Table of Contents - Issue
Recent articles
-
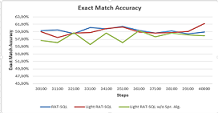 Light RAT-SQL: A RAT-SQL with More Abstraction and Less Embedding of Pre-existing RelationsAuthor: Nathan Manzambi NdongalaDOI: 10.21522/TIJAR.2014.10.02.Art001
Light RAT-SQL: A RAT-SQL with More Abstraction and Less Embedding of Pre-existing RelationsAuthor: Nathan Manzambi NdongalaDOI: 10.21522/TIJAR.2014.10.02.Art001Light RAT-SQL: A RAT-SQL with More Abstraction and Less Embedding of Pre-existing Relations
Abstract:
RAT-SQL is among the popular framework used in the Text-To-SQL challenges for jointly encoding the database relations and questions in a way to improve the semantic parser. In this work, we propose a light version of the RAT-SQL where we dramatically reduced the number of the preexisting relations from 55 to 7 (Light RAT-SQL-7) while preserving the same parsing accuracy. To ensure the effectiveness of our approach, we trained a Light RAT-SQL-2, (with 2 embeddings) to show that there is a statistically significant difference between RAT-SQL and Light RAT-SQL-2 while Light RAT-SQL-7 can compete with RAT-SQL.
Keywords: Deep learning, Natural Language Processing, Neural Semantic Parsing, Relation Aware Transformer, RAT-SQL, Text-To-SQL, Transformer.Light RAT-SQL: A RAT-SQL with More Abstraction and Less Embedding of Pre-existing Relations
References:
[1] B. Wang, R. Shin, X. Liu, O. Polozov, and M. Richardson (2020): “RAT-SQL: Relation-Aware Schema Encoding and Linking for Text-to-SQL Parsers, . [Online]. Available: https://github.com/Microsoft/rat-sql.
[2] B. Hui et al (Mar. 2022): “S$^2$SQL: Injecting Syntax to Question-Schema Interaction Graph Encoder for Text-to-SQL Parsers, [Online]. Available: http://arxiv.org/abs/2203.06958.
[3] T. Scholak, R. Li, D. Bahdanau, H. de Vries, and C. Pal (Oct. 2020): “DuoRAT: Towards Simpler Text-to-SQL Models, doi: 10.18653/v1/2021.naacl-main.103.
[4] T. Yu et al (Sep. 2020), “GraPPa: Grammar-Augmented Pre-Training for Table Semantic Parsing, [Online]. Available: http://arxiv.org/abs/2009.13845.
[5] Z. Lan et al (2020): “Albert: A Lite Bert For Self-Supervised Learning Of Language Representations. [Online]. Available: https://github.com/google-research/ALBERT.
[6] J. Devlin, Ming-Wei Chang, Kenton Lee, and Kristina Toutanova Bert-Ppt (2018): “BERT: Pre-training of Deep Bidirectional Transformers for Language Understanding (Bidirectional Encoder Representations from Transformers).
[7] E. Voita, D. Talbot, F. Moiseev, R. Sennrich, and I. Titov (2019), “Analyzing Multi-Head Self-Attention: Specialized Heads Do the Heavy Lifting, the Rest Can Be Pruned,” [Online]. Available: https://github.com/.
[8] E. F. Codd (1974), “Recent Investigations in Relational Data Base Systems,” in IFIP Congress.
[9] A. Suhr, S. Iyer, Y. Artzi, and P. G. Allen (2018), “Learning to Map Context-Dependent Sentences to Executable Formal Queries. [Online]. Available: https://github.com/clic-lab/atis.
[10] S. Iyer, I. Konstas, A. Cheung, J. Krishnamurthy, and L. Zettlemoyer (Apr. 2017): “Learning a Neural Semantic Parser from User Feedback, [Online]. Available: http://arxiv.org/abs/1704.08760.
[11] J. Herzig and J. Berant (Apr. 2018): “Decoupling Structure and Lexicon for Zero-Shot Semantic Parsing, [Online]. Available: http://arxiv.org/abs/1804.07918.
[12] A. Kamath and R. Das (Dec. 2018), “A Survey on Semantic Parsing”, [Online]. Available: http://arxiv.org/abs/1812.00978.
[13] L. Dong and M. Lapata (May 2018): “Coarse-to-Fine Decoding for Neural Semantic Parsing”, [Online]. Available: http://arxiv.org/abs/1805.04793.
[14] L. Dong and M. Lapata (Jan. 2016): “Language to Logical Form with Neural Attention”, [Online]. Available: http://arxiv.org/abs/1601.01280.
[15] O. Goldman, V. Latcinnik, U. Naveh, A. Globerson, and J. Berant (Nov. 2017): “Weakly-supervised Semantic Parsing with Abstract Examples,”, [Online]. Available: http://arxiv.org/abs/1711.05240.
[16] P. Yin and G. Neubig (Oct. 2018): “TRANX: A Transition-based Neural Abstract Syntax Parser for Semantic Parsing and Code Generation”, [Online]. Available: http://arxiv.org/abs/1810.02720.
[17] P. Yin and G. Neubig (Apr. 2017), “A Syntactic Neural Model for General-Purpose Code Generation”, [Online]. Available: http://arxiv.org/abs/1704.01696.
[18] C. Xiao, M. Dymetman, and C. Gardent (2016): “Sequence-based Structured Prediction for Semantic Parsing,” [Online]. Available: https://github.com/percyliang/sempre.
[19] J. Krishnamurthy, P. Dasigi, and M. Gardner (2017): “Neural Semantic Parsing with Type Constraints for Semi-Structured Tables.
[20] V. L. Shiv and C. Quirk (2019): “Novel positional encodings to enable tree-based transformers,” in Advances in Neural Information Processing Systems, vol. 32.
[21] Q. He, J. Sedoc, and J. Rodu (Dec. 2021): “Trees in transformers: a theoretical analysis of the Transformer’s ability to represent trees, [Online]. Available: http://arxiv.org/abs/2112.11913.
[22] N. Kitaev, Ł. Kaiser, and A. Levskaya (Jan. 2020): “Reformer: The Efficient Transformer”, [Online]. Available: http://arxiv.org/abs/2001.04451.
[23] A. Vaswani et al (Jun. 2017): “Attention Is All You Need”, [Online]. Available: http://arxiv.org/abs/1706.03762.
[24] J. Guo et al (2019): “Towards Complex Text-to-SQL in Cross-Domain Database with Intermediate Representation.
[25] R. Cao, L. Chen, Z. Chen, Y. Zhao, S. Zhu, and K. Yu (Jun. 2021): “LGESQL: Line Graph Enhanced Text-to-SQL Model with Mixed Local and Non-Local Relations, [Online]. Available: http://arxiv.org/abs/2106.01093.
[26] X. V. Lin, R. Socher, and C. Xiong (Dec. 2020): “Bridging Textual and Tabular Data for Cross-Domain Text-to-SQL Semantic Parsing”, [Online]. Available: http://arxiv.org/abs/2012.12627.
[27] A. Gur, S. Yavuz, Y. Su, and X. Yan, “DialSQL: Dialogue Based Structured Query Generation.
[28] B. Bogin, M. Gardner, and J. Berant (2019): “Global Reasoning over Database Structures for Text-to-SQL Parsing.
[29] B. Bogin, M. Gardner, and J. Berant (Apr. 08, 2022): “Representing Schema Structure with Graph Neural Networks for Text-to-SQL Parsing,” pp. 4560–4565, 2019, Accessed [Online]. Available: https://github.com/benbogin/.
[30] C. Xu, W. Zhou, T. Ge, F. Wei, and M. Zhou (2020), “BERT-of-Theseus: Compressing BERT by Progressive Module Replacing . [Online]. Available: https://en.wikipedia.org/wiki/Ship_.
[31] M. Shoeybi, M. Patwary, R. Puri, P. Legresley, J. Casper, and B. Catanzaro, “Megatron-LM (2020): Training Multi-Billion Parameter Language Models Using Model Parallelism,” [Online]. Available: https://github.com/.
[32] V. Sanh, L. Debut, J. Chaumond, and T. Wolf (Oct. 2019): “Distilbert, a distilled version of BERT: smaller, faster, cheaper and lighter, [Online]. Available: http://arxiv.org/abs/1910.01108.
[33] M. Lewis et al (Oct. 2019): “BART: Denoising Sequence-to-Sequence Pre-training for Natural Language Generation, Translation, and Comprehension, [Online]. Available: http://arxiv.org/abs/1910.13461.
[34] Alec Radford, Karthik Narasimhan, Tim Salimans, and Ilya Sutskever (2018): “Improving Language Understanding by Generative Pre-Training, [Online]. Available: https://gluebenchmark.com/leaderboard.
[35] A. Radford, J. Wu, R. Child, D. Luan, D. Amodei, and I. Sutskever (2019): “Language Models are Unsupervised Multitask Learners, [Online]. Available: https://github.com/codelucas/newspaper.
[36] Y. Liu et al (Jul. 2019): “RoBERTa: A Robustly Optimized BERT Pretraining Approach,” [Online]. Available: http://arxiv.org/abs/1907.11692.
[37] T. Wolf et al (Oct. 2019): “HuggingFace’s Transformers: State-of-the-art Natural Language Processing” [Online]. Available: http://arxiv.org/abs/1910.03771.
[38] T. B. Brown et al (2020): “Language Models are Few-Shot Learners. [Online]. Available: https://commoncrawl.org/the-data/.
[39] W. Fedus, B. Zoph, and N. Shazeer (2022): “Switch Transformers: Scaling to Trillion Parameter Models with Simple and Efficient Sparsity.
