Table of Contents - Issue
Recent articles
-
 An Exploration of the Quality Assurance Roles of the Various Regulators of Human Resources for Health Training in ZambiaAuthor: Mabvuto Katwizi KangoDOI: 10.21522/TIJAR.2014.09.04.Art001
An Exploration of the Quality Assurance Roles of the Various Regulators of Human Resources for Health Training in ZambiaAuthor: Mabvuto Katwizi KangoDOI: 10.21522/TIJAR.2014.09.04.Art001An Exploration of the Quality Assurance Roles of the Various Regulators of Human Resources for Health Training in Zambia
Abstract:
This inquiry was conducted following reports that questioned the quality of higher education in Zambia, including the quality of Human Resources for Health (HRH) training. One of the notable reports was from research conducted by the Zambia Medical Association (2019). This inquiry built on all these reports by focusing on the roles of the various regulators (also referred to here as Actors) on how their individual and collective roles can play a role in improving the quality of HRH training in Zambia. Ideally, one does not expect to see any challenges in the quality of HRH training because when reading the acts and mandates of the various actors (summarized in Table 1), such as HPCZ, HEA, ZAQA, and local government authorities, there appears to enough authority to provide quality assurance. The inquiry focused on what could have gone wrong and what could have been improved.
Keywords: Actors, Human Resources for Health (HRH), Intersectoral collaboration, Quality, Regulators, Training.
An Exploration of the Quality Assurance Roles of the Various Regulators of Human Resources for Health Training in Zambia
References:
[1] Zambia Medical Association (2018). Report on the State of Medical Training Institutions in Zambia. Medical Education and Research Board (ZMA-MERB).
[2] Kalaluka, L. (2019). Attorney General Ponders CBU Conflict. Zambia Daily Mail. Available from: http://www.daily-mail.co.zm/attorney-general-ponders-cbu-conflict/ [Accessed: 22nd July 2019].
[3] Kanyika, J. (2019). PSZ Protests Mujajati Sacking. Zambia Daily Mail. Available from: https://www.dailynation.info/psz-protest-mujajati-sacking/ [Accessed: 22nd July 2019].
[4] Higher Education Authority (2019). Public Notice - Universities Operating Illegally in Zambia. Available from: https://www.hea.org.zm/index.php/downloads [Accessed:15th October 2019].
[5] Creswell, J. (2013). Qualitative inquiry and research design: Choosing among five approaches, 2nd ed. London: Sage.
[6] Yin, Robert K. (1981). The Case-Study Crisis: Some Answers. Administrative Science Quarterly, 26 (1), p.58-65.
[7] Yin (2002) cited in Yazan, B. (2015). Three Approaches to Case-Study Methods in Education: Yin, R., Merriam, S. and Stake, R. The Qualitative Report, 20 (2), p. 134-152. Available from: http://www.nova.edu/ssss/QR/QR20/2/yazan1.pdf [Accessed: 13th January 2016].
[8] Riessman, C.K. (1993) ‘Narrative analysis. Qualitative Research Methods’ Series No. 30. Newbury Park, CA: Sage.
[9] Stake (1995) cited in Yazan, B. (2015). Three Approaches to Case-Study Methods in Education: Yin, Merriam, and Stake. The Qualitative Report, 20 (2), p. 134-152. Available from: http://www.nova.edu/ssss/QR/QR20/2/yazan1.pdf [Accessed: 13th January 2016].
[10] Pyone, T., Smith, H., and van den Broek, N. (2017). Frameworks to assess health systems governance: a systematic review. Health Policy and Planning, 32, p. 710–722. Doi: 10.1093/heapol/czx007.
[11] Atkinson (1997). Cited in Riessman, C.K. (1993) ‘Narrative analysis. Qualitative Research Methods’ Series No. 30. Newbury Park, CA: Sage.
[12] Higher Education Authority (2019). Public Notice - Universities Operating Illegally in Zambia. Zambia Daily Mail, 20th September 2019, p.14.
[13] Simukanga, S. (2019). Five Varsities Closed. Daily Nation, September 2019, p.2.
[14] Okeyo, I., Lehmann, U. & Schneider, H. (2020). The impact of differing frames on early stages of intersectoral collaboration: the case of the First 1000 Days Initiative in the Western Cape Province. Health Res Policy Sys 18, 3. Available from: https://doi.org/10.1186/s12961-019-0508-0 (Accessed: 2 August 2022).
[15] Kang, E, Park, H. and Kim, J. (2011). Health Impact Assessment as a Strategy for Intersectoral Collaboration. Journal of Preventive Medicine and Public Health, 44 (5), p.201-209. Available from: http://dx.doi.org/10.3961/jpmph.2011.44.5.201 [Accessed: 20th July 2020].
[16] Lindeman, M. Taylor, K. Kuipers, P., Stothers, K. and Piper, K. (2012). We don’t have anyone with dementia here’: A case for better intersectoral collaboration for remote Indigenous clients with dementia. Australian Journal of Rural Health, 20, p.190–194. Doi: 10.1111/j.1440-1584.2012.01284. x.
[17] Findings in the Area of Community Psychology Reported from the University of Alabama at Birmingham (2019). The Perceived Importance of Intersectoral Collaboration by Health Care Alliances.” Psychology & Psychiatry Journal, 15, p. 178.
[18] Adeleye, O. and Ofili, A. (2010). Strengthening Intersectoral Collaboration for Primary Health Care in Developing Countries: Can the Health Sector Play Broader Roles? Journal of Environmental and Public Health. doi:10.1155/2010/272896.
[19] Anand. S. and Bärnighausen, T. (2007). Health workers and vaccination coverage in developing countries: an econometric analysis. The Lancet, 369, pp. 1277–1285.
[20] Materu, P. (2007). The State of Quality Assurance in Africa Higher Education Quality Assurance in Sub-Saharan Africa. World Bank Working Paper No. 124. World Bank Publications. Available from: https://doi.org/10.1596/978-0-8213-7272-2 [Accessed: 16th October 2019].
[21] Baumgardt, J. and Lekhetho, M. (2013). The Challenges of Quality Assurance in Private Higher Education Institutions in South Africa. Mediterranean Journal of Social Sciences, 4 (3). doi:10.5901/mjss. 2013.v4n3p421.
[22] World Health Organization (2016). Global strategy on human resources for health: Workforce 2030. WHO Library Cataloguing-in-Publication Data, ISBN 978 92 4 151113 1. Available from: 9789241511131-eng.pdf (Accessed: 31 May 2022).
[23] World Bank (2022). Understanding Poverty. Available from:Education Overview: Development news, research, data | World Bank (Accessed: 31 May 2022).
[24] UNESCO (2017). Links between Education, Poverty and Health. Available from:UNESCO Publications Assess Links between Education, Poverty and Health | News | SDG Knowledge Hub | IISD (Accessed: 31 May 2022).
[25] Speybroeck, N et al. (2006). Reassessing the relationship between human resources for health, intervention coverage, and health outcomes. Background paper prepared for the world health report. Evidence and Information for Policy World Health Organization, Geneva. Available from: https://www.who.int/hrh/documents/reassessing_relationship.pdf [Accessed:15th October 2019].
[26] World Health Organisation (2018). Low quality healthcare is increasing the burden of illness and health costs globally. Available from: Low quality healthcare is increasing the burden of illness and health costs globally (who.int) (Accessed: 31st May 2022).
Viewed PDF 826 25 -
 Effects of Gadolinium-Based Contrast Agents on the Kidney, Liver, and Heart of Wistar RatsAuthor: Oluwafemi Olumide EgbeyemiDOI: 10.21522/TIJAR.2014.09.04.Art002
Effects of Gadolinium-Based Contrast Agents on the Kidney, Liver, and Heart of Wistar RatsAuthor: Oluwafemi Olumide EgbeyemiDOI: 10.21522/TIJAR.2014.09.04.Art002Effects of Gadolinium-Based Contrast Agents on the Kidney, Liver, and Heart of Wistar Rats
Abstract:
The harmless potential of gadolinium-based contrast agent (GBCA) used in MRI studies was remarkable until when gadolinium was detected in the brain, bones, and skin. This study aimed to evaluate the effect of four GBCAs on the liver, heart, and kidney of Wistar rats. Twenty-five (25) male Wistar rats weighing 165-239 g were divided into 4 experimental and control groups after obtaining ethical approval from the Institutional Review Board (IRB) of the Nigerian Institute of Medical Research (NIMR). Specimens in the experimental groups received 2.5 mls / day of one GBCA and the control same normal saline through the lateral tail for 5 days consecutively / week. The Livers, Hearts and Kidneys were harvested 4 weeks following last injection. Pathohistology showed all kidney tissues exposed to Gadopentetate, 80 % to Gadodiamide, and 40 % to Dotarem and Cyclolux were inflamed. Sixty percent Gadodiamide and Doterem to the liver tissue, 50 % and 20 % to Gadopentetate and Cyclolux also inflamed. Samples exposed to Gadopentetate and Dotarem had 50 and 40 % of their heart tissue inflamed. Only those to Gadodiamide and Cyclolux were not affected. Injuries like necrosis, degeneration, and hypertrophy were also noted in all the tissues. All GBCAs were statistically significant in all tissue studied. Gadolinium-based contrast agents had a weak negative correlation with inflamed and degenerated tissues, also a weak positive correlation with hypertrophied tissue, but a moderate positive correlation with necrosis tissues of the kidney, liver, and heart.
Keywords: Contrast agents, Heart, Histopathology, Kidney, Liver, Magnetic resonance imaging.Effects of Gadolinium-Based Contrast Agents on the Kidney, Liver, and Heart of Wistar Rats
References:
[1] Nikken, J. J., Krestin, G. P., 2007, MRI of the kidney-state of the art. European Radiology, 17(11), 2780–2793. https://doi.org/10.1007/s00330-007-0701-3.
[2] Mannelli, L., Kim, S., Hajdu, C. H., Babb, J. S., Taouli, B., 2013, Serial diffusion-weighted MRI in patients with hepatocellular carcinoma: Prediction and assessment of response to transarterial chemoembolization. Preliminary experience. European Journal of Radiology, 82(4), 577–582. https://doi.org/10.1016/j.ejrad.2012.11.026.
[3] Guglielmo, F. F., Mitchell, D. G., Gupta, S., 2014, Gadolinium contrast agent selection and optimal use for body MR imaging. Radiologic Clinics of North America, 52(4), 637–656. https://doi.org/10.1016/j.rcl.2014.02.004.
[4] Wáng, Y. X., Schroeder, J., Siegmund, H., Idée, J. M., Fretellier, N., Jestin-Mayer, G., Factor, C., Deng, M., Kang, W., Morcos, S. K., 2015, Total gadolinium tissue deposition and skin structural findings following the administration of structurally different gadolinium chelates in healthy and ovariectomized female rats. Quantitative Imaging in Medicine and Surgery,5(4),534–545. https://doi.org/10.3978/j.issn.2223.4292.2015.05.03.
[5] Nazarian, S., Hansford, R., Rahsepar, A. A., Weltin, V., McVeigh, D., Gucuk Ipek, E., Kwan, A., Berger, R. D., Calkins, H., Lardo, A. C., Kraut, M. A., Kamel, I. R., Zimmerman, S. L., Halperin, H. R., 2017, Safety of Magnetic Resonance Imaging in Patients with Cardiac Devices. The New England Journal of Medicine, 377(26), 2555–2564. https://doi.org/10.1056/NEJMoa1604267.
[6] Das, C. J., Mahalingam, S., Debnath, J., Dhawan, S., 2010, MRI contrast media: what clinicians need to know. The National Medical Journal of India, 23(5), 292–296.
[7] Pullicino, R., Das, K., 2017, Is it Safe to use gadolinium –based contrast Agents in MRI. Journal of the Royal College of Physicians of Edinburgh, 47(3),243-245.
[8] Rogosnitzky, M., Branch, S., 2016, Gadolinium-based contrast agent toxicity: a review of known and proposed mechanisms. Biometals 29,365–376 https://doi.org/10.1007/s10534-016-9931-7.
[9] Nacif, M. S., Arai, A. E., Lima, J. A., Bluemke, D. A., 2012, Gadolinium-enhanced cardiovascular magnetic resonance: administered dose in relationship to United States Food and Drug Administration (FDA) guidelines. Journal of cardiovascular magnetic resonance: official journal of the Society for Cardiovascular Magnetic Resonance, 14(1), 18. https://doi.org/10.1186/1532-429X-14-18.
[10] Gale, E. M., Caravan, P., 2018, Gadolinium-Free Contrast Agents for Magnetic Resonance Imaging of the Central Nervous System. ACS Chemical Neuroscience, 9(3), 395–397. https://doi.org/10.1021/acschemneuro.8b00044.
[11] Schieda, N., Blaichman, J. I., Costa, A. F., Glikstein, R., Hurrell, C., James, M., Jabehdar Maralani, P., Shabana, W., Tang, A., Tsampalieros, A., van der Pol, C. B., Hiremath, S., 2018, Gadolinium-Based Contrast Agents in Kidney Disease: A Comprehensive Review and Clinical Practice Guideline Issued by the Canadian Association of Radiologists. Canadian Journal of Kidney Health and Disease, 5, 2054358118778573. https://doi.org/10.1177/2054358118778573.
[12] Bae, K. T., Tao, C., Zhu, F., Bost, J. E., Chapman, A. B., Grantham, J. J., Torres, V. E., Guay-Woodford, L. M., Meyers, C. M., Bennett, W. M., Consortium for Radiologic Imaging Studies Polycystic Kidney Disease., 2009, MRI-based kidney volume measurements in ADPKD: reliability and effect of gadolinium enhancement. Clinical Journal of the American Society of Nephrology,4(4),719–725. https://doi.org/10.2215/CJN.03750708.
[13] Kanda, T., Fukusato, T., Matsuda, M., Toyoda, K., Oba, H., Kotoku, J., Haruyama, T., Kitajima, K., Furui, S., 2015, Gadolinium-based Contrast Agent Accumulates in the Brain Even in Subjects without Severe Renal Dysfunction: Evaluation of Autopsy Brain Specimens with Inductively Coupled Plasma Mass Spectroscopy. Radiology, 276(1), 228–232. https://doi.org/10.1148/radiol.2015142690.
[14] Bussi, S., Maisano, F., Tedoldi, F., Kirchin, M.A., 2019, Gadolinium retention and clearance after administration of macrocyclic magnetic resonance contrast agents to rats. Pediatric Radiology.,49(8),1110-1111. DOI: 10.1007/s00247-019-04439-9.
[15] Hao, D., Ai, T., Goerner, F., Hu, X., Runge, V. M., Tweedle, M., 2012, MRI contrast agents: basic chemistry and safety. Journal of Magnetic Resonance Imaging: JMRI, 36(5), 1060–1071. https://doi.org/10.1002/jmri.23725.
[16] Maurer, M., Heine, O., Wolf, M., Durmus, T., Wagner, M., Hamm, B., 2012, Tolerability and diagnostic value of gadoteric acid in the general population and in patients with risk factors: results in more than 84,000 patients. European Journal of Radiology, 81, 885–890.
[17] Abujudeh, H. H., Kosaraju, V. K., Kaewlai, R., 2010, Acute adverse reactions to gadopentetate dimeglumine and gadobenate dimeglumine: experience with 32,659 injections. AJR. American Journal of Roentgenology,194(2),430–434. https://doi.org/10.2214/AJR.09.3099.
[18] Neeley, C., Moritz, M., Brown, J.J., Zhou, Y., 2016, Acute side effects of three commonly used gadolinium contrast agents in the Nehra, A. K., McDonald, R. J., Bluhm, A. M., Gunderson, T. M., Murray, D. L., Jannetto, P. J., Kallmes, D. F., Eckel, L. J., & McDonald, J. S. (2018). Accumulation of Gadolinium in Human Cerebrospinal Fluid after Gadobutrol-enhanced MR Imaging: A Prospective Observational Cohort Study. Radiology, 288(2), 416–423. https://doi.org/10.1148/radiol.2018171105.
[19] The Royal College of Radiologists. Clinical radiology UK workforce census 2019 report. London: The Royal College of Radiologists, 2020.
[20] Shirani, F., Teimoori, A., Rashno, M., Latifi, S. M., Karandish, M., 2017, Using rats as a research model to investigate the effect of human adenovirus 36 on weight gain. ARYA Atherosclerosis, 13(4), 167–171.
[21] Sengupta, P., 2012, A Scientific Review of Age Determination for a Laboratory Rat: How old is it in comparison with Human age? Biomedical International, 2,81–9.
[22] Sengupta, P., 2013, The Laboratory Rat: Relating Its Age with Humans. International Journal of Preventive Medicine, 4(6), 624–630.
[23] [23]. Davidson, M. K., Lindsey, J. R., Davis, J. K., 1987, Requirements and selection of an animal model. Israel Journal of Medical Sciences, 23(6),551–555.
[24] Lohrke, J., Frisk, A. L., Frenzel, T., Schöckel, L., Rosenbruch, M., Jost, G., Lenhard, D. C., Sieber, M. A., Nischwitz, V., Küppers, A., Pietsch, H.,2017, Histology and Gadolinium Distribution in the Rodent Brain After the Administration of Cumulative High Doses of Linear and Macrocyclic Gadolinium-Based Contrast Agents. Investigative Radiology, 52(6), 324–333. https://doi.org/10.1097/RLI.0000000000000344.
[25] Parasuraman, S., 2011, Toxicological screening. Journal of Pharmacology and Pharmacotherapy, 2(2),74-79. doi: 10.4103/0976-500X.81895.
[26] Nehra, A. K., McDonald, R. J., Bluhm, A. M., Gunderson, T. M., Murray, D. L., Jannetto, P. J., Kallmes, D. F., Eckel, L. J., McDonald, J. S., 2018, Accumulation of Gadolinium in Human Cerebrospinal Fluid after Gadobutrol-enhanced MR Imaging: A Prospective Observational Cohort Study.Radiology,288(2),416–423. https://doi.org/10.1148/radiol.2018171105.
