Determinants of Immunization Coverage and Associated Factors among Children aged under Two-Year-Old in the National Immunization Program of Mewat district, Haryana (2019-2020)
Abstract:
Background: Vaccination against childhood communicable
diseases through Expanded Program on Immunization is one
of the most cost-effective public health interventions. Additional 1.5 million child
deaths can be prevented if global vaccination coverage is improved. Mewat district
has one of India’s lowest immunization rates despite a long-standing Universal Immunization
Program and continues to sustain a high prevalence of vaccine-preventable diseases.
This study investigates determinants of immunization status among children aged
0-23 months. Methods: A community-based cross-sectional study was conducted from
December 2019 to June 2020, among 800 children aged 0-23months, randomly selected
in one rural and one urban ward each from all 4 blocks of Mewat. Socio-demographic
conditions and vaccine-related data were collected using a semi-structured questionnaire. Immunization
was assessed by vaccination card and by mother’s recall where the card was unavailable.
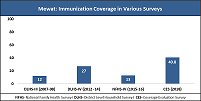
Results: Mewat has increased full immunization coverage from 13.1% in 2015-16 to
59.4%. Immunization card was available with 68.5% (292/426) beneficiaries. Dropout
rates for Pentavalent1 to Pentavalent3 was 27.5% and 54% for Bacillus Calmette-Guerin
to measles. After adjusting for the state of residence, religion, gender, paternal
education, health professional presence during birth, place of vaccination and knowledge
of mother on due dose were significantly associated with full immunization. Awareness
gap and fear of side effects for vaccines were main reasons of vaccine hesitancy.
Conclusion: Full immunization coverage in the district is sub optimal and behind
the desired coverage goal, mainly due to vaccine hesitancy. Enhancing community
knowledge about the benefits of vaccination is recommended.
References:
[1] United Nations
Inter-Agency Group for Child Mortality Estimation (UN IGME) United Nations Children’s
Fund; New York: 2017. Levels & Trends in Child Mortality: Report 2017. Estimates
Developed by the UN Inter-agency Group for Child Mortality Estimation.
[2] National,
regional, and global levels and trends in neonatal mortality between 1990 and 2017,
with scenario-based projections to 2030: a systematic analysis. Lucia Hug,
Monica Alexander, Danzhen You, Leontine Alkema on behalf of the UN Inter-agency
Group for Child Mortality Estimation. Published: June, 2019 DOI: https://doi.org/10.1016/S2214-109X(19)30163-9.
[3] https://www.who.int/immunization/monitoring_surveillance/who-immuniz.pdf.
[4] https://www.who.int/teams/immunization-vaccines-and-biologicals/strategies/global-vaccine-action-plan.
[5] World Health
Organization (WHO).2017.10 Facts on Immunization. retrieved from: http://www.who.int/features/factfiles/immunization/en/.
[6] Gurnani V,
Haldar P, Aggarwal MK, Das MK, Chauhan A, Murray J, et al. Improving vaccination
coverage in India: Lessons from intensified mission Indra Dhanush, cross-sectoral
systems strengthening strategy. BMJ. 2018;363: k4782.
[7] Ministry of Health and Family Welfare. Mission Indradhanush,
operational guidelines. Delhi, India: MOHFW, 2014. http://164.100.158.44/showfile.php?lid=4258.
[8] Ministry of
Health and Family Welfare (MOHFW). Intensified Mission Indradhanush, operational
guidelines. MOHFW, 2017.https://mohfw.gov.in/sites/default/files/Mission%20Indradhanush%20Guidelines.pdf.
[9] International Institute for Population Sciences. District
Level Household and Facility Survey-4: District Fact Sheet Mewat (2012-13). Mumbai:
Ministry of Health and Family Welfare; 2012.
[10] International
Institute for Population Sciences (IIPS) and ICF. National family health survey
(NFHS-4), 2015-16: India. IIPS, 2017. https://dhsprogram.com/pubs/pdf/FR339/FR339.pdf.
[11] https://nhm.gov.in/New_Updates_2018/NHM_Components/Immunization/Guildelines_for_immunization/IMI_CES_Survey_Report.pdf.
