Sickle Cell Disease in Pregnancy: Active Nursing Management
Abstract:
Sickle cell disease is
considered as a major complication and risk factor for perinatal morbidity /mortality.
Literature document that most pregnancies complicated by sickle cell are likely
to result in live birth, but the consequences of influence of the disease for the
pregnancy/newborn remains a significant concern for health care providers worldwide.
According to the bibliography obstetrical-fetal risks are due to the metabolic demands,
hypercoagulable state, and vascular stasis associated with pregnancy characterized
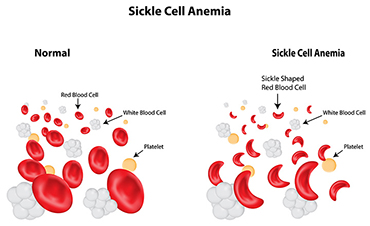
normally for blood cells to be able to carry oxygen to the growing fetus. With sickle
cell anemia, the abnormal red blood cells and anaemic characteristics of the disease
physiopathology may result in lower amounts of oxygen going to the developing baby
with negative outcome for the future newborn.
Research review studies
agreed that access of the pregnant client to a multidisciplinary care team knowledgeable
about sickle cell disease and high-risk obstetrics can significantly decrease feto-maternal
morbidity and mortality. Example: decreases in spontaneous miscarriage, in perinatal
death rates and lowered incidence of preterm labour. Active prenatal management
include: education; genetic counselling and prenatal diagnosis for couples at risk;
improving nutritional status; vaccination for disease prevention, and early detection
of bacterial infection.
Objective of this study was to explore active nursing management
of the pregnant women with sickle cell disease, including education, treatment and
nursing intervention.
Method: use of English Literature
review current through: Jun 2017, Data were searched using MEDLINE,
EMBASE, PUBMED and COCHRANE Systematic Reviews.
Keywords: Sickle Cell Disease, complication,
feto-maternal risk, active nursing management.
References:
[1]. Eugene
Oteng-Ntim, Daveena Meeks, Paul T Seed, Louise Webster, Jo Howard, Pat Doyle, and
Lucy C Chappell. Adverse maternal
and perinatal outcomes in pregnant women with sickle cell disease: systematic review
and meta-analysis. Blood, March 2015 DOI: 10.1182/blood-2014-11-607317
[2].
Goldsmith JC, Bonham VL, Joiner CH,
et al. framing the research agenda for sickle cell trait: building on the current
understanding of clinical events and their potential implications. Am J Hematol
2012; 87:340.
[3]. NHLBI.
Evidence-Based Management of Sickle Cell Disease: Expert Panel Report, 2014. p.24.
http://www.nhlbi.nih.gov/guidelines (Accessed on August 11, 2014).
[4]. Oteng-Ntim E, Meeks D, Seed PT, Webster L,
Howard J, Doyle P, Chappell LC. Adverse maternal and perinatal outcomes in pregnant
women with sickle cell disease: systematic review and meta-analysis. Blood. 2015;
125(21):3316-25. [PubMed]
[5]. Oteng-Ntim
E, Ayesha B, Knight M, Howard J. Pregnancy outcome in patients with sickle cell
disease in the UK--a national cohort study comparing sickle cell anaemia (HbSS)
with HbSC disease. Br J Haematol 2015; 169:129.
[6]. Pintova
S, Cohen HW, Billet HH. Sickle cell trait: is there an increased VTE risk in pregnancy
and the postpartum? PLoS One 2013; 8:e64141.
[7].
Royal
College of Obstetricians and Gynaecologists Green-top. Guideline Management of sickle
cell disease in pregnancy. RCOG.
2011;
61:1–20.
[8]. Souza J.P., Cecatti J.G., Fagundes A., Morais
S.S., Villar J., Carroli G.A. Maternal near miss and maternal death in the World Health Organization's
2005 global survey on maternal and perinatal health. Bull World Health Org. 2010;
88:113–119. [PubMed].