[27] McDonald, R. J., McDonald, J. S., Kallmes, D. F., Jentoft, M. E., Paolini, M. A., Murray, D. L., Williamson, E. E., Eckel, L. J., 2017a, Gadolinium Deposition in Human Brain Tissues after Contrast-enhanced MR Imaging in Adult Patients without Intracranial Abnormalities. Radiology, 285(2), 546–554. https://doi.org/10.1148/radiol.2017161595.
[28] Khairinisa, M. A., Takatsuru, Y., Amano, I., Erdene, K., Nakajima, T., Kameo, S., Koyama, H., Tsushima, Y., Koibuchi, N., 2018, The Effect of Perinatal Gadolinium-Based Contrast Agents on Adult Mice Behavior. Investigative Radiology, 53(2), 110–118.
[29] Guo, B.J, Yang, Z.L., and Zhang, L.J., 2018, Gadolinium Deposition in Brain: Current Scientific Evidence and Future Perspectives. Frontier Molecular Neuroscience, 11:335. doi: 10.3389/fnmol.2018.00335.
[30] Aime, S., Caravan, P., 2009, Biodistribution of gadolinium-based contrast agents, including gadolinium deposition. Journal of Magnetic Resonance Imaging, 30(6),1259–1267. https://doi.org/10.1002/jmri.21969.
[31] Dekkers, I. A., Roos, R., van der Molen, A. J., 2018, Gadolinium retention after administration of contrast agents based on linear chelators and the recommendations of the European Medicines Agency. European Radiology,28(4),1579–1584. https://doi.org/10.1007/s00330-017-5065-8.
[32] Baerlocher, M. O., Asch, M., Myers, A., 2010, The use of contrast media. CMAJ: Canadian Medical Association Journal,182(7), 697. https://doi.org/10.1503/cmaj.090118.
[33] Andreucci, M., Solomon, R., Tasanarong, A., 2014, Side effects of radiographic contrast media: pathogenesis, risk factors, and prevention. BioMedical Research International, 2014, 741018. https://doi.org/10.1155/2014/741018.
[34] Nakajima, T., Lamid-Ochir, O., 2020, Current Clinical Issues: Deposition of Gadolinium Chelates. Rare Earth Elements and their Minerals. DOI: http://dx.doi.org/10.5772/intechopen.91260.
[35] Akgun, H., Gonlusen, G., Cartwright, J., Jr, Suki, W. N., Truong, L. D., 2006, Are gadolinium-based contrast media nephrotoxic? A renal biopsy study. Archives of Pathology & Laboratory Medicine, 130(9),1354–1357. https://doi.org/10.5858/2006-130-1354-AGCMNA.
[36] Thomsen, H.S., 2006, Nephrogenic systemic fibrosis: A serious late adverse reaction to gadodiamide. European Radiology,16(12),2619–2621. https://doi.org/10.1007/s00330-006-0495-8.
[37] Lin, S. P., & Brown, J. J. (2007). MR contrast agents: physical and pharmacologic basics. Journal of Magnetic Resonance Imaging: JMRI,25(5),884–899. https://doi.org/10.1002/jmri.20955.
[38] Elmholdt, T.R., Pedersen, M., Jorgensen, B., Sondergaar, K., Jensen, J.D., Ramsing, M., Olesen, A.B., 2011, Nephrogenic systemic fibrosis is found only among gadolinium-exposed patients with renal insufficiency: a case-control study from Denmark. British Journal of Dermatology, 165,828–836.
[39] Chen, R., Ling, D., Zhao, L., Wang, S., Liu, Y., Bai, R., Baik, S., Zhao, Y., Chen, C., Hyeon, T., 2015, Parallel Comparative Studies on Mouse Toxicity of Oxide Nanoparticle- and Gadolinium-Based T1 MRI Contrast Agents. ACS Nano, 9(12), 12425–12435. https://doi.org/10.1021/acsnano.5b05783.
[40] Murata, N., Gonzalez-Cuyar, L.F., Murata, K., Fligner, C., Dills, R., Hippe, D., Maravilla, K.R., 2016, Macrocyclic and other nongroup 1 gadolinium contrast agents deposit low levels of gadolinium in brain and bone tissue: preliminary results from 9 patients with normal renal function. Investigative Radiology. doi:10.1097/rli.0000000000000252.
[41] McDonald, R. J., McDonald, J. S., Dai, D., Schroeder, D., Jentoft, M. E., Murray, D. L., Kadirvel, R., Eckel, L. J., Kallmes, D. F., 2017b, Comparison of Gadolinium Concentrations within Multiple Rat Organs after Intravenous Administration of Linear versus Macrocyclic Gadolinium Chelates. Radiology, 285(2), 536–545. https://doi.org/10.1148/radiol.2017161594.
[42] Sanyal, S., Marckmann, P., Scherer, S., Abraham, J. L., 2011, Multiorgan gadolinium (Gd) deposition and fibrosis in a patient with nephrogenic systemic fibrosis--an autopsy-based review. Nephrology, dialysis, transplantation: official publication of the European Dialysis and Transplant
Association - European Renal Association, 26(11),3616–3626. https://doi.org/10.1093/ndt/gfr085.[43] Gibby, W.A., Gibby, K.A., Gibby, W.A., 2004, Comparison of Gd DTPA-BMA (Omniscan) versus Gd HP-DO3A (ProHance) retention in human bone tissue by inductively coupled plasma atomic emission 2 eespectroscopy. Investigative Radiology, 39,138–142.
[44] Morcos, S.K., 2009, Chelates and Stability. In: Thomsen HS., ebb JA, (eds). Contrast Media. Medical Radiology (Diagnostic Imaging) [Springer, Berlin, Heidelberg]. https://doi.org/10.1007/978-3-540-72784-2_20.
[45] Robert, P., Lehericy, S., Grand, S., Violas, X., Fretellier, N., Idée, J. M., Ballet, S., Corot, C., 2015, T1-Weighted Hypersignal in the Deep Cerebellar Nuclei After Repeated Administrations of Gadolinium-Based Contrast Agents in Healthy Rats: Difference Between Linear and Macrocyclic Agents. Investigative Radiology, 50(8),473–480. https://doi.org/10.1097/RLI.0000000000000181.
[46] Major, J.L., Meade, T.J., 2009, Bio responsive, cell-penetrating, and multimeric MR contrast agents. Acc Chemical Research, 42,893–903.
Viewed PDF 1127 34 -
 Predictive Factors of IT Systems Adoption by SME Employees in Developing Countries: Evidence from SME Employees in North Kivu, DRCAuthor: Rodrigue KalumendoDOI: 10.21522/TIJAR.2014.09.04.Art003
Predictive Factors of IT Systems Adoption by SME Employees in Developing Countries: Evidence from SME Employees in North Kivu, DRCAuthor: Rodrigue KalumendoDOI: 10.21522/TIJAR.2014.09.04.Art003Predictive Factors of IT Systems Adoption by SME Employees in Developing Countries: Evidence from SME Employees in North Kivu, DRC
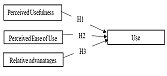
Abstract:
This research aimed to identify the determinants of technology usage among SME employees in the North Kivu Province of the Democratic Republic of Congo. We based our model on the Technology Acceptance Model. In addition to perceived usefulness and ease of use, the proposed model includes relative advantage as a predictor of technology usage. This study used the PLS-SEM method to test the proposed hypotheses from 247 responses. The results confirmed the hypotheses. The research findings demonstrate a positive relationship between perceived usefulness and use, perceived ease of use and use, and relative advantages and use of new technologies. Congolese SME managers can rely on these findings to highlight these key determinants in promoting technology usage among SMEs in a country where technology usage by businesses remains low.
Keywords: Perceived ease of use, Perceived usefulness, Relative advantages, SI adoption, Technology.Predictive Factors of IT Systems Adoption by SME Employees in Developing Countries: Evidence from SME Employees in North Kivu, DRC
References:
[1] Ettoumi, F. E., & Benjelloun, S. (2022). L’impact des systèmes d’information intégrés et décisionnels sur le contrôle de gestion : étude qualitative exploratoire. International Journal of Accounting, Finance, Auditing, Management and Economics, 3(4-3), 174-189. Récupéré sur https://doi.org/10.5281/zenodo.6915755.
[2] Kalumendo, R. (2022). The benefits of technological developments on businesses: a survey conducted among SMEs in Beni, democratic republic of Congo. Texila International Journal of Academic Research. doi :10.21522/TIJAR.2014.SE.22.01.Art012.
[3] Kalumendo, R. (2022). Barriers to SME computerization in developing countries : evidence from SMEs in North Kivu, Democratic Republic of Congo. Texila International Journal of Management, 8(2). doi :10.21522/TIJMG.2015.08.02.Art013.
[4] Panari, C., Lorenzi, G., & Mariani, M. G. (2021). The Predictive Factors of New Technology Adoption, Workers’ Well-Being, and Absenteeism: The Case of a Public Maritime Company in Venice. Int. J. Environ. Res. Public Health, 18(12358). accessed from https://doi.org/10.3390/ijerph182312358.
[5] Dwivedi, Y., Rana, N., Jeyaraj, A., Clement, M., & Williams, M. (2019). Re-examining the Unified Theory of Acceptance and Use of Technology (UTAUT) : Towards a Revised Theoretical Model. Inf. Syst. Front, 21, 719–734. doi :10.1007/s10796-017-9774-y.
[6] Al-Delawi, A. S., & Ramo, W. M. (2020). The impact of accounting information systems on performance management. Polish journal of management studies. doi :10.17512/pjms.2020.21.2.03.
[7] Ahmad, M., & Al-Shbiel, S. O. (2019). The Effect of Accounting Information System on Organizational Performance in Jordanian Industrial SMEs: The Mediating Role of Knowledge Management. International Journal of Business and Social Science, 10(3). doi :10.30845/ijbss.v10n3p9.
[8] Jewer, J., & Compeau, D. R. (2021). Understanding information systems success: à hybrid view. 10.1080/0960085X.2021.1890529.
[9] Thuan, P. Q., Khuong, N. V., Cam Anh, N. D., Hanh, N. T., Thi, V. H., Tram, T. N., & Han, C. G. (2022). The Determinants of the Usage of Accounting Information Systems toward Operational Efficiency in Industrial Revolution 4.0: Evidence from an Emerging Economy. Economies, 10(83). doi: https://doi.org/10.3390/economies10040083.
[10] Avgerou, C. (2008). Information systems in developing countries : a critical research review. Journal of Information Technology volume, 23, 133–146.
[11] Ghobakhlooa, M., & Tanga, S. (2015). Information system success among manufacturing SMEs: case of developing countries. Information Technology for Development. doi :10.1080/02681102.2014.996201.
[12] Walsam, G., & Sahay, S. (2005). Research on information systems in developing countries : Current landscape and future prospects. Information Technology for Development, accessed from https://doi.org/10.1002/itdj.20020.
[13] Lutfi, A. (2022). Factors Influencing the Continuance Intention to Use Accounting Information System in Jordanian SMEs from the Perspectives of UTAUT : Top Management Support and Self-Efficacy as Predictor Factors. Economies, 10(75), accessed from https://doi.org/10.3390/economies10040075.
[14] Taylor, P. (2019, 5 5). Information and Communication Technology (ICT) Adoption by Small and Medium Enterprises in Developing Countries : The Effects of Leader, Organizational and Market Environment Factors. International Journal of Economics, Commerce and Management United Kingdom, VII (5), accessed from https://ssrn.com/abstract=3388391.
[15] Zafar, A., & Mustafa, S. (2017). SMEs and Its Role in Economic and Socio-Economic Development of Pakistan. International Journal of Academic Research in Accounting, Finance and Management Sciences, VI (4).
[16] Lecerf, M., & Omrani, N. (2020). SME Internationalization: the Impact of Information Technology and Innovation. Journal of the Knowledge Economy, 11, 805–824. accessed from https://doi.org/10.1007/s13132-018-0576-3.
[17] Rao, J. J., & Kumar, V. (2019). Technology Adoption in the SME Sector for Promoting Agile Manufacturing Practices. Dans S. C. Satapathy, V. Bhateja, & S. Das, Smart Intelligent Computing and Applications. Smart Innovation, Systems and Technologies (Vol. 105). Singapore : Springer. accessed from https://doi.org/10.1007/978-981-13-1927-3_69.
[18] Rahmana, N. A., Yaacobb, Z., & Radzic, R. M. (2016). An Overview of Technological Innovation on SME Survival : A Conceptual Paper. Procedia-Social and Behavioral Sciences, 224, (pp. 508-515).
[19] DeLone, W. (1988). Determinants of Success for Computer Usage in Small Business. MIS Quarterly, 12(1), 51-61.
[20] Thong, J., & Yap, C.-S. (1997). Effects of resource constraints on information technology implementation in small businesses. Dans T. McMaster, E. Mumford, E. Swanson, B. Warboys, & D. Wastell, Facilitating Technology Transfer through Partnership (pp. 191-206). Springer, Boston, MA.
[21] Cirera, X., Lage, F., & Sabetti, L. (2016). ICT Use, Innovation, and Productivity. Evidence from Sub-Saharan Africa. Policy Research Working Paper ; No. 7868. World Bank, Washington, DC. © World Bank. doi: https://openknowledge.worldbank.org/handle/10986/25313.
[22] Davis, F. D. (1989). Perceived Usefulness, Perceived Ease of Use, and User Acceptance of Information Technology. MIS Quarterly, 13(3), 319-340.
[23] Marangunić, N., & Granić, A. (2015). Technology acceptance model : a literature review from 1986 to 2013. Univ Access Inf Soc, 81–95. Récupéré sur https://doi.org/10.1007/s10209-014-0348-1.
[24] Gupta, C., Gupta, V., & Stachowiak, A. (2021). Adoption of ICT-Based Teaching in Engineering : An Extended Technology Acceptance Model Perspective. IEEE Access, 58652-58666. doi :10.1109/ACCESS.2021.3072580.
[25] Chuttur, M. (2009). Overview of the Technology Acceptance Model : Origins, Developments and Future Directions. Sprouts: Working Papers on Information System, 9(37). accessed from http://sprouts.aisnet.org/9-37.
[26] Présidence de la République. (2019). Plan national du numérique horizon 2025. Pour une RDC connectée et performante. Kinshasa.
[27] Taherdoost, H. (2018). A review of technology acceptance and adoption models and theories. Procedia Manufacturing.
[28] Chen, S.-C., Li, S.-H., & Li, C.-Y. (2011). Recent Related Research in Technology Acceptance Model : A Literature Review. Australian Journal of Business and Management Research, 1(9), 124-127.
[29] Mortenson, M. J., & Vidgen, R. (2016). A computational literature review of the technology acceptance model. International Journal of Information Management, 36(6), 1248-1259.
[30] Osman, R. B., Choo, P. S., & Rahmat, M. K. (2013). Understanding Student Teachers’ Behavioural Intention to Use Technology: Technology Acceptance Model (TAM) Validation and Testing. International Journal of Instruction, 6(1).
[31] Alfadda, H. A., & Mahdi, H. S. (2021). Measuring Students’ Use of Zoom Application in Language Course Based on the Technology Acceptance Model (TAM). Journal of Psycholinguistic Research, 50, 883-900. doi: https://doi.org/10.1007/s10936-020-09752-1.
[32] Verma , S., Bhattacharyya, S. S., & Kumar, S. (2018). An extension of the technology acceptance model in the big data analytics system implementation environment. Information Processing & Management, 54(5), 791-806. accessed from https://doi.org/10.1016/j.ipm.2018.01.004.
[33] Fishbein, M., & Ajzen, I. (1975). Belief, Attitude, Intention, and Behavior : An Introduction to Theory and Research. Reading, MA : Addison-Wesley. Reading, MA : Addison-Wesley.
[34] Ajibade, P. (2018). Technology acceptance model limitations and criticisms: Exploring the practical applications and use in technology-related studies, mixed-method, and qualitative researches. Library Philosophy and Practice (e-journal). accessed from http://digitalcommons.unl.edu/libphilprac/1941.
[35] Lim, W. M. (2018). Dialectic Antidotes to Critics of the Technology Acceptance Model : Conceptual, Methodological, and Replication Treatments for Behavioural Modelling in Technology-Mediated Environments. Australasian Journal of Information Systems, 22. accessed from https://doi.org/10.3127/ajis.v22i0.1651.
[36] Lunceford, B. (2009). Reconsidering Technology Adoption and Resistance : Observations of a Semi-Luddite. Explorations in Media Ecology, 8, 29-48.
[37] Benbasat, I., & Barki, H. (2007). Quo Vadis TAM ? Journal of the Association for Information Systems, 8(4). doi :10.17705/1jais.00126.
[38] Karahanna, E., & Straub, D. W. (1999). The psychological origins of perceived usefulness and ease-of-use. Information & Management, 35, 237-250.
[39] Saeed, K. A., & Abdinnour-Helm, S. (2008). Examining the effects of information system characteristics and perceived usefulness on post adoption usage of information system. Information & Management, 45(6), 376-386. accessed from https://doi.org/10.1016/j.im.2008.06.002.
[40] Lu, H.-P., & Gustafson, D. H. (1994). An empirical study of perceived usefulness and perceived ease of use on computerized support system use over time. International Journal of Information Management, 14(5), 317-329. accessed from https://doi.org/10.1016/0268-4012(94)90070-1.
[41] Igbaria, M., Guimarae, T., & Davis, G. B. (1995). Testing the Determinants of Microcomputer Usage via a Structural Equation Model. Journal of Management Information Systems, 11(4), 87-114. Récupéré sur https://doi.org/10.1080/07421222.1995.11518061.
[42] Sulaiman, Y., & Jauhari, N. (2021). The Factors Influencing Mobile Banking Usage among University Staff. Wseas Transactions on Business and Economics, 18.
[43] Islami, M. M., Asdar, M., & Baumassepe, A. N. (2021). Analysis of Perceived Usefulness and Perceived Ease of Use to the Actual System Usage through Attitude Using Online Guidance Application : A Study on the Online Tutoring Application Ruangguru in Makassar. Hasanuddin Journal of Business Strategy, 3(1). accessed from https://doi.org/10.26487/hjbs.v3i1.410.