[12] Immunization
Division, Ministry of Health and Family Welfare, Government of India. (2019). Road
Map for achieving 90% full immunization coverage in India, a guiding document for
the states. MoHFW: New Delhi.
[13] Directorate
of Census Operations Haryana. Census of India 2011 Haryana: Series-07: Part XII-B:
District Census Handbook Mewat: Village and Town Wise Primary Census Abstract (PCA)
[Internet]. Chandigarh: Ministry of Home Affairs, Government of India; 2011. http://censusindia.gov.in/2011census/dchb/0619_PART_B_DCHB_MEWAT.pdf.
[14] Philip, Rachel. 2017.Breaking Barriers: The Status of
Adolescent Girls’ Education in Mewat, Haryana. Doi. 10.13140/RG.2.2.30113.56160.
[15] Lwanga SK, Lamshhow S. Sample Determination in Health
Studies; A Practical Manual. Geneva: World Health Organization; 1991.
[16] Prinja S,
Monga D, Rana SK, Sharma A, Dalpath S, Bahuguna P, Gupta R, Aggarwal AK. District-Level
Analysis of Routine Immunization in Haryana State: Implications for Mission Indradhanush
under Universal Immunization Programme. Indian J Community Med. 2018 Jul-Sep;43(3):209-214.
doi: 10.4103/ijcm.IJCM_306_17. PMID: 30294090; PMCID: PMC6166503.
[17] Angadi MM,
Jose AP, Udgiri R, Masali KA, Sorganvi V. A Study of Knowledge, Attitude and Practices
on Immunization of Children in Urban Slums of Bijapur City, Karnataka, India. Journal
of Clinical and Diagnostic Research. 2013;7(12): 2803-6.
[18] WHO. Immunization
Coverage [Internet]. World Heal. Organ. Fact Sheet Immun. Cover. 2016. [cited 2017
Mar 6]. Available from: http://www.who.int/mediacentre/factsheets/fs378/en.
[19] Nair TN, Varughese
E (1994) Immunization coverage of infants – the rural-urban difference in Kerala.
Indian Pediatrics 31:139-143.
[20] Agarwal S,
Bhanot A, Goindi G (2005) Understanding and addressing childhood immunization coverage
in urban slums. Indian Pediatrics 42: 653–663.
[21] Desai S, Alva
S (1998) Maternal education and child health: Is there a strong causal relationship?
Demography 35 1: 71–81.
[22] UNICEF (2009)
Coverage Evaluation Survey. Government of India, Ministry of Health and Family Welfare
and UNIC EF. Available: www.unicef.org/india/health_5578.htm and www.unicef.org/india/National_Fact_Sheet_CES_2009.pdf.
[23] Gaudin S,
Yazbeck AS (2006) Immunization in India 1993–1999: Wealth, gender, and regional
inequalities revisited. Social Science and Medicine 62: 694–706.
[24] Mohanty SK,
Pathak PK (2009) Rich-poor gap in utilization of reproductive and child health care
services in India, 1992–2005. Journal of Biosocial Sciences 41 3: 381–398.
[25] Arokiasamy
P, Pradhan J (2011) Measuring wealth-based health inequality among Indian children:
the importance of equity vs. efficiency. Health Policy and Planning 26: 429–440.
[26] Dalal A, Silveira
MP (2005) Immunization status of children in Goa. Indian Paediatrics 42: 401–402.
[27] Kumar A, Mohanty SK (2011) Socioeconomic differentials
in childhood immunization in India, 1992–2006. Journal of Population Research 28
4: 301–324.
[28] Pande R (2003)
Selective Gender differences in childhood nutrition and immunization in rural India:
The role of siblings. Demography 40: 395–418.
[29] Corsi DJ,
Bassani DG, Kumar R, Awasthi S, Jotkar R, et al. (2009) Gender inequity and age-appropriate
immunization coverage in India from 1992 to 2006. BMC International Health Human
Rights 14 Suppl. 1: S3–9.
[30] Singh P, Yadav
RJ (2000) Immunization status of children of India. Indian Pediatrics 37: 1194–1199.
[31] Phukan RK,
Barman MP, Mahanta J (2009) Factors associated with immunization coverage of children
in Assam, India: over the first year of life. Journal of Tropical Pediatrics 55:
249–252.
