Patient-related Factors Associated with type-2 Diabetes Mellitus Control in Peri-Urban Primary Care Setting South Africa
Abstract:
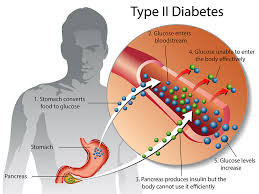
Introduction: Diabetes
mellitus is rising globally. Yet, paucity of data exists on factors associated with its
control at primary care level. Aim was
to explore patient factors associated with type 2 diabetes control. Objectives were
to describe the socio-demographics, proportion of diabetic control and associations
between control and factors. Methods:
The site was in Daveyton township and eight satellite
clinics, Ekurhuleni, South Africa. A cross-sectional descriptive study systematically selected
200 participants by picking every third
patient attending review from March to June 2015. A questionnaire
covering socio-demographics, diabetes information, physical activities, depressive
symptoms, blood pressure, weight, height and glycated hemoglobin was administered
by researchers. Microsoft excel, and strata 13
software were used for data capture and analysis. Chi-square or Fisher’s exact test
was used to compare categorical variables with control. Logistic regression was
used for binary variables and to compare relationships. P-values of <0.05 was
statistically significant. Results and analysis: Good
control was 36% (n=72), significantly associated with mean age of 65 (p=0.001),
formal housing (p=0.020) or income (p=0.001). Hypertension (p=0.056), normal weight
(p=0.056) and physical activities (p=0.059) were not significant. Poor control was
64% (n=128) and significantly associated with younger mean age of 55.66 (p=0.001)
and informal housing (p=0.020). Neither good nor poor control was observed with
depression, compliance, co-morbidities and complications. Conclusion: Older
patients were more likely to be controlled compared to younger ones. To improve
care, effort should focus on younger patients. Further studies should be conducted
on depression and glycaemic control.
References:
[1].
American Diabetes Association.
2019. Diabetes Care. Standards of Medical Care. Jan; 42 (Supplement 1): S1-S2…42
(Supplement 1). S3. https://DOI.ORG/10.2337/DC19-SppC01. Date accessed 30 October
2019.
[2].
International Diabetes Federation
(IDF). 2019. Atlas 8th Edition. Global fact sheet (pdf). Date accessed
20 October 2019.
[3].
SEMDSA. 2017. Guidelines for
the management of Type 2 Diabetes Mellitus. SEMDSA Type 2 Diabetes Mellitus Expert
Committee. JEMDSA 2017; 22 (1) (Supplement 1): S1-196. Date accessed 2 October 2019.
[4]. Statistics South Africa. 2017. www.statsSa.gov.za/?page_id=1021&id
Ekurhuleni-municipality. (Accessed on 14 October 2019).
[5]. World
Health Organization. 2014. Preventing Chronic Diseases - a vital investment. Http://www.who.int>chronic_disease_report 2014 Accessed on 23 May 2017.
[6].
Kendzor
DE, Chen M, Reininger BM, et al. 2014.
The association of depression and anxiety with glycemic control among Mexican Americans
with diabetes living near the U.S.-Mexico border. BMC Public Health 2014, 14:176.
[7].
http://www.biomedcentral.com/1471-2458/14/176.
[8].
Shisana
O, Labadarios D, Rehle T et al. 2014. South Africans National Health &
Nutritional Examination Survey (SANHANES-1) Cape Town 2013. HSRC Press. www.Hsrcpress.ac.za. (Accessed on 20 October 2018)
[9].
Green
B and Zoepke A. 2013. Diabetes and Diabetes Foot ulcers: an often-hidden problem.
S Afr Fam Pract 2013;55(6):515-518.
[10]. Umpierre D, Ribeiro PAB,
Schaan BD, and Ribeiro JP. 2013. Volume of supervised exercise training impacts
glycaemic control in patients with type 2 diabetes: a systematic review with meta-regression
analysis. Diabetologia (2013) 56:242–251 DOI 10.1007/s00125-012-2774-z.
[11]. Ahmad NS, Islahudin F, and
Paraidathathu T. 2013. Factors associated with good glycemic control among patients
with type 2 Diabetes Mellitus. J. Diabetes Investig. 2014 Sep; 5(5): 563–569. Published
online 2013 Dec 5. Doi: 10.1111/jdi.12175.
[12].
http://www.ncbi.nlm.nih.gov/pubmed/Accessed
on 20. April 2019.
[13]. Angamo MT, Melese BH, Ayen
WY. 2013. Determinants of Glycemic Control among Insulin Treated Diabetic Patients
in Southwest Ethiopia: Hospital Based Cross Sectional Study. PLoS ONE 8(4): e61759.
doi: 10.1371/journal.pone.0061759.
[14]. Al-Lawati JA, Barakat MN,
Al-Maskari M, et al. 2012. HbA1c Levels
among Primary Healthcare Patients with type 2 Diabetes Mellitus in Oman. Oman Medical
Journal (2012) Vol. 27, No. 6: 465-470. DOI 10. 5001/omj.2012.111.
[15]. Khan A R, Al-Abdul Lateef
ZN, Al Aithan MA et al. 2012. Factors
contributing to non-compliance among diabetics attending primary health centres
in the Al Hasa district of Saudi Arabia. Journal of Family & Community Medicine;
2012, Vol. 19 Issue 1, p26.
[16]. Juarez DT, Sentell T, Tokumaru
S, et al. 2012. Factors Associated with
Poor Glycemic Control or Wide Glycemic Variability Among Diabetes Patients in Hawaii,
2006–2009. Prev Chronic Dis 2012; 9:120065. DOI: http://dx.doi.org/10.5888/pcd9.120065.
http://www.cdc.gov/pcd/issues/2013/12_0065e.htm. Accessed 24 April 2019.
[17]. Otiniano ME, Snih SA, Goodwin
R. 2012. Factors associated with poor glycemic control in older Mexican American
diabetics aged 75 years and older. J Diabetes Complications. 2012; 26(3): 181–186.
doi: 10.1016/j.jdiacomp.2012.03.10.
[18]. Khattab M, Khader YS, Al-Khawaldeh
A.2010. Factors associated with poor glycemic control among patients with type 2
diabetes. Journal diabetes complications 2010 Mar-Apr;24(2):84-9. doi: 10.1016/j.jdiacomp.

