Factors Associated with the Uptake Severe Acute Respiratory Syndrome Corona Virus Two Vaccination in Zambia: Case of Mongu District
Abstract:
Since the
vaccination against severe acute respiratory syndrome corona virus two (SARS-CoV-2)
became accessible in Zambia, there has been limited uptake. The study aimed to determine
social cognitive aspects linked with SARS-CoV-2 vaccination in Mongu. A descriptive
quantitative Survey was conducted from December 2021 to April 2022. Cochrane single
proportion formula was used to determined sample size of 369 respondents based on
60% herd immunity criterion. Stata version 14 was used to perform Chi square and
binary logistic regression. Findings indicated that, vaccination level is still
below average, and most non-vaccinated people were unwilling to be vaccinated because
they “simply haven’t gotten around to it”. ‘Views on Covid-19 news’, ‘worrying about
getting sick/a household member getting sick from Covid-19,” real financial effect
of Covid-19 at personal level,’ ‘ages of household Members,’ marital status, religion,
academic qualification, and ages of respondents were associated with SAR-CoV-2 vaccination.
Social cognitive predictors of vaccination were 30-49-year-old household members
and worry about household members being sick. Misconceptions about SARS-CoV-2 vaccinations
prevent vaccination. Therefore, there is need scale-up sensitisation, and sensitisation
messages should address the need to protect household members and especially having
the most mobile age groups (30-49 years) to be vaccinated to reduce on community
spread of the infection. Future studies should analyze the proportions of AstraZeneca’s
one-dose recipients who did not return for the second dose and the willingness of
the completely vaccinated to accept a booster shot.
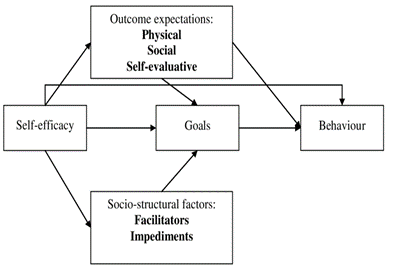
Keywords: Mongu, SARS-CoV-2, Social
cognitive Theory, Vaccine, Uptake, Zambia.
References:
[1] World Health Organization, ‘Covid-19 deaths in
Africa surge more than 40% over previous week’, 2021. [Online]. Available: https://www.afro.who.int/news/covid-19-deaths-africa-surge-more-40-over-previous-week.
[2] C. M. Himwaze et al., ‘Post-mortem examination of
Hospital Inpatient Covid-19 Deaths in Lusaka, Zambia - A Descriptive Whole-body
Autopsy Series’, Int. J. Infect. Dis., vol. 108, pp. 363–369, 2021, doi:
10.1016/j.ijid.2021.06.013.
[3] World Health Organization, ‘Zambia launches the Covid-19
vaccination’, Lusaka, 2021. [Online]. Available: https://www.afro.who.int/news/zambia-launches-covid-19-vaccination.
[4] O. Sarasty, C. E. Carpio, D. Hudson, P. A.
Guerrero-ochoa, and I. Borja, ‘The demand for a Covid-19 vaccine in Ecuador’,
Vaccine, vol. 38, no. 51, pp. 8090–8098, 2020, doi:
10.1016/j.vaccine.2020.11.013.
[5] M. Schoch-spana et al., ‘The public ‘s role in Covid-19
vaccination: Human-centered recommendations to enhance pandemic vaccine awareness,
access, and acceptance in the United States’, Vaccine, no. xxxx, 2020, doi:
10.1016/j.vaccine.2020.10.059.
[6] T. Dzinamarira, B. Nachipo, B. Phiri, and G. Musuka,
‘Covid-19 Vaccine Roll-Out in South Africa and Zimbabwe: Urgent Need to Address
Community Preparedness, Fears and Hesitancy’, 2021.
[7] C. Gosa, ‘Covid-19 Vaccine Update as of March 29th,
2022’, Lusaka, 2022.
[8] J. R. Macneil, J. R. Su, K. R. Broder, A. Y. Guh, J.
W. Gargano, and M. Wallace, ‘Updated Recommendations from the Advisory
Committee on Immunization Practices for Use of the Janssen (Johnson & Johnson)
Covid-19 Vaccine After Reports of Thrombosis with Thrombocytopenia Syndrome
Among Vaccine Recipients — United States, April 2021’, vol. 70, 2021.
