[1]. Adejumo, O. A., Olusola-Faleye,
B., Adepoju, V., Bowale, A., Adesola, S., Falana, A., Owuna, H., Otemuyiwa, K.,
Oladega, S., Adegboye, O., 2018. Prevalence of rifampicin resistant
tuberculosis and associated factors among presumptive tuberculosis patients in
a secondary referral hospital in Lagos Nigeria. Afr Health Sci. 18(3), 472-478.
[2]. Adejoro, L., 2023,
Lagos records 52,652 TB cases in four years – Commissioner. Punch, https://punchng.com/lagos-records-52652-tb-cases-in-four-years-commissioner/
[3]. Adepoju, V. A.,
Etuk, V., Adepoju, O. E., Ogbudebe, C., Adeniyi, M. O., Akerele, B. K.,
Adejumo, O. A., 2022, Knowledge and awareness of tuberculosis in the urban slums
of lagos, Nigeria. The Nigerian Health Journal, Volume 22 No 1, January
to March 2022.
[4]. Adigun, R. and
Singh, R., 2023, Tuberculosis. In: StatPearls [Internet]. Treasure Island (FL):
StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441916/
[5]. Akindele, J.,
Joshua-Oladepo, O., Akano, Richard., 2022, Linguistic Diversity, Nigerian
Indigenous languages and the choice of the english language for nigeria's
national sustainability. voices: A Journal of English Studies, Vol. 6,
72-83.
[6]. Balogun, M. R.,
Sekoni, A. O., Meloni, S. T., Odukoya, O. O., Onajole, A. T., Longe-Peters, O. A.,
2019, Predictors of tuberculosis knowledge, attitudes and practices in urban
slums in Nigeria: a cross-sectional study. Pan Afr Med J, 32:60.
[7]. Baquero-Artigao,
F., Del Rosal, T., Falcón-Neyra, L., Ferreras-Antolín, L., Gómez-Pastrana, D.,
Hernanz-Lobo, A., Méndez-Echevarría, A., Noguera-Julian, A., Pascual Sánchez,
M. T., Rodríguez-Molino, P., Piñeiro-Pérez, R., Santiago-García, B.,
Soriano-Arandes, A., 2023, en representación de los grupos de trabajo en
tuberculosis de la sociedad española de infectología pediátrica y la sociedad
española de neumología pediátrica, update on the diagnosis and treatment of
tuberculosis. Anales de pediatria, 98(6), 460–469.
[8]. Barbosa-Amezcua,
M., Galeana-Cadena, D., Alvarado-Peña, N., Silva-Herzog, E., 2022, The microbiome
as part of the contemporary view of tuberculosis disease. Pathogens,
11:584.
[9]. Behnaz, F.,
Mohammadzade, G., Mousavi-e-Roknabadi, R. S., Mohammadzadeh, M., 2014,
Assessment of knowledge, attitudes and practices regarding tuberculosis among
final year students in Yazd, Central Iran. Journal of epidemiology and
global health, 4(2), 81–85.
[10]. Bensalah, N.,
Hsairi, M., Snene, H., et al., 2017, Community knowledge, attitude, and
practices towards tuberculosis in Tunisia. European Respiratory Journal,
Vol. 50, article PA2612.
[11]. Comberiati, P.,
Di Cicco, M., Paravati, F., Pelosi, U., Di Gangi, A., Arasi, S., Barni, S.,
Caimmi, D., Mastrorilli, C., Licari, A., Chiera, F., 2021, The Role of gut and
lung microbiota in susceptibility to tuberculosis. Int J Environ Res Public
Health, 21;18(22):12220.
[12]. Craciun, O. M.,
Torres, M. D. R., Llanes, A. B., Romay-Barja, M., 2023, Tuberculosis Knowledge,
Attitudes, and practice in middle- and low-income countries: a systematic review.
Journal of tropical Medicine. 2023, 1014666.
[13]. Federal
Ministry of Health, 2020, Department of Public Health. The national strategic
plan for tuberculosis control: towards universal access to prevention,
diagnosis and treatment (2015–2020). abuja: national tuberculosis and leprosy
control programme.
[14]. Fisher, R. A., 1935,
The Logic of Inductive Inference (with discussion). Journal of Royal
Statistical Society, 98, 39–82.
[15]. Ikoba, N. A. and
Jolayemi, E. T., 2021, Investigation of factors contributing to indigenous
language decline in nigeria. The Philippine Statistician, Volume 69,
Number 2 (2020).