[40] K. Clark, M.-T. Luong, Q. v. Le, and C. D. Manning (Mar. 2020): “Electra: Pre-training Text Encoders as Discriminators Rather Than Generators, [Online]. Available: http://arxiv.org/abs/2003.10555.
[41] T. Scholak, N. Schucher, and D. Bahdanau (Sep. 2021): “PICARD: Parsing Incrementally for Constrained Auto-Regressive Decoding from Language Models [Online]. Available: http://arxiv.org/abs/2109.05093.
[42] C. Raffel et al (Oct. 2019): “Exploring the Limits of Transfer Learning with a Unified Text-to-Text Transformer, [Online]. Available: http://arxiv.org/abs/1910.10683.
[43] J. Herzig, P. K. Nowak, T. Müller, F. Piccinno, and J. Eisenschlos (2020): “TaPas: Weakly Supervised Table Parsing via Pre-training, . doi: 10.18653/v1/2020.acl-main.398.
[44] L. Zhao, H. Cao, and Y. Zhao (Jan. 2021) “GP: Context-free Grammar Pre-training for Text-to-SQL Parsers,” [Online]. Available: http://arxiv.org/abs/2101.09901.
[45] X. Deng, A. H. Awadallah, C. Meek, O. Polozov, H. Sun, and M. Richardson (Oct. 2020), “Structure-Grounded Pretraining for Text-to-SQL,” doi: 10.18653/v1/2021.naacl-main.105.
[46] P. Yin, G. Neubig, W. Yih, and S. Riedel (May 2020): “TaBERT: Pretraining for Joint Understanding of Textual and Tabular Data,” pp. 8413–8426, doi: 10.48550/arxiv.2005.08314.
[47] P. Shaw, J. Uszkoreit, G. Brain, and A. Vaswani (2018): “Self-Attention with Relative Position Representations.
[48] O. Vinyals, M. Fortunato, and N. Jaitly (Jun. 2015): “Pointer Networks,” [Online]. Available: http://arxiv.org/abs/1506.03134.
[49] M. Schuster and K. K. Paliwal (1997): “Bidirectional recurrent neural networks,” IEEE Transactions on Signal Processing, vol. 45, no. 11, doi: 10.1109/78.650093.
[50] K. Cho, B. van Merriënboer, D. Bahdanau, and Y. Bengio (2014): “On the properties of neural machine translation: Encoder–decoder approaches,” in Proceedings of SSST 2014 - 8th Workshop on Syntax, Semantics and Structure in Statistical Translation. doi: 10.3115/v1/w14-4012.
[51] S. Hochreiter and J. Schmidhuber (1997): “Long Short-Term Memory,” Neural Comput, vol. 9, no. 8, doi: 10.1162/neco.1997.9.8.1735.
[52] T. Yu et al (Sep. 2018): “Spider: A Large-Scale Human-Labeled Dataset for Complex and Cross-Domain Semantic Parsing and Text-to-SQL Task,” [Online]. Available: http://arxiv.org/abs/1809.08887.
[53] C. D. Manning, M. Surdeanu, J. Bauer, J. Finkel, S. J. Bethard, and D. Mcclosky (2014), “The Stanford CoreNLP Natural Language Processing Toolkit.
[54] J. Pennington, R. Socher, and C. D. Manning (2014): “GloVe: Global Vectors for Word Representation, [Online]. Available: http://nlp.
[55] Y. Gal and Z. Ghahramani (2016): “A Theoretically Grounded Application of Dropout in Recurrent Neural Networks.
[56] A. Paszke et al (2019): “PyTorch: An Imperative Style, High-Performance Deep Learning Library.
[57] D. P. Kingma and J. Ba (Dec. 2014): “Adam: A
Method for Stochastic Optimization, [Online]. Available: http://arxiv.org/abs/1412.6980.Viewed PDF 1881 67 -
 Effect of Marketing Occupational Therapy Services on Client-Centredness in NigeriaAuthor: Victor Oghenenyerovwome IkiDOI: 10.21522/TIJAR.2014.10.02.Art002
Effect of Marketing Occupational Therapy Services on Client-Centredness in NigeriaAuthor: Victor Oghenenyerovwome IkiDOI: 10.21522/TIJAR.2014.10.02.Art002Effect of Marketing Occupational Therapy Services on Client-Centredness in Nigeria
Abstract:
This study assesses marketing strategies that can be adopted in marketing occupational therapy (OT); ascertains the target of OT marketing efforts and identified the barriers to client-centredness in OT. All these were with the view to investigate the extent to which marketing OT services influence client-centredness in Nigeria. A purposive sampling technique was used to select 33 currently licensed and practicing OT practitioners in Nigeria who responded to questions like the types of marketing strategies that OT can adopt, target for OT marketing efforts, the extent to which marketing OT can influence client-centredness, and barriers to client-centredness in OT. Data were summarized using descriptive statistics while the major objective of the study was tested using a one-way analysis of variance. The results of this survey showed that marketing strategies like building relationships with physicians and professionals allied to medicine, improving quality of service and professionalism, and digital marketing/internet have a significant effect on client-centredness in terms of occupational therapists’ desire for professionalism in practice, and respect for client’s subjective experience in occupational performance; targets for OT marketing efforts are clients, physicians and professionals allied to medicine, donors, community services, business managers, developers and investors, policy makers, insurance companies, and attorneys; and barriers to client-centredness in OT are inefficiency of the facility, lack of client demand to contribute during goal-setting and decision making, clients are not aware of client-centredness, indifference and lack of motivation of clients toward achieving occupational performance amongst others. In conclusion, marketing occupational therapy services can significantly affect client-centredness in Nigeria.
Keywords: Client-centredness, Marketing, Nigeria, Occupational therapy, Services.
Effect of Marketing Occupational Therapy Services on Client-Centredness in Nigeria
References:
[1] About Occupational Therapy | WFOT, Date of Access: 14/02/2023. https://wfot.org/about/about-occupational-therapy.
[2] Creek J., 2008, The knowledge base of occupational therapy. In: Occupational therapy and mental health, edited by Creek J., and Lougher, L., 4th ed. (Philadelphia: Elsevier Health Sciences), pp. 31-35.
[3] Client-centredness in Occupational Therapy (Archived) | WFOT, Date of Access: 14/02/2023. https://www.wfot.org/resources/client-centredness-in-occupational-therapy.
[4] Marketing and the 7Ps: A Brief Summary of Marketing and How it Works, Date of Access: 14/02/2023. https://www.cim.co.uk/media/4772/7ps.pdf.
[5] Kotler, P., and Armstrong G., 2000, Principles of Marketing (Englewood Cliffs: Prentice-Hall Incorporated).
[6] Corring, D. J., and Cook, J. V., 1999, Client-centred care means that I am a valued human being. Canadian Journal of Occupational Therapy, 66(2), 71-82. https://doi.org/10.1177/000841749906600203.
[7] Pollock, N., 1993, Client-Centered Assessment. The American Journal of Occupational therapy, 74(4), 298-301. https://doi.org/10.5014/ajot.47.4.298.
[8] Medical Rehabilitation Therapists (Registration) Board of Nigeria - Occupational Therapy (mrtb.gov.ng), Date of Access: 14/02/2023. https://www.mrtb.gov.ng/en/registration/licensure-status/2017/occupational-therapy.
[9] ‘The ratio of occupational therapists to Nigerians is one to a million’ | The Guardian Nigeria News - Nigeria and World News — Features — The Guardian Nigeria News – Nigeria and World News, Date of Access: 14/02/2023. https://guardian.ng/features/health/the-ratio-of-occupational-therapists-to-nigerians-is-one-to-a-million/.
[10] Eleyinde, S. T., Lashmann, B. Y., Olosunde, O. S., and Olugbode, I. O., 2012, Occupational Therapy in Nigeria: Past, Present, and Future. World Federation of Occupational Therapists Bulletin, 65 (1), 62-64, https://doi.org/10.1179/otb.2012.65.1.011.
[11] Eleyinde, S. T., Amu, V., and Eleyinde, A. O, 2018, Recent Development of Occupational Therapy in Nigeria: Challenges and Opportunities. World Federation of Occupational Therapists Bulletin, 74(26), 1-7, https://doi.org/10.1080/14473828.2018.1426543.
[12] Morley, M., and Rennison, J., 2011, Marketing occupational therapy: everybody’s business. British Journal of Occupational Therapy 74(8), 406-408. https://doi.org/10.4276/030802211X13125646371040.
[13] Penn, B., and Penn, J., 1990, Marketing Occupational Therapy: Imperative for the Future? British Journal of Occupational Therapy, 53(2), 64-66. https://doi.org/10.1177/030802269005300207.
[14] Jacobs, K., 1987, Marketing Occupational Therapy. The American Journal of Occupational Therapy, 41(5), 315-320. https://doi.org/10.5014/ajot.41.5.315.
[15] Kash, B. A., and Deshmuck, A. A., 2013, Developing a Strategic Marketing Plan for Physical and Occupational Therapy Services: A Collaborative Project Between a Critical Access Hospital and a Graduate Program in Health Care Management. Health Marketing Quarterly, 30(3), 263-280. https://doi.org/10.1080/07359683.2013.814507.
[16] Beaton, J., 1995, Marketing Occupational Therapy: The Future. The British Journal of Occupational Therapy, 58(4), 145-145. https://doi.org/10.1177/030802269505800401.
[17] Greenhill, E. D., 1994, Are Occupational Therapists Marketing their Services Effectively to the Fundholding General Practitioners? British Journal of Occupational Therapy, 57(4), 133-136. https://doi.org/10.1177/030802269405700408.
