Patients’ perceptions and experiences of Laparoscopic cholecystectomy VS Kocher Incision cholecystectomy: A qualitative phenomenological approach study at various hospitals of Pakistan
Abstract:
Cholecystitis is a common disorder in Pakistani population which
affects the life of individual, pre and post operatively. Repeated pain
episodes cause frequent visit to the emergency reception and repeated hospital
admissions for symptomatic treatment, until individual decides for the gall
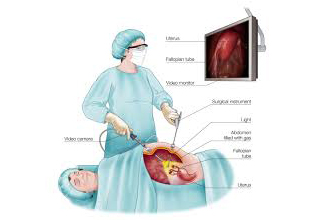
bladder surgery. Cholecystectomy is the most common surgical treatments for
cholecystitis and cholelithiasis. This phenomenological study was conducted to
get a deep understanding of patients’ perceptions and experiences about the
disease and treatment. Ten women and 6 men were scheduled for collecting data.
All were explained about the purpose of study and an interview guide was
developed containing only two questions. Same questions were sent to health
care professionals as an opinionnaire. The answers and responses were categorized
in four main themes by using qualitative software NVIVO. These four themes
describe the patient’s feelings toward their cholecystitis, Cholelithiasis and
cholecystectomy experiences. The patient’s themes indicated they were consumed
with feelings of: (a) Fear of large scar vs Blind holes over entire abdomen (b)
Pain Perception & Pain Experiences (c) Certainty vs Uncertainty (d)
Yearning for speedy recovery. The mentioned findings revealed that individuals
with gallstone disease experience, expressed their feelings of fear of large
scar at gall bladder area, or afraid of making four holes over entire abdomen.
The perception of pain was found equal in both surgeries, fewer reported less
pain in Kocher incision and fewer reported infection in one or two of the four
holes on the abdomen. Uncertainty was found more health care professionals vs
laymen and women. Some participants responded that laparoscopic surgery was
opted due to less length of stay in the hospital.
References:
[1].
Aly S, and Hokkam E.N, (2014) Operative Outcome and Patient
Satisfaction in Early and Delayed Laparoscopic Cholecystectomy for Acute
Cholecystitis: Minimally Invasive Surgery
Published online 2014 Aug 14. doi: [10.1155/2014/162643].
[2].
Anwar HA, Ahmed QA, Bradpiece HA. Removing symptomatic
gallstones at their first emergency presentation. Annals of the Royal College
of Surgeons of England. 2008; 90:394– 397.10.1308/003588408X301037 [PubMed:
18634735].
[3].
Barthelsson C, Lützén K, Anderberg B, Nordström G. Patients’
experiences of laparoscopic cholecystectomy in day surgery. Journal of Clinical
Nursing. 2003; 12:253–259.10.1046/j. 1365-2702.2003.00699.x [PubMed: 12603558].
[4].
Branum, G and et al. (2015) Management of major biliary
complications after laparoscopic cholecystectomy. Annals of Surgery, 217(5):
532–541.
[5].
Costa MJ. The lived perioperative experience of ambulatory
surgery patients. Association of Operation Room Nurse Journal. 2001;
74:874–881.10.1016/S0001-2092(06)61505-6.
[6].
Creswell, JW. Qualitative inquiry and research design:
Choosing among five approaches. 2. Thousand Oaks, CA: Sage; 2007.
[7].
Elwood DR. Cholecystitis. Surgical Clinics of North America.
2008; 88:1241–1252.10.1016/j.suc. 2008.07.008 [PubMed: 18992593].
[8].
Ene KW, Nordberg G, Bergh I, Johansson FG, Sjöström B.
Postoperative pain management – The influence of surgical ward nurses. Journal
of Clinical Nursing. 2008; 17:2042–2050.10.1111/j. 1365-2702.2008.02278.x
[PubMed: 18705781] Ferrell BR.
[9].
Ferrell BR, Rhiner M, Cohen MZ, Grant M. Pain as a metaphor
for illness. Part I: Impact of cancer pain on family caregivers. Oncology
Nursing Forum. 1991; 18:1303–1309. [PubMed: 1762971].
[10].
Gangemi, A. Danilkowics, R, Elli FE, Bianco, F, Masrur M,
Giulianotti P.C (2016) Could ICG-aided robotic cholecystectomy reduce the rate
of open conversion reported with laparoscopic approach? A head to head
comparison of the largest single institution studies. Journal of Robotic
Surgery: (1):77-82. doi: 10.1007/s11701-016-0624-6.
[11].
Gustavsson M, Ung K, Nilsson Å, Ung EJ. Patients’ experiences
of gallstone disease. Gastrointestinal Nursing. 2011; 9:23–27.
[12].
Halpin V, Gupta A. Acute cholecystitis. Clinical Evidence.
2011; 12:1–24.
[13].
Keus F, de Vries J, Gooszen HG, van Laarhoven CJ. Assessing
factors influencing return back to work after cholecystectomy: A qualitative
research. BMC Gastroenterology. 2010; 10:1– 7.10.1186/1471-230X-10-12 [PubMed:
20064220].
[14]. Kleinbeck SV,
Hoffart N. Outpatient recovery after laparoscopic cholecystectomy. Association
of Operation Room Nurse Journal. 1994; 60:394,
397-8–401-2.10.1016/S0966-6532(97)89248-7.
[15]. Koirala, U &
et. al. (2011) Biliary complications after laparoscopic cholecystectomy:
Journal of Nepal Health Research Council: (1): 38- 43.
[16].
Lauterbach, SS. Meanings in mothers’ experience with infant
death: Three phenomenological inquiries: In another world; five years later;
and what forever means. In: Munhall, PL., editor. Nursing research: A
qualitative perspective. Sudbury, MA: Jones & Bartlett; 2007. p. 211-238.
[17]. Rao, A, and et
al. (2017) Safety of outpatient laparoscopic cholecystectomy
in the elderly: analysis
of 15,248 patients using the NSQIP database. Journal of the American College of
Surgeons: 217(6):1038-43.
[18].
Rhiner M, Cohen MZ, Grant M. Pain as a metaphor for illness.
Part I: Impact of cancer pain on family caregivers. Oncology Nursing Forum.
1991; 18:1303–1309. [PubMed: 1762971].
[19].
Rubert, C.P, Higa, R.A. and Farias, F.V (2016) Comparison
between open and laparoscopic elective cholecystectomy in elderly, in a
teaching hospital. doi: 10.1590/0100-69912016001002.43(1):2-5.
[20].
Stinton LM, Myers RP, Shaffer EA. Epidemiology of gallstones.
Gastroenterology Clinics of North America. 2010;
39:157–169.10.1016/j.gtc.2010.02.003 [PubMed: 20478480].
[21].
Wolf AS, Nijsse BA, Sokal SM, Chang Y, Berger DL. Surgical
outcomes of open cholecystectomy in the laparoscopic era. The American Journal
of Surgery. 2009; 197:781–784.10.1016/j.amjsurg. 2008.05.010.