[16]. Kalu, O. O. and
Jimmy, E. E., 2015, Assessment of knowledge, attitude and tuberculosis-related
social stigma among school adolescent in a semi-urban town in Cross River
State, Nigeria. International Journal of Education and research, Vol. 3,
no. 2, pp. 81–90.
[17]. Kasa, A. S.,
Minibel, A. and Bantie, G. M., 2019, Knowledge, attitude and preventive
practice towards tuberculosis among clients visiting public health facilities.
BMC Res Notes 12, 276.
[18]. Macrotrends,
2022, Lagos Nigeria Metro Area Population 1950-2021. Accessed: 20/02/2022.
Available from https://www.macrotrends.net/cities/22007/lagos/population
[19]. Meo,
C. M., Sari, N. K. P. M., Suhardin, S., Halimatunisa, M., 2020, Impact of tb
stigma and intervention strategies: A systematic review. International
Journal of Psychosocial Rehabilitation, 24, 7949-7963.
[20]. Mushtaq, M. U.,
Shahid, U., Abdullah, H. M., et al., 2011, Urban-rural inequities in knowledge,
attitudes and practices regarding tuberculosis in two districts of Pakistan’s
Punjab province. International Journal for Equity in Health, Vol. 10,
no. 1, pg. 8.
[21]. Oladele, D. A.,
Balogun, M. R., Odeyemi, K., Salako, B. L., 2020, A Comparative Study of
Knowledge, attitude, and determinants of tuberculosis-associated stigma in
rural and urban communities of lagos state, nigeria. Tuberculosis Research
and Treatment, Vol 2020: Page 14.
[22]. Onyeonoro, U. U.,
Chukwu, J. N., Oshi, D. C., Nwafor, C. C., and Meka, A. O., 2014, Assessment of
tuberculosis-related knowledge, attitudes and practices in Enugu, Southeast
Nigeria. Journal of Infectious Diseases and Immunity, Vol. 6, no. 1, pp.
1–9.
[23]. Pengpid, S.,
Peltzer, K., Puckpinyo, A., Tiraphat, S., Viripiromgool, S., 2016, Knowledge,
attitudes, and practices about tuberculosis and choice of communication
channels in Thailand. J Infect Dev Ctries, 10(7):694–703.
[24]. Sagili, K. D.,
Satyanarayana, S. and Chadha S. S., 2016, Is knowledge regarding tuberculosis
associated with stigmatising and discriminating attitudes of general population
towards tuberculosis patients? Findings from a community-based survey in 30
districts of India. PLoS One, Vol. 11, no. 2, article e0147274.
[25]. Sermrittirong,
S., Van Brakel, W. H., Kraipui, N., Traithip, S. and Bunders-aelen, J., 2015, Comparing
the perception of community members towards leprosy and tuberculosis
stigmatisation. Leprosy Review, Vol. 86, pp. 54–61.
[26]. Sharma, S. K.,
Mohan, A., Sharma, A., Mitra, D. K., 2005, Miliary tuberculosis: New insights
into an old disease. Lancet Infect. Dis, 5:415–430.
[27]. Solliman, M. A.,
Hassali, M. A., Al-Haddad M., et al., 2012, Assessment of knowledge towards
tuberculosis among general population in Northeast Libya,” Journal of
Applied Pharmaceutical Science, Vol. 2, no. 4, pp. 24–30.
[28]. Tobin, E. A.,
Okojie, P. W. and Isah, E.C., 2013, Community knowledge and attitude to
pulmonary tuberculosis in rural Edo state, Nigeria. Annals of African
Medicine, Vol. 12, no. 3, pp. 148–154.
[29]. Tolossa, D.,
Medhin, G. and M. Legesse, M., 2014, Community knowledge, attitude, and
practices towards tuberculosis in Shinile town, Somali regional state, eastern
Ethiopia: a cross-sectional study. BMC Public Health, Vol. 14, No.1:pg
804.
[30]. Vitoria, M.,
Granich, R., Gilks, C. F., Gunneberg, C., Hosseini, M., Were, W., 2009, The
global fight against HIV/AIDS, tuberculosis, malaria: current status and future
perspective. Am J Clin Pathol, 131(6): 844-848.