[18] Chakravorty, B. G., 1993, Occupational Therapy Services: Awareness among Hospital Consultants and General Practitioners. British Journal of Occupational Therapy, 56(8), 283-286. https://doi.org/10.1177/030802269305600804.
[19] Harms, S., and Law, M., 2001, Issues in Bidding for Contracts for Occupational Therapy Services.
Canadian Journal of Occupational Therapy, 68(3), 157-163. https://doi.org/10.1177/000841740106800304.[20] Wressle, E., and Samuelsson, K., 2009, Barriers and Bridges to Client-Centred Occupational Therapy in Sweden. Scandinavian Journal of Occupational Therapy, 11(1), 12-16. https://doi.org/10.1080/11038120410019135.
[21] Maitra, K. K., and Erway, F., 2006, Perception of Client-Centered Practice. The American Journal of Occupational Therapy, 60(3), 298-310. https://doi.org/10.5014/ajot.60.3.298.
[22] Sumsion, T., and Smyth, G., 2000, Barriers to Client-Centredness and their Resolutions. Canadian Journal of Occupational Therapy, 67(1), 15-21. https://doi.org/10.1177/000841740006700104.
Viewed PDF 1560 50 -
 Patient Safety: A Systematic Review of the Literature with Evidence based Measures to Improve Patient Safety in Healthcare SettingsAuthor: Daniel LunguDOI: 10.21522/TIJAR.2014.10.02.Art003
Patient Safety: A Systematic Review of the Literature with Evidence based Measures to Improve Patient Safety in Healthcare SettingsAuthor: Daniel LunguDOI: 10.21522/TIJAR.2014.10.02.Art003Patient Safety: A Systematic Review of the Literature with Evidence based Measures to Improve Patient Safety in Healthcare Settings
Abstract:
Patient safety is a crucial component of healthcare delivery aimed at minimizing and preventing medical errors that can cause harm or injury to patients. This systematic review identified 50 studies that evaluated interventions aimed at improving patient safety in healthcare settings, including medication reconciliation, surgical safety checklists, hand hygiene programs, and electronic health record systems. The findings suggest that most interventions led to significant improvements in patient safety outcomes, including a reduction in adverse events and preventable harm. Evidence-based measures to improve patient safety include effective communication, hand hygiene, medication safety, patient identification, fall prevention, surgical safety, infection control, and staff training. The implementation of these measures can help improve patient safety and reduce the risk of harm to patients in healthcare settings. Further research is needed to identify the most effective interventions and to evaluate the long-term impact of these interventions on patient outcomes.
Keywords: Adverse events, Interventions, Medical errors, Patient safety, Preventable harm.
Patient Safety: A Systematic Review of the Literature with Evidence based Measures to Improve Patient Safety in Healthcare Settings
References:
[1] National Institute for Health and Care Excellence. (2021). Patient safety. Retrieved from https://www.nice.org.uk/about/what-we-do/our-programmes/nice-guidance/nice-guidelines/patient-safety.
[2] National Patient Safety Foundation. (2018). Patient safety primer. Retrieved from https://www.npsf.org/patient-safety-education-resources/patient-safety-primer/.
[3] World Health Organization. (2019). Patient safety. Retrieved from https://www.who.int/patientsafety/en/.
[4] Joint Commission. (2021). Patient safety. Retrieved from https://www.jointcommission.org/topics/patient-safety/.
[5] Singh, D., Agusti, A., Anzueto, A., Barnes, P.J., Bourbeau, J., Celli, B.R., Criner, G.J., Frith, P., Halpin, D.M., Han, M., and Varela, M.V.L., 2019. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease: the GOLD science committee report 2019. European Respiratory Journal, 53(5).
[6] World Alliance for Patient Safety. (2009). Forward programme 2009-2013. Retrieved from https://www.who.int/patientsafety/information_centre/reports/Alliance_FwdProg_EN.pdf.
[7] Agency for Healthcare Research and Quality. (2020). Patient safety network. Retrieved from https://psnet.ahrq.gov/.
[8] Brennan, T.A., 2000. The Institute of Medicine report on medical errors—could it do harm? New England Journal of Medicine, 342(15), pp.1123-1125.
[9] Rosen, M.A., DiazGranados, D., Dietz, A.S., Benishek, L.E., Thompson, D., Pronovost, P.J. and Weaver, S.J., 2018. Teamwork in healthcare: Key discoveries enabling safer, high-quality care. American Psychologist, 73(4), p.433.
[10] Weaver, S.J., Weeks, K., Pham, J.C. and Pronovost, P.J., 2014. On the CUSP: Stop BSI: Evaluating the relationship between central line–associated bloodstream infection rate and patient safety climate profile. American Journal of Infection Control, 42(10), pp. S203-S208.
[11] Aiken, L.H., Cerón, C., Simonetti, M., Lake, E.T., Galiano, A., Garbarini, A., Soto, P., Bravo, D. and Smith, H.L., 2018. Hospital nurse staffing and patient outcomes. Revista Médica Clínica las Condes, 29(3), pp.322-327.
[12] Makary, M.A. and Daniel, M., 2016. Medical error—the third leading cause of death in the US. Bmj, 353.
[13] Singer, T. and Lamm, C., 2009. The social neuroscience of empathy. Annals of the New York Academy of Sciences, 1156(1), pp.81-96.
[14] Vimalananda, V., Dvorin, K., Fincke, B.G., Tardiff, N. and Bokhour, B.G., 2018. Patient, PCP, and specialist perspectives on specialty care coordination in an integrated health care system. The Journal of ambulatory care management, 41(1), p.15.
[15] Leape, L.L., Shore, M.F., Dienstag, J.L., Mayer, R.J., Edgman-Levitan, S., Meyer, G.S. and Healy, G.B., 2012. Perspective: a culture of respect, part 1: the nature and causes of disrespectful behavior by physicians. Academic Medicine, 87(7), pp.845-852.
[16] Bates, S.M., Rajasekhar, A., Middeldorp, S., McLintock, C., Rodger, M.A., James, A.H., Vazquez, S.R., Greer, I.A., Riva, J.J., Bhatt, M. and Schwab, N., 2018. American Society of Hematology 2018 guidelines for management of venous thromboembolism: venous thromboembolism in the context of pregnancy. Blood Advances, 2(22), pp.3317-3359.
[17] West, C.P., Dyrbye, L.N., Erwin, P.J. and Shanafelt, T.D., 2016. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. The Lancet, 388(10057), pp.2272-2281.
[18] Makary, M.A. and Daniel, M., 2016. Medical error—the third leading cause of death in the US. Bmj, 353.
[19] Donaldson, M.S., Corrigan, J.M. and Kohn, L.T. eds., 2000. To err is human: building a safer health system.
[20] Leape, L.L., 2000. Institute of Medicine medical error figures are not exaggerated. Jama, 284(1), pp.95-97.
[21] Luftman, J., Zadeh, H.S., Derksen, B., Santana, M., Rigoni, E.H. and Huang, Z., 2013. Key information technology and management issues 2012-2013: an international study. Journal of Information Technology, 28(4), pp.354-366.
[22] Knaul, F.M., Farmer, P.E., Krakauer, E.L., De Lima, L., Bhadelia, A., Kwete, X.J., Arreola-Ornelas, H., Gómez-Dantés, O., Rodriguez, N.M., Alleyne, G.A. and Connor, S.R., 2018. Alleviating the access abyss in palliative care and pain relief—an imperative of universal health coverage: the Lancet Commission report. The Lancet, 391(10128), pp.1391-1454.
[23] Russ, S.J., Sevdalis, N., Moorthy, K., Mayer, E.K., Rout, S., Caris, J., Mansell, J., Davies, R., Vincent, C. and Darzi, A., 2015. A qualitative evaluation of the barriers and facilitators toward implementation of the WHO surgical safety checklist across hospitals in England: lessons from the “Surgical Checklist Implementation Project”. Annals of surgery, 261(1), pp.81-91.
[24] Rabbani, A.H., Hayat, K., Gardezi, F.H., Waheed, A. and Zahra, A., 2018. A comparison of nalbuphine and pentazocine in controlling post-operative pain in dogs. Matrix Sci. Med, 2(2), pp.15-20.
[25] Skaugset, L.M., Farrell, S., Carney, M., Wolff, M., Santen, S.A., Perry, M. and Cico, S.J., 2016. Can you multitask? Evidence and limitations of task switching and multitasking in emergency medicine. Annals of emergency medicine, 68(2), pp.189-195.
[26] Cameron, I.D., Dyer, S.M., Panagoda, C.E., Murray, G.R., Hill, K.D., Cumming, R.G. and Kerse, N., 2018. Interventions for preventing falls in older people in care facilities and hospitals. Cochrane database of systematic reviews, (9).