[44] Lanlan, Z., Ahmi, A., & Popoola, O. J. (2019). Perceived ease of use, perceived usefulness and the usage of computerized accounting systems: A performance of micro and small enterprises (mses) in china. International Journal of Recent Technology and Engineering, 8(2), 324-331.
[45] Chen, W.-C., Chen, C.-W., & Chen, W.-K. (2019). Drivers of Mobile Payment Acceptance in China : An Empirical Investigation. Information, 10(12). Récupéré sur https://doi.org/10.3390/info10120384.
[46] Rogers, E. M. (199). Rogers, E. M. (1995). The Diffusion of Innovations, New York : The Free Press.
[47] Agag, G., & El-Masry, A. A. (2016). Understanding consumer intention to participate in online travel community and effects on consumer intention to purchase travel online and WOM : An integration of innovation diffusion theory and TAM with trust. Computers in Human Behavior, 60, 97-111. accessed from https://doi.org/10.1016/j.chb.2016.02.038.
[48] Maduku, D. K., Mpinganjira, M., & Duh, H. (2016). Understanding mobile marketing adoption intention by South African SMEs: A multi-perspective framework. International Journal of Information Management, 36(5), 711–723. Récupéré sur https://doi.org/10.1016/j.ijinfomgt.2016.04.018.
[49] Junglas, I., Goel, L., Ives, B., & Harris, J. (2019). Innovation at work: The relative advantage of using consumer IT in the workplace. Information Systems Journal, 29(2). accessed from https://doi.org/10.1111/isj.12198.
[50] Hair, J. F., Risher, J. J., Sarstedt, M., & Ringle, C. M. (2019). When to use and how to report the results of PLS-SEM. European Business Review.
[51] Al-Maroof, R. A., & Al-Emran, M. (2018). Students Acceptance of Google Classroom : An Exploratory Study using PLS-SEM Approach.
International Journal of Emerging Technologies in Learning (iJET, 13(06), 112–123. doi: https://doi.org/10.3991/ijet.v13i06.8275.[52] Hair, J. F., Hult, G. T., Ringle, C. M., & Sarstedt , M. (2016). A Primer on Partial Least Squares Structural Equation Modeling (PLS-SEM). SAGE Publications.
[53] Al-Nuaimi, M. N., & Al-Emran, M. (2021). Learning management systems and technology acceptance models : A systematic review. Education and Information Technologies, 26, 5499–5533. Récupéré sur https://doi.org/10.1007/s10639-021-10513-3.
[54] Brown, I. J. (2017). Individual and Technological Factors Affecting Perceived Ease of Use of Web-based Learning Technologies in a Developing Country. The Electronic Journal of Information Systems in Developing Countries, 9(1). accessed from https://doi.org/10.1002/j.1681-4835.2002.tb00055.x.
[55] Muñoz-Leiva, F., Climent-Climent, S., & Liébana-Cabanillas, F. (2017). Determinants of intention to use the mobile banking apps: An extension of the classic TAM model. Spanish Journal of Marketing - ESIC, 21(1), 25-38. Récupéré sur https://doi.org/10.1016/j.sjme.2016.12.001.
[56] Rajak, M., & Shaw, K. (2017). An extension of technology acceptance model for Health user adoption. Technology in Society, 67. Récupéré sur https://doi.org/10.1016/j.techsoc.2021.101800.
[57] Alsharida,, R. A., & Hammood, M. M. (2021). Mobile Learning Adoption: A Systematic Review of the Technology Acceptance Model from 2017 to 2020. International Journal of Emerging Technology in Learning. accessed from https://doi.org/10.3991/ijet.v16i05.18093.
Viewed PDF 1081 30 -
 The Impact of Covid 19 on School Administrators’ Leadership Attributes in Selected Schools in JamaicaAuthor: Karla Boswell-LewisDOI: 10.21522/TIJAR.2014.09.04.Art004
The Impact of Covid 19 on School Administrators’ Leadership Attributes in Selected Schools in JamaicaAuthor: Karla Boswell-LewisDOI: 10.21522/TIJAR.2014.09.04.Art004The Impact of Covid 19 on School Administrators’ Leadership Attributes in Selected Schools in Jamaica
Abstract:
Principals have been called upon to utilize their personal leadership resources in Jamaican schools during the novel Corona Virus pandemic. This crisis has forced a radical shift in the landscape of school leadership and management not only in Jamaica but globally. The purpose of this descriptive quantitative study was to ascertain the impact of Covid-19 on principals’ level of compassion and care, openness and communication, adaptiveness, resilience and courage, consultation and collaboration, empowerment, and decisiveness. Additionally, it sought to assess whether there were differences in these leadership attributes based on school level, region, and gender. A 24-item questionnaire developed and validated by Balasubramanian and Fernandes (2022) and achieved an overall Cronbach Alpha of .84 was used to collect data. The sample included 50 principals and vice principals selected conveniently from the 7 regions 18 completed and returned the questionnaire, 15 females and 3 males. The data were coded and imported into the SPSS, version 27, and were screened, cleaned, and analyzed using weighted means and standard deviations and MANOVA. The mean ranges for interpretation include: 1.00 – 2.33 = Low Attribute; 2.34 – 3.67 = Moderate Attribute and 3.68 – 5.00 = High Attribute. The results showed that the principal participants scored high on leadership attributes. These findings hold critical and practical lessons for handling future crises. They show that effective leaders in many schools can function effectively in a crisis given that the policy makers provide adequate guidance and regulations with a relevant resources.
Keywords: Adaptiveness, Compassion and care, Consultation and collaboration, Empowerment and Decisiveness, Openness and Communication, Resilience, and Courage.The Impact of Covid 19 on School Administrators’ Leadership Attributes in Selected Schools in Jamaica
References:
[1] OECD. (2020). A framework to guide an education response to the Covid-19 Pandemic of 2020. Date of Access: 10/09/2022. https://read.oecd-ilibrary.org/view/?ref=126_126988-t63lxosohs&title=A-framework-to-guide-an-education-response-to-the-Covid-19-Pandemic-of-2020.
[2] Alqabbani, S., Almuwais, A.,and Almoayad, F (2020). Readiness towards emergency shifting to remote learning during Covid-19 pandemic among university instructors. E Learning and Digital Media. Online First 18 (5): 1-20.
[3] Anderson, S. (2020). No time to say goodbye How Coronavirus is changing learning. https://patch.com/wisconsin/mountpleasant/no-time-say-goodbye-how-coronavirus-changing-learning?utm_source=facebook.com&utm_medium=social&utm_term=kids+%26+family+&utm_campaign=autopost&utm_content=mountpleasant-sturtevant&fbclid=IwAR1dCunSNxj06KETOvh7hVtjxaxQaCfw5sF5X3IZJ05mM14GHqe9-6cPPQM.
[4] Mladenova, T., Kalmukov, Y., and Valova, I. (2020). Covid 19 – A major cause of digital transformation in education or just an evaluation test. TEM Journal, 9(3), 1163–1170.
[5] Ainsworth, P. (2010). Developing a self-evaluating school: A practical guide. (NY: Continuum International Publishing Group).
[6] Barrow K., Boyle H., Ginsburg M., Leu E., Pier D., Price-Rom A. & Rocha V. (2006) Cross-National Synthesis on Education Quality Report No 2: Professional Development and Teachers’ Conceptions of Educational Quality. US Agency for International Development, Washington DC.
[7] Murphy, M. J., Levant, R. F., Hall, J. E., & Glueckauf, R. L. (2007). Distance education in Professional training in psychology. Professional Psychology: Research and Practice, 38(1), 97-103.
[8] Crossfield, D. (2018) Improving the Academic Performance of Boys in Jamaica: An Intervention Model. In C. Beckford the contemporary Caribbean: Issues, Challenges, and opportunities. Central America and the Caribbean, ISBN 978-1-53614-088-0.
[9] Crossfield, D. & Bourne, P. A. (2018). An Inquiry into Teachers Perception of at-Risk Students in Jamaica: A Phenomenological Approach. International Journal of Emergency Mental Health and Human Resilience, Vol.20, No. 2, pp 1-10© 2018 OMICS International ISSN 1522-4821. Retrieved May 2020 from: https://www.researchgate.net/publication/326249045.
[10] Slater, G. B. (2015). Education as Recovery: Neoliberalism, School Reform, and the Politics of Crisis. Journal of Education Policy 30 (1): 1–20.
[11] Arnold, B., Rahimi, M. & Riley, P. (2021). “Working through the First Year of the Pandemic: A Snapshot of Australian School Leaders’ Work Roles and Responsibilities and Health and Wellbeing during Covid-19.” Journal of Educational Administration and History 53 (3–4):301–309. doi: https://doi.org/10.1080/00220620.2021.1975367.
[12] Thomson, P., Greany, T. & Martindale, N. (2021). “The Trust Deficit in England: Emerging Research Evidence about School Leaders and the Pandemic.” Journal of Educational Administration and History 53 (3–4): 296–300. doi: https://doi.org/10.1080/00220620.2021.1975366.
[13] Reid, D. B. (2022). “Suppressing and Sharing: How School Principals Manage Stress and Anxiety during Covid-19.” School Leadership & Management 42 (1): 62–78. doi: https://doi.org/10.1080/13632434.2021.1974827.
[14] Haslam, S. A., Steffens, N. K., Reicher, S. D., & Bentley, S. V. (2021). Identity leadership in a crisis: A 5R framework for learning from responses to Covid-19. Social Issues and Policy Review, 15(1), 35–83. https://doi.org/10.1111/sipr.12075.
[15] Kaul, V., Shah, V. H., & El-Serag, H. (2020). Leadership during crisis: Lessons and Applications from the Covid-19 pandemic. Gastroenterology, 159(3), 809–812. https://doi.org/10.1053/j.gastro.2020.04.076.
[16] Dirani, K. M., Abadi, M., Alizadeh, A., Barhate, B.,Garza, R. C., Gunasekara, N., Ibrahim, G., & Majzun, Z. (2020). Leadership competencies and the essential role of human resource development in times of crisis: A response to Covid-19 pandemic. Human Resource Development International, 23(4), 380–394. https://doi.org/10.1080/13678868.2020.1780078.
[17] Deloitte (2020a). The heart of resilient leadership: Responding to Covid-19: A guide for senior executives. https://www2.deloitte.com/us/en/insights/economy/covid-19/heart-of-resilient-leadership-responding-to-covid-19.html.
[18] Forster, B. B., Patlas, M. N., & Lexa, F. J. (2020). Crisis Leadership During and Following Covid-19. Canadian Association of Radiologists’ Journal, 71(4), 421–422. https://doi.org/10.1177/0846537120926752.
[19] Stoller, J. K. (2020). Reflections on leadership in the time of Covid-19. BMJ Leader, 4(1), 1–3. https://doi.org/10.1136/leader-2020-000244.
[20] Ramalingam, B., Nabarro, D., Oqubay, A., Carnall, D. A., & Wild, L. (2020). 5 principles to guide adaptive leadership. Harvard Business Review. https://hbr.org/2020/09/5-principles-to-guide-adaptive-leadership.
[21] Folkman, J. (2017). New Research: 7 Ways to Become a More Resilient Leader, Date of Access: 12/09/2022. https://www.forbes.com/sites/joefolkman/2017/04/06/new-research-7-ways-to-become-a-more-resilient-leader/?sh=50292c157a0c.
[22] UN Global Compact (2020). Covid-19: What makes a good leader during a crisis. https://unglobalcompact.org/take-action/20th-anniversary-campaign/covid-19-what-makes-a-good-leader-during-a-crisis.
[23] Sadiq, A. A., Kapucu, N., & Hu, Q. (2021). Crisis leadership during Covid-19: The role of governors in the United States. International Journal of Public Leadership, 17 (1), 65–80. https://doi.org/10.1108/IJPL-08-2020-0071.
[24] Lagowska, U., Sobral, F., & Furtado, L. M. G. P. (2020). Leadership under crises: A research agenda for the post-Covid-19 Era. BAR − Brazilian Administration Review, 17(2), 1–5.
[25] Coleman, H. J. (1996). Why employee empowerment is not just a fad. Leadership and Organization Development Journal, 17(4), 29–36. https://doi.org/10.1108/01437739610120574.
[26] Quinn, R. E., & Spreitzer, G. M. (1997). The road to empowerment: Seven questions every leader should consider. Organizational Dynamics, 26(2), 37–49. https://doi.org/10.1016/S0090-2616(97)90004-8.
[27] Bradbury, A., Braun, A., Sam Duncan, S., Harmey, S., Levy, R. & Moss, G. (2022). Crisis policy enactment: primary school leaders’ responses to the Covid-19 pandemic in England. Retrieved September 2022 from: https://www.tandfonline.com/doi/full/10.1080/02680939.2022.2097316.
[28] Harvard Kennedy School (2022). A Female Leadership Trust Advantage in Times of Crisis: Under What Conditions? Retrieved September 2022 from: https://gap.hks.harvard.edu/female-leadership-trust-advantage-times-crisis-under-what-conditions.
[29] Oakes, K. (2022). The invisible danger of the ‘glass cliff’. Retrieved September 2022 from: https://www.bbc.com/future/article/20220204-the-danger-of-the-glass-cliff-for-women-and-people-of-colour.
[30] Cresswell, J. (2013). Steps in conducting a scholarly mixed methods study. Presentation, University of Nebraska, London. https://digitalcommons.unl.edu/cgi/viewcontent.cgi?article=1047&context=dberspeakers.
[31] Bradt, J., Burns, D., and Creswell, J. (2013) Mixed methods research in music therapy research. Journal of Music Therapy, 50(2), 123-148.
[32] Babbie, E. R. (2010). The Practice of Social Research Quantitative Research in Education with SPSS. SAGE Publications, 12, 1-4.
[33] Fotheringham, P., Harriott, T., Healy, G., Arenge, G. & Wilson, E. (2021), Pressures and influences on school leaders navigating policy development during the Covid-19 pandemic. British Educational Research Journal. https://doi-org.am.e-nformation.ro/10.1002/berj.3760.
Viewed PDF 1300 35 -
 Covid-19 Vaccine Hesitancy in Northern NigeriaAuthor: Adeniyi, D.S.DOI: 10.21522/TIJAR.2014.09.04.Art005
Covid-19 Vaccine Hesitancy in Northern NigeriaAuthor: Adeniyi, D.S.DOI: 10.21522/TIJAR.2014.09.04.Art005Covid-19 Vaccine Hesitancy in Northern Nigeria
Abstract:
The rapid development of the Covid-19 vaccine candidates through new and improved technologies and the rapidity with which these vaccine candidates were trialed and approved for public administration was highly commendable. However, the rapid administration of the Covid-19 vaccines raises a lot of concern among various world populations. This concern, relating directly to the safety and intents of the big pharmaceutical companies and governments, has led to the greatest form of health promotion initiative resistance in recorded human history. The universal level of hesitancy against the Covid-19 vaccines is now a subject of major concern among public health experts. This study which seeks to identify factors fostering Covid-19 vaccine hesitancy was conducted among the COVID-19 vaccine hesitant populations in Northern Nigeria. Findings from this study indicate that 84% of the study population makes use of the internet and other social media platforms for their news information sources. 42% of the study population would follow the guidance of their healthcare workers on issues relating to the Covid-19 vaccines. Covid-19 vaccine hesitancy in Northern Nigeria is largely fostered by a lack of appropriate information and a huge knowledge gap about the Covid-19 vaccines. It is, therefore, imperative that Government engages the young people of Northern Nigeria as critical stakeholders in the fight against Covid-19 vaccine hesitancy. Proper and tailored health educational programs, and meaningful engagements of religious leaders, parents, and healthcare workers in health promotion activities can help overcome the current challenge of Covid-19 vaccine hesitancy in Northern Nigeria.
Keywords: Covid-19, Healthcare Workers, Immunization, Vaccine, Northern Nigeria, Vaccine Hesitancy.Covid-19 Vaccine Hesitancy in Northern Nigeria
References:
[1] Timmis, K., & Brüssow, H. (2020). The Covid‐19 pandemic: some lessons learned about crisis preparedness and management, and the need for international benchmarking to reduce deficits. Environmental Microbiology.
[2] Song, P., & Karako, T. (2020). Scientific solidarity in the face of the Covid-19 pandemic: researchers, publishers, and medical associations. Global Health & Medicine.
[3] Kumar, A., & Nayar, K. R. (2021). Covid 19 and its mental health consequences. Journal of Mental Health, 30(1), 1-2.
[4] Mahase, E. (2020). Covid-19: What do we know about “long covid”? bmj, 370.
[5] Rosenblum, H. G., Hadler, S. C., Moulia, D., Shimabukuro, T. T., Su, J. R., Tepper, N. K., & Oliver, S. E. (2021). Use of Covid-19 vaccines after reports of adverse events among adult recipients of Janssen (Johnson & Johnson) and mRNA Covid-19 vaccines (Pfizer-BioNTech and Moderna): update from the Advisory Committee on Immunization Practices—United States, July 2021. Morbidity and Mortality Weekly Report, 70(32), 1094.
[6] Asundi, A., O’Leary, C., & Bhadelia, N. (2021). Global Covid-19 vaccine inequity: The scope, the impact, and the challenges. Cell host & microbe, 29(7), 1036-1039.
[7] Adeniyi, D.S. (2022). Vaccine Hesitancy: A 21st Century Challenge of Global Health Importance. International Journal of Advanced Academic Research, 8(8), 102-109.
[8] Ogundele, O. A., Ogundele, T., & Beloved, O. (2020). Vaccine hesitancy in Nigeria: contributing factors–way forward. The Nigerian journal of general practice, 18(1), 1.
[9] Olawade, D. B., Wada, O. Z., Odetayo, A., Akeju, O. O., Asaolu, F. T., & Owojori, G. O. (2022). Covid-19 vaccine hesitancy among Nigerian youths: Case study of students in Southwestern Nigeria. Journal of Education and Health Promotion, 11(1), 244.