[31]. World Health
Organization, 2016, On the road to ending TB: highlights from the 30 highest TB
burden countries. Accessed: February 20, 2022. Available from https://apps.who.int/iris/handle/10665/204662
[32]. World Health
Organization, 2017, Guidelines on treatment of drug-susceptible tuberculosis
and patient care (2017 update), Geneva, https://apps.who.int/iris/bitstream/handle/10665/255052/9789241550000-eng.pdf
[33]. World Health
Organization, 2020, WHO consolidated guidelines on tuberculosis, Module 4:
Treatment -drug-resistant tuberculosis treatment. Geneva, https://www.who.int/publications/i/item/9789240007048
[34]. World Health
Organization, 2021, Global Tuberculosis Report 2021. WHO; 2021. Accessed: 20/02/2022.
https://www.who.int/publications/digital/global-tuberculosis-report-2021/prevention
[35]. World Health
Organization, 2022, WHO: Implementing the end TB strategy: the essentials.
Geneva: World Health Organization; Accessed: 20/02/2022. http://www.who.int/tb/publications/2015/end_tb_essential.pdf?ua=1
[36]. World Health Organization, 2023, Global Tuberculosis Report 2023, https://www.who.int/publications/i/item/9789240083851
 Local Content Policies in Petroleum-Rich Nations: A Comparative View of Four CountriesAuthor: Visham BudhooDOI: 10.21522/TIJAR.2014.12.01.Art001
Local Content Policies in Petroleum-Rich Nations: A Comparative View of Four CountriesAuthor: Visham BudhooDOI: 10.21522/TIJAR.2014.12.01.Art001 Impact of AI Technologies in Optimizing Manufacturing Processes in Manufacturing Industry in NigeriaAuthor: Osita AmaugoDOI: 10.21522/TIJAR.2014.12.01.Art002
Impact of AI Technologies in Optimizing Manufacturing Processes in Manufacturing Industry in NigeriaAuthor: Osita AmaugoDOI: 10.21522/TIJAR.2014.12.01.Art002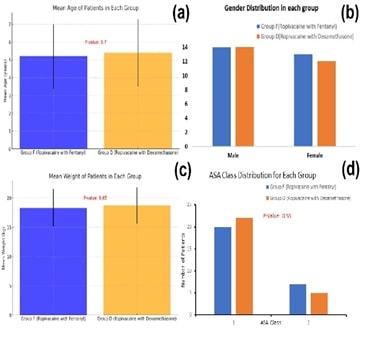 Analgesic Efficacy of Fentanyl and Dexamethasone with Caudal Ropivacaine in Pediatric Infraumbilical SurgeriesAuthor: Bhagyavardhan BottaDOI: 10.21522/TIJAR.2014.12.01.Art003
Analgesic Efficacy of Fentanyl and Dexamethasone with Caudal Ropivacaine in Pediatric Infraumbilical SurgeriesAuthor: Bhagyavardhan BottaDOI: 10.21522/TIJAR.2014.12.01.Art003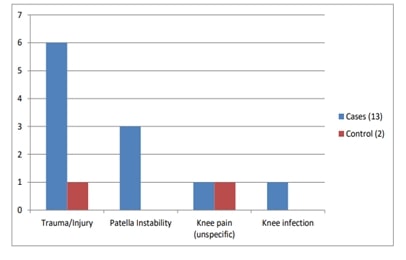 Childhood Knee Problem as a Risk Factor for Adulthood Knee Osteoarthritis: A Case-Control StudyAuthor: Altine Aliyu NuradeenDOI: 10.21522/TIJAR.2014.12.01.Art004
Childhood Knee Problem as a Risk Factor for Adulthood Knee Osteoarthritis: A Case-Control StudyAuthor: Altine Aliyu NuradeenDOI: 10.21522/TIJAR.2014.12.01.Art004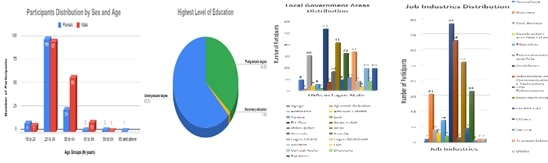 Assessment of Tuberculosis Awareness and Perspectives among the Working Population Across Lagos StateAuthor: Akande, Kehinde AyooluwaDOI: 10.21522/TIJAR.2014.12.01.Art005
Assessment of Tuberculosis Awareness and Perspectives among the Working Population Across Lagos StateAuthor: Akande, Kehinde AyooluwaDOI: 10.21522/TIJAR.2014.12.01.Art005 Application of Health Belief Model; Tuberculosis in Healthcare Workers: Risk Reduction Measures at Asokoro District Hospital (ADH) Abuja FCT NigeriaAuthor: Titilayo Oluwatoyin IlesanmiDOI: 10.21522/TIJAR.2014.12.01.Art006