Viewed PDF 1461 91 -
 Revisiting the Endogeneity of Adolescent Pregnancy and Child Marriage in Low- and Middle-Income Countries: A Review with Practical SolutionsAuthor: Barnabas MwansaDOI: 10.21522/TIJAR.2014.10.02.Art004
Revisiting the Endogeneity of Adolescent Pregnancy and Child Marriage in Low- and Middle-Income Countries: A Review with Practical SolutionsAuthor: Barnabas MwansaDOI: 10.21522/TIJAR.2014.10.02.Art004Revisiting the Endogeneity of Adolescent Pregnancy and Child Marriage in Low- and Middle-Income Countries: A Review with Practical Solutions
Abstract:
Adolescence is an important time for promoting health and preventing disease. The World Health Organization (WHO) defines an adolescent as an individual in the 10-19 years age group and usually uses the term young person to denote those between 10 and 24 years. Adolescent health encompasses changing transitions within multiple domains, including the physical, social, emotional, cognitive, and intellectual. These changes have important implications for health. During this period of increasing independence, adolescents face critical choices about health-related behaviors in areas such as sexuality, physical activity, diet, and use of health care services. These behaviors affect health during adolescence and young adulthood and, in the long-term, are related to many of the leading causes of adult morbidity and mortality. Therefore, the protection and promotion of health during this life stage is of great importance and has been shown to yield benefits not only for adolescents now, but also for their future adult lives and for their future children. This paper explore two key issues underpinning adolescent health, teen pregnancy, and child marriage. Trends in early marriage and early childbearing help determine national poverty levels and economic productivity. Decisions about whether to remain in school, whether to marry, or whether to engage in sexual activity have implications for education and health. The paper argues that failure to understand the interrelationship between adolescent pregnancy and child marriage may jeopardize earlier investments in maternal and child health, erodes future quality and length of life, and escalates suffering, inequality, and social instability.
Keywords: Adolescent Health, Child Marriage, Teen Pregnancy.Revisiting the Endogeneity of Adolescent Pregnancy and Child Marriage in Low- and Middle-Income Countries: A Review with Practical Solutions
References:
[1] WHO. Adolescent pregnancy: WHO factsheet. 2022 https://www.who.int/news-room/fact-sheets/detail/adolescent-pregnancy (accessed March 15,2023).
[2] WHO.The Global Health Observatory available online https://www.who.int/data/gho/indicator-metadata-registry/imr-details/4669 (accessed March 15, 2023).
[3] Siniša F (2018) Adolescent Pregnancy is a Serious Social Problem. J Gynecol Res Obstet.
[4] Sedgh G et al. (2015). Adolescent pregnancy, birth, and abortion rates across countries: levels and recent trends. J Adolesc Health. 2015 Feb;56(2):223-30.
[5] Huda MM et al. (2020) Time trends and sociodemographic inequalities in the prevalence of adolescent motherhood in 74 low-income and middle-income countries: a population-based study. Lancet Child & Adolescent Health. 2020.
[6] United Nations, Department of Economic and Social Affairs (UNDESA), Population Division. World population prospects 2019. Online edition, revision 1, 2019. https://population.un.org/wpp/.
[7] UNFPA (2013a). Adolescent pregnancy: A review of the evidence. New York: UNFPA; 2013.
[8] UNFPA (2013b). Motherhood in Childhood: Facing the challenge of adolescent pregnancy. New York: UNFPA; 2013.
[9] UNICEF. Child marriage, Adolescent pregnancy, and Family formation in West and Central Africa: Patterns, trends, and drivers of change. New York: UNICEF; 2015.
[10] Petroni S et al. (2017) New findings on child marriage in sub-Saharan Africa. Annals of global health. 2017.
[11] WHO (FACTSHEET,2023) Adolescent Pregnancy https://www.who.int/news-room/fact-sheets/detail/adolescent-pregnancy (accessed March 10,2023).
[12] UNFPA (2017) Adolescent pregnancy: A matter of human rights https://www.unfpa.org/adolescent-pregnancy#readmore-expand (accessed March 15, 2023).
[13] Patton GC, Coffey C, Sawyer SM, et al. Global patterns of mortality in young people: a systematic analysis of population health data. The Lancet. 2009.
[14] Maheshwari MV, Khalid N, Patel PD, Alghareeb R, Hussain A. Maternal and Neonatal Outcomes of Adolescent Pregnancy: A Narrative Review. Cureus. 2022 Jun.
[15] National Research Council (US) Panel on Adolescent Pregnancy and Childbearing; Hofferth SL, Hayes CD, editors. Risking the Future: Adolescent Sexuality, Pregnancy, and Childbearing, Volume II: Working Papers and Statistical Appendices. Washington (DC): National Academies Press (US); 1987. Chapter 8, The Children of Teen Childbearers. Available from: https://www.ncbi.nlm.nih.gov/books/NBK219236/.
[16] Ahman E, Shah IH (2011). New estimates and trends regarding unsafe abortion mortality. Journal of Gynecology and Obstetrics. 2011 Nov.
[17] United Nations Children’s Fund (UNICEF). Undernourished and Overlooked: A Global Nutrition Crisis in Adolescent Girls and Women. UNICEF Child Nutrition Report Series, 2022. UNICEF, New York, 2023.
[18] UNICEF. Progress for Children. A Report Card on Adolescents. New York, NY, USA: UNICEF; 2012.
[19] United Nations Children’s Fund. Covid-19: A threat to progress against child marriage. UNICEF, New York, 2021.
[20] UNICEF (2014) Ending child marriage: progress and prospects. New York: UNICEF, 2014. https://gdc.unicef.org/resource/ending-child-marriage-progress-and-prospects. (Accessed March 16, 2023.
[21] Centre for Reproductive Rights. Adolescent sexual and reproductive health and rights. Centre for Reproductive Rights. https://reproductiverights.org/our-issues/adolescent-sexual-and-reproductive-health-and-rights/. (Accessed March 16, 2023).
[22] Nour NM. Health consequences of child marriage in Africa. Emerg Infect Dis.
[23] Presler-Marshall, E.; Jones, N. (2012). Charting the future: Empowering girls to prevent early pregnancy. London: Overseas Development Institute (ODI) and Save the Children.
[24] Hindin, M. J. & Fatusi, A. O. (2009). Adolescent sexual and reproductive health in developing countries: an overview of trends and interventions. Int Perspect Sex Reprod Health, 35(2), 58-62.
[25] Erulkar, A. (2013). Adolescence lost: the realities of child marriage. J Adolesc Health, 52(5), 513-514.
[26] Jensen, R.; Thornton, R. (2003). Early Female Marriage in the Developing World. Gender and Development, 11(2), 11.
[27] UNFPA and Save the Children. Adolescent Sexual and Reproductive Health: Toolkit for Humanitarian Settings. A Companion to the Inter-Agency Field Manual on Reproductive Health in Humanitarian Settings. UNFPA and Save the Children, September 2009.
[29] Nguyen, M. C.; Wodon, Q. (2012). Global Trends in Child Marriage. Washington, DC, USA: World Bank
[30] Mensch, B. S.; Grant, M.J.; Blanc, A.K. (2006). The Changing Contect of Sexual Initiation in Sub-Saharan Africa. Population and Development Review.
[31] Population Council (2014). BALIKA (Bangladeshi Association for Life Skills, Income, and Knowledge for Adolescents) Retrieved March 31, 2014.
[32] Mekonnen, T., Dune, T. & Perz, J. Maternal health service utilisation of adolescent women in sub-Saharan Africa: A Systematic scoping review. BMC Pregnancy Childbirth 19, 366 (2019).
[34] Ninsiima, L.R., Chiumia, I.K. & Ndejjo, R. Factors influencing access to and utilisation of youth-friendly sexual and reproductive health services in sub-Saharan Africa: A Systematic Review. Reprod Health 18, 135 (2021).
[35] Geary RS, Gómez-Olivé FX, Kahn K, Tollman S, Norris SA. Barriers to and facilitators of the provision of a youth-friendly health services programme in rural South Africa. BMC Health Serv Res. 2014;14(1):1–8.
[36] Mazur A, Brindis CD, Decker MJ. Assessing youth-friendly sexual and reproductive health services: A Systematic Review. BMC Health Serv Res. 2018;18(1):1–12.
[37] Onukwugha FI, Hayter M, Magadi MA. Views of service providers and adolescents on use of sexual and reproductive health services by adolescents: a systematic review. Afr J Reprod Health. 2019.
[38] Efevbera Y, Bhabha J, Farmer P, Fink G. Girl child marriage, socioeconomic status, and undernutrition: evidence from 35 countries in Sub-Saharan Africa. BMC Med. 2019 Mar 8;17(1):55.
[39] Loaiza SE, Wong S. Marrying too young: end of child marriage. New York: United Nations Population Fund; 2012.
[40] Lloyd, C. B., & Mensch, B. S. (2008). Marriage and childbirth as factors in dropping out from school: an analysis of DHS data from sub-Saharan Africa.
[41] Psaki et al. (2021) What Are the Drivers of Child Marriage? A Conceptual Framework to Guide Policies and Programs. J Adolescent Health. 2021.
[42] Munthali AC, Zulu EM. The timing and role of initiation rites in preparing young people for adolescence and responsible sexual and reproductive behaviour in Malawi. Afr J Reprod Health. 2007 Dec;11(3):150-67.
[43] Crooks, R., Bedwell, C. & Lavender, T. Adolescent experiences of pregnancy in low-and middle-income countries: a meta-synthesis of qualitative studies. BMC Pregnancy Childbirth 22, 702 (2022).
[44] Jaruseviciene L et al (2014) Perceptions of quality in primary health care: perspectives of patients and professionals based on focus group discussions. BMC Fam Pract. 2014 Jun 28; 15:128.
[45] Khan, S.; Mishra, V. (2008). Youth Reproductive and Sexual Health DHS Comparative Reports. Calverton, MD, USA: Macro International Inc.
[46] Girls as Brides (2015) Setting the age of marriage at 18 can have a huge impact on child marriage https://www.girlsnotbrides.es/articulos/three-laws-that-countries-can-adopt-to-address-child-marriage/ (accessed March 17, 2023).