[10] Iliyasu, Z., Umar, A. A., Abdullahi, H. M., Kwaku, A. A., Amole, T. G., Tsiga-Ahmed, F. I., ... & Aliyu, M. H. (2021). “They have produced a vaccine, but we doubt if Covid-19 exists”: correlates of Covid-19 vaccine acceptability among adults in Kano, Nigeria. Human Vaccines & Immunotherapeutics, 17(11), 4057-4064.
[11] Dror, A. A., Eisenbach, N., Taiber, S., Morozov, N. G., Mizrachi, M., Zigron, A., ... & Sela, E. (2020). Vaccine hesitancy: the next challenge in the fight against Covid-19. European journal of epidemiology, 35(8), 775-779.
[12] Ghatak, N., Marzo, R. R., Saleem, S. M., Sharma, N., Bhattacharya, S., & Singh, A. (2020). Impact on routine immunization services during the lockdown period in India: Implications and future recommendations. European Journal of Molecular and Clinical Medicine, 35-40.
[13] Marzo, R. R., Shrestha, R., Sapkota, B., Acharya, S., Shrestha, N., Pokharel, M., ... & Su, T. T. Covid-19 Vaccine Hesitancy in Rural and Urban Communities: A global survey. Frontiers in Public Health, 3103.
[14] Brackstone, K., Marzo, R. R., Bahari, R., Head, M. G., Patalinghug, M. E., & Su, T. T. (2022). Covid-19 Vaccine Hesitancy and Confidence in the Philippines and Malaysia: A Cross-sectional Study of Sociodemographic Factors and Information-Seeking. medRxiv.
[15] Aiyewumi, O., & Okeke, M. I. (2020). The myth that Nigerians are immune to SARS-CoV-2 and that Covid-19 is a hoax are putting lives at risk. Journal of global health, 10(2).
[16] Uwalaka, T., Nwala, B., & Chinedu, A. C. (2021). Social media, fake news, and fake Covid-19 cures in Nigeria. Journal of African Media Studies, 13(3), 435-449.
[17] Ezeibe, C. C., Ilo, C., Ezeibe, E. N., Oguonu, C. N., Nwankwo, N. A., Ajaero, C. K., & Osadebe, N. (2020). Political distrust and the spread of Covid-19 in Nigeria. Global Public Health, 15(12), 1753-1766.
[18] Nche, G. C. (2022). Is it yet uhuru? How religious institutions disconnect with the governments in the fight against Covid-19 in Nigeria. Journal of Contemporary African Studies, 40(2), 286-303.
[19] Kabakama, S., Konje, E. T., Dinga, J. N., Kishamawe, C., Morhason-Bello, I., Hayombe, P., ... & Dzinamarira, T. (2022). Commentary on Covid-19 Vaccine Hesitancy in sub-Saharan Africa. Tropical Medicine and Infectious Disease, 7(7), 130.
[20] Neel, A. H., Closser, S., Villanueva, C., Majumdar, P., Gupta, S. D., Krugman, D., & Alonge, O. (2021). 30 years of polio campaigns in Ethiopia, India, and Nigeria: the impacts of campaign design on vaccine hesitancy and health worker motivation. BMJ Global Health, 6(8), e006002.
[21] Sato, R. (2022). Covid-19 Vaccine Hesitancy and Trust in Government in Nigeria. Vaccines, 10(7), 1008.
[22] Marzo, R. R., Su, T. T., Ismail, R., Htay, M. N. N., Essar, M. Y., Chauhan, S., ... & Lin, Y. (2022). Digital health literacy for Covid-19 vaccination and intention to be immunized: A cross-sectional multi-country study among the general adult population. Frontiers in Public Health, 10.
[23] Marzo, R. R., Ahmad, A., Abid, K., Khatiwada, A. P., Ahmed, A., Kyaw, T. M., ... & Shrestha, S. (2022). Factors influencing the acceptability of COVID-19 vaccination: a cross-sectional study from Malaysia. Vacunas (English Edition), 23, 33-40.
[24] Marzo, R. R., Ahmad, A., Islam, M. S., Essar, M. Y., Heidler, P., King, I., ... & Yi, S. (2022). Perceived Covid-19 vaccine effectiveness, acceptance, and drivers of vaccination decision-making among the general adult population: A global survey of 20 countries. PLoS neglected tropical diseases, 16(1), e0010103.
[25] Marzo, R. R., Sami, W., Alam, M., Acharya, S., Jermsittiparsert, K., Songwathana, K., & Yi, S. (2022). Hesitancy in Covid-19 vaccine uptake and its associated factors among the general adult population: a cross-sectional study in six Southeast Asian countries. Tropical Medicine and Health, 50(1), 1-10.
[26] Elsayed, M., El-Abasiri, R. A., Dardeer, K. T., Kamal, M. A., Htay, M. N. N., Abler, B., & Marzo, R. R. (2021). Factors influencing decision making regarding accepting the Covid-19 vaccination in Egypt: A cross-sectional study in an urban, well-educated sample. Vaccines, 10(1), 20.
[27] Osubor, K. M., Fatusi, A. O., & Chiwuzie, J. C. (2006). Maternal health-seeking behavior and associated factors in a rural Nigerian community. Maternal and child health journal, 10(2), 159-169.
[28] Hussin, H. B., Marzo, R. R., Mamat, N. B., Safee, N. F. B., Omar, N. B., & Yin, T. S. (2020). The barriers of child immunization completion among parents in the community health centre, Johor Bahru. Article | IMSEAR | ID: sea-215923.
[29] Kaufman, J., Tuckerman, J., Bonner, C., Durrheim, D. N., Costa, D., Trevena, L., ... & Danchin, M. (2021). Parent-level barriers to uptake of childhood vaccination: a global overview of systematic reviews. BMJ global health, 6(9), e006860.
[30] Bangura, J. B., Xiao, S., Qiu, D., Ouyang, F., & Chen, L. (2020). Barriers to childhood immunization in sub-Saharan Africa: a systematic review. BMC Public Health, 20(1), 1-15.
[31] Peters, M. D. (2022). Addressing vaccine hesitancy and resistance for Covid-19 vaccines. International Journal of Nursing Studies, 104241.
[32] Afolabi, A. A., & Ilesanmi, O. S. (2021). Dealing with vaccine hesitancy in Africa: the prospective Covid-19 vaccine context. The Pan African Medical Journal, 38.
[33] Burgess, R. A., Osborne, R. H., Yongabi, K. A., Greenhalgh, T., Gurdasani, D., Kang, G., ... & McKee, M. (2021). The Covid-19 vaccines rush: participatory community engagement matters more than ever. The Lancet, 397(10268), 8-10.
[34] Olu-Abiodun, O., Abiodun, O., & Okafor, N. (2022). COVID-19 vaccination in Nigeria: A rapid review of vaccine acceptance rate and the associated factors. PloS one, 17(5), e0267691.
[35] Ekwebene, O. C., Obidile, V. C., Azubuike, P. C., Nnamani, C. P., Dankano, N. E., & Egbuniwe, M. C. (2021). Covid-19 Vaccine Knowledge and Acceptability among Healthcare Providers in Nigeria. immunity, 8, 9.
[36] Amuzie, C. I., Odini, F., Kalu, K. U., Izuka, M., Nwamoh, U., Emma-Ukaegbu, U., & Onyike, G. (2021). Covid-19 vaccine hesitancy among healthcare workers and its socio-demographic determinants in Abia State, Southeastern Nigeria: a cross-sectional study. The Pan African Medical Journal, 40.
Viewed PDF 1114 31 -
 Access to Finance: The Determinants and Limitations to the Supply Side of Finance for Liberia’s Rural MarketAuthor: Andy Saye GbatuDOI: 10.21522/TIJAR.2014.09.04.Art006
Access to Finance: The Determinants and Limitations to the Supply Side of Finance for Liberia’s Rural MarketAuthor: Andy Saye GbatuDOI: 10.21522/TIJAR.2014.09.04.Art006Access to Finance: The Determinants and Limitations to the Supply Side of Finance for Liberia’s Rural Market
Abstract:
This critical piece of research paper reviews the literature on the key determinants of finance for Liberia’s rural market. It also takes into account the limitations of the supply of finance for the rural market of Liberia, with the unabated need for the diversification of the Liberian economy in the face of intermittent shocks in the global economy. The study unearthed that investment in agricultural small and medium-sized enterprises (SMEs) will prove adequate in triggering sustainable economic growth and development through poverty alleviation, job creation, and food security which are the drivers of the supply of finance for rural dwellers in Liberia. Notwithstanding, the study found that the supply of finance for Liberian agricultural SMEs is constrained by the lack of creditworthiness information, weak judicial enforcement of contracts and corporate transparency, land ownership, high non-performing loans, and financial literacy. The keywords used in this article include gross domestic product, small and medium-sized enterprises, non-performing loans, inflation, credit rating, bankruptcy, value chain, urbanization, food security, human capital, and risk aversion.
Keywords: Bankruptcy, Credit rating, Human capital, Inflation, Small and medium-sized enterprises, Value chain.Access to Finance: The Determinants and Limitations to the Supply Side of Finance for Liberia’s Rural Market
References:
[1] IMF Country Report No.16/239, July 2016 https://www.imf.org/external/pubs/ft/scr/2016/cr16239.pdf.
[2] The World Bank Group. The Global Findex Database 2020. Washington, DC: World Bank https://www.worldbank.org/en/publication/globalfindex.
[3] Central Bank of Liberia 2021 Annual Report https://www.cbl.org.lr/.
[4] World Bank Annual Report 2021. From Crisis to Green, Resilient, and Inclusive Recovery. Washington, DC: World Bank http://www.worldbank.org/annualreport.
[5] Liberia Revenue Authority, Annual Report, FY2019/2020, Pg.46 https://revenue.lra.gov.lr/.
[6] UNDP Report, December 2021: Financing Agricultural SMEs in Liberia, Livelihoods and Employment Creation Project, https://www.uncdf.org/article/7381/financing-agricultural-msmes-in-liberia---livelihoods-and-employment-creation-project.
[7] Chattopadhyay, S. K. (2011). Financial inclusion in India: A case study of West Bengal. MPRA Paper, University Library of Munich, Germany.
[8] Paramasivan, C., & Ganeshkumar, V. (2013). Overview of financial inclusion in India. International Journal of Management and Development Studies, 2(3), 45–49.
[9] Chakravarty, S. R., & Pal, R. (2013). Financial inclusion in India: An axiomatic approach. Journal of Policy Modeling, 35(5), 813–837.
[10] Garg, S., & Agarwal, P. (2014). Financial inclusion in India: A review of initiatives and achievements. IOSR Journal of Business and Management, 16(6), 52–61.
[11] Anand, S., & Chhikara, K. S. (2013). A theoretical and quantitative analysis of financial inclusion and economic growth. Management and Labour Studies, 38(1), 103–133.
[12] Lal, T. (2017). Exploring the Role of Cooperatives in Enhancing the Social Empowerment of Rural Households through Financial Inclusion. The Indian Journal of Commerce, 70(2), 76–84.
[13] Kabakova, O., & Plaksenkov, E. (2018). Analysis of factors affecting financial inclusion: Ecosystem view. Journal of Business Research, 89, 198–205.
[14] Shankar, S. (2013). Financial inclusion in India: Do microfinance institutions address access barriers. ACRN Journal of Entrepreneurship Perspectives, 2(1), 60–74.
[15] Sarma, M., & Pais, J. (2011). Financial inclusion and development. Journal of International Development, 23(5), 613–628.
[16] Dixit, R., & Ghosh, M. (2013). Financial inclusion for inclusive growth of India: A study of Indian states. International Journal of Business Management & Research, 3(1), 147–156.
[17] Anand, S., & Chhikara, K. S. (2013). A theoretical and quantitative analysis of financial inclusion and economic growth. Management and Labour Studies, 38(1), 103–133.
[18] Shafi, M., & Medabesh, A. H. (2012). Financial inclusion in developing countries: Evidence from an Indian State. International Business Research, 5(8), 116.
[19] Kelkar, V. (2010). Financial inclusion for inclusive growth. ASCI Journal of Management, 39(1), 55–68.
[20] Kabakova, O., & Plaksenkov, E. (2018). Analysis of factors affecting financial inclusion: Ecosystem view. Journal of Business Research, 89, 198–205.
[21] Bongomin, G. O. C., Mpeera Ntayi, J., Munene, J. C., & Malinga Akol, C. (2017). Financial intermediation and financial inclusion of poor households: Mediating role of social networks in rural Uganda. Cogent Economics & Finance, 5(1), 1–16.
[22] Sharma, A., & Kukreja, S. (2013). An analytical study: Relevance of financial inclusion for developing nations. International Journal of Engineering and Science, 2(6), 15–20.
[23] Ramakrishna, S., & Trivedi, P. (2018). What determines the success of financial inclusion? An empirical analysis of demand-side factors. Review of Economics & Finance, 14, 98–112.
[24] Rastogi, S., & Ragabiruntha, E. (2018). Financial inclusion and socioeconomic development: Gaps and solution. International Journal of Social Economics, 45(7), 1122–1140.
[25] Fischer, G. (2011). Access to finance: A functional approach to supply and demand. LSE Research Online Documents on Economics 38369, London School of Economics and Political Science, LSE Library.
[26] Rai, K., Dua, S., & Yadav, M. (2019). Association of financial attitude, financial behaviour and financial knowledge towards financial literacy: A structural equation modeling approach. FIIB Business Review, 8(1), 51–60.
[27] Shankar, S. (2013). Financial inclusion in India: Do microfinance institutions address access barriers. ACRN Journal of Entrepreneurship Perspectives, 2(1), 60–74.
[28] Corsi, A. & J. Findeis (2000). “True State Dependence and Heterogeneity in Off-Farm Labour
[29] Participation”, European Review of Agricultural Economics, vol. 27, no. 2, pp. 127-151.
[30] Van Herck, K. (2009). Deliverable 7.4: A Comparative Analysis of Rural Labour Markets.
[31] [Online]. SCARLED Project. Available from: http://www.scarled.eu/uploads/media/SCARLED_D7.4.pdf.
[32] Ellis, F. (1993). Peasant Economics: Farm Households and Agrarian Development, Cambridge University Press, Cambridge.
[33] Huffman, W.E. (1980). “Farm and Off-Farm Work Decisions: The Role of Human Capital”,
[34] The Review of Economics and Statistics, vol. 62, no. 1, pp. 14-23.
[35] Sumner, D.A. (1982). “The Off-Farm Labor Supply of Farmers”. American Journal of Agricultural Economics, vol. 64, no. 3, pp. 499-509.
[36] Kimhi, A. (1994). “Participation of Farm Owners in Farm and Off-Farm Work Including the Option of Full-Time Off-Farm Work”. Journal of Agricultural Economics, vol. 45, no.2, pp. 232-239.
[37] Goodwin, B.K. & M.T. Holt (2002). “Parametric and Semiparametric Modeling of the Off- Farm Labor Supply of Agrarian Households in Transition Bulgaria”. American Journal of Agricultural Economics, vol. 84, no. 1, pp. 184-209.
[38] Juvančič, L. & E. Erjavec (2005). “Intertemporal Analysis of Employment Decisions on Agricultural Holdings in Slovenia”. Agricultural Economics, vol. 33, no. 2, pp. 153-161.10 | Tocco, Davidova & Bailey.
[39] Benjamin, C. & A. Kimhi (2006). “Farm Work, Off-Farm Work, and Hired Farm Labour: Estimating a Discrete-Choice Model of French Farm Couples’ Labour Decisions”. European Review of Agricultural Economics, vol. 33, no. 2, pp. 149-171.
[40] Ahearn, M.C., H. El-Osta & J. Dewbre (2006).”The Impact of Coupled and Decoupled Government Subsidies on Off-Farm Labor Participation of U.S. Farm Operators”. American Journal of Agricultural Economics, vol. 88, no. 2, pp. 393-408.
[41] Lopez, R.E. (1984). “Estimating Labor Supply and Production Decisions of Self-Employed Farm Producers”. European Economic Review, vol. 24, no. 1, pp. 61-82.
[42] Fall, M. & T. Magnac (2004). “How Valuable Is On-Farm Work to Farmers?”. American Journal of Agricultural Economics, vol. 86, no. 1, pp. 267-281.
[43] Rizov, M. & J.F.M. Swinnen (2004). “Human capital, market imperfections, and labor reallocation in transition”. Journal of Comparative Economics, vol. 32, no. 4, pp. 745-774.
[44] Macours, K. & J.F.M. Swinnen (2005). “Agricultural Labor Adjustments in Transition Countries: The Role of Migration and Impact on Poverty”. Review of Agricultural Economics, vol. 27, no. 3, pp. 405-411.
[45] Dries, L. & J.F.M. Swinnen (2002). “Institutional Reform and Labor Reallocation During Transition: Theory Evidence From Polish Agriculture”. World Development, vol. 30, no. 3, pp. 457-474.
[46] European Commission (2006). Employment in Rural Areas: Closing the Jobs Gap, Brussels. [Online] Available from: http://ec.europa.eu/agriculture/publi/reports/ruralemployment/sec1772_en.pdf.
[47] Kancs, d., J.F.M. Swinnen & L. Vranken (2009). Rural Labour Markets in Transition. [Online]. In Deliverable 2.1: Conceptual Framework for Analysing Structural Change in Agriculture and Rural Livelihoods, SCARLED Project. Available from: http://www.scarled.eu/uploads/media/SCARLED_D2.1_01.pdf.
[48] Davis, J. & D. Pearce (2001). The Non-agricultural Rural Sector in Central and Eastern Europe. Natural Resources Institute, Chatham, U.K.
[49] Kevane, M. (1996), “Agrarian Structure and Agricultural Practice: Typology and Application to Western Sudan”, American Journal of Agricultural Economics, vol. 78, no. 1, pp. 236-245.
[50] ILO (2008). Report IV: Promotion of Rural Employment for Poverty Reduction. International Labour Conference, 97th Session, 2008. ILO, Geneva.
[51] Swinnen, J.F.M., L. Dries & E. Mathijs (2001). “Critical Constraints to Rural Development in Central and Eastern Europe”. The Challenge of Rural Development in the EU Accession Countries, eds. C. Csaki & Z. Lerman, Proceedings of the Third World Bank/FAO Workshop, Sofia, Bulgaria, June 17-20, 2000, The World Bank, Washington, D.C.
