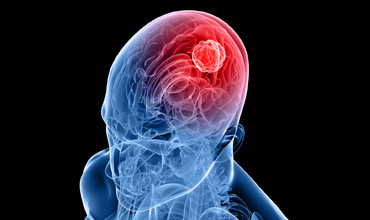
Brain Tumors – The Role of Monoclonal Antibodies Therapy and Challenges of Blood Brain Barriers
Abstract:
This review critically reviews the article monoclonal
antibodies therapy in neuro oncology The Brain tumors In applying mAb therapy
to brain tumors, both expectations and interpretation are seems difficult due
to blood-brain barrier (BBB).It prevents the antibodies from entry into the
brain but in case of brain tumors their entry is more complex. Brain tumors
(the target), antibodies (the magic), how antibodies attack tumor (the bullet)
and how they reach it (through blood brain barrier) are reviewed .With this as
introduction, practical experience with mAbs for brain tumor targets is by Clinical
experience with mAbs in brain tumor therapy indicates that it is less
inherently toxic than the conventional therapies and far safer for widespread
delivery
Three of the best-studied antibody/target combinations
Bevacizumab and GBM. It hard to define the effect of the antibody itself
on tumor growth bevacizumab primarily reduces edema. Other questions concern
response criteria. How to weigh overall survival as opposed to progression-free
survival; Rituximab and PCNSL Rituximab targets the common B-cell marker CD20
PCNSL, which is typically a B-cell lymphoma. Trastuzumab and metastastic breast
cancer Monoclonal antibodies (mAbs) serve as tumor-specific magic bullets in
two ways. As bullets, they would move through the blood to reach and attack
tumor targets and specificity of a single antibody would provide the magic ,
breast cancer patients respond to systemic mAb treatment, but then metastases
appear in the brain. Limitations of clinical trials and drawbacks of
pre-clinical models interpretation of clinical results difficult - increase in
overall or progression-free survival, or simply an improved quality of life,
are certainly of benefit to brain tumor patients- delivery strategies and tumor
sites
References:
[1.] Beduneau, A., Saulnier, P., & Benoit, JP., (2007).
Active targeting of brain tumors using nanocarriers. Biomaterials.
28:4947–4967.
[2.] Cheng, X., & Hung, MC., (2007). Breast cancer
brain metastases. Cancer Metastasis 26:635–643.
[3.] Choi, YK., & Kim, KW.,(2008). Blood-neural
barrier: its diversity and coordinated cell-to-cell communication.
[4.] Deeken, JF.,& Loscher, W., (2007). The blood-brain
barrier and cancer: transporters, treatment and Trojan horses.
[5.] Ferreri, AJ., & Reni, M.,( 2007). Primary central
nervous system lymphoma. Crit Rev Oncol Hematol.
[6.] Gerstner, ER., & Fine, RL.,( 2007). Increased
permeability of the blood-brain barrier to chemotherapy in metastatic brain
tumors: establishing a treatment paradigm.
[7.] Kim, WY.,& Lee, HY.,( 2009).Brain angiogenesis in
developmental and pathological processes: mechanism and therapeutic
intervention in brain tumors.
[8.] Neelapu, SS., Kwak, LW., Kobrin, CB., Reynolds, CW.,
Janik, JE., & Dunleavy, K,, et al.( 2005).Vaccine-induced tumor-specific
immunity despite severe B-cell depletion in mantle cell lymphoma.
[9.] Poulsen, HS., Grunnet, K., Sorensen, M., Olsen, P.,
Hasselbalch, B., & Nelausen, K,, et al. . (2009). Bevacizumab plus
irinotecan in the treatment patients with progressive recurrent malignant brain
tumours.
[10.] Rubenstein, JL., Kim, J., Ozawa, T., Zhang, M.,
Westphal, M.,& Deen, DF., et al(2000).Anti-VEGF antibody treatment of
glioblastoma prolongs survival but results in increased vascular cooption.
Neoplasia.
[11.] Sathornsumetee, S., Rich, & JN.,(
2007).Antiangiogenic therapy in malignant glioma: promise and challenge.
Pubmed-NCBI.
[12.] Saunders, NR., Ek, CJ.,& Habgood, MD.,( 2008).
Dziegielewska KM, Barriers in the brain: a renaissance.
[13.] Strome, SE., Sausville, EA., & Mann, D.,(2007)A
mechanistic perspective of monoclonal antibodies in cancer therapy beyond
target-related effects. Oncologist12:1084–1095.
[14.] Takahashi, JA., Llena, JF., & Hirano, A.,(1996)
Pathology of cerebral metastases. Neurosurg Clin N Am.7:345–367.