Viewed PDF 956 19 -
 Factors Associated with Accessibility and Utilization of Adolescent Health Services in Chingola, ZambiaAuthor: Judith MusondaDOI: 10.21522/TIJAR.2014.10.02.Art005
Factors Associated with Accessibility and Utilization of Adolescent Health Services in Chingola, ZambiaAuthor: Judith MusondaDOI: 10.21522/TIJAR.2014.10.02.Art005Factors Associated with Accessibility and Utilization of Adolescent Health Services in Chingola, Zambia
Abstract:
The purpose of this paper was to explore the factors associated with accessibility and utilization of adolescent health services in Chingola, Zambia. The study was done among secondary school students in their junior and senior grades. Data were collected from four focus group discussions and four key informants’ interviews. Data management analysis principles illuminating verbatim quotations are used to illustrate findings. The study findings indicate that lack of information and stigmatization were some of the factors identified to be the barriers to adolescents’ health. The paper further outlines the proposed solutions which include establishing and strengthening the linkage between the schools and health facilities adolescent health services and creating awareness among the adolescents. Further, the paper gives the future direction that clinics and health centres should take advantage of technology and use electronic means to increase awareness of available reproductive health services for adolescents and that they should have door to door programs for the community aimed at sensitizing adolescents on reproductive health. In conclusion, it is indicated that improving the utilization of adolescent health services is a global dream. This dream can be realized only if the efforts are made to reach the adolescent population.
Keywords: Accessibility, Adolescent Health Services, Stigmatization, Utilization.Factors Associated with Accessibility and Utilization of Adolescent Health Services in Chingola, Zambia
References:
[1] World Health Organization [WHO] (2015). A standards-driven approach to improve the quality of healthcare services for adolescents. WHO; Geneva available at: https://www.who.int/publications-detail-redirect/9789241549332.
[4] Ramarao, J. K, and Costello, A. (2013) A reproductive health approach to the objectives and assessment of family planning programs. In: G. Sen, A. Germain, & L. Chen (Eds.), Population policies reconsidered: Health, empowerment, and rights (pp. 193–210). Boston, MA: Harvard University Press. Available at: https://www.hup.harvard.edu/catalog.php?isbn=9780674690035.
[5] Shivaram K, Nandini C., and Malleshappa1 K. (2021) Knowledge and attitude about reproductive health among rural adolescent girls in Kuppam mandal: an intervention study. Biomed Res;14(3):305–310. https://www.researchgate.net/publication/285867336_Knowledge_and_attitude_about_reproductive_health_among_rural_adoles-cent_girls_in_Kuppam_mandal_An_intervention_study.
[6] Thongmixay S, Essink DR, De Greeuw T, Vongxay V, Sychareun V, Broerse JE. (2019) Perceived barriers in accessing sexual and reproductive health services for youth in Lao People’s Democratic Republic. PLoS One;14(10): e0218296. https://doi.org/10.1371/journal.pone.0218296.
[8] Central Statistical Office (CSO). (2019) Zambia Demographic and Health Survey 2019. Calverton, Maryland, USA: CSO and Macro International Inc. chrome-extension://efaidnbmnnnibpcajpcglclefindmkaj/https://dhsprogram.com/pubs/pdf/FR361/FR361.pdf.
[9] Ministry of Health (2011) Adolescent Health Strategic Plan 2011-2015. Ministry of Health, Lusaka. Available at: https://healtheducationresources.unesco.org/library/documents/adolescent-health-strategic-plan-2011-2015#:~:text=The%20national%20Adolescent%20Health%20Strategic,throughout%20the%20country%2C%20aimed%20at.
[10] Nkonde-Bwalya, B. (2016). Factors affecting access to and utilisation of reproductive health services among adolescents in Lusaka District: case study of Kamanga Compound. University of Zambia, Lusaka (Unpublished thesis). Avalaible at: http://dspace.unza.zm/bitstream/handle/123456789/4697/Barbara%27%20s%20Dissertation_2016.pdf?sequence=1&isAllowed=y.
[11] United Nations International Children’s Emergency Fund [UNICEF] (2016). For every child end aids – seventh stocktaking report. UNICEF; New York, NY: https://www.unicef.org/reports/every-child-end-aids-seventh-stocktaking-report-2016.
[13] Aaron, A. A. and Anaba, A. B. (2018). Barriers on access to and use of adolescent health services in Ghana. Journal of Health Research 33(3) pp. 197-207 https://www.emerald.com/insight/content/doi/10.1108/JHR-10-2018-0119/full/html.
[14] Mukondwa, K., Gonah, L. (2016). Accessing Adolescent Sexual and Reproductive Health Services among Undocumented Migrants in South Africa: A Documentary Review. Medical Journal of Zambia, 43 (4): 247 – 251 https://www.ajol.info/index.php/mjz/article/view/152180.
[18] World Health Organization. Adolescent (2018) Health risks and solutions [homepage on the Internet]. 2018 [cited 2017 May 01]. Available from: http://www.who.int/news-room/fact-sheets/detail/adolescents-health-risks-and-solutions.
[19] Hale DR, Viner RM. (2016) The correlates and course of multiple health risk behaviour in adolescence. BMC Public Health;16(1):458. https://doi.org/10.1186/s12889-016-3120-z.
Viewed PDF 995 34 -
 Secondary School Students’ Mathematics Anxiety: A Zimbabwean PerspectiveAuthor: Caleb MoyoDOI: 10.21522/TIJAR.2014.10.02.Art006
Secondary School Students’ Mathematics Anxiety: A Zimbabwean PerspectiveAuthor: Caleb MoyoDOI: 10.21522/TIJAR.2014.10.02.Art006Secondary School Students’ Mathematics Anxiety: A Zimbabwean Perspective
Abstract:
This study employed a mixed-methods technique to examine the spectrum of mathematics anxiety levels felt and expressed by Zimbabwean students studying Ordinary level mathematics. Ninety-one pupils from forms 3 and 4 (N = 91) made up the convenient sample; of them, 41 were male and 50 were female. The instrument used was the Hopko-adapted amalgamated mathematics anxiety scale (aMAS) (2003). While focus group conversations were audio recorded and transcribed to explore in-depth, social settings and learning environments that cause anxiety, the quantitative data was analysed using SPSS, version 23.0. The key categories were then thematically classified and analysed with quantitative information. To test a hypothesis based on the data, an independent samples t-test was run to see whether males and females’ anxiety levels differed by mean. The results showed that the participants experienced significant mathematics anxiety, and many situations—including parental and social pressure, instructional methods, and learning environments—reinforce math fear. Findings also show that, society exerts significant pressure on learners due to high expectations of success in mathematics. Additionally, some teachers were viewed as fuelling the anxiety through their repertoire and that classroom environments may unintentionally cause discomfort to mathematically challenge peers. Interesting suggestions were made by respondents regarding how to help people with math anxiety. The study offers a compelling case for its relevance to teacher education, research, and instructional practice. The study also recommends conducting comparative studies as one method of comprehending the issue.
Keywords: Cognitive achievement, Mathematics-anxiety, Teaching-learning, Gender issues, Social phenomena.Secondary School Students’ Mathematics Anxiety: A Zimbabwean Perspective
References:
[1] R. Hembree, “The nature, effects, and relief of mathematics anxiety,” J. Res. Math. Educ., vol. 21, no. 1, pp. 33–46, 1990.
[2] M. H. Ashcraft, “Math anxiety: Personal, educational, and cognitive consequences,” Curr. Dir. Psychol. Sci., vol. 11, no. 5, pp. 181-185., 2002.
[3] E. Carey, F. Hill, A. Devine, and D. Szűcs, “The modified abbreviated math anxiety scale: A valid and reliable instrument for use with children,” Front. Psychol., vol. 8, no. 1, p. 11, 2017.
[4] P. B. Cemen, “The nature of mathematics anxiety (report no. SE 048 689),” Stillwater OK Okla. State Univ. ERIC Doc. Reprod. Serv. No ED287729, 1987.
[5] R. M. Suinn and E. H. Winston, “The mathematics anxiety rating scale, a brief version: psychometric data,” Psychol. Rep., vol. 92, no. 1, pp. 167-173., 2003.
[6] K. H. Dew, J. P. Galassi, and M. D. Galassi, “Math anxiety: Relation with situational test anxiety, performance, physiological arousal, and math avoidance behavior,” J. Couns. Psychol., vol. 31, no. 4, p. 580, 1984.
[7] E. Zakaria, N. M. Zain, N. A. Ahmad, and A. Erlina, “Mathematics anxiety and achievement among secondary school students,” Am. J. Appl. Sci., vol. 9, no. 11, p. 1828, 2012.
[8] R. M. Liebert and L. W. Morris, “Cognitive and emotional components of test anxiety: A distinction and some initial data,” Psychol. Rep., vol. 20, no. 3, pp. 975–978, 1967.
[9] A. Wigfield and J. L. Meece, “Math anxiety in elementary and secondary school students.,” J. Educ. Psychol., vol. 80, no. 2, p. 210, 1988.
[10] Alzahrani and E. Stojanovski, “Assessment of anxiety on mathematics for students in secondary school in Qatar,” Proceedings–22nd Int. Congr. Model. Simul. MODSIM 2017, 2017.
[11] P. Mutodi and H. Ngirande, “Exploring Mathematics Anxiety: Mathematics Students’ Experiences,” Mediterr. J. Soc. Sci., 2014.
[12] S. E. Ruff and S. R. Boes, “The Sum of All Fears: The Effects of Math Anxiety on Math Achievement in Fifth Grade Students and the Implications for School Counsellors,” Ga. Sch. Couns. Assoc. J., vol. 21, no. 1, p. n1, 2014.
[13] J. J. Rolison, K. Morsanyi, and E. Peters, “The role of math anxiety, subjective numeracy, and objective numeracy,” Med. Decis. Making, vol. 40, no. 2, pp. 222–234, 2020.