[52] The World Bank Group. Economy Profile Liberia. Doing Business 2020. Washington, DC: World Bank https://www.doingbusiness.org/content/dam/doingBusiness/country/l/liberia/LBR.pdf.
Viewed PDF 2405 46 -
 Assessment of Knowledge about Hygiene during Covid-19 Pandemic in Catchment Area of Kaziba Health CentreAuthor: Bontango Kweme FredericDOI: 10.21522/TIJAR.2014.09.04.Art007
Assessment of Knowledge about Hygiene during Covid-19 Pandemic in Catchment Area of Kaziba Health CentreAuthor: Bontango Kweme FredericDOI: 10.21522/TIJAR.2014.09.04.Art007Assessment of Knowledge about Hygiene during Covid-19 Pandemic in Catchment Area of Kaziba Health Centre
Abstract:
Introduction: Hygiene is an essential element of public health that could reduce transmission of several diseases and their consequences. In Sub-Saharan Africa, water and sanitation-related diseases are highly prevalent, causing illness, disease and even death. The main objective of this study is to assess knowledge about hygiene in context of Covid-19 in catchment area of Kaziba health centre from January to October 2021. Materials and Method: our study was descriptive and prospective cross-sectional. A random sampling was carried out to collect data through survey questionnaire with 384 participants. Data was captured in Excel spreadsheet and imported into SPSS for analysis. Results: 93.2% of households had heard about hygiene. 43.8% of households did not know correct definition of hygiene. 98.4% of households had a toilet within the courtyard which ¾ were traditional. 53.1% of toilets had cleaning material. 72.1% of households washed their hands using soap (50.5%). 68.5% of households did not know the WHO’s handwashing technique. 57.3% of households had running water. 61.2% of water well or fountain were protected. 37% of households disposed their wastewater in the public places. More than ¾ of heads of households knew waterborne diseases. Negligence of environmental sanitation was 79.2%. 66.4% of households suffered from poor hygiene-related diseases such as Covid-19 (6.5%). Conclusion: poor of knowledge about hygiene in the population of this catchment area due to the existence of certain diseases related to poor hygiene observed in our results. There is need to increase awareness channels on hygienic practices and environmental sanitation.
Keywords: Covid-19, Household, Hygiene, health, Kaziba.Assessment of Knowledge about Hygiene during Covid-19 Pandemic in Catchment Area of Kaziba Health Centre
References:
[1] Billions of people will lack access to safe water, sanitation, and hygiene in 2030 unless progress quadruples – warn WHO, UNICEF, 2021, July 1). Retrieved September 19, 2021, from https://www.who.int/news/item/01-07-2021-billions-of-people-will-lack-access-to-safe-water-sanitation-and-hygiene-in-2030-unless-progress-quadruples-warn-who-unicef.
[2] Sustainable Development Goals | United Nations Development Programme. (n.d.). UNDP. Retrieved September 10, 2021, from https://www.undp.org/sustainable-development-goals?utm_source=EN&utm_medium=GSR&utm_content=US_UNDP_PaidSearch_Brand_English&utm_campaign=CENTRAL&c_src=CENTRAL&c_src2=GSR&gclid=CjwKCAjwpqCZBhAbEiwAa7pXeX9ghf9479PB6FFcF5XNHWgteAm262e_dnAZ9ILwyk7adS2DWG6XRhoCqSwQAvD_BwE#clean-water-and-sanitation.
[3] Billions of people will lack access to safe water, sanitation and hygiene in 2030 unless progress quadruples – warn WHO, UNICEF. (n.d.). Retrieved September 11, 2021, from https://www.unicef.org/romania/press-releases/billions-people-will-lack-access-safe-water-sanitation-and-hygiene-2030-unless.
[4] Rodriguez, L. 2019, 4 Factors Driving the Water & Sanitation Crisis in Africa. Global Citizen. Retrieved September 13, 2021, from https://www.globalcitizen.org/en/content/water-and-sanitation-crisis-sub-saharan-africa/?template=next.
[5] A Water, Sanitation, And Hygiene Revolution in Africa Using Smart Technologies | AUDA-NEPAD. (n.d.). Retrieved September 14, 2021, from https://www.nepad.org/blog/water-sanitation-and-hygiene-revolution-africa-using-smart-technologies.
[6] Chan, J. F. W., Lau, S. K. P., To, K. K. W., Cheng, V. C. C., Woo, P. C. Y., & Yuen, K. Y., 2015, Middle East Respiratory Syndrome Coronavirus: Another Zoonotic Betacoronavirus Causing SARS-Like Disease. Clinical Microbiology Reviews, 28(2), 465–522. https://doi.org/10.1128/cmr.00102-14.
[7] WHO. (2020, February 24). Report of the WHO-China Joint Mission on Coronavirus Disease 2019. Retrieved October 13, 2021, from https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf.
[8] Organisation Mondiale de la Santé. (2020, April 24). Recommandations aux États Membres pour améliorer les pratiques d’hygiène des mains par un accès universel à des postes publics d’hygiène des mains afin d’aider à prévenir la transmission du virus de la Covid-19 : orientations provisoires, 1er avril 2020. Retrieved September 10, 2021, from https://apps.who.int/iris/handle/10665/331854.
[9] Gould, D. J., Moralejo, D., Drey, N., Chudleigh, J. H., & Taljaard, M., 2017, Interventions to improve hand hygiene compliance in patient care. Cochrane Database of Systematic Reviews, 2017(9). https://doi.org/10.1002/14651858.cd005186.pub4.
[10] Coste, C. A. D., 2018, L’Hygiène des Mains Revue Documentaire [Thèse]. Universite Paul-Sabatier de Toulouse.
[11] Handwashing with soap, critical in the fight against coronavirus, is ‘out of reach’ for billions – UNICEF. (n.d.). Retrieved September 9, 2021, from https://www.unicef.org/eap/press-releases/handwashing-soap-critical-fight-against-coronavirus-out-reach-billions-unicef.
[12] Kangombe, T. K., 2020, Approvisionnement en eau potable en milieu rural en République Démocratique du Congo face à l’Objectif 6 de Développement Durable, Exemple de la province du Maniema [Thèse]. Selinus University of Science and Literature.
[13] People using at least basic sanitation services (% of population) - Sub-Saharan Africa | Data. (n.d.). Retrieved September 1, 2021, from https://data.worldbank.org/indicator/SH.STA.BASS.ZS?locations=ZG.
[14] Fredj, A., 2020, Étude de l’utilisation des produits hydro-alcooliques concernant l’hygiène des mains : enquête menée en ligne [Master Degree]. Universite Mohamad Boudiaf de M’sila.
[15] Emergency Response to the Ebola and Cholera Outbreak in North Kivu Province - COD182 - Democratic Republic of the Congo. (2018, December 11). Relief Web. Retrieved September 21, 2021, from https://reliefweb.int/report/democratic-republic-congo/drc-emergency-response-ebola-and-cholera-outbreak-north-kivu.
[16] Longembe, E. B., & Kitronza, P. L., 2020, Observance de l’hygiène des mains dans les hôpitaux généraux de référence de la ville de Kisangani en République Démocratique du Congo. Pan African Medical Journal, 35. https://doi.org/10.11604/pamj.2020.35.57.18500.
[17] Lewis, D., 2021, Covid-19 rarely spreads through surfaces. So why are we still deep cleaning? Nature, 590(7844), 26–28. https://doi.org/10.1038/d41586-021-00251-4.
[18] Yamontché, S. K. H., Johnson, R. C., Gouissi, F. M., Boni, G., Degbey, C., & Houssou, C. S., 2020, Etat Des Lieux et Facteurs Associés en Matière D’eau, D’hygiène Et D’assainissement Dans la Commune d’Abomey-Calavi Au Bénin. European Scientific Journal, ESJ, 16(6), 524. https://doi.org/10.19044/esj.2020.v16n6p524.
[19] Développer l’hygiène et l’assainissement en milieu rural au Burkina Faso. (2018, September 23). Burkina Doc! Retrieved September 21, 2021, from http://www.burkinadoc.milecole.org/eco-developpement/article-developper-lhygiene-lassainissement-en-milieu-rural-au-burkina-faso/.
[20] Phélinas, P., Ciriez, C., & Ciriez, C., 2022, Comportement des ménages brésiliens face à la Covid-19. Revue D’économie Du Développement, Vol. 29(1), 217–260. https://doi.org/10.3917/edd.351.0217.
[21] Azage, M., Motbainor, A., & Gedamu, G., 2021, Access to improved water and household water treatment practice in rural communities of Amhara Region, Ethiopia. PAMJ - One Health, 6. https://doi.org/10.11604/pamj-oh.2021.6.4.28481.
[22] Diallo, A. I., Diongue, M., Leye, M. M. M., Bassoum, O., Diongue, F. B., Ndiaye, M., Sarr, F. M., Ndiaye, I., Diegane Tina, J. A., Sougou, N. M., Niang, K., Faye, A., & Seke, I., 2021, Study of the Factors Associated with the Treatment of Drinking Water in Semi-Urban Areas in Senegal. Journal of Public Health, Hygiene and Safety 3(1), 103.
[23] Beck L., 2015, Enquête ménage : comportements en matière d’hygiène et d’assainissement et volonté de payer en milieu rural au Sénégal. Retrieved July 23, 2021, from https://www.wsp.org.
[24] Simiyu, S. N., Kweyu, R. M., Antwi-Agyei, P., & Adjei, K. A., 2020, Barriers and opportunities for cleanliness of shared sanitation facilities in low-income settlements in Kenya. BMC Public Health, 20(1). https://doi.org/10.1186/s12889-020-09768-1.
[25] McGuinness, S. L., O’Toole, J., Barker, S. F., Forbes, A. B., Boving, T. B., Giriyan, A., Patil, K., D’Souza, F., Vhaval, R., Cheng, A. C., & Leder, K., 2020, Household Water Storage Management, Hygiene Practices, and Associated Drinking Water Quality in Rural India. Environmental Science &Amp; Technology, 54(8), 4963–4973. https://doi.org/10.1021/acs.est.9b04818.
[26] WASHplus, 2016, Etude de base sur l’Eau, l’Hygiene, l’Assainissement et les Maladies Tropicales Négligées y Associées. Districts de Manni et de Bogande dans la Province de la Gnagna-Burkina Faso. Washington DC, USA. USAID/WASHplus Project.
[27] John, J., Van Aart, C. J. C., & Grassly, N. C., 2016, The Burden of Typhoid and Paratyphoid in India: Systematic Review and Meta-analysis. PLOS Neglected Tropical Diseases, 10(4), e0004616. https://doi.org/10.1371/journal.pntd.0004616.
[28] Lifewater International., 2020, Community Hygiene: Definition, Facts, and Impact in Rural Villages. Retrieved September 16, 2022, from https://lifewater.org/blog/hygiene-community/.
[29] Paul, P., 2020, Socio-demographic and environmental factors associated with diarrheal disease among children under five in India. BMC Public Health, 20(1). https://doi.org/10.1186/s12889-020-09981-y.
[30] Vijayan, B., & Ramanathan, M., 2020, Prevalence and clustering of diarrhoea within households in India: some evidence from NFHS-4, 2015–16. Journal of Biosocial Science, 53(1), 108–120. https://doi.org/10.1017/s0021932020000073.
Viewed PDF 1017 15 -
 Making the Law Work for Human Resources for Health (HRH) Training in ZambiaAuthor: Mabvuto Katwizi KangoDOI: 10.21522/TIJAR.2014.09.04.Art008
Making the Law Work for Human Resources for Health (HRH) Training in ZambiaAuthor: Mabvuto Katwizi KangoDOI: 10.21522/TIJAR.2014.09.04.Art008Making the Law Work for Human Resources for Health (HRH) Training in Zambia
Abstract:
There are several institutions in Zambia that play an important role in regulating the quality of higher education, including Human Resources for Health (HRH) training. However, there were reports of overlaps in the legal mandates of these institutions. In 2021, one of the institutions, the Higher Education Authority (HEA), responded to this challenge by successfully facilitating the amendment of the laws that regulated the quality of higher education. This research investigated whether the amended laws were still suitable enough to ensure quality in higher education and in HRH training.
Keywords: Actors, HRH, Law, Regulators, Training, Quality.Making the Law Work for Human Resources for Health (HRH) Training in Zambia
References:
[1] Kalaluka, L. (2019). Attorney General Ponders CBU Conflict. Zambia Daily Mail. Available from: http://www.daily-mail.co.zm/attorney-general-ponders-cbu-conflict/ [Accessed: 22nd July 2019].
[2] Zambia Medical Association (2019). Report on the State of Medical Training Institutions in Zambia. Medical Education and Research Board (ZMA-MERB).
[3] Yin, Robert K. (1981). The Case-Study Crisis: Some Answers. Administrative Science Quarterly, 26 (1), p.58-65.
[4] Creswell, J. (2013). Qualitative inquiry and research design: Choosing among five approaches, 2nd ed. London: Sage.
[5] Yin (2002) cited in Yazan, B. (2015). Three Approaches to Case-Study Methods in Education: Yin, R., Merriam, S. and Stake, R. The Qualitative Report, 20 (2), p. 134-152. Available from: http://www.nova.edu/ssss/QR/QR20/2/yazan1.pdf[Accessed: 13th January 2016].
[6] Riessman, C.K. (1993) ‘Narrative analysis. Qualitative Research Methods’ Series No. 30. Newbury Park, CA: Sage.
[7] Stake (1995) cited in Yazan, B. (2015). Three Approaches to Case-Study Methods in Education: Yin, Merriam, and Stake. The Qualitative Report, 20 (2), p. 134-152. Available from: http://www.nova.edu/ssss/QR/QR20/2/yazan1.pdf [Accessed: 13th January 2016].
[8] Pyone,T., Smith, H. and van den Broek, N. (2017). Frameworks to assess health systems governance: a systematic review. Health Policy and Planning, 32, p. 710–722. doi: 10.1093/heapol/czx007.
[9] Atkinson (1997). Cited in Riessman, C.K. (1993) ‘Narrative analysis. Qualitative Research Methods’ Series No. 30. Newbury Park, CA: Sage.
[10] National Assembly (2013). The Higher Education 2013. Act Number: Act 4 of 2013. Available from: https://www.parliament.gov.zm/node/3097 (Accessed: 9 June 2022).
[11] HEA (2021). The Higher Education (Amendment) Bill, 2021. Available from: https://hea.org.zm/the-higher-education-amendment-bill-2021/ (Accessed: 9th June 2022).
[12] Higher Education Authority (2021). Higher Education (Amendment) Act No. 23 of 2021. Available from: Higher Education Act and Statutory Instruments – Higher Education Authority (Accessed: 3rd June 2022).
[13] HEA (2019). HEA Reinstates Registration of Africa Research University and Rockview University. Available from: https://www.hea.org.zm/index.php/component/k2/item/104-hea-reinstates-registration-of-africa-research-university-and-rockview-university [Accessed: 23rd July 2019].
[14] Higher Education Authourity (2021). Illegally Operating Universities in Zambia. Available from: https://hea.org.zm/illegally-operating-universities-in-zambia/ (Accessed: 7 June 2022).
[15] Zambia National Broadcasting Corporation (2021). Four Universities Operating Illegally. Available from: https://www.znbc.co.zm/news/4-universities-operating-illegally/#:~:text=Four%20Universities%20in%20Lusaka%20and,as%20Shalome%20University%20in%20Kitwe (Accessed: 7 June 2022).
[16] Daily Advent Nigeria (2021). Zambian Authority Releases 12 Names of Illegal Universities (Full List) – Daily Advent Nigeria. Available From: http://ng.dailyadvent.com/education/2019/09/21/zambian-authority-releases-12-names-of-illegal-universities-full-list/ (Accessed: 7 June 2022).
[17] Zambia Legal Information Institute (ZambiaLii, 2022). Judgements. Available from: https://zambialii.org (Accessed: 7 June 2022).
[18] Zambia Corporate Insolvency Act (2017) Act No. 9 of 2017. Available from: link https://osall.org.za/docs/2019/07/Zambia-Corporate-Insolvency-Act-9-of-2017.pdf (Accessed: 7 June 2022).
[19] Sheikh, K., Saligram, P. and Hort, K. (2015). What explains regulatory failure? Analysing the architecture of health care regulation in two Indian states. Health Policy and Planning, 30, pp. 30:39–55. doi:10.1093/heapol/czt095.
[20] Indeed, Editorial Team (2021). What Is a Subject Matter Expert? Indeed. Available from: https://www.indeed.com/career-advice/career-development/what-is-a-subject-matter-expert (Accessed: 21 July 2022).
[21] Aarohan Healthcare Services (2020). Importance of Subject Matter Experts in Healthcare Marketing Campaigns. Available from: https://aarohanhealthcare.com/blog/importance-of-subject-matter-experts-in-healthcare-marketing-campaigns/ (Accessed: 31 July 2022).