Application of Health Belief Model; Tuberculosis in Healthcare Workers: Risk Reduction Measures at Asokoro District Hospital (ADH) Abuja FCT NigeriaAuthor: Titilayo Oluwatoyin IlesanmiDOI: 10.21522/TIJAR.2014.12.01.Art006 The Impact of Fintech and Digital Platforms on Financial Inclusion in the Informal Sector of GhanaAuthor: Felix SackeyDOI: 10.21522/TIJAR.2014.12.01.Art007
The Impact of Fintech and Digital Platforms on Financial Inclusion in the Informal Sector of GhanaAuthor: Felix SackeyDOI: 10.21522/TIJAR.2014.12.01.Art007 Current State of Financial Inclusion in the Informal Sector of GhanaAuthor: Felix SackeyDOI: 10.21522/TIJAR.2014.12.01.Art008
Current State of Financial Inclusion in the Informal Sector of GhanaAuthor: Felix SackeyDOI: 10.21522/TIJAR.2014.12.01.Art008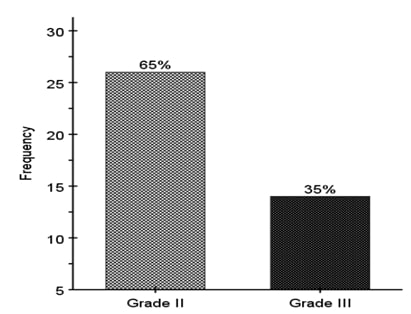 Prevalence of Breast Cancer in First Time Patients Visiting the Federal Medical Centre, Abuja, NigeriaAuthor: Aleruchi ChukuDOI: 10.21522/TIJAR.2014.12.01.Art009
Prevalence of Breast Cancer in First Time Patients Visiting the Federal Medical Centre, Abuja, NigeriaAuthor: Aleruchi ChukuDOI: 10.21522/TIJAR.2014.12.01.Art009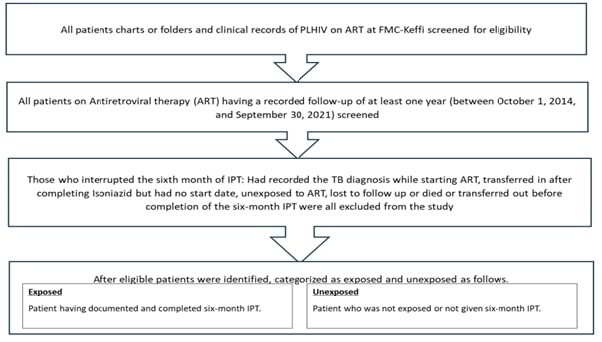 Effectiveness of Isoniazid Preventive Therapy among Patients on ART in Federal Medical Centre – Keffi, Nasarawa State, Nigeria: A Retrospective Cohort StudyAuthor: Samuel Eleojo AbujahDOI: 10.21522/TIJAR.2014.12.01.Art010
Effectiveness of Isoniazid Preventive Therapy among Patients on ART in Federal Medical Centre – Keffi, Nasarawa State, Nigeria: A Retrospective Cohort StudyAuthor: Samuel Eleojo AbujahDOI: 10.21522/TIJAR.2014.12.01.Art010 Prevalence and Determinants of Non-Communicable Diseases Risk Factors Among In-School Adolescents in Rural and Urban Areas of Adamawa StateAuthor: Jenewari, J. ADOI: 10.21522/TIJAR.2014.12.01.Art011
Prevalence and Determinants of Non-Communicable Diseases Risk Factors Among In-School Adolescents in Rural and Urban Areas of Adamawa StateAuthor: Jenewari, J. ADOI: 10.21522/TIJAR.2014.12.01.Art011 Association between Perceived Health Risks of Smoking and Cessation Intent among Youths in the Gambia: Global Youth Tobacco Survey (GYTS) 2017Author: Yankuba SinghatehDOI: 10.21522/TIJAR.2014.12.01.Art012
Association between Perceived Health Risks of Smoking and Cessation Intent among Youths in the Gambia: Global Youth Tobacco Survey (GYTS) 2017Author: Yankuba SinghatehDOI: 10.21522/TIJAR.2014.12.01.Art012 The Price of Transparency: How Exposing Personal Information in Mobile Money Transactions Fuels Social Engineering in GhanaAuthor: Daniel Adjei OdaiDOI: 10.21522/TIJAR.2014.12.01.Art013
The Price of Transparency: How Exposing Personal Information in Mobile Money Transactions Fuels Social Engineering in GhanaAuthor: Daniel Adjei OdaiDOI: 10.21522/TIJAR.2014.12.01.Art013