[14] Arem, “Conquering math anxiety,” Nelson Educ., 2009.
[15] Denhere, “Casual attributions of maths anxiety among Zimbabwean secondary school – learners,” Int. J. Acad. Res. Reflect., vol. 3, no. 1, 2015.
[16] M. Lyons and S. L. Beilock, “Math Anxiety Predicts Pain Network Activation in Anticipation of Doing Math.,” PLoS ONE, vol. 7, no. 10, 2012, doi: (10): e48076.doi: 10.1371/journal.pone.0048076.
[17] B. Young, S. S. Wu, and V. Menon., “The neurodevelopmental basis of math anxiety,” Psychol. Sci., vol. 23, no. 5, pp. 492–501, 2012.
[18] R. D. Zettle and L. Houghton L., “The relationship between mathematics anxiety and social desirability as a function of gender,” Coll. Stud. J., vol. 32, no. 1, pp. 81–86, 1998.
[19] M. Kyttala and P. M. Bjorn, “The role of literacy skills in adolescents’ mathematics word problem performance: Controlling for visuo-spatial ability and mathematics anxiety,” Learn. Individ. Differ. vol. 29, no. 1, pp. 59–66, 2014.
[20] T. Khatoon and S. Mahmood, “Mathematics anxiety among secondary school students in India and its relationship to achievement in mathematics,” Eur. J. Soc. Sci. 161, vol. 16, no. 1, pp. 75–86, 2010.
[21] Dove, J. Montague, and T. E. Hunt, “An exploration of primary school teachers’ maths anxiety using interpretative phenomenological analysis,” Int. Online J. Prim. Educ. IOJPE, vol. 10, no. 1, pp. 32–49, 2021.
[22] M. I. Núñez-Peña, M. Suárez-Pellicioni, G. Guilera, and C. Mercadé-Carranza, “A Spanish version of the short mathematics anxiety rating scale (sMARS),” Learn. Individ. Differ, vol. 24, no. 1, pp. 204–210, 2013.
[23] Cipora, K. Willmes, A. Szwarc, and H. Nuerk C., “Norms and validation of the online and paper-and-pencil versions of the Abbreviated Math Anxiety Scale (AMAS) for Polish adolescents and adults,” J. Numer. Cogn, vol. 3, no. 3, pp. 667–693, 2018.
[24] J. M. Furner and M. L. Duffy, “Equity for all students in the new millennium: Disabling math anxiety,” Interv. Sch. Clin., vol. 38, no. 2, pp. 67–74, 2002.
[25] A. Maloney, Erin, G. Ramirez, E. Gundeson A., C. Susan, and S. C. Beilock, “Intergenerational effects of parents’ math anxiety on children’s math achievement and anxiety,” Psychol. Sci., vol. 26, no. 9, pp. 1480–1488, 2015.
[26] S. Haimovitz and C. Dweck, “What predicts children fixed and growth intelligence mind-sets? Not their parents’ views of intelligence but their parents’ views of failure,” Psychol. Sci., vol. 27, no. 6, pp. 859–869, 2016.
[27] Clark, “Reducing student frustration through math instruction,” 2020, [Online]. Available: http://hdl.handle.net/20.500.11803/873.
[28] M. Marshall, R. V. Staddon, D. A. Wilson, and V. E. Mann, “Addressing maths anxiety and engaging students with maths within the curriculum,” MSOR Connect., vol. 15, no. 3, 2016.
[29] S. Mandina, S. Mashingaidze S., and J. Mafuta, “Increasing female participation in advanced level mathematics: A perspective from students and teachers in Zimbabwe,” Afr. Educ. Res. J., vol. 1, no. 3, pp. 183–190, 2013.
[30] C. Primi et al., “The Early Elementary School Abbreviated Math Anxiety Scale (the EES-AMAS): A newly adapted version of the AMAS to measure math anxiety in young children,” Front. Psychol., vol. 11, no. 1, p. 1014, 2020.
[31] B. Taylor A. and B. J. Fraser, “The Influence of Classroom Environment on High School Students’ Mathematics Anxiety,” Pap. Present. Annu. Meet. Am. Educ. Res. Assoc. Chic. IL April 21, 2003, 2003.
[32] World Health Organisation, “Communicating risk in public health emergencies: a WHO guideline for emergency risk communication (ERC) policy and practice,” WHO, 2017.
[33] D. R. Hopko, “The abbreviated math anxiety scale (AMAS) construction, validity, and reliability,” Assess. 102 178-182, vol. 10, no. 2, pp. 178–182, 2003.
[34] K. Huysamen, “Metodologie vir die sosiale en gedragswetenskappe. Boekuitgewers (Edms),” BpkHalfweghuis South., p. 125, 1993.
A. Dowker and H. Sheridan, “Relationships between mathematics performance and attitude to mathematics: influences of gender, test anxiety, and working memory,” Front. Psychol., vol. 13, no. 1, 2022.
[35] T, E. Hunt, V. Simms., A. Cahoo, and C. M. Muwonge, “Socio-cognitive-affective barriers to mathematics education in developing nations,” Encycl. UN Sustain. Dev. GoalsQuality Educ. Springer, 2021.
Viewed PDF 1295 44 -
 Dental Pulp Stem Cells in Regenerative TherapyAuthor: Prabhadevi MaganurDOI: 10.21522/TIJAR.2014.10.02.Art007
Dental Pulp Stem Cells in Regenerative TherapyAuthor: Prabhadevi MaganurDOI: 10.21522/TIJAR.2014.10.02.Art007Dental Pulp Stem Cells in Regenerative Therapy
Abstract:
Stem cells, also known as progenitor/precursor cells, have the unique trait of self-renewal and multi-lineage differentiation. Dental stem cells (DSCs) are holding a pivotal role during recent times as they thrive as the cornerstone for the development of cell transplantation therapies that correct periodontal disorders and damaged dentin. DSCs are used therapeutically for different organ systems and numerous diseases, including neurological disorders, diabetes, liver disease, bone tissue engineering, and dentistry. In dentistry, the focus is on predominantly regenerating the pulp and damaged dentin, repairing perforations, and periodontal regenerations. Above all, whole tooth regeneration has been constantly under research. The next decade could be a crucial junction where huge leaps in stem cell-based regenerative therapies could become a reality with successful tissue engineering therapies this could be a biological alternative to synthetic materials that are in use currently. But dental stem cells have their share of challenges for which the research must happen effectively adhering to social responsibilities at all levels.
Keywords: Stem cells, Regeneration, Regenerative therapy, SHED.Dental Pulp Stem Cells in Regenerative Therapy
References:
[1] Chalisserry, E. P., Nam, S. Y., Park, S. H., & Anil, S., 2017, Therapeutic potential of dental stem cells. Journal of Tissue Engineering, 8, 2041731417702531.
[2] Nakao, K., & Tsuji, T., 2008, Dental regenerative therapy: Stem cell transplantation and bioengineered tooth replacement, Japanese dental science review, 44(1), 70-75.
[3] Nakashima, M., & Akamine, A., 2005, The application of tissue engineering to regeneration of pulp and dentin in endodontics. Journal of Endodontics, 31(10), 711–718.
[4] Nakashima, M., Iohara, K., Murakami, M., Nakamura, H., Sato, Y., Ariji, Y., & Matsushita, K., 2017, Pulp regeneration by transplantation of dental pulp stem cells in pulpitis: a pilot clinical study. Stem cell research & therapy, 8(1), 61.
[5] Soudi, A., Yazdanian, M., Ranjbar, R., Tebyanian, H., Yazdanian, A., Tahmasebi, E., Keshvad, A., & Seifalian, A., 2021, Role and application of stem cells in dental regeneration: A comprehensive overview. Excli Journal, 20, 454–489.
[6] Bansal, R., & Jain, A., 2015, Current overview on dental stem cells applications in regenerative dentistry. Journal of Natural Science, Biology, and Medicine, 6(1), 29–34.
[7] Mason, C., & Dunnill, P., 2008. A brief definition of regenerative medicine. Regenerative Medicine, 3(1), 1–5.
[8] Gronthos, S., Mankani, M., Brahim, J., Robey, P. G., & Shi, S., 2000, Postnatal human dental pulp stem cells (DPSCs) in vitro and in vivo. Proceedings of the National Academy of Sciences of the United States of America, 97(25), 13625–13630.
[9] Panitvisai, P., & Messer, H. H.,1995, Cuspal deflection in molars in relation to endodontic and restorative procedures. Journal of endodontics, 21(2), 57–61.
[10] Schwartz, R. S., & Robbins, J. W., 2004, Post placement and restoration of endodontically treated teeth: a literature review. Journal of Endodontics, 30(5), 289–301.
[11] Yoshida, S., Tomokiyo, A., Hasegawa, D., Hamano, S., Sugii, H., & Maeda, H., 2020, Insight into the Role of Dental Pulp Stem Cells in Regenerative Therapy. Biology, 9(7), 160.
[12] Guo, R., & Yu, J., 2022, Multipotency & immunomodulatory Benefits of Stem Cells from Human Exfoliated Deciduous Teeth: Front. Dent. Med, 3, 805875.
[13] Miura, M., Gronthos, S., Zhao, M., Lu, B., Fisher, L. W., Robey, P. G., & Shi, S., 2003, SHED: stem cells from human exfoliated deciduous teeth. Proceedings of the National Academy of Sciences of the United States of America, 100(10), 5807–5812.
[14] Rosa, V., Zhang, Z., Grande, R. H., & Nör, J. E., 2013, Dental pulp tissue engineering in full-length human root canals. Journal of Dental Research, 92(11), 970–975.