Viewed PDF 1292 16 -
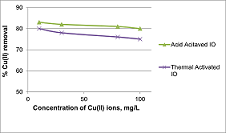 Adsorptive Removal of Copper (II) Ions from Aqueous Solution using Acid and Thermally Activated Iron Oxide SandAuthor: Adwell LibboholeDOI: 10.21522/TIJAR.2014.09.04.Art009
Adsorptive Removal of Copper (II) Ions from Aqueous Solution using Acid and Thermally Activated Iron Oxide SandAuthor: Adwell LibboholeDOI: 10.21522/TIJAR.2014.09.04.Art009Adsorptive Removal of Copper (II) Ions from Aqueous Solution using Acid and Thermally Activated Iron Oxide Sand
Abstract:
Heavy metal pollution of water bodies is a common problem in Zambia, whose economy depends on copper mining. Removal of Cu2+ ions from the solution via adsorption using iron oxide ore was investigated. The composition of the adsorbent was determined by XRF and ICP-OES. Iron oxide had predominantly Fe2O3 at 60 % with less than 3% of SiO2 and Al2O3. The Cu2+ ion concentrations were measured before and after adsorption using Atomic Absorption Spectroscopy (AAS). The effects of initial concentration, pH, acid activation, and thermal activation of the adsorbent on adsorption were investigated. A decrease in the adsorption of Cu2+ ions with an increase in the initial concentration of adsorbate (Cu2+) was observed. The adsorption of Cu2+ ions on acid-activated Iron oxide compared to thermally activated iron oxide ranged from 83-73%, respectively. Adsorption of Cu2+ ions was pH dependent with an optimum pH of 7. Acid activation of the adsorbent had better absorptivity since acids cause mineral dissolution, which increases the surface area and porosity of the adsorbent. Iron Oxide adsorbents have the potential to the removal of Cu2+ ions from aqueous solutions.Keywords: Adsorption, Copper ions, Heavy metals, Iron oxide, Pollution.Adsorptive Removal of Copper (II) Ions from Aqueous Solution using Acid and Thermally Activated Iron Oxide Sand
References:
[1] Aljamali, Nagham & Jawad, Aseel & Alabbasy, Anaam & Salih, Layla & Aljamali, Dr.Nagham & J, Aseel & M, Jawad & A, Nagham & Mahmood, Aljamali. (2019). A Literature Review on Types of Contamination (Biological, Chemical, Medical). International Journal of Green Chemistry, Vol. 5, pp. 7-14.
[2] Tchounwou PB, Yedjou CG, Patlolla AK, Sutton DJ. 2012, Heavy Metals Toxicity and the Environment. Experientia supplementum (EXS, Vol. 101, pp. 133-164.
[3] Ma. del Rosario Moreno Virgen, Omar Francisco González Vázquez, Virginia Hernández Montoya, and Rigoberto Tovar Gómez., 2018, ‘Removal of Heavy Metals Using Adsorption Processes Subject to an External Magnetic Field’, in H. E. M. Saleh, R. F. Aglan (eds.), Heavy Metals, IntechOpen, London. 10.5772/intechopen.74050.
[4] Akbal, F. and Camci, 2011, Copper, chromium, and nickel removal from metal plating wastewater by Desalination. Desalination, Vol. 269, pp. 214-2221.
[5] Mohsen-Nia, M., Montazeri, P. and Modarress, H, 2007, Removal of Cu2+ and Ni2+ from wastewater with a chelating agent and reverse osmosis processes. Desalination, Vol. 217, pp. 276-281.
[6] Rahmanian, Bashir & Pakizeh, Majid & Esfandyari, Morteza & Heshmatnezhad, Fazlollah & Maskooki, Abdolmajid. (2011). Fuzzy modeling and simulation for lead removal using micellar-enhanced ultrafiltration (MEUF). Journal of hazardous materials. 192. 585-92. 10.1016/j.jhazmat.2011.05.051.
[7] Lertlapwasin, Ratthaya & Bhawawet, Nakara & Imyim, Apichat & Fuangswasdi, Saowarux. (2010). Ionic liquid extraction of heavy metal ion by 2-aminothiophenol in 1-butyl-3-methylimidazolium hexafluorophosphate and their association constants. Separation and Purification Technology. 72. 70–76. 10.1016/j.seppur.2010.01.004.
[8] Wang, X and Li, Y, 2011, Measurement of Cu and Zn adsorption onto surficial sediment components: new evidence for less importance of clay minerals. J Hazard Mater, Vol. 189, pp. 719-723.
[9] Bajda, T. and Klapyta, K., 2013, Adsorption of chromate from aqueous solutions by HDTMA-modified clinoptilolite, glauconite and montmorillonite. Appl Clay Sci, Vol. 86, pp. 169-173.
[10] Hegazi, H., 2013, Removal of heavy metals from wastewater using agricultural and industrial wastes as adsorbents. HBRC Journal, Vol. 9, pp. 276-282.
[11] Clive, Mitchel. 2000. Industrial Mineral Resources of Zambia.
[12] Haidong, Hu and Ke, Xu. 2020, High-Risk Pollutants in Wastewater, Elsevier, pp. 169-207.
[13] Ugwu, I. M and Igbokwe, O. 2019, Sorption of Heavy Metals on Clay Minerals and Oxides: A Review. In: Advanced Sorption Process Applications. pp. 1-4.
[14] Phenny Mwaanga, Mathews Silondwa, George Kasali, Paul M. Banda, 2019, Preliminary review of mine air pollution in Zambia. Heliyon.5(9).
[15] Mudenda, Lee. 2018. Assessment of Water pollution arising from copper mining in Zambia: a case study of Munkulungwe stream in Ndola, Copperbelt province. Cape Town: University of Cape Town (UCT).
[16] Ikenaka, Yoshinori & Nakayama, Shouta & Muzandu, Kaampwe & Choongo, Kennedy & Teraoka, Hiroki & Mizuno, Naoharu & Ishizuka, Mayumi. (2010). Heavy Metal Contamination of Soil and Sediment in Zambia. African Journal of Environmental Science and Technology. 4. 729-739. 10.4314/ajest.v4i11.71339.
[17] Obayomia, K and Autab, M. 11, 2019, Development of microporous activated Aloji clay for adsorption of lead (II) ion from aqueous solution. Heliyon, Vol. 5, pp. 27-99.
[18] Univeristy, James Cook. Element-to-stoichiometric oxide conversion factors. [Online] 2020. [Cited: April 3, 2021.] t: https://www.jcu.edu.au/advanced-analytical-centre/resources/element-to-stoichiometric-oxideconversion-factors.
[19] Krachler, Michael & Mohl, Carola & Emons, Hendrik & Shotyk, William. (2002). Influence of digestion procedures on the determination of rare earth elements in peat and plant samples by USN-ICP-MS. Journal of Analytical Atomic Spectrometry. 17. 10.1039/B200780K.
[20] Novikova, L., Belchinskaya, L., 2016, ‘Adsorption of Industrial Pollutants by Natural and Modified Aluminosilicates’, in G. M. d. Nascimento (ed.), Clays, Clay Minerals and Ceramic Materials Based on Clay Minerals, Intech Open, London. 10.5772/61678.
[21] Ahmed Z. Khalifa, Özlem Cizer, Yiannis Pontikes, Andrew Heath, Pascaline Patureau, Susan A. Bernal, Alastair T.M. Marsh, 2020, Advances in alkali-activation of clay minerals. Advances in alkali-activation of clay minerals, Vol. 132, ISSN 0008-8846.
[22] Shuang Xie, Zhang Wen, Hongbin Zhan, Menggui Jin.2018, An Experimental Study on the Adsorption and Desorption of Cu (II) in Silty Clay. Geofluids, Vol. 4, pp. 1-12.
[23] Alandis, N. & Mekhamer, Waffa & Aldayel, Omar & Hefne, Jameel & Alam, Manawwer. (2019). Adsorptive Applications of Montmorillonite Clay for the Removal of Ag(I) and Cu (II) from Aqueous Medium. Journal of Chemistry. 2019. 1-7. 10.1155/2019/7129014.
[24] Abbar, Bouamama & Alem, Abdellah & Marcotte, Stéphane & Anne, Pantet & Ahfir, Nasre-Dine & Bizet, Laurent & Duriatti, Davy. (2017). Experimental investigation on removal of heavy metals (Cu 2+, Pb 2+, and Zn 2+) from aqueous solution by flax fibres. Process Safety and Environmental Protection. 109. 10.1016/j.psep.2017.05.012.
Viewed PDF 1394 55 -
 Gadolinium Distribution in the Kidney, Liver, and Heart of Wistar Rats after Administration of Gadolinium-Based Contrast AgentsAuthor: Oluwafemi Olumide EgbeyemiDOI: 10.21522/TIJAR.2014.09.04.Art010
Gadolinium Distribution in the Kidney, Liver, and Heart of Wistar Rats after Administration of Gadolinium-Based Contrast AgentsAuthor: Oluwafemi Olumide EgbeyemiDOI: 10.21522/TIJAR.2014.09.04.Art010Gadolinium Distribution in the Kidney, Liver, and Heart of Wistar Rats after Administration of Gadolinium-Based Contrast Agents
Abstract:
Magnetic resonance imaging (MRI) is an established non-invasive and non-destructive medical imaging modality for the assessment of various organ systems in the human body. Gadolinium-Based Contrast Agent (GBCA) enhanced and improved images from MRI and was believed to be entirely excreted through urine in normal kidney function within 24 hours after injection. Previous studies identified gadolinium accumulations in the brain, bones, and skin of animals. This study evaluated gadolinium retention in normal kidneys, Liver, and heart of Wistar rats after administration of GBCAs in male Wistar rats. Twenty-five male Wistar rats of ages ≥ 5 weeks or ≤ 6 weeks in 4 experimental and 1 control groups were studied. Ethical considerations were obtained from the Institutional Review Board (IRB) of the Nigerian Institute of Medical Research (NIMR), Nigeria. Samples in experimental groups each administered 2.5 mls of 4 different GBCAs, and the control group same per day of saline intravenously through the lateral tail for five days a week and continued for 4 weeks. The kidney, Liver, and Heart tissues of these samples were harvested 4 weeks after the last injection and sent for spectrometry evaluation. Samples in the control group had no gadolinium accumulation. Groups administered gadopentetate dimeglumine, and gadodiamide had greater cardiac metrics (0.397 and 0.390). The higher renal metric was experienced by samples that received dotarem and cyclolux (0.397 and 0.377), though the sample exposed to cyclolux reported more Liver metric (0.407) than other concentrations. Wistar rats’ Kidneys, Liver, and Heart retained gadolinium weeks after injection of GBCAs.
Keywords: Dotarem and Cyclolux, Gadolinium, Gadodiamide, Gadopentetate dimenglumine, Magnetic resonance imaging.Gadolinium Distribution in the Kidney, Liver, and Heart of Wistar Rats after Administration of Gadolinium-Based Contrast Agents
References:
[1] Yadollahpour, A., Venkateshwarlu, G., 2016, Applications of gadolinium nanoparticles in magnetic resonance imaging: A review on recent advances in clinical imaging. International Journal of Pharmacology and Technology, 8: 11379-11393.
[2] Perazella, M., 2009, Status of gadolinium toxicity in patients with kidney disease. Clinical Journal of American Society of Nephrology, 4,461-469.
[3] Ramalho, J., Semelka, R.C., Ramalho, M., Nunes, R., Obaidy, M.A.I., Castillo, M., 2016, Gadolinium-based Contrast Agent Accumulation and Toxicity: An Update. American Journal of Neuroradiology. 37(7),1192-1198.
[4] Leyba, K.., Wagner, B., 2019, Gadolinium-based contrast agents: why nephrologists need to be concerned. Current Opinion in Nephrology and Hypertension, 28(2),154–162. https://doi.org/10.1097/MNH.0000000000000475
[5] Rogosnitzky, M., Branch, S., 2016, Gadolinium-based contrast agent toxicity: a review of known and proposed mechanisms. Biometals 29,365–376 https://doi.org/10.1007/s10534-016-9931-7.
[6] Quattrocchi, C. C., van der Molen, A. J. ,2017, Gadolinium Retention in the Body and Brain: Is It Time for an International Joint Research Effort?. Radiology, 282(1),12–16. https://doi.org/10.1148/radiol.2016161626.
[7] Gale, E. M., Caravan, P., 2018, Gadolinium-Free Contrast Agents for Magnetic Resonance Imaging of the Central Nervous System. ACS Chemical Neuroscience, 9(3), 395–397. https://doi.org/10.1021/acschemneuro.8b00044.
[8] Kanda, T., Fukusato, T., Matsuda, M., Toyoda, K., Oba, H., Kotoku, J., Haruyama, T., Kitajima, K., Furui, S., 2015a, Gadolinium-based Contrast Agent Accumulates in the Brain Even in Subjects without Severe Renal Dysfunction: Evaluation of Autopsy Brain Specimens with Inductively Coupled Plasma Mass Spectroscopy. Radiology, 276(1), 228–232. https://doi.org/10.1148/radiol.2015142690.
[9] Radbruch, A., Weberling, L.D., Kieslich, P.J., Eidel, O., Burth, S., Kickingereder, P., Heiland, S., Wick, W., Schlemmer, H., Bendszus., 2015, Gadolinium retention in the dentate nucleus and globus pallidus is dependent on the class of contrast agent. Radiology 275:783–791.
[10] Kanda, T., Ishii, K., Kawaguchi, H., Kitajima, K., Takenaka, D., 2014, High signal intensity in the dentate nucleus and globus pallidus on unenhanced T1-weighted MR images: relationship with increasing cumulative dose of a gadolinium-based contrast material. Radiology, 270(3),834–841. https://doi.org/10.1148/radiol.13131669.
[11] Khairinisa, M. A., Takatsuru, Y., Amano, I., Erdene, K., Nakajima, T., Kameo, S., Koyama, H., Tsushima, Y., Koibuchi, N., 2018, The Effect of Perinatal Gadolinium-Based Contrast Agents on Adult Mice Behavior. Investigative Radiology, 53(2), 110–118.
[12] Pass, D., Freeth, G.,1993, The rat. Anzccart News. 6,1–4.
[13] Quinn, R., 2005, Comparing rats to human’s age: How old is my rat in people years? Nutrition. 21:775–7.
[14] Sengupta, P., 2012, A Scientific Review of Age Determination for a Laboratory Rat: How old is it in comparison with Human age? Biomedical International, 2,81–9.
[15] Mugikura, S., Takase, K., 2017, Fear of linear gadolinium-based contrast agents and the Japanese radiologist’s choice. Japanese Journal of Radiology. 35(11), 695–696.
[16] Davidson, M. K., Lindsey, J. R., Davis, J. K., 1987, Requirements and selection of an animal model. Israel Journal of Medical Sciences, 23(6), 551–555.
[17] Sengupta, P., 2013, The Laboratory Rat: Relating Its Age with Human’s. International Journal of Preventive Medicine, 4(6), 624–630.
[18] Shirani, F., Teimoori, A., Rashno, M., Latifi, S. M., Karandish, M., 2017, Using rats as a research model to investigate the effect of human adenovirus 36 on weight gain. Arya Atherosclerosis, 13(4), 167–171.
[19] Lohrke, J., Frisk, A. L., Frenzel, T., Schöckel, L., Rosenbruch, M., Jost, G., Lenhard, D. C., Sieber, M. A., Nischwitz, V., Küppers, A., Pietsch, H.,2017, Histology and Gadolinium Distribution in the Rodent Brain After the Administration of Cumulative High Doses of Linear and Macrocyclic Gadolinium-Based Contrast Agents. Investigative Radiology, 52(6), 324–333. https://doi.org/10.1097/RLI.0000000000000344.
[20] Parasuraman, S., 2011, Toxicological screening. Journal of Pharmacology and Pharmacotherapy, 2(2),74-79. doi: 10.4103/0976-500X.81895
[21] Kanda, T., Osawa, M., Oba, H., Toyoda, K., Kotoku, J., Haruyama, T., Takeshita, K., & Furui, S. (2015b). High Signal Intensity in Dentate Nucleus on Unenhanced T1-weighted MR Images: Association with Linear versus Macrocyclic Gadolinium Chelate Administration. Radiology, 275(3), 803–809. https://doi.org/10.1148/radiol.14140364.
[22] McDonald, R. J., McDonald, J. S., Kallmes, D. F., Jentoft, M. E., Paolini, M. A., Murray, D. L., Williamson, E. E., Eckel, L. J., 2017a, Gadolinium Deposition in Human Brain Tissues after Contrast-enhanced MR Imaging in Adult Patients without Intracranial Abnormalities. Radiology, 285(2), 546–554. https://doi.org/10.1148/radiol.2017161595.
[23] Murata, N., Gonzalez-Cuyar, L.F., Murata, K., Fligner, C., Dills, R., Hippe, D., Maravilla, K.R., 2016, Macrocyclic and other nongroups 1 gadolinium contrast agents deposit low levels of gadolinium in brain and bone tissue: preliminary results from 9 patients with normal renal function. Investigative Radiology. doi:10.1097/rli.0000000000000252.
[24] Wáng, Y. X., Schroeder, J., Siegmund, H., Idée, J. M., Fretellier, N., Jestin-Mayer, G., Factor, C., Deng, M., Kang, W., Morcos, S. K., 2015, Total gadolinium tissue deposition and skin structural findings following the administration of structurally different gadolinium chelates in healthy and ovariectomized female rats. Quantitative Imaging in Medicine and Surgery,5(4),534–545. https://doi.org/10.3978/j.issn.2223.4292.2015.05.03.
[25] Gibby, W.A., Gibby, K.A., Gibby, W.A., 2004, Comparison of Gd DTPA-BMA (Omniscan) versus Gd HP-DO3A (ProHance) retention in human bone tissue by inductively coupled plasma atomic emission 2 eespectroscopy. Investigative Radiology, 39,138–142.
Viewed PDF 923 16 -
 Impact of Training on Virtual Instructional Leadership in Jamaica During the Covid-19 PandemicAuthor: Karla Boswell-LewisDOI: 10.21522/TIJAR.2014.09.04.Art011
Impact of Training on Virtual Instructional Leadership in Jamaica During the Covid-19 PandemicAuthor: Karla Boswell-LewisDOI: 10.21522/TIJAR.2014.09.04.Art011Impact of Training on Virtual Instructional Leadership in Jamaica During the Covid-19 Pandemic
Abstract:
Globally, instructional leadership is critical to the educational reform agenda of schools. The purpose of this study was to ascertain educators’ perceived effectiveness of virtual instructional leadership training on school leadership in Jamaica during the Covid-19 pandemic. It also sought to examine if there are statistically significant differences in the scores of the composite dependent (instructional resource provider; maintain visible presence; professional development; maximize instructional time; monitoring students’ progress; feedback on teaching learning; curriculum implementation) based on school level, capacity in which educators work and gender. The instrument used to collect data for this study was adopted by the researcher. The instrument was converted into a Google Form to make it easier for distribution and data collection. The authors reported that the instrument achieved reliability of Cronbach Alpha amongst the tenets ranging from 0.87-0.80. Overall, the instruments’ reliability statistic is. 95. The data was analyzed using weighted means and MANOVA. The results revealed that the educators rated four dimensions of the instructional leadership scale High, maintaining visible presence; professional development; feedback on teaching learning, and curriculum implementation. In addition, instructional resource provider; maximize instructional time, and monitoring students’ progress were rated moderate. Another finding of this study is that there is no statistically significant difference in the scores of the composite dependent variables based on school level, capacity served, and gender. Another implication of the finding of this research is that principals must ensure that instructional time is maximized by managing and planning for instruction, assessment, and other teacher-student activities while developing strong relationships with teachers and students by rewarding them for achieving targets.Keywords: Covid 19 Pandemic, Curriculum implementation, Feedback on teaching and learning, Instructional resource provider, Maintain visible presence, Maximize instructional time, Monitoring students’ progress, Professional development, Virtual instructional leadership.Impact of Training on Virtual Instructional Leadership in Jamaica During the Covid-19 Pandemic
References:
[1] Waters, J. T., Marzano, R. J., & McNulty, B. A. (2003). Balanced leadership: What 30 of research tells us about the effect of leadership on student achievement. Aurora, CO: Mid-Continent Research for Education and Learning.