[9] K. P. Iyengar, R. Vaishya, V. K. Jain, and P. Ish.,
‘BAME community hesitancy in the UK for Covid-19 vaccine: suggested solutions’,
no. vii, pp. 1–2, 2020, doi: 10.1136/postgradmedj-2021-139957.
[10] R. Muqattash, I. Niankara, and R. I. Traoret,
‘Survey data for Covid-19 vaccine preference analysis in the United Arab
Emirates’, Data Br., vol. 33, p. 106446, 2020, doi: 10.1016/j.dib.2020.106446.
A.
Bandura,
‘Self-efficacy: Toward a Unifying Theory of Behavioral Change’, Psychol. Rev.,
vol. 84, no. 2, pp. 191–215, 1977.
[11] A. Alsaeed and U. Rabbani, ‘Explaining covid-19
vaccine rejection using social cognitive theory in Qassim, Saudi Arabia’,
Vaccines, vol. 9, no. 11, 2021, doi: 10.3390/vaccines9111304.
[12] Q. Mwabu, ‘MQHZ calls for Awareness Among Zambians
Ahead of Next Month’s National Covid-19 Vaccination’, Lusaka Times, Lusaka,
2021.
[13] S. T. Masebo, ‘Ministry of Health Zambia (2022)
Statement on Covid-19 In Zambia’, Lusaka, 2022.
[14] Zambian Ministry of Health, ‘Daily Vaccination Summary’,
Mongu, 2021.
[15] T. F. L. Matenga, J. M. Zulu, L. Moonzwe Davis, and
M. P. Chavula, ‘Motivating factors for and barriers to the Covid-19 vaccine
uptake: A review of social media data in Zambia’, Cogent Public Heal., vol. 9,
no. 1, 2022, doi: 10.1080/27707571.2022.2059201.
[16] W. Cochran, Sampling Techniques. New York: Wiley,
1963.
[17] V. Hall et al., ‘Effectiveness of BNT162b2 mRNA
vaccine against infection and Covid-19 vaccine coverage in healthcare workers
in England’, Pre-print, 2021.
[18] J. Holder, ‘Tracking Coronavirus Vaccinations Around
the World’, New York Times, New York, May 17, 2021.
A.
R. Mercadante
and A. V Law, ‘Research in Social and Administrative Pharmacy Will they, or won’t
they? Examining patients ‘vaccine intention for flu and Covid-19 using the
Health Belief Model’, Res. Soc. Adm. Pharm., no. xxxx, 2020, doi:
10.1016/j.sapharm.2020.12.012.
B.
Ateghang-awankem,
L. Deluca, E. Shadzeka, and K. Y. Anchang, ‘Good Participatory Practice,
Clinical Trials Awareness and Covid-19 Vaccine Acceptance in Sub-Sahara
Africa’, vol. 9, no. 3, pp. 90–95, 2021, doi: 10.12691/ajphr-9-3-1.
[19] J. V. Lazarus et al., ‘A global survey of potential
acceptance of a Covid-19 vaccine’, Nat. Med., 2020.
[20] L. Hamel, L. Lopes, G. Sparks, M. Stokes, and M.
Brodie, ‘KFF Covid-19 Vaccine Monitor: June 2021’, Kaiser Fam. Found., no.
June, pp. 1–28, 2021, [Online]. Available: https://www.kff.org/coronavirus-covid-19/poll-finding/kff-covid-19-vaccine-monitor-april-2021/.
[21] World Health Organization, ‘Good Participatory
Practice for Covid-19: a toolbox’, Geneva, 2020.
[22] W. SR, ‘National routine adult immunization programs
among World Health Organization member states: an assessment of health systems
to deploy future SARS-CoV-2 vaccines’, MedRxiv, Dec. 16, 2020.
[23] S. L. Wilson and C. Wiysonge, ‘Social media and
vaccine hesitancy’, BMJ Glob. Heal., 2020.
[24] M. E. Schuster and P. Duclos, ‘SAGE Working Group.
Review of Vaccine Hesitancy: Rationale, Remit, and Methods’, Vaccine, vol. 33,
no. 34, pp. 4157–4160, 2015.
[25] N. MacDonald, ‘Vaccine hesitancy: Definition, Scope
and Determinants’, Vaccine, vol. 33, no. 34, pp. 4161–4164, 2015.
[26] H. Larson, C. Jarrett, E. Eckersberger, D. Smith,
and P. Paterson, ‘Understanding vaccine hesitancy around vaccines and
vaccination from a global perspective: A systematic review of published
literature’.