[15] Cordeiro, M. M., Dong, Z., Kaneko, T., Zhang, Z., Miyazawa, M., Shi, S., Smith, A. J., & Nör, J. E., 2008, Dental pulp tissue engineering with stem cells from exfoliated deciduous teeth. Journal of Endodontics, 34(8), 962–969.
[16] Zhai, Q., Dong, Z., Wang, W., Li, B., & Jin, Y., 2019, Dental stem cell and dental tissue regeneration. Frontiers of Medicine, 13(2), 152–159.
[17] Iohara, K., Imabayashi, K., Ishizaka, R., Watanabe, A., Nabekura, J., Ito, M., Matsushita, K., Nakamura, H., & Nakashima, M., 2011, Complete pulp regeneration after pulpectomy by transplantation of CD105+ stem cells with stromal cell-derived factor-1. Tissue engineering. Part A, 17(15-16), 1911–1920.
[18] Rosa, V., Zhang, Z., Grande, R. H., & Nör, J. E., 2013, Dental pulp tissue engineering in full-length human root canals. Journal of dental research, 92(11), 970–975.
[19] Gronthos, S., Mankani, M., Brahim, J., Robey, P. G., & Shi, S., 2000, Postnatal human dental pulp stem cells (DPSCs) in vitro and in vivo. Proceedings of the National Academy of Sciences of the United States of America, 97(25), 13625–13630.
[20] Gronthos, S., Brahim, J., Li, W., Fisher, L. W., Cherman, N., Boyde, A., DenBesten, P., Robey, P. G., & Shi, S., 2002, Stem cell properties of human dental pulp stem cells. Journal of dental research, 81(8), 531–535.
[21] Wang, J., Ma, H., Jin, X., Hu, J., Liu, X., Ni, L., & Ma, P. X., 2011, The effect of scaffold architecture on odontogenic differentiation of human dental pulp stem cells. Biomaterials, 32(31), 7822–7830.
[22] Wang, J., Ma, H., Jin, X., Hu, J., Liu, X., Ni, L., & Ma, P. X., 2011, The effect of scaffold architecture on odontogenic differentiation of human dental pulp stem cells. Biomaterials, 32(31), 7822–7830.
[23] Batouli, S., Miura, M., Brahim, J., Tsutsui, T. W., Fisher, L. W., Gronthos, S., Robey, P. G., & Shi, S., 2003, Comparison of stem-cell-mediated osteogenesis and dentinogenesis. Journal of dental research, 82(12), 976–981.
[24] Sun, H. H., Chen, B., Zhu, Q. L., Kong, H., Li, Q. H., Gao, L. N., Xiao, M., Chen, F. M., & Yu, Q., 2014, Investigation of dental pulp stem cells isolated from discarded human teeth extracted due to aggressive periodontitis. Biomaterials, 35(35), 9459–9472.
[25] Chun, S. Y., Lee, H. J., Choi, Y. A., Kim, K. M., Baek, S. H., Park, H. S., Kim, J. Y., Ahn, J. M., Cho, J. Y., Cho, D. W., Shin, H. I., & Park, E. K., 2011, Analysis of the soluble human tooth proteome and its ability to induce dentin/tooth regeneration. Tissue engineering. Part A, 17(1-2), 181–191.
[26] Takeda, T., Tezuka, Y., Horiuchi, M., Hosono, K., Iida, K., Hatakeyama, D., Miyaki, S., Kunisada, T., Shibata, T., & Tezuka, K., 2008, Characterization of dental pulp stem cells of human tooth germs. Journal of dental research, 87(7), 676–681.
[27] Moussa, D. G., & Aparicio, C., 2019, Present and future of tissue engineering scaffolds for dentin-pulp complex regeneration. Journal of tissue engineering and regenerative medicine, 13(1), 58–75.
[28] Petersen, P. E., & Ogawa, H., 2005, Strengthening the prevention of periodontal disease: the WHO approach. Journal of periodontology, 76(12), 2187–2193.
[29] Seo, B.M., Miura, M., Gronthos, S., Bartold, P.M., Batouli, S., Brahim, J., Young, M., Robey, P.G., Wang, C.Y., Shi, S., 2004, Investigation of multipotent postnatal stem cells from human periodontal ligament. Lancet, 364: 149-155.
[30] Shi, S., Gronthos, S., Chen, S., Reddi, A., Counter, C. M., Robey, P. G., & Wang, C. Y., 2002, Bone formation by human postnatal bone marrow stromal stem cells is enhanced by telomerase expression. Nature biotechnology, 20(6), 587–591.
[31] Aoki, A., Mizutani, K., Schwarz, F., Sculean, A., Yukna, R. A., Takasaki, A. A., Romanos, G. E., Taniguchi, Y., Sasaki, K. M., Zeredo, J. L., Koshy, G., Coluzzi, D. J., White, J. M., Abiko, Y., Ishikawa, I., & Izumi,. Y.,2015, Periodontal and peri-implant wound healing following laser therapy. Periodontology 2000, 68(1), 217–269.
[32] Tsumanuma, Y., Iwata, T., Washio, K., Yoshida, T., Yamada, A., Takagi, R., Ohno, T., Lin, K., Yamato, M., Ishikawa, I., Okano, T., & Izumi, Y., 2011, Comparison of different tissue-derived stem cell sheets for periodontal regeneration in a canine 1-wall defect model. Biomaterials, 32(25), 5819–5825.
[33] Han, J., Menicanin, D., Marino, V., Ge, S., Mrozik, K., Gronthos, S., & Bartold, P. M., 2014, Assessment of the regenerative potential of allogeneic periodontal ligament stem cells in a rodent periodontal defect model. Journal of periodontal research, 49(3), 333–345.
[34] Ninomiya, T., Hiraga, T., Hosoya, A., Ohnuma, K., Ito, Y., Asashima, M., & Nakamura, H.,2014, Enhanced Bone-Forming Activity of Side Population Cells in the Periodontal Ligament. Cell Transplantation. 2014;23(6):691-701.
[35] Kuo, T.F., Huang, A.T., Chang, H.H., Lin, F.H., Chen, S.T., Chen, r.S., Chou, C.H., Lin, H.C., Chiang, H., & Chen, M.H., 2008, Regeneration of dentin-pulp complex with cementum and periodontal ligament formation using dental bud cells in gelatin-chondroitin-hyaluronan tri-copolymer scaffold in swine. Journal of Biomedical Materials research. Part A. 2008 Sep;86(4):1062-1068.
[36] Robey, P.G., & Bianco, P., 2006, The use of adult stem cells in rebuilding the human face. J Am Dent Assoc, 137(7): 961–972.
[37] Aly L. A., 2015, Stem cells: Sources, and regenerative therapies in dental research and practice. World journal of stem cells, 7(7), 1047–1053.
[38] Duailibi, M. T., Duailibi, S. E., Young, C. S., Bartlett, J. D., Vacanti, J. P., & Yelick, P. C., 2004, Bioengineered teeth from cultured rat tooth bud cells. Journal of dental research, 83(7), 523–528.
[39] Sumita, Y., Honda, M. J., Ohara, T., Tsuchiya, S., Sagara, H., Kagami, H., & Ueda, M., 2006, Performance of collagen sponge as a 3-D scaffold for tooth-tissue engineering. Biomaterials, 27(17), 3238–3248.
[40] Honda, M. J., Tsuchiya, S., Sumita, Y., Sagara, H., & Ueda, M., 2007, The sequential seeding of epithelial and mesenchymal cells for tissue-engineered tooth regeneration. Biomaterials, 28(4), 680–689.
[41] Yamamoto, H., Kim, E. J., Cho, S. W., & Jung, H. S., 2003, Analysis of tooth formation by reaggregated dental mesenchyme from mouse
embryo. Journal of electron microscopy, 52(6), 559–566.[42] Hu, B., Nadiri, A., Bopp-Kuchler, S., Perrin-Schmitt, F., Wang, S., Lesot, H., 2005, Dental epithelial histo-morphogenesis in the mouse: positional information versus cell history. Arch Oral Biol, 50, 131-136.
[43] Hu, B., Nadiri, A., Kuchler-Bopp, S., Perrin-Schmitt, F., Peters, H., & Lesot, H., 2006, Tissue engineering of tooth crown, root, and periodontium. Tissue engineering, 12(8), 2069–2075.
[44] Sonoyama, W., Liu, Y., Fang, D., Yamaza, T., Seo, B. M., Zhang, C., Liu, H., Gronthos, S., Wang, C. Y., Wang, S., & Shi, S., 2006, Mesenchymal stem cell-mediated functional tooth regeneration in swine. PloS one, 1(1), e79.
[45] Nakao, K., Morita, R., Saji, Y., Ishida, K., Tomita, Y., Ogawa, M., Saitoh, M., Tomooka, Y., & Tsuji, T., 2007, The development of a bioengineered organ germ method. Nature methods, 4(3), 227–230.
[46] Herberts, C. A., Kwa, M. S., & Hermsen, H. P., 2011, Risk factors in the development of stem cell therapy. Journal of translational medicine, 9, 29.
[47] Saini, R., Saini, S., & Sharma, S., 2009, Stem cell therapy: the eventual future. International journal of trichology, 1(2), 145–146.