[2] Krug, S. E. (1992). Instructional leadership: A constructivist perspective. Educational Administration Quarterly, 28(3), 430–443.
[3] Smith, W. & Andrews, R. (1989). Instructional leadership: How principals make a difference. Alexandria, VA: Association for Supervision and Curriculum Development.
[4] Andrews, R., & Soder, R. (1987). Principal leadership and student achievement. Educational Leadership, 44, (6), 9-11.
[5] Whitaker, B. (1997). Instructional leadership and principal visibility. The Clearinghouse, 70(3), 155–156.
[6] Blase, J., & Blase, J. (2000). Effective instructional leadership: Teachers’ perspectives on how principals promote teaching and learning in schools. Journal of Educational Administration, 38(2), 130–141.
[7] Southworth, G. (2002). Instructional leadership in schools: Reflections and empirical evidence. School Leadership & Management, 22(1), 73–91.
[8] Hallinger, P. (2011). Leadership for learning: Lessons from 40 years of empirical research. Journal of Educational Administration, 49(2), 125–142.
[9] Jenkins, B. (2009). What it takes to be an instructional leader. Principal, 88 (3), 34-37.
[10] Zepeda, S. J. (2003). Instructional Supervision: Applying Tools and Concepts. Larchmont, NY: Eye on Education. Zepeda, S. J. (2004). Instructional Leadership for School Improvement. NY: Eye on Education.
[11] Glickman, C., Gordon, S., & Ross-Gordon, J. (2001). Supervision and instructional leadership: A
developmental approach (5th ed.). Needham Heights, MA: Allyn and Bacon.[12] Khaki, J. E. A. (2009). Leading leaders: A school leadership development experience in Pakistan. The Sindh University Journal of Education, 38, 18–32.
[13] Zepeda, S. J. (2014). The principal as instructional leader: A handbook for supervisors. New York: Routledge.
[14] Yunas, M., & Iqbal, M. (2013). Dimensions of instructional leadership role of principal. Interdisciplinary Journal of Contemporary Research in Business, 4(10), 629–637.
[15] Issa, Y. (2012) Institutional factors influencing head teachers’ instructional supervision practices in secondary schools in Mandera East district, Kenya. Working Paper, University of Nairobi.
[16] Goldring, E., Huff, J., May, H. and Camburn, E. (2008). School context and individual characteristics: what influences principal practice? Journal of Educational Administration, 46(3), 332-352.
[17] Hallinger, P. (2003). Leading educational change: Reflections on the practice of instructional and transformational leadership. Cambridge Journal of Education, 33(3), 329–352.
[18] Kis, A & Konan, N. (2014) A Meta-Analysis of Gender Differences in Terms of Teacher Views on the Instructional Leadership Behavior of Principals. Educational Sciences: Theory and Practice, 14(6), 2139-2145.
[19] Hallinger, P., Dongyu, L., and Wang, W. (2016) Gender Differences in Instructional Leadership: A Meta-Analytic Review of Studies Using the Principal Instructional Management Rating Scale. Educational Administration Quarterly, 52(4), 567-601.
[20] Eagly A. H., Carli L. L. (2003). The female leadership advantage: An evaluation of the evidence. Leadership Quarterly, 14, 807-834.
Viewed PDF 1141 29 -
 Drivers of Covid-19 Vaccine Hesitancy in Southern NigeriaAuthor: Adeniyi, D.S.DOI: 10.21522/TIJAR.2014.09.04.Art012
Drivers of Covid-19 Vaccine Hesitancy in Southern NigeriaAuthor: Adeniyi, D.S.DOI: 10.21522/TIJAR.2014.09.04.Art012Drivers of Covid-19 Vaccine Hesitancy in Southern Nigeria
Abstract:
Hesitancy against the Covid-19 vaccines cuts across all nations of the world, but this may not be unconnected to the trolls of misinformation and politicization surrounding the Covid-19 science. Findings from this study reveal that 84.7% of the study population lacks adequate information about the Covid-19 vaccines. 50% of the study population is skeptical about the safety of the Covid-19 vaccines. 100% of the study participants make use of the internet and other social media platforms for their sources of news information. 55.3% of the study population would follow the advice of their healthcare workers pertaining to the Covid-19 vaccines. 26.7% of the study population would listen to instructions given by their parents pertaining to the Covid-19 vaccines, while 20.7% of the study population would follow the guidance of their religious leaders respectively. Thus, the main drivers of Covid-19 vaccine hesitancy in Southern Nigeria are a lack of correct information about the Covid-19 vaccines, misinformation on social media platforms, resistance from religious leaders and parents, and a lack of support for the Covid-19 vaccine uptake on the part of healthcare workers. It is, therefore, imperative that in order to overcome the present challenge, the population of Southern Nigeria should be educated on Covid-19 related subjects and engaged with health promotion initiatives. While accepting the Covid-19 vaccines by the hesitant populations in Southern Nigeria is largely dependent upon the attitudes and influences of religious leaders, parents, and healthcare workers, a much larger study is required to fully establish the ramifications of these important findings.
Keywords: Covid-19, Healthcare Workers, Immunization, SARS-CoV-2, Southern Nigeria, Vaccine Hesitancy.Drivers of Covid-19 Vaccine Hesitancy in Southern Nigeria
References:
[1] Abdulkarim, A. A., Ibrahim, R. M., Fawi, A. O., Adebayo, O. A., & Johnson, A. W. B. R. (2011). Vaccines and immunization: The past, present, and future in Nigeria. Nigerian Journal of Pediatrics, 38(4), 186-194.
[2] Idris, A. J. (2014). Health Personnel and the Success of Immunization in Nigeria: A Study of Selected Local Government Areas in Kaduna State. Review of Public Administration and Management, 2(6).
[3] Cooper, S., Betsch, C., Sambala, E. Z., Mchiza, N., & Wiysonge, C. S. (2018). Vaccine hesitancy–a potential threat to the achievements of vaccination programmes in Africa. Human vaccines & immunotherapeutics, 14(10), 2355-2357.
[4] Rappuoli, R. (2014). Vaccines: science, health, longevity, and wealth. Proceedings of the National Academy of Sciences, 111(34), 12282-12282.
[5] Bolsen, T., & Palm, R. (2022). Politicization and Covid-19 vaccine resistance in the US. Progress in molecular biology and translational science, 188(1), 81.
[6] Cucinotta, D., & Vanelli, M. (2020). WHO declares Covid-19 a pandemic. Acta Bio Medica: Atenei Parmensis, 91(1), 157.
[7] Altindis, E. (2022). Inequitable Covid-19 vaccine distribution and intellectual property rights prolong the pandemic. Expert review of vaccines, 21(4), 427-430.
[8] Tao, K., Tzou, P. L., Nouhin, J., Gupta, R. K., de Oliveira, T., Kosakovsky Pond, S. L., & Shafer, R. W. (2021). The biological and clinical significance of emerging SARS-CoV-2 variants. Nature Reviews Genetics, 1-17.
[9] Sallam, M. (2021). Covid-19 vaccine hesitancy worldwide: a concise systematic review of vaccine acceptance rates. Vaccines, 9(2), 160.
[10] Farayibi, A., & Asongu, S. (2020). The economic consequences of the Covid-19 pandemic in Nigeria. European Xtra mile Centre of African Studies, WP/20/042 (2020).
[11] Ghatak, N., Marzo, R. R., Saleem, S. M., Sharma, N., Bhattacharya, S., & Singh, A. (2020). Impact on routine immunization services during the lockdown period in India: Implications and future recommendations. European Journal of Molecular and Clinical Medicine, 35-40.
[12] Hassan, W., Kazmi, S. K., Tahir, M. J., Ullah, I., Royan, H. A., Fahriani, M., & Rosa, S. G. (2021). Global acceptance and hesitancy of Covid-19 vaccination: A narrative review. Narra J, 1(3).
[13] Reiter, P. L., Pennell, M. L., & Katz, M. L. (2020). Acceptability of a Covid-19 vaccine among adults in the United States: How many people would get vaccinated? Vaccine, 38(42), 6500-6507.
[14] Bell, S., Clarke, R., Mounier-Jack, S., Walker, J. L., & Paterson, P. (2020). Parents’ and guardians’ views on the acceptability of a future Covid-19 vaccine: A multi-methods study in England. Vaccine, 38(49), 7789-7798.
[15] Machingaidze, S., & Wiysonge, C. S. (2021). Understanding Covid-19 vaccine hesitancy. Nature Medicine, 27(8), 1338-1339.
[16] Adebisi, Y. A., Alaran, A. J., Bolarinwa, O. A., Akande-Sholabi, W., & Lucero-Prisno, D. E. (2021). When it is available, will we take it? Public perception of hypothetical Covid-19 vaccine in Nigeria. medRxiv.
[17] Eze, U. A., Ndoh, K. I., Ibisola, B. A., Onwuliri, C. D., Osiyemi, A., Ude, N., ... & Abdullahi, A. (2021). Determinants for acceptance of Covid-19 vaccine in Nigeria. Cureus, 13(11).
[18] MacDonald, N. E. (2015). Vaccine hesitancy: Definition, scope, and determinants. Vaccine, 33(34), 4161-4164.
[19] Murphy, J., Vallières, F., Bentall, R. P., Shevlin, M., McBride, O., Hartman, T. K., & Hyland, P. (2021). Psychological characteristics associated with Covid-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nature communications, 12(1), 1-15.
[20] King, W. C., Rubinstein, M., Reinhart, A., & Mejia, R. (2021). Time trends, factors associated with, and reasons for Covid-19 vaccine hesitancy: A massive online survey of US adults from January-May 2021. PloS one, 16(12), e0260731.
[21] Agha, S.; Chine, A.; Lalika, M.; Pandey, S.; Seth, A.; Wiyeh, A.; Seng, A.; Rao, N.; Badshah, A. Drivers of Covid-19 Vaccine Uptake amongst Healthcare Workers (HCWs) in Nigeria. Vaccines 2021, 9, 1162 https://doi.org/10.3390/vaccines9101162.
[22] Orji, P. C., Allagoa, D. O., Obagah, L., Tekenah, E. S., Ohaeri, O. S., & Atemie, G. (2021). Perception about Covid-19 vaccine among patients at the Federal Medical Centre, Yenagoa, South-South Nigeria. Int J Res Med Sci, 9(5), 1281-1287.
[23] Hussin, H. B., Marzo, R. R., Mamat, N. B., Safee, N. F. B., Omar, N. B., & Yin, T. S. (2020). The barriers to child immunization completion among parents in the community health centre, Johor Bahru. Article | IMSEAR | ID: sea-215923.
[24] Kaufman, J., Tuckerman, J., Bonner, C., Durrheim, D. N., Costa, D., Trevena, L., ... & Danchin, M. (2021). Parent-level barriers to uptake of childhood vaccination: a global overview of systematic reviews. BMJ global health, 6(9), e006860.
[25] Bangura, J. B., Xiao, S., Qiu, D., Ouyang, F., & Chen, L. (2020). Barriers to childhood immunization in sub-Saharan Africa: a systematic review. BMC Public Health, 20(1), 1-15.
[26] Marzo, R. R., Su, T. T., Ismail, R., Htay, M. N. N., Essar, M. Y., Chauhan, S., ... & Lin, Y. (2022). Digital health literacy for Covid-19 vaccination and intention to be immunized: A cross-sectional multi-country study among the general adult population. Frontiers in Public Health, 10.
[27] Lockyer, B., Islam, S., Rahman, A., Dickerson, J., Pickett, K., Sheldon, T., ... & Bradford Institute for Health Research Covid‐19 Scientific Advisory Group. (2021). Understanding Covid‐19 misinformation and vaccine hesitancy in context: Findings from a qualitative study involving citizens in Bradford, UK. Health Expectations, 24(4), 1158-1167.
[28] Kricorian, K., Civen, R., & Equils, O. (2022). Covid-19 vaccine hesitancy: Misinformation and perceptions of vaccine safety. Human Vaccines & Immuno therapeutics, 18(1), 1950504.
[29] Kanozia, R., & Arya, R. (2021). “Fake news”, religion, and Covid-19 vaccine hesitancy in India, Pakistan, and Bangladesh. Media Asia, 48(4), 313-321.
[30] Marzo, R. R., Ahmad, A., Abid, K., Khatiwada, A. P., Ahmed, A., Kyaw, T. M., ... & Shrestha, S. (2022). Factors influencing the acceptability of Covid-19 vaccination: a cross-sectional study from Malaysia. Vacunas (English Edition), 23, 33-40.
[31] Marzo, R. R., Ahmad, A., Islam, M. S., Essar, M. Y., Heidler, P., King, I., ... & Yi, S. (2022). Perceived Covid-19 vaccine effectiveness, acceptance, and drivers of vaccination decision-making among the general adult population: A global survey of 20 countries. PLoS neglected tropical diseases, 16(1), e0010103.
[32] Marzo, R. R., Sami, W., Alam, M., Acharya, S., Jermsittiparsert, K., Songwathana, K., ... & Yi, S. (2022). Hesitancy in Covid-19 vaccine uptake and its associated factors among the general adult population: a cross-sectional study in six Southeast Asian countries. Tropical Medicine and Health, 50(1), 1-10.
[33] Elsayed, M., El-Abasiri, R. A., Dardeer, K. T., Kamal, M. A., Htay, M. N. N., Abler, B., & Marzo, R. R. (2021). Factors influencing decision making regarding the acceptance of the Covid-19 vaccination in Egypt: A cross-sectional study in an urban, well-educated sample. Vaccines, 10(1), 20.
[34] Brackstone, K., Marzo, R. R., Bahari, R., Head, M. G., Patalinghug, M. E., & Su, T. T. (2022). Covid-19 Vaccine Hesitancy and Confidence in the Philippines and Malaysia: A Cross-sectional Study of Sociodemographic Factors and Information-Seeking. medRxiv.
Viewed PDF 1053 17 -
 Attitudes and Intentions of Health Personnel towards Covid-19 Vaccination in Kaziba Health ZoneAuthor: Bontango Kweme FredericDOI: 10.21522/TIJAR.2014.09.04.Art013
Attitudes and Intentions of Health Personnel towards Covid-19 Vaccination in Kaziba Health ZoneAuthor: Bontango Kweme FredericDOI: 10.21522/TIJAR.2014.09.04.Art013Attitudes and Intentions of Health Personnel towards Covid-19 Vaccination in Kaziba Health Zone
Abstract:
Introduction: SARS-CoV-2 is a virus of the coronavidae family and of the beta coronavirus group, such as those responsible for SARS and MERS. This Covid-19 is more contagious than SARS and MERS but with a lower death rate. Covid-19 vaccine is a pharmaceutical tool to control the transmission of Covid-19 among the health personnel and the general population. The acceptance of Covid-19 vaccination remains reluctant among the health personnel. The purposes of this study are to determine the intentions and attitudes of health personnel vis-à-vis to Covid-19 vaccination and, to determine the reasons for accepting and refusing Covid-19 vaccination among health personnel in Kaziba Health Zone from 15 to 28 July 2021. Material and methods: our study was descriptive retrospective cross-sectional study. A random sampling method was carried out to collect the data through survey questionnaire with 102 health personnel. The data was analyzed with SPSS and Chi-square test was carried out. Results: the intentions and attitudes of the health personnel vis-à-vis to Covid-19 vaccination was (31.4%), and the participants who declared the mandatory Covid-19 vaccination was 31.4%. The health personnel who accepted the covid-19 vaccine were 21.6%, however, those who refused was 45.1%. Conclusion: health personnel do not have acceptable intentions and attitudes towards Covid-19 vaccination. Only nurses and midwives, physicians and healthcare assistance staff were agreeable to Covid-19 vaccination to control the pandemic. Lack of information was the main refusal reason for Covid-19 vaccination. The health personnel were not willingly too mandatory Covid-19 vaccination.
Keywords: Attitudes, Covid-19, Health personnel, Intentions, Kaziba, SARS-CoV-2, Vaccination.Attitudes and Intentions of Health Personnel towards Covid-19 Vaccination in Kaziba Health Zone
References:
[1] Banerjee, A., Kulcsar, K., Misra, V., Frieman, M., & Mossman, K., 2019, Bats and Coronaviruses. Viruses, 11(1), 41. https://doi.org/10.3390/v11010041.
[2] WHO. (2020, February 12). Covid-19 Public Health Emergency of International Concern (PHEIC) Global Research and Innovation Forum. Retrieved August 9, 2021, from https://www.who.int/publications/m/item/covid-19-public-health-emergency-of-international-concern-(pheic)-global-research-and-innovation-forum.
[3] CDC. (2021, August 17). Benefits of Getting a Covid-19 Vaccine. Centers for Disease Control and Prevention. Retrieved September 9, 2021, from https://www.cdc.gov/coronavirus/2019-ncov/vaccines/vaccine-benefits.html.