[32] Babirye JN,
Engebretsen IMS, Makumbi F, Fadnes LT, Wamani H, Tylleskar T, et al. timeliness
of childhood vaccinations in Kampala Uganda: a community-based cross-sectional study.
PLoS One. 2012; 7:1–6. 24.
[33] Etana B, Deressa
W, Angela G, Zulfiqar B, Lulu B, Aly G, et al. Factors associated with complete
immunization coverage in children aged 12–23 months in ambo Woreda, Central Ethiopia.
BMC Public Health. 2012; 12:566. 25.
[34] Reynolds HW,
Wong EL, Tucker H. Adolescents’ use of maternal and child health services in developing
countries. Int Fam Plan Perspect. 2006; 32:6–16.
[35] Nath L, Kaur
P, Tripathi S. Evaluation of the universal immunization program and challenges in
coverage of migrant children in Haridwar, Uttarakhand, India. Indian J Community
Med [Internet] [cited 2020 Nov 10]. Available from: http://www.ijcm.org.in/article.asp?issn=0970-0218;year=2015;volume=40;issue=4;spage=239;epage=245;aulast=Nath.
[36] Vohra. Immunization
coverage and its determinants among 12-23 months old children of Lucknow [Internet]
[cited 2020 Nov 10]. Available from: http://www.mjmsr.net/article.asp?issn=0975-9727;year=2013;volume=4;issue=2;spage=90;epage=95;aulast=Vohra.
[37] Nath B, Singh
JV, Awasthi S, Bhushan V, Kumar V, Singh SK. A study on determinants of immunization
coverage among 12-23 months old children in urban slums of Lucknow district, India.
Indian J Med Sci. 2007; 61:598–606.
[38] Madhavi N,
Manikyamba D. Evaluation of immunization status and factors responsible for dropouts
in primary immunization in children between 1-2 years – A hospital-based study.
Pediatr Rev Int J Pediatr Res. 2016; 3:332. Available from: http://medresearch.in/index.php/IJPR/article/view/747.
[39] Singhal G,
Mathur H, Dixit M, Khandelwal A. Factors affecting immunization among children of
the rural population of block Malpura, district Tonk, Rajasthan, India. Int J Community
Med Public Health. 2016; 3:641–6.
[40] Kumar D, Aggarwal
A, Gomber S. Immunization status of children admitted to a tertiary-care hospital
of North India: Reasons for partial immunization or non-immunization. J Health,
Popul Nutr. 2010;28(3):300-4.
[41] Kumar A, George
K, Bose A. Immunization coverage among children aged 12-23 months in Surajgarha
Block, Lakhisarai District, Bihar: A cluster sampling survey. National J Community
Med. 2018; 9:5.
[42] Ahmad J, Khan
ME, Hazra A. Increasing complete immunization in rural Uttar Pradesh. J Fam Welf.
2010; 56:65–72.
[43] Datta A, Baidya
S, Datta S, Mog C, Das S. A study to find out the full immunization coverage of
12- to 23-month-old children and areas of under-performance using LQAS technique
in a Rural Area of Tripura. J Clin Diagn Res JCDR. 2017;11:LC01–4.
[44] Murhekar MV,
Kamaraj P, Kanagasabai K, Elavarasu G, Rajasekar TD, Boopathi K, et al. Coverage
of childhood vaccination among children aged 12-23 months, Tamil Nadu, 2015, India.
Indian J Med Res. 2017; 145:377.
[45] Khargekar
NC, Khargekar VC, Shingade PP. Immunization status of children under 5 years in
a Tribal Area, Parol, Thane District. Natl J Community Med. 2015; 6:522–7.
[46] Kadri AM,
Singh A, Jain S, Mahajan RG, Trivedi A. Study on immunization coverage in urban
slums of Ahmedabad City. Indian J Public Health Res Dev. 2010; 33:5.
[47] Prusty RK,
Kumar A (2014) Socioeconomic Dynamics of Gender Disparity in Childhood Immunization
in India, 1992–2006. PLoS ONE 9(8): e104598. doi: 10.1371/journal.pone.0104598.