Viewed PDF 978 33 -
 Regenerative Therapy in Dentistry: A ReviewAuthor: Satish VishwanathaiahDOI: 10.21522/TIJAR.2014.10.02.Art008
Regenerative Therapy in Dentistry: A ReviewAuthor: Satish VishwanathaiahDOI: 10.21522/TIJAR.2014.10.02.Art008Regenerative Therapy in Dentistry: A Review
Abstract:
Despite millions of people suffering from dental caries and periodontitis to date, we don’t have effective treatments that guarantee complete restoration of the impacted tissues. The current procedures mostly help in delaying the disease progress, and hence, bringing alternative approaches for whole tooth replacement has become indispensable. Considering the scenario, regenerative medicine seems to be the novel approach, given its innovative therapeutic techniques that aid in the repair and replacement of damaged, aged, diseased, or congenitally defective tissues and organs. While we are yet to overcome various challenges, including effective ways to control the size, color, and shape of the tooth and come up with the perfect implantation sites for the jaw to enable in vitro tooth development, the ongoing research and their favorable results reveal that whole-tooth regeneration and bioengineered functional tooth are not a distant dream.
Keywords: Regeneration, Regenerative therapy, Scaffolds, Tissue engineering.Regenerative Therapy in Dentistry: A Review
References:
[1] Birjandi, A. A., Neves, V. C., & Sharpe, P., 2021, Advances in regenerative dentistry; building with biology. Regenerative medicine, 16(4), 343–345.
[2] Cooper L. F., 2009, The current and future treatment of edentulism. Journal of prosthodontics: official journal of the American College of Prosthodontists, 18(2), 116–122.
[3] Holm-Pedersen, P., Schultz-Larsen, K., Christiansen, N., & Avlund, K., 2008, Tooth loss and subsequent disability and mortality in old age. Journal of the American Geriatrics Society, 56(3), 429–435.
[4] Nakao, K., & Tsuji, T., 2008, Dental Regenerative Therapy: Stem Cell Transplantation & Bioengineered Tooth Replacement, Japanese dental science review, 44(1),70—75.
[5] Langer, R. S., & Vacanti, J. P., 1999, Tissue engineering: the challenges ahead. Scientific American, 280(4), 86–89.
[6] Atala A., 2005, Tissue engineering, stem cells and cloning: current concepts and changing trends. Expert opinion on biological therapy, 5(7), 879–892.
[7] Sharpe, P., 2020, Regenerative Dentistry, Front. Dent. Med, 1, 3.
[8] Are Stem Cells and Regenerative Medicine Living Up To Their Promises? Stem cells and regenerative medicine: Failed promises or real potential? (medicalnewstoday.com) accessed on 29.03.2023.
[9] Potdar, P. D., & Jethmalani, Y. D., 2015, Human dental pulp stem cells: Applications in future regenerative medicine. World Journal of Stem Cells, 7(5), 839–851.
[10] Aly L. A., 2015, Stem cells: Sources, and regenerative therapies in dental research and practice. World Journal of Stem Cells, 7(7), 1047–1053.
[11] Abou Neel, E. A., Chrzanowski, W., Salih, V. M., Kim, H. W., & Knowles, J. C., 2014, Tissue engineering in dentistry. Journal of Dentistry, 42(8), 915–928.
[12] Wang, L., Shen, H., Zheng, W., Tang, L., Yang, Z., Gao, Y., Yang, Q., Wang, C., Duan, Y., & Jin, Y., 2011, Characterization of stem cells from alveolar periodontal ligament. Tissue engineering. Part A, 17(7-8), 1015–1026.
[13] Soudi, A., Yazdanian, M., Ranjbar, R., Tebyanian, H., Yazdanian, A., Tahmasebi, E., Keshvad, A., & Seifalian, A., 2021, Role and application of stem cells in dental regeneration: A comprehensive overview. EXCLI Journal, 20, 454–489.
[14] Goldberg, M., Farges, J. C., Lacerda-Pinheiro, S., Six, N., Jegat, N., Decup, F., Septier, D., Carrouel, F., Durand, S., Chaussain-Miller, C., Denbesten, P., Veis, A., & Poliard, A., 2008, Inflammatory and immunological aspects of dental pulp repair. Pharmacological Research, 58(2), 137–147.
[15] Yen, A. H., & Yelick, P. C., 2011, Dental tissue regeneration - a mini-review. Gerontology, 57(1), 85–94.
[16] Wang, H. L., Greenwell, H., Fiorellini, J., Giannobile, W., Offenbacher, S., Salkin, L., Townsend, C., Sheridan, P., Genco, R. J., & Research, Science and Therapy Committee., 2005, Periodontal regeneration. Journal of Periodontology, 76(9), 1601–1622.
[17] Miura, M., Gronthos, S., Zhao, M., Lu, B., Fisher, L. W., Robey, P. G., & Shi, S., 2003, SHED: stem cells from human exfoliated deciduous teeth. Proceedings of the National Academy of Sciences of the United States of America, 100(10), 5807–5812.
[18] Thesleff I., 1976, Differentiation of odontogenic tissues in organ culture. Scandinavian Journal of Dental Research, 84(6), 353–356.
[19] Peterka, M., Mandys, V., & Peterková, R.,1991, A modification of tooth germ cultivation in vitro and in ovo. Cytotechnology, 7(1), 49–53.
[20] Isogawa, N., Terashima, T., Nakano, Y., Kindaichi, J., Takagi, Y., Takano, Y., 2004, The induction of enamel and dentin complexes by subcutaneous implantation of reconstructed human and murine tooth germ elements. Arch Histol Cytol, 67(1), 65–77.
[21] Hu, B., Nadiri, A., Kuchler-Bopp, S., Perrin-Schmitt, F., Peters, H., & Lesot, H., 2006, Tissue engineering of tooth crown, root, and periodontium. Tissue engineering, 12(8), 2069–2075.
[22] Kuo, T.F., Huang, A.T., Chang, H.H., Lin, F.H., Chen, S.T., Chen, R.S., Chou, C.H., Lin, H.C., Chiang, H., Chen, M.H., 2008, Regeneration of dentin-pulp complex with cementum and periodontal ligament formation using dental bud cells in gelatin-chondroitin-hyaluronan tricopolymer scaffold in swine. J Biomed Mater Res A, 86(4), 1062–1068.
[23] Zhang, L., Morsi, Y., Wang, Y., Li, Y., Ramakrishna, S., 2013, Review Scaffold Design & Stem Cells for Tooth Regeneration, Japanese dental science review, 49(1), 14-26.
[24] Demarco, F. F., Conde, M. C., Cavalcanti, B. N., Casagrande, L., Sakai, V. T., & Nör, J. E., 2011, Dental pulp tissue engineering. Brazilian dental journal, 22(1), 3–13.
[25] Cavalcanti, B. N., Zeitlin, B. D., & Nör, J. E., 2013, A hydrogel scaffold that maintains viability and supports differentiation of dental pulp stem cells. Dental materials: official publication of the Academy of Dental Materials, 29(1), 97–102.
[26] Chisini, L. A., Conde, M. C., Alcázar, J. C., Silva, A. F., Nör, J. E., Tarquinio, S. B., & Demarco, F. F., 2016, Immunohistochemical Expression of TGF-β1 and Osteonectin in engineered and Ca (OH)2-repaired human pulp tissues. Brazilian oral research, 30(1), e93.
[27] Demarco, F. F., Casagrande, L., Zhang, Z., Dong, Z., Tarquinio, S. B., Zeitlin, B. D., Shi, S., Smith, A. J., & Nör, J. E., 2010, Effects of morphogen and scaffold porogen on the differentiation of dental pulp stem cells. Journal of Endodontics, 36(11), 1805–1811.
[28] Demarco, G, T., Kirschnick, L, B., Watson, L.B., Conde, M, C, M., Demarch, F.F., Chisnini, L, A., 2017, What is the Clinical Applicability of Regenerative Therapies in Dentistry? Rev Gauch Odontol, 65(4), 359-367.
[29] Pradeep, A. R., Rao, N. S., Agarwal, E., Bajaj, P., Kumari, M., & Naik, S. B., 2012, Comparative evaluation of autologous platelet-rich fibrin and platelet-rich plasma in the treatment of 3-wall intrabony defects in chronic periodontitis: a randomized controlled clinical trial. Journal of Periodontology, 83(12), 1499–1507.
[30] Pradeep, A. R., Nagpal, K., Karvekar, S., Patnaik, K., Naik, S. B., & Guruprasad, C. N., 2015, Platelet-rich fibrin with 1% metformin for the treatment of intrabony defects in chronic periodontitis: a randomized controlled clinical trial. Journal of Periodontology, 86(6), 729–737.
[31] Kim, J. Y., Xin, X., Moioli, E. K., Chung, J., Lee, C. H., Chen, M., Fu, S. Y., Koch, P. D., & Mao, J. J., 2010, Regeneration of dental-pulp-like tissue by chemotaxis-induced cell homing. Tissue engineering. Part A, 16(10), 3023–3031.
[32] Kim, K., Lee, C. H., Kim, B. K., & Mao, J. J., 2010, Anatomically shaped tooth and periodontal regeneration by cell homing. Journal of dental research, 89(8), 842–847.
[33] Sonoyama, W., Liu, Y., Fang, D., Yamaza, T., Seo, B. M., Zhang, C., Liu, H., Gronthos, S., Wang, C. Y., Wang, S., & Shi, S., 2006, Mesenchymal stem cell-mediated functional tooth regeneration in swine. PloS one, 1(1), e79.
[34] Balic A., 2018, Biology Explaining Tooth Repair and Regeneration: A Mini-Review. Gerontology, 64(4), 382–388.
[35] Morsczeck, C., & Reichert, T. E. ,2018, Dental stem cells in tooth regeneration and repair in the future. Expert opinion on biological therapy, 18(2), 187–196.
Viewed PDF 925 22