[4] Yang, J., Marziano, V., Deng, X., Guzzetta, G., Zhang, J., Trentini, F., Cai, J., Poletti, P., Zheng, W., Wang, W., Wu, Q., Zhao, Z., Dong, K., Zhong, G., Viboud, C., Merler, S., Ajelli, M., & Yu, H., 2021, To what extent do we need to rely on non-pharmaceutical interventions while Covid-19 vaccines roll out in 2021? MedRxiv, 12. https://doi.org/10.1101/2021.02.03.21251108.
[5] Wang, B., & Ping, Y., 2022, A comparative analysis of Covid-19 vaccination certificates in 12 countries/regions around the world: Rationalizing health policies for international travel and domestic social activities during the pandemic. Health Policy, 126(8), 755–762. https://doi.org/10.1016/j.healthpol.2022.05.016.
[6] WHO. (2021, April 19). Statement on the seventh meeting of the International Health Regulations (2005) Emergency Committee regarding the coronavirus disease (Covid-19) pandemic. Retrieved August 27, 2021, from https://www.who.int/news/item/19-04-2021-statement-on-the-seventh-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-coronavirus-disease-(covid-19)-pandemic.
[7] WHO. (2020, November 13). Feuille de route du SAGE de l’OMS pour l’établissement des priorités concernant l’utilisation des vaccins anti-Covid-19 dans un contexte d’approvisionnement limité. Retrieved August 31, 2021, from https://www.who.int/fr/publications/m/item/who-sage-roadmap-for-prioritizing-uses-of-covid-19-vaccines-in-the-context-of-limited-supply.
[8] Africa Centres for Disease Control and Prevention. (2021, August 24). Concerns about Capacity and Capability of Africa’s Public Health Institutions. Retrieved 21–08-30, from https://africacdc.org/.
[9] WHO. (2020a, June 29). Chronologie de l’action de l’OMS face à la Covid-19. Retrieved August 15, 2021, from https://www.who.int/fr/news/item/29-06-2020-covidtimeline.
[10] Voysey, M., Costa Clemens, S. A., Madhi, S. A., Weckx, L. Y., Folegatti, P. M., Aley, P. K., Angus, B., Baillie, V. L., Barnabas, S. L., Bhorat, Q. E., Bibi, S., Briner, C., Cicconi, P., Clutterbuck, E. A., Collins, A. M., Cutland, C. L., Darton, T. C., Dheda, K., Dold, C, Zuidewind, P., 2021, Single-dose administration and the influence of the timing of the booster dose on immunogenicity and efficacy of ChAdOx1 nCoV-19 (AZD1222) vaccine: a pooled analysis of four randomized trials. The Lancet, 397(10277), 881–891. https://doi.org/10.1016/s0140-6736(21)00432-3.
[11] Chan, J. F. W., Lau, S. K. P., To, K. K. W., Cheng, V. C. C., Woo, P. C. Y., & Yuen, K. Y., 2015, Middle East Respiratory Syndrome Coronavirus: Another Zoonotic Betacoronavirus Causing SARS-Like Disease. Clinical Microbiology Reviews, 28(2), 465–522. https://doi.org/10.1128/cmr.00102-14.
[12] Shim, E., Tariq, A., Choi, W., Lee, Y., & Chowell, G., 2020, Transmission potential and severity of Covid-19 in South Korea. International Journal of Infectious Diseases, 93, 339–344. https://doi.org/10.1016/j.ijid.2020.03.031.
[13] Boseley, S., & Oltermann, P., 2020, Hopes rise for end of pandemic as Pfizer says vaccine has 90% efficacy. The Guardian. Retrieved July 31, 2021, from https://www.theguardian.com/world/2020/nov/09/covid-19-vaccine-candidate-effective-pfizer-biontech.
[14] Ledda, C., Costantino, C., Cuccia, M., Maltezou, H. C., & Rapisarda, V., 2021, Attitudes of Healthcare Personnel towards Vaccinations before and during the Covid-19 Pandemic. International Journal of Environmental Research and Public Health, 18(5), 2703. https://doi.org/10.3390/ijerph18052703.
[15] Detoc, M., Bruel, S., Frappe, P., Tardy, B., Botelho-Nevers, E., & Gagneux-Brunon, A., 2020, Intention to participate in a Covid-19 vaccine clinical trial and to get vaccinated against Covid-19 in France during the pandemic. Vaccine, 38(45), 7002–7006. https://doi.org/10.1016/j.vaccine.2020.09.041.
[16] Loomba, S., de Figueiredo, A., Piatek, S. J., de Graaf, K., & Larson, H. J., 2021, Measuring the impact of Covid-19 vaccine misinformation on vaccination intent in the UK and USA. Nature Human Behaviour, 5(3), 337–348. https://doi.org/10.1038/s41562-021-01056-1.
[17] Nachega, J. B., Sam-Agudu, N. A., Masekela, R., van der Zalm, M. M., Nsanzimana, S., Condo, J., Ntoumi, F., Rabie, H., Kruger, M., Wiysonge, C. S., Ditekemena, J. D., Chirimwami, R. B., Ntakwinja, M., Mukwege, D. M., Noormahomed, E., Paleker, M., Mahomed, H., Tamfum, J. J. M., Zumla, A., & Suleman, F., 2021, Addressing challenges to rolling out Covid-19 vaccines in African countries. The Lancet Global Health, 9(6), e746–e748. https://doi.org/10.1016/s2214-109x(21)00097-8.
[18] Riccò, M., Ferraro, P., Peruzzi, S., Balzarini, F., & Ranzieri, S., 2021, Mandate or Not Mandate: Knowledge, Attitudes, and Practices of Italian Occupational Physicians towards SARS-CoV-2 Immunization at the Beginning of Vaccination Campaign. Vaccines, 9(8), 1–16. https://doi.org/10.3390/vaccines9080889.
[19] Halbrook, M., Martin-Blais, R., Gray, A., Tobin, N. H., Ferbas, K. G., Aldrovandi, G. M., & Rimoin, A. W., 2021, Cross-sectional Assessment of Covid-19 Vaccine Acceptance among Health Care Workers in Los Angeles. Annals of Internal Medicine. https://doi.org/10.7326/m20-7580.
[20] Verger, P., Scronias, D., Dauby, N., Adedzi, K. A., Gobert, C., Bergeat, M., Gagneur, A., & Dubé, E., 2021, Attitudes of healthcare workers towards Covid-19 vaccination: a survey in France and French-speaking parts of Belgium and Canada, 2020. Eurosurveillance, 26(3). https://doi.org/10.2807/1560-7917.es.2021.26.3.2002047.
[21] Kose, S., Mandiracioglu, A., Sahin, S., Kaynar, T., Karbus, O., & Ozbel, Y., 2020, Vaccine hesitancy
of the Covid‐19 by health care personnel. International Journal of Clinical Practice, 75(5), 1–4. https://doi.org/10.1111/ijcp.13917.[22] Helmy, Y. A., Fawzy, M., Elaswad, A., Sobieh, A., Kenney, S. P., & Shehata, A. A., 2020, The Covid-19 Pandemic: A Comprehensive Review of Taxonomy, Genetics, Epidemiology, Diagnosis, Treatment, and Control. Journal of Clinical Medicine, 9(125), 22.
[23] Castaneda-Vasquez, D. E., & Ruiz-Padilla, J. P., 2021, Vaccine Hesitancy against SARS-CoV-2 in Health Personnel of Northeastern Mexico and Its Determinants. JOEM, 63(8), 4.
[24] Khamis, F., Badahdah, A., al Mahyijari, N., al Lawati, F., al Noamani, J., al Salmi, I., & al Bahrani, M., 2021, Attitudes towards Covid-19 Vaccine: A Survey of Health Care Workers in Oman. Journal of Epidemiology and Global Health, 12(1), 1–6. https://doi.org/10.1007/s44197-021-00018-0.
[25] Adane, M., Ademas, A., & Kloos, H., 2022, Knowledge, attitudes, and perceptions of Covid-19 vaccine and refusal to receive Covid-19 vaccine among healthcare workers in northeastern Ethiopia. BMC Public Health, 22(1), 1–12. https://doi.org/10.1186/s12889-021-12362-8.
Viewed PDF 945 14 -
 Access to Finance: Determinants and Limitations to the Demand Side of Finance for Liberia’s Rural MarketAuthor: Andy Saye GbatuDOI: 10.21522/TIJAR.2014.09.04.Art014
Access to Finance: Determinants and Limitations to the Demand Side of Finance for Liberia’s Rural MarketAuthor: Andy Saye GbatuDOI: 10.21522/TIJAR.2014.09.04.Art014Access to Finance: Determinants and Limitations to the Demand Side of Finance for Liberia’s Rural Market
Abstract:
This study reviews the theoretical literature regarding determinants and the limitations to the demand side of rural finance in Liberia with the coming into effect of the National Financial Inclusion Strategy (NFIS). The outcome of this study reveals that education, income level, households’ assets, and agriculture rank as the outstanding drivers of the demand for finance in Liberia’s rural market. Obviously, the demand for financial services in the rural market of Liberia is very high. However, the demand is limited by a litany of factors such as slow economic growth & lack of job opportunities, poor public infrastructure, structural unemployment, few diversification opportunities, seasonality in agriculture, imperfect information & supervision, and poor social protection and market failures. The keywords used by the author in this article encompass credit worthiness, information asymmetry, financial inclusion, pareto efficiency, poverty alleviation, and rural finance.
Keywords: Credit worthiness, Financial inclusion, Information asymmetry, Pareto efficiency, Poverty alleviation, Rural finance.Access to Finance: Determinants and Limitations to the Demand Side of Finance for Liberia’s Rural Market
References:
[1] World Bank Group. 2020. Liberia Digital Economy Assessment. Summary Report. Washington, DC: World Bank. License: Creative Commons Attribution CC BY 3.0 IGO.
[2] Fletcher Leadership Program in Financial Inclusion (FLPFI). Research Brief, Sept 10, 2020 https://sites.tufts.edu/flpfi/.
[3] Central Bank Liberia Annual Report. December 2021 https://www.cbl.org.lr/.
[4] World Bank Group. 2014. Global Financial Development Report 2014. Financial Inclusion. Washington, DC: World Bank. https://openknowledge.worldbank.org/handle/10986/16238.
[5] Morgan, P. J., Y. Zhang, and D. Kydyrbayev. 2018. Overview of Financial Inclusion, Regulation, Financial Literacy, and Education in Central Asia and South Caucasus. ADBI Working Paper 878. Tokyo: Asian Development Bank Institute. Available: https://www.adb.org/publications/financial-inclusion-regulation-literacy-education-centralasia-south-caucasus.
[6] Alliance for Financial Inclusion, 2010. The 2010 AFI survey report on financial inclusion policy in developing countries. Nua, Wattana, Bangkok 10110, Thailand. http://www.afi-global.org.
[7] Consultative Group to Assist the Poor, 2013. Financial Inclusion: Helping Countries Meet the Needs of the Under-Bank and the Under-Served. https://www.worldbank.org/en/results/2013/04/02/financial-inclusion-helping-countries-meet-the-needs-of-the-underbanked-and-underserved.
[8] ADBI Working Paper 591, September 2016 https://www.adb.org/sites/default/files/publication/190672/adbi-wp591.pdf.
[9] Pearce, D., Davis, J., Onumah, G., & Butterworth, R. (2004). Making rural finance count for the poor. Working paper. Agriculture and Natural Resources Team, Department for International Development (DFID).
[10] FinDev Gateway-Microfinance Gateway, 2013 https://www.findevgateway.org/organization/institute-microfinance.
[11] Brief History of Rural Finance.pd https://www.rfilc.org/wp-content/uploads/2020/08/1151419192777.
[12] Adams, D. W. (1998). The decline in debt directing: An unfinished agenda. Paper presented at the Second Annual Seminar on New Development Finance, Goethe University of Frankfurt am Main, Germany.
[13] Zeller, M., M. Sharma, C. Henry, and C. Lapenu. (2001). An operational tool for evaluating poverty outreach of development policies and projects. Discussion Paper No. 111, Food Consumption and Nutrition Division, International Food Policy Research Institute, Washington, D.C, June.
[14] Lorenzoni, G., & Guerrieri, V. (2011). Credit crises, precautionary savings, and the liquidity trap (NBER Working Paper No. 17583). doi:10.3386/w17583
[15] Eggertsson, G. B., & Krugman, P. (2012). Debt, deleveraging, and the liquidity trap: A Fisher-Minsky-Koo approach. The Quarterly Journal of Economics, 127(3), 1469–1513. https://doi.org/10.1093/qje/qjs023.
[16] Modigliani, F. (1986). Life cycle, individual thrift, and the wealth of nations. American Economic Review, 76(3), 297–313. Retrieved from http://www.jstor.org/stable/1813352.
[17] Barba, A., & Pivetti, M. (2009). Rising household debt: Its causes and macroeconomic implications-a long-period analysis. Cambridge Journal of Economics, 33(1), 113–137. doi:10.1093/cje/ben030.
[18] Lusardi, A., & Tufano, P. (2015). Debt literacy, financial experiences, and over-indebtedness. Journal of Pension Economics & Finance, 14(4), 332–368. doi:10.1017/s1474747215000232 Magri, S. (2002). Italian households.
[19] Del-Río, A., & Young, G. (2005). The determinants of unsecured borrowing: Evidence from the British Household Panel Survey (Bank of England Working Paper Series, p. 262). doi:10.2139/ssrn.824147.
[20] Fabbri, D., & Padula, M. (2004). Does poor legal enforcement make households credit-constrained? Journal of Banking & Finance, 28(10), 2369–2397. doi:10.1016/j. jbankfin.2003.09.009.
[21] Magri, S. (2002). Italian households’ debt: Determinants of demand and supply. Temi di discussione, 454. Retrieved from http://www.bancaditalia.it/pubblicazioni/temidisc%20%200454/tema_454_02.pdf.
[22] Yilmazer, T., & DeVaney, S. A. (2005). Household debt over the life cycle. Financial Services Review, 14(4), 285. Retrieved from http://ezproxy.um.edu.my:2048/login?url=http://search.proquest.com/docview/212005236?accountid=28930.
[23] Livingstone, S. M., & Lunt, P. K. (1992). Predicting personal debt and debt repayment: Psychological, social and economic determinants. Journal of Economic Psychology, 13(1), 111–134. doi:10.1016/0167-4870(92)90055-C.
[24] Togba, E. L. (2012). Microfinance and households’ access to credit: Evidence from Côte d’Ivoire. Structural Change and Economic Dynamics, 23(4), 473–486. https://doi.org/10.1016/j.strueco.2012.08.002.
[25] Crook, J. (2006). Household debt demand and supply: A cross-country comparison. In G. Bertola, R. Disney, & C. Grant (Eds.), The economics of consumer credit (pp. 63–92). Retrieved from https://books.google.com.my/books?id=X8ZaBJpRiTsC&lpg=PA63&ots=MdPS3H7xc&lr&pg=PA63#v=onepage&q&f=false.
[26] Petrides, M., & Karagrigoriou, A. (2008). Determinants of debt: An econometric analysis based on the cyprus survey of consumer finances. Financial Theory and Practice, 32(1), 45–64. Retrieved from http://hrcak.srce.hr/34904.
[27] Tudela, M., & Young, G. (2005). The determinants of household debt and balance sheets in the United Kingdom. Bank of England. Quarterly Bulletin, 45(3), 373. Retrieved from https://ezproxy.um.edu.my/docview/215017808?account%20id=28930.
[28] Kim, H., & DeVaney, S. A. (2001). The determinants of outstanding balances among credit card revolvers. Journal of Financial Counseling and Planning, 12(1), 67–9.
[29] Andrews, D., Sanchez, A. C., & Johansson, Å. (2011). Housing markets and structural policies in OECD countries (OECD Economic Department Working Papers, p. 836). doi:10.1787/5kgk8t2k9vf3-en.
[30] World Bank, August 2022. Liberia Rural Population- World Bank Data. Washington, DC: World Bank https://data.worldbank.org/indicator/SP.RUR.TOTL?locations=LR.
[31] Country Commercial-Guide: Liberia, August 3, 2022. https://www.trade.gov/country-commercial-guides/liberia-agricultural-sectors.
[32] Reference Module in Earth & Environmental Sciences, 2016 https://scitechconnect.elsevier.com/resources/reference-module-earth-sciences-environmental-systems/.
[33] Y. Wamah, personal communication, July 9, 2022.
[34] Liberia Unemployment Rate, 1960-2021. https://knoema.com.
[35] European Commission (2006), Employment in Rural Areas: Closing the Jobs Gap, Brussels. [Online] Available from: http://ec.europa.eu/agriculture/publi/reports/ruralemployment/sec1772_en.pdf.
[36] De Janvry, A., M. Fafchamps & E. Sadoulet (1991), “Peasant Household Behaviour with Missing Markets: Some Paradoxes Explained”, The Economic Journal, vol. 101, no. 409, pp. 1400-1417.
[37] Swinnen, J.F.M., L. Dries & K. Macours (2001), “Transition and Agricultural Labour.”, presented at the American Agricultural Economics Association Meeting, August 5-8, 2001, Chicago.
[38] Borjas, G.J. (2005), Labor Economics, McGraw Hill, New York.
[39] Juvančič, L. & E. Erjavec (2005), “Intertemporal Analysis of Employment Decisions on Agricultural Holdings in Slovenia”, Agricultural Economics, vol. 33, no. 2, pp. 153-161.
[40] Schnicke, H., K. Happe & C. Sahrbacher (2007), Structural Change and Farm Labour Adjustments in a Dualistic Farm Structure: A Simulation Study for the Region Nitra in Southwest Slovakia, IAMO Discussion Paper, Report number: 112. Leibniz Institute of Agricultural Development in Central and Eastern Europe.
[41] Davis, J. & D. Pearce (2001), The Non-agricultural Rural Sector in Central and Eastern Europe, Natural Resources Institute, Chatham, U.K.
[42] World Bank Group. 2012. Liberia - A Diagnostic of Social Protection. Washington, DC: World Bank. https://socialprotection.org/discover/publications/liberia-diagnostic-social-protection.
[43] ILO (2008). Report IV: Promotion of Rural Employment for Poverty Reduction. International Labour Conference, 97th Session, 2008. ILO, Geneva.
Viewed PDF 1314 60

