about it? Devex, https://www.devex.com/news/sponsored/opinion-how-will-covid-19-affect-global-access-to-contraceptives-and-what-can-we-do-about-it-96745.
[5] Marie Stopes
International,2020. Stories from the frontline: in the shadow of the Covid-19 pandemic,
https://www.mariestopes.org/covid-19/stories-from-the-frontline.
[6] International
Planned Parenthood Federation, 2020. Covid-19 pandemic cuts access to sexual and
reproductive healthcare for women around the world, 2020, https://www.ippf.org/news/covid-19-pandemic-cuts-access-sexual-and-reproductive-healthcare-women-around-world.
[7] Falcone R E, Detty A. 2015. “The Next Pandemic:
Hospital Response.” Emergency Medical Reports 36 (26): 1–16.
[8] International Federation of Gyanecology and
Obsteric, 2020. Covid-19 Contraception and Family Planning: Contraceptive
and Family Planning services and supplies are CORE components of essential health
services, and access to these services is a fundamental human right.
[9] Guanjian Li, Dongdong
Tang et al., 2020: Impact of the Covid-19 Pandemic on Partner Relationships and
Sexual and Reproductive Health: Cross-Sectional, Online Survey Study, Published on 6.8.2020 in Vol 22, No 8 (2020).
[10] Kavita Nanda, et al, 2020. Contraception in
the Era of Covid-19, Glob Health Sci Pract. 2020 Jun 30; 8(2): 166–168. Published
online 2020 Jun 30. Doi: 10.9745/GHSP-D-20-00119 PMCID: PMC7326510, PMID: 32312738.
[11] Weinberger M, Hayes B, et al., 2020: Doing things
differently: what it would take to ensure continued access to contraception during
Covid-19. Glob Health Sci Pract, 8, pp. 169-175.
[12] Modupe Taiwo, et al, 2020. Gendered Impact of
Covid-19 on the Decision-Making Power of Adolescents in Northern Nigeria, Save the
Children Nigeria.
[13] Kantorová V, et al.,2020 Estimating progress
towards meeting women’s contraceptive needs in 185 countries: A Bayesian hierarchical
modelling study. PloS Med 17(2): e1003026. https://journals.plos.org/plosmedicine/articleid=10.1371/journal.pmed.1003026.
[14] United Nations, Department of Economic and Social
Affairs, Population Division, 2019. Family Planning and the 2030 Agenda for Sustainable
Development. New York: United Nations.
[15] WHO, 2007. Maternal mortality in 2005; Estimates
Developed by WHO, UNICEF, UNFPA, and The World Bank, WHO, Geneva 2007.
[16] Lule E, et al., 2007. Fertility regulation behavior
and their costs: contraception and unintended pregnancies in Africa and Eastern
Europe and Central Asia. Washington: World Bank; 2007.
[17] Kayode Afolabi, 2020. Sustaining FP & Sexual
Reproductive Reproductive Health Services Delivery amidst Covid-19 Pandemic, Director/Head
RH Division, Federal Ministry of Health.
[18] Aishat Bukola
Usman, Olubunmi Ayinde, et al, 2020. Epidemiology
of Corona Virus Disease 2019 (Covid-19) Outbreak Cases in Oyo State, Southwest Nigeria
March -April 2020. DOI:10.21203/rs.3.rs-29502/v1.
[19] National Population Commission (NPC) [Nigeria]
and ICF. 2019. Nigeria Demographic and Health Survey 2018. Abuja, Nigeria, and Rockville,
Maryland, USA A: NPC and ICF.
[20] Ezugwu EC, Nkwo PO, Agu PU, Ugwu EO, Asogwa
AO, 2014. Contraceptive use among HIV-positive women in Enugu, southeast Nigeria.
Int J Gynaecol Obstet 2014; 126:14-7.
[21] USAID, 2020. Monitoring Covid-19’s Effects on
Family Planning: What Should We Measure?
[22] FP2020, Measurement, no date, http://progress.familyplanning2020.org/measurement.
[23] Michelle Weinberger et al, 2020: Doing Things Differently: What It Would Take to
Ensure Continued Access to Contraception During Covid-19. Global Health:
Science and Practice, 8(2):169-175; https://doi.org/10.9745/GHSP-D-20-00171.
[24] Sorpreso ICE, et al, 2015. Sexually vulnerable women:
could long-lasting reversible contraception be the solution? Rev Bras Ginecol
E Obstet.; 37:395–396.
[25] Taylor Riley et al.,
2020. Estimates of the Potential
Impact of the Covid-19 Pandemic on Sexual and Reproductive Health in Low- and Middle-Income
Countries, International Perspectives on Sexual and Reproductive
Health, A journal of peer-reviewed research, volume 46, page 73-76.