[48] Parpiev Z,
Yusupov K (2009) Intrahousehold gender-based discrimination among children in Uzbekistan.
Working paper, No 09/10E. Economics Education and Research Consortium.
[49] Nasir R, Kalla
AK (2006) Kinship system, fertility, and son preferences among the Muslims: A review.
Anthropologist 8 4: 275–281.
[50] Pande R, Astone
NM (2007) Explaining son preference in rural India: The independent role of structural
versus individual factors. Population Research and Policy Review 26(1):1–29.
[51] Partha D,
Bhattacharya BN. Determinants of child immunization in four less-developed states
of north India. J Child Health Care. 2002 Mar;6(1):34-50. doi: 10.1177/136749350200600105.
PMID: 12036175.
[52] Rammohan A,
Awofeso N, Fernandez RC. Paternal education status significantly influences infants’
measles vaccination uptake, independent of maternal education status. BMC Public
Health. 2012;12(1):336. (http://dx.doi.org/10.1186/1471-2458-12-336).
[53] Mathew JL.
Inequity in childhood immunization in India: a systematic review. Indian Pediatr.
2012;49(3):203–223. http://dx.doi.org/10.1007/s13312-012-0063-z.
[54] Vikram K.,
Vanneman R., Desai S. Linkages between maternal education and childhood immunization
in India. Soc. Sci. Med. 2012; 75:331–339. doi: 10.1016/j.socscimed.2012.02.043.
[55] P.K. Singh,
C. Kumar, R.K. Rai, L. Singh. Factors associated with maternal healthcare services
utilization in nine high focus states in India: a multilevel analysis based on 14
385 communities in 292 districts. Health Policy Plan, 29 (5) (2014), pp. 542-559.
(http://dx.doi.org/10.1093/heapol/czt039).
[56] Kumar A, Mohanty
SK. Socioeconomic differentials in childhood immunization in India,
1992–2006. J Popul Res. 2011;28(4):301–324. (http://dx.doi.org/10.1007/s12546-011-9069-y).
[57] Joe W, Mishra
US, Navaneetham K. Socio-economic inequalities in child health: recent evidence
from India. Glob Public Health. 2010;5 (5):493–508. (http://dx.doi.org/10.1080/17441690903213774).
[58] Fernandez
R, Rammohan A, Awofeso N. Correlates of the first dose of measles vaccination delivery
and uptake in Indonesia. Asian Pac J Trop Med. 2011; 4:140–5. 14.
[59] Gatchell M,
Thind A, Hagigi F. Informing state-level health policy in India: the case of childhood
immunizations in Maharashtra and Bihar. Acta Paediatr. 2008;97(1):124–126. (http://dx.doi.org/10.1111/j.1651-2227.2007.00569.x).
[60] Manjunath
U, Pareek RP. Maternal knowledge and perceptions about the routine immunization
program. A study in a semi-urban area in Rajasthan. India J Med Sci. 2003; 57:158-63.
[61] Mbengue MAS,
Sarr M, Faye A, Badiane O, Camara FBN, Mboup S, et al. Determinants of complete
immunization among Senegalese children aged 12–23 months: evidence from the demographic
and health survey. BMC Public Health. 2017; 17:630. 39.
[62] Lakew Y, Bekele
A, Biadgilign S. Factors influencing full immunization coverage among 12–23 months
of age children in Ethiopia: evidence from the national demographic and health survey
in 2011. BMC Public Health. 2015; 15:728. 40.
[63] Adedokun ST,
Uthman OA, Adekanmbi VT, Wiysonge CS. Incomplete childhood immunization in Nigeria:
a multilevel analysis of individual and contextual factors. BMC Public Health. 2017;
17:236.
[64] Sia D, Fournier
P, Kobiané J-F, Sondo BK. Rates of coverage and determinants of complete vaccination
of children in rural areas of Burkina Faso (1998-2003). BMC Public Health. 2009;
9:416.
[65] Abbey M. Jones,
Saad B. Omer, Rober A. Bednarczyk, Neal A. Halsey, Lawrence H. Moulton, and Daniel
A. Salmon. Advances in Preventive Medicine. Volume 2012, Article ID 932741. Doi:10.1155/2012/932741.

